Abstract
Background
Comparative morbidity after either sternotomy or non-resuscitative thoracotomy in penetrating cardiac injuries (PCI) is unknown.
Methods
Retrospective review of adults with PCI who underwent either sternotomy or non-resuscitative thoracotomy using the National Trauma Data Bank 2007-2015. Since there is no unique International Classification of Diseases Procedure Coding System (ICD-PCS) codes assigned for resuscitative vs. non-resuscitative thoracotomy, and both procedures were coded as “thoracotomy”, propensity score (PS) methods were applied to avoid inclusion of resuscitative thoracotomy.
Results
Despite well PS matching on injury severity score the non-thoracotomy group compared to the sternotomy group had a significantly increased risk of mortality (30 percent vs 8 percent, p<0.0001). The morbidity differed as well—25 percent vs. 12 percent, p=0.0007.
Conclusions
The differences in mortality in PCI patients who underwent non-resuscitative thoracotomy vs. sternotomy may be biased by unintentional inclusion of resuscitative thoracotomy. To accurately capture thoracotomy type, separate unique resuscitative and non-resuscitative thoracotomy procedure codes should be created in future revisions of the ICD PCS.
Keywords: Thoracotomy, sternotomy, resuscitative thoracotomy, penetrating cardiac injury
Introduction
Penetrating cardiac injuries (PCI) present a significant challenge to trauma surgeons. These injuries are largely considered highly lethal because an estimated 60-80 percent of patients will die on the scene or en route to a trauma facility1-3; with overall survival to discharge estimated around only 20 percent.4-6 Factors such as the cause of injury, transport time, and condition of the patient on arrival to the hospital naturally impact outcomes.3, 7
However, surgical intervention may increase the chance of survival by 24 percent to 60 percent for selected patients who demonstrate signs of life upon arrival at a trauma center.8 For these high-risk patients, it is imperative to effectively address the injuries as soon as possible.
For patients sustaining a PCI there are three surgical approaches: resuscitative thoracotomy, non-resuscitative thoracotomy and sternotomy. Resuscitative and non-resuscitative thoracotomies involve surgically opening the left chest in the fifth intercostal space whereas a median sternotomy involves midline division of the sternum. All these approaches allow the surgeon access to the heart in order to repair cardiac injuries. Although resuscitative thoracotomy and non-resuscitative thoracotomy utilize the same surgical incision, they are performed under much different clinical situations, require use of different resources, and result in different outcomes.
A resuscitative thoracotomy is an emergency procedure only performed on moribund patients who are in extremis or without vital signs. It is always performed in the emergency department, often under non-sterile conditions and without general anesthesia. This procedure is performed as a last chance at survival and allows for life-saving maneuvers including the release of cardiac tamponde, direct massage of the heart, and temporary repair of cardiac and other devastating intrathoracic injuries. After temporary control is established, the patient is taken to the operating room for further definitive surgical management. Overall, this procedure carries a greater than 90 percent mortality rate.9, 10
Non-resuscitative thoracotomy and sternotomy are performed in the operating room, under sterile conditions and general anesthesia, on patients who are not in extremis, and who were stable enough to tolerate the additional time to be brought to the operating room for the procedure. Both surgical approaches have advantages and limitations. A sternotomy provides better exposure of the anterior and lateral surfaces of the heart; however, it is more resource-intensive, time-consuming, and requires particular surgical skills and surgical instruments. It provides less exposure of both lungs and to the posterior surface of the heart.2 Non-resuscitative thoracotomy allows for quicker access to the heart and can be extended to the right chest if additional exposure is needed. Compared to median sternotomy, it violates the left thoracic cavity, which can potentially lead to lung-related complications.
In patients sustaining PCI without a direct indication for resuscitative thoracotomy, the surgical approach (sternotomy vs. non-resuscitative thoracotomy) is variable. The location of wounds, anticipated cardiac and other associated injuries, patient stability, and surgeon experience are all contributing factors2, 11 to determine the optimal surgical approach (sternotomy vs. non-resuscitative thoracotomy), though specifics vary widely in the literature. Studies that have directly compared these two approaches, particularly with respect to patient outcomes, 12, 13 are limited by smaller sample sizes.
