Abstract
Objective
Delayed revascularisation in patients with ST‐segment elevation myocardial infarction (STEMI) is associated with poor prognosis. The aim of this study is to investigate how the timeline in STEMI treatment was affected during the Covid‐19 outbreak.
Method
Consecutive 165 STEMI patients were enrolled in the study during the Covid‐19 pandemic period (Pandemic period) and the prepandemic period (Control period). The time period until patients' leaving their current position after the onset of pain (home delay), the time from the onset of pain to the first medical contact (FMC delay), door‐to‐balloon time, procedure time and hospitalisation time were recorded.
Results
A total of 165 patients, 82 in the Pandemic period and 83 in the Control period, were included in the study. When compared with the control period, home delay [30 (5‐6912) minutes vs 165 (10‐360) minutes, P < .001] and FMC delay [61 (20‐6932) minutes vs 190 (15‐3660) minutes, P < .001] were significantly prolonged during the pandemic period. In addition, non‐IRA PCI rate (8.8% vs 19.3% P = .043) and hospitalisation time [71 (15‐170) vs 74.2 (37‐329) hours, P = .045] were decreased.
Conclusion
During the Covid‐19 pandemic period, prolonged prehospital time parameters were observed in STEMI patients. Therefore, additional measures may be required to prevent unfavourable delays in STEMI patients during the outbreak.
1. INTRODUCTION
Acute ST‐segment elevation MI (STEMI) is the most dramatic clinical presentation of atherosclerotic heart disease. Rapid myocardial injury usually occurs caused by an acute occluded coronary artery. Since the myocardial damage is irreversible most of the time, the infarct‐related artery (IRA) should be recanalised immediately. 1 , 2 Therefore, current guidelines strongly recommend a time‐dependent algorithm from the onset of symptoms. 3 However, the time lost between symptom onset and treatment initiation interacts with many factors connected to both the patient and the healthcare system. 4 , 5
The coronavirus disease (COVID‐19), which started in Wuhan, China, in December 2019, has turned into a worldwide pandemic. 6 As of May 10, around 4 million people became infected and nearly three hundred thousand people died globally as a result of the spread of the virus. 7 As a definitive treatment and vaccine against Covid‐19 virus has not been developed yet, it has become the main policy to prevent the spread of the virus through social isolation worldwide. Patients were especially advised to stay away from environments such as hospitals with high contact risk, as much as possible. Therefore, isolation recommendations during the Covid‐19 outbreak may have negatively affected the time curve of STEMI patients. In a recent cohort, it was observed that there was a significant decrease in the rate of patients admitted to the hospital in the first 48 hours after lockdown because of Covid‐19. 8 In the study presented, the pre‐ and postpandemic time parameters of STEMI patients in our region were examined.
2. METHOD
2.1. Study population
This study consisted of patients with STEMI undergoing primary percutaneous coronary intervention (PPCI) at 3 different hospitals capable of 24/7 PPCI of Turkey: Samsun Ondokuz Mayis University; Samsun Education and Research Hospital; Sivas Cumhuriyet University. The patients were divided into 2 groups according to the time period they applied. STEMI patients who admitted during the Covid‐19 pandemic period were considered as Covid‐19 group (Pandemic period) and patients who applied before the pandemic were considered as Control group (Control period). The period after 10 March 2020, in which the first Covid‐19 case was reported in our country, was accepted as the Pandemic period and the period before 13 January 2020, when the Covid‐19 outbreak in the world was first described as pandemic, was accepted as the Pre‐pandemic period. After March 10, 2020, patients were enrolled in the study forwards, and before January 13, 2020, they were enrolled backwards consecutively. Acute stent thrombosis, patients over 85 years of age, patients who had MI during hospitalisation and patients who refused treatment were excluded from the study.
Delays in the period from the onset of the STEMI symptoms of patients included in the study until they were discharged from the hospital, the mode of transportation to the PCI centre, revascularisation strategy and some angiographic parameters were recorded.
