Abstract
Introduction
The coronavirus disease (COVID‐19) pandemic has continued to have a devastating impact on health worldwide. There has been a rapid evolution of evidence, establishing an increased risk of morbidity and mortality associated with diabetes and concurrent COVID‐19. The objective of this review is to explore the current evidence for inpatient assessment and management of diabetes during the COVID‐19 pandemic and highlight areas requiring further exploration.
Methods
A literature search of databases was conducted to November 2020 using variations on keywords SARS‐CoV‐2, COVID‐19, SARS, MERS and diabetes. Information relating to the impact of diabetes on severity of COVID‐19 infection, the impact of COVID‐19 infection on diabetes management and diabetes‐related complications was integrated to create a narrative review.
Discussion
People with diabetes and COVID‐19 are at an increased risk of morbidity and mortality. It is important that people with both known and previously unrecognised diabetes and COVID‐19 be promptly identified and assessed during acute illness, with close monitoring for clinical deterioration or complications. People with diabetes may require titration or alteration of their glycaemic management due to the potential for worse outcomes with hyperglycaemia and COVID‐19 infection. Comprehensive discharge planning is vital to optimise ongoing glycaemic management.
Conclusion
Further understanding of the risk of adverse outcomes and optimisation of glycaemic management for people with diabetes during COVID‐19 is required to improve outcomes. Increased glucose and ketone monitoring, substitution of insulin for some oral anti‐hyperglycaemic medications and careful monitoring for complications of diabetes such as diabetic ketoacidosis should be considered.
Keywords: coronavirus disease, severe acute respiratory syndrome coronavirus 2, diabetes
Novelty statement.
People with diabetes have an increased risk of morbidity and mortality due to COVID‐19.
Comprehensive assessment is required for people with diabetes on admission to hospital to assess for disease severity and the presence of complications of diabetes.
It is vital that people with undiagnosed diabetes be identified when unwell with COVID‐19.
Further research is required to optimise the management of COVID‐19 in people with diabetes during hospital admissions.
Evidence for the impact of COVID‐19 will require ongoing evaluation during the pandemic.
1. INTRODUCTION
Following the identification of initial cases in Wuhan, China in December 2019, the severe acute respiratory syndrome corona virus 2 (SARS‐CoV‐2) has continued to spread world‐wide, with coronavirus disease (COVID‐19) declared a pandemic on 11 March 2020. 1
In all, 62,844,837 people had tested positive for COVID‐19 with 1,465,144 deaths internationally as of the 1st of December. 2 While the majority of cases have mild symptoms, a proportion of cases progress to severe disease, leading to acute respiratory distress syndrome (ARDS), multiple organ dysfunction syndrome (MODS) and death. 3 , 4 There is evidence that people with diabetes and other co‐morbidities are at an increased risk of being severely affected by COVID‐19. 5 , 6 At present, there is evolving evidence for glycaemic management in people with diabetes and COVID‐19.
It is estimated that 463 million adults have diabetes globally 7 ; therefore, a significant proportion of the population may be at higher risk of adverse outcomes due to COVID‐19. While the underlying pathophysiology of this increased risk is yet to be fully determined, contributing factors may include increased inflammation, predisposition to severe infection and worsening of co‐morbidities. Current data predominately pertain to observational studies, with evidence from randomised control studies lacking, yet being necessary. It is important that assessment and management of people with diabetes in the hospital setting be optimised at this time to mitigate risk. For people with diabetes and confirmed or suspected COVID‐19, this involves close monitoring to rapidly identify and prevent deterioration, in conjunction with continued close glycaemic management to prevent acute complications such as diabetic ketoacidosis (DKA), hyperosmolar hyperglycaemic state (HHS) or hypoglycaemic episodes. This may require titration of individual's current medication dosages, cessation of some medications or transition to alternate therapies in unwell individuals. More specifically, the role of hyperglycaemia in increasing risk of severe COVID‐19 in people with diabetes, as well as in‐hospital glucose management and its role in mitigating any potential risk, requires further investigation.
The aim of this review is to summarise the current information regarding COVID‐19, its impact on people with diabetes and to provide suggestions for hospital assessment management of people with diabetes with COVID‐19.
2. METHODS
A search of PubMed was conducted using variations on keywords SARS‐CoV‐2, COVID‐19, severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS) and diabetes to November 2020. This was supplemented with hand searching of reference lists, relevant medical society media releases and expert opinion pieces. Given the rapidly changing nature of evidence related to COVID‐19, searches were run repeatedly to ensure emerging information was included. Information relating to the impact of diabetes on severity of COVID‐19 infection, morbidity and mortality, the impact of COVID‐19 infection on management of diabetes and diabetes‐related complications was integrated to create a narrative review.
3. COVID‐19
SARS‐CoV‐2 is an enveloped single‐strand positive‐sense RNA virus believed to have originated from a zoonotic source. 4 It enters human cells through binding of the coronavirus spike protein receptor binding domains with angiotensin‐converting enzyme (ACE2), a cell surface receptor 8 (Figure 1). Entry to the body is via the pulmonary system, with ACE2 expressed in a variety of organs, including the lungs, heart, kidney and intestine. 9 Two other coronaviruses, severe acute respiratory syndrome coronavirus (SARS‐CoV) and Middle East respiratory syndrome coronavirus (MERS‐CoV), have caused similarly severe respiratory symptoms in humans while other coronaviruses only cause common cold symptoms. 10 Coronaviruses have a high frequency of recombination events, leading to unpredictable changes in virulence secondary to a high genetic diversity. 10 Sustained human to human transmission is believed to occur primarily via respiratory droplets or aerosols through direct contact and contaminated surfaces. 3 , 11 , 12
FIGURE 1.
