Abstract
This study described the results of online interprofessional education (IPE) between physical therapy and health information management students. Using the published Student Perceptions of Interprofessional Clinical Education – Revised, version 2 (SPICE-R2) survey, this study measured changes in perception about IPE before and after three online interactions. Survey results included an overall score and three factors: Interprofessional Teamwork and Team-Based Practice (T), Roles/Responsibilities for Collaborative Practice (R), and Patient Outcomes from Collaborative Practice (O). Data were analyzed using two-way analysis of variance tests using time and program as factors. The overall scores improved significantly for time (ρ=.019). The T factor demonstrated a significant change for program (ρ=.006) and the R factor improved significantly over time (ρ=.005) and by program (ρ=.022). Narrative student comments focused on role and responsibility clarification, communication and coordination, and participation in a realistic experience involving multiple professions. The students believed that the experience was beneficial and important.
Keywords: Interprofessional education, electronic health records, physical therapy, health information management, SPICE-R2, online education, distance learning
Introduction
This study described interprofessional education (IPE) activities between Doctor of Physical Therapy (DPT) students and Master of Health Information Management (MHIM) students at one large public university in Texas. Using online collaboration tools, students learned about each other's roles and responsibilities in health care, provided and received feedback about a medical documentation assignment, and discussed electronic health record (EHR) systems. The objectives of this study were to 1) determine student perceptions of interprofessional core competencies, and 2) measure the effectiveness of a planned online interprofessional learning experience. IPE is encouraged for all healthcare professions as important for addressing patient safety issues including medical errors.1 We found no existing literature describing a study of IPE targeting physical therapist (PT) and health information management (HIM) students, which necessitated this study, with the hypothesis that there would be a significant change between pre- and post-experience perceptions of PT and HIM students.
Participation in IPE activities is appropriate and timely for HIM students and practitioners. The HIM profession has evolved rapidly in recent years with increased involvement with EHR systems, data integrity, informatics, data analytics, cybersecurity, and other relevant areas. IPE activities provide opportunities to raise awareness among other healthcare related professions about the expanding roles of HIM professionals.
Background
IPE is defined by the World Health Organization as activities in which “students from two or more professions learn with, from, and about each other to enable effective collaboration and improve health outcomes.” 1 The explicit goal of IPE is to transform professional identities, practices, and relationships within and across health professions through the development of interprofessional practice.2
The Interprofessional Education Collaborative (IPEC) was formed in 2009 by six national associations of schools of health professionals to promote and encourage interprofessional learning.3 By 2016-2017, IPEC had grown to include over 20 institutional members committed to addressing “the urgent need for health professionals to work together.”4 The urgency was driven by continuing concern about patient safety with medical errors persisting as the third leading cause of death in the United States.5 IPEC has identified four core competencies for IPE which guided this study.
Values/Ethics: Work with individuals of other professions to maintain a climate of mutual respect and shared values.
Roles/Responsibilities: Use the knowledge of one's own role and those of other professions to appropriately assess and address the healthcare needs of patients and promote and advance the health of populations.
Interprofessional Communication: Communicate with patients, families, communities, and professionals in healthcare and other fields in a responsive and responsible manner that supports a team approach to the promotion and maintenance of health, and the prevention and treatment of disease.