2.2. Time definitions
Home delay was defined as the time in minutes from the onset of pain until patients’ leaving their current position. FMC delay was defined as the time in minutes from the onset of pain to the first medical contact. Door‐to‐balloon time was defined as the time starting with the arrival of patients at a PCI‐capable hospital and ending when a catheter guide‐wire crosses the infarct‐related artery. Procedure time was defined as the time in minutes from the first image to the last image in PCI records.
2.3. Definitions of Covid‐19 status
During the pandemic period, patients were evaluated in 3 categories according to the clinical and laboratory results at the time of admission: Considered Covid‐19 Negative: Patients without respiratory symptoms, fever and suspected contact; Suspected Covid‐19: Patients with respiratory symptoms or a suspected history of contact with a covid‐19‐positive patient; Confirmed Covid‐19: Patients with previous positive test results or those with Covid‐19 compatible involvement in CT, if performed. 9 Except the negative patient group, nasopharyngeal swab was taken from all patients and thorax CT was performed before PPCI.
During the study period, routine PCR tests were not applied to asymptomatic STEMI patients in our country.
Ethical Committee Approval for this study was granted by the Ondokuz Mayis University Hospital Ethics Committee.
2.4. Statistical analysis
Statistical analysis was carried out using Statistical Package for the Social Sciences for Windows 15.0 (SPSS Inc Chicago, Illinois, USA). Descriptive statistics were provided as median (min‐max), mean ± SD and percentage. The Kolmogorov‐Smirnov test was used for normal distribution analysis of the data. Non‐parametric Mann‐Whitney U‐test was used for non‐normally distributed data, and sample t‐test was used for normally distributed data. For categorical data, chi‐square test was used. Kruskal‐Wallis Test was used to compare patients who were divided into 3 groups according to the Covid‐19 infection status. Values of P < .05 were considered statistically significant.
3. RESULTS
A total of 165 patients, 82 in the Pandemic period and 83 in the Control period, were included in the study. Age, gender, frequency of diabetes, anterior MI rate, choice of P2Y12 and use of glycoprotein inhibitors (GPI) were similar among the groups. Of the applicants in the pandemic period, 57 (69.5%) were considered covid‐19 negative, 23 (28%) were suspected Covid‐19 and 2 (2.4%) confirmed Covid‐19. Patients were found to have significantly higher rates of ambulance use during the pandemic period (45.1% and 28.9% P = .031). In the first stage, the number of patients who reached the PPCI‐capable centre was also higher during the pandemic period (28.1% vs 13.3% P = .019) (Table 1).
TABLE 1.
Basal characteristics of groups
| Covid‐19 Period (n = 82) | Control Period (n = 83) | P | |
|---|---|---|---|
| Clinical data | |||
| Age (years) | 61.2 ± 11.4 | 60.7 ± 10.5 | .771 |
| Men, n (%) | 61 (74.4) | 61 (73.5) | .896 |
| Diabetes mellitus, n (%) | 28 (34.1) | 27 (32.5) | .826 |
| Hypertension, n (%) | 58 (70.7) | 55 (66) | .615 |
| Current smoking, n (%) | 31 (37.8) | 37 (44.5) | .430 |
| Prior MI, n (%) | 10 (12) | 7 (8.4) | .454 |
| Anterior STEMI, n (%) | 32 (39) | 35 (42.2) | .681 |
| Transport with ambulance, n (%) | 37 (45.1) | 24 (28.9) | .031 |
| Direct PCI centre, n (%) | 23 (28.1) | 11 (13.3) | .019 |
| Distance to PCI centre (km) | 40 (6‐114) | 40 (8‐114) | .257 |
| Drug | |||
| GPI, n (%) | 16 (20) | 22 (27.2) | .285 |
| P2Y12, n (%) | .381 | ||
| Clopidogrel, n (%) | 42 (51.9) | 49 (59.8) | |
| Ticagrelor, n (%) | 31 (38.3) | 29 (35.4) | |
| Prasugrel, n (%) | 8 (9.9) | 4 (4.9) | |
Abbreviations: GPI, glycoprotein inhibitors; PCI, percutaneous coronary intervention; STEMI, ST‐elevation myocardial infarction.
