Abstract
Despite decades of research establishing the importance of breastfeeding, skin‐to‐skin contact and mother–infant closeness, the response to the coronavirus disease 2019 (COVID‐19) pandemic has underscored the hidden assumption that these practices can be dispensed with no consequences to mother or child. This article aims to support shared decision‐making process for infant feeding and care with parents and health care providers during the unprecedented times of the pandemic. It proposes a structure and rationale to guide the process that includes (1) discussing with parents evidence‐based information and the different options to feed and care for an infant and young child in the context of the pandemic as well as their potential benefits, risks and scientific uncertainties; (2) helping parents to recognize the sensitive nature of the decisions and to clarify the value they place on the different options to feed and care for their infant or young child; and (3) providing guidance and support needed to make and implement their decisions. A shared decision‐making process will help parents navigate complex feeding and care decisions for their child as we face the different stages of the COVID‐19 pandemic.
Keywords: breastfeeding, breastfeeding support, childhood infections, COVID‐19, infant and child nutrition, infant and young child feeding in emergencies, infant care, infant feeding decisions, rooming‐in, skin‐to‐skin contact
Key messages.
The response to the COVID‐19 pandemic has underscored the hidden assumption that essential infant‐related practices such as breastfeeding, skin‐to‐skin contact and mother–infant closeness can be dispensed with without consequences.
When deciding on these practices, parents should be supported using a shared decision‐making process. This includes discussing with parents the evidence‐based information together with different options to feed and care for an infant and young child, recognizing the sensitive nature of decisions and providing the support needed.
A shared decision‐making process will help parents navigate complex feeding and care decisions as we face the different stages of the pandemic.
1. INTRODUCTION
Since the World Health Organization (WHO) declared the pandemic coronavirus disease 2019 (COVID‐19) on 11 March 2020, public health organizations and governments worldwide have published guidelines to care for pregnant women, infants and young children. Although the WHO recommends breastfeeding, skin‐to‐skin contact, rooming‐in and maintaining close proximity for mothers with suspected or confirmed COVID‐19 (WHO, 2020a, 2020b, 2020d), some national and professional organizations have differed from the WHO recommendations. For example, the United States (American Academy of Pediatrics, 2020c; Centers for Disease Control and Prevention, 2020), China (Wang et al., 2020) and India (Hethyshi, 2020) initially favoured the option of separation of mothers and infants, not supporting direct breastfeeding (i.e. at the breast) but allowing for provision of expressed milk. Conversely, Canada (Canadian Paediatric Society, 2020b; Public Health Agency of Canada, 2020; The Society of Obstetricians and Gynaecologists of Canada, 2020), Italy (Davanzo et al., 2020) and the United Kingdom (Royal College of Obstetricians and Gynaecologists, 2020) have stayed close to the WHO guidelines. In addition, the United Nations Children's Fund (UNICEF) reported that many low‐ and middle‐income countries continued the implementation of skin‐to‐skin contact, rooming‐in, breast milk expression and breastfeeding counselling, despite the pandemic (UNICEF, 2020).
In general, initial guidance for the COVID‐19 pandemic has privileged a hospital‐centric precautionary approach that has overshadowed breastfeeding as the norm for infant and young child nutrition. Establishment of breastfeeding is difficult without the normal physiology of early and uninterrupted skin‐to‐skin contact, rooming‐in and direct breastfeeding after birth. Separated mothers and infants may be unable to establish breastfeeding even once reunited. Furthermore, most guidelines do not consistently take into consideration that breastfeeding can continue for months or even years, and thus, the great majority of susceptible mothers making ongoing feeding and care decisions for their infants and young children are at home.
Despite decades of research establishing the importance of breastfeeding and the risks of breast milk substitutes (Victora et al., 2016), the pandemic has underscored the hidden assumption that breastfeeding can be dispensed with no consequences to mother or child (Tomori, Gribble, Palmquist, Ververs, & Gross, 2020). This assumption stems from a history in which feeding breast milk substitutes has been for decades common in many countries, during which layers of health policy recommendations were formed and built. As a result, today's breastfeeding rates have not met the international targets (WHO/UNICEF, 2014), and there continues to be a failure to recognize the importance of breastfeeding on infant health, even under nonemergency conditions (Tomori, Gribble, Palmquist, Ververs, & Gross, 2020) or normal times. This leads to a number of unintended consequences that are relevant to the pandemic:
If the general recommendation to breastfeed is not clearly communicated to mothers with COVID‐19 by health care providers, parents are left to make decisions without this guidance. Parents may not be presented with appropriate information as to the true risks of not breastfeeding to mother and infant. A discussion of risks should particularly include the known risks of severe lower respiratory tract infections in infants who are not exclusively breastfed (Bachrach, Schwarz, & Bachrach, 2003; Christensen et al., 2020; Ip et al., 2007), and this risk now also potentially includes the risk of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection.
Much of the negative messaging about the risk to the infant centres only around risk of viral transmission, with little attention to the more relevant issue of risk of clinically significant infection which appears to be uncommon (Dumitriu et al., 2020; Patil et al., 2020; Salvatore et al., 2020; Walker et al., 2020; Woodworth et al., 2020).
Policies of separation of mothers and infants in the health care setting fail to consider that few families have the resources to continue separation at home. Even if separation prevents exposure during the hospital stay, it does not prevent exposure after discharge (Stuebe, 2020). Most evidence shows that there are no adverse outcomes if infants room in with their infected mothers (Dumitriu et al., 2020; Patil et al., 2020; Salvatore et al., 2020; Walker et al., 2020). The only publication opposing this view did not meet the level of evidence sufficient to include in the discussions with parents because separation is not defined (Raschetti et al., 2020).
Recommendations for mothers with COVID‐19 are focused on precautions while breastfeeding rather than on general precautions while in close contact with their infants. Conversely, there have been little guidance and precautions for babies who are fed breast milk substitutes with a bottle even though this mode of feeding also involves close contact, which may put such infants at additional risk.
There were concerns about some initial recommendations based on abundance of precautions (e.g. washing the breast area before each feeding at the breast or wrapping the infant in a towel or blanket to prevent skin‐to‐skin contact while breastfeeding) that would negatively impact breastfeeding (these have since been, for the most part, deleted from the directives).
The abundance of precautions to avoid transmission from COVID‐19 mothers to their babies may spill over onto mothers who are not known to have the infection but nevertheless fear transmitting it to their child. This may interfere with evidence‐based care practices with the potential to cause undue stress to the dyad.
The measures to avoid transmission, such as prolonged lockdowns, increase the prevalence of depression and anxiety during early post‐partum period (Brown & Shenker, 2020; Ceulemans, Hompes, & Foulon, 2020).
