Abstract
Prostate cancer is the most common malignancy in men with high incidence of recurrence following treatment. Biochemical recurrence, as indicated by rising PSA levels following successful treatment of the primary disease, is a frequent encounter in routine clinical practice. 68Gallium-PSMA positron emission tomography/computer tomography has been widely accepted as the modality of choice with the highest impact in management of this group of patients. Pitfalls of this diagnostic technique stem from the diversity of histological entities, other than prostate tumour cells, which can demonstrate increased uptake of the radiotracer. We present a case of intracranial uptake of PSMA by meningioma in a patient with BCR, as a pitfall in imaging of prostate cancer. Knowledge of normal distribution of the tracer is of utmost importance when reading positron emission tomography/computer tomography imaging especially given the relative novelty of usage of 68Gallium-PSMA.
Keywords: Nuclear medicine, radionuclide studies, gallium68, PSMA PET/CT
Introduction
Prostate cancer is the most common malignant tumour in men worldwide,1 with annual age-adjusted incidence rates approaching 86 and 60 per 100,000 in North America and Europe, respectively.2 The clinical course of prostate cancer is highly variable with up to 30% of the patients experiencing biochemical recurrence within five years of primary curative treatment and a lethal potential in advanced cases.3
As such, modern health systems have evolved efficient assessment pathways for patients presenting with suspected and confirmed primary and recurrent prostate cancer. Despite advances in the workup of prostate cancer, upstaging and upgrading occur in up to one-third of cases.4
68Gallium prostate-specific membrane antigen (PSMA) positron emission tomography/computed tomography (PET/CT) is a non-invasive imaging technique for the detection of recurrent prostate cancer. The current literature suggests that 68Ga-PSMA PET/CT could result in a change in management intent in up to 51% of patients.5 Due to the unique properties of PSMA, it has been widely adopted as a promising, novel target for binding radiolabelled ligands and is a staple of the workup of prostate cancer in modern tertiary centres.
We present a case of a typical patient undergoing PSMA PET/CT, in which a common clinical pitfall was encountered.
Case report
Clinical history
A 67-year-old male with a history of treatment with brachytherapy in 2010 for prostate cancer, underwent surveillance PSMA PET/CT due to rising PSA levels. There was also history of incidental left frontal meningioma withheld at the time of reporting the study.
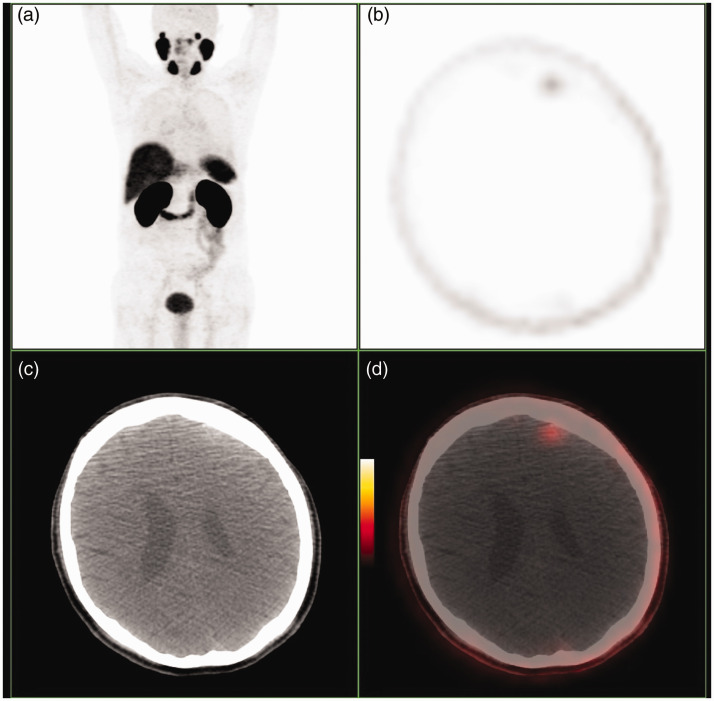
Fig. 1.
MIP (a), axial attenuation corrected PET (b), axial CT (c) and axial fused images (d). There is a focus of abnormal uptake in the left frontal lobe which correlates with a subtle hyperdensity on non-contrast CT, consistent with meningioma.