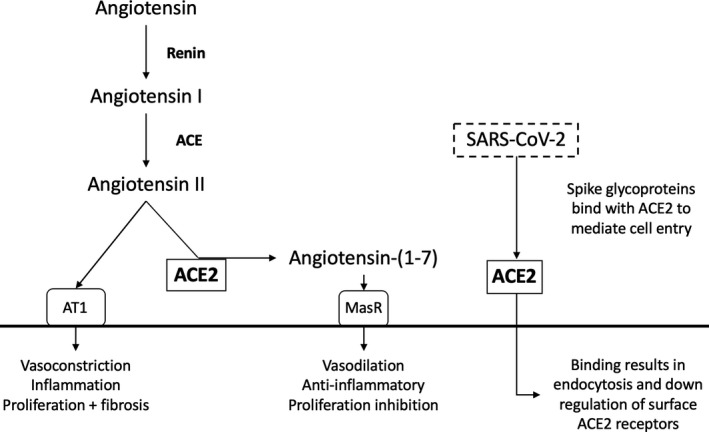
ACE2 and its role in the renin angiotensin system and SARS‐CoV‐2 infection. ACE2 is located on cell membranes and mediates entry of SARS‐COV‐2 through binding to spike glycoproteins resulting in endocytosis. This leads to downregulation of ACE2, which is required for cleaving of angiotensin II into angiotensin‐(1‐7) which exerts anti‐inflammatory vasoprotective effects. Angiotensin converting enzyme (ACE), angiotensin converting enzyme inhibitor (ACEi), angiotensin converting enzyme 2 (ACE2), AT1 angiotensin II receptor type 1 (AT1), Mas receptor (MasR)
SARS‐CoV‐2 infections range from asymptomatic to mild to severe. Common symptoms are fever, cough, dyspnoea and myalgias. Rhinorrhoea, anosmia, ageusia, diarrhoea, nausea and vomiting, and headaches are less commonly experienced symptoms. 3 , 13 , 14 People may also present atypically with cerebrovascular accidents, 15 cardiac presentations including myocarditis 16 and dermatologic presentations. 17 In a meta‐analysis, median incubation was reported as 5.8 days with a median of 5.1 days. 18 It has been estimated that the majority of symptomatic presentations are mild (81%), with approximately 14% severe and 5% critically unwell. 3 However, asymptomatic presentations have also been identified. 3 Older people and those with medical co‐morbidities are more likely to have severe disease and require ICU admission. 3 , 14 , 19 , 20 , 21 However, severe cases do occur in young and otherwise well people. 3 The case fatality rate of COVID‐19 has been estimated to be 1.38%, 22 lower than both SARS and MERS. 3 , 19 This is constantly changing in different countries, possibly reflecting healthcare resources, 25 spatial distancing measures, testing 23 and the demographics of affected individuals—in particular, age. 23
Assessment of people with COVID‐19 involves clinical examination, radiological investigation and biochemical as well as definitive diagnosis through reverse transcription polymerase chain reaction (RT‐PCR) testing. Radiographic findings are common, with bilateral areas of consolidation seen on CT in a majority of people. 9 , 24 Lymphopaenia, leukopaenia, elevated d‐dimer, elevated alanine aminotransferase (ALT) and aspartate aminotransferase (AST) have been observed in people with COVID‐19. 20 People with severe disease can have increased levels of pro‐inflammatory cytokines including tumour necrosis factor (TNF)‐alpha and interleukin (IL)‐6 and IL‐8. 25
There is also evidence to suggest that the severity of lymphopaenia correlates with disease severity, with the most pronounced lymphopaenia seen in non‐survivors. 20 Interestingly, a retrospective study of people with type 2 diabetes and COVID‐19 demonstrated lower minimal lymphocyte count compared to people with COVID‐19 but without diabetes (p = 0.001) and earlier occurrence of the minimal lymphocyte count (p = 0.042). 26 Overactivation of CD4+ and CD8+ T cells has been reported, 9 , 25 with decreased levels of CD4+ and CD8+ as well as absolute T lymphocytes in severe cases 9 , 24 potentially due to functional exhaustion. 27 Furthermore, infiltration of the lungs by inflammatory cells, with prominent lymphocyte involvement, has been reported in people with severe COVID. 28 This may lead to disease progression as a result of overall lowered circulating T‐cell activity. 27
Additionally, COVID‐19 leads to ACE2 protein down‐regulation, possibly through binding to the SARS‐CoV spike protein 29 (Figure 2). Viral replication in ACE2 containing organs, and the subsequent epithelial and endothelial cell apoptosis, creates a systemic response by releasing pro‐inflammatory cytokines, potentially leading to multi‐organ dysfunction. 9 , 30 Down‐regulation of pulmonary ACE2 function may enhance vascular permeability, resulting in increased lung oedema and leading to further respiratory compromise by precipitating ARDS. 9 , 30 ACE2 expression on islet cells of the pancreas may also lead to direct viral injury, and possible hyperglycaemia due to hypoinsulinaemia in people with COVID‐19 similar to findings in SARS. 31 However, as all organs containing ACE2 are not equally represented in COVID‐19 clinical presentations, involvement of other mechanisms in this process is likely and requires further exploration. 32
FIGURE 2.