In this context, the COVID‐19 era may risk lowering exclusive and nonexclusive breastfeeding rates particularly during the critical period from birth to 6–8 weeks when mothers are known to abandon breastfeeding owing to difficulties and concerns (Charette & Haiek, 2019) and to constraints in accessing in‐person lactation support if needed (Gribble, Marinelli, Tomori, & Gross, 2020; Hull, Kam, & Gribble, 2020). This gap in services may leave an opening for the formula industry to capitalize on the crisis (WHO, 2020c) and to widen the inequities in families more likely to be affected by growing unemployment and sporadic food shortage (Hand & Noble, 2020). Lower breastfeeding rates may have the additional consequence of leaving the infant vulnerable to severe lower respiratory tract infections (Bachrach, Schwarz, & Bachrach, 2003; Christensen et al., 2020; Ip et al., 2007), including COVID‐19, as well as other infections and noncommunicable diseases (WHO European Region, 2020), and may also compromise maternal health (Bartick et al., 2017). As the initial waves of the pandemic shift in many parts of the world, it is imperative to give full consideration not only to the risks of serious morbidity and mortality related to the COVID‐19 crisis but also to the public health crisis that would result if the exclusivity and duration of breastfeeding decline.
This article aims at supporting a shared decision‐making process during the unprecedented times of the COVID‐19 pandemic that could be applicable to other public health emergencies. It addresses parents with concerns about COVID‐19 or mothers with suspected or confirmed infection at the time of delivery or while caring for their young children at home. Munro et al. describe shared decision‐making is a form of nondirective counselling where the health care provider and patient come together as experts, in clinical evidence and lived experience respectively. This division of power shifts the conversation from giving patient education to exchanging information to help the parents reach their goals, balancing the consequences of decisions for the health of both the mother and her infant. The ideal outcome of a shared decision‐making process is a parental decision that is informed, consistent with their personal preferences and values, and acted upon (Munro, Buckett, Sou, Bansback, & Lau, 2019).
Health care providers would benefit from building competencies to support the decision‐making process related to infant care and feeding during the pandemic. The suggested steps to follow are presented based on a framework to structure the process (BFI Strategy for Ontario, 2017; Hamilton et al., 2017; Hospital of Ottawa, 2015) and are presented below. To maintain and expand their competencies on infant feeding and care through emergencies, health care teams are encouraged to assess their continuing educational needs by reviewing emerging or existing tools addressing decision‐making (Hospital of Ottawa, 2015) and breastfeeding (WHO/UNICEF, 2020) as well as other approaches developed specifically to address COVID‐19 (Cheema et al., 2020).
While the term ‘mother’ is used throughout the article, the authors understand that not all parents identify as women or mothers. Health care providers are encouraged to use gender‐inclusive language most acceptable to the parents. Whenever the mother is not physically able to participate in the decision‐making process (e.g. if she is very ill), it is important to include her appointed alternate decision maker.
2. SHARED DECISION‐MAKING PROCESS FOR INFANT CARE AND FEEDING DECISIONS DURING THE PANDEMIC
The suggested shared decision‐making process includes the following steps: (1) discussing with parents evidence‐based information and the different options to feed and care for an infant and young child in the context of the pandemic as well as their potential benefits, risks and scientific uncertainties; (2) helping parents to recognize the sensitive nature of the decision and to clarify the value they place on the different options to feed and care for their infant or young child; and (3) providing guidance and support needed to make and implement their decisions.
2.1. Step 1: Explore what the parents know—‘What have you heard about infant feeding and care during the COVID‐19 pandemic?
Health care providers have the responsibility to provide accurate, evidence‐based information on the consequences of a parent's decisions on their infants' feeding and care, just as on any other health‐related decisions. They should also acknowledge the areas of uncertainty due to the novelty of the virus and the rapidly changing information and evolving understanding of the infection and its transmission.
They should start the conversation by asking open‐ended questions, listening actively and reflecting back to show that they have heard what the parents have said (Hamilton et al., 2017).
Then, they should ask permission to build on what the parents already know, trying to tailor the discussion to their individual needs, clarifying any misunderstandings (evolving information and myths), identifying sources of anxieties and fears and addressing any gaps in essential information needed to make a decision (Hamilton et al., 2017).
The sections below review the evidence that may need to be shared according to the situation of eachdyad. Figure 1 schematizes this information to guide the exchange with mothers with suspected or confirmed COVID‐19 infection or with those without the infection but who are considering taking precautions.
FIGURE 1.
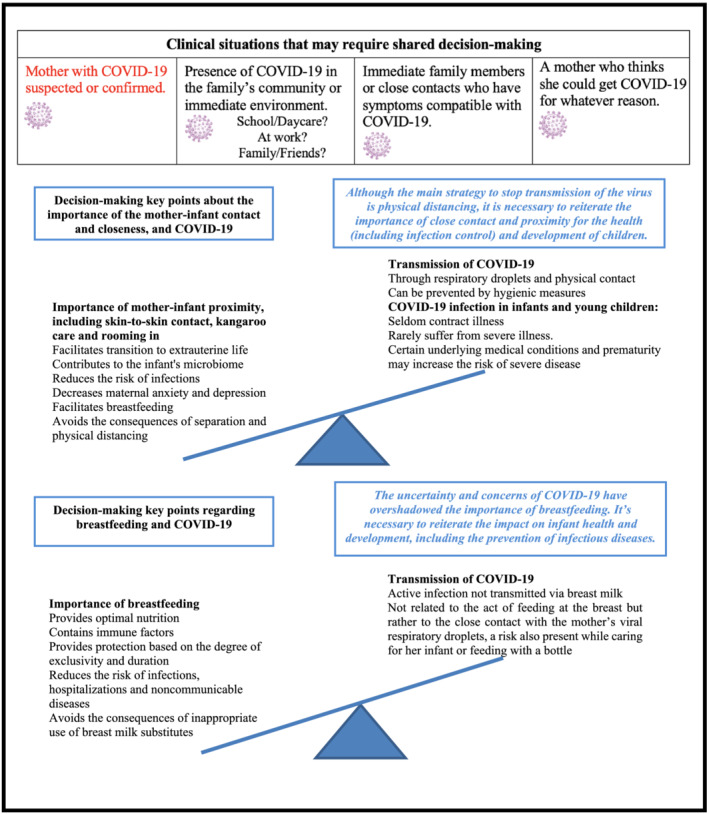
Schematization of elements to exchange with mothers with suspected or confirmed coronavirus disease 2019 (COVID‐19) infection or with those without the infection but who are considering taking precautions
2.1.1. What we currently know about COVID‐19 infection in infants and young children
The risk of transmission from mother with COVID‐19 to her infant or young child
Transmission of the virus from the infected mother to her infant is mainly through respiratory droplets and direct contact, and it is unlikely to occur if hygienic measures are taken (Salvatore et al., 2020; Vogel et al., 2020).
Concerns about transmission related to breastfeeding are not related to the act of suckling milk at the breast but to the risk of respiratory transmission from the mother; a risk is also present if a mother is feeding with a bottle or whenever a mother is caring for her infant.
