Abstract
Aim:
This study aims to assess how optimism, social support, and perceived susceptibility are associated with depressive symptoms and health-related quality of life among elderly patients during the COVID-19 pandemic in Israel.
Methods:
In a cross-sectional study, 256 participants age 60 through 95 completed the following self-administered questionnaires: Perceived Susceptibility, Life Orientation Test (LOT-R), Multidimensional Scale of Perceived Social Support (MSPSS), Symptoms of Depression (CES-D) and health-related quality of life (SF-12v2 Health Survey). Data were collected from June to July 2020, 3 months after the COVID-19 state of emergency was declared in Israel. Participants were interviewed by family medicine residents via telephone. Statistical analyses included Pearson correlations, t-tests between groups, regression analyses, and Hayes’ PROCESS to analyze a moderated mediation model.
Results:
Of the elderly participants, 37.5% were classified as having depression. Optimism, social support and health-related quality of life were positively associated. Higher optimism and social support were related to lower perceived susceptibility and lower depression. Results of a multivariate regression explained 29% of the variance in depression and 19% of the variance in health-related quality of life. The relationships assessed by 4 Process models were significant, such that higher optimism and social support were related to lower perceived susceptibility, which in turn was related to higher depression and lower health-related quality of life.
Conclusions:
Optimism and social support may be effective in coping with challenges and buffering depression. Perceived susceptibility may mediate the association of optimism and social support with higher depression and lower health-related quality of life. The conclusions of this study underscore the need to treat depression among older adults during this period. Hence, healthcare providers should also support elderly patients living at home. In giving this type of help, healthcare providers should strive to increase social support and optimism among older adults.
Keywords: COVID-19, depression, health-related quality of life, older adults, optimism perceived susceptibility, social support
Introduction
The coronavirus disease (COVID-19) pandemic has initiated worldwide research efforts to identify people at greatest risk of developing critical illnesses and of dying. Initial data point toward older individuals as being particularly vulnerable.1-5 From its initial stages, the COVID-19 pandemic was portrayed in Israel as a problem for the older population.5-7 Older adults were increasingly encouraged to isolate themselves from younger people, thereby creating an age distinction in the perceived consequences of COVID-19.4 The probable rise in the incidence of serious health complications from COVID-19 among older adults, particularly those with pre-existing conditions, has intensified their physical and social isolation, which may increase the prevalence and severity of anxiety and depression among this population group.3 Indeed, social isolation generates significant risk factors for depression in older adults.8 At the same time, studies point to lower levels of depression and higher levels of coping with threats among older adults.9
Not only are older adults liable to experience the mental stress of possible infection and the pain of not being able to see their relatives and loved ones, they are also likely to experience physical stress. The rapid spread of the COVID-19 pandemic, the rising mortality rates, self-isolation, social distancing and quarantine can all exacerbate the risk of developing new health problems or of worsening existing ones, as well as the risk of emotional consequences.10,11
The Cognitive Model in the Present Study
The present study is based on the cognitive model of coping with stressors proposed by Lazarus and Folkman.12 According to this model, coping involves persistently changing cognitive and behavioral efforts in order to manage specific external and/or internal demands that are seen as taxing or exceeding one’s resources. This model explains the relations between the source of stress, the choice of a coping strategy and the way the chosen strategy can affect a person within a stressful environment. The stress associated with a particular situation depends on how individuals appraise the situation and the behaviors they devote to managing the stress. This model proposes that the psychological and physical health outcomes of coping with chronic and intense stressors are influenced by personal resources (eg, optimism, perceived social support), stressor appraisals (eg, perceived susceptibility), and psychological and physical outcomes (eg, depressive symptoms, health-related quality of life).
