Abstract
Background
The Australasian Integrative Medicine Association (AIMA) established a working group to develop the AIMA Guiding Principles for Letter Writing and Letter Writing Templates. The guiding principles were developed to promote effective communication between the diverse range of healthcare practitioners (HCPs) that patients choose to consult. Following the development of the Interprofessional Communication (IPC) resources, AIMA undertook a public consultation as part of a quality assurance process to evaluate the relevance and utility of the resource.
Aim
This study reports stakeholder feedback on AIMA’s draft guiding principles document. It explores stakeholder attitudes towards IPC and HCPs letter-writing, and interest in ongoing continuing professional development (CPD).
Methods
A cross-sectional survey involving 1) an online public consultation survey and 2) a paper survey collected following IPC CPD activities. Quantitative data were analysed using Chi square and Fisher-Freeman-Halton Test. Responses to open ended questions were coded and subject to a thematic analysis.
Results
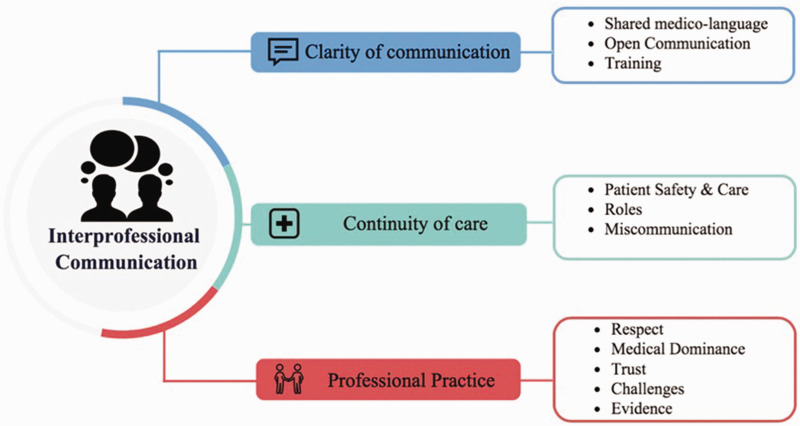
The 64 survey participants and 55 CPD participants represented the Australian healthcare sectors and lay community. Most thought IPC is important (n = 112/117; 96%) and the resources were informative (n = 112/119; 94%), understandable (n = 111/119; 93%), and clinically relevant (n = 105/117; 90%). HCP reported wide variations in their frequency of correspondence with other practitioner types, with rates often concerningly low. Key IPC themes identified were the importance of continuity of care, clarity of communication, and professional practice. CPD participants were most interested in further IPC training (p = 0.001).
Conclusions
The IPC resources affirm the role of formal communication pathways, such as letters of correspondence to support coordinated, patient-centred and multidisciplinary care. Challenges with letter writing and IPC signal the need for more student and professional education on the subject to promote continuity of patient care and the delivery of high quality, integrative medicine and health care services.
Keywords: professional education, interdisciplinary communication, cultural competency, professional practice, continuity of patient care, integrative medicine
Introduction
Interprofessional communication (IPC) is the liaison between different healthcare practitioners and the community to facilitate patient-centred care and patient safety, 1 and is integral to achieving coordinated patient care. Undeniably, communication failure between healthcare practitioners (HCPs) is recognised as a leading cause of avoidable patient harm. 2 HCPs attribute having insufficient time, different approaches and terminology, challenges with working within a medically dominant health system, and a lack of knowledge about other HCP roles as the main reasons for poor IPC. 3–5 In addition, disparities between the professional culture, the values and attitudes held, and real and perceived differences between HCPs further impede effective IPC. 3 These disparities are particularly apparent when comparing conventional medicine with traditional and complementary medicine (T&CM) practice. 4
Communication breakdown between conventional and T&CM practitioners is a concern. For instance, in a given year, an estimated 63% of Australians consult T&CM practitioners or use T&CM treatments, 6 and T&CM use tends to be higher for people with chronic diseases and higher pharmaceutical use.6–8 Non-disclosure of T&CM use is prevalent,9–12 and a recognised risk. 13 Such risks are further compounded by a lack of communication between HCPs and are potentially avoidable. 2
Effective IPC between all the HCPs that a patient chooses to consult, is key to coordinating safe and effective multidisciplinary care. Although communication pathways between medical doctors are well established, communication with other HCPs tends to be more ad-hoc. The resulting fragmentation healthcare, places additional an burden onto patients who are left to manage and coordinate their own care. 14
Strategies to support effective IPC includes a variety of evidence-based communication frameworks, for example: the SBAR (Situation, Background, Assessment, Recommendation) approach, 15 the Strategies and Tools to Enhance Performance and Patient Safety (Team STEPPS) curriculum 16 and Crew Resource Management. 17 The use of practical communication tools has been encouraged and includes the development of standardized communication tools such as interprofessional letter writing templates. 18 A shortcoming to date, is that strategies to support IPC have mostly focused on improving communication between the medical and nursing professions, and to a lesser extent with allied health practitioners, pharmacists and T&CM practitioners. 4
In response, the Australasian Integrative Medicine Association (AIMA) responded to practitioner and patient calls for guidance and education to improve IPC. AIMA is an independent, peak professional body representing medical practitioners and other HCPs who practice integrative medicine in Australasia. 19 In 2017, volunteer AIMA members comprising healthcare practitioners, academics and educators in Australia formed the AIMA IPC Working Group. The working group collaborated on preparing a draft document titled “Interprofessional Communication: AIMA Guiding Principles for Letter Writing” (hereafter referred to as the AIMA IPC Guidelines) that includes formal letter writing templates. Communication of confidential patient information should be sent via secure electronic or delivery services. As such, the focus on developing formal letter writing templates that could be sent by postal services or imbedded in secure electronic systems were considered the most relevant to the needs of Australian HCPs. For this study, Australian terminology is used when referring to different types of HCPs. Allied health practitioners refers to conventional HCPs that are not part of the medical, dental, nursing or pharmacy professions. T&CM practitioners refers to HCPs who provide healthcare services that are considered to be outside the dominant, conventional healthcare system. Medical doctors comprise primary care, general practitioners (GPs) and secondary care, medical specialists. Integrative medicine (IM) practitioners refers to any type of conventional HCP who integrates T&CM in their clinical practice.
