Abstract
Background
In ovarian mucinous carcinoma, invasive pattern is the important factor but there were less reposts to investigate it. The aim of this study was to examine the association between prognosis and invasive patterns of ovarian mucinous carcinoma and to investigate the biomarkers of the diagnosis and prognosis immunochemically. Patients with ovarian mucinous carcinoma at our institution between 1984 and 2018 were identified. A pathological review was conducted using the 2020 World Health Organization criteria. The prognosis of infiltrative invasion and expansile invasion of ovarian mucinous carcinoma were retrospectively compared. In addition, immunohistochemical staining was conducted for all cases, and the immunohistochemical differences between the two invasive patterns were compared.
Results
After the pathological review, 25 cases with infiltrative invasion and 24 cases with expansile invasion were included. Ovarian mucinous carcinoma with infiltrative invasion showed significantly worse progression-free survival (PFS, p < 0.01) and overall survival (OS, p < 0.01) than those with expansile invasion. Multivariate analysis demonstrated that the pattern of infiltrative invasion was a worse prognostic factor for PFS (hazard ratio 9.01, p < 0.01) and OS (hazard ratio 17.56, p < 0.01). Immunohistochemically, cytokeratin (CK) 5/6 (p = 0.01), cluster of differentiation (CD) 24 (p = 0.02), and epithelial growth factor receptor (EGFR) (p < 0.01) were statistically related to infiltrative invasion. The PFS (p = 0.04) and OS (p = 0.02) of cases with EGFR-positive OMC were worse than those with negative OMC.
Conclusions
Infiltrative invasion was observed to be a prognostic factor showing worse outcomes for ovarian mucinous carcinoma compared to expansile infiltration. CK5/6, CD24, and EGFR might be biomarkers of the diagnosis.
Keywords: Ovarian mucinous carcinoma, Invasive pattern, Infiltrative invasion, Expansile invasion, 2020 World Health Organization, Prognosis
Background
Ovarian carcinoma (OC) is the most lethal gynecological carcinoma [1]. The histology of OC is an important factor related to the prognosis, in addition to the International Federation of Gynecology and Obstetrics (FIGO) stage and residual tumor at surgery [2–7]. Histologically, OCs are classified into type I and type II based on distinctive morphological and molecular genetic features [8, 9]. Type I tumors are discovered at an early stage and have an indolent clinical course [8, 9]. In contrast, type II tumors are detected at an advanced stage and exhibit highly aggressive behavior [8, 9]. Because ovarian mucinous carcinoma (OMC) is classified as a type I tumor, it is considered a nonaggressive histological subtype.
The incidence of OMC among OCs ranges from 3 to 11 % [10]. The majority (65–80 %) of OMC cases are diagnosed at an early stage [11]. OMC is known to be poorly responsive to conventional chemotherapy, and its prognosis depends on the FIGO stage and residual tumor size after the primary surgery [4–7, 11–13]. The prognosis of OMC in the early stage is not different from that of other histological subtypes; however, it is worse in the advanced stage [10, 11]. Thus, a new treatment for OMC is needed.
According to the 2020 World Health Organization (WHO) classification, the invasive patterns of OMC are classified into two categories: infiltrative invasion and expansile invasion [14]. Infiltrative invasion is characterized by irregular glands, nests, and single cells with malignant cytological features infiltrating the stroma, which is often desmoplastic. Expansile invasion is characterized by marked glandular crowding with little intervening stroma, creating a labyrinthine appearance, and a cribriform pattern might be present. In addition to the above-mentioned prognostic factors, several reports have demonstrated that the invasive pattern is associated with the prognosis of OMC [15–20]. We considered that a study examining the relationship between the invasive patterns and prognosis of OMC is necessary owing to the rarity of OMC.
The aim of the present study was to revalidate the differences in the clinicopathological features, prognosis, and immunohistochemical features between infiltrative invasion and expansile invasion of OMC through a pathological review. Further, we reviewed the existing literature.
Results
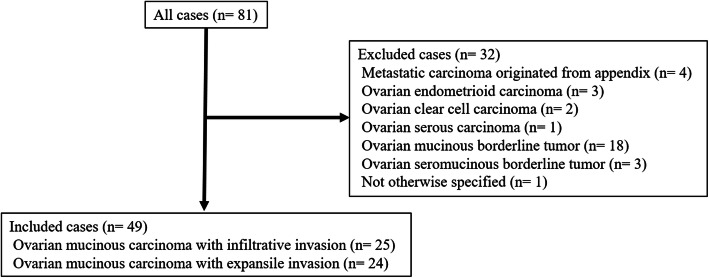
A total of 81 patients with OMC were identified. The results of the pathological review are shown in Fig. 1. The pathological diagnosis of 49 cases was OMC and that of 32 cases was changed from OMC to other histological subtypes, including metastatic carcinoma originating from the appendix in 4 cases, ovarian endometrioid carcinoma in 3 cases, ovarian clear cell carcinoma in 2 cases, ovarian serous carcinoma in 1 case, ovarian mucinous borderline tumor in 18 cases, ovarian seromucinous borderline tumor in 3 cases, and not otherwise specified in 1 case.
Fig. 1.