There is no evidence to date that active infection with SARS‐CoV‐2 can be transmitted via breast milk. Despite reports of detection of SARS‐CoV‐2 RNA in breast milk, detection of viral genetic material does not equate to infectivity by a viable virus (Bastug et al., 2020; Buonsenso et al., 2020; Chambers et al., 2020; Chen et al., 2020; Groß et al., 2020; Kirtsman et al., 2020; Wu et al., 2020). SARS‐CoV‐2 has not been cultured from breast milk (Chambers et al., 2020). Rapid and systematic reviews have not found evidence of transmission of infectious virus to the infant through breast milk (Centeno‐Tablante et al., 2020; Martins‐Filho, Santos, & Santos, 2020; Vogel et al., 2020; WHO, 2020a; Yang et al., 2020) and suggest a low risk of transmission by ingesting breast milk (Centeno‐Tablante et al., 2020).
In order for an infant to acquire COVID‐19, it would require not only the presence of a replicative and infectious virus but also reaching target sites and overwhelming the infant's immune system (WHO, 2020a).
After SARS‐CoV‐2 was experimentally added to breast milk, Holder pasteurization was sufficient to inactivate the virus. This indicates that use of pasteurized donor milk would be safe even in the event that the infectious form of the virus is discovered in the milk (Unger et al., 2020).
Consequence of acquiring COVID‐19 for infants and young children
Studies show that peripartum–postnatal transmission is rare (American Academy of Pediatrics, 2020c, 2020e; Dumitriu et al., 2020; Salvatore et al., 2020) or uncommon (Maraschini, Corsi, Salvatore, Donati, & It, 2020; Marin Gabriel et al., 2020; Patil et al., 2020; Walker et al., 2020), and even larger studies show serious neonatal outcomes are rare (American Academy of Pediatrics, 2020e; Marin Gabriel et al., 2020). The rate of infection is no greater when the newborn is delivered vaginally, breastfed or kept together with the mother (American Academy of Pediatrics, 2020c; Centers for Disease Control and Prevention, 2020; Dumitriu et al., 2020; Patil et al., 2020; Walker et al., 2020).
Moreover, older infants and young children who do contract COVID‐19 seem to get mild or no symptoms and rarely get sick (American Academy of Pediatrics, 2020b; Bixler et al., 2020; Hoang et al., 2020; Kim et al., 2020). The risk of hospitalization, including intensive care, for children under 24 months of age infected with COVID‐19 appears to be higher than for older children (Kim et al., 2020). This is similar to the known risk in infants for several other common respiratory viruses, and it substantiates the possibility that severe disease is the result of coexisting viral infections (Gribble, Marinelli, Tomori, & Gross, 2020). Certain underlying medical conditions and prematurity may increase the risk for severe disease in children (Bixler et al., 2020; Hoang et al., 2020; Kim et al., 2020).
2.1.2. What is known about the importance of the mother–infant contact and closeness, and the risks of separation during the pandemic?
Immediate skin‐to‐skin contact at birth is an unrecoverable moment in the physiology of the transition to extrauterine life. This contact is crucial for the early initiation of suckling at the breast, the regulation of the infant's homeostasis of vital signs and blood glucose levels, and the colonization of the infant's microbiome (WHO/UNICEF, 2018). It also decreases the risk of maternal anxiety in the immediate post‐partum period and depression in the first year after birth (The Society of Obstetricians and Gynaecologists of Canada, 2020).
Rooming‐in enables mothers to recognize and respond to their infants' cues for feeding. This, along with the close presence of the mother to her infant, will facilitate the establishment of breastfeeding (WHO/UNICEF, 2018) and reduce the risk of newborn respiratory infection. Given the significant mental health burden of giving birth during the pandemic, prioritizing close contact for the mother–infant unit is of particular importance (The Society of Obstetricians and Gynaecologists of Canada, 2020).
Infants have a right to be cared for by their parent. Parents should be aware that their infant should not be separated from them except when such separation is necessary for the best interests of the child (Office of the United Nations High Commissioner for Human Rights, 1989). Nevertheless, during the pandemic, policies may be in place that require separation owing to concerns of infection control.
At home, physical closeness between mother and babies continues to be important for the health (including prevention of infections) and development of children. Although the main strategy to stop transmission of the virus is physical distancing, this does not apply to young children. Close contact facilitates the development of positive parent–infant relationships; it can also enhance the parent's confidence and capabilities in providing care for their newborn (Flacking et al., 2012). Responding consistently, quickly and warmly to infant needs or distress is essential for a secure attachment (Canadian Paediatric Society, 2019). Skin‐to‐skin contact (Moore, Bergman, Anderson, & Medley, 2016) and proximity, especially at night‐time, facilitate breastfeeding duration and exclusivity (Blair et al., 2020; L. A. Smith et al., 2016). Keeping infants in the same room as the parents for at least 6 months, or ideally, until 1 year can prevent sudden infant death syndrome (SIDS) (American Academy of Pediatrics, 2020d). Room sharing may support the ability of the infant to arouse, which is considered a physiologically protective factor (failure to arouse makes an infant vulnerable to SIDS) (Moon & Hauck, 2017). Placing the child's sleep surface close to the parent's bed so that the infant is within view and reach can also help make it easier to feed, comfort and monitor the infant (American Academy of Pediatrics, 2020d).
2.1.3. What is known about the protection conferred by breastfeeding and the known risks of not breastfeeding during the pandemic?
The many immune factors in breast milk complement and contribute to the development of the infant's immune system. Breast milk induces the microbiota (intestinal flora) that protect the infant throughout his or her life against several infections or diseases (Victora et al., 2016). In fact, breastfeeding generally confers the infant personalized protection against infections.
Feeding breast milk substitutes increases three‐fold the risk of serious lower respiratory tract infections resulting in hospitalizations. The protection is associated to the degree of exclusivity and duration (Canadian Paediatric Society, 2020a; Christensen et al., 2020); each additional month of exclusive breastfeeding may reduce by as much as 30% hospital admissions secondary to infection, primarily respiratory (Paricio Talayero et al., 2006). Supplementation with infant formula significantly alters the microbiota (Forbes et al., 2018; WHO/UNICEF, 2018).
Increase in breastfeeding exclusivity and duration translates into reduced treatment costs of hospitalizations and childhood disorders (Smith, Thompson, & Ellwood, 2002; Victora et al., 2016).
Antibodies against SARS‐CoV‐2 have been found in breast milk of unvaccinated mothers (Fox et al. 2020) and have not yet been studied in those vaccinated. Further study is needed to confirm their presence and protective effect against COVID‐19.
Breastfeeding ensures optimal nutrition at all times and is readily available during emergencies, and unlike breast milk substitutes, it is not subject to supply chain interruptions. As rising unemployment and poverty due to the pandemic are likely to increase the prevalence of food insecurity (Perez‐Escamilla, Cunningham, & Moran, 2020; Roberton et al., 2020), breastfeeding can help reduce health inequities by ensuring food security (Hand & Noble, 2020). Ethical considerations of using breast milk substitutes should include safety, sustainability and consistent availability including costs during a time of economic uncertainty for many families (Breastfeeding Committee for Canada, 2020).