Along with supporting IPC in general, a key objective was to assist all practitioners with navigating the relatively new terrain of integrative medicine (IM) and to foster professional cultural competence between the diverse range of HCPs that patients choose to involve in their health care. Prior to ratifying the AIMA IPC Guidelines, 20 AIMA undertook a public consultation process for quality assurance. The contents of the draft document and letter-writing templates were also presented in a workshop format at various AIMA continuing professional development (CPD) events. This paper presents the results obtained from the feedback collected during the public consultation and CPD events. The aim was to collate and analyse the feedback on the relevance and utility of the AIMA IPC Guidelines; explore participants’ attitudes towards, and perceptions of interprofessional communication; and ascertain healthcare professionals’ needs and preferences for further education.
Methods
A cross-sectional survey design was employed involving 1) an online public consultation survey and 2) a paper survey collected following IPC CPD activities. The 13-item, public consultation survey (Supplementary File 1), was administered online via SurveyMonkey. 21 It was open from the 7th January to the 9th September 2019. The survey was advertised through the AIMA website and newsletters. Emails were sent to key stakeholders of AIMA comprising – 12 professional associations, 29 educational institutions, 2 registration bodies, 4 natural therapy foundations and individuals on the AIMA email list, inviting them to participate in the public consultation and when relevant, requesting the organisation to invite their staff or members to participate via their own newsletter or electronic mailout. Participants were given the option of providing anonymous or confidential responses, the latter included providing a contact email address. Skip questions were used so that only HCP were asked about their clinical practice and continuing professional education. Written consent was given prior to using de-identified responses for the purpose of this research study.
CPD participants were recruited from two events that were held in Australia between August 2017 and May 2018. The events were led by AIMA PC authors (CE, AT, AF and LF) and open to all types of HCP, including non-AIMA members. Anonymous, voluntary feedback from the attendees was provided via an 11-item paper survey questionnaire (Supplemental File 2). CPD participants were verbally advised that their de-identified responses would be used when finalising the draft document and letter templates, and to inform future IPC educational activities.
Participants from both sample sources were asked to rank statements regarding the importance, clarity, and relevance of the AIMA IPC Guidelines and accompanying letter writing templates 20 using a 5-point Likert scale. Statements were followed with an option to provide free-text responses for explanatory justification of choice and/or provide further comments. The purpose of these and other open-ended questions was to explore the attitudes and opinions of participants regarding IPC, letter writing templates and their educational needs.
At the completion of data collection, the open ended responses provided in the CPD surveys and public consultation were screened to determine whether there was sufficient qualitative data for a thematic analysis. 22 Thematic analysis drew upon Braun and Clarke’s method that begins with data familiarisation, followed by coding using an inductive approach to identify themes and subthemes, and ends with a thematic review. 23 NVivo version 12 24 were used for the analysis of the responses to the open-ended questions. The thematic analyses of the responses to open-ended questions were conducted by Author JN and these were independently reviewed by JEH and JHu to check for accuracy and reliability. Different interpretations and disagreements were discussed until a consensus was reached.
The quantitative data collected from paper-based surveys were first manually entered into a second electronic survey in SurveyMonkey. 21 Following data cleaning, corresponding questions from the two datasets were merged into a single dataset and analysed in Statistical Package for Social Sciences version 25 (SPSS). 25 To help reduce the number of empty cells and low counts in cells, response categories were amalgamated when it was logically reasonable to do so. We investigated if there were any significant differences between the two groups (public consultation and CPD events) according to the different types of HCPs who participated, their feedback on the IPC resources and guidelines, their views on the importance of IPC, their interest in more IPC training and support, and preferred formats for IPC training. We hypothesised there would be differences between HCPs’ reported letter writing activities, both in the frequency of letter writing and to whom they commonly wrote to. Missing data was not imputed. The denominators presented in the results represent the number of responses to each question. The Pearson Chi square and Fisher-Freeman-Halton tests for r × c contingency tables were used for the inferential statistics. The level of significance for the 14 planned inferential tests was set at p = 0.05. All the authors had access to the data and met throughout the analysis to discuss the emerging findings and reach a consensus on their interpretation and the overall results.
Approval to undertake this study was obtained from the Human Research Ethics Committee at the University of Sydney (2018/517) and included retrospective approval to include de-identified CPD events responses.
Results
A total of 120 responses were received, 64 from the public consultation and 56 from the CPD events. One CPD questionnaire was excluded due to being illegible, leaving a total 119 included in the final analysis. The response rates for the two CPD events were 79% (n = 27/34) and 67% (n = 29/43). Most surveys were fully completed as per the reported denominators. The response rate to the public consultation could not be determined due to the broad reach and multiple stakeholders invited to the participate.
Most participants were HCPs representing a wide range of practitioner types, many of whom from the online survey also represented various professional bodies and educational institutions (Table 1). T&CM HCP were well represented, particularly in the CPD events. Underrepresented HCPs were specialist medical practitioners, registered nurses, and pharmacists. A significant difference between the various types of HCPs who participated in the public consultation and CPD events was found (Fisher-Freeman-Halton exact test p = 0.02). For example, a larger proportion of GPs participated in the public consultation (Table 1). Of the online GP participants, five specifically stated they practiced IM. Other IM practitioners included a biological dentist and a health coach with medical training.
Table 1.
