Abstract
Background and Aims
The most restrictive nonpharmaceutical interventions (NPIs) for controlling the spread of COVID‐19 are mandatory stay‐at‐home and business closures. Given the consequences of these policies, it is important to assess their effects. We evaluate the effects on epidemic case growth of more restrictive NPIs (mrNPIs), above and beyond those of less‐restrictive NPIs (lrNPIs).
Methods
We first estimate COVID‐19 case growth in relation to any NPI implementation in subnational regions of 10 countries: England, France, Germany, Iran, Italy, Netherlands, Spain, South Korea, Sweden and the United States. Using first‐difference models with fixed effects, we isolate the effects of mrNPIs by subtracting the combined effects of lrNPIs and epidemic dynamics from all NPIs. We use case growth in Sweden and South Korea, 2 countries that did not implement mandatory stay‐at‐home and business closures, as comparison countries for the other 8 countries (16 total comparisons).
Results
Implementing any NPIs was associated with significant reductions in case growth in 9 out of 10 study countries, including South Korea and Sweden that implemented only lrNPIs (Spain had a nonsignificant effect). After subtracting the epidemic and lrNPI effects, we find no clear, significant beneficial effect of mrNPIs on case growth in any country. In France, for example, the effect of mrNPIs was +7% (95% CI: −5%‐19%) when compared with Sweden and + 13% (−12%‐38%) when compared with South Korea (positive means pro‐contagion). The 95% confidence intervals excluded 30% declines in all 16 comparisons and 15% declines in 11/16 comparisons.
Conclusions
While small benefits cannot be excluded, we do not find significant benefits on case growth of more restrictive NPIs. Similar reductions in case growth may be achievable with less‐restrictive interventions.
1. INTRODUCTION
The spread of COVID‐19 has led to multiple policy responses that aim to reduce the transmission of the SARS‐CoV‐2. The principal goal of these so‐called nonpharmaceutical interventions (NPI) is to reduce transmission in the absence of pharmaceutical options in order to reduce resultant death, disease and health system overload. Some of the most restrictive NPI policies include mandatory stay‐at‐home and business closure orders (‘lockdowns’). The early adoption of these more restrictive nonpharmaceutical interventions (mrNPIs) in early 2020 was justified because of the rapid spread of the disease, overwhelmed health systems in some hard‐hit places and substantial uncertainty about the virus’ morbidity and mortality. 1
Because of the potential harmful health effects of mrNPI—including hunger, 2 opioid‐related overdoses, 3 missed vaccinations, 4 , 5 increase in non‐COVID diseases from missed health services, 6 , 7 , 8 , 9 domestic abuse, 10 mental health and suicidality, 11 , 12 and a host of economic consequences with health implications 13 , 14 —it is increasingly recognized that their postulated benefits deserve careful study. One approach to evaluating NPI benefits uses disease modelling approaches. One prominent modelling analysis estimated that, across Europe, mrNPIs accounted for 81% of the reduction in the effective reproduction number (), a measure of disease transmission. 15 However, in the absence of empirical assessment of the policies, their effects on reduced transmission are assumed rather than assessed. 16 , 17 That analysis attributes nearly all the reduction in transmission to the last intervention, whichever intervention happened to be last, complete lockdowns in France or banning of public events in Sweden. 16
Another, more empirically grounded approach to assessing NPI effects uses statistical regression models and exploits variation in the location and timing of NPI implementations to identify changes in epidemic spread following various policies. 18 These empirical studies find large reductions in the growth rate of new cases that are attributable to NPIs. An important challenge with these analyses is that they use pre‐policy growth rates to determine the ‘counterfactual’ trajectory of new cases—the expected case growth rate in the absence of NPIs. This is problematic because it is widely recognized that epidemic dynamics are time‐varying, and brakes on disease transmission occur without any interventions (through resolution of infections), as well as from behaviour changes unrelated to the NPIs. 19 , 20 These epidemic dynamics are demonstrated by an analysis showing that slowing of COVID‐19 epidemic growth was similar in many contexts, in a way that is more consistent with natural dynamics than policy prescriptions. 21
These challenges suggest that assessing the impact of mrNPIs is important, yet difficult. We propose an approach that balances the strengths of empirical analyses while taking into consideration underlying epidemic dynamics. We compare epidemic spread in places that implemented mrNPIs to counterfactuals that implemented only less‐restrictive NPIs (lrNPIs). In this way, it may be possible to isolate the role of mrNPIs, net of lrNPIs and epidemic dynamics.
