Abstract
Vohwinkel Syndrome, also known as Keratoderma Hereditarium Mutilans, is an extremely rare dominant autosomal keratosis. It typically presents with “starfish” keratoses on the knuckles, palmoplantar keratoderma (PPK), hearing impairment and mutilating digital constriction bands (pseudoainhum) that cause strangulation, often leading to autoamputation of the affected digit. Both medical and surgical treatment haven’t shown to date consistent results, in the treatment of pseudoainhum. In this study we present the case of a woman with Vohwinkel syndrome who showed constriction bands causing ischemic changes of the 5th digit of the right hand for which she was treated with surgery. We also present a review of the literature for the management of this disease.
Key words: Pseudoainhum, Hand surgey, Genetic disease, Vohwinkel Syndrome
Introduction
Vohwinkel syndrome, or hereditary mutilating keratodermia, is a rare connective tissue disease, and only a few cases have been described in the literature. It most commonly affects caucasian women, and it occurs during childhood with worsening in adolescence. It can be sporadic, or inherited with an autosomal dominant pattern and a variable phenotype.1-3
It was described by Vohwinkel in 1929, and it is caused by a heterozygous mutation of the GJB2 gene, which codes for the connexin 26 protein.4 The classic variant of this disease is characterized by fibrous bands (pseudoainhum) on the fifth finger that can lead to a progressive self-amputation, starfish-shaped keratosis on the elbows, knees, wrists and knuckles of the hand, and deafness. Nail dystrophy, alopecia, onychogrifosis and various neurological anomalies may also occur. Another variant of this disease is the Camisa variant. This is caused by a mutation of the loricrina protein - synthesized in the grainy layer of the epidermis - and leads to ichthyosis.5Medical treatment includes systemic synthetic retinoids derived from vitamin A, which improve the differentiation and proliferation of the epidermal tissues.6,7 Different experimental surgical techniques, such as local tissue rearrangements, local flaps and skin grafts, have been described for the treatment of pseudoainhum. In the present study we report the case of a fifty-year-old woman affected by Vohwinkel syndrome showing constriction bands (pseudoainhum) in the right fifth digit.
Case Report
A 55-year-old caucasian woman, with bilateral sensorineural hearing loss, came to our attention complaining of severe pain in the fifth digit of the right hand. The pain had been mild during the last year and became acute in the last two months. Clinical examination showed “honeycomb” palmar keratosis, starfish keratosis on the dorsal side of both hands and feet (which the patient had been suffering since the age of five), digital constriction bands in the proximal interphalangea (PIP) joint of the right fifth digit and skin dyschromia (Figure 1a). Neurovascular deficit with pain, paresthesia and hypoesthesia of the fifth finger were also present. Her father, sister and grandmother had the same syndromic pattern. Based on these clinical findings a diagnosis of Vohwinkel syndrome was made. Plain radiographs of the right hand showed periosteal thinning of the proximal phalanx of the fifth digit and soft tissue alteration (Figure 1b).
MR confirmed the periosteal thinning and showed a lack of visualization of a segment (8 mm) of the extensor tendon at the proximal interphalangeal joint of the fifth digit, compatible with a complete lesion (Figure 1c). Marked thinning of the fifth digit’s flexor tendon, thickening of the flexor tendons of the other fingers, and thinning of their extensor counterparts, were also evident.
Conservative surgical treatment was proposed to the patient, but owing to the high recurrence rate described in the literature she refused this type of approach and preferred amputation of the proximal phalanx of the fifth digit of the right hand.
In anesthesia, a skin incision was made through the proximal interphalangeal joint and a capsulotomy was performed. We then proceeded with the amputation and disarticulation of the head of the proximal phalanx, followed by proper hemostasis, tendon plasty procedure and suturing (Figure 2). The incision was medicated with sterile gauzes, and an elastic dressing was applied.
Post-surgical follow-up consisted in anterior-posterior and latero-lateral radiographs of the right hand, and an inhospital observation period of 24 hours during which neither vascular nor nervous deficits emerged. Optimal articular range of motion was maintained and pain was greatly reduced. Histological examination showed (severe hyperkeratosis, hypergranulosis, and mild acanthosis, of the cutaneous component consistent with the diagnosis of Vohwinkel Syndrome (Figure 3).
