Summary
The clinical severity, rapid transmission and human losses due to coronavirus disease 2019 (Covid‐19) have led the World Health Organization to declare it a pandemic. Traditional epidemiological tools are being significantly complemented by recent innovations especially using artificial intelligence (AI) and machine learning. AI‐based model systems could improve pattern recognition of disease spread in populations and predictions of outbreaks in different geographical locations. A variable and a minimal amount of data are available for the signs and symptoms of Covid‐19, allowing a composite of maximum likelihood algorithms to be employed to enhance the accuracy of disease diagnosis and to identify potential drugs. AI‐based forecasting and predictions are expected to complement traditional approaches by helping public health officials to select better response and preparedness measures against Covid‐19 cases. AI‐based approaches have helped address the key issues but a significant impact on the global healthcare industry is yet to be achieved. The capability of AI to address the challenges may make it a key player in the operation of healthcare systems in future. Here, we present an overview of the prospective applications of the AI model systems in healthcare settings during the ongoing Covid‐19 pandemic.
Keywords: artificial intelligence, covid‐19, epidemiology, diagnosis, SARS‐CoV‐2, therapeutic developments
Abbreviations
- AI
artificial intelligence
- ARDS
acute respiratory distress syndrome
- ARIMA
autoregressive integrated moving average
- ARIS
artificial immune recognition system
- BiPathCNN
Bi‐path convolutional neural networks
- CNN
convolutional neural network
- CRF
conditional random field
- CoV
coronavirus
- Covid‐19
coronavirus disease 2019
- Covid‐19 SMS
covid‐19 smart management system
- DT
decision trees
- GARCH
generalized autoregressive conditional heteroscedasticity
- GISAID, Global Initiative on Sharing Avian Influenza Data; GPS, global positioning system; GRSVs
Google relative search volumes
- GT
Google trends
- hsCRP
high‐sensitivity C‐reactive protein
- ICT
information and communication technologies
- ICU
intensive care unit
- IDVI
Infectious Disease Vulnerability Index
- IoT
internet of things
- JAK
Janus kinase
- LDA
linear discriminant analysis
- LDH
lactic dehydrogenase
- LR
logistic regression
- MERS
Middle East respiratory syndrome
- Mpro
main protease
- ML
machine learning
- NB
Naive Bayes
- NEC
NEC OncoImmunity AS bioinformatics company
- NLP
natural language processing
- ODEs
ordinary differential equations
- RdRp
RNA‐dependent RNA polymerase
- RF
random forest
- RNNs
recurrent neural networks
- R0
reproduction number
- SARS
severe acute respiratory syndrome
- SARS‐CoV‐2
severe acute respiratory syndrome‐coronavirus‐2
- SVM
support vector machines
- SVR
support vector regression
- VHP
virus host prediction
- WHO
World Health Organization
1. INTRODUCTION
Recent progress in healthcare and medicine has increased the accumulation of an extensive background data of patients and their related medications. During the 20th century, researchers developed and proposed many advanced medical support systems to diagnose diseases. 1 Advancement of knowledge led to the development of mathematical tools that helped scientists improve understanding of the nature of pathogens, identify potential drug targets, predict epidemics based on the available digital data, and benefited healthcare professionals in better control of diseases. Among all the analytical tools, artificial intelligence (AI) based model systems are projected as the most promising. 2 Some AI‐based approaches that emerged during the 1970s assisted in the interpretation of diseases, 3 electrocardiography, 4 the choice of an appropriate treatment 5 and helped clinicians generate hypotheses about complex diseases. 6 , 7 AI‐based technologies summarize the personal health data of patients and use it to create a knowledge dataset that facilitates clinicians in making decisions and charting a personalized care routine for patients. Primarily, the AI‐based technologies in the field of healthcare examine the effects of disease treatments, disease prevention and ultimately, their relative outcome for patients. Several approaches based on machine learning (ML), convolutionary and deep neural networks and Bayesian networks are implemented to assist in healthcare improvements with the help of intelligent computing systems. Currently, progress in information and communication technologies has led to an enormous increase in the amount of data obtained from public health surveillance. AI‐based tools along with reliable disease management platforms have the potential to create an avenue for a robust analysis, enabling stakeholders to respond effectively to an infectious disease outbreak. 8 , 9
Previously, confirming the diagnosis in tuberculosis was a tedious and time‐consuming process that hampered its control globally. Currently, an early detection system has been achieved to a fair extent using an AI‐based tool, artificial immune recognition system (ARIS). Likewise, ARIS has paved the way for AI‐assisted diagnosis in several other difficult infections. 10 Another example of AI utilization in human healthcare is its successful implementation in the accurate diagnosis of malaria. It is a simple automated system that circumvents the complex processing and staining protocols, thus serves clinicians in minimizing potential errors. 11 , 12
AI‐based technologies have also been effectively implemented in the epidemiology of infectious diseases such as Kyasanur forest disease, 13 Middle East respiratory syndrome (MERS), 14 Chikungunya, 15 Zika 16 , 17 and Ebola. 18 Several research groups demonstrated the successful prediction of infectious diseases by implementing AI through autoregressive integrated moving average (ARIMA). 19 , 20 , 21 AI algorithms on prediction of genome and protein ultra‐structures of successive generations of viruses may have an immense value in preparedness against possible viral infections 22 ; such algorithms when applied to datasets from Newcastle disease virus in China and South Korea, could predict mutated nucleotides with a 70% accuracy. 23 The data generated on a daily basis through the internet of things along with classical datasets, can help us better understand the dynamics of infectious diseases, their progression, response to treatment and transmission if used cautiously.
AI‐driven strategies in the crisis arising from infectious diseases are generally characterized by a poor quality of data and lack of immediate response. In such cases, composites of maximum likelihood approaches are used to address the issues such as small sample size or missing information. The proven maximum likelihood algorithms designed and tested for other infectious diseases following a similar set of natural history in the past can be very useful in predictions and decision‐making. 18 This strategy worked well during severe acute respiratory syndrome (SARS) outbreak to ensure a quick response to public health needs. The previous experiences have acted as a major source of information during the decision‐making for new global public health threat named Covid‐19. 24 The Covid‐19 smart management system utilized the data from sources such as credit cards, security camera records, global positioning system data from cars, or cell phones to effectively trace the movement of individuals with Covid‐19 and their contacts in South Korea. 25 AI‐based technologies are helping better understand the transmission pattern of severe acute respiratory syndrome‐coronavirus‐2 (SARS‐CoV‐2), assisting in development of novel diagnostics and effective therapeutic approaches, 26 proposing candidate drug molecules by screening millions of compounds, fostering vaccines in a time efficient and reliable manner. AI‐based technologies also help to identify the most susceptible individuals based on their personalized genetic, physiological and biochemical profiles. 27 , 28 Applications of AI‐based approaches that could assist as key components of the Covid‐19 pandemic are presented in Figure 1 and Table 1.