Here, we use Sweden and South Korea as the counterfactuals to isolate the effects of mrNPIs in countries that implemented mrNPIs and lrNPIs. Unlike most of its neighbours that implemented mandatory stay‐at‐home and business closures, Sweden's approach in the early stages of the pandemic relied entirely on lrNPIs, including social distancing guidelines, discouraging of international and domestic travel, and a ban on large gatherings. 22 , 23 South Korea also did not implement mrNPIs. Its strategy relied on intensive investments in testing, contact tracing and isolation of infected cases and close contacts. 24 , 25
2. METHODS
We isolate the effect of more restrictive NPIs (mrNPIs) by comparing the combined effect size of all NPIs in 8 countries that implemented more restrictive policies (England, France, Germany, Iran, Italy, the Netherlands, Spain and the United States) with the effect size of all NPIs in the 2 countries that only implemented less‐restrictive NPIs (lrNPIs). In effect, we follow the general scheme:
We analyse only these countries because the analysis depends on subnational data, which were only available for those countries, as explained further below.
The conceptual model underlying this approach is that, prior to meaningful population immunity, individual behaviour is the primary driver of reductions in transmission rate, and that any NPI may provide a nudge towards individual behaviour change, with response rates that vary between individuals and over time. lrNPIs could have large anti‐contagion effects if individual behavioural response is large, in which case additional, more restrictive NPIs may not provide much additional benefit. On the other hand, if lrNPIs provide relatively small nudges to individual behaviour, then mrNPIs may result in large behavioural effects at the margin, and large reductions in the growth of new cases. However, because underlying epidemic dynamics are imprecisely characterized and are important for estimating the policy effects, our models test the extent to which mrNPIs had additional effect on reducing transmission by differencing the sum of NPI effects and epidemic dynamics in countries that did not enact mrNPIs from the sum of NPI effects and epidemic dynamics in countries that did.
We estimate the unique effects of mrNPIs on case growth rate during the Northern Hemisphere spring of 2020 in England, France, Germany, Iran, Italy, the Netherlands, Spain and the United States by comparing the effect of NPIs in these countries to those in Sweden and South Korea (separately). The data we use build on an analysis of NPI effects and consist of daily case numbers in subnational administrative regions of each country (eg regions in France, provinces in Iran, states in the United States and counties in Sweden), merged with the type and timing of policies in each administrative region. 18 , 26 We use data from a COVID‐19 policy databank and previous analyses of policy impacts to determine the timing and location of each NPI. 18 , 27 Each observation in the data, then, is identified by the subnational administrative region and the date, with data on the number of cases on that date and indicators characterizing the presence of each policy. We include indicators for changes in case definitions or testing technologies to capture abrupt changes in case counts that are not the result of the underlying epidemic (these are mostly single‐day indicators), as suggested in a previous analysis. 18
We define the dependent variable as the daily difference in the natural log of the number of confirmed cases, which approximates the daily growth rate of infections (). We then estimate the following linear models:
The model terms are indexed by country (), subnational unit (), day () and NPI indicator (. is a series of fixed effects for the subnational unit, and is country‐specific day‐of‐week fixed effects. The parameters of interest are , which identify the effect of each policy on the growth rate in cases. The parameter is a single‐day indicator that models changes in case definitions that result in short discontinuities in case counts that are not due to underlying epidemic changes.
We estimate these models separately for each pair of countries (one with mrNPIs, one without), for a total of 16 models. We then add the coefficients of all the policies for the country with mrNPIs (yielding the combined effects of all NPIs in the mrNPI country) and subtract the combined effects of all NPIs in the comparator country without mrNPI. As noted above, the difference isolates the effect of mrNPIs on case growth rates. We estimate robust standard errors throughout, with clustering at the day‐of‐week level to account for serial correlation.