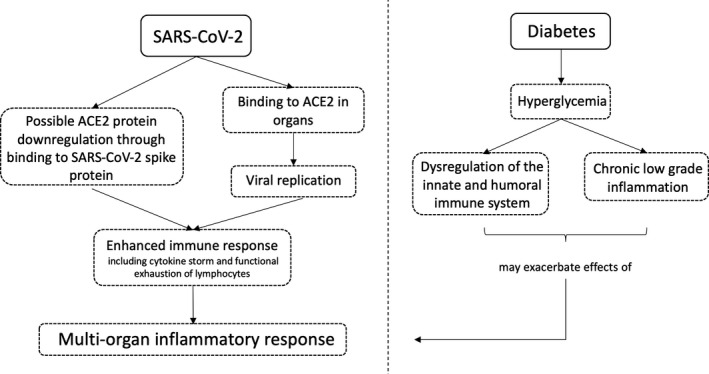
The potential interplay of SARS‐CoV‐2 and diabetes. SARS‐CoV‐2 is characterized by a local and systemic immune response mediated by virus entry to cells via ACE2 (angiotensin converting enzyme 2) leading to multi‐organ inflammation. This response may be exacerbated by hyperglycaemia in patients with diabetes, affecting both the immune system and the inflammatory response
3.1. COVID‐19‐related morbidity and mortality in people with diabetes
There is increasing evidence suggesting that co‐morbidities elevate the risk of morbidity and mortality related to COVID‐19. Cohort studies have indicated people with diabetes are more likely to present with severe infection and require more intensive management, including the need for respiratory support and admission to intensive care units (ICU). 6 , 21 , 33 , 34 A meta‐analysis of 13 Chinese studies showed that people with diabetes were over‐represented in the critically ill population (OR = 3.68; 95% CI (2.68, 5.03); p < 0.00001). 35 An analysis of data from 7,162 people in the United States showed 10.9% of all cases had diabetes. 36 However, 32% of ICU admissions and 24% of hospitalised non‐ICU admissions had diabetes. 36 People with COVID‐19 and diabetes also have higher mortality rates. 37 , 38 In an analysis of 44,672 participants, the Chinese Centre for Disease Control mortality rate was reported at 7.3% in people with diabetes compared to 2.3% in the whole population, 3 with a further Chinese meta‐analysis also finding a significant association between diabetes and mortality (relative risk (RR) 2.12 (1.44, 3.11); p < 0.001; I 2: 72%, p < 0.001). 39 In Italy, of 355 deaths from COVID‐19 reviewed, 35.5% had diabetes, 23 with an estimated total community population prevalence of diabetes of 20.3%. 40
Assessment of prevalence of diabetes among people with COVID has shown no definitive increase in the risk of contracting COVID‐19 in people with diabetes. In addition to evidence from the United States and Italy above, a meta‐analysis of Chinese participants demonstrated a prevalence of 10.3% of diabetes in the COVID‐19 population, compared to an estimated nationwide prevalence of diabetes in China of 10.9%. 40 At present, there is minimal delineation in the evidence base between type I and type II diabetes 41 ; however, an analysis of cases of COVID‐19 in England demonstrated higher mortality in both people with type 1 diabetes (2.86 times more likely to die in hospital; 95% CI: 2.58–3.18) and type 2 diabetes (1.80 times more likely to die in hospital; 95% CI 1.75–1.86) compared to people without diabetes. 42 However, data in children with diabetes have demonstrated no significantly increased risk of hospitalisation consistent with evidence from the general population. 43 Ongoing analysis is required to further clarify factors contributing to the higher risk of mortality and morbidity in adults with type 1 and type 2 diabetes and potentially an even higher risk in people with type 1 diabetes compared to type 2.
The pathophysiology underlying the greater risk of severe infection and death from COVID‐19 in people with diabetes is not yet fully understood. Diabetes mellitus is characterised by a chronic low‐grade inflammatory state with alterations in glucose and lipid metabolism and the development of diabetes‐related complications comprising retinopathy, nephropathy, neuropathy and cardiovascular disease. 44 Overall, people with diabetes are at an increased risk of infections compared to the general population, 45 and pneumonia is one of the leading causes of death in people with diabetes. 46
Hyperglycaemia is associated with dysregulation of the innate and humoral immune system with impaired neutrophil chemotaxis, phagocytosis and bactericidal activity, respiratory burst capacity, complement fixation and opsonisation of microorganisms, and altered chemokine production (Figure 1). 44 , 47 Multiple observational studies have shown a strong relationship between hyperglycaemia and adverse outcomes from COVID‐19; however, there is a lack of randomised control evidence. In people with long‐term hyperglycaemia, a large English cohort study of people with type 2 diabetes in England has shown that there was an association between people with higher mortality rates and raised glycated haemoglobin (HbA1c). 48 Participants with a HbA1c of ≥59 mmol/mol (7.6%) had significantly higher mortality compared to those with a HbA1c of 48–53 mmol/mol (6.5–7%). 48 This risk also increased with greater HbA1c, with the highest risk seen in participants with a HbA1c ≥86 mmol/L (10%) (HR 1.61; 1.47–1.77, p < 0.0001). 48 Similar findings were demonstrated in people with type 1 diabetes, with higher mortality also related to HbA1c of ≥86 mmol/L (10%) (HR 2.23; 95% CI: 1.50–3.30, p < 0.0001). 48 In more acute settings, Zhu et al found inpatient plasma glucose levels more than 10 mmol/L were associated with increased prevalence of ARDS (hazard ratio (HR) 0.41; 95% CI: 0.25–0.66; p < 0.001), acute heart injury (HR 0.21; 95% CI: 0.07–0.59; p = 0.003) and all‐cause mortality (HR 0.13; 95% CI: 0.04–0.44; p < 0.001) from SARS‐CoV‐2 compared to the well‐managed type 2 diabetes mellitus group (blood glucose <10 mmol/L). 49 In people presenting with moderate COVID‐19, those with hyperglycaemia >7.7 mmol/L on admission have demonstrated a significantly greater risk of progression to pneumonia (p < 0.01), elevated inflammatory markers with raised IL‐6 and d‐dimer (p < 0.001) and composite end point (admission to ICU, use of mechanical ventilation or death) (p < 0.01). 50 Recent evidence also suggests improved glycometabolic management during hospitalisation is associated with better outcomes (S51). 50 Moreover, similar findings were reported in SARS, with fasting hyperglycaemia in people with a known history of diabetes being significantly associated with death (odds ratio (OR) 3.3; 95% CI: 1.4–7.7; p = 0.006) (S52). However, differentiation between the effects of stress hyperglycaemia and hyperglycaemia secondary to diabetes must be considered as worse outcomes have also been identified in in people with uncontrolled stress hyperglycaemia without diabetes (S53). The roles of chronic versus acute elevated blood glucose may also require further demarcation. People with diabetes have previously been described as not having an increased risk of ARDS (S54, S55), suggesting further pathological mechanisms need to be considered as evidence evolves. Further analysis of acute and chronic hyperglycaemia is required to assess its pathophysiology and impact on COVID‐19 outcomes (S56).