In terms of treatment strategies, PPCI was performed to 73 (89%) patients in the pandemic period and 80 (96.4%) patients in the control period. While 9 (11%) patients were treated with thrombolytic or emergency coronary bypass surgery (e‐CABG) in the pandemic period, this number was only 3 (3.6%) in the control period (P = .069).
When the components of the ischemic time were examined, home delay was 30 (5‐6912) minutes in the control period, whereas 165 (10‐360) minutes in the pandemic period (P < .001). FMC delay was 61 (20‐6932) minutes in the control period and 190 (15‐3660) minutes in the pandemic period (P < .001). While the number of patients with FMC delay > 120 minutes was 24 (29.3%) in the control period, it increased to 54 (65.9%) in the pandemic period (P < .001). In addition, door‐to‐balloon time was 83 (28‐488) minutes in the pandemic period, while it was 69 (11‐455) minutes in the control period (P = .076) (Figure 1) (Table 2).
FIGURE 1.
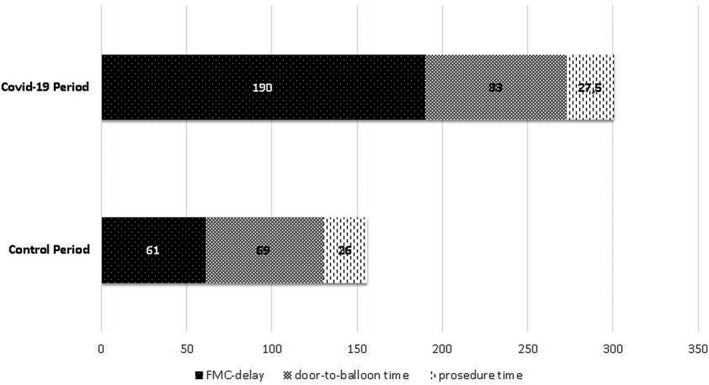
Timeline of patients with STEMI according to the Covid‐19 pandemic period
TABLE 2.
Treatment and time parameters of groups
| Covid‐19 Period (n = 82) | Control Period (n = 83) | P | |
|---|---|---|---|
| Primary Revascularization strategy | .069 | ||
| Primary PCI, n (%) | 73 (89) | 80 (96.4) | |
| Thrombolytic or e‐CABG, n (%) | 9 (11) | 3 (3.6) | |
| Preprocedural Time parameters | |||
| Home delay, min (min‐max) | 165 (10‐3600) | 30 (5‐6912) | <.001 |
| FMC delay, min (min‐max) | 190 (15‐3660) | 61 (20‐6932) | <.001 |
| Door‐to‐balloon time, min (min‐max) | 83 (28‐488) | 69 (11‐455) | .076 |
| Procedural parameters | |||
| Infarct‐related artery | .478 | ||
| Left main coronary artery, n (%) | 1 (1.3) | 0 | |
| Left anterior descending artery, n (%) | 31 (38.8) | 34 (41.5) | |
| Left circumflex artery, n (%) | 15 (18.8) | 13 (15.9) | |
| Right coronary artery, n (%) | 31 (38.8) | 35 (42.7) | |
| Saphenous vein graft, n (%) | 2 (2.5) | 0 | |
| Syntax I score | 17.3 ± 5.1 | 16.9 ± 4.5 | .602 |
| Non‐IRA PCI, n (%) | 7 (8.8) | 16 (19.3) | .043 |
| No reflow, n (%) | 5 (6.3) | 4 (4.9) | .703 |
| Procedure time, min (min‐max) | 27.5 (5‐77) | 26 (9‐71) | .373 |
| Postprocedural parameters | |||
| Hospitalization time, h (min‐max) | 71 (15‐170) | 74.2 (37‐329) | .045 |
| Hospital death, n (%) | 6 (7.3) | 3 (3.7) | .304 |
| Acute stent thrombosis, n (%) | 0 | 0 | |
Abbreviations: e‐CABG, emergency coronary artery bypass grafting surgery; FMC, first medical contact; IRA, infarct‐related artery; PCI, percutaneous coronary intervention.