Optimism is a personal resource defined as a general expectation or belief that good things will happen frequently in the future, while bad things will happen only rarely.13 Perceived social support is defined as the perceived availability of support if needed. Studies indicate that optimism and perceived social support are effective resources for coping with adversity and challenges and may serve as a main source of personal care and subjective well-being, especially in old age.13-15 In the current study, perceived stressors were conceptualized as perceived susceptibility, as this factor may influence mental and physical health.16,17
Depression is likely to be negatively associated with health-related quality of life. Studies have found that COVID-19 patients with depression reported lower health-related quality of life compared to those without depression.18 Similar findings were also found for other diseases, such as diabetes19 and gastrointestinal diseases.20 In a study conducted among healthcare workers during the COVID-19 epidemic, older workers enjoyed better mental health though not better physical health.21 Based on the above review, understanding the implications of the COVID-19 restrictions on the health and well-being of older adults is of major importance.
Research Aims
The aim of this study was to assess how optimism, perceived social support, and perceived susceptibility are related to depressive symptoms and health-related quality of life among older adults. In addition, the study assessed the role of perceived susceptibility in mediating between personal resources (optimism, perceived social support) and depressive symptoms and health-related quality of life.
Methods
We conducted a cross-sectional survey 3 months after the COVID-19 state of emergency was declared in Israel. Prior to commencing the study, we obtained approval from the Institutional Review Board of Clalit Health Services, the largest not-for-profit insurer and health provider organization in Israel (approval number 0060-20-COM2). Data were collected in June and July 2020, a period during which the first wave of COVID-19 had subsided in Israel. During this time, many individuals were asked to take an unpaid leave of absence or to work from home. A new routine was established in Israel that included mandatory wearing of face masks and strict social distancing measures.
Participants
A total of 256 older adults participated in the study. Inclusion criteria were being a resident of Israel insured by the Clalit Health Services, being over the age of 60, and being a Hebrew speaker. Cognitive impairment was the exclusion criterion. Potential participants who met the inclusion criteria were identified by the managers of 8 clinics, half located in urban settings and half in rural areas. The contact details of these potential participants were forwarded to 6 family medicine residents, who contacted them and explained the details and importance of the study. Patients who agreed to participate were interviewed by the family medicine residents via telephone, using a structured pre-tested questionnaire. A total of 276 older adults were contacted, with a response rate of 93%. The main reasons for refusing to participate were infirmity, lack of interest and hearing difficulties.
Participants’ mean age was 71.83 years, and 46.9% were male (Table 1). Most were married (74%) and had about 3 children on average. Their mean education level was about 13 years. With respect to living circumstances, 70.6% lived with an intimate partner, while the others lived alone (18%) or with family members (10%). Their perceived health status generally ranged from mediocre to bad (80%), and most (84%) reported having various chronic illnesses.
Table 1.
Participants’ Demographic Characteristics (n = 256).
| Health characteristics | N (%) |
|---|---|
| Gender (%) | |
| Male | 120 (46.9) |
| Female | 136 (53.1) |
| Mean age (SD), range | 71.83 (6.92), 60-95 |
| Marital status (%) | |
| Married | 188 (74.0) |
| Not married | 66 (26.0) |
| Mean number of children (SD), range | 3.04 (1.28), 0-10 |
| Mean number of years of education (SD), range | 13.10 (3.12), 6-24 |
| Living with (%) | |
| Alone | 46 (18.5) |
| Intimate partner | 175 (70.6) |
| Family member/s | 26 (10.5) |
| Formal caregiver | 1 (0.4) |
| Perceived health status (%) | |
| Moderate-bad | 148 (79.5) |
| Good | 38 (20.5) |
| Chronic disease (%) | |
| Yes | 216 (84.4) |
| No | 40 (15.6) |
| Types of other chronic diseases (%) | |
| Hypertension | 63 (29.2) |
| Diabetes | 19 (8.8) |
| Coronary heart disease | 22 (10.2) |
| Cancer | 25 (11.6) |
| Lung disease | 12 (5.6) |
| Diabetes and hypertension | 41 (19.0) |
| Other | 34 (15.7) |
| Mean Depression (SD), range | 9.31 (6.57), 0-30 |
| Depression cutoff – positive (%) | 96 (37.5) |
| Mean Health-related quality of life (SD), range | 54.79 (31.20), 0-100 |
Measures
The following measures were used in the study:
Depressive symptoms were measured using a modified 10-item version of the Center for Epidemiological Studies Depression Scale (CESD-10).22 The CESD-10 is a 4-point Likert-type scale that assesses the extent to which individuals experienced depressive symptoms during the previous week (eg, “I was bothered by things that don’t usually bother me”). Total scores range from 0 to 30. Most studies used a cut-off of 10+ to classify participants at high risk of depression.23 After negative statements were reversed, the mean score was calculated, with higher scores reflecting higher levels of depression (Cronbach’s α = 0.89).