Change of histological type in all cases after a pathological review
Eighty-one cases of ovarian mucinous carcinoma (OMC) were initially identified. After a pathological review, 4 cases were diagnosed with metastatic carcinoma originating from the appendix, 3 cases were diagnosed with ovarian endometrioid carcinoma, 2 cases with ovarian clear cell carcinoma, 1 case with ovarian serous carcinoma, 18 cases with ovarian mucinous borderline tumor, 3 cases with ovarian seromucinous borderline tumor, and 1 case was not otherwise specified; additionally, these cases were excluded. Finally, 25 cases of OMC with infiltrative invasion and 24 cases of OMC with expansile invasion were included
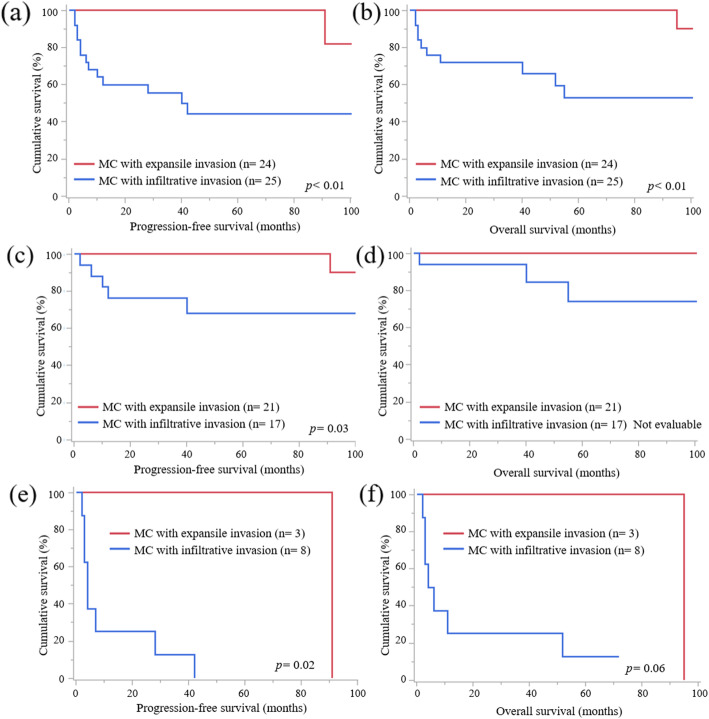
Among the 49 patients diagnosed with OMC, 25 (51 %) cases with infiltrative invasion and 24 (49 %) cases with expansile invasion were included in our analysis. The median observation period in the OMC cases was 53 (1–262) months. The characteristics of OMC according to the invasive patterns are listed in Table 1. It was observed that OMC with infiltrative invasion was more frequently treated with adjuvant chemotherapy (p = 0.02) and more often recurred (p < 0.01) than OMC with expansile invasion. There was no statistical difference in the response rate between the two groups; however, all cases with expansile invasion that had residual tumor at primary debulking surgery (PDS) achieved complete response or partial response after adjuvant chemotherapy. Other factors showed no statistically significant differences between the two groups. OMC with infiltrative invasion showed worse PFS (Fig. 2a, p < 0.01) and OS (Fig. 2b, p < 0.01) than OMC with expansile invasion in all FIGO stages. In FIGO stage I and II, OMC with infiltrative invasion showed worse PFS than OMC with expansile invasion (Fig. 2c, p = 0.03), but OS was not evaluable because no patients with expansile invasion died for diseases (Fig. 2d). Also, in FIGO stage III and IV, OMC with infiltrative invasion showed worse PFS (Fig. 2e, p = 0.02) but not OS than OMC with expansile invasion (Fig. 2f , p = 0.06).
Table 1.
Characteristics of 49 patients with ovarian mucinous carcinoma according to invasive patterns
| Ovarian mucinous carcinoma with infiltrative invasion |
Ovarian mucinous carcinoma with expansile invasion |
p-Value | |
|---|---|---|---|
| Variables | n = 25 | n = 24 | |
| Age (years) | 0.16 | ||
| < 51 | 16 (64) | 10 (42) | |
| ≥ 51 | 9 (36) | 14 (58) | |
| FIGO stage (%) | 0.26 | ||
| I | 16 (64) | 20 (84) | |
| II | 1 (4) | 1 (4) | |
| III | 6 (24) | 1 (4) | |
| IV | 2 (8) | 2 (8) | |
| Tumor site (%) | 0.35 | ||
| Unilateral | 21 (84) | 23 (96) | |
| Bilateral | 4 (4) | 1 (4) | |
| Standard surgery (%) | 0.78 | ||
| Yes | 15 (60) | 13 (54) | |
| No | 10 (40) | 11 (46) | |
| Peritoneal cytology (%) | 0.78 | ||
| Positive | 12 (48) | 10 (42) | |
| Negative | 13 (52) | 14 (58) | |
| Residual tumor diameter at PDS (%) | 0.58 | ||
| No residual tumor | 18 (72) | 20 (83) | |
| < 1.0 cm | 1 (4) | 1 (4) | |
| ≥ 1.0 cm | 6 (24) | 3 (13) | |
| Adjuvant chemotherapy (%) | 0.02 | ||
| Not done | 4 (16) | 12 (50) | |
| Done | 21 (84) | 12 (50) | |
| Regimen of the adjuvant chemotherapy | |||
| Paclitaxel and carboplatin | 5 (24) | 2 (17) | 0.20 |
| Platinum-based therapy a | 16 (76) | 10 (83) | |
| Response rate of adjuvant chemotherapy for patients with residual tumor which received adjuvant chemotherapy (%) | 0.20 | ||
| CR/PR | 3 (43) | 3 (100) | |
| S D/PD | 4 (57) | 0 (0) | |
| Recurrence (%) | < 0.01 | ||
| Yes | 13 (52) | 2 (8) | |
| No | 12 (48) | 22 (92) |
Abbreviations:SD standard deviation; FIGO International Federation of Gynecology and Obstetrics; PDS primary debulking surgery; cm centimeter; CR complete response; PR partial response; SD stable disease; PD progressive disease
a Platinum-based therapy included the combination with cyclophosphamide, doxorubicin, and cisplatin, the combination with cyclophosphamide and cisplatin, the combination with etoposide and cisplatin, and the combination with irinotecan and nedaplatin
Fig. 2.
PFS and OS curves according to FIGO stage status
a PFS curves of cases of OMC with infiltrative invasion and expansile invasion in all FIGO stages. OMC with infiltrative invasion showed worse PFS than OMC with expansile invasion. b OS curves of cases of OMC with infiltrative invasion and expansile invasion in all FIGO stages. OMC with infiltrative invasion exhibited worse OS than OMC with expansile invasion. c PFS curves of cases of OMC with infiltrative invasion and expansile invasion in FIGO stage I and II. OMC with infiltrative invasion showed worse PFS than OMC with expansile invasion. d OS curves of cases of OMC with infiltrative invasion and expansile invasion in FIGO stage I and II. There were no statistical significances about OS between two groups. e PFS curves of cases of OMC with infiltrative invasion and expansile invasion in FIGO stage III and IV. OMC with infiltrative invasion showed worse PFS than OMC with expansile invasion. d OS curves of cases of OMC with infiltrative invasion and expansile invasion in FIGO stage III and IV. There were no statistical significances about OS between two groups
The univariate analysis of PFS and OS revealed that FIGO stage, residual tumor at PDS, and invasive pattern were prognostic factors. The multivariate analysis for PFS and OS using these variables revealed that infiltrative invasion was a worse prognostic factor for PFS (hazard ratio [HR] 9.01, p < 0.01) and OS (HR 17.56, p < 0.01) (Table 2).
Table 2.