Teams and Teamwork: Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/populations-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable.3
The importance of IPE has been recognized by Health Professions Accreditors Collaborative (HPAC) members including the Commission on Accreditation in Physical Therapy Education (CAPTE) and the Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM). The HPAC members “recognize that accreditation must play an important role promoting quality IPE that leads to effective health outcomes.”4 Current standards for accreditation in physical therapy include: “6F. The didactic and clinical curriculum includes interprofessional education; learning activities are directed toward the development of interprofessional competencies including, but not limited to, values/ethics, communication, professional roles and responsibilities, and teamwork,”6 which aligns closely with the IPEC core competencies. Curriculum requirements for accredited health informatics programs include a domain of knowledge, skills, and attitudes for interprofessional collaborative practice.7 Curriculum guidance for health information management includes competencies to “design effective teams … that are interprofessional and interdisciplinary” to address “development of interprofessional relationships” and to promote “diversity in interprofessional relationships.”8
Although health informatics and information management professionals are often not direct patient care providers, they do have an impact on patient outcomes through management of clinical data, information, and systems used by clinicians to make clinical decisions and to coordinate and communicate about patient care.9 With electronic health records and health information technology used by practitioners across all health professions, the collective field of health informatics and information management is inherently interprofessional.10
IPE approaches vary from dedicated programs to shared course offerings11 and short-term small group activities. A systematic review and meta-analysis by Guraya and Barr reported significant improvements in knowledge, skills, and attitudes after IPE activities in 11 of 12 articles reviewed.12
The tool used in this study to measure changes in perception about interprofessional education was the Student Perceptions of Interprofessional Clinical Education – Revised, version 2 (SPICE-R2) instrument. It contained ten Likert items which represented three factors: Interprofessional Teamwork and Team-Based Practice (Teamwork), Roles/Responsibilities for Collaborative Practice (Roles/Responsibilities), and Patient Outcomes from Collaborative Practice (Outcomes). Two of these factors were based on the IPEC core competencies (2) Roles/Responsibilities and (4) Teams and Teamwork. Although “clinical education” is in the name of the survey, this is not a clinical education outcome tool and has been used in many settings besides clinical education.
The SPICE-R2, used in the current study, was “designed for all health professions students”13 and was validated in a study of 1,708 multi-disciplinary students across five institutions, including 157 PT students. Another multi-institutional study presented in 2017 by Zorek, Lockeman, Eickhoff, and Gunaldo involving 810 medical, nursing, and PT students at three large public academic institutions confirmed the model structure of the SPICE-R2.14 The SPICE-R2 has good reliability (0.83) and acceptable-to-good reliability across factor subscales Teamwork (0.74), Roles/Responsibilities (0.72), and Outcomes (0.83). Profession-specific reliability for physical therapy is excellent (0.83).13 Reliability for health information management has not been established.
Methods
The design of this study was a two-group pre- and post-test survey. The SPICE-R2 survey as previously published15 was used with permission from one of the authors. In the survey, students rated their level of agreement with 10 statements. A five-point Likert scale was used with one (1) as strongly disagree and five (5) as strongly agree. The survey measured three of the four IPEC competency factors focusing on Teams and Teamwork (T), items 1, 4, 7, & 10; Roles/Responsibilities (R), items 2, 5, & 8; and Outcomes (O), items 3, 6, & 9. The maximum score for the survey was 50, with the T maximum score of 20, the R maximum of 15, and for O the maximum score was 15.15 Four additional administrative and demographic items were included in the survey: consent to use responses in this research project, student age and gender, and the course in which the student was enrolled. The post-survey instrument also included three open-ended questions eliciting comments from students about their perception of IPE experience. Those questions were: 1) Briefly describe what elements of the IPE activity you thought were MOST beneficial to you, 2) Briefly describe what elements of the IPE activity you thought were LEAST beneficial to you, and 3) What changes would make the IPE activity even more beneficial to future students?
Subjects
A convenience sample was used targeting students enrolled in specific courses. Thirty-eight PT students and seven HIM students participated in an IPE activity from February through April 2019. One PT student did not consent to participate in the research portion of the activities, resulting in 37 PT student responses. The PT students were enrolled in a face-to-face doctoral professional (entry-level) program and were in the sixth semester of a nine-semester program. This was the final semester of full-time academic coursework prior to the PT students completing 36 weeks of full-time clinical education. The seven HIM students were enrolled in a master's degree program delivered entirely online to geographically distributed students in US. Some of the HIM students had recently completed undergraduate HIM degrees and were continuing immediately to graduate school while others were HIM professionals with many years of experience. The HIM course was an elective, not required, and therefore had relatively low enrollment. These courses were selected by the coordinating faculty members because they involved subject matter and assignments that invited interdisciplinary engagement and were offered during the same semester.