International and national organizations consistently state that breastfeeding continues to be recommended during the pandemic (American Academy of Pediatrics, 2020a, 2020c; Davanzo et al., 2020; Public Health Agency of Canada, 2020; Royal College of Obstetricians and Gynaecologists, 2020; The Society of Obstetricians and Gynaecologists of Canada, 2020; WHO, 2020d). There is widespread consensus on the importance of providing breast milk to infants of infected mothers, but there are varying directives with respect to direct breastfeeding, which involves close physical contact. WHO and UNICEF continue to recommend direct breastfeeding recognizing that the numerous benefits of breastfeeding substantially outweigh the potential risks of COVID‐19 transmission and illness (UNICEF, 2020; WHO, 2020d).
2.2. Step 2: Explore what value the parents place on the benefits, risk and scientific uncertainties related to infant feeding and care decisions—‘Tell me about any concerns you may have about feeding and caring for your baby?’
Health care providers should help parents recognize the sensitive nature of the decisions around infant feeding and care and clarify the value they place on the benefits, risks and scientific uncertainties. The values to explore could include their views on the long‐term outcomes on the mother and infant's health, protecting against infection ‘at all cost’, financial considerations, etc. To help mothers move forward in the decision‐making, it is also important to explore and acknowledge fears or other emotions that can impair comprehension of the information provided to them. These conversations will vary depending on whether the mother has a COVID‐19 infection or has concerns about contracting it.
For example, a mother with COVID‐19 is trying to decide how to feed her baby and expresses the value of protecting her baby from infection while also sharing her fears of transmitting the infection while feeding at the breast. The health care provider needs to acknowledge these concerns and fears and to clarify with the mother the benefits, risks and scientific uncertainties according to her particular situation. The discussion needs to address the questionable benefit of not feeding at the breast in order to prevent transmission to her infant and revisit the available evidence as described in Step 1. The discussion should also address the harms that could arise, including concerns about risks of complications such as engorgement and mastitis if she decides to wean abruptly, maintaining milk production during the episode of illness if she decides to express milk and expectations about continuing exclusive breastfeeding or reaching breastfeeding goals.
2.3. Step 3: Support parents to make and implement their decision—‘How do you see your situation now and how may I help you?’
Once the parents make a decision that is informed and consistent with their values, health care providers involved in the different aspects of perinatal care should help them reach their goals. The support offered will vary depending on whether the mother is in the hospital/birthing centre or at home as well as on her COVID‐19 status.
2.3.1. In the hospital/birthing centre
Recommendations from national and professional organization have placed emphasis on prevention of infection from COVID‐19 over full consideration of the importance of skin‐to‐skin contact and breastfeeding (WHO, 2020d). Routine clinical practices outlined in the Baby‐friendly Hospital Initiative (WHO/UNICEF, 2018) continue to be recommended, unless justifiable medical indications to the contrary. Particularly, skin‐to‐skin contact for vaginal or caesarean delivery, early initiation of breastfeeding and 24‐h rooming‐in are recommended even if mother is infected at the time of birth and should not be limited or scaled back during the pandemic. The Baby‐friendly Hospital Initiative is intended for all mothers, regardless of their infant feeding decisions.
Table 1 presents the specific hygienic measures currently recommended for mothers with suspected or confirmed COVID‐19 in the hospital setting or birthing centres. Directives may vary in different countries and may evolve over time. Because mothers and infants are kept together whenever possible, the primary concern is to avoid transmitting the infection to the infant via respiratory droplets by following enhanced hygiene (WHO, 2020d; Yang et al., 2020). It is important that mothers understand that the time frame for these precautions only applies while they are infective (WHO, 2020e).
TABLE 1.
Specific measures should apply to mothers with suspected or confirmed COVID‐19 in the hospital/birthing centre or at home (Jones, 2019; Vogel et al., 2020; WHO, 2020d)
| While caring or feeding for her infant and young child at the breast |
Recommended hygienic measures: ° Washing hands before each contact with the infant and breastfeeding. ° Wearing a medical mask if available when close to the infant (less than 2 m) or expressing her breast milk. Even if the mother does not have a medical mask, breastfeeding should be continued. ° Routinely cleaning and disinfecting surfaces that the mother has touched. |
| While expressing breast milk by hand or pump |
Recommended hygienic measures: ° Washing hands before expressing her breast milk. ° If a breast pump is used, all components that can be cleaned must be disassembled and rinsed with lukewarm water, washed with hot water and soap, rinsed with hot water and dried with a clean cloth or paper towel. The surfaces of the breast pump should be disinfected. ° If bottles and nipples are used, cleaning and disinfection are required as usual. |
| While in isolation |
Recommended measures for isolation: ° In the hospital or birthing centre, if space permits, mothers should be counselled about the possible decreased risk of transmission of the virus to her infant if she keeps 2 m of distance in the same room (when she is not feeding or caring for her infant) versus the possible increased difficulties with breastfeeding and bonding by doing so. If mothers do not have space to maintain such distance in their own homes, maintaining such a distance in the hospital may not provide benefit. ° Mothers isolating at home should be physically distancing, if possible, from other healthy members in the household, with the only exception being their infant or young child. ○ If the mother is too sick to feed or care for her infant and young child, another person in the household can do it following the same hygienic measures. |
| Time frame to apply measures | While the period the mother is infective, this may depend on the presence and duration of symptoms and may vary according to national or local directives. |
Abbreviation: COVID‐19, coronavirus disease 2019.
If a mother with suspected or confirmed COVID‐19 is too ill—or is not able—to breastfeed, the best alternatives to breastfeeding a newborn or young infant are the mother's expressed breast milk, pasteurized donor human milk and lastly breast milk substitutes if neither are available.
Mothers with COVID‐19 of an infant admitted to the neonatal or paediatric intensive care unit in which infection prevention and control measures may prevent their presence in the unit should be encouraged to express their breast milk and provide it to the unit. These mothers should be advised to express breast milk frequently, with a view towards achieving successful breastfeeding once she is able to be reunited with her infant. Although separation is required, mothers could be offered to connect with their baby through virtual modalities and consider the need for mental health and psychosocial support (Breastfeeding Committee for Canada, 2020; Canadian Paediatric Society, 2020b).
2.3.2. At home
If COVID‐19 is prevalent in their community or in their close environment (e.g. work setting or day care services) or if family members present COVID‐19‐related symptoms or if a mother thinks she might have COVID‐19, health care providers should inform them that there is no reason to physically distance from their infant or to avoid or stop breastfeeding. However, mothers that have suspected or confirmed COVID‐19 must be counselled on implementing the hygiene measures described in Table 1. Furthermore, health care providers can address these situations by revisiting the pertinent stages of the shared decision‐making process.
Throughout the period that the mother breastfeeds, skilled health care providers must be available to answer questions or address issues. During a pandemic and other emergency situations, accessibility to infant feeding support services may be impacted. Decreasing breastfeeding services is a result of health systems shifting to manage COVID‐19 cases and maternal health care‐seeking behaviours affected by lockdowns or concerns of contracting the disease while seeking health services (UNICEF, 2020). This lack of services is likely to be felt more in families at socio‐economic risk, exacerbating existing health inequities (Akseer, Kandru, Keats, & Bhutta, 2020; Brown & Shenker, 2020; Roberton et al., 2020).