Univariate and multivariate analysis for PFS and OS in all patients with OMC
| Progression-free survival | Overall survival | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | Univariate analysis | Multivariate analysis | |||||
| Variables | HR (95 % CI) | p-value | HR (95 % CI) | p-value | HR (95 % CI) | p-value | HR (95 % CI) | p-value |
| Age (years) | ||||||||
| ≥51 vs. <51 | 0.51 (0.17–1.42) | 0.20 | 0.71 (0.20–2.35) | 0.57 | ||||
| FIGO stage | ||||||||
| I vs. II, III, IV | 0.11 (0.04–0.32) | < 0.01 | 0.12 (0.02–0.61) | 0.01 | 0.06 (0.01–0.22) | < 0.01 | 0.09 (0.01–0.84) | 0.04 |
| Residual tumor at PDS | ||||||||
| Optimal vs. Suboptimal | 0.17 (0.06–0.50) | < 0.01 | 0.95 (0.20–3.55) | 0.94 | 0.09 (0.02–0.29) | < 0.01 | 0.37 (0.05–1.68) | 0.21 |
| Invasive pattern | ||||||||
| Infiltrative invasion vs. Expansile invasion | 8.69 (2.37–55.86) | < 0.01 | 9.01 (2.28–61.41) | < 0.01 | 12.52 (2.37-230.59) | < 0.01 | 17.56 (2.58-393.24) | < 0.01 |
Abbreviations: PFS Progression-free survival, OS Overall survival, OMC ovarian mucinous carcinoma, HR hazard ratio, CI confidence interval, PDS primary debulking surgery
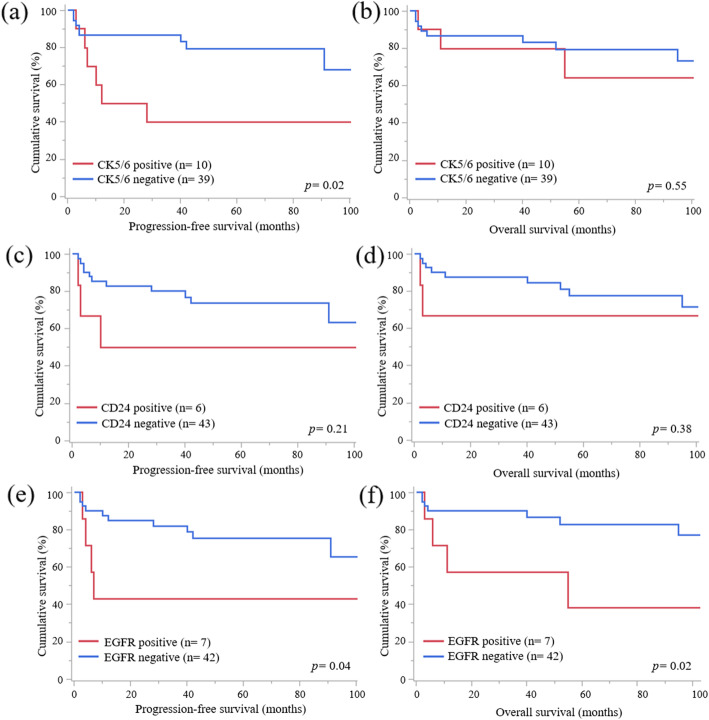
The results of immunohistochemical staining for each invasive pattern are listed in Table 3. It is notable that more cases of OMC with infiltrative invasion were positive for cytokeratin 5/6 (CK5/6) (p = 0.01), cluster of differentiation 24 (CD24) (p = 0.02), and epithelial growth factor receptor (EGFR) (p < 0.01) than those of OMC with expansile invasion. Only two cases were positive for all CK5/6, CD24, and EGFR. There were no statistical differences between several proteins and invasive patterns. The patients with CK5/6-positive OMC had worse PFS (Fig. 3a, p = 0.02) but not OS (Fig. 3b, p = 0.55) than those with negative OMC. There were no statistical differences of PFS (Fig. 3c, p = 0.21) and OS (Fig. 3d, p = 0.38) according to CD24 status. The patients with EGFR-positive OMC had worse PFS (p = 0.04) and OS (p = 0.02) than those with negative OMC (Fig. 3e and f). There were no statistical significances of PFS (p = 0.53) and OS (p = 0.36) between patients with or without positive CK5/6, CD24, and EGFR. However, there were no statistically significant differences between other proteins and the prognosis.
Table 3.
The results of immunohistochemistry staining for ovarian mucinous carcinoma
| Ovarian mucinous carcinoma with infiltrative invasion |
Ovarian mucinous carcinoma with expansile invasion |
p-Value | ||||
|---|---|---|---|---|---|---|
| Molecule | n = 25 | n = 24 | ||||
| CK7 (n (%)) | Positive | 24 | (96.0) | 24 | (100.0) | 0.99 |
| Negative | 1 | (4.0) | 0 | (0.0) | ||
| CK20 (n (%)) | Positive | 11 | (44.0) | 15 | (62.5) | 0.24 |
| Negative | 14 | (56.0) | 9 | (37.5) | ||
| CDX2 (n (%)) | Positive | 21 | (84.0) | 23 | (95.8) | 0.35 |
| Negative | 4 | (16.0) | 1 | (4.2) | ||
| HER-2 (n (%)) | Positive | 7 | (28.0) | 10 | (41.7) | 0.38 |
| Negative | 18 | (72.0) | 14 | (58.3) | ||
| CK 5/6 (n (%)) | Positive | 9 | (36.0) | 1 | (4.2) | 0.01 |
| Negative | 16 | (64.0) | 23 | (95.8) | ||
| Androgen receptor (n (%)) | Positive | 2 | (8.0) | 0 | (0.0) | 0.49 |
| Negative | 23 | (92.0) | 24 | (100.0) | ||
| ALDH1 (n (%)) | Positive | 9 | (36.0) | 10 | (41.7) | 0.77 |
| Negative | 16 | (64.0) | 14 | (58.3) | ||
| CD24 (n (%)) | Positive | 6 | (24.0) | 0 | (0.0) | 0.02 |
| Negative | 19 | (76.0) | 24 | (100.0) | ||
| CD133 (n (%)) | Positive | 8 | (32.0) | 5 | (20.8) | 0.52 |
| Negative | 17 | (68.0) | 19 | (79.2) | ||
| PD-1 (n (%)) | Positive | 2 | (8.0) | 0 | (0.0) | 0.49 |
| Negative | 23 | (92.0) | 24 | (100.0) | ||
| PD-L1 (n (%)) | Positive | 6 | (24.0) | 6 | (25.0) | 0.99 |
| Negative | 19 | (76.0) | 18 | (75.0) | ||
| ZEB1 (n (%)) | Positive | 1 | (4.0) | 1 | (4.2) | 0.99 |
| Negative | 24 | (96.0) | 23 | (95.8) | ||
| c-Met (n (%)) | Positive | 6 | (24.0) | 4 | (16.7) | 0.73 |
| Negative | 19 | (76.0) | 20 | (83.3) | ||
| EGFR (n (%)) | Positive | 7 | (28.0) | 0 | (0.0) | < 0.01 |
| Negative | 18 | (72.0) | 24 | (100.0) | ||
| Snail-2 (n (%)) | Positive | 1 | (4.0) | 1 | (4.2) | 0.99 |
| Negative | 24 | (96.0) | 23 | (95.8) | ||
Abbreviations: CK7 Cytokeratin 7, CK20 Cytokeratin 20, CDX2 Caudal type homeobox 2, HER-2 Human epidermal growth factor receptor 2, CK5/6 Cytokeratin 5/6, ALDH1 Aldehyde dehydrogenase 1, CD24 Cluster of differentiation 24, CD133 Cluster of differentiation 133, PD-1 Programmed cell death 1, PD-L1 Programmed cell death 1- ligand 1, ZEB1 Zinc finger E-box binding homeobox 1, EGFR Epithelial growth factor receptor
Fig. 3.