It is important to note that because the true number of infections is not visible in any country, it is impossible to assess the impact of national policies on transmission or new infections. 28 Instead, we follow other studies evaluating the effects of NPIs that use case numbers, implicitly assuming that their observed dynamics may represent a consistent shadow of the underlying infection dynamics. 18
The code for the data preparation, analysis and visualization is provided along with the article (Supplementary Material).
3. RESULTS
The growth rate in new cases prior to implementation of any NPIs was positive in all study countries (Figure 1). The figure shows that, across all subnational units in all ten countries, the average growth rate prior to NPIs ranged from 0.23 in Spain (23% daily growth; 95% CI: 0.13 to 0.34) to 0.47 (95% CI: 0.39 to 0.55) in the Netherlands. The average across all 10 countries was 0.32, and in South Korea and Sweden, the 2 countries without mrNPIs, the pre‐NPI growth rates were 0.25 and 0.33, respectively. The variation of pre‐policy growth rates in cases may reflect epidemic intensity, testing coverage (higher growth may be a reflection of expanding testing capacity and of more people wishing to be tested) and pre‐policy behaviour changes that led to increased or decreased transmission.
FIGURE 1.
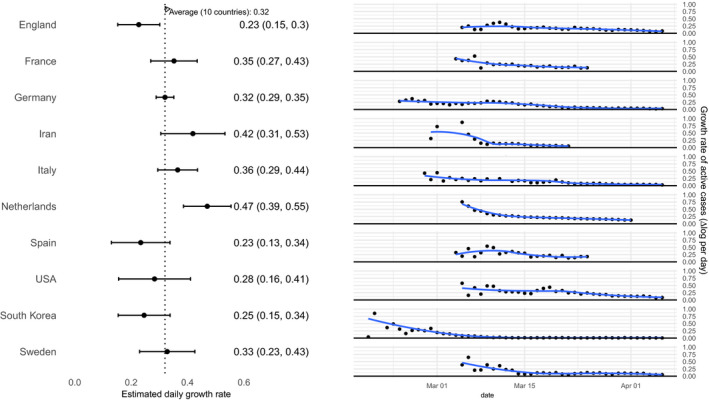
Growth rate in cases for study countries. The black bars demonstrate the average growth rate in cases in each subnational unit (95% CI) prior to any policies implemented. The figures to the right show the daily growth rate in cases for each of the countries and demonstrate the shared decline in case growth across all countries, including the countries that did not implement mrNPIs (South Korea and Sweden)
Figures 2 and 3 and demonstrate the effects of individual NPIs (Figure 2) and all NPIs combined (Figure 3) on daily growth in case counts. While the effects of 3 individual NPIs were positive—that is, contributing paradoxically to case growth—and significant (one in Germany, one in Italy and one in Spain, out of 51 individual NPIs in all 10 countries), the effects of about half of individual NPIs were negative and significant. The combined effects of all NPIs (Figure 3) were negative and significant in 9 out of 10 countries, where their combined effects ranged from −0.10 (95% CI: −0.06 to −0.13) in England to −0.33 (95% CI: −0.09 to −0.57) in South Korea. Spain was the only country where the effect of NPIs was not distinguishable from 0 (−0.02; 95% CI: −0.12 to 0.07).
FIGURE 2.
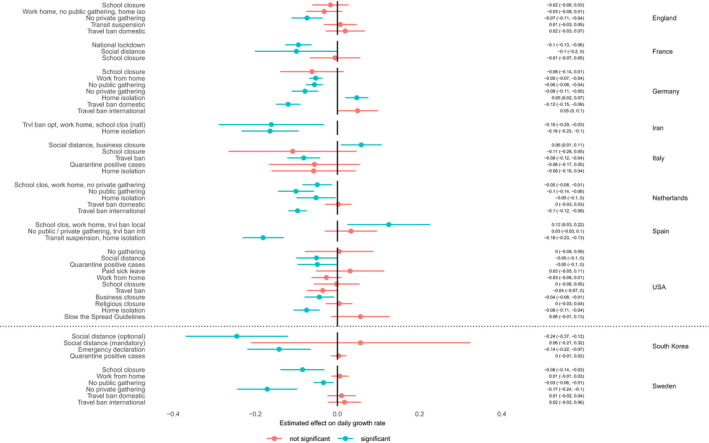
Effects of individual NPIs in all study countries. The variation in the timing and location of NPI implementation allows us to identify the effects of individual NPIs on the daily growth rate of cases. Where multiple NPIs were implemented simultaneously (in the same day) across all subnational units (eg school closure, work from home and no private gatherings in Spain), their overall effect cannot be identified individually and is shown combined
FIGURE 3.