The inclusion criteria were enrollment in either PT 7165, Clinical Decision-Making IV, or HIM 5340, Healthcare Informatics, and being over 18 years of age. There were no exclusion criteria. The study was approved by the Texas State University Institutional Review Board (IRB) (IRB #6240).
Procedures
The researchers met in person and online to develop the IPE experience for approximately six hours. They developed the learning objectives, activities, and assessments prior to beginning the semester. The PT faculty developed a patient case study and an associated assignment in which the PT students used an electronic documentation format. The HIM faculty developed a corresponding assignment for the HIM students to audit the PT students' documentation and provide feedback.
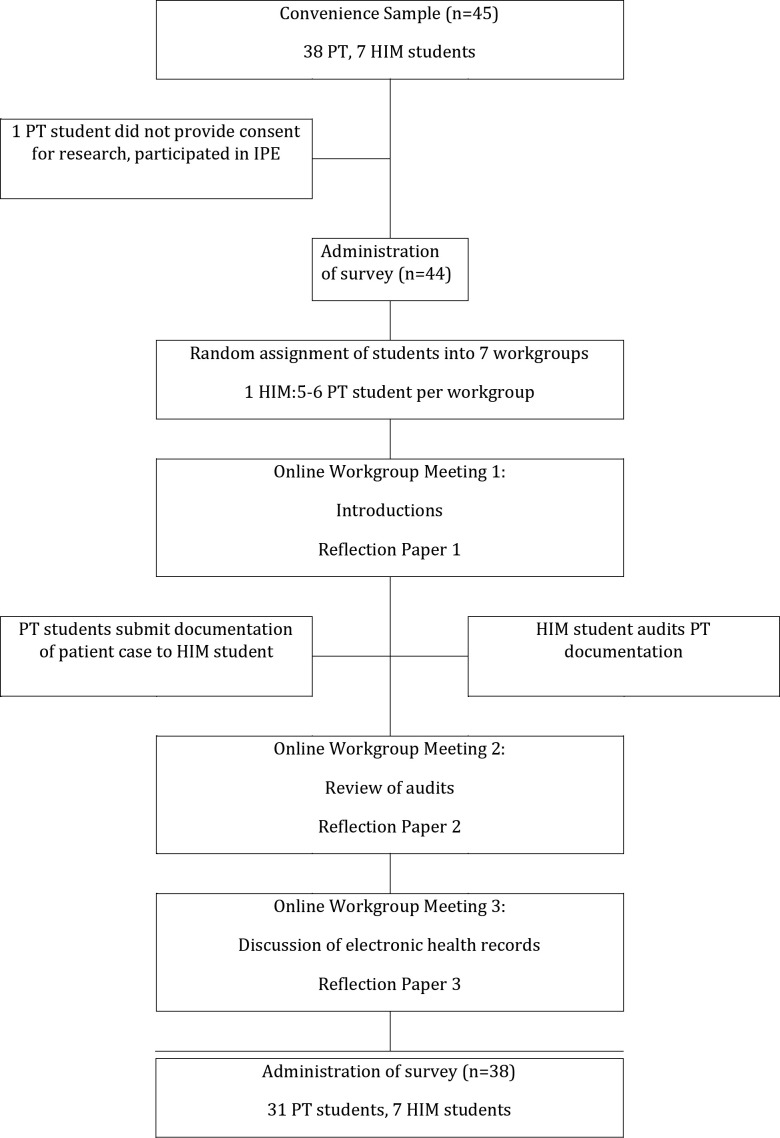
Once the semester began, students were randomly assigned to one of the seven groups, with each group consisting of five to six PT students and one HIM student. Students interacted together three times during the term. Figure 1 provides a flowchart of the sequence of activities used in the study. Pre-Meeting Work by Students: All participants submitted the pre-IPE survey (SPICE-R2 and demographic questions) through the university's online learning management system in their respective courses.