PFS and OS curves according to CK5/6, CD24, and EGFR status
a PFS curves of cases according to the CK5/6 status. Cases which were positive for CK5/6 had significantly worse prognosis about PFS. b OS curves of cases according to the CK5/6 status. There was no statistical significance between 2 groups. c PFS curves of cases according to the CD24 status. There was no statistical significance between 2 groups. d OS curves of cases according to the CD24 status. There was no statistical significance between 2 groups. e PFS curves of cases according to the EGFR status. Cases which were positive for EGFR had significantly worse prognosis about PFS. f OS curves of cases according to the EGFR status. Cases which were positive for EGFR had significantly worse prognosis about OS
Discussion
In our study, 25 (51.0 %) cases with infiltrative invasion and 24 (49.0 %) cases with expansile invasion were included. The cases with infiltrative invasion were more frequently treated with adjuvant chemotherapy and more often showed recurrence. Furthermore, the PFS and OS of cases with infiltrative invasion were worse than those of cases with expansile invasion; multivariate analysis revealed that infiltrative invasion was a negative prognostic factor for PFS and OS. In addition, immunohistochemical staining revealed that CK5/6, CD24, and EGFR were related to infiltrative invasion compared with expansile invasion.
The findings of the review of literature reports published from 2000, including the present study, on the invasive patterns of OMC identified through a pathological review are shown in Table 4 [15–19]. According to our review, infiltrative invasion was relatively frequently diagnosed (135 of 250 cases, 54 %). Furthermore, the cases with an infiltrative invasion pattern were discovered at a more advanced stage (p < 0.01), had a higher recurrence rate (40 % vs. 7 %, p < 0.01), had a higher mortality rate (33 % vs. 9 %, p < 0.01), and showed worse prognoses than cases with expansile invasion. Thus, although previous reports identified OMC as type I OC and a nonaggressive tumor [8, 9], OMC with infiltrative invasion was considered to be an aggressive subtype.
Table 4.
Findings of literature review on invasive patterns of ovarian mucinous carcinoma including the present study
| Authors | Total no. of cases | No. of cases in each invasive pattern (%) | FIGO stage | p-Value | Recurrence (%) | p-Value | Prognosis | p-Value | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II–IV | Alive with and without diseases | Death due to diseases or any reason | ||||||||
| Lee and Scully [15] | 21 | Infiltrative invasion | 11 (52) | 5 (46) | 6 (54) | 0.01 | 6 (54) | 0.01 | 5 (46) | 6 (54) | 0.01 |
| Expansile invasion | 10 (48) | 10 (100) | 0 (0) | 0 (0) | 10 (100) | 0 (0) | |||||
| Rodriguez and Prat [16] | 26 | Infiltrative invasion | 15 (58) | 9 (60) | 6 (40) | 0.02 | 9 (60) | < 0.01 | 7 (47) | 8 (53) | 0.04 |
| Expansile invasion | 11 (42) | 11 (100) | 0 (0) | 0 (0) | 10 (91) | 1 (9) | |||||
| Muyldermans et al. [17] | 44 | Infiltrative invasion | 21 (48) | 12 (57) | 9 (43) | 0.01 | 9 (43) | 0.01 | 12 (57) | 9 (43) | 0.04 |
| Expansile invasion | 23 (52) | 21 (91) | 2 (9) | 2 (9) | 20 (87) | 3 (13) | |||||
| Khunamornpong et al. [18] | 46 | Infiltrative invasion | 28 (61) | 22 (79) | 6 (21) | 0.07 | 11 (39) | 0.02 | 20 (71) | 8 (29) | 0.07 |
| Expansile invasion | 18 (39) | 18 (100) | 0 (0) | 1 (6) | 17 (94) | 1 (6) | |||||
| Gouy et al. [19] | 64 | Infiltrative invasion | 35 (55) | 35 (100) | - | - | 6 (17) | 0.49 | 31 (89) | 4 (11) | 0.37 |
| Expansile invasion | 29 (45) | 29 (100) | - | 3 (10) | 28 (97) | 1 (3) | |||||
| Present study | 49 | Infiltrative invasion | 25 (51) | 16 (64) | 9 (36) | 0.2 | 13 (52) | < 0.01 | 15 (60) | 10 (40) | 0.11 |
| Expansile invasion | 24 (49) | 20 (83) | 4 (17) | 2 (8) | 20 (87) | 4 (13) | |||||
| Total | 250 | Infiltrative invasion | 135 (54) | 99 (73) | 36 (27) | < 0.01 | 54 (40) | < 0.01 | 90 (67) | 45 (33) | < 0.01 |
| Expansile invasion | 115 (46) | 109 (95) | 6 (5) | 8 (7) | 105 (91) | 10 (9) | |||||
The diagnosis of OMC is cumbersome. The metastatic carcinomas from other sites are often misdiagnosed as primary OMC because of the histological resemblance between these tumors [10, 21]. In fact, out of the cases initially diagnosed as OMC, 50–70 % were diagnosed with metastatic carcinoma after a pathological review [10]. In our study, 4 of 81 (5 %) cases were diagnosed with metastatic carcinoma originating from the appendix. The number of metastatic carcinoma cases was lower in this study than in previous reports because we preoperatively performed gastroscopy and colonofiberscopy in addition to the detailed examination of the appendix by a digestive surgeon. Furthermore, ovarian borderline tumors are often misdiagnosed as primary OMC [22]. Previous reports show that OMC often exhibits a continuum of differentiation from benign epithelium to borderline malignancy to invasive carcinoma, and ovarian mucinous borderline tumors resemble invasive well-differentiated OMCs [22, 23]. In our study, the diagnosis of 18 of 81 (22 %) cases was changed from OMC to ovarian mucinous borderline tumors, which indicated the difficulty in the diagnosis. However, the association between CK5/6, CD24, and EGFR and invasive patterns was identified. These markers might be useful as biomarkers for diagnosis.
In a previous report, high-grade serous carcinoma was classified into four molecular subtypes, which were related to the prognosis [24]. A subsequent report showed the relationship between the histopathological classification and prognostically distinct gene expression subtypes of HGSC [25]. In the case of OMC, several gene mutations or amplifications have been reported [10]. HER-2 amplification/overexpression and KRAS mutation in OMC were reported to be associated with a decreased likelihood of disease recurrence or death [26]. Furthermore, an association between HER-2 expression and invasive patterns has been reported [27]. However, this relationship was not observed in our study.