Combined effects of all NPIs in study countries. The point estimate and 95% CI of the combined effect of NPIs on growth rate in cases, estimated from a combination of individual NPIs. The estimates show significant effects in all countries except Spain and range from a 33% (9%‐57%) decline in South Korea to 10% (6%‐13%) in England. The point estimate of the effect in Spain is also negative but small (2%) and not significant
Figure 4 shows the effect of mrNPIs in the 8 countries where mrNPIs were implemented, after accounting for the effects of lrNPIs and underlying epidemic dynamics. In none of the 8 countries and in none out of the 16 comparisons (against Sweden or South Korea) were the effects of mrNPIs significantly negative (beneficial). The point estimates were positive (point in the direction of mrNPIs resulting in increased daily growth in cases) in 12 out of 16 comparisons (significantly positive in 3 of the 12, in Spain and in England compared with Sweden). The only country where the point estimates of the effects of mrNPIs were negative in both comparisons was Iran (−0.07 [95% CI: −0.21 to 0.07] compared with Sweden; −0.02 [95% CI: −0.28 to 0.25] compared with South Korea). The 95% confidence intervals excluded a 30% reduction in daily growth in all 16 comparisons.
FIGURE 4.
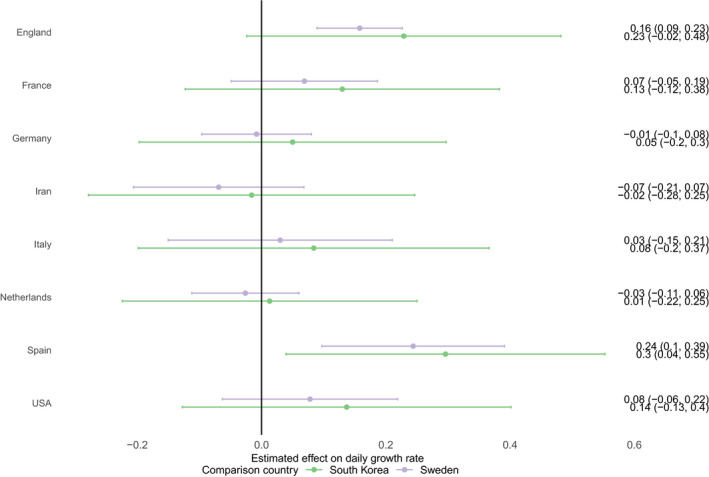
Effect of mrNPIs on daily growth rates after accounting for the effects of lrNPIs in South Korea and Sweden. Under no comparison is there evidence of reduction in case growth rates from mrNPIs, in any country. The point estimates are positive (point in the direction of mrNPIs resulting in increased daily growth in cases) in 12 out of 16 comparisons
4. DISCUSSION
In the framework of this analysis, there is no evidence that more restrictive nonpharmaceutical interventions (‘lockdowns’) contributed substantially to bending the curve of new cases in England, France, Germany, Iran, Italy, the Netherlands, Spain or the United States in early 2020. By comparing the effectiveness of NPIs on case growth rates in countries that implemented more restrictive measures with those that implemented less‐restrictive measures, the evidence points away from indicating that mrNPIs provided additional meaningful benefit above and beyond lrNPIs. While modest decreases in daily growth (under 30%) cannot be excluded in a few countries, the possibility of large decreases in daily growth due to mrNPIs is incompatible with the accumulated data.
The direction of the effect size in most scenarios points towards an increase in the case growth rate, though these estimates are only distinguishable from zero in Spain (consistent with nonbeneficial effect of lockdowns). Only in Iran do the estimates consistently point in the direction of additional reduction in the growth rate, yet those effects are statistically indistinguishable from zero. While it is hard to draw firm conclusions from these estimates, they are consistent with a recent analysis that identified increased population‐level transmission and cases in Hunan, China, during the period of stay‐at‐home orders, attributed to increased intra‐household density and transmission. 29 In other words, it is possible that stay‐at‐home orders may facilitate transmission if they increase person‐to‐person contact where transmission is efficient such as closed spaces.