Figure 1.
Flowchart of methods
Online Workgroup Meeting 1: Students in assigned workgroups introduced themselves and discussed their professional educational backgrounds and roles via an online meeting tool such as Zoom, Teams, Facetime, or similar tools chosen by the students. Although the PT students were together on campus, the online HIM students were in different geographical areas, so no in-person meetings took place involving all students in the workgroups. After the meeting, each student wrote a reflection paper summarizing what they learned about themselves and the other professional discipline.
Between-Meetings 1 and 2: The PT students completed an initial evaluation of a patient case study and submitted the resulting documentation. The documentation was distributed for auditing by the HIM student in the group. The HIM students also received a copy of the case and a rubric identifying important information.
Online Workgroup Meeting 2: After the HIM students completed the audit of the PT students' documentation, the students met in their assigned workgroups via the online meeting platform to discuss the findings of the audit. Students provided rationales for decisions made while producing and auditing the documentation. Afterward, students wrote a paper reflecting on their interpersonal skills and communication as well as their experience of being part of an interprofessional team.
Online Workgroup Meeting 3: The workgroups met via the online meeting platform a final time to discuss the pros and cons of electronic versus paper medical records and of specific electronic health record (EHR) systems. Since EHR systems are used by both PT and HIM practitioners, this topic of common interest was specified in the assignment to motivate engagement. This approach was based on earlier studies that demonstrated the value of using EHR systems to link student assignments16 and studies to motivate students to learn about EHRs.17, 18 Students wrote a final paper reflecting what they learned about themselves from the IPE experience. After all student meetings concluded, the students completed the post-IPE survey (SPICE-R2 and additional questions).
Data Analysis
Demographic information was analyzed using descriptive statistics. The t-test for unequal variances was used to identify any difference in the ages between the PT and HIM students. The results of the survey were analyzed using four Two-Way ANOVAs (program x time) for the overall SPICE-R2 and the R, T, and O factors. Data analysis was conducted using SPSS.
Results
Thirty-seven of 38 (97.37%) PT students completed the pre-test and 31 (81.58%) completed the post-test. All seven HIM students (100%) completed both the pre- and post-test.
Of the 37 PT students who participated in the study, 24 were female and 13 were male with the mean age of 27.10 and a range of 23-40 years. The mean age of the seven HIM students was 27.14 with a range of 23-36 and all were females. There were no statistical differences in age between the two groups (t= -.237, ρ= .814).
Means and standard deviations (SD) for the overall SPICE-R2 pretest scores for the PT students were 38.36 (SD=3.58) and 40.14 (SD=3.18) for the HIM students. The post-test mean scores and standard deviations were 40.77 (SD=4.51) for the PT students and 43.43 (SD=4.65) for the HIM students, as seen in Table 1.
Table 1.
Descriptive Statistics
| Physical Therapist Student Mean (Standard Deviation) | Health Information Management Student Mean (Standard Deviation) | |
|---|---|---|
| Overall | ||
|
| ||
| Pre-test | 38.36 (3.58) | 40.14 (3.18) |
|
| ||
| Post-test | 40.77 (4.51) | 43.43 (4.65) |
|
| ||
| Team/Teamwork (T) | ||
|
| ||
| Pre-test | 16.25 (2.23) | 18 (1.29) |
|
| ||
| Post-test | 17.097 (1.68) | 18.57 (1.62) |
|
| ||
| Roles/ Responsibilities (R) | ||
| Pre-test | 9.56 (1.52) | 10.57 (2.44) |
|
| ||
| Post-test | 10.87 (2.17) | 12.43 (1.51) |
|
| ||
| Patient Outcomes (O) | ||
|
| ||
| Pre-test | 12.56 (1.80) | 11.57 (1.27) |
| Post-test | 12.81 (1.82) | 12.43 (1.90) |
The differences in the overall SPICE-R2 scores by program (PT, HIM) and time (pre- and post-test) was significant for the main effect of time (F=5.784, ρ=.019), but not for program (ρ= .065) or the interaction of program and time (ρ= .714). Examining the individual factors, there was a significant difference in the main effect of program (F= 8.121, ρ= .006) for the T factor and no significant difference for time (ρ= .214) or for the interaction of program and time (ρ=.808). The R factor had significant differences for both main effects, program (ρ=.022) and time (ρ=.005), but not for the interaction of program and time (ρ =.625). There were no significant differences for the main effects of program (ρ=.196) or time (ρ=.292) or the interaction of program and time (ρ=.563) for the O factor scores, as seen in Table 2.