CK5/6 was consistently expressed in the stratified epithelia and derived neoplasms, such as squamous cell carcinoma and was related to the prognosis of ovarian carcinoma [28, 29]. CD24 is one of the ovarian cancer stem cell markers, and the overexpression of CD24 in OCs was associated with a more aggressive phenotype and increased metastasis and invasion capacity [30–32]. EGFR is a growth-factor-receptor tyrosine kinase that is related to transformation of cellular phenotypes and growth and survival of tumor cells [33]. Additionally, EGFR was associated with poor overall and disease-free survival outcomes [34]. Our study showed that OMC with infiltrative invasion was more frequently positive for CK5/6, CD24, and EGFR, which might suggest that CK5/6, CD24, and EGFR were associated with the aggressive features of OMC with infiltrative invasion. Additionally, the EGFR status was associated with worse prognoses, and EGFR inhibitors might be a new strategy for OMC with infiltrative invasion.
In several previous report, the diagnosis of mucinous carcinoma was difficult because benign tumors, borderline tumors, and invasive carcinomas could coexist, and appropriate sampling of tissue was needed to diagnose small areas of invasion due to large size [23, 35–38]. In our study, OMC with infiltrative invasion was positive for CK5/6, CD24, and EGFR and these makers might be useful for the diagnostic biomarker.
This study had some limitations, including the small sample size from a single institution and retrospective analysis. As a result, our study included a small number of cases; however, our study had a large sample size relative to several other reports. Further large-scale studies are needed to confirm the clinical significance of OMC in the future.
Conclusions
The invasive patterns were associated with prognoses, as previous reports have shown. Particularly, OMC with an infiltrative pattern showed worse prognoses and positive for CK5/6, CD24, and EGFR. Also, EGFR was related with the worse prognosis. These biomarkers may be useful for the development of new treatment strategy and diagnostic biomarker in the clinical practice.
Methods
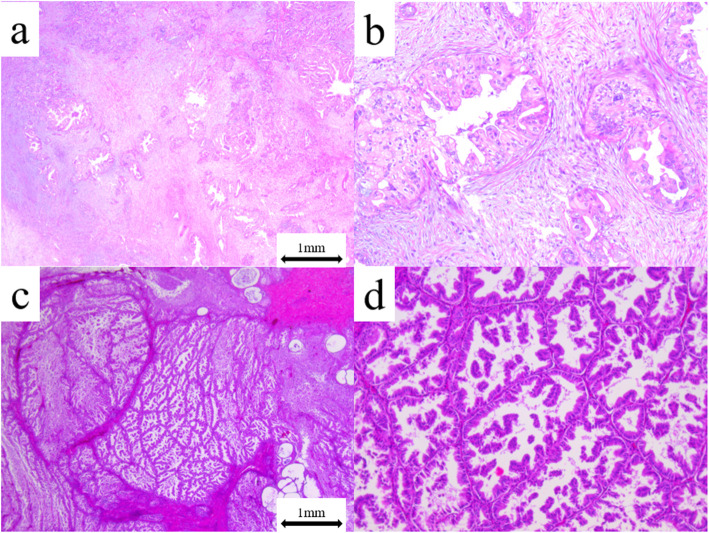
Patients with OMC who underwent a minimum of unilateral salpingo-oophorectomy and resection of the primary lesion at our hospital between 1984 and 2018 were identified. Those without clinical information or surgical tissue were excluded. A pathological review was conducted using the 2020 WHO criteria [14], and cases with infiltrative invasion and those with expansile invasion were identified. Briefly, infiltrative invasion was defined as a destructive stromal invasion by malignant glands, cell nests, or individual cells with a desmoplastic stromal reaction. Expansile invasion was defined as a confluent glandular growth pattern with little intervention of normal ovarian stroma (minimal or no stromal invasion). The representative images of infiltrative invasion and expansile invasion of OMC are shown in Fig. 4.
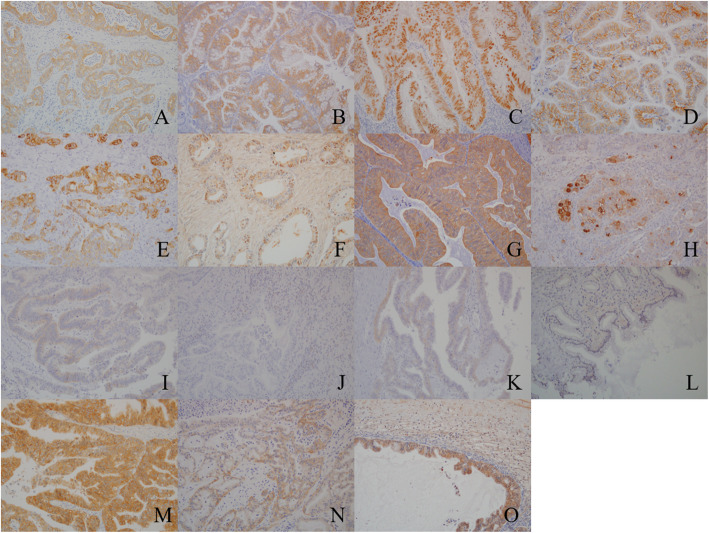
Fig. 4.
Representative images of ovarian mucinous carcinoma (OMC) with infiltrative invasion and expansile invasion
a OMC with infiltrative invasion was defined as obvious evidence of destructive stromal invasion measuring > 5 mm in the greatest linear extent (x 20). b Stromal invasion was associated with malignant glands, cell nests, and a desmoplastic stromal reaction (x 100). c OMC with expansile invasion was defined as marked glandular crowding with little intervening stroma, creating a labyrinthine appearance with little intervening normal ovarian stroma (x 10). d A cribriform pattern was present (x 100)
Formalin-fixed paraffin-embedded tissues were used for immunohistochemistry. All the slides were deparaffinized and rehydrated using graded ethanol series. The endogenous peroxidase activity was blocked by adding methanol to 0.3 % hydrogen peroxidase. Antigen retrieval was performed using citrate buffer (pH 6.0) and Tris/EDTA buffer (pH 9.0). Additionally, all the slides were boiled in an autoclave at 121°C for 5 min in a citrate buffer or in Tris/EDTA buffer at 98°C for 40 min. The primary antibodies are listed in Table 5. All the slides were incubated with these antibodies at room temperature for 24 h. Following incubation, the samples were reacted with the DAKO EnVision + system-HRP labeled polymer as a secondary antibody for 30 min at room temperature. Specific antigen-antibody reactions were visualized with 0.2 % diaminobenzidine tetrahydrochloride and hydrogen peroxide and counterstained with Mayer’s hematoxylin. The control tissue sections and interpretations for each antibody are listed in Table 5. In case of the presence of tumor cells, the representative images of positive cells from each immunohistochemical staining are shown in Fig. 5.