There was no significant difference between the groups in terms of IRA detected during the angiography of the patients (P = .478). The non‐IRA intervention rate during the index procedure was significantly lower during the pandemic period (8.8% vs 19.3% P = .043). No reflow developed in 5 (6.3%) patients during the pandemic period and in 4 (4.9%) patients before the pandemic period (P = .703). The median procedure time was 27.5 (5‐77) minutes during the pandemic period, while it was 26 (9‐71) minutes in the prepandemic period (P = .373).
In terms of postprocedural parameters, the hospitalisation time was calculated shorter during the pandemic period [71 (15‐170) hours vs 74.2 (37‐329) hours P = .045]. In‐hospital mortality was not different between the groups and acute stent thrombosis was not observed in any case.
When patients were grouped according to the Covid‐19 infection status, there were significant differences in confirmed or suspected Covid‐19 cases in terms of home delay (P < .001), FMC delay (P < .001), door‐to‐balloon time (P = .015) and hospitalisation time (P = .037). However, the procedure time was similar between the groups (Table 3) (Figure 2).
TABLE 3.
Comparisons of time parameters in patients according to Covid‐19 status
| Covid‐19 period | Control period (n = 83) | P | ||
|---|---|---|---|---|
| Covid‐19 positive or suspective (n = 25) | Considered Covid‐19 negative (n = 57) | |||
| Home delay, min (min‐max) | 180 (20‐2880) a | 150 (10‐3600) a | 30 (5‐6912) | <.001 |
| FMC delay, min (min‐max) | 210 (20‐2940) a | 150 (15‐3660) a | 61 (20‐6932) | <.001 |
| Door‐to‐balloon time, min (min‐max) | 118 (40‐488) a , b | 73 (28‐260) | 69 (11‐455) | .015 |
| Procedure time, min (min‐max) | 26.5 (13‐54) | 29 (5‐77) | 26 (9‐71) | .714 |
| Hospitalization time, h (min‐max) | 80 (37‐160) | 70 (15‐124) a | 74.2 (37‐329) | .037 |
Abbreviation: FMC, first medical contact.
Compared with group III P < .016.
Compared with group II P < .016.
FIGURE 2.
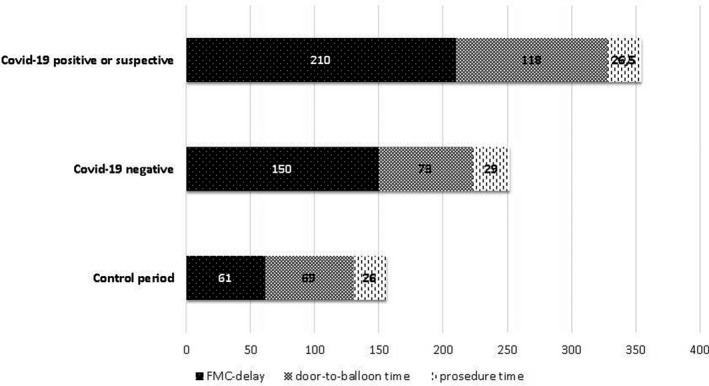
Timeline of patients with STEMI according to the Covid‐19 status
4. DISCUSSION
In our study, changes in prehospital delays and treatment applications were determined in STEMI patients who applied during the Covid‐19 pandemic period. While home delay and FMC delay increased during the pandemic period, non‐IRA PCI rate and discharge time were decreased. On the other hand, there was no significant change in door‐to‐balloon time and procedure time. To the best of our knowledge, this is the first randomised controlled study to analyse these parameters.