Table 2.
Results of Two-Way ANOVA
| Comparison | Program Main Effect | Time Main Effect | Interaction Program × Time |
|---|---|---|---|
| Overall | ρ=.065 | ρ=.019* | ρ=.714 |
|
| |||
| Teams/Teamwork | ρ=.006* | ρ=.214 | ρ=.808 |
|
| |||
| Roles/Responsibility | ρ=.022* | ρ=.005* | ρ=.625 |
|
| |||
| Patient Outcomes | ρ=.196 | ρ=.292 | ρ=.563 |
Key: indicates significant finding, with alpha = .05.
Discussion
The IPE activities promoted a positive perception of PT and HIM students working in a collaborative interprofessional manner, confirming the hypothesis. The overall SPICE-R2 and the R factor scores for PT and HIM students combined improved from the pre- to the post-test survey. The T and R factor scores showed significant differences in pre- and post-test scores between the PT and HIM students.
Qualitative results from this study will be reported separately, but briefly the narrative responses to open-ended survey questions and reflection paper assignments demonstrated that most PT and HIM students found the IPE experience valuable. Three themes emerged from the narrative data: roles and responsibilities, communication and coordination, and participating in an activity that simulates realistic engagement between healthcare professionals.
Another important point demonstrated by this study was that benefits from IPE can be achieved when students are geographically distributed by using widely available online collaboration tools. As other studies have shown, the same strategies and tools that are increasingly used to facilitate online teaching and learning within disciplines can also be used across disciplines.19 In our study, synchronous online collaboration platforms were effectively used to facilitate IPE among students distributed across geographically separate locations. While students reported challenges of scheduling meetings with multiple attendees, the logistical challenges would have been even more significant if travel time and physical presence were required.
This study demonstrated that students may realize benefits from IPE without substantial time commitments from faculty. The two instructors involved in this study spent no more than six hours throughout the semester on IPE activities, including planning, delivery, and assessment. Following a strategy of awareness and integration before creation, the instructors recognized the opportunity to make slight adjustments to existing courses and assignments rather than creating entirely new IPE activities.20 This approach also avoided issues related to managing the total number of hours allowed for accredited programs and was consistent with the HPAC recommendation to integrate IPE activities into existing professional curriculum.4
Limitations
This study was limited by several factors. A potential limitation is that the SPICE-R2 has not yet been validated for HIM students and that in the 2017 study by Zorek et al., there was suboptimal fit and questions about reliability for PT students in the roles/responsibilities (0.61) and patient outcomes (0.69) even though the overall profession-specific reliabilities were good for physical therapy (0.86).14 Although the SPICE-R2 has good psychometric properties, a correlation between its scores and acquisition of interprofessional skills has not been established.15 Despite these limitations, the authors of the current study believe that it was an appropriate instrument to use. The SPICE-R2 provided information about perceptions of IPE, but without a focus on any particular profession. The survey was relevant to all participants in this study because the questions focused on interprofessional collaboration rather than direct patient care. It is an appropriate instrument to measure differences between health professions, to measure differences between students with and without healthcare experience, and differences before and after an IPE.21
Another limitation was the scope of the study being focused on one university and two disciplines. Future research could expand this approach to include more institutions and more disciplines to increase the generalizability of the results.