Table 5.
Primary antibodies
| Molecule | Type | Antibody Clone/Code | Manufacturer | Dilution | Localization | Control tissue | Antigen retrieval | Interpretation |
|---|---|---|---|---|---|---|---|---|
| CK7 | Monoclonal (Mouse) | OV-TL12/30 | Dako | x50 | Cytoplasm | Colorectal carcinoma | Citrate | More than 10 % positive cell with staining intensity score 1 to 3 was defined as positive. |
| CK20 | Monoclonal (Mouse) | Ks20.8 | Dako | x50 | Cytoplasm | Colorectal carcinoma | Citrate | More than 10 % positive cell with staining intensity score 1 to 3 was defined as positive. |
| CDX2 | Monoclonal (Rabbit) | CDX2-88 | Novocastra | x100 | Nucleus | Colon | Citrate | More than 10 % positive cell with staining intensity score 1 to 3 was defined as positive. |
| HER-2 | Monoclonal (Rabbit) | 4B5 | Ventana medical system | Ready to use | Membrane | Mammary gland | Citrate | More than 10 % positive cell with staining intensity score 1 to 3 was defined as positive. |
| CK 5/6 | Monoclonal (Mouse) | D5/13 B4 | Dako | x100 | Cytoplasm | Mammary gland | EDTA | More than 10 % positive cell with staining intensity score 1 to 3 was defined as positive. |
| Androgen receptor | Monoclonal (Mouse) | AR441 | Dako | x50 | Nucleus | Mammary gland | Citrate | More than 10 % positive cell with staining intensity score 1 to 3 was defined as positive. |
| ALDH1 | Monoclonal (Mouse) | clone 44 | BD Biosciences | x500 | Cytoplasm | Kidney | Citrate | More than 10 % positive cell with staining intensity score 1 to 3 was defined as positive. |
| CD24 | Monoclonal (Mouse) | SN3 | ThermoFisher | x25 | Membrane | Tonsil | Citrate | More than 10 % positive cell with staining intensity score 1 to 3 was defined as positive. |
| CD133 | Monoclonal (Mouse) | AC133/1 | Miltenyi Biotec | x500 | Cytoplasm | Colorectal carcinoma | EDTA | More than 10 % positive cell with staining intensity score 1 to 3 was defined as positive. |
| PD-1 | Monoclonal (Mouse) | NAT105 | Abcam | x50 | lymphocytes | Tonsil | Citrate | Even minimally positive lymphocyte with staining intensity score 1 to 3 was defined as positive. |
| PD-L1 | Monoclonal (Rabbit) | EPR19759 | Abcam | x250 | Membrane and endomembrane | Placenta | Citrate | More than 10 % positive cell with staining intensity score 1 to 3 was defined as positive. |
| ZEB1 | Polyclonal (Rabbit) | ab87280 | Abcam | x100 | Nucleus | MCF, MDA-MB-231 | EDTA | More than 1 % positive cell with staining intensity score 1 to 3 was defined as positive. |
| c-Met | Monoclonal (Rabbit) | D1C2 | Cell Signaling Technology | x300 | Membrane and cytoplasm | Colorectal carcinoma | Citrate | More than 10 % positive cell with staining intensity score 1 to 3 was defined as positive. |
| EGFR | Monoclonal (Rabbit) | D38B1 | Cell Signaling Technology | x100 | Membrane | Epidermis | EDTA | More than 10 % positive cell with staining intensity score 2 or 3 was defined as positive. |
| Snail-2 | Polyclonal (Rabbit) | PAB1923 | Abnova | x200 | Nucleus | MCF, MDA-MB-231 | Citrate | More than 10 % positive cell with staining intensity score 1 or 3 was defined as positive. |
Abbreviation: CK7 Cytokeratin 7, CK20 Cytokeratin 20, CDX2 Caudal type homeobox 2, HER-2 Human epidermal growth factor receptor 2, CK5/6 Cytokeratin 5/6, ALDH1 Aldehyde dehydrogenase 1, CD24 Cluster of differentiation 24, CD133 Cluster of differentiation 133, PD-1 Programmed cell death 1, PD-L1 Programmed cell death 1- ligand 1, ZEB1 Zinc finger E-box binding homeobox 1, EGFR Epithelial growth factor receptor
Fig. 5.
Representative images of positive cells of each immunohistochemistry
a Cytokeratin 7 (x200); b Cytokeratin 20 (x200); c Caudal type homeobox 2 (x200); d Human epidermal growth factor receptor 2 (x200); e Cytokeratin 5/6 (x200); f Androgen receptor (x200); g Aldehyde dehydrogenase 1 (x200); h Cluster of differentiation 24 (x200); i Cluster of differentiation 133 (x200); j Programmed cell death 1 (x200); k Programmed cell death 1- ligand 1 (x200); l Zinc finger E-box binding homeobox 1 (x200); m Met (x200); n Epithelial growth factor receptor (x200); o Snail-2 (x200)
Proportion score, defined as the percentage of cells in carcinoma tissues, was as follows:0, no tumor cells stained in entire carcinoma tissue; 1+, form ≥ 1 % to < 10 % cells stained in entire carcinoma tissue; 2+, from ≥ 10 % to < 50 %; 3+, ≥ 50 %. Staining intensity score is defined as follows:0, no tumor cells stained in entire carcinoma tissue; 1+, incomplete staining and/or faint or barely perceptible cytoplasmic staining detected; 2+, entire carcinoma cells stained and/or moderate to strong staining. Immunochemical interpretation was listed Table 5.
According to the protocol at our hospital, all the patients preoperatively underwent gastroscopy and colonofiberscopy to exclude the metastatic OC originating from the gastrointestinal tract. Furthermore, when swelling of the appendix was observed intraoperatively, resection of the appendix was performed by a digestive surgeon to exclude appendiceal cancer.
Clinical information was obtained from the medical records. The tumor stage was reevaluated according to the 2014 FIGO criteria [3]. The standard surgery was bilateral salpingo-oophorectomy with hysterectomy, omentectomy, or multiple peritoneal biopsy and lymphadenectomy. The residual tumor was evaluated using the operation records after the primary surgery. The Response Evaluation Criteria in Solid Tumors version 1.1 [39] were used to evaluate the treatment effectiveness. Progression-free survival (PFS) was defined as the period from the day of PDS to the day of death or recurrence/progression of the disease. Overall survival (OS) was defined as the period from the day of PDS to the day of death or the last confirmation of survival.