When consulted, providers should conduct a structured clinical assessment (Charette & Haiek, 2019), either by telephone or videoconference or in person (e.g. significant breastfeeding difficulties in the newborn or doubts about the infant's weight gain). It may also be possible to support mothers that decide to resume breastfeeding (relactation) after breastfeeding is discontinued. These interactions could be used to screen for and provide psychological support or refer to appropriate resources, if needed. Moreover, involving parents in the process is likely to result in less uncertainty, anxiety and decisional regret (Vlemmix et al., 2013).
3. CONCLUSION
The COVID‐19 pandemic has heightened the importance of a tailored approach in which parents consider complex feeding and care decisions for their child. These decisions can have a lifelong effect on the health of infants and young children as well as of their mothers.
When counselling families, it is important to convey the message that breastfeeding and close contact between mothers and their infants and young children are recommended during the COVID‐19 pandemic, even if the mother is affected by the virus.
Health care providers should identify their needs for capacity building on competencies related to infant feeding and shared decision‐making. This will allow them to support the decision process respecting parents' values, sharing evidence‐based information and advising on the hygienic measures when needed. A shared decision‐making process will help health care providers and families move forward together as we face the different stages of the COVID‐19 pandemic.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interests.
CONTRIBUTIONS
All authors contributed in writing the paper.
ACKNOWLEDGMENTS
The authors would like to thank Ghislaine Reid, IBCLC, as well as parents Candi Edwards, IBCLC, and Claire Gallant for their help in revising and commenting on the manuscript.
Haiek LN, LeDrew M, Charette C, Bartick M. Shared decision‐making for infant feeding and care during the coronavirus disease 2019 pandemic. Matern Child Nutr. 2021;17:e13129. 10.1111/mcn.13129
REFERENCES
- Akseer, N. , Kandru, G. , Keats, E. C. , & Bhutta, Z. A. (2020). COVID‐19 pandemic and mitigation strategies: Implications for maternal and child health and nutrition. The American Journal of Clinical Nutrition, 112(2), 251–256. 10.1093/ajcn/nqaa171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Pediatrics . (2020a, November 16). Breastfeeding guidance post hospital discharge for mothers or infants with suspected or confirmed SARS‐Co V‐2 infection (updated July 29 and September 18, 2020). Retrieved from https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/breastfeeding-guidance-post-hospital-discharge/
- American Academy of Pediatrics . (2020b, November 16). Children and COVID‐19: State‐level data report (updated November 16, 2020). Retrieved from https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/
- American Academy of Pediatrics . (2020c, November 16). FAQs: Management of infants born to mothers with suspected or confirmed COVID‐19 (updated May 21, 2020, July 22 and September 10, 2020). Retrieved from https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/faqs-management-of-infants-born-to-covid-19-mothers/
- American Academy of Pediatrics . (2020d, November 16). How to keep your sleeping baby safe: AAP policy explained (updated February 10, 2020). Retrieved from https://www.healthychildren.org/English/ages-stages/baby/sleep/Pages/A-Parents-Guide-to-Safe-Sleep.aspx
- American Academy of Pediatrics . (2020e). Section on neonatal and perinatal medicine. NPC‐19 Registry, updated 10/3/20 infographic 2020 (updated November 15, 2020). Retrieved from https://my.visme.co/view/ojq9qq8e-npc-19-registry
- Bachrach, V. R. , Schwarz, E. , & Bachrach, L. R. (2003). Breastfeeding and the risk of hospitalization for respiratory disease in infancy: A meta‐analysis. Archives of Pediatrics & Adolescent Medicine, 157(3), 237–243. 10.1001/archpedi.157.3.237 [DOI] [PubMed] [Google Scholar]
- Bartick, M. C. , Schwarz, E. B. , Green, B. D. , Jegier, B. J. , Reinhold, A. G. , Colaizy, T. T. , … Stuebe, A. M. (2017). Suboptimal breastfeeding in the United States: Maternal and pediatric health outcomes and costs. Maternal & Child Nutrition, 13(1). 10.1111/mcn.12366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastug, A. , Hanifehnezhad, A. , Tayman, C. , Ozkul, A. , Ozbay, O. , Kazancioglu, S. , & Bodur, H. (2020). Virolactia in an asymptomatic mother with COVID‐19. Breastfeeding Medicine, 15(8), 488–491. 10.1089/bfm.2020.0161 [DOI] [PubMed] [Google Scholar]
- BFI Strategy for Ontario . (2017, November 16). Informed decision making: Having meaningful conversations regarding infant feeding. Retrieved from https://breastfeedingresourcesontario.ca/resource/informed-decision-making-having-meaningful-conversations-regarding-infant-feeding
- Bixler, D. , Miller, A. D. , Mattison, C. P. , Taylor, B. , Komatsu, K. , Peterson Pompa, X. , … Pediatric Mortality Investigation Team (2020). SARS‐CoV‐2‐associated deaths among persons aged <21 years—United States, February 12–July 31, 2020. MMWR. Morbidity and Mortality Weekly Report, 69(37), 1324–1329. 10.15585/mmwr.mm6937e4 [DOI] [PubMed] [Google Scholar]
- Blair, P. S. , Ball, H. L. , McKenna, J. J. , Feldman‐Winter, L. , Marinelli, K. A. , Bartick, M. C. , & Academy of Breastfeeding, M . (2020). Bedsharing and breastfeeding: The academy of breastfeeding medicine protocol #6, revision 2019. Breastfeeding Medicine, 15(1), 5–16. 10.1089/bfm.2019.29144.psb [DOI] [PubMed] [Google Scholar]
- Breastfeeding Committee for Canada . (2020, November 16). Key messages: Infant feeding and COVID‐19. Retrieved from https://breastfeedingcanada.ca/en/
- Brown, A. , & Shenker, N. (2020). Experiences of breastfeeding during COVID‐19: Lessons for future practical and emotional support. Maternal & Child Nutrition, 17(1), e13088. 10.1111/mcn.13088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buonsenso, D. , Costa, S. , Sanguinetti, M. , Cattani, P. , Posteraro, B. , Marchetti, S. , … Valentini, P. (2020). Neonatal late onset infection with severe acute respiratory syndrome coronavirus 2. American Journal of Perinatology, 37, 869–872. 10.1055/s-0040-1710541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Paediatric Society . (2019, November 16). Relationships matter: How clinicians can support positive parenting in the early years. Retrieved from https://www.cps.ca/en/documents/position/positive-parenting#ref38 [DOI] [PMC free article] [PubMed]