The presence of other co‐morbidities in people with diabetes has also shown a significant increase in mortality rates, with increased body mass index (BMI), impaired renal function and previous admission to hospital for heart failure or cardiovascular disease including ischemic heart disease, peripheral artery disease and stroke identified as contributing conditions. 48 The role of these co‐morbidities as independent risk factors should be considered in conjunction with their combined impact to help establish the pathophysiology of this increased disease severity. Significantly higher BMI has been reported in people with severe illness and in non‐survivors with COVID‐19 independent of diabetes (S57, S58). It has been suggested that this may be due to impaired immune and metabolic responses in obesity, and an increased risk of poorer cardiovascular and cardiorenal outcomes (S57). Furthermore, obesity impairs respiratory function, decreasing functional capacity and diaphragmatic movement (S57), and is an independent predictor of respiratory failure (S58). Hypertension and cardiovascular disease (CVD), co‐morbidities commonly seen in people with diabetes, are among the most common co‐morbidities in people with COVID, and are also independently shown to increase the risk of severe disease (S59). Similar associations between co‐morbidities and worse outcomes were identified in SARS with heart disease (S60) and MERS with hypertension, ischaemic heart disease, congestive heart failure, end‐stage renal disease and chronic kidney disease (S61). Therefore, when assessing people with diabetes and COVID‐19, a holistic approach considering the acute infection, underlying co‐morbidities and glycaemia must be considered to optimise management and prognosis.
4. SUGGESTIONS FOR MANAGEMENT OF HOSPITAL INPATIENTS WITH DIABETES DURING THE COVID‐19 PANDEMIC
At present, there is minimal evidence for inpatient management of diabetes during the COVID‐19 pandemic. Current suggestions are largely the product of expert panels based on evidence from case studies, retrospective cohort studies, clinical experience and the pathophysiology of diabetes and known mechanism of action of current therapies. Integrated management involving medical, endocrinology and intensive care teams should be encouraged to facilitate holistic management of people with COVID‐19 and diabetes, particularly in severe disease with complications related to COVID‐19, underlying diabetes or other co‐morbidities.
4.1. Assessment of people with diabetes and COVID‐19 infection
Due to the risk of increased morbidity and mortality in people with diabetes and COVID‐19, these individuals should be promptly identified when presenting to hospital. People with diabetes should have their blood glucose level (BGL), HbA1c, ketones and venous blood gas (VBG) checked on admission to facilitate assessment of their glycaemic state and screen for complications of diabetes including DKA and HHS. There are reports of increased DKA presentations in people with COVID‐19 (S62, S63), as well as cases where presentations with DKA and COVID‐19 have revealed newly diagnosed diabetes (S64). While infection is a known precipitating factor of DKA in people with type I diabetes or people with type 2 diabetes taking sodium glucose cotransporter 2 inhibitors (SGLT2i) (S65), DKA can occur in all unwell people with diabetes and should still be considered at initial and subsequent assessment. In people who are well enough to be managed at home, sick day management plans should be provided including principles of ketone testing, adequate hydration, increased insulin dosing and withholding of oral medications if required (S66). If requiring admission to hospital, monitoring and management should be tailored to the severity of COVID‐19, current diabetes management plan and glycaemic variability.
Increased BGL monitoring during admission allows for optimisation of glycaemia management and prompt identification of hyperglycaemia, facilitating rapid investigation of any precipitating factor signifying clinical deterioration. Two to four hourly BGL monitoring has been recommended (S66, S67), with more frequent or continuous monitoring in critically unwell or hypoglycaemic people (S66). In a small cohort (n = 9) of people with COVID‐19 and diabetes who did not require intensive care, early use of continuous glucose monitoring (CGM) to decide corrective insulin coverage showed good correlation with a mean absolute relative difference (MARD) of 9.77% with no adverse events (S68). It has been suggested that CGM also be used in critically unwell people requiring ICU admission (S69, S70). For people with type 1 diabetes (S70) and potentially for those with type 2 diabetes admitted with COVID‐19 infections, use of flash glucose monitoring may be useful for frequent monitoring while minimising bedside care time (S71), as it has demonstrated high‐retest reliability and accuracy without the need for calibration and with reduced people contact (S70). Tighter glycaemia management has been suggested for younger people with no co‐morbidities, with more relaxed control targets for elderly people or those with co‐morbidities and a higher risk of hypoglycaemia (S72). An observational study has suggested glycaemic targets of 7.77–9.99 mmol/L (140–180 mg/dl) may improve outcomes while minimising the risk of hypoglycaemia. 50 However, factors should be considered on a case‐by‐case basis (S73, S74), and further evidence is required for specific ranges. Careful glucose management is especially important as intensive glucose control and hypoglycaemia are associated with an increased risk of mortality in critically ill people (S75, S76).
Monitoring of BGLs should be supplemented with ketone monitoring and monitoring of oral intake. There is some evidence to suggest that people with COVID‐19 and complications of diabetes may have a higher mortality rate, with a study of 174 participants demonstrating that those with diabetic ketoacidosis and infectious shock were more likely to die (p = 0.045) (S77). It has also been suggested COVID‐19 may drive ketosis (S78), and close clinical monitoring is encouraged (S79). Therefore, regular inpatient ketone monitoring may assist early identification and management of this potential trigger for deterioration. For unwell people with type 1 diabetes, capillary ketone testing may be considered with BGL testing. For people with type 2 diabetes and no history of ketosis, capillary ketones should be checked daily, if BGLs are >15 mmol/L or if signs of clinical deterioration are present. A VBG should be performed where ketones are elevated ≥1.5 mmol/L to assess for DKA and metabolic derangement. In addition to biochemical monitoring, oral intake should be recorded to allow for identification of dehydration and reduced carbohydrate intake to facilitate accurate medication titration (S80). People on insulin requiring enteral feeding in ICU also require close monitoring to prevent possible hypoglycaemic events if feeds are interrupted, as well as hyperglycaemia as insulin requirements change over the course of illness.