Studies have shown that the delay in FMC is associated with an increase in mortality and complication rate. 10 , 11 Candiello et al 12 reported the median FMC delay time in their study as 75 minutes, while Pereira et al 13 reported as 114 minutes. In the study of Viana et al, 10 the STEMI rate with FMC delay below 120 minutes was found to be 56.7%. In our study, in order to understand the patient‐related delay better, we calculated another time that we defined as home delay in addition to FMC delay. In our study, home delay and FMC delay were prolonged compared with the prepandemic period. In addition, the rate of patients with FMC delay time > 120 minutes during the pandemic period was doubled. In the report published by Tam CF et al 14 during the Covid‐19 outbreak, FMC delay was reported as 82.5‐91.5 minutes before the pandemic period, whereas 318 minutes during the pandemic period. However, this report showed that only 7 STEMI patients were analysed during the pandemic period. In our study, it was noticeable that the delay in the prehospital period was more evident in the home‐delay stage. During the Covid‐19 pandemic period, “Stay at home” calls were made to increase social isolation compliance. Therefore, many of the STEMI patients in the pandemic period seemed to have made their decision to go to the hospital later in their symptoms.
The mode that STEMI patients prefer for transportation to the hospital affects ischemic time. It has been reported that total ischemic time of patients transported by ambulance was shorter and the rate of transportation to the correct centre was higher. 15 , 16 However, in studies conducted in our country, it was demonstrated that STEMI patients preferred self‐transport rather than ambulance. 16 , 17 In our study, the transportation of the patients by ambulance was 28.9% in the prepandemic period and 45.1% during the pandemic period. This may be because of the fact that social isolation measures during the pandemic period, such as curfews, increased the ambulance use. In addition, the rate of transportation to a PCI‐capable centre in parallel with the use of ambulance also increased during the pandemic period. However, during the pandemic period, only a quarter of the patients reached the centre that performed PPCI in the first stage.
Another determinant of the ischemic time depends on the practices of the centre performing PCI. 1 , 18 Prolongation in this period is mostly related to delays in Emergency Medical Services (EMS). 19 The door‐to‐balloon time calculated in our study during the pandemic period increased numerically but did not reach statistical significance (P = .076). However, this period was significantly higher in patients with confirmed or suspected Covid‐19. The reason for this may be the prolongation of the process with chest imaging, nasopharyngeal swab sampling and infection department consultation before being taken to the catheter laboratory. Another potential cause of delay is using of the personal protection equipment of the team that perform the intervention to these patients. A Korean study on the MERS‐CoV epidemic period stated that potential difficulties in the use of protective equipment affect healthcare delivery. 20 On the other hand, it may be thought that the rapid triage habits of the centres in STEMI patients may have prevented the significant prolongation in the door‐to‐balloon time.
In the outbreak period, numerical increase tendency was observed in thrombolytic or emergency surgical revascularisation applications as a method of revascularisation. The reason for this may be the operator concern about contamination and publications recommending thrombolytic therapy. 21 , 22 Current European guidelines do not recommend routine non‐IRA PCI during index procedure in patients with multivessel disease presenting with STEMI. 3 However, because of contradictory data in research, the complexity of the case, the experience and preference of the operator are also effective in practice. 23 , 24 , 25 In our study, the rate of non‐IRA PCI during the index procedure significantly decreased during the pandemic period compared with the prepandemic period. This is most likely related to the operator's tendency to shorten catheter time to reduce the risk of transmission. A similar situation was observed in the discharge time of the patients. It was noteworthy that the discharge time was shorter, especially for Covid‐19‐negative patients.
Finally, the procedure time during the pandemic period did not change compared with the prepandemic period. Although the number of non‐IRA interventions was less during the pandemic period, the procedure time was found to be numerically longer. This may be related to the protective measures taken against the virus in the catheter laboratory during the pandemic period and the more controlled and slower work of the staff against the risk of transmission.
4.1. Study limitation
The data obtained in our study belonged only to 3 centres in two cities. During the study period, as seen in some metropolitan cities of the world, there was no tragic pandemic intensity in these two cities. Therefore, the data obtained may not reflect more intense outbreak areas.