Participant Characteristics.
| Respondent group |
Public Consultation n (%) |
CPD Events n (%) |
Total n (%) |
|---|---|---|---|
| Participants* | |||
| Allied Health Practitioner | 3 (5) | 5 (9) | 8 (7) |
| Complementary Medicine Practitioner | 32 (50) | 37 (67) | 69 (58) |
| General Practitioner | 15 (23) | 4 (7) | 19 (16) |
| Other Healthcare Practitioner | 2 (3) | 3 (5) | 5 (4) |
| Pharmacist | 3 (5) | 0 (0) | 3 (3) |
| Registered Nurse | 2 (3) | 1 (2) | 3 (3) |
| Specialist Medical Practitioner | 0 (0) | 2 (4) | 2 (2) |
| Lay Community | 5 (8) | 1 (2) | 6 (5) |
| Not Specified† | 2 (3) | 2 (4) | 4 (3) |
| Total | 64 (100) | 55 (100) | 119 (100) |
CPD: Continuing professional development.
*Difference between participants from public consultation and CPD events: Fisher-Freeman-Halton exact test p = 0.02.
† all the respondents in the Not Specified category of the public consultation survey were healthcare practitioners.
HCPs were asked how often they wrote letters to other types of HCPs within a 12-month period. The Fisher-Freeman-Halton exact test was used to determine if there were any differences between the three HCP groups (medical/dental, T&CM HCPs, and allied health/other HCPs) and their frequency of letter writing that was categorised as often (at least twice a month), sometimes/rarely, or never. Except for the frequency of letter writing to GPs (p = 0.98) and managers (p = 0.65), significant differences were found between the three HCP groups’ reported frequency of letter writing to medical specialists (p = 0.000), pharmacists (p = 0.004), nurses (p = 0.000), allied health (p = 0.000), and T&CM HCPs (p = 0.03) (Supplementary File 3). Notable findings included most of the medical/dental HCPs reporting they wrote to specialist medical practitioners (n = 18/22) at least twice a month, compared to less than one tenth of the allied health/other HCP (n = 1/15) and T&CM HCPs (n = 5/54). Similarly, compared to the allied health/other HCPs (n = 1/15) and T&CM HCPs (n = 5/54) groups, a larger proportion of the medical/dental HCPs (n = 13/22) reported often writing to allied health practitioners. At least half of the allied health/other HCPs and T&CM HCPs reported they never wrote to specialists, pharmacists, and nurses. Around half of the allied health/other HCPs (n = 8/14) also reported never writing to T&CM HCPs, whilst around a quarter of medical/dental HCPs never wrote to T&CM HCPs (n = 6/22). Over two-thirds of all the HCPs reported never writing to healthcare administrators or practice managers.
Most participants (81%, n = 95/117) held the opinion that formal communication such as letters of correspondence between HCPs was very important and no-one thought it was not important at all (Table 2). No statistically significance difference was found between the public consultation and CPD participant responses (Fisher-Freeman-Halton exact test p = 0.075).
Table 2.
Opinions About Formal Communication and IPC Education.
|
Public Consultation n (%) |
CPD Events n (%) |
Total n (%) |
p-Value | |
|---|---|---|---|---|
| Importance of Formal Communication | ||||
| Very important | 52 (81) | 43 (81) | 95 (81) | 0.075* |
| Somewhat important | 11 (17) | 6 (11) | 17 (15) | |
| Undecided | 0 (0) | 4 (8) | 4 (3) | |
| Unimportant | 1(2) | 0 (0) | 1 (1) | |
| Not important at all | 0 (0) | 0 (0) | 0 (0) | |
| Total | 64 (100) | 53 (100) | 117 (100) | |
| HCP interest in IPC training/support‡ | ||||
| Yes | 19 (33) | 33 (63) | 52 (48) | 0.001† |
| Maybe | 23 (40) | 16 (31) | 39 (36) | |
| No | 15 (26) | 3 (6) | 18 (17) | |
| Total | 57 (100)‡ | 52 (100) | 109 (100) | |
| Most preferred CPD format** | ||||
| Face to face | 9 (21) | 22 (49) | 31 (36) | 0.012 † |
| Downloaded written material | 14 (33) | 14 (31) | 28 (32) | |
| Webinars/online learning | 19 (45) | 9 (20) | 28 (32) | |
| Total | **42 (100) | 45 (100) | 87 (100) | |
CPD: Continuing professional development; HCP: Healthcare practitioner; IPC: Interprofessional communication.
* Fisher-Freeman-Halton exact test.
† X2 test for independence.
‡: question skipped for non-HCP.
** question skipped if HCP was not interested in further training or support for IPC.
In contrast, less than half (48%, n = 52/109) confirmed their interest in further training or support for IPC and the two groups had different preferences for CPD formats (Table 2). Significantly more CPD participants were interested in further IPC training and support (X2 (2, N = 109) = 12.82; p = 0.001) and preferred to receive this face-to-face in seminars and workshops (X2 (2, N = 87) = 8.93; p = 0.012).
CPD participants were asked to provide feedback about the CPD event and the accompanying two-page summary document and letter templates. Participants in the public consultation were asked to provide feedback on the longer AIMA IPC Guidelines that also included letter templates. Overall, the feedback was very positive (Table 3).
Table 3.