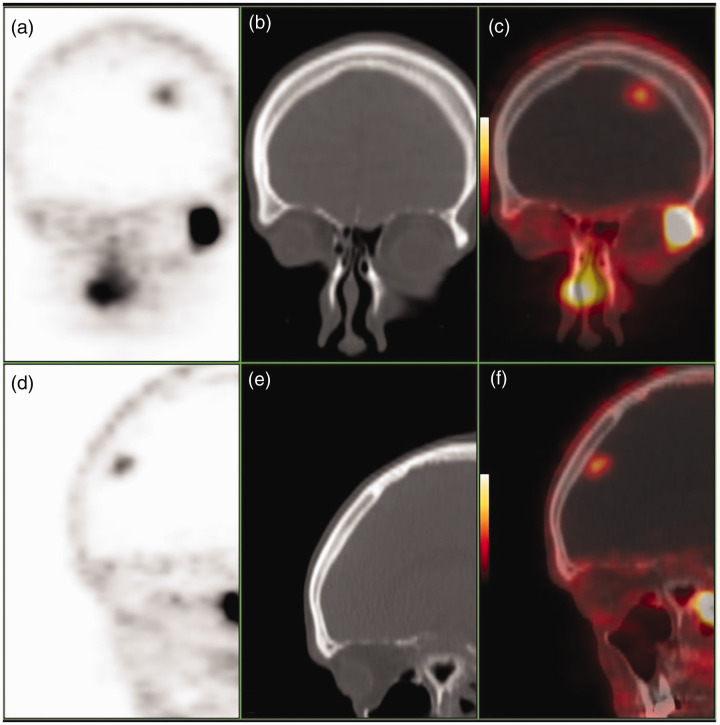
Fig. 2.
Coronal attenuation corrected PET (a), coronal CT (b), coronal fused image (c), sagittal attenuation corrected PET (d), sagittal CT (e) and sagittal fused image (f). Further demonstration of the focus of abnormal uptake in the left frontal lobe. The hyperdensity is readily appreciated on CT views.
Imaging findings
A PET/CT study with oral contrast from the vertex of the skull through the pelvis was performed. This demonstrated a focus of abnormal uptake within the left frontal lobe (Fig. 1). On initial assessment, a mis-registered metastatic focus within the adjacent skull seemed likely. Further scrutiny resulted in appreciation of a subtle hyperdensity within the frontal parenchyma. Furthermore, correcting for mis-registration beyond the skull resulted in more confidence in allocating the uptake to the brain rather than skull (Fig. 2). Subsequently, history consistent with the previously diagnosed meningioma confirmed the diagnosis.
Discussion
68Gallium is one of the first positron-emitting radionuclides to have been used in diagnostic imaging, having been used as early as the 1960s.6 Despite this early clinical use, the US FDA only approved the first kit for the preparation of 68Gallium in June 2016, partly due to complex manufacturing procedure of earlier Gallium-generators using ethylenediaminetetraacetic acid (EDTA) which led to complex, expensive preparation of the radiopharmaceutical. Optimisation of 68Gallium purification methods was only commercially available lately with promising results.
Imaging with 68Gallium is currently applied to the localisation of somatostatin receptor positive neuroendocrine tumours and detection of biochemical recurrence of previously treated prostate cancer, the latter through labelling with prostate-specific membrane antigen (PSMA) ligands.7
PSMA is a type II transmembrane protein, normally expressed in the cytoplasm and on the apical surface of prostatic ductal epithelium. There is a 100 to 1000 fold increase in expression of PSMA in prostate cancer cells.8 The use of 68Gallium PSMA PET/CT has been shown to provide accurate localisation of tumour lesions in patients with intermediate and high-risk prostate cancer (sensitivity 68.42% and specificity 98.23% in high risk groups).9
Meningiomas are the most common primary intracranial tumour with the prevalence of subclinical cases estimated as up to 2.8% of the population.10 Meningiomas represent a benign process in 95% of cases.11 Meningiomas have been shown to express somatostatin-receptor-2 resulting in increased uptake of 68Gallium-labelled somatostatin analogues such as DOTATATE.12 Meningioma demonstrating PSMA uptake is a pitfall in imaging of prostate cancer, which may result in false positive diagnosis.