Our study builds on the findings of overall effectiveness of NPIs in reducing case growth rate. This has a plausible underlying behavioural mechanism: NPIs are motivated by the notion that they lead to anti‐contagion behaviour changes, either directly through personal compliance with the interventions, or by providing a signal about disease risk, as communicated by policymakers, which is used in deciding on individual behaviours. The degree to which risk communications motivate personal behaviours has been used to explain South Korea's response to NPIs, where large personal behaviour changes were observed following less‐restrictive NPIs. 30
This analysis ties together observations about the possible effectiveness of NPIs with COVID‐19 epidemic case growth changes that appear surprisingly similar despite wide variation in national policies. 31 , 32 , 33 Our behavioural model of NPIs—that their effectiveness depends on individual behaviour for which policies provide a noisy nudge—helps explain why the degree of NPI restrictiveness does not seem to explain the decline in case growth rate. Data on individual behaviours such as visits to businesses, walking or driving show dramatic declines days to weeks prior to the implementation of business closures and mandatory stay‐at‐home orders in our study countries, consistent with the behavioural mechanisms noted above. 34 , 35 , 36 These observations are consistent with a model where the severity of the risk perceived by individuals was a stronger driver of anti‐contagion behaviours than the specific nature of the NPIs. In other words, reductions in social activities that led to reduction in case growth were happening prior to implementation of mrNPIs because populations in affected countries were internalizing the impact of the pandemic in China, Italy and New York, and noting a growing set of recommendations to reduce social contacts, all of which happened before mrNPIs. This may also explain the highly variable effect sizes of the same NPI in different countries. For example, the effects of international travel bans were positive (unhelpful) in Germany and negative (beneficial) in the Netherlands (Figure 2).
While this study casts doubt on any firm conclusions about the effectiveness of restrictive NPIs, it also underscores the importance of more definitive evaluations of NPI effects. NPIs can also have harms, besides any questionable benefits, and the harms may be more prominent for some NPIs than for others. For example, school closures may have very serious harms, estimated at an equivalent of 5.5 million life years for children in the United States during the spring school closures alone. 37 Considerations of harms should play a prominent role in policy decisions, especially if an NPI is ineffective at reducing the spread of infections. Of note, Sweden did not close primary schools throughout 2020 as of this writing.
While we find no evidence of large anti‐contagion effects from mandatory stay‐at‐home and business closure policies, we should acknowledge that the underlying data and methods have important limitations. First, cross‐country comparisons are difficult: countries may have different rules, cultures and relationships between the government and citizenry. For that reason, we collected information on all countries for which subnational data on case growth were obtainable. Of course, these differences may also exist across subnational units, as demonstrated in the case of different states in the United States. Additional countries could provide more evidence, especially countries that had meaningful epidemic penetration and did not use mrNPIs for epidemic control. Second, confirmed case counts are a noisy measure of disease transmission. Testing availability, personal demand for or fear of getting tested, testing guidelines, changing test characteristics and viral evolution all interfere in the relationship between the underlying infections and case counts. Because the location and timing of policies are endogenous to perceived epidemic stage, the noise in case counts is associated with the policies, making bias possible and very difficult to eradicate. The fixed‐effects approach provides unbiased estimates so long as the location or timing of policies is quasi‐arbitrary with respect to the outcome. This may fail to hold in this assessment of NPI effects because the underlying epidemic dynamics are nonlinear, and the policies respond to—and modify—the epidemic stage. This limitation also holds for all other empirical assessments of NPI effects. 18
Third, our findings rest on a conceptualization, common in the literature, of NPIs as ‘reduced‐form’ interventions: an upstream policy has expected downstream effects on transmission. This allows us to use Sweden and South Korea as comparators, since they had applied less‐restrictive interventions, which then enable netting out the combined effect of lrNPIs and the underlying epidemic dynamics. While contextual factors that mediate the effects of NPIs are important—countries implemented different variants of the same NPI, and the population responded differently—many analyses examining the effects of NPIs have a similar ‘reduced‐form’ structure. 18 , 31 , 38 In that sense, our comparison is positioned squarely within the literature on the effects of NPIs.