Perceived susceptibility was assessed by 2 questions asking participants how likely they think it is they will contract COVID-19.24 Participants responded on a 5-point Likert scale ranging from 1 (not at all likely) to 5 (very likely), so that higher scores indicated greater perceived threat. Items were scored and summed, with higher scores indicating higher levels of perceived susceptibility (Cronbach’s α = 0.79).
Optimism was tested with the Life Orientation Test-Revised (LOT-R).25 Participants answered on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) (eg, “In uncertain times, I usually expect the best”). After the negative statements were reversed, a mean score was calculated, with higher scores indicating a higher level of optimism (Cronbach’s α = 0.62).
Multidimensional Scale of Perceived Social Support (MSPSS) was used to assess social support.26 Twelve items measured the perceived adequacy of social support from 3 sources: family members, friends, and other significant people. Participants rated these 12 items on a 7-point Likert-type scale ranging from 1 (very strongly disagree) to 7 (very strongly agree) (eg, “My family really tries to help me”). The mean score was calculated, with higher scores indicating higher levels of perceived social support (Cronbach’s α = 0.81).
The SF-12v2 Health Survey27 was used to assess health-related quality of life. The survey consists of 8 domains as well as a physical component summary (PCS) and a mental component summary (MCS). In the current study we used 4 subscales: physical functioning (PF), role limitations due to physical problems (role-physical—RP), bodily pain (BP), general health perceptions (GH). These measures were chosen due to their importance for older adults and the need to shorten the interviews, which were conducted by telephone. We did not use the sub-scales measuring mental health in order not to create an overlap with the depression questionnaire. In accordance with the instructions for the tool, each item was converted to a scale ranging from 0 to 100, and a mean score was computed for each sub-scale. After that, an overall mean in the 0 to 100 range was computed for the 4 scales, with a high score indicating better health-related quality of life (Cronbach’s α = 0.88).
A sociodemographic questionnaire was used to tap into participants’ background characteristics: gender, age, years of education, marital status, number of children, chronic illnesses.
Statistical Analyses
Data were analyzed using SPSS ver. 26. Descriptive statistics were used to describe the participants’ demographic characteristics and the research variables. Pearson correlations were calculated to assess the associations between the research variables.
Two multiple hierarchical regressions were calculated, with depression and health-related quality of life as the dependent variables. Gender, age, and years of education were entered in the first step, optimism and social support in the second step, and perceived susceptibility in the third step. The mediating role of perceived susceptibility was examined with the Process procedure28 using model 4, with bootstrapping of 5000 samples and 95% confidence interval. For this purpose, all independent, mediating, and control variables were standardized. Optimism and social support were defined as the independent variables, perceived susceptibility as the mediating variable, and depression and health-related quality of life as the dependent variables. Gender, age, and years of education were control variables. This procedure follows the theoretical steps determined by Baron and Kenny29: It examines the direct relationship between the independent and the dependent variable, the relationship between the independent and the mediating variable, and the relationship between the mediating and the dependent variable, controlling for the independent variable.
Results
As depicted in Table 2, mean depression was moderate-low, and the mean for health-related quality of life was moderate. Still, 37.5% (n = 96) of the participants were classified as suffering from depression. Mean optimism and social support were moderate-high, and mean perceived susceptibility was moderate. Significant correlations were found among the study variables. Optimism, social support and health-related quality of life exhibited positive low-to-moderate correlations. Further, higher optimism and social support were related to lower perceived susceptibility and to lower depression. Lower perceived susceptibility was related to lower depression and to higher health-related quality of life. Depression and health-related quality of life were negatively related.