For perioperative individuals with diabetes and COVID‐19, the known link between hyperglycaemia and poor surgical outcomes means early communication between endocrinologists or experienced physicians, anaesthetists, and surgical teams should be encouraged to allow optimisation of glycaemic management. Pre‐operative testing of HbA1c in people with diabetes undergoing elective surgery has long been suggested to allow for optimisation prior to surgery (S81), and should continue during the pandemic as surgery resumes. It is currently unknown if COVID‐19 infection exacerbates intraoperative glycaemia levels. Recent studies have demonstrated postoperative pulmonary complications in 51.2% of 1,128 participants with perioperative SARS‐CoV‐2 and 30‐day mortality of 23.8% in people with COVID‐19 who have surgery (S82). However, diabetes was not significantly associated with 30‐day mortality or pulmonary complications (S82). Further research is required to determine if diabetes influences to peri‐operative outcomes in people with diabetes during the COVID‐19 pandemic.
4.2. Inpatient glycaemic management of people with diabetes and COVID‐19 infection
To optimise glycaemic management, medications may need to be altered while people are infected with and are recovering from COVID‐19. In a study of 174 inpatients in China, 37.5% of people transitioned from oral therapies to insulin during their admission and 29.2% were discharged with an increased insulin dose (S77). While the full impact of COVID‐19 on management of diabetes is still being determined, suggestions for optimising glycaemic management can be made based on the mechanism of medications and their known complications. Current recommendations suggest that medications which may cause volume depletion and hypoglycaemia should be avoided when unwell, medications with known risks associated with illness should be withheld in people with COVID‐19, and oral medication doses may need to be reduced (S80, S83). It should be noted that these suggestions are made on available evidence, with guidelines changing as further information comes to light. There is ongoing discussion regarding the potential benefits of some oral anti‐hyperglycaemic agents during COVID‐19 based on anti‐inflammatory properties; however, further evidence for their efficacy is required to allow for true evaluation of risk versus benefit.
In people with type 1 diabetes and COVID‐19, it is important that urgent endocrinology or experienced physician input be sought regarding medication titration. Insulin should be continued in people with type 1 diabetes throughout periods of acute illness (S67, S84). In people who are critically unwell, intravenous insulin infusions have been recommended (S71). For patients with moderate COVID‐19 not requiring ICU, people with hyperglycaemia (glucose >7.77 mmol/L) managed with a continuous insulin infusion aiming for BGL 7.77–9.99 mmol/L demonstrated a significantly reduced risk of a composite end point (admission to ICU, use of mechanical ventilation or death) (p < 0.01) and greater glucose reduction (p < 0.001). 50 Basal‐bolus regimens have also been suggested where oral medications are not suitable either due to adverse effects or insufficient impact, for those transitioning off intravenous insulin, or in people who were on pre‐existing basal‐bolus regimens (S85). When considering a basal‐bolus regimen for people with diabetes, it is important to ensure that there is adequate enteral nutrition or regular oral intake (S85). Oral anti‐hyperglycaemic medications, which may be utilised in patients/people with type 1 diabetes as an adjunct for cardiovascular or renal benefits, may need to be withheld during periods of acute illness as outlined below. These medications should be resumed once patients have recovered and have returned to normal oral intake. Regular monitoring of BGLs and ketones is required to assess adequacy of dosing regimens for people both on pump and injection insulin to facilitate appropriate titration (S67, S84). People with severe COVID‐19 and diabetes have been reported to have higher insulin requirements (S62), although further quantification of this relationship is needed.
In people with type 2 diabetes, oral anti‐hyperglycaemic medications should be reviewed on admission in terms of illness severity, acute glycaemic presentation, chronic glycaemic management, and factors that may precipitate medication‐related adverse events such as dehydration and decreased oral intake (Table 1). It has been suggested that metformin be ceased temporarily in people with dehydration due to a risk of lactic acidosis (S62, S66, S83, S86), although emerging evidence described in a recent meta‐analysis suggests metformin use may reduce mortality rates (RR 0.54; 95% CI: 0.32–0.90, p = 0.02, I 2 = 54%); however, further assessment of dose regimens and confounding factors is required (S87). It has also been suggested that renal function be monitored due to a risk of kidney injury (S62), particularly given the risk of kidney injury identified with COVID‐19. A similar recommendation has been made for sodium glucose cotransporter 2 inhibitors (SGLT2i, empagliflozin, dapagliflozin, canagliflozin, ertugliflozin) (S62, S66, S80, S83, S86) based on the small but significant risk of diabetic ketoacidosis in unwell people taking these medications (S65) and emerging reports in people with COVID‐19 (S88, S89). Sulphonylureas (gliclazide, glipizide, glibenclamide, tolbutamide, chlorpropamide) have been recommended to be ceased during acute illness with decreased oral intake due to a risk of hypoglycaemic events (S86). For glucagon‐like peptide (GLP)‐1 receptor agonists (liraglutide, dulaglutide, exenatide), close monitoring (S62) or temporary cessation (S66, S90) has been suggested during periods of decreased fluid intake due to the potential for renal injury with volume contraction (S91). Regarding resuming these medications, current guidelines suggest they be restarted when illness has resolved and when oral intake has normalised for 24–48 hours (S90). When medications are used in combination, individual components should be considered and continued if appropriate, with supplemental therapy as required. Given the potentially prolonged recovery time reported in some people with COVID‐19, regular clinical review and evaluation of medications are recommended to ascertain whether or not restarting is appropriate. In the interim, insulin has been suggested as the medication of choice in unwell people requiring hospital admission (S62, S83).
TABLE 1.