At 15 days follow-up, the surgical wound was clean, no sign of infection was evident, and the patient didn’t complain any pain. At 12-month follow-up, the patient did not report pain, and plain radiographs showed no abnormalities at the site of amputation.
Discussion and Conclusions
In our case the diagnosis of Vohwinkel syndrome was made on the basis of clinical findings and then confirmed by histological examination, as previously reported in the literature.8 Our patient showed a typical clinical pattern with honeycomb, diffuse palmoplantar keratoderma, starfish keratosis of the dorsal surfaces of the digits, fibrous constriction bands (pseudoainhum) of the 5th digit, hearing loss, deaf mutism and scarring alopecia. Differential diagnosis includes other keratodermas presenting with digital autoamputation, such as: Mal de Meleda, Olmsted syndrome, acral keratoderma, pachyonychia congenita, palmoplantar keratoderma of Sybert, and palmoplantar keratoderma of Gamborg- Nielsen, as well as acquired dermatoses that can lead to the appearance of constricting bands, such as leprosy, tertiary syphilis, ainhum, scleroderma, amniotic bands, Raynaud syndrome, and syringomyelia.9 There are no sufficiently distinctive histopathological pictures to differentiate palmoplantar keratoderma in one type or another.10,11 In our case histological examination showed hyperkeratosis, acanthosis, and hypergranulosis which are suggestive for pseudoainhum.12,13 Unlike other Authors, Luk et al.1 considered hypogranulosis an atypical histological finding for pseudoainhum. Pseudo-ainhum is a congenital disorder characterized by fibrous bands development on fingers and toes, while ainhum is an idiopathic disease involving the fifth toe of black people. In both cases, if not treated, fibrosis can progressively compromise the mobility and the neurovascular function leading to selfamputation. 14 In the few cases of Vohwinkel syndrome reported in the literature the results of medical and surgical treatments were often inconsistent owing to the lack of histologic examination and uncertain diagnosis.2,6,15-17 Systemic retinoids and derivatives of vitamin A have been used to treat these patients, since they may facilitate the differentiation and proliferation of the epidermal skin layer, which could help to treat pseudoainhum. However, this therapy has given only modest results, and its use is very limited due to its toxicity and teratogenicity. To date no standard surgical treatment or guidelines exist for the treatment of pseudoainhum in patients with Vohwinkel disease, however four surgical techniques have been described for the treatment pseudoainhum (Table 1). Z-plasty has been used to treat early stages of ainhum (phase I-II) to release the constrictive base. For phases III and IV, amputation is generally necessary, unless self-amputation has not already taken place.18 Z-plasty, consisting in the surgical excision of the fiber band and lengthening by Z-plasty, was the first technique to be used in 1986 by Luk et al.1 and then by Pisoh et al. in 1995.17 However, the lack of follow-up data represents an important limit of these two studies. Two other cases reported in the literature, treated with Z-plasty describe the recurrence of the fiber band 36 and 6 months after surgery, respectively.2,12 Crossing finger flap used by Bassetto et al.19 and Solis RR20 is a technique to cover the palmar area of the PIP - in which the fibrous band was removed - and had satisfactory results at 18-month follow-up. This procedure was used for the first time by Atasoy et al.21 in 1979 to treat digital injuries. The limit of this technique is the thinness and the lack of adequate subcutaneous tissue at the level of the proximal interphalangeal joints.
Figure 1.

a) Palmar keratosis, starfish keratosis and digital constriction bands on the PIP joint; b) radiographs show periosteal thinning of the proximal phalanx; c) MRI shows periosteal thinning and a lack of visualization of the extensor tendon at the proximal PIP.
Figure 2.
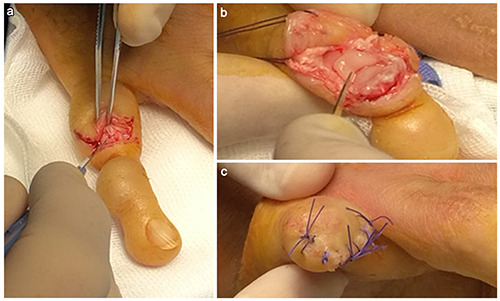
a) Incision; b) disarticulation of the head of the proximal phalanx, followed by proper hemostasis, tendon plasty procedure, and c) suturing.