Table 2.
Means, Standard Deviations, Ranges, and Pearson Correlations for the Study Variables (n = 256).
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Gender | – | |||||||
| 2. Age | 0.02 | – | ||||||
| 3. Education years | −0.03 | 0.02 | – | |||||
| 4. Optimism | 0.03 | −0.16* | 0.25*** | – | ||||
| 5. Social support | −0.09 | −0.14* | 0.24*** | 0.24*** | – | |||
| 6. Perceived susceptibility | −0.07 | 0.14* | −0.06 | −0.21** | −0.19** | – | ||
| 7. Depression | −0.16* | 0.11 | −0.26*** | −0.45*** | −0.26*** | 0.34*** | – | |
| 8. Health-related quality of life | 0.14* | −0.16* | 0.27*** | 0.20** | 0.22*** | −0.32*** | −0.51*** | – |
| Mean | 0.47 | 71.83 | 13.10 | 3.65 | 4.03 | 2.87 | 0.93 | 54.79 |
| SD | 0.50 | 6.92 | 3.12 | 0.66 | 0.76 | 0.90 | 0.66 | 31.20 |
| Possible range | 1-5 | 1-5 | 1-5 | 0-3 | 0-100 | |||
| Actual range | 60-95 | 6-24 | 1.3-5 | 1-5 | 1-5 | 0-2.75 | 0-100 |
P < .05, **P < .01, ***P < .001, for gender (1-men, 0-women) – Point bi-serial correlation.
Depression was higher among women (M = 1.03, SD = 0.66) than among men (M = 0.82, SD = 0.63) (t(254) = 2.58, P = .011), and health-related quality of life was higher among men (M = 59.29, SD = 31.02) than among women (M = 50.83, SD = 30.93) (t(254) = 2.18, P = .030). Age exhibited a negative association to health-related quality of life (r = −0.16, P = .017), and years of education exhibited a negative association to depression (r = −0.25, P < .001) and a positive association to health-related quality of life (r = 0.27, P < .001). These demographic variables were controlled for in further analyses.
Two multiple regression analyses were calculated, with depression and health-related quality of life as the dependent variables, gender (1-male, 0-female), age, and years of education as the control variables, and optimism, social support, and perceived susceptibility as the independent variables (Table 3).
Table 3.
Multiple Hierarchical Regressions for Depression and Health-Related Quality of Life (n = 256).
| Depression | Health-related quality of life | |||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | β | Adj. R2 | B | SE | β | Adj. R2 | |
| Step 1 | 0.10*** | 0.12*** | ||||||
| Gender | −0.25 | 0.09 | −0.19** | 12.56 | 4.12 | 0.20** | ||
| Age | 0.01 | 0.01 | 0.13 | −0.80 | 0.30 | −0.18** | ||
| Education years | −0.05 | 0.01 | −0.24*** | 2.60 | 0.66 | 0.26*** | ||
| Step 2 | 0.25*** | 0.14*** | ||||||
| Gender | −0.25 | 0.08 | −0.19** | 13.24 | 4.09 | 0.21** | ||
| Age | 0.00 | 0.01 | 0.04 | −0.64 | 0.30 | −0.14* | ||
| Education years | −0.02 | 0.01 | −0.11 | 2.05 | 0.70 | 0.20** | ||
| Optimism | −0.36 | 0.07 | −0.36*** | 2.51 | 3.31 | 0.05 | ||
| Social support | −0.14 | 0.06 | −0.16* | 7.05 | 2.97 | 0.16* | ||
| Step 3 | 0.29*** | 0.19*** | ||||||
| Gender | −0.22 | 0.08 | −0.17** | 11.74 | 4.00 | 019** | ||
| Age | 0.01 | 0.01 | 0.03 | −0.56 | 0.29 | −0.13 | ||
| Education years | −0.02 | 0.01 | −0.12 | 2.10 | 0.68 | 0.21** | ||
| Optimism | −0.32 | 0.06 | −0.32*** | 0.69 | 3.27 | 0.01 | ||
| Social support | −0.11 | 0.06 | −0.13* | 5.58 | 2.92 | 0.13 | ||
| Perceived susceptibility | 0.16 | 0.05 | 0.22*** | −7.96 | 2.31 | −0.23*** | ||
Depression: F(6, 249) = 14.71, P < .001; Health related quality of life: F(6, 249) = 8.84, P < .001.