As the first attempt at this type of IPE between PT and HIM at our university, the participants were limited to students enrolled in courses taught by the collaborating researchers during the study period. The course in which the HIM students were enrolled was an elective and therefore participants' number was small compared to the PT students who were enrolled in a required course. Expanding the scope to additional courses and across additional healthcare disciplines would improve future studies of this type. The study was also limited by the time of being a single academic semester. Future research monitoring the benefits of IPE from matriculation to graduation from an academic program would be beneficial.
Conclusion
This study described interprofessional learning activities between PT and HIM students that consisted of homework assignments and three synchronous online workgroup meetings which provided a unique learning experience for both sets of students. Students met online to learn about their roles and responsibilities in health care, to provide and receive feedback about a documentation assignment, and to discuss different types of electronic health record systems. Students' scores on the overall survey improved significantly as did the T and R factors. Students' reflections focused on role clarification, communication and coordination, and participating in a realistic experience. The students believed that the experience was beneficial and important to them.
Authors
Lois Stickley, PT, PhD, (lois.stickley@txstate.edu) is an associate professor at Texas State University College of Health Professions in the Department of Physical Therapy.
David Gibbs, PhD, CPHIMS, CPHI, CHPS, CISSP, FHIMSS, (dgibbs@txstate.edu) is an assistant professor at Texas State University College of Health Professions in the Department of Health Information Management.
Contributor Information
Lois Stickley, (lois.stickley@txstate.edu) is an associate professor at Texas State University College of Health Professions in the Department of Physical Therapy..
David Gibbs, (dgibbs@txstate.edu) is an assistant professor at Texas State University College of Health Professions in the Department of Health Information Management..
References
- 1.World Health Organization. Framework for Action on Interprofessional Education and Collaborative Practice. WHO Press; 2010. http://apps.who.int/iris/bitstream/10665/70185/1/WHO_HRH_HPN_10.3_eng.pdf . [PubMed] [Google Scholar]
- 2.Olson RE, Brosnan C. Examining interprofessional education through the lens of interdisciplinarity: power, knowledge and new ontological subjects. Minerva: A Review of Science, Learning and Policy . (2017);55(no. 3):299. doi:10.1007/s11024-017-9316-2. [Google Scholar]
- 3.Interprofessional Education Collaborative. Core Competencies for Interprofessional Collaborative Practice: 2016 Update. Washington, DC:: Interprofessional Education Collaborative; 2016. https://www.tamhsc.edu/ipe/research/ipec-2016-core-competencies.pdf . [Google Scholar]
- 4.Health Professions Accreditors Collaborative. Guidance on Developing Quality Interprofessional Education for the Health Professions. Chicago, IL:: 2019. https://healthprofessionsaccreditors.org/wp-content/uploads/2019/02/HPACGuidance02-01-19.pdf . [Google Scholar]
- 5.Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ . (2016);353(no. 1):i2139. doi: 10.1136/bmj.i2139. doi: https://doi.org/10.1136/bmj.i2139. [DOI] [PubMed] [Google Scholar]
- 6.Commission on Accreditation in Physical Therapy Education. Standards and Required Elements for Accreditation of Physical Therapist Education Programs. Commission on Accreditation in Physical Therapy Education; 2016. http://www.capteonline.org/AccreditationHandbook . [Google Scholar]
- 7. HI Curriculum Requirements. Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM); 2017. Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM). [Google Scholar]
- 8.American Health Information Management Association (AHIMA) 2018 Graduate Curriculum Guidance. Chicago, IL: American Health Information Management Association; 2019. [Google Scholar]