In the study, the same months of the year before and after the pandemic were not analysed. Considering the seasonal character of STEMI, this may partially affect the outcome.
5. CONCLUSION
The Covid‐19 outbreak has emerged as a virus infection with high risk of transmission and has spread rapidly around the world. It is not surprising that both patient and physician behaviours are affected during this pandemic period, since the transmission and mortality rates are higher among healthcare professionals. In our study, it has been determined that ischemia times in STEMI patients, especially in the patient‐related part, are prolonged during the pandemic period. Therefore, informing the public about heart attack symptoms as a part of the outbreak measures may reduce possible delays.
DISCLOSURE
None to declare.
Soylu K, Coksevim M, Yanık A, Bugra Cerik I, Aksan G. Effect of Covid‐19 pandemic process on STEMI patients timeline. Int J Clin Pract. 2021;75:e14005. 10.1111/ijcp.14005
DATA AVAILABILITY STATEMENT
Data available on request from the authors.
REFERENCES
- 1. Fokkema ML, Wieringa WG, van der Horst IC, Boersma E, Zijlstra F, de Smet BJ. Quantitative analysis of the impact of total ischemic time on myocardial perfusion and clinical outcome in patients with ST‐elevation myocardial infarction. Am J Cardiol. 2011;108:1536‐1541. [DOI] [PubMed] [Google Scholar]
- 2. De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223‐1225. [DOI] [PubMed] [Google Scholar]
- 3. Neumann FJ, Sousa‐Uva M, Ahlsson A, et al. [2018 ESC/EACTS Guidelines on myocardial revascularization. The Task Force on myocardial revascularization of the European Society of Cardiology (ESC) and European Association for Cardio‐Thoracic Surgery (EACTS)]. G Ital Cardiol. 2019;20(7–8 Suppl 1):1s‐61s. [DOI] [PubMed] [Google Scholar]
- 4. Bata I, Armstrong PW, Westerhout CM, et al. WEST Study Group. Time from first medical contact to reperfusion in ST elevation myocardial infarction: a which early ST elevation myocardial infarction therapy (WEST) substudy. Can J Cardiol. 2009;25:463‐468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Scholz KH, Maier SK, Jung J, et al. Reduction in treatment times through formalized data feedback: results from a prospective multicenter study of ST‐segment elevation myocardial infarction. JACC Cardiovasc Interv. 2012;5:848‐857. [DOI] [PubMed] [Google Scholar]
- 6. Dalia A, Geetha K, Mona A, Rajalakshimi V, Sriram C. Review on the coronavirus disease (COVID‐19) pandemic: its outbreak and current status. Int J Clin Pract. 2020;74:e13637. 10.1111/ijcp.13637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. WHO . Novel coronavirus (2019‐nCoV) situation report ‐111 (Web Site); 2020. https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200510covid‐19‐sitrep‐111.pdf?sfvrsn=1896976f_2. Accessed May 10, 2020. [Google Scholar]
- 8. Mesnier J, Cottin Y, Coste P, et al. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID‐19 and patient profile in France: a registry study. Lancet Public Health. 2020;5(10):e536–e542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. UpToDate . Coronavirus disease 2019 (COVID‐19): Epidemiology, virology, clinical features, diagnosis, and prevention; 2020. https://www.uptodate.com/contents/coronavirus‐disease‐2019‐covid‐19‐epidemiology‐virology‐clinical‐features‐diagnosis‐and‐prevention?csi=e8c325c2‐17dc‐46a3‐8f7a‐8789ccfa5802&source=contentShare.