FIGURE 1.
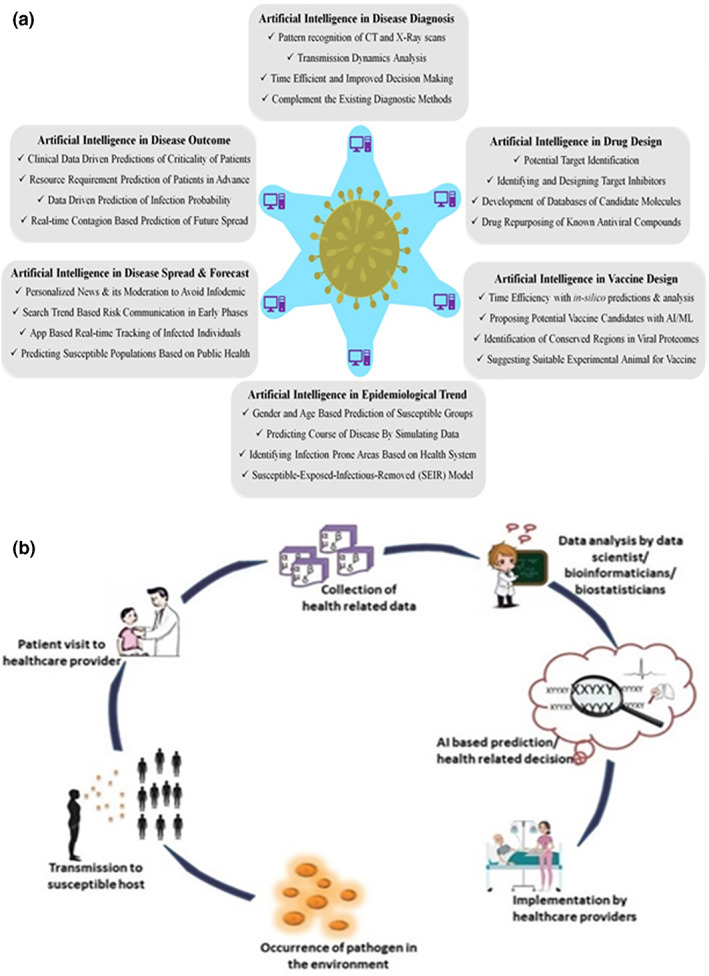
The scope of implementation of AI‐based approaches in infectious diseases: (a) AI‐based applications in infectious disease management including diagnosis, epidemiology, modelling, prediction, pathogen characterization, prevention, control and development of vaccines and therapeutics. (b) Control stages of infectious diseases from the emergence of infection in the environment until the implementation of the AI‐based predictions and decisions by healthcare providers; AI, Artificial Intelligence; CT, computed tomography
TABLE 1.
Applications of artificial intelligence in healthcare and biomedical field
| Research | Detection | Prevention | Clinical development | Response | Recovery |
|---|---|---|---|---|---|
|
|
|
|
|
|
Abbreviation: GPS, global positioning system.
Covid‐19 pandemic is a major global challenge 29 , 30 to public health along with devastating social, economic and political impacts. The daily increase in the number of infected cases combined with a high death rate is likely to be a repetition of the Spanish flu pandemic in 1918. Therefore, countries are striving to restrict the spread of the virus by conducting regular testing among the public, carrying out contact tracing, imposing lockdowns, limiting travel, quarantining citizens and maintaining physical distancing. The World Health Organization (WHO) declared the disease a Public Health Emergency of International Concern (PHEIC) on 30 January, 2020 and later a pandemic on 11 March 2020. The WHO is working continuously to analyse data, provide guidelines coordinate with partners and help countries prepare to fight against this pandemic by increasing supplies and managing expert networks. Researchers are also working tirelessly to develop more efficient and robust diagnostic techniques using advanced technologies such as CRISPR‐Cas, therapeutic drugs and vaccines.
SARS‐CoV‐2, the current global health threat, has infected more than 70 million people across the world and 1.6 million reported deaths (WHO Weekly epidemiological update, 15 December 2020) ‐ statistics were updated on 09 January 2021 after first online publication). This virus belongs to the genus Betacoronavirus under family Coronaviridae and subfamily Orthocoronavirinae. Other important genera under Coronaviridae family are Alphacoronavirus, Gammacoronavirus and Deltacoronavirus. CoVs are positive sense, enveloped, single‐stranded RNA viruses. The complete virion size varies between 80 and 220 nm in diameter, with several 20 nm long crown‐like spikes protruding from a host‐derived lipid envelope, which gives the virus resemblance of radiation (Latin: corona) of sun under the electron microscopy, hence specified its name coronavirus. It carries 26–30 kb genome which currently the largest among known pathogenic RNA viruses. Since the identification of SARS‐CoV‐2 as the cause of atypical pneumonia in December 2019 in Wuhan, China, speculations are emerging on its origin from bats or wildlife animal hosts like pangolins.
Considering the Covid‐19 situation, worldwide research laboratories and firms are developing rapid detection kits. Among these test kits being developed, a rapid intelligent technique, where the transmission dynamics of the disease spread can be assessed in real‐time is of the utmost need. Therefore, AI‐based tools are being evaluated and used in preliminary screening of SARS‐CoV‐2 infected individuals. Through the AI‐based learning frameworks, individuals are being screened for any eventual infections leading to their categorizations as low, moderate, or high risk individuals. 31 , 32 , 33 Recently, the AI and ML algorithm have been used to identify SARS‐CoV‐2 specific intrinsic genomic signatures for a rapid, scalable and highly accurate phylogenetic analysis of the virus. 33 During the course of the current pandemic, the AI tools may contribute significantly in better understanding the nature of the etiological virus (SARS‐CoV‐2), designing vaccines, identifying therapeutic targets, diagnosis of the disease and predicting new outbreaks spots based on the available digital data. 34
1.1. Covid‐19 datasets
The availability of sufficient amount of high‐quality data is crucial for a successful implementation of AI in the management of Covid‐19. Several online resources have been created to provide a free online access to different types of data related to Covid‐19 35 . The Center for Systems Science and Engineering at Johns Hopkins University created one of the most extensive datasets, named as ‘2019 Novel Coronavirus Visual Dashboard’, providing information related to the real‐time number of infected, recovered and deceased individuals on daily basis in addition to demographic data and data related to incidence and hospitalization rate. 36 Likewise, there are databases like Covid‐19 image database which contain computed tomography (CT) scan and X‐ray radiographic data from large number of Covid‐19 and non‐Covid‐19 patients that may foster the development of AI‐based tools for differential diagnosis of Covid‐19. 37 One of the climatic factors related dataset provided by Havard Dataverse (https://dataverse.harvard.edu) contains information on humidity, temperature and air quality in Covid‐19 affected areas in China since January 2020, 38 while another resource, WorldPop (https://www.worldpop.org), provides demographic datasets of South America, Asia and Africa. 39 These datasets may have unstructured data including noise, therefore, the software provider, C3.ai, compiled and structured the data from different sources to create a ‘C3 AI. Covid‐19 Data Lake’ which contains ready to analyse data on Covid‐19. (C3.ai, C3.ai releases COVID-19 data lake v2. C3.ai. https://c3.ai/c3-ai-releases-covid-19-data-lake-v2)
1.2. Covid‐19 and AI
AI‐based approaches are being implemented in the diagnosis of Covid‐19. Some of the AI‐based tools have demonstrated to perform efficient classification of the level of severity of Covid‐19 by using radiographic images such as X‐ray and CT‐scans. 35 , 40 For the diagnosis of Covid‐19, supervised learning algorithms such as convolutional neural network (CNN), linear discriminant analysis, Naive Bayes, support vector machines, decision trees, logistic regression and random forest are being used. 35 , 40 These algorithms use different datasets to classify the images in multiple groups which help determine the level of disease severity and also differentiate Covid‐19 from other similar diseases characterized by similar symptoms and pneumonia.