During the Northern Hemisphere fall and winter of 2020, many countries, especially in Europe and the United States, experienced a large wave of COVID‐19 morbidity and mortality. Those waves were met with new (or renewed) NPIs, including mrNPIs in some countries (eg England) and lrNPIs in others (eg Portugal) that had used mrNPIs in the first wave. The spread of infections in countries that were largely spared in the spring (eg Austria and Greece) further highlights the challenges and limited ability of NPIs to control the spread of this highly transmissible respiratory virus. Empirical data for the characteristics of fatalities in the later wave before mrNPIs were adopted as compared with the first wave (when mrNPIs had been used) show that the proportion of COVID‐19 deaths that occurred in nursing homes was often higher under mrNPIs rather than under less‐restrictive measures. 39 This further suggests that restrictive measures do not clearly achieve protection of vulnerable populations. Some evidence also suggests 40 that sometimes under more restrictive measures, infections may be more frequent in settings where vulnerable populations reside relative to the general population. 40
In summary, we fail to find strong evidence supporting a role for more restrictive NPIs in the control of COVID in early 2020. We do not question the role of all public health interventions, or of coordinated communications about the epidemic, but we fail to find an additional benefit of stay‐at‐home orders and business closures. The data cannot fully exclude the possibility of some benefits. However, even if they exist, these benefits may not match the numerous harms of these aggressive measures. More targeted public health interventions that more effectively reduce transmissions may be important for future epidemic control without the harms of highly restrictive measures.
5. ROLE OF THE FUNDING ORGANIZATION OR SPONSOR
The funding organizations had no role in the design or execution of this analysis.
AUTHOR CONTRIBUTIONS
EB conceived the project; EB and CO designed the analyses, prepared the data and executed the analyses; JB and JPAI were involved in discussing and interpreting the results, and drafting, revising and improving the manuscript. All authors have approved the final manuscript.
Supporting information
Fig S1
Supplementary Material
Bendavid E, Oh C, Bhattacharya J, Ioannidis JPA. Assessing mandatory stay‐at‐home and business closure effects on the spread of COVID‐19. Eur J Clin Invest. 2021;51:e13484. 10.1111/eci.13484
FUNDING INFORMATION
The study was funded with support from the Stanford COVID‐19 Seroprevalence Studies Fund.
REFERENCES
- 1. Bassett BA. Strict lower bound on the COVID‐19 fatality rate in overwhelmed healthcare systems. medRxiv. Published online April 27, 2020:2020.04.22.20076026. doi:10.1101/2020.04.22.20076026.
- 2. Virus‐linked hunger tied to 10 000 child deaths each month. AP NEWS. Published July 27, 2020. https://apnews.com/5cbee9693c52728a3808f4e7b4965cbd. Accessed August 26, 2020.
- 3. Issue brief: Reports of increases in opioid related overdose and other concerns during the COVID pandemic. https://www.ama‐assn.org/system/files/2020‐08/issue‐brief‐increases‐in‐opioid‐related‐overdose.pdf. Accessed August 26, 2020.
- 4. Guha‐Sapir D, Moitinho de Almeida M, Keita M, Greenough G, Bendavid E. COVID‐19 policies: remember measles. Science. 2020;369(6501):261. 10.1126/science.abc8637 [DOI] [PubMed] [Google Scholar]
- 5. O’Leary ST, Trefren L, Roth H, Moss A, Severson R, Kempe A. Number of childhood and adolescent vaccinations administered before and after the COVID‐19 outbreak in Colorado. JAMA Pediatr. Published online December 7, 2020. doi:10.1001/jamapediatrics.2020.4733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Report 18 ‐ The potential public health impact of COVID‐19 on malaria in Africa. Imperial College London. http://www.imperial.ac.uk/medicine/departments/school‐public‐health/infectious‐disease‐epidemiology/mrc‐global‐infectious‐disease‐analysis/covid‐19/report‐18‐malaria/. Accessed August 26, 2020.
- 7. Report 19 ‐ The potential impact of the COVID‐19 epidemic on HIV, TB and Malaria in low‐ and middle‐income countries. Imperial College London. http://www.imperial.ac.uk/medicine/departments/school‐public‐health/infectious‐disease‐epidemiology/mrc‐global‐infectious‐disease‐analysis/covid‐19/report‐19‐hiv‐tb‐malaria/. Accessed August 26, 2020.