Statistical analysis was performed using JMP Pro 14 software (SAS Institute Inc., Cary, NC, USA). The chi-square test, Fisher’s exact test, Mann-Whitney U test, and Wilcoxon test were used to evaluate the clinical significance of the clinicopathological factors. The PFS and OS curves were generated using the Kaplan-Meier method. The survival distribution was compared using the log-rank test. Univariate and multivariate analysis was performed by cox proportional hazard regression models. Firstly, Univariate analysis for PFS and OS was performed with several factors. Secondly, multivariate analysis for PFS and OS was done using the only factors with statistical significances by univariate analysis as the parameter. Statistical significance was defined as p < 0.05. This study was approved by the Ethics Committee of the National Defense Medical College, Tokorozawa, Japan.
Acknowledgements
We would like to thank Editage (www.editage.jp) for their English language editing services.
Abbreviations
- OC
Ovarian carcinoma
- FIGO
The International Federation of Gynecology and Obstetrics
- OMC
Ovarian mucinous carcinoma
- CK
Cytokeratin
- CD
Cluster of differentiation
- EGFR
Epithelial growth factor receptor
- PFS
Progression free survival
- PDS
Primary debulking surgery
- OS
Overall survival
- CK
Cytokeratin
- CD
Cluster of differentiation
- EGFR
Epithelial growth factor receptor
Authors’ contributions
TH, MM, and MT contributed to protocol/project development. HI, HM, TS, SK, and HI contributed to data collection and management. TH, MM, and HT performed data analysis. TH, MM, and MT wrote and edited the manuscript. The author(s) read and approved the final manuscript.
Funding
This study was conducted without any financial support.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article.
Ethics approval and consent to participate
This study was approved by the institutional review board of the National Defense Medical College, Tokorozawa, Japan. Records/information of all women in the study were completely anonymized and de-identified prior to analysis. The present study was exempt from collecting informed consent from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Webb PM, Jordan SJ. Epidemiology of epithelial ovarian cancer. Best Pract Res Clin Obstet Gynaecol. 2017;41:3–14. doi: 10.1016/j.bpobgyn.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Kossaï M, Leary A, Scoazec JY, Genestie C. Ovarian cancer: a heterogeneous disease. Pathobiology. 2018;85:41–9. doi: 10.1159/000479006. [DOI] [PubMed] [Google Scholar]
- 3.Pereira A, Pérez-Medina T, Magrina JF, Magtibay PM, Rodríguez-Tapia A, Peregrin I, et al. International Federation of Gynecology and Obstetrics staging classification for cancer of the ovary, fallopian tube, and peritoneum: estimation of survival in patients with node-positive epithelial ovarian cancer. Int J Gynecol Cancer. 2015;25:49–54. doi: 10.1097/IGC.0000000000000316. [DOI] [PubMed] [Google Scholar]
- 4.du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomizes phase 3 multicenter trials. Cancer. 2009;115:1234–44. doi: 10.1002/cncr.24149. [DOI] [PubMed] [Google Scholar]
- 5.Chi DS, Eisenhauer EL, Lang J, Huh J, Haddad L, Abu-Rustum NR, et al. What is the optimal goal of primary cytoreductive surgery for bulky stage IIIC epithelial ovarian carcinoma (EOC)? Gynecol Oncol. 2006;103:559–64. doi: 10.1016/j.ygyno.2006.03.051. [DOI] [PubMed] [Google Scholar]
- 6.Terauchi F, Nishi H, Moritake T, Kobayashi Y, Nagashima T, Onodera T, et al. Prognostic factor on optimal debulking surgery by maximum effort for stage IIIC epithelial ovarian cancer. J Obstet Gynaecol Res. 2009;35:315–9. doi: 10.1111/j.1447-0756.2008.00928.x. [DOI] [PubMed] [Google Scholar]
- 7.Chi DS, Eisenhauer EL, Zivanovic O, Sonoda Y, Abu-Rustum NR, Levine DA, et al. Improved progression-free and overall survival in advanced ovarian cancer as a result of a change in surgical paradigm. Gynecol Oncol. 2009;114:26–31. doi: 10.1016/j.ygyno.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 8.Kurman RJ, Shih IeM. The origin and pathogenesis of epithelial ovarian cancer: a proposed unifying theory. Am J Surg Pathol. 2010;34:433–43. doi: 10.1097/PAS.0b013e3181cf3d79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurman RJ, Shih IeM. The dualistic model of ovarian carcinogenesis: revisited, revised, and expanded. Am J Pathol. 2016;186:733–47. doi: 10.1016/j.ajpath.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perren TJ. Mucinous epithelial ovarian carcinoma. Ann Oncol. 2016;27(Suppl 1):i53–7. doi: 10.1093/annonc/mdw087. [DOI] [PubMed] [Google Scholar]
- 11.Morice P, Gouy S, Leary A. Mucinous ovarian carcinoma. N Engl J Med. 2019;380:1256–66. doi: 10.1056/NEJMra1813254. [DOI] [PubMed] [Google Scholar]
- 12.Simons M, Ezendam N, Bulten J, Nagtegaal I, Massuger L. Survival of patients with mucinous ovarian carcinoma and ovarian metastasis: a population-based cancer registry study. Int J Gynecol Cancer. 2015;25:1208–15. doi: 10.1097/IGC.0000000000000473. [DOI] [PubMed] [Google Scholar]
- 13.Hess V, A’Hern R, Nasiri N, King DM, Blake PR, Barton DP, et al. Mucinous epithelial ovarian cancer: a separate entity requiring specific treatment. J Clin Oncol. 2004;22:1040–4. doi: 10.1200/JCO.2004.08.078. [DOI] [PubMed] [Google Scholar]
- 14.WHO classification of tumors editorial board . female Ge nital Organs. 5. Lyon: International Agency for Research on Cancer; 2020. [Google Scholar]