Feedback on AIMA IPC Guidelines.
| Public Consultationn (%) | CPD Eventsn (%) | Totaln (%) | p-Value† | |
|---|---|---|---|---|
| Informative | ||||
| Strongly Agree | 34 (53) | 27 (49) | 61 (51) | 0.65 |
| Agree | 25 (39) | 26 (47) | 51 (43) | |
| Undecided | 4 (6) | 1 (2) | 5 (4) | |
| Disagree or Strongly disagree | 1 (2) | 1 (2) | 2 (2) | |
| Total | 64 (100) | 55 (100) | 119 (100) | |
| Clear and easily understood | ||||
| Strongly Agree | 24 (38) | 25 (45) | 49 (41) | 0.50 |
| Agree | 37 (58) | 25 (45) | 62 (52) | |
| Undecided | 2 (3) | 4 (7) | 6 (5) | |
| Disagree or Strongly disagree | 1 (2) | 1 (2) | 2 (2) | |
| Total | 64 (100) | 55 (100) | 119 (100) | |
| Relevant to clinical practice | ||||
| Strongly Agree | 33 (52) | 23 (43) | 56 (48) | 0.65 |
| Agree | 25 (39) | 24 (45) | 49 (42) | |
| Undecided | 6 (9) | 5 (9) | 11(9) | |
| Disagree or Strongly disagree | 0 (0) | 1 (2) | 1 (1) | |
| Total | 64 (100) | 53 (100) | 117 (100) |
†Fisher-Freeman-Halton exact test.
Comments specific to the presentation of the IPC resources mostly focused on the letter writing templates, for example “they should be a lot simpler” and recommendations for additional content such as “[for a] doctor reassessing particular medications patient is on” (GP-5) and “more information… to include regarding herbs prescribed and their functions” (GP-9)
None of the CPD participants provided extended responses. Extended responses from 41 participants in the online public consultation survey to questions concerning IPC and formal communication provided a range of opinions that the authors deemed to justify conducting a thematic analysis. A strong interest was expressed about the value and importance of formal communication including letters of correspondence. This view was supported by the quantitative results. Three meta-themes: 1) Clarity of communication, 2) Continuity of care and 3) Professional practice, and eleven sub-themes were identified (Figure 1). The thematic analysis and indicative quotes extracted directly from the participant responses are presented in Table 4.
Figure 1.
Themes and Sub-Themes.
Table 4.
Metathemes Subthemes and Quotes.
| THEME 1—Clarity of communication |
|
Subtheme 1: Shared medico-language “Is very important to not only have a common language for communication by also accepted way of communicating key information specially in the model of shared care” (General Practitioner 1) Subtheme 2: Open Communication “It is essential that I am aware of a patient's entire medical history, medications, supplements and other therapies if I am to provide them with optimal care” (General Practitioner 2) “Each side needs to know exactly what the other is doing in order to avoid conflicts with patient treatment” (Allied HCP 1) “Helps document what is going on, helps reduce errors (especially when the patient receives correspondence), and provides a time line or history for the patient.” (T&CM HCP 1) Subtheme 3: Training “Naturopaths need more training in it” (Allied HCP 2) “Missed diagnoses etc are mostly in the mind of the conservative medical professionals. Let’s try to keep this simple, not such a high standard that no-one will be able to achieve it.” (General Practitioner 2) “Perhaps advice on how to manage bad experiences received from medical professionals” (T&CM HCP 2) |
|
THEME 2 – Continuity of care Subtheme 1: Patient Safety and Care “If quality communication can be instigated between various complementary medicine practitioners, there will be improved patient care” (General Practitioner 3) “It is vital that the medical profession work cooperatively with alternative health care practitioners to give the patient the best chance to improve their health. Working together, helps recognize diagnosable conditions so that a treatment plan can be formulated involving relevant health practitioners and the patient. Formal communication helps document what is going on, helps reduce errors (especially when the patient receives correspondence)” (T&CM HCP 1) “It is collaborative and respectful and should foster continuity of care and reduce risks of adverse outcomes.” (Registered Nurse 1) “It's imperative for the client/patient's care that any health care provider works collaboratively with others who are treating that person” (Allied HCP 2) Subtheme 2: Roles “Open communication to understand each other’s…modality of treatment would enhance patient care” (General Practitioner 4) Subtheme 3: Miscommunication “Verbal communication from the client from other professionals with a hand written note is usually the form of communication” (T&CM HCP 3) “Ensure there is no miscommunication or error in the relay of information” (Pharmacist 1) “Prevent misunderstanding, allowing us to reinforce the same health messages and prevent over-ordering of pathology/ radiology and over-prescribing” (General Practitioner 5) THEME 3—Professional Practice Subtheme 1: Respect “Very [important] for remedial massage therapists to know how to write referral letters to GPs, so that they can be taken seriously” (T&CM HCP 3) “It is definitely the way forward for respect and understanding between all health practitioners and may subconsciously be some of the reason why many General Practitioners seem to despise naturopaths” (General practitioner 6) Subtheme 2: Medical Dominance “Complementary medical practitioners are often dismissed and some specialists dissuade patients from complementary medicine” (General Practitioner 7) “Whether the letters are read. With the exception of specialists, who are generally more inclined to respond, I rarely receive a reply from GPs.” (Allied HCP 2) Subtheme 3: Trust “Increase trust and working together between the professions” (T&CM HCP 4) “It helps establish professional relationship across the full scope of medical services and modalities” (Allied HCP 3) Subtheme 4: Challenges ‘These requirements are so onerous that it will impact on the HCP’s ability to provide care in the time available as it’ll increase time by a significant percentage’ and it’ll add ‘another layer of admin [Integrative Medicine General Practitioners] are not keen on’ (General Practitioner 7) “I think natural therapists are asking for too many tests and this is putting stress onto the doctors” (T&CM HCP 5) “I'm still not sure about the legal ramifications, particularly with the proposed Medical Board of Australia guidelines on complementary medicine” (General Practitioner 3) Subtheme 5: Evidence “It can be used as a way of evidence that communication took place in case an incident happens to the patient as an outcome” (Pharmacist 2) |
HCP: Healthcare practitioner; T&CM: Traditional & complementary medicine practitioner
The data obtained from HCPs provided perspectives which informed the final meta-themes illustrated in Table 4. Participants suggested strategies to achieve open and transparent IPC including training to overcome “bad experiences” and having a common medico-language to share patient information. To promote patient safety, mitigation of common concerns such as miscommunication and clarity of HCP roles were raised. For instance, an allied health practitioner claimed:
“Sometimes, I don’t receive reports back from practitioners I have referred to which means I rely on my client to give me a sense of how their diagnosis and treatment went”. (AH-1)
Hence, there were consistent responses from HCPs encouraging the endorsement of formal documents such as the AIMA IPC Guidelines to ensure continuity of care and reduction in “adverse [health] outcomes”.