- 8. Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the number of US patients with newly identified cancer before and during the coronavirus disease 2019 (COVID‐19) pandemic. JAMA Netw Open. 2020;3(8):e2017267. 10.1001/jamanetworkopen.2020.17267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fragala MS, Kaufman HW, Meigs JB, Niles JK, McPhaul MJ. Consequences of the COVID‐19 pandemic: reduced hemoglobin A1c diabetes monitoring. Population Health Management. Published online June 29, 2020. doi:10.1089/pop.2020.0134. [DOI] [PMC free article] [PubMed]
- 10. Wenham C, Smith J, Davies SE, et al. Women are most affected by pandemics — lessons from past outbreaks. Nature. 2020;583(7815):194‐198. 10.1038/d41586-020-02006-z [DOI] [PubMed] [Google Scholar]
- 11. Loades ME, Chatburn E, Higson‐Sweeney N, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID‐19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218‐1239.e3. 10.1016/j.jaac.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sher L. The impact of the COVID‐19 pandemic on suicide rates. QJM. 2020;113(10):707‐712. 10.1093/qjmed/hcaa202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cahan E. Charities that fund research face deep revenue declines. Science. 2020;368(6498):1412. 10.1126/science.368.6498.1412 [DOI] [PubMed] [Google Scholar]
- 14. Roelfs DJ, Shor E, Davidson KW, Schwartz JE. Losing life and livelihood: a systematic review and meta‐analysis of unemployment and all‐cause mortality. Soc Sci Med. 2011;72(6):840‐854. 10.1016/j.socscimed.2011.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Flaxman S, Mishra S, Gandy A, et al. Estimating the effects of non‐pharmaceutical interventions on COVID‐19 in Europe. Nature. 2020;584(7820):257‐261. 10.1038/s41586-020-2405-7 [DOI] [PubMed] [Google Scholar]
- 16. Bryant P, Elofsson A. The limits of estimating COVID‐19 intervention effects using Bayesian models. medRxiv. Published online August 16, 2020:2020.08.14.20175240. doi:10.1101/2020.08.14.20175240.
- 17. Lockdowns, science and voodoo magic. Nec Pluribus Impar. Published December 4, 2020. https://necpluribusimpar.net/lockdowns‐science‐and‐voodoo‐magic/. Accessed December 7, 2020.
- 18. Hsiang S, Allen D, Annan‐Phan S, et al. The effect of large‐scale anti‐contagion policies on the COVID‐19 pandemic. Nature. 2020;584(7820):262‐267. 10.1038/s41586-020-2404-8 [DOI] [PubMed] [Google Scholar]
- 19. Kermack WO, McKendrick AG, Walker GT. A contribution to the mathematical theory of epidemics. Proc R Soc Lond A Math Phys Sci. 1927;115(772):700‐721.doi:10.1098/rspa.1927.0118. [Google Scholar]
- 20. Philipson T. Chapter 33 Economic epidemiology and infectious diseases. In: Handbook of Health Economics. Vol 1. Elsevier; 2000:1761‐1799. 10.1016/S1574-0064(00)80046-3 [DOI] [Google Scholar]
- 21. Atkeson A, Kopecky K, Zha T. Four stylized facts about COVID‐19. Natl Bur Econ Res. 2020. 10.3386/w27719 [DOI] [Google Scholar]
- 22. Baker S. Sweden’s no‐lockdown strategy is beginning to look like less of an outlier, but still doesn’t compare well to other countries. Business Insider. https://www.businessinsider.com/sweden‐coronavirus‐rates‐fall‐but‐other‐countries‐still‐fare‐better‐2020‐8. Accessed August 31, 2020.
- 23. Habib H. Has Sweden’s controversial covid‐19 strategy been successful? BMJ. 2020;369: 10.1136/bmj.m2376 [DOI] [PubMed] [Google Scholar]
- 24. NormileMar . 17 D, 2020, Am 8:00. Coronavirus cases have dropped sharply in South Korea. What’s the secret to its success? Science | AAAS. Published March 17, 2020. https://www.sciencemag.org/news/2020/03/coronavirus‐cases‐have‐dropped‐sharply‐south‐korea‐whats‐secret‐its‐success. Accessed August 31, 2020.