Summary of current suggestions for withholding oral anti‐hyperglycaemic medication in patients with diabetes and COVID‐19
| Medication | Suggested withholding in patients with COVID‐19 |
|---|---|
| Metformin | Temporarily withhold while unwell due to risk of lactic acidosis (S62, S66, S83, S86) |
|
SGLT2‐I empagliflozin, dapagliflozin, canagliflozin, ertugliflozin |
Temporarily withhold while unwell due to risk of diabetic ketoacidosis (S62, S66, S80, S83, S86) |
|
Sulphonylureas gliclazide, glipizide, glibenclamide, tolbutamide, chlorpropamide |
Temporarily withhold while unwell due to risk of hypoglycaemic events (S86) |
|
GLP‐1 receptor agonists liraglutide, dulaglutide, exenatide |
Continue with close monitoring (S62) OR temporarily withheld while unwell (S66, S90) due to risk of volume contraction |
|
DPP4i sitagliptin, vildagliptin, saxagliptin, linagliptin |
Consider withholding saxagliptin and alogliptin in critically unwell patients due to risk of exacerbated heart failure (S71). Continuation of DPP4i in mild disease may be considered (S62) |
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Dipeptidyl peptidase 4 inhibitors (sitagliptin, vildagliptin, saxagliptin, linagliptin) have been highlighted as a potential target for reducing inflammation in SARSCoV‐2 (S92). Dipeptidyl peptidase 4 enzymes exist as a Type 2 transmembrane glycoprotein and not only play a major role in glucose and insulin metabolism but also immune regulation and activation of T cells and up‐regulating pro‐inflammatory cytokines (S92). Human DPP4 has been shown to be a functional receptor for spike proteins in MERS‐COV (S93, S94) and hence its interest as a target has been revived during the COVID‐19 pandemic. However, it is important to note that in human studies, the use of DPP4 inhibitors (sitagliptin, vildagliptin, saxagliptin) did not prevent or reduce MERS‐CoV infection (S94). More importantly, there remains conflicting evidence on whether increase susceptibility to infections, particularly pneumonia, occurs with DPP4 inhibitors (S95, S96). One case control study has suggested that DPP4 inhibitors in addition to standard care may improve COVID‐19 infection in people with diabetes who present with pneumonia and hypoxia, with reduced mortality (18% vs. 37%; HR 0.44; 95% CI: 0.29–0.66; p = 0.0001), as well as need for mechanical ventilation (HR 0.27; CI: 0.11–0.62; p = 0.003) or intensive care (HR 0.51; CI 0.27–0.95; p = 0.03) compared to people receiving standard care alone (S51). However, this was a retrospective non‐randomised trial without blinding or use of a placebo‐control. An observational study demonstrated reduced mortality in those using DPP‐4 inhibitors compared to those using insulin at baseline; however, this study was limited by a small sample size and residual confounding (S97). It has been suggested that these medications may be continued (S62), although in critically unwell people withholding has also been suggested (S71).
Further discussion is also taking place around the role of ACEi and ARBs in people with COVID‐19. Despite initial concern that these medications may increase severity of COVID‐19 due to up‐regulation of the ACE2 receptor protein seen in animal models, emerging evidence suggests no adverse effects from their continued use (S98). While further research is conducted, current specialist guidelines state that these medications should be continued to prevent worsening of cardiovascular outcomes (S99).
4.3. Deterioration and complications of diabetes in patients with COVID‐19
At present, there is minimal evidence outlining definitive reasons for an increased risk of deterioration in people with diabetes and COVID‐19, although factors including a predisposition to secondary bacterial infection, higher risk of increased body mass and concurrent co‐morbidities including cardiovascular disease have been suggested (S62). To attempt to reduce this risk, markers of complications related to both COVID‐19 and to underlying diabetes should be closely monitored. Regarding COVID‐19 itself this includes monitoring clinically and biochemically for renal, cardiovascular, respiratory and thrombotic dysfunction. There may be an increased risk of hypercoagulable state in people with diabetes, with d‐dimer levels being significantly higher in this population (S77); however, further assessment of outcomes is required. Secondary bacterial infection is also a significant concern in people with diabetes. Regular monitoring of inflammatory markers such as ferritin, white cell and platelet counts, C‐reactive protein (CRP) and erythrocyte sedimentation rate (ESR) has been suggested (S62), particularly as people with increased derangement of these markers have shown a significantly increased risk of mortality. 33
With reports suggesting an increase in presentations for DKA and HHS during the COVID‐19 pandemic (S63), the impact of COVID‐19 on management of these complications of diabetes must be considered. When managing DKA and HHS, fluid resuscitation may carry a risk of precipitating ARDS and worsening damage to the lung parenchyma (S64, S80) due to increased vascular permeability caused by increased angiotensin II levels (S64). In people with confirmed or suspected COVID‐19, cautious fluid resuscitation has been suggested (S63), although at present there is minimal evidence describing outcomes related to fluid resuscitation. The use of subcutaneous insulin rather than intravenous insulin has also been suggested as a potential strategy for mild and moderate DKA to decrease bedside treatment time required for glucose monitoring and insulin titration (S100). Therefore, early identification and prompt management of hyperglycaemia and complications are important in preventing clinical deterioration with potential multi‐organ involvement. Reinforcement of home monitoring and sick day management plans is also vital for prevention of these complications (S100).
It is also very important to acknowledge that COVID‐19 may carry a risk of increased psychological distress for people with diabetes, both in terms of COVID‐19 infection itself and the negative impact of the infection the management of their diabetes (S80, S101). Ensuring adequate education regarding medication changes and clear planning of ongoing management may help alleviate diabetes‐specific psychological distress.
4.4. People with diabetes without COVID‐19
Preventative strategies for people living with diabetes must be utilised to avoid COVID‐19 exposure and infection in both the community and inpatient setting, and to reduce morbidity and mortality if they become infected (S62). These include appropriate preventative measures such as personal protective equipment (PPE) and hand hygiene practices (S56, S83) as well as limiting exposure to the hospital environment (S62). Early initiation of discharge planning (S90), including diabetes‐specific measures such as early referral to endocrinology for medication optimisation, may assist in timely discharge, minimising hospital exposure. Linking in with services such as diabetes nurse educators in the hospital setting and planning outpatient follow‐up may allow for improved glycaemic management on discharge and decreased readmission rates (S102, S103). As the pandemic continues, telehealth will continue to be a key method of healthcare delivery as it allows for engagement regardless of the level of COVID‐19 restrictions(S104); however, individual access to technology must be considered when planning for its implementation. The use of CGM may also help support individuals with diabetes in the community, providing real‐time data for medication titration (S104). In people who go on to develop complications of diabetes with unclear cause, it may be prudent to consider testing for COVID‐19 as there is emerging evidence that presentation with complications such as DKA may be the first indication of infection in otherwise minimally symptomatic people (S64).