- 9.Mccullough JS, Parente ST, Town R. Health information technology and patient outcomes: the role of information and labor coordination. RAND Journal of Economics . (2016);47(no. 1):207–236. doi:10.1111/1756-2171.12124. [Google Scholar]
- 10.Cummins MR, Gundlapalli AV, Murray P, Park HA, Lehmann CU. Nursing informatics certification worldwide: history, pathway, roles, and motivation. Yearbook of Medical Informatics . (2016);(no. 1):264–271. doi: 10.15265/IY-2016-039. doi:10.15265/IY-2016-039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sittig S, Hazelwood A. Health information management course sharing: an interprofessional/multidisciplinary perspective. Educational Perspectives in Health Informatics & Information Management (EPHIM) no. (2018):1–12. https://perspectives.ahima.org/himcoursesharing. [Google Scholar]
- 12.Guraya SY, Barr H. The effectiveness of interprofessional education in healthcare: a systematic review and meta-analysis. Kaohsiung Journal of Medical Sciences 34. (2018);(no. 3):160–165. doi: 10.1016/j.kjms.2017.12.009. doi:10.1016/j.kjms.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 13.Zorek JA, Fike DS, Eickhoff JC, Engle JA, Maclaughlin EJ, Dominguez DG, Seibert CS. Refinement and validation of the student perceptions of physician-pharmacist interprofessional clinical education instrument. American Journal of Pharmaceutical Education 80. (2016);(no. 3):1–8. doi: 10.5688/ajpe80347. doi:10.5688/ajpe80347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zorek JA, Lockeman KS, Eickhoff JC, Gunaldo TP. ” Presentation at American Interprofessional Health Collaborative and Canadian Interprofessional Health Collaborative. Collaborating Across Borders Meeting; Banff, Canada: Multi-institutional validation of the student perceptions of interprofessional clinical education-revised instrument, version 2 (SPICE-R2). 10/2/2017. doi:10.13140/RG.2.2.25756.80003. [Google Scholar]
- 15.Lockeman KS, Lanning SK, Dow AW, Zorek JA, Diazgranados D, Ivey CK, Soper S. Outcomes of introducing early learners to interprofessional competencies in a classroom setting. Teaching and Learning in Medicine 29. (2017);(no. 4):433–443. doi: 10.1080/10401334.2017.1296361. doi:10.1080/10401334.2017.1296361. [DOI] [PubMed] [Google Scholar]
- 16.Kavanaugh-Burke L. The EHR project: linking curricular components. Educational Perspectives in Health Informatics & Information Management (EPHIM) Fall, no. (2017):1–9. https://perspectives.ahima.org/theehrproject. [Google Scholar]
- 17.Mcleod A, Hewitt B, Gibbs D, Kristof C. Evaluating motivation for the use of an electronic health record simulation game. Perspectives in Health Information Management no. (2017):1–19. https://perspectives.ahima.org/evaluatingmotivation. [PMC free article] [PubMed] [Google Scholar]
- 18.Gibbs D, Hewitt B, Mcleod A. The gamification of electronic health records: a systematic literature review. Educational Perspectives in Health Informatics and Information Management no. (2016) https://perspectives.ahima.org/the-gamification-of-electronic-health-records-a-systematic-literature-review. [Google Scholar]
- 19.Mckenna L, Boyle M, Palermo C, Molloy E, Williams B, Brown T. Promoting interprofessional understandings through online learning: a qualitative examination. Nursing and Health Sciences 16, no. (2014):321–326. doi: 10.1111/nhs.12105. doi:10.1111/nhs.12105. [DOI] [PubMed] [Google Scholar]
- 20.Lalani KH, Gibbs DL. Relevance of interprofessional education for HIM professionals. Journal of AHIMA 89, no. (2018);10:18–23. http://bok.ahima.org/doc?oid=302603#.XlJzlEp7mUk . [Google Scholar]
- 21.Dominguez DG, Fike DS, Maclaughlin EJ, Zorek JA. A comparison of the validity of two instruments assessing health professional student perceptions of interprofessional education and practice. Journal of Interprofessional Care 29, no. (2015);2:144–149. doi: 10.3109/13561820.2014.947360. doi:10.3109/13561820.2014.947360. [DOI] [PubMed] [Google Scholar]