- 25. Yoon D, South Korea, facing coronavirus surge, resists tightest restrictions. Wall Street Journal. https://www.wsj.com/articles/south‐korea‐facing‐coronavirus‐surge‐resists‐tightest‐restrictions‐11598440860. Published August 26, 2020. Accessed August 31, 2020.
- 26. Sweden: coronavirus cases by region. Statista. https://www.statista.com/statistics/1103949/number‐of‐coronavirus‐covid‐19‐cases‐in‐sweden‐by‐region/. Accessed August 27, 2020.
- 27. Coronavirus Government Response Tracker. https://www.bsg.ox.ac.uk/research/research‐projects/coronavirus‐government‐response‐tracker. Accessed August 27, 2020.
- 28. Peirlinck M, Linka K, Sahli Costabal F, et al. Visualizing the invisible: the effect of asymptomatic transmission on the outbreak dynamics of COVID‐19. Comput Methods Appl Mech Eng. Published online September 8, 2020:113410. doi:10.1016/j.cma.2020.113410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sun K, Wang W, Gao L, et al. Transmission heterogeneities, kinetics, and controllability of SARS‐CoV‐2. Science. Published online November 24, 2020. doi:10.1126/science.abe2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Travaglino GA, Moon C. Explaining compliance with social distancing during the COVID‐19 pandemic: the roles of cultural orientations, trust and self‐conscious emotions in the US, Italy, and South Korea. PsyArXiv. 2020. 10.31234/osf.io/8yn5b [DOI]
- 31. Hatchett RJ, Mecher CE, Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc Natl Acad Sci USA. 2007;104(18):7582‐7587. 10.1073/pnas.0610941104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cheatley J, Vuik S, Devaux M, et al.The effectiveness of non‐pharmaceutical interventions in containing epidemics: a rapid review of the literature and quantitative assessment. medRxiv. Published online April 10, 2020:2020.04.06.20054197. doi:10.1101/2020.04.06.20054197.
- 33. Garchitorena A, Gruson H, Cazelles B, Roche B. Quantifying the efficiency of non‐pharmaceutical interventions against SARS‐COV‐2 transmission in Europe. medRxiv. Published online August 18, 2020:2020.08.17.20174821. doi:10.1101/2020.08.17.20174821.
- 34. COVID‐19 ‐ Mobility Trends Reports. Apple. https://www.apple.com/covid19/mobility. Accessed August 28, 2020.
- 35. Valentino‐DeVries J, Koeze E, Maheshwari S. Virus alters where people open their wallets, hinting at a halting recovery. The New York Times. https://www.nytimes.com/interactive/2020/08/18/business/economy/coronavirus‐economic‐recovery‐states.html. Published August 19, 2020. Accessed August 28, 2020.
- 36. Badr HS, Du H, Marshall M, Dong E, Squire MM, Gardner LM. Association between mobility patterns and COVID‐19 transmission in the USA: a mathematical modelling study. Lancet Infect Dis. 2020;20(11):1247‐1254. 10.1016/S1473-3099(20)30553-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Christakis DA, Van Cleve W, Zimmerman FJ. Estimation of US children’s educational attainment and years of life lost associated with primary school closures during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3(11):e2028786. 10.1001/jamanetworkopen.2020.28786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pan A, Liu L, Wang C, et al. Association of public health interventions with the epidemiology of the COVID‐19 outbreak in Wuhan. China. JAMA. 2020;323(19):1915‐1923. 10.1001/jama.2020.6130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ioannidis JPA, Axfors C, Contopoulos‐Ioannidis DG. Second versus first wave of COVID‐19 deaths: shifts in age distribution and in nursing home fatalities. medRxiv. Published online November 30, 2020:2020.11.28.20240366. doi:10.1101/2020.11.28.20240366. [DOI] [PMC free article] [PubMed]
- 40. Ioannidis JPA. Precision shielding for COVID‐19: metrics of assessment and feasibility of deployment. medRxiv. Published online November 4, 2020:2020.11.01.20224147. doi:10.1101/2020.11.01.20224147. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1
Supplementary Material