4.5. People with unrecognised diabetes
It is estimated that up to one in two adults with diabetes are unrecognised globally. 7 Programmes such as the Diabetes Discovery programme established at Austin Health, whereby inpatients have routine HbA1c measurements ordered on admission using the electronic medical record, have allowed for identification of people with unrecognised diabetes and those with elevated HbA1c (S105). During this time, it is important these individuals are identified to allow for initiation of appropriate management and accurate risk evaluation during COVID‐19 (S106). Furthermore, new onset diabetes has also been reported in patients with COVID‐19 (S79, S107), although further evidence is required to determine if this is due to infection itself. Recent multicentre data from the UK has reported an apparent 80% increase in new onset type 1 diabetes in children during the pandemic (S108). It has been suggested that new onset diabetes may be due to alterations in glucose metabolism (S106) or to the expression of ACE2 receptors in the pancreas leading to cell damage due to COVID‐19 infection (S79).
There is emerging evidence of increased risk of mortality in people with unrecognised diabetes (fasting glucose ≥7 mmol/L and/or HbA1c ≥6.5%) and COVID‐19, with a study of 453 participants demonstrating an increased risk of mortality in newly diagnosed diabetes (HR 9.42; 95% CI: 2.18–40.7) than in known diabetes (HR 4.63; 95% CI: 1.02–21.0) compared to participants with normal glucose, independent of major cardiovascular risk factors (S109). Furthermore, a recent meta‐analysis showed a pooled proportion of 14.4% of people with COVID‐19 and diabetes who were hospitalised were newly diagnosed (S110), suggesting there is a sizeable population that needs to be urgently identified. Elevated HbA1c has previously been shown to be associated with worse renal outcomes where participants had multiple admissions (S111), and worse cardiovascular outcomes in high‐risk people (S112). As adverse outcomes in COVID‐19 have been associated with renal involvement (S113) and myocardial injury, 16 it is particularly important that all factors that may impact prognosis be identified and optimised while further study of the pathophysiology of COVID‐19 is undertaken. Diagnosis of underlying diabetes also allows for appropriate post‐admission care, including linking in with diabetes services, arranging follow‐up and education regarding diabetes, its complications and sick day management plans. This has the potential to improve short‐ and long‐term health outcomes for this population during the COVID‐19 pandemic.
4.6. Discharge planning and considerations for ongoing management for people with diabetes during the COVID‐19 pandemic
Disease management and monitoring beyond the acute hospital admission must also be considered for people with diabetes who have recovered from COVID‐19. Clear discharge planning involving all medical and nursing teams as well as the people and any caregivers should be undertaken early in admissions to ensure appropriate glycaemic management post‐discharge (S103). Close monitoring 4 weeks post‐admission has been suggested for people with COVID‐19 and diabetes (S73, S80). Early follow‐up via telehealth where appropriate and linking in with community diabetes services including diabetes nurse educators, primary care physicians and endocrinologists should ideally be included in discharge plans. In the longer term, it is unknown what the ongoing implications of COVID‐19 will be for people with diabetes, both in terms of organ dysfunction related to the diabetes itself and glycaemic management. Ongoing education and adaptation of management strategies may be necessary for people with diabetes as new evidence comes to light.
5. CONCLUSION
People with diabetes are at an increased risk of more severe COVID‐19 presentations and have a higher risk of mortality. As the pandemic continues to evolve, it is crucial that people with diabetes be identified when presenting to hospital to ensure prompt and appropriate assessment as well as management of their diabetes and relevant co‐morbidities (Table 2). During acute illness, people with diabetes require increased glycaemic monitoring due to the risk of deterioration and potentially increased risk of complications of diabetes including DKA and HHS. Hyperglycaemia during inpatient admission has been associated with poorer outcomes and increased mortality. Currently, there is limited evidence to support particular management strategies for people with diabetes during COVID‐19, with further research required. Physicians must therefore remain aware of emerging evidence, in particular from randomised control trials that may alter existing guidelines and influence ongoing management strategies in hospital and the community. Further research is required to assess the long‐term impacts of COVID‐19 on people with diabetes and its complications in terms of both glycaemic management and COVID‐19‐related sequelae.
TABLE 2.
Key learning points
| People with diabetes are at increased risk of severe disease and worse outcomes due to COVID‐19 |
| Strict PPE use and hand hygiene must be encouraged |
| Monitoring of BGLs and ketones should be increased in unwell people with diabetes and COVID‐19 in hospital |
| People with diabetes and COVID‐19 must be closely monitored for signs of clinical deterioration |
| In people presenting with complications of diabetes (DKA/HHS) of unclear cause, consider testing for COVID‐19 |
| People admitted with COVID‐19 infection should have HbA1c tested to ensure patients with undiagnosed diabetes are identified and appropriate glycaemic management is initiated |
| In people with diabetes and COVID‐19 admitted to hospital, consider withholding most oral hypoglycaemic agents and commencing insulin as required |
| Review sick day management plans and community care arrangements prior to discharge |
| Ensure follow‐up is arranged post‐discharge, particularly where medication changes have been made to ensure medications are restarted when appropriate |
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
Supporting information
Supplementary Material
REFERENCES
- 1. WHO Director‐General's opening remarks at the media briefing on COVID‐19 ‐ 11 March 2020: World Health Organisation; 2020.
- 2. WHO Coronavirus Disease (COVID‐19) Dashboard. World Health Organisation; 2020.