Many HCPs expressed concerns about medico-legal uncertainties or the addition of administrative duties upon enactment of the AIMA IPC Guidelines. The manifestation of medical dominance towards other HCPs, particularly T&CM and allied health practitioners alluded to the idea that these letters of correspondence may be a waste of time, as GPs rarely reply or are dismissive of other therapies. Conversely, other HCPs noted that letters can also serve as a tool for formally documenting clinical information and providing evidence of the clinical encounter. Despite these concerns, participants recognised that formal communication tools were an important aspect of professional practice that can help minimise miscommunication and build the foundations of trust and respect between the HCPs.
Discussion
The results of this quality assurance and feedback process reinforces the value and importance HCPs place on the role of formal communication pathways to promote the delivery of coordinated, patient-centered, quality healthcare. 4 Letters of correspondence were thought to demonstrate professionalism, provide opportunities to informally educate other HCPs about different philosophies and approaches to medicine and health, and facilitate patient involvement. Participants acknowledged there is a need to ‘speak the same language for our patients’ sake.’ However, apart from correspondence between medical practitioners, HCPs tended not to routinely write letters of correspondence to other HCPs. To this end, like other communication tools and frameworks,15,16 the AIMA IPC Guidelines and accompanying letter templates could play an important role in supporting IPC and collaborative, integrative practice.
What differentiates this study and the AIMA IPC Guidelines from previous work, is the inclusion of the broader spectrum of HCP with a focus on IM and T&CM practitioners. To our knowledge, these professions have not been previously considered in formal IPC resources. This diverse and inclusive approach aligns with broader calls to improve cultural competence in contemporary health care that includes addressing professional cultural divides.4,26 The AIMA IPC Guidelines defines cultural competence in Integrative Medicine as “an awareness of, and respect for the diverse range of health care practices, paradigms and terminologies that patients and practitioners use.” Cultural competence enables HCPs to work effectively with each other and their patients in cross-cultural situations, and for healthcare systems to deliver services that meet the social, cultural, and linguistic needs of patients and HCPs. 4 All HCPs therefore need to be aware of how their own cultural and professional biases can negatively impact communication with patients, informal and formal caregivers, and other HCPs. 26
Known communication barriers between HCPs include real and perceived power differentials that are reflected in the use of professional jargon, rather than a commonly shared language. 26 This can impair the continuity of a patient’s care that is reliant on the transmission of relevant, accurate and understandable information about the patient’s clinical history and current management. The recommendation in the AIMA IPC Guidelines to limit the use of technical words that are universally understood was well received by study participants. In keeping with other research,27,28 participants highlighted that the use of different ‘medico’ languages and terminology can negatively impact the clarity of communication.
Interprofessional differences in health care knowledge and lack of clarity about different roles were also noted to further influence what information is communicated and how it is received, understood, and incorporated into patient care, along with its perceived importance. Respondent feedback highlighted that letters of correspondence can be utilized to help clarify roles and build trust between HCPs. Understanding and respecting the roles of other types of HCPs is important and can benefit patients by facilitating continuity of care, 29 and collaborative practice, 28 so that the expertise and skills of each HCP can be used in a timely and appropriate way to optimize patient care and outcomes. 4
Cultural, language and professional barriers between conventional and T&CM HCPs are often cited as a reason for implementing educational strategies that support effective IPC and collaborative practice.3,4,28 Central to this is an agreed, standardized healthcare-language that promotes a clearer understanding of the different approaches used by HCPs,27,28 and our study supports this premise. Education and training that focus on clarity of communication can promote effective and easily understood information during patient handover. 4 For example, the SBAR framework (Situation, Background, Assessment and Recommendation) and extended ISBAR framework (I: Identify) is a verbal communication tool designed to bridge IPC barriers and has been shown to support patient handover and cultivate collaboration between different HCPs. 15 The AIMA letter writing resources adopted a modified framework version of ISBAR that extended ‘A’ to include ‘Actions’ and ‘R’ to include ‘Requests’ so that the acronym more readily applies to letter writing. The results of our study suggest that HCPs could see the relevance of the structured ISBAR approach within the context of letter writing, and how this approach could help reduce miscommunication.
Like previous studies being ‘time poor’ was cited as another barrier to writing letters of correspondence.4,27,29 Electronic health systems have been proposed to increase the likelihood of comprehensive documentation by HCPs. 30 It has also been reported that writing letters of correspondence positively correlates with the quality of a practitioner’s clinical records. 5 Therefore, we suggest that letter templates, like those that were the subject of this study, are considered for integration into electronic clinical record systems. This view is supported in our results suggesting a more concise resource implemented within the electronic health system or program would be suited to the limited time HCPs have to devote to letter writing.