This case represents a typical clinical scenario in which a patient undergoes surveillance imaging for disease recurrence. However, the detection of intracranial radiotracer uptake could be misconstrued as a concerning finding, especially given the relative novelty of usage of 68Gallium-PSMA. Careful technical attention should be given when acquiring the images to avoid mis-registration, and the reader should take the technical imperfections into consideration.
In conclusion, 68Gallium-PSMA uptake is not entirely unique to prostate cancer and may be seen in a range of benign as well as malignant pathologies.13 To this end, the knowledge of normal distribution of the tracer is paramount and acquiring collateral history is mandatory. It would be imperative to convey the benign nature of the findings to the requesting physician, as the images would be available externally to the multidisciplinary teams who may not be familiar with this modality. Final diagnosis: Left frontal meningioma detected on 68Gallium-PSMA PET/CT. Differential diagnosis: Spurious activity due to contamination of the skin with mis-registration, mis-registered activity from an occult skull metastasis from prostate cancer and brain metastasis from prostate cancer.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Michael Courtney https://orcid.org/0000-0002-9790-6401
Afshin Nasoodi https://orcid.org/0000-0002-1762-6830
Consent to participate/consent for publication
The requirement to obtain informed consent was waived according to institutional guidelines.
References
- 1.Siegel R, Ma J, Zou Z, et al. Cancer statistics, 2014. CA Cancer J Clin 2014; 64:9–29. [DOI] [PubMed] [Google Scholar]
- 2.Center MM, Jemal A, Lortet-Tieulent J, et al. International variation in prostate cancer incidence and mortality rates. Eur Urol 2012; 61:1079–1092. [DOI] [PubMed] [Google Scholar]
- 3.Uchio EM, Aslan M, Wells CK, et al. Impact of biochemical recurrence in prostate cancer among US veterans. Arch Intern Med 2010; 170:1390–1395. [DOI] [PubMed] [Google Scholar]
- 4.Brassetti A, Lombardo R, Emiliozzi P, et al. Prostate-specific antigen density is a good predictor of upstaging and upgrading, according to the new grading system: the keys we are seeking may be already in our pocket. Urology 2018; 111:129–135. [DOI] [PubMed] [Google Scholar]
- 5.Roach PJ, Francis R, Emmett L, et al. The impact of 68Ga-PSMA PET/CT on management intent in prostate cancer: results of an Australian prospective multicenter study. J Nucl Med 2018; 59:82–88. [DOI] [PubMed] [Google Scholar]
- 6.Anger HO, Gottschalk A. Localization of brain tumors with the positron scintillation camera. J Nucl Med 1963; 4:326–330. [PubMed] [Google Scholar]
- 7.Afshar-Oromieh A, Malcher A, Eder M, et al. PET imaging with a [68Ga] gallium-labelled PSMA ligand for the diagnosis of prostate cancer: biodistribution in humans and first evaluation of tumour lesions. Eur J Nucl Med Mol Imaging 2013; 24:486–495. [DOI] [PubMed] [Google Scholar]
- 8.Maurer T, Eiber M, Schwaiger M, et al. Current use of PSMA-PET in prostate cancer management. Nat Rev Urol 2016; 13:226. [DOI] [PubMed] [Google Scholar]
- 9.El Hajj A, Yacoub B, Mansour M, et al. Diagnostic performance of Gallium-68 prostate-specific membrane antigen positron emission tomography-computed tomography in intermediate and high risk prostate cancer. Medicine 2019; 98:e17491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krampla W, Newrkla S, Pfisterer W, et al. Frequency and risk factors for meningioma in clinically healthy 75-year-old patients: results of the Transdanube Ageing Study (VITA). Cancer 2004; 100:1208–1212. [DOI] [PubMed] [Google Scholar]
- 11.Wiemels J, Wrensch M, Claus EB. Epidemiology and etiology of meningioma. J Neurooncol 2010; 99:307–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mettler F, Guiberteau M. Essentials of nuclear medicine and molecular imaging 7th ed Philadelphia, PA: Elsevier, 2019. [Google Scholar]
- 13.de Galiza Barbosa F, Queiroz MA, Nunes RF, et al. Nonprostatic diseases on PSMA PET imaging: a spectrum of benign and malignant findings. Cancer Imag 2020; 20: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]