P < .05. **P < .01. ***P < .001.
Both regression models were found to be significant, with 29% of the variance explained in depression and 19% explained in health-related quality of life. Optimism and social support added 15% and 2% to the explained variance in depression and health-related quality of life, respectively, beyond the demographic variables. Perceived susceptibility added another 4% and 5% to the explained variance in depression and health-related quality of life, respectively, beyond the independent variables. As the table shows, beyond the demographic variables, depression is related to optimism, social support, and perceived susceptibility, such that lower optimism, lower social support, and higher perceived susceptibility are associated with greater depression. Beyond the demographic variables, health-related quality of life is related to perceived susceptibility, such that lower perceived susceptibility is associated with better health-related quality of life.In order to assess the mediating role of perceived susceptibility, we examined 4 Process models (Model 4),28 with optimism and social support as the independent variables, and depression and health-related quality of life as the dependent variables. Gender, age, and years of education served as control variables. Continuous variables were standardized. The results are shown in Table 4 and Figure 1.
Table 4.
Path Coefficients and Indirect Effects for the Mediation Models (n = 256).
| DV | Variable | Path coefficients | Indirect effects | ||
|---|---|---|---|---|---|
| To DV estimate (SE) | To mediator estimate (SE) | Estimate (SE) | 95%CI | ||
| Depression | Optimism | −0.22*** (0.04) | −0.19* (0.07) | −0.03 (0.01) | −0.06, −0.01 |
| Perceived susceptibility | 0.16*** (0.04) | ||||
| Depression | Social support | −0.09* (0.04) | −0.16* (0.07) | −0.03 (0.01) | −0.06, −0.01 |
| Perceived susceptibility | 0.19*** (0.04) | ||||
| Health related quality of life | Optimism | 0.89 (2.17) | −0.19* (0.07) | 1.46 (0.73) | 0.22, 3.11 |
| Perceived susceptibility | −7.74*** (2.07) | ||||
| Health related quality of life | Social support | 3.44 (2.12) | −0.16* (0.07) | 1.17 (0.61) | 0.15, 2.57 |
| Perceived susceptibility | −7.42*** (2.04) | ||||
P < .05. ***P < .001.
Figure 1.
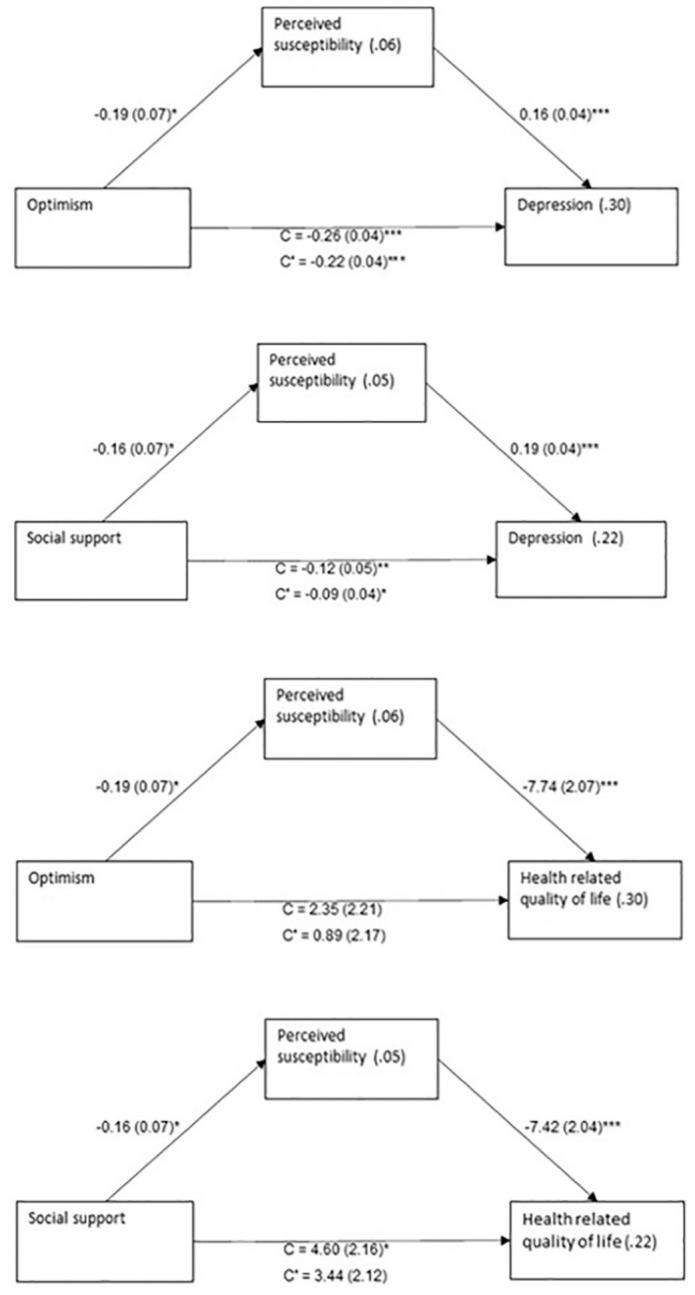
The mediating role of perceived susceptibility in the relationship between study variables.
Values on arrows: B(SE), values within rectangles: R2, C = total effect, C′ = direct effect.
*P < .05. **P < .01. ***P < .001.
As the table shows, all mediated relationships were significant. That is, higher optimism and social support were related to lower perceived susceptibility, which in turn was related to higher depression and lower health-related quality of life.
Discussion
The COVID-19 pandemic constitutes a major threat to public health, with older adults particularly vulnerable to severe health consequences.1-3,5 The present study sought to investigate how optimism, social support and perceived susceptibility are related to depressive symptoms and health-related quality of life and to examine these relations among older adults living in Israel. Our findings suggest that older adults experienced moderate levels of depression and health-related effects on quality of life during the COVID-19 pandemic. This finding is compatible with the findings of previous research.3,4,30 The stated aim of many government responses to COVID-19 has been to protect older adults and other at-risk groups. Yet lockdowns and arbitrary age restrictions may also place additional strain on older adults.6,8