1.3. AI in anti‐SARS‐CoV‐2 drug design
Scientists across the world are working on the design and development of therapeutic molecules against the potential targets of SARS‐CoV‐2. The main protease (Mpro) and RNA‐dependent RNA polymerase (RdRp) are the most potent protein targets and inhibition of these viral proteins would substantially limit virus replication. Some of the AI‐based approaches demonstrated their potential in identifying putative targets and proposed small molecule protease inhibitors. For instance, a recent study reported implementation of deep neural network‐based models for de novo design of Mpro protease inhibitors and identified thirty‐one natural product based compounds. Two of these inhibitors displayed significant similarities with a plant product, aurantiamide, which may be used for Covid‐19 treatment. 41 Another study reported some novel non‐covalent inhibitors of Mpro that were designed using generative deep learning approaches as potential drugs for treating Covid‐19 patients. 35 Furthermore, a molecular docking study of 1903 approved drugs against Mpro to select six drugs, viz. eszopiclone, perampanel, nelfinavir, pitavastatin, praziquantel and zopiclone, based on shape similarity analysis and docking scores. Nelfinavir was further selected as a potential drug candidate based on binding free energy calculation. 35 In another computational screening performed on clinically approved medicines, 36 ten drugs were identified to form hydrogen bonds with critical residues within the binding pocket of Mpro protease of SARS‐CoV‐2 and may have a higher tolerance to resistance mutations. However, these AI based findings need to be validated using in vitro studies first and then in vivo studies to prove that the AI based binding is significant. Thus, AI could help select few molecules out of thousands to be further tested for developing into a therapeutic drug. Following selection, the traditional drug development approaches need to be followed to determine the safety and efficacy.
One ML database, consisting of data on already known drugs with antiviral action against known viruses, coupled with a second one, containing known 3‐chymotrypsin‐like protease (3CLpro) inhibitors, predicted marketed drugs with potential for use against SARS‐CoV‐2. 37 In another study on drug repurposing, rapid sequencing of SARS‐CoV‐2 viral genome along with molecular modelling suggested the effectiveness of available antiviral treatment such as the combination of anti‐HIV lopinavir and ritonavir. Baricitinib, an inhibitor of Janus kinase (JAK)‐1 and JAK‐2 38 which is clinically approved for the treatment of rheumatoid arthritis in adults, has been predicted to reduce the ability of SARS CoV‐2 to infect lung cells. 39 Based on the plasma concentration of baricitinib, which is sufficient to inhibit JAK‐1, the drug is expected to resist viral entry and reduce inflammation in Covid‐19 patients. 42 All such studies used AI or machine learning based methods directly or indirectly at different stages of computer aided drug designing.
1.4. AI in SARS‐CoV‐2 vaccine design
The vaccine development strategies against the pathogenic human CoVs including SARS and MERS have targeted either the whole virus or its structural proteins nucleoprotein (N), spike protein (S) or membrane protein (M). AI and machine learning based approach may play a critical role in vaccine design by contributing to the entire process using in silico‐based analysis, prediction and validation. 40 , 43 AI‐based approaches have been implemented to predict the blueprints to design SARS‐CoV‐2 specific broad‐spectrum T‐cell epitope‐based vaccine. A comprehensive epitope mapping was generated by profiling the viral proteome across the frequently occurring HLA alleles in human population using NEC OncoImmunity AS (http://www.oncoimmunity.com) bioinformatics company Immune Profiler suite of tools. An optimal collection of epitope hotspots from the conserved region of viral proteome was identified that could assist in vaccine formulation, thus providing maximum coverage across the global population. 44 , 45 Use of reverse vaccinology tools to analyse the SARS‐CoV‐2 proteome predicted its six proteins (S protein and five non‐structural proteins‐nsp3, 3CL‐pro and nsp8, nsp9, and nsp10) to be adhesins, that are important for virus attachment and host cell entry. 46 In‐silico approaches identified a chimeric protein which could simultaneously elicit both humoural and cell‐mediated immune responses. 40 AI can also be used to identify immunodominant conformational peptides containing B‐cell epitopes to design a vaccine that could induce neutralizing antibody. Further advances in AI‐based approaches could mitigate the Covid‐19 pandemic and similar upcoming infectious disease threats by enhancing the arsenal of immunoprophylactic agents against virus threats.