Our findings further confirm ongoing concerns and uncertainties about potential medico-legal risks to conventional HCPs when referring to T&CM practitioners.31,32 Comments from some of the medical doctors suggested that a lack of clarity about T&CM professional roles and responsibilities, and no statutory regulation for some T&CM practitioners underpinned these concerns. Formal communication strategies that advance practice and build trust between HCPs would, therefore, benefit from a stronger regulatory framework for T&CM practitioners in Australia. Furthermore, in line with patients’ healthcare choices, conventional healthcare systems will need to find ways to shift from the current culture in which medical doctors are placed in professional silos, to a more equitable system that enables patients to readily benefit from the skills and expertise of the broader team of HCPs that they seek to include in their health care.33,34
The finding that GPs reported writing to other conventional HCPs more than T&CM practitioners was not surprising. In Australia, a written GP referral is a requisite for patients accessing public and private health insurance rebates for consultations with medical specialists and some allied health practitioners. Further, sending and receiving referral letters, discharge letters and other patient reports are an established practice and the most common reasons for formal communications between conventional HCP. 5 Given the frequent concurrent use of pharmaceutical and T&CMs,6–8 the low rates of written communication between T&CM practitioners, pharmacists, and medical practitioners was concerning. Whilst pharmacists can play a central role in identifying and preventing T&CM-drug interactions, 35 particularly since the most common place of purchase of T&CM products is pharmacy outlets, the extent to which this is occurring is unclear. T&CM practitioners reported writing to GPs more often than to pharmacists, so it is possible that medication reconciliation (that includes T&CM products) occurs through this line of communication. However, communication between these practitioners was still low, and these communication gaps may be set to widen, as most T&CM practitioner groups do not have authority to access Australia’s shared electronic communication platforms, including the national electronic patient health record, ‘My Health Record’.
Core to the AIMA IPC Guidelines is patient-centered care that is respectful, inclusive and actively involves patients in their healthcare. Continuity of care is improved when patients play an integral role in the transmission of their medical/health information.36,37 Further, patients who have a detailed understanding of the therapies they are using, have a reduced risk of harm associated with poor communication. 38 As such, the AIMA letter writing templates include prompts to c.c. the patient. Whilst it was not explored in this study, future research could investigate how often patients are included in letters of correspondence between their HCP, the circumstances in which this occurs, and most importantly, patients’ perspectives and outcomes.
Limitations of this study include the views of HCPs less interested in IPC and integrative medicine and health are unlikely to have been captured. Thus, the positive views expressed by participants may not be representative of the broader healthcare system. The underrepresentation of some HCPs in the study, in particular pharmacists, nurses, and medical specialists, may also limit the generalizability of our findings. Also limiting the generalizability was that only Australian participants were included. Further studies would be helpful to gauge the perspectives of more HCP and to compare differences between countries and health care systems. The absence of the ‘patients voice’ is another limitation of this study, as only a handful of lay persons participated. We strongly encourage additional research that explores patients views about IPC and letter writing with a focus on integrative medicine and health. Combining the quantitative and qualitative data for the analysis may have resulted in double counting as it was not possible to know whether a participant completed both the CPD event questionnaire and online survey. Further, statistically significant differences between the two groups according to their characteristics (Table 1) and views about IPC education (Table 2) may have influenced the participants’ responses to questions about ongoing IPC education and frequency of letter writing. For example, not writing letters may be a reason why participants attended the IPC CPD events or wanted more IPC education. However, the sample sizes were too small to conduct a multivariate analysis to adjust for any potential confounding effects. Other limitations of the statistical analysis included not calculating the sample sizes and power a priori. As such, the likelihood of type 1 and 2 errors cannot be assessed. The large p values for all but one non-significant result lowers the likelihood of a false negative result. The only borderline non-significant result was the importance of formal communication (Table 2) that reflected marginal differences in the proportions who thought formal communication was somewhat important, unimportant or were undecided. Setting the p value at 0.01 rather than 0.05, would lower the risk of false positive results. 39 In this case, the differences between the types of HCPs who participated in the public consultation compared to the CPD activities in Table 1 and the differences between the three HCP groups’ reported frequency of letter writing to T&CM practitioners would no longer be significant. Finally, manually generating a code book for the qualitative data analysis may have strengthened the analysis of the open-ended responses. 40 Despite these study limitations, the feedback was sufficient for AIMA’s quality assurance process regarding their draft AIMA IPC Guidelines and helped shed light on important aspects of IPC and how potential differences between healthcare professions might impact patient care.
Next steps
Following the completion of the study, and in response to the feedback obtained during the public consultation process, minor revisions were made to the AIMA IPC Guidelines. The final version was ratified by the AIMA Board and published in 2020. 20 In response to the expression of interest by study participants and from AIMA members for more IPC education, a CPD online module was developed by two academics, one an accredited naturopath and tenured academic, the other a medical doctor, naturopath and educator. The CPD module was scaffolded on the AIMA IPC Guidelines and the letter writing templates were used to model these principles in a concise and pragmatic manner. The module is currently undergoing peer review, after which it will be made available through AIMA to its members and potentially more widely.
Conclusion
The conventional, allied and T&CM healthcare practitioners that were included in this study distinctly valued the importance of effective IPC in facilitating coordinated patient-centered care. The IPC resources that were the subject of this study were considered relevant and practical. There are multiple, complex factors impacting effective IPC and the AIMA IPC Guidelines will not solely address all of these. Further research and strategies, such as IPC education that aim to foster continuity of care, clarity in communication, and professional practice are encouraged.