The levels of depression and the lower health-related quality of life found in this study may be explained by the fact that some older adults chose to isolate themselves. While isolation can help contain and control the spread of infectious diseases, it also has major negative psychological effects.31,32 Older people may have more trouble dealing with isolation than younger people and may need more support.4,6,8 Another explanation for the findings of this study can be seen in previous studies showing that older adults may also express more anxiety and concern about their family, leading them to adopt more healthy behaviors.33 Despite their desire to meet with family members they may be worried about transmitting COVID-19 to them.6
The present study showed that optimism and social support were positively related to health-related quality of life. Higher optimism and social support were associated with lower perceived susceptibility and lower depression. These associations are in line with cognitive theory12 and with previous studies examining chronic stress situations.14,15,24 Optimism and social support may serve as a buffer against the main source of stress and the psychological situation, especially in old age.13-17
Our results also suggest that depression exhibits a strong negative association with health-related quality of life. This finding is supported by previous studies that found a negative association between these factors, such that older people had better mental but not physical health.18,20,21 One possible explanation for our findings may lie in the levels of depression and health-related quality of life found in our study. Mean depression was moderate-low, and the mean for health-related quality of life was moderate. It may be that higher levels of depression would have had a negative impact on participants’ health-related quality of life. Another explanation may lie in the fact that 84.4% of the research participants reported chronic health problems. This lower health-related quality of life before the pandemic may be associated with the participants’ emotional state and may have influenced or even worsened it. In addition, some older population groups, such as people living with cancer or other chronic diseases, may be at increased risk for developing mental health problems during a pandemic as a result of their tenuous physical health, as well as barriers to accessing medical treatment, higher risks of COVID-19 infection, and higher probability of severe illness if infected.24
In this study we assessed the mediating role of perceived susceptibility by means of 4 Process models.28 All mediated relationships were significant. Depression was associated with lower optimism, lower social support, and higher perceived susceptibility, while health-related quality of life was associated with lower optimism, lower social support, and lower perceived susceptibility. One possibility is that perceived susceptibility increases depression, especially during uncertainty situations.13-15 It is plausible to assume that individuals with higher depression levels also perceive their situation as more threatening or that individuals who are more depressed manifest higher levels of health-related quality of life.16,17 The present results are cross-sectional and thus cannot explain the causes either of depression or of health-related quality of life. Nevertheless, they do suggest that different pathways may exist for the development of each of the symptoms, especially in view of the possible somatization of psychological symptoms exhibited at older ages. Another possible explanation is that participants’ health-related quality of life was already low prior to the COVID-19 crisis and therefore did not affect their threat perceptions.