1.5. AI in disease diagnosis
Chest CT based diagnosis is the fastest approach to clinically diagnose Covid‐19 in suspected patients within certain limitations. A recent study implemented a deep learning based model for Covid‐19 to differentiate between community‐acquired pneumonia and Covid‐19 separately. 34 , 47 With a paucity of point‐of‐care diagnosis, the transmission dynamics of SARS‐CoV‐2 among different population groups and the risk of disease spread may be complemented with AI driven tools. Currently, the active learning process in AI devices is reported to increase confidence during the decision making processes. 48 Thus, protocols must be standardized for development of AI‐based devices which may be used in the event of such disasters. Deep learning methods using chest CT and X‐ray images are complementary in the diagnosis of Covid‐19 positive cases. 34 , 49 , 50 , 51 , 52 According to recent reports, chest CT of Covid‐19 patients revealed typical radiographic features such as multifocal patchy consolidation, ground‐glass opacities and/or interstitial changes with peripheral distribution. 53 A CNN‐based approach was able to distinguish between influenza A and Covid‐19 infected pneumonic lungs with an overall accuracy of 86.7%. 54 A transfer learning approach to design a CNN‐based model to perform disease diagnosis from the chest anterior‐posterior radiographs of patients could predict with 96.3% accuracy with a high sensitivity and specificity. 55 A meta‐analysis review on published research with independent dataset on CT scan and other imaging techniques for diagnosis of Covid‐19 showed excellent prediction accuracy. 54
Apart from clinical signs‐based diagnosis, the present diagnostic approach for Covid‐19 which uses real‐time reverse‐transcriptase polymerase chain reaction (rRT‐PCR), is more reliable. However, this diagnostic tool is analytically sensitive enough to detect the viral nucleic acid in the samples but the sample quality, time of sample collection and laboratory errors may primarily affect the rRT‐PCR test accuracy. A false negative rate of up to 20% was reported in rRT‐PCR. 47 , 56 It is also observed that some initial false‐negative rRT‐PCR results, when complemented by AI‐based deep learning computer‐aided diagnostic system, were later confirmed positive. 48 Thus, a more reliable diagnosis of Covid‐19 can be achieved by complementary combined AI‐based approaches, such as the application of CT derived deep leaning methods along with rRT‐PCR. As interpretation of the lung CT assisted by the deep learning‐based method through computer‐aided diagnostic system, which is pre‐trained with a large number of the CT scans of Covid‐19 patients, could enhance the accuracy of diagnosis and cover events missed by the use of rRT‐PCR alone.
The use of AI‐based algorithms, that integrate chest CT findings with laboratory testing, clinical symptoms and exposure history are as sensitive as radiological disease diagnosis. 34 Many researchers have developed AI coupled radiological image findings to distinguish between infected and non‐infected individuals. 57 Another study implemented robust 2D and 3D deep learning models for automated detection and patient monitoring. The deep learning CT image analysis including a set of 157 international patients showed an accurate measurement of disease progression with 98.2% sensitivity and 92.2% specificity. It was also demonstrated that a high accuracy in the diagnosis of Covid‐19 could be achieved in a time efficient manner when complemented with AI‐based image analysis. 58 A comprehensive machine learning was used to design a CRISPR‐based nucleic acid detection of SARS‐CoV‐2 and symptomatically related pathogens that could be used for diagnostic and surveillance purposes. 59 The CRISPR‐Cas13 detection system was experimentally tested based on lateral‐flow assay to demonstrate its speed and sensitivity using synthetic targets. 59 Therefore, AI approaches that can go hand‐in‐hand with the existing molecular diagnostic procedures could help in diagnosis and assist in early control of disease spread. AI‐based tools can impart swiftness in the healthcare set up amidst the Covid‐19 pandemic crisis through AI/ML algorithms, which are well‐tested and verified in several disease outbreaks.
1.6. AI in prediction of Covid‐19 pandemic outcomes
Hitherto studies are conducted to increase the clinical skills for the identification and progression of Covid‐19. 60 An AI framework having predictive analytics capabilities was built and applied to clinical data to provide support to clinical decision making. The predictive models could learn from previous health‐related data of Covid‐19 patients to predict which patient will develop severe symptoms that is, acute respiratory distress syndrome or who will require intensive care unit facility. The most predictive clinical features included elevated alanine aminotransferases, body aches and high haemoglobin levels. The predictive models could achieve up to 80% accuracy in predicting severe cases.
In yet another study, the effect of Covid‐19 pandemic was predicted by implementing recurrent neural networks on publicly available data from the WHO and the Johns Hopkins University. The results indicated that errors between validated and predicted data as compared to the actual corresponding trends were low. The study concluded that repeated peaks are anticipated on the epidemic curve of Covid‐19 which is a propagated source epidemic. 61
A machine learning‐based prognostic model with clinical data from Tongji hospital, in Wuhan in China predicted the survival of critically ill Covid‐19 patients with almost 90% accuracy using three parameters that is, lactic dehydrogenase, lymphocyte count and high‐sensitivity C‐reactive protein out of more than 300 clinical and laboratory features. 62
1.7. AI in predicting the spread and management of Covid‐19
Addressing issues like the global viral outbreaks is often considered to be of national and global interest. Increased data sharing is a foremost necessity to better understand the pandemics and to develop highly efficient AI‐based model systems. A recent study analysed Google trends (GT), particularly to understand the popular search terminologies concerning the Covid‐19 outbreak in the Taiwanese population. 60 The results reveal that GT could be instrumental in predicting the exact time to react concerning risk communication among the public. In a study conducted in six cities in Taiwan based on Covid‐19 searches, a high to moderate correlation was found between Google relative search volumes and Covid‐19 cases. The findings based on Google activities preceded an increase in Covid‐19 cases. 60 A suitable risk communication plan will help in avoiding the threat of infodemic and hoax calls.
Covid‐19, with a basic reproduction number (R0) was reported as exceeding 2.0, making it highly infectious to an immunological naive population. 63 The early phase risk communication could be the most important way of curtailing the spread on a global basis. This could help create awareness not only among public health officials and scientists but also among the public about the events occurring at ground zero of the outbreak. The efforts for effective development and use of decision‐making AI algorithms in literature may help in searching for the scientists/researchers as well as the medical staff attending the cases, who can seek assistance from such platforms. 64 The ML‐based algorithms, for improving the identifications of infected cases through mobile phone‐based web surveys, may support in reducing spread among susceptible populations. 32
BlueDot report using an AI algorithm on global ticketing data from airlines released first warning about the Covid‐19 outbreak as early as of December 31, 2019. 65 A conditional random field model based on the location of key symptomatic individuals and affected patients in NewYork, USA used geographical location linked to social media user updates to assess the spread of infection. 66 Similar models could be exploited for larger areas to prevent a global spread of infection. A natural language processing and methods based on AI along with unstructured patient data collected through Tele‐conversations could be used for predicting the positive results and subsequently prioritizing the testing of such cases. 67
The international travel pattern was assessed from Wuhan, China, to anticipate the pattern of disease spread across different countries. 68 The Infectious Disease Vulnerability Index (IDVI) scores on the basis of metrics such as disease dynamics, demographic, public health, political (domestic or international), healthcare and economics were reported for countries receiving a large number of passengers from Wuhan. Countries are given IDVI scores between 0 and 1 with higher scores reflecting a better ability to respond to a disease outbreak. The study revealed that among the countries receiving a significant number of passengers from Tokyo (Japan), Wuhan (China), Hong Kong, Bangkok (Thailand), Taipei (Taiwan), Dubai (UAE), Sydney (Australia) and Victoria (Canada) had high IDVI scores. Further, a similar study evaluated the vulnerability and preparedness (based on IDVI) of African countries for Covid‐19. 65
1.8. AI in determination of epidemiological trend
Epidemiological data are required to develop intervention strategies and create necessary awareness about Covid‐19 outbreaks. In this context, a population‐level observational study was performed based on various national and international news reports on Covid‐19. 69 A list of SARS‐CoV‐2 infected patients along with national and international counts between 13 and 31 January, 2020 were compiled. The trend of Covid‐19 epidemiology and its progression across China were assessed, and it was shown that the median age of infected individuals was 46 years and most were male. Furthermore, the age‐related data of Chinese patients confirmed that the infection rate among children was not significant. It was also reported that the time gap between symptom onset and reporting by the patient to a hospital were longer in Hubei province than in other parts of China and the rest of the world.