Figure 3.
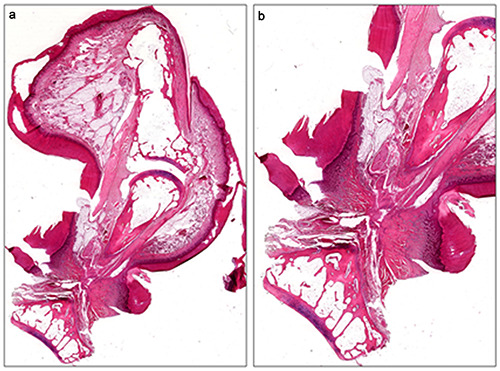
a) Orthokeratotic hyperkeratosis, acanthosis and hypergranulosis of the finger and constriction of the proximal PIP; b) Higher magnification of circumferential hyperkeratotic constriction band in the proximal interphalangeal joint. a,b) ematoxylin and eosin stain. Original magnifications: a) 10×; b) 20×.
Table 1.
Different surgical techniques for the treatment of pseudo ainhum.
| Author (year) | N. of patients | Age | Sex | Family history | Hystology | Surgery | Medical treatment | Follow-up |
|---|---|---|---|---|---|---|---|---|
| Luk et al. (1986)1 | 1 | 54 | M | No | Yes | Z-plasties | No | 12 months |
| Pisoh et al. (1995)17 | 1 | 33 | F | Yes | Yes | Z-plasty + skin graft | Vitamin A ointments | 2 months |
| Solis et al. (2001)20 | 1 | 17 | F | Yes | Yes | Cross finger-flap coverage + split thickness skin grafts | Ammonium lactate 12% lotion | No |
| Atabay et al. (2001)12 | 1 | 24 | F | No | Yes | Z-plasties | No | 12 months |
| Sinha et al. (2009)2 | 2 | 46, 30 | M, F | Yes | No | 1) Z and Y-V plasties; 2) thickness skin graft | 1) Acetretin; 2) no | 5 years, 8 years |
| Bassetto et al. (2010)19 | 1 | 48 | F | Not available | No | Cross finger flap | Systemic retinoids | 18 months |
| Liebman et al. (2013)16 | 1 | 23 | F | Not available | No | Full-thickness skin graft | No | 16 months |
| Zhang et al. (2016)13 | 1 | 24 | F | Yes | Yes | Abdominal skin flap | No | 18 months |
| Zamiri et al. (2018)15 | 1 | 62 | M | Not available | No | Full thickness skin grafts | Acitretin | 36 months |
The full-thickness skin graft consists of full-thickness excision of the constriction band with identification and preservation of the neurovascular bundles, and application of a skin graft harvested from the groin crease or from the forearm.16,17 Lieban et al. used this technique successfully, with amelioration of the pseudo-ainhum, without recurrence of the treated area after 16 months of follow-up. Zamiri et al. also reported a successful treatment of pseudoainhum using the full-thickness excision techniques, with no recurrence after 36 months. In 2016, Zhang et al.13 designed a surgical approach for digital constriction bands using a distant abdominal skin flap to repair the wound after excising the constriction band from the digits. No recurrence occurred after 18 months of follow-up. Using a distant abdominal skin flap can ensure blood supply, and flap survival as well as improve the appearance. This technique may permanently solve the constriction band recurrence problem; however, it requires a long treatment period, with 3 operations under local anesthesia, and a relatively long local immobilization time.
In our case we had to perform an amputation due to the patient’s poor compliance, and to the clinical severity (neurovascular impairment of the finger). According to the literature, with special reference to the work of Liebamann et al.,16 the excision of the constriction bands may not be sufficient. Indeed, the condition could recur over time considering the characteristics of the disease, and its tendency towards specific areas of the fingers. The skin graft tends to maintain the characteristics of the donor site, therefore it could definitively solve the problem, if taken from not affected areas.
In our review of the literature we report many surgical techniques for the treatment of psudoainhum, however in all cases the authors report a short term follow up which doesn’t allow to define a resolutive treatment.
We believe that a multidisciplinary approach for the management of these patients could help to prevent long-term selfamputation.
Funding Statement
Funding: None.