The study has a number of limitations. Its main limitation lies its cross-sectional design. As a result, conclusions about directionality or causality in the relationships should be treated with caution. A second limitation is that the present study is based on participants’ self-report questionnaires. Despite the high response rates in this study, it is still reasonable to expect a sampling bias, for example due to physical difficulties in answering the phone or due to hearing problems. The third limitation is that the data refer only to the period in which they were collected. Given the dynamics of the virus, the figures may change over time. Further longitudinal research is needed in Israel and around the world.
Our findings suggest that the pandemic had immediate negative influences on the mental health of older adults. At the same time, this population group has internal and external resources that can help them and significantly reduce their perceived susceptibility. An important avenue for future research will be to evaluate how these effects on physical and mental health unfold over time.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval and Consent to Participate: Before the research began, the Ethics Committee of Clalit Health Services approved the study (Authorization No. 0060-20-COM2). All study data were stored safely, and only the researcher had access to the data. All personal data were coded, so that the identities of the participants remained confidential.
ORCID iDs: Inbar Levkovich  https://orcid.org/0000-0003-1582-3889
https://orcid.org/0000-0003-1582-3889
Shiri Shinan-Altman  https://orcid.org/0000-0003-1340-2909
https://orcid.org/0000-0003-1340-2909
Availability of Data and Materials: The authors have the research data, which is available upon request.
References
- 1. Santini ZI, Jose PE, Cornwell EY, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 2020;5:e62-e70. [DOI] [PubMed] [Google Scholar]
- 2. Davies NG, Klepac P, Liu Y, Prem K, Jit M, Eggo RM. Age-dependent effects in the transmission and control of COVID-19 epidemics. MedRxiv. Published online May 3, 2020. doi: 10.1101/2020.03.24.20043018 [DOI] [PubMed] [Google Scholar]
- 3. Gorrochategi MP, Munitis AE, Santamaria MD, Etxebarria NO. Stress, anxiety, and depression in people aged over 60 in the COVID-19 outbreak in a sample collected in Northern Spain. Am J Geriat Psychiat. 2020;28:993-998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shrira A, Hoffman Y, Bodner E, Palgi Y. COVID-19 related loneliness and psychiatric symptoms among older adults: the buffering role of subjective age. Am J Geriat Psychiat. 2020;28:1200-1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Levkovich I. The impact of age on negative emotional reactions, compliance with health guidelines and knowledge about the virus during the COVID-19 epidemic: a longitudinal study from Israel. J Prim Care Community Health. Published online December 2020. doi: 10.1177/2150132720981540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ayalon L. There is nothing new under the sun: ageism and intergenerational tension in the age of the COVID-19 outbreak. Int Psychogeriatr. 2020;32:1221-1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shinan-Altman S, Levkovich I. COVID-19 precautionary behavior: the Israeli case in the initial stage of the outbreak. BMC Public Health. 2020;20:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5:e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bruine de Bruin W. Age differences in COVID-19 risk perceptions and mental health: evidence from a national US survey conducted in March 2020. J Gerontol B Psychol Sci Soc Sci. 2021;76:e24-e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Levkovich I, Shinan-Altman S. Emotional rections and subjective health status during the COVID-19 in Israel: the mediating role of perceived susceptibility. Psychol Health Med. Published online December 15, 2020. doi: 10.1080/13548506.2020.1858490 [DOI] [PubMed] [Google Scholar]