Supplemental Material
Supplemental material, sj-pdf-1-gam-10.1177_2164956121992338 for Can We All Speak the Same ‘Language’ for Our Patients’ Sake? Feedback on Interprofessional Communication and Related Resources by Janet Nguyen, BPharm (Hons), Jennifer Hunter, BMed, MScPH, PhD, Lorraine Smith, BA (Hons), PhD and Joanna E Harnett, BHSc, MHSc, PhD, Grad Cert Educational Studies in Global Advances in Health and Medicine
Supplemental material, sj-pdf-2-gam-10.1177_2164956121992338 for Can We All Speak the Same ‘Language’ for Our Patients’ Sake? Feedback on Interprofessional Communication and Related Resources by Janet Nguyen, BPharm (Hons), Jennifer Hunter, BMed, MScPH, PhD, Lorraine Smith, BA (Hons), PhD and Joanna E Harnett, BHSc, MHSc, PhD, Grad Cert Educational Studies in Global Advances in Health and Medicine
Supplemental material, sj-pdf-3-gam-10.1177_2164956121992338 for Can We All Speak the Same ‘Language’ for Our Patients’ Sake? Feedback on Interprofessional Communication and Related Resources by Janet Nguyen, BPharm (Hons), Jennifer Hunter, BMed, MScPH, PhD, Lorraine Smith, BA (Hons), PhD and Joanna E Harnett, BHSc, MHSc, PhD, Grad Cert Educational Studies in Global Advances in Health and Medicine
Acknowledgments
Special thanks to the AIMA Board for collecting the CPD feedback and facilitating the public consultation, and the AIMA IPC Working Group (Jennifer Hunter (Chair), Brian Callan, Marc Cohen, Kylie Dodsworth, Caroline Ee, Amy Forth, Louise Furney, Elysia Humphries, Joanna Harnett, Paulette Maroun, Teresa Mitchell-Paterson, Paul Orrock and Amy Tyler) for the preparation of the draft AIMA Guiding Principles for Letter Writing.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Author J.Hu. (Jennifer Hunter), is the Chair of the Australasian Integrative Medicine Association Interprofessional Communication Working Group that prepared the AIMA IPC Guidelines, is engaged in integrative medicine primary care clinical practice, and is affiliated with NICM Health Research Institute. As a medical research institute, NICM Health Research Institute receives research grants and donations from foundations, universities, government agencies, individuals and industry. Sponsors and donors provide untied funding for work to advance the vision and mission of the institute. Author J.Ha. (Joanna Harnett) is engaged T&CM education and research at The University of Sydney. As a researcher in the field of complementary medicine, receives research grants and donations from industry and internal and external funding bodies. J.Ha. serves on the board of the Australasian Integrative Medicine Association who actively promotes IPC between conventional and T&CM HCP. The project that is the subject of this article was not undertaken as part of a contractual relationship with any donor or sponsor. All other authors declare no conflicts of interest. Authors J.N. and L.S. have nothing to declare.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Jennifer Hunter https://orcid.org/0000-0002-6109-9134
Joanna E Harnett https://orcid.org/0000-0001-9904-2144
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Claramita M, Riskiyana R, Susilo AP, Huriyati E, Wahyuningsih MS, Norcini JJ. interprofessional communication in a socio-hierarchical culture: development of the Tri-O guide. J Multidisciplin Healthcare. 2019; 12:191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Joint Commission. (2016). Summary data of sentinel events 2004-2015. https://www.jointcommission.org/assets/1/18/2004-2015_SE_Stats_Summary.pdf. Accessed January 22, 2021.
- 3.Hall P. Interprofessional teamwork: professional cultures as barriers. J Interprofession Care. 2005; 19(sup1):188–196. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen J, Smith L, Hunter J, Harnett JE. Conventional and complementary medicine health care practitioners’ perspectives on interprofessional communication: a qualitative rapid review. Medicina. 2019; 55(10):650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vermeir P, Vandijck D, Degroote S, et al. Communication in healthcare: a narrative review of the literature and practical recommendations. Int J Clin Pract. 2015; 69(11):1257–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steel A, McIntyre E, Harnett J, et al. Complementary medicine use in the Australian population: results of a nationally-representative cross-sectional survey. Sci Rep. 2018; 8(1):17325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leach MJ. Profiling the Australian consumer of complementary and alternative medicine: a secondary analysis of national health survey data. Alternat Ther Health Med. 2016; 22(4):64–72. [PubMed] [Google Scholar]
- 8.Harnett JE, McIntyre E, Steel A, Foley H, Sibbritt D, Adams J. Use of Complementary medicine products: a nationally representative cross-sectional survey of 2019 Australian adults. BMJ Open. 2019; 9(7):e024198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang H-Y, Chang H-L, Siren B. Exploring the decision to disclose the use of natural products among outpatients: a mixed-method study. BMC Complement Alternat Med. 2013; 13(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jou J, Johnson PJ. Nondisclosure of complementary and alternative medicine use to primary care physicians: findings from the 2012 National Health Interview Survey. JAMA Intern Med. 2016; 176(4):545–546. [DOI] [PubMed] [Google Scholar]
- 11.Stub T, Quandt SA, Arcury TA, Sandberg JC, Kristoffersen AE. Complementary and conventional providers in cancer care: experience of communication with patients and steps to improve communication with other providers. BMC Complement Alternat Med. 2017; 17(1):301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sullivan A, Gilbar P, Curtain C. Complementary and alternative medicine use in cancer patients in rural Australia. Integrat Cancer Ther. 2015; 14(4):350–358. [DOI] [PubMed] [Google Scholar]
- 13.Wardle JJL, Adams J. Indirect and non-health risks associated with complementary and alternative medicine use: an integrative review. Eur J Integrat Med. 2014; 6(4):409–422. [Google Scholar]
- 14.Kern LM, Safford MM, Slavin MJ, et al. Patients’ and providers’ views on causes and consequences of healthcare fragmentation in the ambulatory setting: a qualitative study. J Gen Intern Med. 2019; 34(6):899–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Müller M, Jürgens J, Redaèlli M, Klingberg K, Hautz WE, Stock S. Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open. 2018; 8(8):e022202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gaston T, Short N, Ralyea C, Casterline G. Promoting patient safety: results of a TeamSTEPPS® initiative. JONA: J Nurs Admin. 2016; 46(4):201–207. [DOI] [PubMed] [Google Scholar]
- 17.Gross B, Rusin L, Kiesewetter J, et al. Crew resource management training in healthcare: a systematic review of intervention design, training conditions and evaluation. BMJ Open. 2019; 9(2):e025247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tattersall MH, Butow PN, Brown JE, Thompson JF. Improving doctors’ letters. Med J Australia. 2002; 177(9):516–520. [DOI] [PubMed] [Google Scholar]
- 19.AIMA. About AIMA. https://www.aima.net.au/about/. Published 2018. Accessed January 22, 2021.