The objective of this study was to compare the morbidity of patients with isolated penetrating cardiac injuries who underwent either sternotomy or non-resuscitative thoracotomy using the largest published cohort to date, derived from the National Trauma Data Bank (NTDB). The present study only considered those patients for whom non-resuscitative thoracotomy or sternotomy would have been indicated, based on the available data.
We hypothesized that non-resuscitative thoracotomy patients would have a higher risk of postoperative complications compared to sternotomy.
Material and Methods
This is a retrospective review of the research data sets (RDS) of the American College of Surgeon's (ACS) National Trauma Data Bank (NTDB). The Institutional Review Board at Tufts Medical Center approved the study.
The NTDB RDS for years 2007-15 were queried for adult (15 years of age and older) patients with PCI. The International Classification of Diseases, Ninth Revision, Procedure Coding System (ICD-9-PCS) was used to identify patients who underwent thoracotomy (34.02) and sternotomy (77.31). We used the ICD-9-PCS as oppose to ICD-10-PCS for two reasons. Firstly, only three years of ICD-10 coded data were available in NTDB (2015-2017) so the data from these three years would not provide us a significant number of subjects. Secondly, similar to ICD-9-PCS, no unique ICD-10-PCS codes were assigned for resuscitative and non-resuscitative thoracotomy but both procedures were coded as thoracotomy (Table 1).
Table 1.
Coding of thoracotomy and sternotomy
| Thoracotomy | ||||
|
| ||||
| ICD-9 | Description | ICD-10 | Description | |
|
| ||||
| 34.02 | Exploratory Thoracotomy | 02JA0ZZ | Inspection of Heart, Open Approach | |
|
| ||||
| 0WJC0ZZ | Inspection of Mediastinum, Open Approach | |||
|
| ||||
| Sternotomy | ||||
|
| ||||
| ICD-9 | Description | ICD-10 | Description | |
|
| ||||
| 77.31 | Other division of bone, scapula, clavicle, and thorax | 0P800ZZ | Division of Sternum, Open Approach | |
|
| ||||
| 0P803ZZ | Division of Sternum, Percutaneous Approach | |||
|
| ||||
| 0P804ZZ | Division of Sternum, Percutaneous Endoscopic Approach | |||
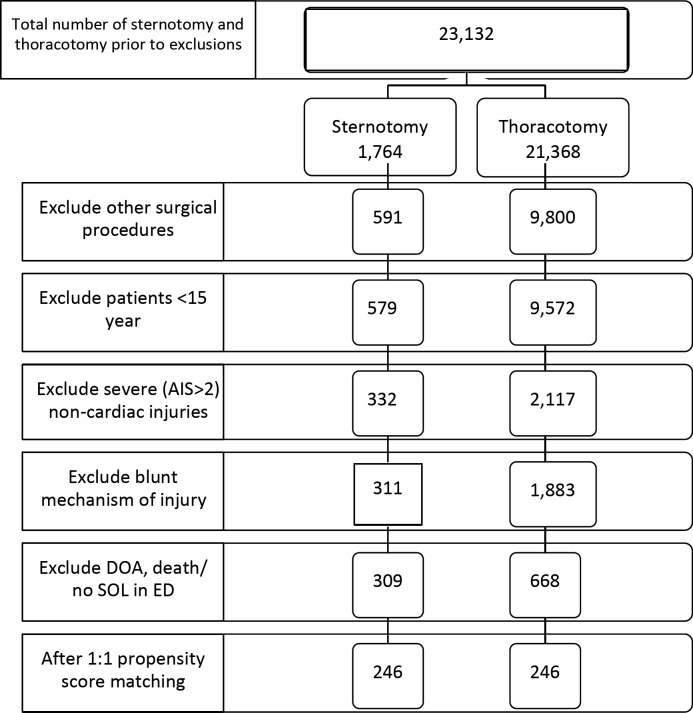
Cardiac injuries were identified using The Association for the Advancement of Automobile Medicine's Abbreviated Injury Scale 98 (AIS-98) codes that further specify injuries to the heart and pericardium. AIS-98 codes were used as opposed to AIS-05 since the use and reporting of AIS codes to the NTDB between 2007-2015 was not uniform, with AIS-98 coding being more consistent.14 Figure 1% represents the cohort selection process.