Prophet (an additive regression model developed by Facebook), an ARIMA model, and a Holt‐Winters Exponential Smoothing model combined with Generalized Autoregressive Conditional Heteroscedasticity were developed for online forecasting of Covid‐19 every 24 h which can further help develop containment strategy of Covid‐19. 70 The AI‐based technologies may also contribute to detecting clusters of cases and predicting the future course of the disease spread through modelling in a city, state and country by analysing all previous data collected during the course of Covid‐19 pandemic. 71
1.9. AI in disease forecasting
AI‐based models are not just limited to assistance in addressing the disease spread when it originates but could play a significant role in forecasting a disease outbreak even before it has started. Multi‐model and integrated ensembles are being used to forecast influenza season to improve public health response. 72 With the emergence of previously unknown CoVs in different animal host species and humans, the prediction of infectivity and the host species are of the utmost importance. The machine learning based support vector regression (SVR) has been used as a forecast model for dengue by using the data generated from dengue surveillance, meteorological data and internet query information. The R‐squared value of SVR model ranged from 0.976 to 0.997, giving it utility to predict future outbreaks. 73 Among such models, Virus Host Prediction (VHP) model implemented bi‐path convolutional neural networks by using the viral sequences available online to predict potential host of 50 different coronaviruses. 74 Currently, the epidemiological data on human CoVs generated by different laboratories all over the world are made available at Global Initiative on Sharing Avian Influenza Data (GISIAD, https://www.gisaid.org). Recently, the dynamics of Covid‐19 outbreak at local levels were analysed by coupled system of ordinary differential equations (ODEs), 75 wherein it is observed that the effects of diagnostic tests and preventive measures such as social and physical distancing and quarantine were estimated by a basic reproductive number, R0 and predicting the total number of infected cases and related deaths in Wuhan in China were predicted with a high level of accuracy. Similar forecasts were also done in Turkey having different levels of diagnostic testing and preventive measures. There is a need for AI, Cytomics or multi‐OMICS based approaches for the development of rapid and easy to use assays to distinguish between severe and mild cases and to identify the patients expected to become critically ill. 76 This would take some of the pressure off clinicians, hospitals and public healthcare system to manage the Covid‐19 pandemic through optimal utilization of resources.
1.10. Pitfalls of AI
The major limitations and challenges to success of AI‐based approaches include the nature of disease manifestation. The SARS‐CoV‐2 infection has varied manifestations ranging from asymptomatic to severe clinical disease, which may require huge and complex data, and pose difficulty in designing practical AI‐based algorithms. Similar constraints were reported while developing algorithms of prediction using line classifiers for MERS in the past. 77 , 78 The digital systems used to gather the data are unlikely to achieve the required uptake using the voluntary system without any incentives; a smart phone based application generated data can be suppressed to an extent of 80% as observed in a simulation study. 79 Apart from that, a compromise between autonomy and privacy for an uncertain public health benefit can only be put into use after a warranted pilot project on modelling with sufficient benefit at the cost of privacy. The present AI‐based algorithms in healthcare systems can offer a binary response to specific question about a disease in context, but may not give the alternative predictions, it would be hard and complicated to build such a comprehensive AI‐based algorithm for health monitoring. 80 Every stakeholder in healthcare system should really focus on how meaningful and deep data can be generated at each point in healthcare activity from disease surveillance to treatment to bring an all‐inclusive robust AI modality to the level where it fundamentally improves medicine. As huge volume of articles is being published on the Covid‐19, AI‐based bibliometric analysis could be used to improve our understanding and manage Covid‐19 in a better way. 81 The implementation of AI‐based approaches may not be accessible in resource limited countries where the disease may hit the population hard, therefore a call of AI‐based global health initiative is recommended.
2. CONCLUSIONS AND FUTURE PROSPECTS
AI‐based methods are useful in epidemiological modelling of the ongoing Covid‐19 pandemic, and to forecast the urgent need of healthcare infrastructure, medical supplies, human resource requirement in future when the disease spread, which could aid public health agencies in adopting timely prevention and control strategies. However, the accuracy of the AI based predictions is based on the input data and assumptions, we need to be aware that the real time situation may vary from the predictions. The AI‐based technologies and methods are helpful in improving disease diagnosis and could be explored to select the candidates for developing vaccines and drugs, understanding virus evolution and identifying potential drug candidates for repurposing against Covid‐19. AI plays an important role in healthcare industry as well as in public health. In this review, we highlighted the uses of AI‐based approaches in healthcare during the course of the Covid‐19 pandemic where AI‐based technologies and methods have been deployed in modelling the virus spread and optimal utilization of resources. Availability of huge amount of high‐quality data enriched with information may help the AI‐based approaches effectively study the complicated real‐life health related issues leading to a better management. Promising initial results have been obtained by researchers using AI‐based technology but the regulation around data exchange is the major hurdle in its implementation in real life. The AI‐based approaches have helped address the key issues but a significant impact on the global healthcare industry is yet to be achieved. The capability of AI to address the challenges may make it a key player in deciding the operation of healthcare systems in future.