- 20.The Australasian Integrative Medicine Association Interprofessional Communication Working Group:AIMA Guiding Principles for Letter Writing. Terrigal New South Wales Australia: AIMA; 2020:61. http://www.aima.net.au/interprofessional-communications-guiding-principles/ ISBN: 978-0-646-82907-4
- 21.Creswell JW, Klassen AC, Plano Clark VL, Smith KC. Best practices for mixed methods research in the health sciences. Bethesda (Maryland): National Institutes of Health. 2011; 2013:541–545. [Google Scholar]
- 22.Farmer T, Robinson K, Elliott SJ, Eyles J. Developing and implementing a triangulation protocol for qualitative health research. Qualitat Health Res. 2006; 16(3):377–394. [DOI] [PubMed] [Google Scholar]
- 23.Braun V, Clarke V. Using thematic analysis in psychology. Qualitat Res Psychol. 2006; 3(2):77–101. [Google Scholar]
- 24.NVivo Qualitative Data Analysis Software; 2018.
- 25.IBM SPSS Statistics for Windows VRICA; 2017.
- 26.Keller KB, Eggenberger TL, Belkowitz J, Sarsekeyeva M, Zito AR. Implementing successful interprofessional communication opportunities in health care education: a qualitative analysis. Int J Med Educ. 2013; 4:253. [Google Scholar]
- 27.Morley L, Cashell A. Collaboration in health care. J Med Imag Radiat Sci. 2017; 48(2):207–216. [DOI] [PubMed] [Google Scholar]
- 28.Suter E, Arndt J, Arthur N, Parboosingh J, Taylor E, Deutschlander S. Role understanding and effective communication as core competencies for collaborative practice. J Interprofession Care. 2009; 23(1):41–51. [DOI] [PubMed] [Google Scholar]
- 29.Mills JE, Francis K, Birks M, Coyle M, Henderson S, Jones J. Registered nurses as members of interprofessional primary health care teams in remote or isolated areas of Queensland: collaboration, communication and partnerships in practice. J Interprofession Care. 2010; 24(5):587–596. [DOI] [PubMed] [Google Scholar]
- 30.Schwarz CM, Hoffmann M, Schwarz P, Kamolz LP, Brunner G, Sendlhofer G. A systematic literature review and narrative synthesis on the risks of medical discharge letters for patients’ safety. BMC Health Serv Res. 2019; 19(1):158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Phelps K, Hassed C. General Practice: The Integrative Approach. Chatswood: Elsevier; 2011. [Google Scholar]
- 32.Brophy E. Referral to complementary practitioners. J Complement Med. 2003; 2(6):42. [Google Scholar]
- 33.Eassey D, McLachlan AJ, Brien JA, Krass I, Smith L. “I have nine specialists. They need to swap notes!” Australian patients’ perspectives of medication‐related problems following discharge from hospital. Health Expect. 2017; 20(5):1114–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. BMJ Qual Saf. 2004; 13(suppl 1):i85–i90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harnett JE, Ung COL, Hu H, Sultani M, Desselle SP. Advancing the pharmacist’s role in promoting the appropriate and safe use of dietary supplements. Complement Ther Med. 2019; 44:174–181. [DOI] [PubMed] [Google Scholar]
- 36.Eggins S, Slade D. Communication in clinical handover: improving the safety and quality of the patient experience. J Public Health Res. 2015; 4(3):666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weetman K, Wong G, Scott E, MacKenzie E, Schnurr S, Dale J. Improving best practice for patients receiving hospital discharge letters: a realist review. BMJ Open. 2019; 9(6):e027588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Newell S, Jordan Z. The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. JBI Database Syst Rev Implement Rep. 2015; 13(1):76–87. [DOI] [PubMed] [Google Scholar]
- 39.Feise RJ. Do multiple outcome measures require p-value adjustment? BMC Med Res Methodol. 2002; 2(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Roberts K, Dowell A, Nie J-B. Attempting rigour and replicability in thematic analysis of qualitative research data; a case study of codebook development. BMC Med Res Methodol. 2019; 19(1):66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-gam-10.1177_2164956121992338 for Can We All Speak the Same ‘Language’ for Our Patients’ Sake? Feedback on Interprofessional Communication and Related Resources by Janet Nguyen, BPharm (Hons), Jennifer Hunter, BMed, MScPH, PhD, Lorraine Smith, BA (Hons), PhD and Joanna E Harnett, BHSc, MHSc, PhD, Grad Cert Educational Studies in Global Advances in Health and Medicine
Supplemental material, sj-pdf-2-gam-10.1177_2164956121992338 for Can We All Speak the Same ‘Language’ for Our Patients’ Sake? Feedback on Interprofessional Communication and Related Resources by Janet Nguyen, BPharm (Hons), Jennifer Hunter, BMed, MScPH, PhD, Lorraine Smith, BA (Hons), PhD and Joanna E Harnett, BHSc, MHSc, PhD, Grad Cert Educational Studies in Global Advances in Health and Medicine
Supplemental material, sj-pdf-3-gam-10.1177_2164956121992338 for Can We All Speak the Same ‘Language’ for Our Patients’ Sake? Feedback on Interprofessional Communication and Related Resources by Janet Nguyen, BPharm (Hons), Jennifer Hunter, BMed, MScPH, PhD, Lorraine Smith, BA (Hons), PhD and Joanna E Harnett, BHSc, MHSc, PhD, Grad Cert Educational Studies in Global Advances in Health and Medicine