Figure 1.
Selection of the study cohort
Since there is no unique ICD-9 code for resuscitative thoracotomy, patients who arrived without signs of life were excluded, to avoid including patients who potentially underwent resuscitative thoracotomy in the non-resuscitative thoracotomy group. To minimize the impact of other significant injuries and procedures on outcomes, patients with associated extra-thoracic injuries with an AIS severity code of ≥ 3; injuries of trunk vessels, long bones and joint injuries; and those underwent surgery for brain, spine, neck, or abdominal/pelvic organ injuries were excluded.
The final cohort was divided into two study groups: those who underwent sternotomy versus non-resuscitative thoracotomy. Data were extracted on patient demographics (age, gender, race), causes of penetrating injury (stab wound or gunshot wound (GSW)), admission vital signs, Glasgow Coma Scale (GCS), presence of respiratory assistance, associated non-thoracic injuries, pre-existing comorbidities, and injury severity score (ISS). Data on outcomes included discharge disposition (including in-hospital mortality), hospital length of stay (LOS), intensive care unit (ICU) LOS, and days on mechanical ventilation. In addition, data were extracted on type of treating institution i.e.: community, academic, non-teaching, trauma level designation, hospital bed volume, number of surgeons, and geographic region.
The primary outcome of the study was a risk of morbidity. Secondary outcomes included days on mechanical ventilation, total ICU LOS, hospital LOS, and mortality.
Statistical Analysis
To further exclude those patients who may have undergone resuscitative thoracotomy, propensity score (PS) methods were used in an attempt to limit the analysis of outcomes to patients who had similar likelihood to have undergone either sternotomy or non-resuscitative thoracotomy based on the data available in the NTDB. Propensity for sternotomy (vs non-resuscitative thoracotomy) was calculated in a logistic regression model that included baseline patient and hospital characteristics potentially associated with choice of surgical procedure, including age, race (white, black, other, missing), year, admission systolic blood pressure, cause of injury (gunshot wound, stab wound), ISS, AIS severity of cardiac injury (range: 1 to 6), presence of extrathoracic injuries, trauma center level (I-II, all others), hospital bed size (1-350, 351-500, >500), US geographic region (Northeast, South, Midwest, West, missing), hospital teaching status (community, non-teaching, university), and number of trauma surgeons (0-3, 4-6, >6, missing). Categorical variables with missing values retained a missing indicator in order to retain those individuals in the PS model. Other admission vital signs and comorbidities were considered for inclusion, but ultimately discarded due to missing data. Sternotomy patients were then matched 1:1 on the propensity score with non-resuscitative thoracotomy patients, using a caliper width equal to 20 percent of the standard deviation of the logit of the propensity score.15
The balance of baseline characteristics between the groups (both before and after matching) was assessed using standardized differences, with values ≤0.1 indicating reasonable balance.
The risk of complications and mortality between groups was compared using McNemar's test for matched pairs. Among those patients who survived to be discharged, differences in days on mechanical ventilation, hospital LOS, and ICU LOS were compared with Wilcoxon rank-sum tests. Statistical analysis was performed using SAS v94, and all tests were two-sided with alpha=0.05.
Results
Prior to PS matching, the study cohort included 977 patients; 309 (31.6 percent) of them underwent sternotomy while 668 (68.4 percent) thoracotomy (Figure 1). Following 1:1 PS-matching, there were 246 patients in each procedure group. The groups were well matched on baseline demographics, admission blood pressure, injury severity score, and institutional characteristics (Table 2).
Table 2.