References
- 1.Luk KD, Wu PC, Chow SP. Keratoma hereditaria mutilans: report of a case with successful surgical treatment. J Hand Surg Am 1986;11:269-72. [DOI] [PubMed] [Google Scholar]
- 2.Sinha M, Watson SB. Keratodermia hereditarium mutilans (Vohwinkel syndrome). J Hand Surg Eur 2009; 34:235-7. [DOI] [PubMed] [Google Scholar]
- 3.Vohwinkel KH. Keratoderma hereditarium mutilans. Arch Dermtol Syph 1929;158:354-64. [Google Scholar]
- 4.Maestrini E, Korge BP, Ocana-Sierra J, et al. A missense mutation in connexin26, D66H, causes mutilating keratoderma with sensorineural deafness (Vohwinkel’s syndrome) in three unrelated families. Hum Mol Genet 1999;8:1237-43. [DOI] [PubMed] [Google Scholar]
- 5.Corte LD, Silva MV, Oliveira CF, et al. Vohwinkel syndrome, ichthyosiform variant--by Camisa--case report. An Bras Dermatol 2013;88:206-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heller EH, Shiffman NJ. Synthetic retinoids in dermatology. Can Med Assoc J 1985;132:1129-36. [PMC free article] [PubMed] [Google Scholar]
- 7.Wereide K. Mutilating palmoplantar keratoderma successfully treated with etretinate. Acta Derm Venereol 1984;63:181. [PubMed] [Google Scholar]
- 8.Peris K, Salvati EF, Torlone G, et al. Keratoderma hereditarium mutilans (Vohwinkel’s syndrome) associated with congenital deafmutism. Br J Dermatol 1995;132:617-20. [DOI] [PubMed] [Google Scholar]
- 9.Cavalcante LIS, Almeida TLP, Holanda EM, Accioly-Filho JW. Vohwinkel´s mutilating keratoderma: report of three familial cases. An Bras Dermatol 2003;78:311-8. [Google Scholar]
- 10.Montgomery H, editor: Dennatopathology, volt. New York, 1967, Harper & Row, pp 66-70 [Google Scholar]
- 11.Den Kaloustian VM, Kurban AK, editors: Genetic disease of the skin. New York, 1979, Springer-Verlag, pp 42-6. [Google Scholar]
- 12.Atabay K, Yavuzer R, Latifoğlu O, Ozmen S. Keratoderma hereditarium mutilans (Vohwinkel syndrome): an unsolved surgical mystery. Plast Reconstr Surg 2001;108:1276-80. [DOI] [PubMed] [Google Scholar]
- 13.Zhang M, Song K, Ding N, et al. Using a Distant Abdominal Skin Flap to Treat Digital Constriction Bands: A Case Report for Vohwinkel Syndrome. Medicine (Baltimore) 2016;95:e2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tchouakam DN, Tochie JN, Guifo ML, Choukem SP. Ainhum, a rare mutilating dermatological disease in a female Cameroonian: a case report. BMC Dermatol 2019;19:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zamiri M. Loricrin palmoplantar keratoderma: full-thickness skin grafting for pseudoainhum. Watson S Clin Exp Dermatol 2019;44:444-6. [DOI] [PubMed] [Google Scholar]
- 16.Liebman JJ, Liu Y. Successful surgical management of keratoderma hereditaria mutilans. Hand (N Y) 2013;8:102-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pisoh T, Bhatia A, Oberlin C. Surgical correction of pseudo-ainhum in Vohwinkel syndrome. J Hand Surg Br 1995;20:338-41 [DOI] [PubMed] [Google Scholar]
- 18.Prabhu R, Subbaraju Kannan N, Vinoth S, Praveen CB. Ainhum - A Rare Case Report. J Clin Diagn Res 2016;10:PD17-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bassetto F, Tiengo C, Sferrazza R, Belloni-Fortina A, et al. Vohwinkel syndrome: treatment of pseudo-ainhum. Int J Dermatol 2010;49:79-82. [DOI] [PubMed] [Google Scholar]
- 20.Solis RR, Diven DG, Trizna Z. Vohwinkel's syndrome in three generations. J Am Acad Dermatol 2001;44:376-8. [DOI] [PubMed] [Google Scholar]
- 21.Atasoy E. The Reverse Cross Finger Flap. J Hand Surg Am 2016;41:122-8. [DOI] [PubMed] [Google Scholar]