It is agreed that AI‐based tools may not completely replace human brain in terms of observations made by virologists, epidemiologists or clinicians, however the value of AI will play a significant and complementary role by reducing the burden on each stakeholder. The decision makers at each level can have a few preferred choices suggested by AI tools, which can be further scrutinized with the help of human intelligence before taking final decision for having a control on the impacts of epidemic. In the disease epidemic situation, whether AI is being used solely or in conjunction with other tools, factors such as understanding epidemiological features, incubation period, transmissibility, risk populations, reproduction ratio (R0), mortality rate, natural history of the infection, ultra‐details of the pathogen, stability, virulence and pathogenic potentials are key for efficient public health response. It may be concluded that the AI‐based approaches can go hand‐in‐hand with existing conventional procedures which may encourage an early diagnosis, develop or repurpose drugs, design vaccines and assist in the early control of the spread of the disease. The AI‐based interventions are currently playing a key role in understanding the global progression of the Covid‐19 pandemic and it also helps make evidence‐based decision at each level starting from understanding the pathogen to suggesting effective prevention and control measures by epidemiological modelling. As the AI based modelling and other interventions will have profound implication on the decision making at national level, its accuracy needs to be assured.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
AUTHOR CONTRIBUTION STATEMENT
Yashpal Singh Malik, Shubhankar Sircar, Sudipta Bhat, Mohd Ikram Ansari and Tripti Pande involved in the conceptualization, design, interpretation of data and manuscript drafting. Prashant Kumar, Basavaraj Mathapati and Balasubramanian Ganesh involved in the collection of data on AI applications, manuscript drafting and reviewing. Rahul Kaushik, Senthilkumar Natesan, Sayeh Ezzikouri, Mohamed E. El Zowalaty and Kuldeep Dhama contributed to writing, revisions, editing, updating and approving the final version of the manuscript. Mohamed E. El Zowalaty and Yashpal Singh Malik contributed in critical revisions and editing the manuscript. All authors agree to be accountable for its contents.
ACKNOWLEDGMENTS
All the authors acknowledge and thank their respective Institutes and Universities. YSM thank the Education Division, Indian Council of Agricultural Research, New Delhi for the ICAR‐National Fellowship.
Malik YS, Sircar S, Bhat S, et al. How artificial intelligence may help the Covid‐19 pandemic: Pitfalls and lessons for the future. Rev Med Virol. 2021;31(5):e2205. doi: 10.1002/rmv.2205
[Correction added on 09 January 2021 after first online publication: References have been updated in this version]
Contributor Information
Yashpal Singh Malik, Email: malikyps@gmail.com.
Kuldeep Dhama, Email: kdhama@rediffmail.com.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in public domain resources.
REFERENCES
- 1. Miller RA. Medical diagnostic decision support systems—past, present, and future: a threaded bibliography and brief commentary. J Am Med Inf Assoc. 1994;1(1):8‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Makridakis S. The forthcoming artificial intelligence (AI) revolution: its impact on society and firms. Futures. 2017;90:46‐60. [Google Scholar]
- 3. Szolovits P, Patil RS, Schwartz WB. Artificial intelligence in medical diagnosis. Ann Intern Med. 1988;108(1):80‐87. [DOI] [PubMed] [Google Scholar]
- 4. Kundu M, Nasipuri M, Basu DK. Knowledge‐based ECG interpretation: a critical review. Pattern Recogn. 2000;33(3):351‐373. [Google Scholar]
- 5. De Dombal F, Leaper D, Staniland JR, McCann A, Horrocks JC. Computer‐aided diagnosis of acute abdominal pain. Br Med J. 1972;2(5804):9‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shortliffe EH, Davis R, Axline SG, Buchanan BG, Green CC, Cohen SN. Computer‐based consultations in clinical therapeutics: explanation and rule acquisition capabilities of the MYCIN system. Comput Biomed Res. 1975;8(4):303‐320. [DOI] [PubMed] [Google Scholar]
- 7. Barnett GO, Cimino JJ, Hupp JA, Hoffer EP. DXplain: an evolving diagnostic decision‐support system. J Am Med Assoc. 1987;258(1):67‐74. [DOI] [PubMed] [Google Scholar]
- 8. Wong ZS, Zhou J, Zhang Q. Artificial intelligence for infectious disease big data analytics. Infect Dis Health. 2019;24(1):44‐48. [DOI] [PubMed] [Google Scholar]
- 9. Xu J, Wickramarathne TL, Chawla NV. Representing higher‐order dependencies in networks. Sci Adv. 2016;2(5):e1600028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Saybani MR, Shamshirband S, Golzari S, et al. RAIRS2 a new expert system for diagnosing tuberculosis with real‐world tournament selection mechanism inside artificial immune recognition system. Med Biol Eng Comput. 2016;54(2‐3):385‐399. [DOI] [PubMed] [Google Scholar]
- 11. Go T, Kim JH, Byeon H, Lee SJ. Machine learning‐based in‐line holographic sensing of unstained malaria‐infected red blood cells. J Biophot. 2018;11(9):e201800101. [DOI] [PubMed] [Google Scholar]
- 12. Pillay E, Khodaiji S, Bezuidenhout BC, Litshie M, Coetzer TL. Evaluation of automated malaria diagnosis using the Sysmex XN‐30 analyser in a clinical setting. Malar J. 2019;18(1):1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Majumdar A, Debnath T, Sood SK, Baishnab KL. Kyasanur forest disease classification framework using novel extremal optimization tuned neural network in fog computing environment. J Med Syst. 2018;42(10):187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sandhu R, Sood SK, Kaur G. An intelligent system for predicting and preventing MERS‐CoV infection outbreak. J Supercomput. 2016;72(8):3033‐3056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sood SK, Mahajan I. Wearable IoT sensor based healthcare system for identifying and controlling chikungunya virus. Comput Ind. 2017;91:33‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sareen S, Gupta SK, Sood SK. An intelligent and secure system for predicting and preventing Zika virus outbreak using Fog computing. Enterp Inf Syst. 2017;11(9):1436‐1456. [Google Scholar]
- 17. Sareen S, Sood SK, Gupta SK. Secure internet of things‐based cloud framework to control zika virus outbreak. Int J Technol Assess Health Care. 2017;33(1):11. [DOI] [PubMed] [Google Scholar]
- 18. Colubri A, Silver T, Fradet T, Retzepi K, Fry B, Sabeti P. Transforming clinical data into actionable prognosis models: machine‐learning framework and field‐deployable app to predict outcome of Ebola patients. PLoS Negl Trop Dis. 2016;10(3):e0004549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yanchun P, Mingxia Z, Zhimin C, Ming Z, Zuoyao Z. An ARIMA based model for forecasting the patient number of epidemic disease. Paper presented at: 2016 13th International Conference on Service Systems and Service Management (ICSSSM) June 24‐26, 2016. Availabe at: https://ieeexplore.ieee.org/xpl/conhome/7527137/proceeding. 10.1109/ICSSSM.2016.7538560. [DOI] [Google Scholar]