Patient and treating institution characteristics
| Non-Resuscitative Thoracotomy n=246 | Sternotomy n=246 | Standardized Difference | |
|---|---|---|---|
| A. Demographics | |||
|
| |||
| Age* | 33.6 (13.9) | 34.0 (13.1) | 0.03 |
|
| |||
| Male | 224 (91) | 220 (89) | 0.05 |
|
| |||
| Race | 89 (36) | 89 (36) | |
|
| |||
| White | 157 (64) | 157(64) | 0.07 |
|
| |||
| Non-white | |||
|
| |||
| B. Admission and Injury characteristics | |||
|
| |||
| SBP*, mmHg | 106.7±44.5 | 108.8 ±32.6 | 0.05 |
|
| |||
| AIS severity of cardiac injury >2, | 214(87) | 208 (85) | 0.08 |
|
| |||
| Presence of extra-thoracic injuries | 73 (30) | 77 (31) | 0.04 |
|
| |||
| (AIS 1-2) | |||
|
| |||
| ISS* | 27.7 ± 20.0 | 25.2 ± 19.4 | 0.13 |
|
| |||
| C. Treating institution | |||
|
| |||
| Community | 73 (30) | 68 (28) | |
|
| |||
| University | 161 (66) | 168 (68) | 0.07 |
|
| |||
| Non-teaching | 12 (5) | 10 (4) | |
|
| |||
| Trauma Level | 240 (98) | 241 (98) | 0.03 |
|
| |||
| I-II | |||
|
| |||
| Bed Size ≤ 350 351-500 >500 |
67 (27) 86 (35) 93 (38) |
62 (25) 88 (36) 96 (39) |
0.05 |
|
| |||
| Number of Surgeons 0-3 4-6 >6 |
13 (5) 108 (44) 111 (45) |
12 (5) 111 (45) 112 (46) |
0.09 |
|
| |||
| Missing | 14 (6) | 11 (5) | |
All data are presented as n (percent) unless indicated otherwise. AIS, Abbreviated Injury Scale; ISS, injury severity score; SBP, systolic blood pressure; *, mean ±standard deviation.
The majority of patients in both groups were admitted to Level 1 trauma centers, and were seen at academic university hospitals. Hospital size and number of trauma surgeons on staff were balanced between the facilities to which thoracotomy and sternotomy patients were admitted.
Outcomes
In-hospital mortality was higher in the non-resuscitative thoracotomy group (30 percent vs 8 percent, McNemar's p<0.0001). The risk of any complication occurring was significantly higher in the non-resuscitative thoracotomy group compared to the sternotomy group (25 percent versus 12 percent; McNemar's p=0.0007), in patients in whom data were available. The individual types of complications rarely occurred in either group so any meaningful comparison was impossible to perform. Non-resuscitative thoracotomy patients had more days on mechanical ventilation (p=0.0018) and both longer ICU and hospital length of stay (p=0.0133 and p=0.0003, respectively) (Table 3).
Table 3.
Outcomes
| Non-Resuscitative Thoracotomy (n=246) | Sternotomy (n=246) | p-value | |
|---|---|---|---|
| Any complication(s)* | 48/190 (25) | 23/190 (12) | 0.0007 |
|
| |||
| Mortality | 73 (30) | 20 (8) | >0.0001 |
|
| |||
| Duration among those discharged alive | |||
|
| |||
| Median DMV (IQR)* | n=66 2 (1, 3) |
n=66 1 (1, 2) |
0.0018 |
|
| |||
| Median ICU LOS days (IQR)* | n=147 3 (2, 5) |
n=147 (3 (2, 4) |
0.0133 |
|
| |||
| Median LOS days (IQR)* | n=161 8 (6, 11) |
n=161 7 (5, 9) |
0.0003 |
ALL data are presented as n (percent).
Denominators differ due to missing data
DMV, days on mechanical ventilation; ICU, intensive care unit; LOS, Length of stay; SD, standard deviation; IQR, interquartile range.