- 10. Viana M, Laszczyńska O, Araújo C, Borges A. Patient and system delays in the treatment of acute coronary syndrome. Rev Port Cardiol. 2020;39(3):123‐131. 10.1016/j.repc.2019.07.007. [DOI] [PubMed] [Google Scholar]
- 11. Kolul S, Andell P, Martinsson A, et al. Delay from first medical contact to primary PCI and all‐cause mortality: a nationwide study of patients with ST‐elevation myocardial infarction. J Am Heart Assoc. 2014;3:e000486. 10.1161/JAHA.113.000486. PMCID: PMC4187473. Published online 2014 Apr 25. PMID: 24595190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Candiello A, Cohen F, Lasave L, et al. Impact of an evaluation system of times to reperfusion in ST‐segment elevation acute myocardial infarction. Rev Argent Cardiol. 2020;88:32‐38. 10.7775/rac.v88.i1.15783. [DOI] [Google Scholar]
- 13. Pereira H, Calé R, Pinto FJ, et al. Factors influencing patient delay before primary percutaneous coronary intervention in ST‐segment elevation myocardial infarction: the Stent for life initiative in Portugal. Rev Port Cardiol. 2018;37:409‐421. [DOI] [PubMed] [Google Scholar]
- 14. Tam C‐C, Cheung K‐S, Lam S, et al. Impact of coronavirus disease 2019 (COVID‐19) outbreak on ST‐segment‐elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13:e006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cui CY, Zhou MG, Chen AF, et al. Impact of different admission ways on treatment efficiency in patients with acute ST‐segment elevation myocardial infarction. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:302‐307. [DOI] [PubMed] [Google Scholar]
- 16. Demirkan B, Ege MR, Doğan P, İpek EG, Güray U, Güray Y. Factors influencing the use of ambulance among patients with acute coronary syndrome: results of two centers in Turkey. Anatol J Cardiol. 2013;13:516‐522. [DOI] [PubMed] [Google Scholar]
- 17. Başar C, Özhan H, Albayrak ES, Türker Y. Evaluation of transfer parameters in patients admitted to our hospital with ST‐elevation myocardial infarction. Turk Kardiyol Dern Ars. 2016;44:30‐36. 10.5543/tkda.2015.04680. [DOI] [PubMed] [Google Scholar]
- 18. Scholz KH, Maier SKG, Maier LS, et al. Impact of treatment delay on mortality in ST‐segment elevation myocardial infarction (STEMI) patients presenting with and without haemodynamic instability: Results from the German prospective, multicentre FITT‐STEMI trial. Eur Heart J. 2018;39:1065‐1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nallamothu BK, Normand S‐L, Wang Y, et al. Relation between door‐to‐balloon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet. 2015;385:1114‐1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kang JH, Kim EJ, Choi JH, et al. Difficulties in using personal protective equipment: Training experiences with the 2015 outbreak of Middle East respiratory syndrome in Korea. Am J Infect Control. 2018;46:235‐237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Han Y, Zeng H, Jiang H, et al. CSC expert consensus on principles of clinical management of patients with severe emergent cardiovascular diseases during the COVID‐19 epidemic. Circulation. 2020;141(20):e810‐e816. 10.1161/CIRCULATIONAHA.120.047011. [DOI] [PubMed] [Google Scholar]
- 22. Aktoz M, Altay H, Aslanger E, et al. Consensus report from Turkish society of cardiology: COVID‐19 and cardiovascular diseases. What cardiologists should know (25th March 2020). Turk Kardiyol Dern Ars. 2020;48:1‐48. [DOI] [PubMed] [Google Scholar]
- 23. Engstrøm T, Kelbæk H, Helqvist S, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST‐segment elevation myocardial infarction and multivessel disease (DANAMI‐3‐PRIMULTI): an open‐label, randomised controlled trial. Lancet. 2015;386:665‐671. [DOI] [PubMed] [Google Scholar]
- 24. Smits PC, Abdel‐Wahab M, Neumann F‐J, et al. Fractional flow reserve‐guided multivessel angioplasty in myocardial infarction. N Engl J Med. 2017;376:1234‐1244. [DOI] [PubMed] [Google Scholar]
- 25. Thiele H, Akin I, Sandri M, et al. CULPRIT‐SHOCK Investigators. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med. 2017;377:2419‐2432. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the authors.