- Canadian Paediatric Society . (2020a, November 16). The Baby‐Friendly Initiative: Protecting, promoting and supporting breastfeeding (updated January 1, 2020). Retrieved from https://www.cps.ca/en/documents/position/baby-friendly-initiative-breastfeeding [PMC free article] [PubMed]
- Canadian Paediatric Society . (2020b, November 16). Breastfeeding when mothers have suspected or proven COVID‐19 (Updated May 6 and November 16, 2020). Retrieved from https://www.cps.ca/en/documents/position/breastfeeding-when-mothers-have-suspected-or-proven-covid-19
- Centeno‐Tablante, E. , Medina‐Rivera, M. , Finkelstein, J. L. , Rayco‐Solon, P. , Garcia‐Casal, M. N. , Rogers, L. , … Mehta, S. (2020). Transmission of SARS‐CoV‐2 through breast milk and breastfeeding: A living systematic review. Annals of the New York Academy of Sciences. 10.1111/nyas.14477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2020, November 16). Evaluation and management considerations for neonates at risk for COVID‐19 (Updated May 20, 2020, August 3, 2020, and October 23). Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/hcp/caring-for-newborns.html
- Ceulemans, M. , Hompes, T. , & Foulon, V. (2020). Mental health status of pregnant and breastfeeding women during the COVID‐19 pandemic: A call for action. International Journal of Gynecology & Obstetrics, 151(1), 146–147. 10.1002/ijgo.13295 [DOI] [PubMed] [Google Scholar]
- Chambers, C. D. , Krogstad, P. , Bertrand, K. , Contreras, D. , Bode, L. , Tobin, N. , & Aldrovandi, G. (2020). Evaluation of SARS‐CoV‐2 in breastmilk from 18 infected women. medRxiv, 324(13), 1347–1348. 10.1101/2020.06.12.20127944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charette, C. , & Haiek, L. N. (2019). Allaitement et période critique. L'urgence d'agir dès une difficulté ! Le Médecin du Québec, 54(12), 23–28. [Google Scholar]
- Cheema, R. , Partridge, E. , Kair, L. R. , Kuhn‐Riordon, K. M. , Silva, A. I. , Bettinelli, M. E. , … Blumberg, D. (2020). Protecting breastfeeding during the COVID‐19 pandemic. American Journal of Perinatology. 10.1055/s-0040-1714277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, H. , Guo, J. , Wang, C. , Luo, F. , Yu, X. , Zhang, W. , … Zhang, Y. (2020). Clinical characteristics and intrauterine vertical transmission potential of COVID‐19 infection in nine pregnant women: A retrospective review of medical records. Lancet, 395(10226), 809–815. 10.1016/S0140-6736(20)30360-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen, N. , Bruun, S. , Sondergaard, J. , Christesen, H. T. , Fisker, N. , Zachariassen, G. , … Husby, S. (2020). Breastfeeding and Infections in early childhood: A cohort study. Pediatrics, 146(5), e20191892. 10.1542/peds.2019-1892 [DOI] [PubMed] [Google Scholar]
- Davanzo, R. , Moro, G. , Sandri, F. , Agosti, M. , Moretti, C. , & Mosca, F. (2020). Breastfeeding and coronavirus disease‐2019: Ad interim indications of the Italian Society of Neonatology endorsed by the Union of European Neonatal & Perinatal Societies. Maternal & Child Nutrition, 16(3), e13010. 10.1111/mcn.13010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumitriu, D. , Emeruwa, U. N. , Hanft, E. , Liao, G. V. , Ludwig, E. , Walzer, L. , … Gyamfi‐Bannerman, C. (2020). Outcomes of neonates born to mothers with severe acute respiratory syndrome coronavirus 2 infection at a large medical center in New York City. JAMA Pediatrics. 10.1001/jamapediatrics.2020.4298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flacking, R. , Lehtonen, L. , Thomson, G. , Axelin, A. , Ahlqvist, S. , Moran, V. H. , … Closeness Experiences in the Neonatal Environment, g . (2012). Closeness and separation in neonatal intensive care. Acta Paediatrica, 101(10), 1032–1037. 10.1111/j.1651-2227.2012.02787.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes, J. D. , Azad, M. B. , Vehling, L. , Tun, H. M. , Konya, T. B. , Guttman, D. S. , … Canadian Healthy Infant Longitudinal Development Study, I . (2018). Association of exposure to formula in the hospital and subsequent infant feeding practices with gut microbiota and risk of overweight in the first year of life. JAMA Pediatrics, 172(7), e181161. 10.1001/jamapediatrics.2018.1161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox, A. , Marino, J. , Amanat, F. , Krammer, F. , Hahn‐Holbrook, J. , Zolla‐Pazner, S. , & Powell, R. L. (2020). Evidence of a significant secretory‐IgA‐dominant SARS‐CoV‐2 immune response in human milk following recovery from COVID‐19. medRxiv, 2020.2005.2004.20089995. 10.1101/2020.05.04.20089995 [DOI] [Google Scholar]
- Gribble, K. , Marinelli, K. A. , Tomori, C. , & Gross, M. S. (2020). Implications of the COVID‐19 pandemic response for breastfeeding, maternal caregiving capacity and infant mental health. Journal of Human Lactation, 890334420949514, 36, 591–603. 10.1177/0890334420949514 [DOI] [PubMed] [Google Scholar]
- Groß, R. , Conzelmann, C. , Müller, J. A. , Stenger, S. , Steinhart, K. , Kirchhoff, F. , & Münch, J. (2020). Detection of SARS‐CoV‐2 in human breastmilk. Lancet, 395(10239), 1757–1758. 10.1016/s0140-6736(20)31181-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton, J. G. , Lillie, S. E. , Alden, D. L. , Scherer, L. , Oser, M. , Rini, C. , … Waters, E. A. (2017). What is a good medical decision? A research agenda guided by perspectives from multiple stakeholders. Journal of Behavioral Medicine, 40(1), 52–68. 10.1007/s10865-016-9785-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hand, I. L. , & Noble, L. (2020). Covid‐19 and breastfeeding: what's the risk? Journal of Perinatology, 40(10), 1459–1461. 10.1038/s41372-020-0738-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hethyshi, R. (2020). Breast feeding in suspected or confirmed cases of COVID 19—A new perspective. The Journal of Obstetrics and Gynecology of India, 70(4), 267–271. 10.1007/s13224-020-01336-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoang, A. , Chorath, K. , Moreira, A. , Evans, M. , Burmeister‐Morton, F. , Burmeister, F. , … Moreira, A. (2020). COVID‐19 in 7780 pediatric patients: A systematic review. EClinicalMedicine, 24, 100433. 10.1016/j.eclinm.2020.100433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hospital of Ottawa . (2015, November 16). Ottawa Decision Support Framework (ODSF). Retrieved from https://decisionaid.ohri.ca/odsf.html
- Hull, N. , Kam, R. L. , & Gribble, K. D. (2020). Providing breastfeeding support during the COVID‐19 pandemic: Concerns of mothers who contacted the Australian Breastfeeding Association. medRxiv, 2020.2007.2018.20152256. 10.1101/2020.07.18.20152256 [DOI] [Google Scholar]