Discussion
Our study originally aimed to investigate the rate of complications in patients with PCI who underwent either sternotomy or non-resuscitative thoracotomy using the National Trauma Data Bank data. For the purposes of the study, our intent was to exclude patients who required a resuscitative thoracotomy. We found that patients with PCI in the non-resuscitative thoracotomy group had significantly higher mortality in comparison to the sternotomy group. This finding raises a question about the validity of our non-resuscitative thoracotomy group. First, previous studies directly comparing sternotomy and non-resuscitative thoracotomy in PCI did not demonstrate a significant difference in mortality.12, 13 Second, the lack of a specific code for resuscitative thoracotomy precluded us from confidently excluding these patients from the study cohort. Despite strict exclusion criteria and propensity score matching, it is likely that the non-resuscitative thoracotomy group included patients who were treated with either resuscitative or non-resuscitative thoracotomy, or both.
Our study found that the mortality in the non-resuscitative thoracotomy group was 30 percent, compared to only 8 percent in the sternotomy group. Based on published reports, we did not expect to find such a significant difference in mortality. Besir et. al, retrospectively reviewed the data of 40 patients who underwent surgery for a PCI at a single Turkish hospital over a 10-year period12. Twenty-six of the patients underwent a non-resuscitative thoracotomy, and 14 patients underwent sternotomy. Hemodynamic instability was not a determinant on the choice of the incision, and no patient underwent a resuscitative thoracotomy. The results showed the non-resuscitative thoracotomy group had greater blood transfusion requirements and longer LOS, but there were no significant differences in mortality between the two groups: 26.9 percent vs 14 percent, p=0.45. Mitchell et al. reviewed 115 PCI patients who were operated on over a 15-year period at their institution.13 No significant difference in mortality was found between the non-resuscitative thoracotomy and sternotomy groups (17.5 percent vs 7 percent, p=0.28). The mortality rate was 85 percent in those who required resuscitative thoracotomy.
The extremely high mortality rate of resuscitative thoracotomy is well established and is explained by the moribund conditions of these patients on whom the surgery is performed, rather than by the nature of the procedure itself. The resuscitative thoracotomy is performed in patients in extremis or those without vital signs. The Eastern Association for the Surgery of Trauma Practice Management Guidelines EAST10 analyzed data from 64 studies published over 50 years and showed a survival rate of only 10.6 percent (95 percent confidence interval: 9.8 to 11.3 percent) in patients with PCI who underwent a resuscitative thoracotomy. The survival of patients who did not require resuscitative thoracotomy is significantly higher. Morse et al1 reported their experience of managing PCI at a level one trauma center over a 36 year period. The overall mortality in the study cohort was 31 percent. The subgroup analysis showed a mortality rate of 64 percent in those receiving a resuscitative thoracotomy versus 18.6 percent in those that did not.
During the creation of the study protocol we realized the lack of specific coding for non-resuscitative thoracotomy could skew our findings. Therefore, we attempted to eliminate subjects who would potentially require a resuscitative thoracotomy by applying strict exclusion criteria and using propensity score matching. For example, patients with two common indications for resuscitative thoracotomy: arrival to emergency department with no signs of life, and “death on arrival” were excluded. Next, based on demographics, admission vital signs, and the injury severity score, we performed the propensity score matching between non-resuscitative thoracotomy and sternotomy groups. Both groups were matched appropriately, including the injury severity score. The injury severity score is an indicator of the overall injury significance and is a strong predictor of mortality in trauma patients.
Since institutional staffing and resources can vary, treating facility characteristics were addressed as well to understand procedural differences and patient outcomes. There were no significant structural differences among the treating facilities in our study.
Our study was done based on the ICD-9-PCS; however, the recently adopted ICD-10 classification codes similarly do not contain separate codes for resuscitative versus non-resuscitative thoracotomy (Table 1). The absence of the unique procedure code for the resuscitative thoracotomy does not allow researchers to perform nationwide analysis of the rate of this procedure and outcomes. The existing literature is limited to the reports from level one and two trauma centers that have the highest level of expertise. The results of these reports cannot be generalized as they are biased by the individual institutions' characteristics. The known differences between non-resuscitative and resuscitative thoracotomy in terms of indications, resources required to perform these procedures, and clinical outcomes are other considerations to suggest the creation of the unique procedure code for the resuscitative thoracotomy.