- 3. Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID‐19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239‐1242. [DOI] [PubMed] [Google Scholar]
- 4. Zhu NA, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727‐733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Li BO, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID‐19 in China. Clin Res Cardiol. 2020;109(5):531‐538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934‐943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Diabetes atlas: international diabetes federation 2019, 9th. https://www.diabetesatlas.org/en/ [PubMed]
- 8. Chowdhury R, Maranas CD. Biophysical characterization of the SARS‐CoV2 spike protein binding with the ACE2 receptor explains increased COVID‐19 pathogenesis. bioRxiv. 2020;2020.03.30.015891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jin Y, Yang H, Ji W, et al. Virology, epidemiology, pathogenesis, and control of COVID‐19. Viruses. 2020;12(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Su S, Wong G, Shi W, et al. Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol. 2016;24(6):490‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID‐19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wilson N, Corbett S, Tovey E. Airborne transmission of covid‐19. BMJ. 2020;370:m3206. [DOI] [PubMed] [Google Scholar]
- 13. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Guan W‐J, Ni Z‐Y, Hu YU, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683‐690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID‐19). JAMA Cardiol. 2020;5(7):1‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sachdeva M, Gianotti R, Shah M, et al. Cutaneous manifestations of COVID‐19: report of three cases and a review of literature. J Dermatol Sci. 2020;98(2):75‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McAloon C, Collins Á, Hunt K, et al. Incubation period of COVID‐19: a rapid systematic review and meta‐analysis of observational research. BMJ Open. 2020;10(8):e039652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Li L‐Q, Huang T, Wang Y‐Q, et al. COVID‐19 patients’ clinical characteristics, discharge rate, and fatality rate of meta‐analysis. J Med Virol. 2020;92(6):577‐583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS‐CoV‐2 pneumonia in Wuhan, China: a single‐centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475‐481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wang D, Hu BO, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061‐1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model‐based analysis. Lancet Infect Dis. 2020;20(6):669‐677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Onder G, Rezza G, Brusaferro S. Case‐fatality rate and characteristics of patients dying in relation to COVID‐19 in Italy. JAMA. 2020;323(18):1175‐1176. [DOI] [PubMed] [Google Scholar]
- 24. Chen G, Wu DI, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130(5):2620‐2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Yuki K, Fujiogi M, Koutsogiannaki S. COVID‐19 pathophysiology: a review. Clin Immunol. 2020;215:108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wu D, Gao S. Analysis of the lymphocyte count in type 2 diabetic patients with coronavirus disease (COVID‐19): A retrospective study in a centralized treatment center. Diabetes Res Clin Pract. 2020;166:108340 10.1016/j.diabres.2020.108340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zheng M, Gao Y, Wang G, et al. Functional exhaustion of antiviral lymphocytes in COVID‐19 patients. Cell Mol Immunol. 2020;17(5):533‐535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID‐19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420‐422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kuba K, Imai Y, Rao S, et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus–induced lung injury. Nat Med. 2005;11(8):875‐879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fu Y, Cheng Y, Wu Y. Understanding SARS‐CoV‐2‐mediated inflammatory responses: from mechanisms to potential therapeutic tools. Virol Sin. 2020;35(3):266‐271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Somasundaram NP, Ranathunga I, Ratnasamy V, et al. The impact of SARS‐Cov‐2 virus infection on the endocrine system. J Endocr Soc. 2020;4(8):bvaa082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bourgonje AR, Abdulle AE, Timens W, et al. Angiotensin‐converting enzyme‐2 (ACE2), SARS‐CoV‐2 and pathophysiology of coronavirus disease 2019 (COVID‐19). J Pathol. 2020;251:228‐248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yan Y, Yang Y, Wang F, et al. Clinical characteristics and outcomes of patients with severe covid‐19 with diabetes. BMJ Open Diabetes Res Care. 2020;8(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic features and clinical course of patients infected with SARS‐CoV‐2 in Singapore. JAMA. 2020;323(15):1488‐1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID‐19 cases: a systematic literature review and meta‐analysis. J Infect. 2020;81(2):e16‐e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019 — United States. February 12–March 28, 2020. Centre for Disease Control; 2020. [DOI] [PMC free article] [PubMed]
- 37. Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID‐19) implicate special control measures. J Med Virol. 2020;92(6):568‐576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Huang I, Lim MA, Pranata R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID‐19 pneumonia – a systematic review, meta‐analysis, and meta‐regression. Diabetes Metab Syndr. 2020;14(4):395‐403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Fadini GP, Morieri ML, Longato E, Avogaro A. Prevalence and impact of diabetes among people infected with SARS‐CoV‐2. J Endocrinol Invest. 2020;43(6):867‐869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Gentile S, Strollo F, Ceriello A. COVID‐19 infection in Italian people with diabetes: Lessons learned for our future (an experience to be used). Diabetes Res Clin Pract. 2020;162:108137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Barron E, Bakhai C, Kar P, et al. Associations of type 1 and type 2 diabetes with COVID‐19‐related mortality in England: a whole‐population study. Lancet Diabetes Endocrinol. 2020;S2213–8587(20):30272‐30282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cardona‐Hernandez R, Cherubini V, Iafusco D, Schiaffini R, Luo X, Maahs DM. Children and youth with diabetes are not at increased risk for hospitalization due to COVID‐19. Pediatr Diabetes. 2020;Epub; ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Berbudi A, Rahmadika N, Tjahjadi AI, Ruslami R. Type 2 diabetes and its impact on the immune system. Curr Diabetes Rev. 2020;16(5):442‐449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Carey IM, Critchley JA, DeWilde S, Harris T, Hosking FJ, Cook DG. Risk of infection in type 1 and type 2 diabetes compared with the general population: a matched cohort study. Diabetes Care. 2018;41(3):513‐521. [DOI] [PubMed] [Google Scholar]
- 46. Wu H, Lau ESH, Ma RCW, et al. Secular trends in all‐cause and cause‐specific mortality rates in people with diabetes in Hong Kong, 2001–2016: a retrospective cohort study. Diabetologia. 2020;63(4):757‐766. [DOI] [PubMed] [Google Scholar]
- 47. Jafar N, Edriss H, Nugent K. The effect of short‐term hyperglycemia on the innate immune system. Am J Med Sci. 2016;351(2):201‐211. [DOI] [PubMed] [Google Scholar]
- 48. Holman N, Knighton P, Kar P, et al. Risk factors for COVID‐19‐related mortality in people with type 1 and type 2 diabetes in England: a population‐based cohort study. Lancet Diabetes Endocrinol. 2020;8(10):823‐833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Zhu L, She Z‐G, Cheng XU, et al. Association of blood glucose control and outcomes in patients with COVID‐19 and pre‐existing type 2 diabetes. Cell Metab. 2020;31(6):1068‐1077.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sardu C, D’Onofrio N, Balestrieri ML, et al. Outcomes in patients with hyperglycemia affected by COVID‐19: can we do more on glycemic control? Diabetes Care. 2020;43(7):1408‐1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