- Ip, S. , Chung, M. , Raman, G. , Chew, P. , Magula, N. , DeVine, D. , Trikalinos T, Lau, J. (2007). Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep)(153), 1‐186. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/17764214 [PMC free article] [PubMed] [Google Scholar]
- Jones, F. (2019). Best practice for expressing, storing and handling human milk in hospitals, homes and child care settings (4th edition ed.). Fort Worth, Texas: Human Milk Banking Association of North America. [Google Scholar]
- Kim, L. , Whitaker, M. , O'Halloran, A. , Kambhampati, A. , Chai, S. J. , Reingold, A. , … Team, C.‐N. S . (2020). Hospitalization rates and characteristics of children aged <18 years hospitalized with laboratory‐confirmed COVID‐19—COVID‐NET, 14 States, March 1–July 25, 2020. MMWR. Morbidity and Mortality Weekly Report, 69(32), 1081–1088. 10.15585/mmwr.mm6932e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirtsman, M. , Diambomba, Y. , Poutanen, S. M. , Malinowski, A. K. , Vlachodimitropoulou, E. , Parks, W. T. , … Shah, P. S. (2020). Probable congenital SARS‐CoV‐2 infection in a neonate born to a woman with active SARS‐CoV‐2 infection. Canadian Medical Association Journal, 192(24), E647–E650. 10.1503/cmaj.200821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maraschini, A. , Corsi, E. , Salvatore, M. A. , Donati, S. , & It, O. S. S. C.‐W. G . (2020). Coronavirus and birth in Italy: Results of a national population‐based cohort study. Annali dell'Istituto Superiore di Sanità, 56(3), 378–389. 10.4415/ANN_20_03_17 [DOI] [PubMed] [Google Scholar]
- Marin Gabriel, M. A. , Reyne Vergeli, M. , Caserio Carbonero, S. , Sole, L. , Carrizosa Molina, T. , Rivero Calle, I. , … Neo, C.‐R. G. (2020). Maternal, perinatal and neonatal outcomes with COVID‐19: A multicenter study of 242 pregnancies and their 248 infant newborns during their first month of life. The Pediatric Infectious Disease Journal, 39(12), e393–e397. 10.1097/INF.0000000000002902 [DOI] [PubMed] [Google Scholar]
- Martins‐Filho, P. R. , Santos, V. S. , & Santos, H. P. Jr. (2020). To breastfeed or not to breastfeed? Lack of evidence on the presence of SARS‐CoV‐2 in breastmilk of pregnant women with COVID‐19. Revista Panamericana de Salud Pública, 44, e59. 10.26633/RPSP.2020.59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon, R. Y. , & Hauck, F. R. (2017). Are there long‐term consequences of room‐sharing during infancy? Pediatrics, 140(1), e20171323. 10.1542/peds.2017-1323 [DOI] [PubMed] [Google Scholar]
- Moore, E. R. , Bergman, N. , Anderson, G. C. , & Medley, N. (2016). Early skin‐to‐skin contact for mothers and their healthy newborn infants. Cochrane Database of Systematic Reviews, 11, CD003519. 10.1002/14651858.CD003519.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munro, S. , Buckett, C. , Sou, J. , Bansback, N. , & Lau, H. (2019). Shared decision making and breastfeeding: Supporting families' informed choices. British Columbia Medical Journal, 61(10), 394. Retrieved from. https://www.bcmj.org/bccdc/shared-decision-making-and-breastfeeding-supporting-families-informed-choices [Google Scholar]
- Office of the United Nations High Commissioner for Human Rights . (1989, November 16). Convention on the rights of the child. Retrieved from http://www.ohchr.org/en/professionalinterest/pages/crc.aspx
- Paricio Talayero, J. M. , Lizán‐García, M. , Otero Puime, A. , Benlloch Muncharaz, M. J. , Beseler Soto, B. , Sánchez‐Palomares, M. , … Rivera, L. L. (2006). Full breastfeeding and hospitalization as a result of infections in the first year of life. Pediatrics, 118(1), e92–e99. 10.1542/peds.2005-1629 [DOI] [PubMed] [Google Scholar]
- Patil, U. P. , Maru, S. , Krishnan, P. , Carroll‐Bennett, R. , Sanchez, J. , Noble, L. , & Wasserman, R. (2020). Newborns of COVID‐19 mothers: Short‐term outcomes of colocating and breastfeeding from the pandemic's epicenter. Journal of Perinatology, 40(10), 1455–1458. 10.1038/s41372-020-0765-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez‐Escamilla, R. , Cunningham, K. , & Moran, V. H. (2020). COVID‐19 and maternal and child food and nutrition insecurity: A complex syndemic. Maternal & Child Nutrition, 16(3), e13036. 10.1111/mcn.13036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health Agency of Canada . (2020, November 16). Pregnancy, childbirth and caring for newborns: Advice for mothers during COVID‐19 (updated June 1, 2020). Retrieved from https://www.canada.ca/en/public-health/services/publications/diseases-conditions/pregnancy-advise-mothers.html
- Raschetti, R. , Vivanti, A. J. , Vauloup‐Fellous, C. , Loi, B. , Benachi, A. , & De Luca, D. (2020). Synthesis and systematic review of reported neonatal SARS‐CoV‐2 infections. Nature Communications, 11(1), 5164. 10.1038/s41467-020-18982-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberton, T. , Carter, E. D. , Chou, V. B. , Stegmuller, A. R. , Jackson, B. D. , Tam, Y. , … Walker, N. (2020). Early estimates of the indirect effects of the COVID‐19 pandemic on maternal and child mortality in low‐income and middle‐income countries: a modelling study. The Lancet Global Health, 8(7), e901–e908. 10.1016/S2214-109X(20)30229-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royal College of Obstetricians and Gynaecologists . (2020, November 16). Coronavirus infection and pregnancy . Retrieved from https://www.rcog.org.uk/en/guidelines-research-services/guidelines/coronavirus-pregnancy/covid-19-virus-infection-and-pregnancy/#infectionpost
- Salvatore, C. M. , Han, J. Y. , Acker, K. P. , Tiwari, P. , Jin, J. , Brandler, M. , … DeLaMora, P. (2020). Neonatal management and outcomes during the COVID‐19 pandemic: An observation cohort study. Lancet Child Adolesc Health., 4, 721–727. 10.1016/S2352-4642(20)30235-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, J. P. , Thompson, J. F. , & Ellwood, D. A. (2002). Hospital system costs of artificial infant feeding: estimates for the Australian Capital Territory. Australian and New Zealand Journal of Public Health, 26(6), 543–551. 10.1111/j.1467-842x.2002.tb00364.x [DOI] [PubMed] [Google Scholar]
- Smith, L. A. , Geller, N. L. , Kellams, A. L. , Colson, E. R. , Rybin, D. V. , Heeren, T. , & Corwin, M. J. (2016). Infant sleep location and breastfeeding practices in the United States, 2011–2014. Academic Pediatrics, 16(6), 540–549. 10.1016/j.acap.2016.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuebe, A. (2020). Should infants be separated from mothers with COVID‐19? First, do no harm. Breastfeeding Medicine, 15(5), 351–352. 10.1089/bfm.2020.29153.ams [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Society of Obstetricians and Gynaecologists of Canada . (2020, November 16). Committee opinion no. 400—COVID‐19 in pregnancy (updated May 14, 2020). Retrieved from https://www.sogc.org/en/content/featured-news/Committee-Opinion-No-400%E2%80%93COVID-19-in-Pregnancy-updated-May-14-2020.aspx