- 11. Gustavsson J, Beckman L. Compliance to recommendations and mental health consequences among elderly in Sweden during the initial phase of the COVID-19 pandemic—a cross sectional online survey. Int J Environ Res Public Health. 2020;17:5380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lazarus RS, Folkman S. Stress, Appraisal, and Coping. Springer; 1984: 14. [Google Scholar]
- 13. Altman S, Levkovich I, Dror M. Are daily hassles associated with happiness in old age? The contribution of personal resources. Int J Gerontol. 2020;14:239-297. [Google Scholar]
- 14. Levkovich I, Cohen M, Alon S, et al. Symptom cluster of emotional distress, fatigue and cognitive difficulties among young and older breast cancer survivors: the mediating role of subjective stress. J Geriatr Oncol. 2018;9:469-475. [DOI] [PubMed] [Google Scholar]
- 15. Şahin DS, Özer Ö, Yanardağ MZ. Perceived social support, quality of life and satisfaction with life in elderly people. Educ Gerontol. 2019;45:69-77. [Google Scholar]
- 16. Bolton CD, Sunil TS, Hurd T, Guerra H. Hispanic men and women’s knowledge, beliefs, perceived susceptibility, and barriers to clinical breast examination and mammography practices in south Texas colonias. J Commun Health. 2019;44:1069-1075. [DOI] [PubMed] [Google Scholar]
- 17. Levkovich I, Shinan-Altman S. Impact of the COVID-19 pandemic on stress and emotional reactions in Israel: a mixed-methods study. Int Health. Published online October 13, 2020. doi: 10.1093/inthealth/ihaa08120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ma YF, Li W, Deng HB, et al. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J Affect Disord. 2020;275:145-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Eren I, Erdi Ö, Şahin M. The effect of depression on quality of life of patients with type II diabetes mellitus. Depress Anxiety. 2008;25:98-106. [DOI] [PubMed] [Google Scholar]
- 20. Sainsbury K, Mullan B, Sharpe L. Reduced quality of life in coeliac disease is more strongly associated with depression than gastrointestinal symptoms. J Psychosom Res. 2013;75:135-141. [DOI] [PubMed] [Google Scholar]
- 21. Zhang SX, Liu J, Jahanshahi AA, et al. At the height of the storm: healthcare staff’s health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain Behav Immun. 2020;87:144-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc. 1991;20:149-166. [DOI] [PubMed] [Google Scholar]
- 23. Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D. Am J Prev Med. 1994;10:77-84. [PubMed] [Google Scholar]
- 24. Shinan-Altman S, Levkovich I, Tavori G. Healthcare utilization among breast cancer patients during the COVID-19 outbreak. Palliat Support Care. 2020;18:385-391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67:1063-1078. [DOI] [PubMed] [Google Scholar]
- 26. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988;52:30–41. [DOI] [PubMed] [Google Scholar]
- 27. Ware JE, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220-233. [DOI] [PubMed] [Google Scholar]
- 28. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis. 2nd ed. The Guilford Press; 2018: 29. [Google Scholar]
- 29. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic and statistical considerations. J Pers Soc Psychol. 1986;51:1173-1182. [DOI] [PubMed] [Google Scholar]
- 30. Pieh C, Budimir S, Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res. 2020;136:110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhang Y, Ma ZF. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int J Environ Res Public Health. 2020;17:2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Djernes JK. Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatr Scand. 2006;113:372-387. [DOI] [PubMed] [Google Scholar]
- 33. Yanover C, Mizrahi B, Kalkstein N, et al. What factors increase the risk of complications in SARS-CoV-2–infected patients? A cohort study in a nationwide Israeli health organization. JMIR Public Health Surveill. 2020;6:e20872. [DOI] [PMC free article] [PubMed] [Google Scholar]