- 15.Lee KR, Scully RE. Mucinous tumors of the ovary: a clinicopathologic study of 196 borderline tumors (of intestinal type) and carcinomas, including an evaluation of 11 cases with ’pseudomyxoma peritonei’. Am J Surg Pathol. 2000;24:1447–64. doi: 10.1097/00000478-200011000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Rodríguez IM, Prat J. Mucinous tumors of the ovary: a clinicopathologic analysis of 75 borderline tumors (of intestinal type) and carcinomas. Am J Surg Pathol. 2002;26:139–52. doi: 10.1097/00000478-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Muyldermans K, Moerman P, Amant F, Leunen K, Neven P, Vergote I. Primary invasive mucinous ovarian carcinoma of the intestinal type: importance of the expansile versus infiltrative type in predicting recurrence and lymph node metastasis. Eur J Cancer. 2013;49:1600–8. doi: 10.1016/j.ejca.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Khunamornpong S, Settakorn J, Sukpan K, Suprasert P, Siriaunkgul S. Primary ovarian mucinous adenocarcinoma of intestinal type: a clinicopathologic study of 46 cases. Int J Gynecol Pathol. 2014;33:176–85. doi: 10.1097/PGP.0b013e318289452e. [DOI] [PubMed] [Google Scholar]
- 19.Gouy S, Saidani M, Maulard A, Bach-Hamba S, Bentivegna E, Leary A, et al. Characteristics and Prognosis of Stage I Ovarian Mucinous Tumors According to Expansile or Infiltrative Type. Int J Gynecol Cancer. 2018;28:493–9. doi: 10.1097/IGC.0000000000001202. [DOI] [PubMed] [Google Scholar]
- 20.Brown J, Frumovitz M. Mucinous tumors of the ovary: current thoughts on diagnosis and management. Curr Oncol Rep. 2014;16:389. doi: 10.1007/s11912-014-0389-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seidman JD, Kurman RJ, Ronnett BM. Primary and metastatic mucinous adenocarcinomas in the ovaries: incidence in routine practice with a new approach to improve intraoperative diagnosis. Am J Surg Pathol. 2003;27:985–93. doi: 10.1097/00000478-200307000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Matsuo K, Machida H, Mandelbaum RS, Grubbs BH, Roman LD, Sood AK, et al. Mucinous borderline ovarian tumor versus invasive well-differentiated mucinous ovarian cancer: difference in characteristics and outcomes. Gynecol Oncol. 2019;153:230–7. doi: 10.1016/j.ygyno.2019.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prat J, D’Angelo E, Espinosa I. Ovarian carcinomas: at least five different diseases with distinct histological features and molecular genetics. Hum Pathol. 2018;80:11–27. doi: 10.1016/j.humpath.2018.06.018. [DOI] [PubMed] [Google Scholar]
- 24.Cancer Genome Atlas Research Network Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474:609–15. doi: 10.1038/nature10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murakami R, Matsumura N, Mandai M, Yoshihara K, Tanabe H, Nakai H, et al. Establishment of a novel histopathological classification of high-grade serous ovarian carcinoma correlated with prognostically distinct gene expression subtypes. Am J Pathol. 2016;186:1103–13. doi: 10.1016/j.ajpath.2015.12.029. [DOI] [PubMed] [Google Scholar]
- 26.Anglesio MS, Kommoss S, Tolcher MC, Clarke B, Galletta L, Porter H, et al. Molecular characterization of mucinous ovarian tumors supports a stratified treatment approach with HER2 targeting in 19 % of carcinoma. J Pathol. 2013;229:111–20. doi: 10.1002/path.4088. [DOI] [PubMed] [Google Scholar]
- 27.Kim SK, Cho NH. HER-2 positive mucinous adenocarcinomas of the ovary have an expansile invasion pattern associated with a favorable prognosis. Int J Clin Exp Pathol. 2014;7:4222–30. [PMC free article] [PubMed] [Google Scholar]
- 28.Taube ET, Denkert C, Sehouli J, Unger U, Kunze CA, Budczies J, et al. Cytokeratin 5/6 expression, prognosis, and association with estrogen receptor alpha in high-grade serous ovarian carcinoma. Hum Pathol. 2017;67:30–6. doi: 10.1016/j.humpath.2017.03.020. [DOI] [PubMed] [Google Scholar]
- 29.Chu PG, Weiss LM. Expression of cytokeratin 5/6 in epithelial neoplasms: an immunohistochemical study of 509 cases. Mod Pathol. 2002;15(1):6–10. doi: 10.1038/modpathol.3880483. [DOI] [PubMed] [Google Scholar]
- 30.Akbari-Birgani S, Paranjothy T, Zuse A, Janikowski T, Cieślar-Pobuda A, Likus W, et al. Cancer stem cells, cancer-initiating cells and methods for their detection. Drug Discov Today. 2016;21:836–42. doi: 10.1016/j.drudis.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 31.Gao MQ, Choi YP, Kang S, Youn JH, Cho NH. CD24 + cells from hierarchically organized ovarian cancer are enriched in cancer stem cells. Oncogene. 2010;29:2672–80. doi: 10.1038/onc.2010.35. [DOI] [PubMed] [Google Scholar]
- 32.Tarhriz V, Bandehpour M, Dastmalchi S, Ouladsahebmadarek E, Zarredar H, Eyvazi S. Overview of CD24 as a new molecular marker in ovarian cancer. J Cell Physiol. 2019;234:2134–42. doi: 10.1002/jcp.27581. [DOI] [PubMed] [Google Scholar]
- 33.Huang SM, Harari PM. Epidermal growth factor receptor inhibition in cancer therapy: biology, rationale and preliminary clinical results. Investig New Drugs. 1999;17:259–69. doi: 10.1023/A:1006384521198. [DOI] [PubMed] [Google Scholar]
- 34.Psyrri A, Kassar M, Yu Z, Bamias A, Weinberger PM, Markakis S, et al. Effect of epidermal growth factor receptor expression level on survival in patients with epithelial ovarian cancer. Clin Cancer Res. 2005;11:8637–43. doi: 10.1158/1078-0432.CCR-05-1436. [DOI] [PubMed] [Google Scholar]
- 35.Prat J. Pathology of borderline and invasive cancers. Best Pract Res Clin Obstet Gynaecol. 2017;41:15–30. doi: 10.1016/j.bpobgyn.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 36.Perren TJ. Mucinous epithelial ovarian carcinoma. Ann Oncol. 2016;27:i53-7. doi: 10.1093/annonc/mdw087. [DOI] [PubMed] [Google Scholar]
- 37.Ludwick C, Gilks CB, Miller D, Yaziji H, Clement PB. Aggressive behavior of stage I ovarian mucinous tumors lacking extensive infiltrative invasion: a report of four cases and review of the literature. Int Gynecol Pathol. 2005;24:205–17. doi: 10.1097/01.pgp.0000159935.38913.57. [DOI] [PubMed] [Google Scholar]
- 38.Yemelyanova AV, Vang R, Judson K, Wu LS, Ronnett BM. Distinction of primary and metastatic mucinous tumors involving the ovary: analysis of size and laterality data by primary site with reevaluation of an algorithm for tumor classification. Am J Surg Pathol. 2008;32:128–38. doi: 10.1097/PAS.0b013e3180690d2d. [DOI] [PubMed] [Google Scholar]
- 39.Schwartz LH, Bogaerts J, Ford R, Shankar L, Therasse P, Gwyther S, et al. Evaluation of lymph nodes with RECIST 1.1. Eur J Cancer. 2009;45:261–7. doi: 10.1016/j.ejca.2008.10.028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is included within the article.