Conclusions
Analysis of our findings in light of the existing surgical literature suggest that the significant differences in morbidity and mortality in patients with isolated penetrating cardiac injuries who underwent non-resuscitative thoracotomy vs. sternotomy may be biased by the inclusion of resuscitative thoracotomy patients in the non-resuscitative thoracotomy group. The lack of a specific procedure code for resuscitative thoracotomy did not allow us to confidently exclude these patients from the non-resuscitative thoracotomy group. In order to accurately capture thoracotomy type, separate unique resuscitative and non-resuscitative thoracotomy procedure codes should be created in future revisions of the ICD PCS. Further studies with ICD PCS codes for resuscitative and non-resuscitative thoracotomy will need to be performed to confirm our findings.
Authors
Nikolay Bugaev, MD, (nbugaev@tuftsmedicalcenter.org), is associate director of trauma, Division of Trauma & Acute Care Surgery, Tufts Medical Center, Tufts University School of Medicine, Assistant Professor of Surgery.
Janis L. Breeze, MPH, (jbreeze@tuftsmedicalcenter.org) is associate director and an epidemiologist, Tufts Clinical and Translational Science Institute, Tufts University, and Institute for Clinical Research and Health Policy Studies, Tufts Medical Center.
Alyssa M. Tutunjian, MPH, (alyssa.tutunjian@tufts.edu) is a medical student at Tufts University School of Medicine.
Horacio Hojman, MD, (hhojman@tuftsmedicalcenter.org) is trauma medical director, Division of Trauma & Acute Care Surgery, Tufts Medical Center, Tufts University School of Medicine, Assistant Professor of Surgery.
Eric J Mahoney, MD, (emahoney1@tuftsmedicalcenter.org) is attending surgeon, Division of Trauma & Acute Care Surgery, Tufts Medical Center, Tufts University School of Medicine, Assistant Professor of Surgery
Benjamin P. Johnson, MD, (bjohnson5@tuftsmedicalcenter.org) is attending surgeon, Division of Trauma & Acute Care Surgery, Tufts Medical Center, Tufts University School of Medicine, Assistant Professor of Surgery.
Sandra S. Arabian, MBA, (sarabian@tuftsmedicalcenter.org) is trauma program manager, Division of Trauma & Acute Care Surgery, Tufts Medical Center.
Contributor Information
Nikolay Bugaev, (nbugaev@tuftsmedicalcenter.org), is associate director of trauma, Division of Trauma & Acute Care Surgery, Tufts Medical Center, Tufts University School of Medicine, Assistant Professor of Surgery..
Janis L Breeze, (jbreeze@tuftsmedicalcenter.org) is associate director and an epidemiologist, Tufts Clinical and Translational Science Institute, Tufts University, and Institute for Clinical Research and Health Policy Studies, Tufts Medical Center..
Alyssa M Tutunjian, (alyssa.tutunjian@tufts.edu) is a medical student at Tufts University School of Medicine..
Horacio M Hojman, (hhojman@tuftsmedicalcenter.org) is trauma medical director, Division of Trauma & Acute Care Surgery, Tufts Medical Center, Tufts University School of Medicine, Assistant Professor of Surgery..
Eric J Mahoney, (emahoney1@tuftsmedicalcenter.org) is attending surgeon, Division of Trauma & Acute Care Surgery, Tufts Medical Center, Tufts University School of Medicine, Assistant Professor of Surgery.
Benjamin P Johnson, (bjohnson5@tuftsmedicalcenter.org) is attending surgeon, Division of Trauma & Acute Care Surgery, Tufts Medical Center, Tufts University School of Medicine, Assistant Professor of Surgery..
Sandra S. Arabian, (sarabian@tuftsmedicalcenter.org) is trauma program manager, Division of Trauma & Acute Care Surgery, Tufts Medical Center..