- Tomori, C. , Gribble, K. , Palmquist, A. E. L. , Ververs, M.‐T. , & Gross, M. S. (2020). When separation is not the answer: Breastfeeding mothers and infants affected by COVID‐19. Maternal & Child Nutrition, 16(4), e13033. 10.1111/mcn.13033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger, S. , Christie‐Holmes, N. , Guvenc, F. , Budylowski, P. , Mubareka, S. , Gray‐Owen, S. D. , & O'Connor, D. L. (2020). Holder pasteurization of donated human milk is effective in inactivating SARS‐CoV‐2. CMAJ, 192, E871–E874. 10.1503/cmaj.201309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . (2020). Adoption of breastfeeding recommendations in the context of COVID‐19. Key findings from an online survey in low and middle‐income countries. November 16. Retrieved from https://mcusercontent.com/fb1d9aabd6c823bef179830e9/files/3a61b1ba-9a63-4500-a672-ed743fcfd904/Breastfeeding_survey_COVID19_Brief_final.pdf
- Victora, C. G. , Bahl, R. , Barros, A. J. D. , França, G. V. A. , Horton, S. , Krasevec, J. , … Rollins, N. C. (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. The Lancet, 387(10017), 475–490. 10.1016/S0140-6736(15)01024-7 [DOI] [PubMed] [Google Scholar]
- Vlemmix, F. , Warendorf, J. K. , Rosman, A. N. , Kok, M. , Mol, B. W. , Morris, J. M. , & Nassar, N. (2013). Decision aids to improve informed decision‐making in pregnancy care: A systematic review. BJOG, 120(3), 257–266. 10.1111/1471-0528.12060 [DOI] [PubMed] [Google Scholar]
- Vogel, J. P. , Tendal, B. , Giles, M. , Whitehead, C. , Burton, W. , Chakraborty, S. , … National, C.‐C. E. T . (2020). Clinical care of pregnant and postpartum women with COVID‐19: Living recommendations from the National COVID‐19 Clinical Evidence Taskforce. The Australian & New Zealand Journal of Obstetrics & Gynaecology, 1–12. 10.1111/ajo.13270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker, K. F. , O'Donoghue, K. , Grace, N. , Dorling, J. , Comeau, J. L. , Li, W. , & Thornton, J. G. (2020). Maternal transmission of SARS‐COV‐2 to the neonate, and possible routes for such transmission: A systematic review and critical analysis. BJOG: An International Journal of Obstetrics & Gynaecology, 127(11), 1324–1336. 10.1111/1471-0528.16362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, L. , Shi, Y. , Xiao, T. , Fu, J. , Feng, X. , Mu, D. , … Control of the novel coronavirus, I . (2020). Chinese expert consensus on the perinatal and neonatal management for the prevention and control of the 2019 novel coronavirus infection (first edition). Ann Transl Med, 8(3), 47. 10.21037/atm.2020.02.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodworth, K. R. , Olsen, E. O. , Neelam, V. , Lewis, E. L. , Galang, R. R. , Oduyebo, T. , … Infant Linked Outcomes, T . (2020). Birth and infant outcomes following laboratory‐confirmed SARS‐CoV‐2 infection in pregnancy—SET‐NET, 16 Jurisdictions, March 29–October 14, 2020. MMWR. Morbidity and Mortality Weekly Report, 69(44), 1635–1640. 10.15585/mmwr.mm6944e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2020a, November 16). Breastfeeding and COVID‐19 (June 23, 2020). Retrieved from https://www.who.int/news-room/commentaries/detail/breastfeeding-and-covid-19
- World Health Organization . (2020b, November 16). Clinical management of COVID‐19 (updated May 27, 2020). Retrieved from https://www.who.int/publications/i/item/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected
- World Health Organization . (2020c, November 16). Countries failing to stop harmful marketing of breast‐milk substitutes, warn WHO and UNICEF (May 27, 2020). Retrieved from https://www.who.int/news-room/detail/27-05-2020-countries-failing-to-stop-harmful-marketing-of-breast-milk-substitutes-warn-who-and-unicef
- World Health Organization . (2020d, November 16). Frequently asked questions: Breastfeeding and COVID‐19 for health care workers (updated May 12, 2020). Retrieved from https://www.who.int/publications/m/item/frequently-asked-questions-breastfeeding-and-covid-19
- World Health Organization . (2020e, November 16). Home care for patients with suspected or confirmed COVID‐19 and management of their contacts (released August 13, 2020). Retrieved from https://www.who.int/publications/i/item/home-care-for-patients-with-suspected-novel-coronavirus-(ncov)-infection-presenting-with-mild-symptoms-and-management-of-contacts
- World Health Organization European Region . (2020, November 16). COVID‐19 and breastfeeding—Position paper (April 8, 2020). Retrieved from https://www.euro.who.int/en/health‐topics/health‐emergencies/coronavirus‐covid‐19/technical‐guidance/2020/covid‐19‐and‐breastfeeding‐position‐paper,‐8‐april‐2020‐produced‐by‐the‐who‐european‐region?fbclid=IwAR0a‐XV538cLX0kPV3Ioqt5FUVTecMh9phFgWldjF3Fnv1YPeLC4TBMZ6Rs
- World Health Organization/UNICEF . (2014). Global nutrition targets 2025: Breastfeeding policy brief. November 16. Retrieved from https://www.who.int/nutrition/publications/globaltargets2025_policybrief_breastfeeding/en/
- World Health Organization/UNICEF . (2018, November 16). Implementation guidance: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services—The revised Baby‐friendly Hospital Initiative. Retrieved from https://www.who.int/nutrition/publications/infantfeeding/bfhi-implementation/en/
- World Health Organization/UNICEF . (2020, November 16). Competency verification toolkit: Ensuring competency of direct care providers to implement the Baby‐friendly Hospital Initiative. Retrieved from https://www.who.int/publications/i/item/9789240008854
- Wu, Y. , Liu, C. , Dong, L. , Zhang, C. , Chen, Y. , Liu, J. , … Huang, H. (2020). Coronavirus disease 2019 among pregnant Chinese women: Case series data on the safety of vaginal birth and breastfeeding. BJOG: An International Journal of Obstetrics & Gynaecology, 127(9), 1109–1115. 10.1111/1471-0528.16276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, N. , Che, S. , Zhang, J. , Wang, X. , Tang, Y. , Wang, J. , … o. b. o . (2020). Breastfeeding of infants born to mothers with COVID‐19: A rapid review. Annals of Translational Medicine, 8(10), 618. Retrieved from. http://atm.amegroups.com/article/view/43613, 10.21037/atm-20-3299 [DOI] [PMC free article] [PubMed] [Google Scholar]