- 20. Wei W, Jiang J, Liang H, et al. Application of a combined model with autoregressive integrated moving average (ARIMA) and generalized regression neural network (GRNN) in forecasting hepatitis incidence in Heng County, China. PLoS One. 2016;11(6):e0156768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Azeez A, Obaromi D, Odeyemi A, Ndege J, Muntabayi R. Seasonality and trend forecasting of tuberculosis prevalence data in Eastern Cape, South Africa, using a hybrid model. Int J Environ Res Publ Health. 2016;13(8):757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Park Y, Casey D, Joshi I, Zhu J, Cheng F. Emergence of new disease: how can artificial intelligence help? Trends Mol Med. 2020;26(7):627‐629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Salama MA, Hassanien AE, Mostafa A. The prediction of virus mutation using neural networks and rough set techniques. J Bioinform Syst Biol. 2016;2016(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McCall B. COVID‐19 and artificial intelligence: protecting health‐care workers and curbing the spread. Lancet Digit Health. 2020;2(4):e166‐e167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lin L, Hou Z. Combat COVID‐19 with artificial intelligence and big data. J Trav Med. 2020;27(5):taaa080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kim J, Zhang J, Cha Y, et al. Advanced bioinformatics rapidly identifies existing therapeutics for patients with coronavirus disease‐2019 (COVID‐19). J Transl Med. 2020;18(1):257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Alimadadi A, Aryal S, Manandhar I, Munroe PB, Joe B, Cheng X. Artificial intelligence and machine learning to fight COVID‐19. Physiol Genomics. 2020;52(4):200‐202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Adly AS, Adly MS. Can artificial intelligence and internet be the solution to prevent the exponential spread of COVID‐19? J Med Internet Res. 2020;22(8):e19104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chakraborty I, Maity P. COVID‐19 outbreak: migration, effects on society, global environment and prevention. Sci Total Environ. 2020;728:138882 2020/08/01/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nicola M, Alsafi Z, Sohrabi C, et al. The socio‐economic implications of the coronavirus pandemic (COVID‐19): a review. Int J Surg. 2020;78:185‐193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Albahri AS, Hamid RA, Alwan Jk, et al. Role of biological data mining and machine learning techniques in detecting and diagnosing the novel coronavirus (COVID‐19): a systematic review. J Med Syst. 2020;44(7):122 2020/05/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rao ASS, Vazquez JA. Identification of COVID‐19 can be quicker through artificial intelligence framework using a mobile phone–based survey when cities and towns are under quarantine. Infect Control Hosp Epidemiol. 2020;41(7):826‐830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Randhawa GS, Soltysiak MP, El Roz H, de Souza CP, Hill KA, Kari L. Machine learning using intrinsic genomic signatures for rapid classification of novel pathogens: COVID‐19 case study. PLoS One. 2020;15(4):e0232391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mei X, Lee H‐C, Diao K‐y, et al. Artificial intelligence–enabled rapid diagnosis of patients with COVID‐19. Nat Med. 2020;26:1224‐1228. 10.1038/s41591-020-0931-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Zhavoronkov A, Aladinskiy V, Zhebrak A, et al. Potential COVID‐2019 3C‐like protease inhibitors designed using generative deep learning approaches. ChemRxiv. 2020. 10.26434/chemrxiv.11829102.v2. [DOI] [Google Scholar]
- 36. Liu X, Wang X‐J. Potential inhibitors against 2019‐nCoV coronavirus M protease from clinically approved medicines. J Genet Genomics. 2020;47(2):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ke Y‐Y, Peng T‐T, Yeh T‐K, et al. Artificial intelligence approach fighting COVID‐19 with repurposing drugs. Biomed J. 2020;43(4):355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fridman JS, Scherle PA, Collins R, et al. Selective inhibition of JAK1 and JAK2 is efficacious in rodent models of arthritis: preclinical characterization of INCB028050. J Immunol. 2010;184(9):5298‐5307. [DOI] [PubMed] [Google Scholar]
- 39. Stebbing J, Krishnan V, de Bono S, et al. Mechanism of baricitinib supports artificial intelligence‐predicted testing in COVID‐19 patients. EMBO Mol Med. 2020;12:e12697. 10.15252/emmm.202012697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Enayatkhani M, Hasaniazad M, Faezi S, et al. Reverse vaccinology approach to design a novel multi‐epitope vaccine candidate against COVID‐19: an in silico study. J Biomol Struct Dyn. 2020:1‐16. 10.1080/07391102.2020.1756411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bung N, Krishnan SR, Bulusu G, Roy A. De novo design of new chemical entities (NCEs) for SARS‐CoV‐2 using artificial intelligence. ChemRxiv. 2020. 10.26434/chemrxiv.11998347.v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Richardson P, Griffin I, Tucker C, et al. Baricitinib as potential treatment for 2019‐nCoV acute respiratory disease. Lancet. 2020;395(10223):e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Zawawi A, Forman R, Smith H, et al. In silico design of a T‐cell epitope vaccine candidate for parasitic helminth infection. PLoS Pathog. 2020;16(3):e1008243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Malone B, Simovski B, Moliné C, et al. Artificial intelligence predicts the immunogenic landscape of SARS‐CoV‐2 leading to universal blueprints for vaccine designs. Sci Rep. 2020;10:22375. 10.1038/s41598-020-78758-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Senior AW, Evans R, Jumper J, et al. Improved protein structure prediction using potentials from deep learning. Nature. 2020;577(7792):706‐710. [DOI] [PubMed] [Google Scholar]
- 46. Ong E, Wong MU, Huffman A, He Y. COVID‐19 coronavirus vaccine design using reverse vaccinology and machine learning. Frontiers in Immunology. 2020;11:1581. 10.3389/fimmu.2020.01581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Li L, Qin L, Xu Z, et al. Artificial intelligence distinguishes COVID‐19 from community acquired pneumonia on chest CT. Radiology. 2020;0(0):200905. [Google Scholar]
