Dear Editor,
In recent months, there have been reported several dermatologic manifestations in COVID‐19 patients such as erythematous rash, widespread urticarial, chickenpox‐like vesicles, acroischemia, chilblain‐like eruptions and petechial rash mimicking dengue. 1 , 2
In this study, we present a case of alopecia areata (AA) in a patient who tested positive for COVID‐19. Our purpose is to further characterize dermatologic manifestations of this disease.
At the end of September, a 38‐year‐old healthy male patient presented to the dermatologic department because of sudden appearance of bald spots affecting the beard.
The patient had been diagnosed with SARS‐CoV‐2 infection in August, a month before the appearance of the bald spots.
He referred no other underlying diseases and denied taking any drugs during the last year, except for the paracetamol used as a symptomatic treatment for SARS‐CoV‐2 infection. No family history for AA and other autoimmune diseases was present.
Physical examination revealed sharply demarcated bald patches on the beard. The patches were round, variously distributed on the beard area. The underlying skin was unscarred and looks superficially normal (Figure 1).
FIGURE 1.

Pictures showing round bold patches variously distributed on the beard area
Our diagnosis was confirmed by trichoscopy showing yellow dots, black dots, broken hairs and short vellus hairs (Figure 2).
FIGURE 2.

Pictures showing trichoscopic findings of Alopecia Areata of the beard: black dots, yellow dots, broken hairs, vellus hairs
Further examination including liver, kidney and thyroid functionality were within normal limits. Serologic tests were negative for HIV, HBV, HCV and parvovirus B19. Nasopharyngeal swab was negative for SARS‐CoV‐2 as well. After 2 weeks of treatment with a trichological lotion with nicotinic acid, resorcinol and hyaluronic acid , the patient presented with an important improvement of the old lesions and the appearance of new ones (Figure 3).
FIGURE 3.

Pictures showing an improvement of the old lesions and the appearance of new ones, after two weeks of treatment with a trichological lotion with nicotinic acid, resorcinol and hyaluronic acid
Only few cases of AA in SARS‐CoV‐2‐infected patients have been reported in the literature. 3 The interplay among genetic factors (ie, HLA‐DR, CTLA4 and ULBP3) and environmental factors (ie, emotional/physical stress, hormones and infections) has been shown to play a key role in the AA etiology and progression. 4 , 5
Although the exact pathophysiology remains unknown, it seems to be related to an autoimmune reaction against the hair follicles. Supporting the autoimmune genesis of AA, several studies refer its association with other autoimmune diseases, such as type I diabetes and vitiligo. 4 We assume that SARS‐CoV‐2 could be an additional risk factor in the pathogenesis of AA. Referring to this, viral infection seems to be involved in autoimmune pathogenesis by two mechanisms: According to bystander theory, the presence of pathogens increases the release of costimulatory signals allowing the dendritic cells to present antigens more effectively, both pathogen and self‐antigens. If this occurs in genetically predisposed individuals, the activation of self‐reactive T lymphocytes could develop and progress (Figure 4).
FIGURE 4.
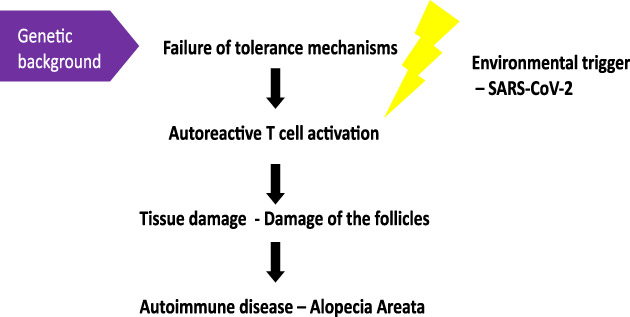
Possible role of SARS‐CoV‐2 in the pathogenesis of Alopecia Areata
As stated in the molecular mimicry theory, the virus could have antigens which cross‐react with self‐antigens, so that the immune response turns against host tissues. 6 Moreover, considering the significant impact of COVID‐19 pandemic on mental health, psychological stress appears to be another possible risk factor of AA. 5 , 7
SARS‐CoV‐2 could act as a trigger in different autoimmune pathways, by creating an inflammatory environment which allows the nonspecific activation of the immune system or by a cross‐reaction between its antigens and host antigens.
In both cases, antigens expressed at the level of the follicles are recognized and attacked by the immune system. Apart from the psychological effect, we believe that SARS‐CoV‐2 has an important role in the onset of AA. As we do not know the long‐term effects of SARS‐CoV‐2 infection, we will make periodical follow‐ups on our patient. These observations represent a further confirmation of AA as a multifactorial disease, but further studies are needed to confirm the relation between AA and COVID‐19.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
AUTHOR CONTRIBUTIONS
Severino Persechino conceived the research idea. Alessandro Capalbo, Charalampos Georgios Balampanos and Federica Orrù wrote the paper. Domenico Giordano, Nazareno Gagliostro and Flavia Persechino collected the data.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Recalcati S. Cutaneous manifestations in COVID‐19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34(5):e212‐e213. 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- 2. Wollina U, Karadağ AS, Rowland‐Payne C, Chiriac A, Lotti T. Cutaneous signs in COVID‐19 patients: a review. Dermatol Ther. 2020;33:e13549. 10.1111/dth.13549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sgubbi P, Savoia F, Calderoni O, Longo R, Stinchi C, Tabanelli M. Alopecia areata in a patient with SARS‐Cov‐2 infection. Dermatol Ther. 2020;XX:e14295. 10.1111/dth.14295. [DOI] [PubMed] [Google Scholar]
- 4. Baldini E, Odorisio T, Tuccilli C, et al. Thyroid diseases and skin autoimmunity. Rev Endocr Metab Disord. 2018;19(4):311‐323. [DOI] [PubMed] [Google Scholar]
- 5. Ricciardi A, Ruberto A, García‐Hernández MJ, et al. Alopecia areata with comorbid depression: early resolution with combined paroxetine‐triamcinolone treatment. J Eur Acad Dermatol Venereol. 2006;20(8):1000‐1001. 10.1111/j.1468-3083.2006.01592.x. [DOI] [PubMed] [Google Scholar]
- 6. Abbas AK, Lichtman AH, Pillai S, Cellular and Molecular Immunology, (8th ed.). California: Saunders; 2015. [Google Scholar]
- 7. Salari N, Hosseinian‐Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID‐19 pandemic: a systematic review and meta‐analysis. Global Health. 2020;16(1):57. 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