References
- 1.Morse BC, et al. Penetrating cardiac injuries: A 36-year perspective at an urban, Level I trauma center. Journal of Trauma and Acute Care Surgery . (2016);81(no. 4):623–631. doi: 10.1097/TA.0000000000001165. [DOI] [PubMed] [Google Scholar]
- 2.Clarke DL, et al. Emergency operation for penetrating thoracic trauma in a metropolitan surgical service in South Africa. The Journal of thoracic and cardiovascular surgery . (2011);142(no. 3):563–8. doi: 10.1016/j.jtcvs.2011.03.034. [DOI] [PubMed] [Google Scholar]
- 3.Kaljusto ML, et al. Survival predictor for penetrating cardiac injury; a 10-year consecutive cohort from a scandinavian trauma center. Scandinavian Journal Of Trauma, Resuscitation And Emergency Medicine . (2015);23(no. 41) doi: 10.1186/s13049-015-0125-z. doi: 10.1186/s13049-015-0125-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang AL, et al. Postdischarge complications after penetrating cardiac injury: a survivable injury with a high postdischarge complication rate. Archives of Surgery . (2011);146(no.9):1061–6. doi: 10.1001/archsurg.2011.226. [DOI] [PubMed] [Google Scholar]
- 5.Rhee PM, et al. “Penetrating Cardiac Injuries: A Population-Based Study.”. The Journal of Trauma . (1998);45(no. 2):366–70. doi: 10.1097/00005373-199808000-00028. [DOI] [PubMed] [Google Scholar]
- 6.O'Connor J, Ditillo M, Scalea T. Penetrating cardiac injury. Journal of the Royal Army Medical Corps . (2009);155(no 3):185–90. doi: 10.1136/jramc-155-03-02. [DOI] [PubMed] [Google Scholar]
- 7.Asensio JA, et al. Penetrating cardiac injuries: a complex challenge. Injury . (2001);32(no.7):533–43. doi: 10.1016/s0020-1383(01)00068-7. [DOI] [PubMed] [Google Scholar]
- 8.Stranch EW, Zarzaur BL, Savage SA. Thinking outside the box: re-evaluating the approach to penetrating cardiac injuries. European journal of trauma and emergency surgery: official publication of the European Trauma Society . (2017);43(no.5):617–622. doi: 10.1007/s00068-016-0680-7. [DOI] [PubMed] [Google Scholar]
- 9.Rhee PM, et al. Survival after emergency department thoracotomy: review of published data from the past 25 years. Journal of the American College of Surgeons . (2000);190(no.3):288–98. doi: 10.1016/s1072-7515(99)00233-1. [DOI] [PubMed] [Google Scholar]
- 10.Seamon MJ, et al. An evidence-based approach to patient selection for emergency department thoracotomy: A practice management guideline from the Eastern Association for the Surgery of Trauma. The journal of trauma and acute care surgery . (2015);79(no.1):159–73. doi: 10.1097/TA.0000000000000648. [DOI] [PubMed] [Google Scholar]
- 11.Navid F, Gleason TG. Great vessel and cardiac trauma: diagnostic and management strategies. Seminars in thoracic and cardiovascular surgery . (2008);20(no.1):31–8.. doi: 10.1053/j.semtcvs.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 12.Beşir Y, et al. Choice of incision in penetrating cardiac injuries: Which one must we prefer: Thoracotomy or sternotomy? Ulusal travma ve acil cerrahi dergisi = Turkish journal of trauma & emergency surgery: TJTES . (2015);21(no.4):266–70. doi: 10.5505/tjtes.2015.52882. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell ME, et al. Surgical approach of choice for penetrating cardiac wounds. The Journal of Trauma; . (1993);34(no.1):17–20. doi: 10.1097/00005373-199301000-00003. [DOI] [PubMed] [Google Scholar]
- 14.National Trauma Data Bank. American College of Surgeons. Trauma Quality Programs (TQP) Participant Use File (PUF). User Manual Admission Years 2007-2016. https://web4.facs.org/TQIPFiles/TQPpercent20PUFpercent20Userpercent20Manualpercent202007percent20-percent202016.pdf. Updated June 2019. Accessed December 16, 2019.
- 15.Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharmaceutical Statistics . (2011);10(no.2):150–161. doi: 10.1002/pst.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate behavioral research . (2011);46(no.3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]