- 48. Santosh K. AI‐driven tools for coronavirus outbreak: need of active learning and cross‐population train/test models on multitudinal/multimodal data. J Med Syst. 2020;44(5):1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chen J, Wu L, Zhang J, et al. Deep learning‐based model for detecting 2019 novel coronavirus pneumonia on high‐resolution computed tomography. Sci Rep. 2020; 10:19196. 10.1038/s41598-020-76282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sahlol AT, Yousri D, Ewees AA, et al. COVID‐19 image classification using deep features and fractional-order marine predators algorithm. Sci Rep 10, 15364. 2020. 10.1038/s41598-020-71294-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Jain R, Gupta M, Taneja S, Hemanth DJ. Deep learning based detection and analysis of COVID‐19 on chest X‐ray images. Applied Intelligence. 2020. 10.1007/s10489-020-01902-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Xu X, Jiang X, Ma C, Du P, Li X, Lv S, Yu L, Ni Q, Chen Y, Su J, Lang G. A. A deep learning system to screen novel coronavirus disease 2019 pneumonia. Engineering. 2020;6(10):1122–1129. 10.1016/j.eng.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Chung M, Bernheim A, Mei X, et al. CT imaging features of 2019 novel coronavirus (2019‐nCoV). Radiology. 2020;295(1):202‐207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ito R, Iwano S, Naganawa S. A review on the use of artificial Intelligence for medical Imaging of the lungs of patients with coronavirus disease 2019. Diagn Interven Radiol. 2020;26:443–448. 10.5152/dir.2019.20294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Vaid S, Kalantar R, Bhandari M. Deep learning COVID‐19 detection bias: accuracy through artificial intelligence. Int Orthop. 2020;44:1539–1542. 10.1007/s00264-020-04609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for typical 2019‐nCoV pneumonia: relationship to negative RT‐PCR testing. Radiology. 2020;0(0):200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ozturk T, Talo M, Yildirim EA, Baloglu UB, Yildirim O, Rajendra Acharya U. Automated detection of COVID‐19 cases using deep neural networks with X‐ray images. Comput Biol Med. 2020;121:103792 June. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Gozes O, Frid‐Adar M, Greenspan H, et al. Rapid AI development cycle for the coronavirus (COVID‐19) pandemic: Initial results for automated detection & patient monitoring using deep learning ct image analysis. arXiv. 2020. https://arxiv.org/abs/2003.05037v3. [Google Scholar]
- 59. Metsky HC, Freije CA, Kosoko‐Thoroddsen T‐SF, Sabeti PC, Myhrvold C. CRISPR‐based COVID‐19 surveillance using a genomically‐comprehensive machine learning approach. bioRxiv. 2020. 10.1101/2020.02.26.967026. [DOI] [Google Scholar]
- 60. Husnayain A, Fuad A, Su EC‐Y. Applications of Google Search Trends for risk communication in infectious disease management: a case study of the COVID‐19 outbreak in Taiwan. Int J Infect Dis. 2020;95:221‐223 2020/06/01/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kolozsvari LR, Berczes T, Hajdu A, et al. Predicting the epidemic curve of the coronavirus (SARS‐CoV‐2) disease (COVID‐19) using artificial intelligence. medRxiv. 2020. 10.1101/2020.04.17.20069666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Yan L, Zhang H‐T, Goncalves J, et al. A machine learning‐based model for survival prediction in patients with severe COVID‐19 infection. medRxiv. 2020. 10.1101/2020.02.27.20028027. [DOI] [Google Scholar]
- 63. Liu Y, Gayle AA, Wilder‐Smith A, Rocklöv J. The reproductive number of COVID‐19 is higher compared to SARS coronavirus. J Trav Med. 2020;27(2):taaa021. 10.1093/jtm/taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Rada G, Verdugo‐Paiva F, Ávila C, et al. Evidence synthesis relevant to COVID‐19: a protocol for multiple systematic reviews and overviews of systematic reviews. Medwave. 2020;20(3). [DOI] [PubMed] [Google Scholar]
- 65. Gilbert M, Pullano G, Pinotti F, et al. Preparedness and vulnerability of African countries against importations of COVID‐19: a modelling study. The Lancet. 2020;395(10227):871–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Sadilek A, Kautz H, Silenzio V. Predicting disease transmission from geo‐tagged micro‐blog data. In: AAAI'12: Proceedings of the Twenty‐Sixth AAAI Conference on Artificial Intelligence. (12th), AI Access Foundation; 2012:136–142. [Google Scholar]
- 67. Obeid JS, Davis M, Turner M, Meystre SM, Heider PM, Lenert LA. An AI approach to COVID‐19 infection risk assessment in virtual visits: a case report. J Am Med Inf Assoc. 2020;27(8):1321–1325. 10.1093/jamia/ocaa105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Bogoch II, Watts A, Thomas‐Bachli A, Huber C, Kraemer MU, Khan K. Pneumonia of unknown aetiology in Wuhan, China: potential for international spread via commercial air travel. J Trav Med. 2020;27(2):taaa008. 10.1093/jtm/taaa008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Sun K, Chen J, Viboud C. Early epidemiological analysis of the coronavirus disease 2019 outbreak based on crowdsourced data: a population‐level observational study. Lancet Digital Health. 2020;2(4):e201‐e208. 2020/04/01/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Abdulmajeed K, Adeleke M, Popoola L. Online forecasting of COVID‐19 cases in Nigeria using limited data. Data Brief. 2020;30:105683 2020/06/01/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Vaishya R, Javaid M, Khan I, Haleem A. Artificial intelligence (AI) applications for COVID‐19 pandemic. Diabetes & metabolic syndrome. Clin Res Rev. 2020;14(4):337‐339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Reich NG, McGowan CJ, Yamana TK, et al. Accuracy of real‐time multi‐model ensemble forecasts for seasonal influenza in the U.S. PLoS Comput Biol. 2019;15(11):e1007486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Guo P, Liu T, Zhang Q, et al. Developing a dengue forecast model using machine learning: a case study in China. PLoS Negl. Trop. Dis. 2017;11(10):e0005973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Guo Q, Li M, Wang C, et al. Host and Infectivity prediction of Wuhan 2019 novel coronavirus using deep learning algorithm. bioRxiv. 2020. 10.1101/2020.01.21.914044. [DOI] [Google Scholar]
- 75. Aslan iH, Demir M, Wise MM, Lenhart S. Modeling COVID‐19: Forecasting and analyzing the dynamics of the outbreak in Hubei and Turkey. medRxiv. 2020. 10.1101/2020.04.11.20061952. [DOI] [Google Scholar]
- 76. Tárnok A. Machine learning, COVID‐19 (2019‐nCoV), and multi‐OMICS. Cytometry. 2020;97(3):215‐216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Abdullah M, Altheyab M, Lattas AM, Algashmari WF. MERS‐CoV disease estimation (MED) a study to estimate a MERS‐CoV by classification algorithms. In: de Alencar M.S. eds. Communication. Management. Information Technology. 1st ed., Taylor & Francis; 2016: 633‐638. [Google Scholar]
- 78. Jang S, Lee S, Choi S‐M, Seo J, Choi H, Yoon T. Comparison between SARS CoV and MERS CoV Using Apriori Algorithm, Decision Tree, SVM. MATEC Web of Conferences. 2016;49:08001. 10.1051/matecconf/20164908001. [DOI] [Google Scholar]
- 79. Cohen IG, Gostin LO, Weitzner DJ. Digital smartphone tracking for COVID‐19: public health and civil liberties in tension. J Am Med Assoc. 2020;323(23):2371‐2372. [DOI] [PubMed] [Google Scholar]
- 80. Desai AN. Artificial intelligence: promise, pitfalls, and perspective. J Am Med Assoc. 2020;323(24):2448‐2449. [DOI] [PubMed] [Google Scholar]
- 81. De Felice F, Polimeni A. Coronavirus disease (COVID‐19): a machine learning bibliometric analysis. In Vivo. 2020;34(3 suppl):1613‐1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available in public domain resources.


