Abstract
The botulinum neurotoxin, the caustic agent that causes botulism, is the most lethal toxin known to man. The neurotoxin composed of a heavy chain (HC) and a light chain (LC) enters neurons and cleaves SNARE proteins, leading to flaccid paralysis, which, in severe occurrences, can result in death. A therapeutic target for botulinum neurotoxin (BoNT) intoxication is the LC, a zinc metalloprotease that directly cleaves SNARE proteins. Herein we report dipeptides containing an aromatic connected to the N-terminus via a sulfonamide and a hydroxamic acid at the C-terminus as BoNT/A LC inhibitors. On the basis of a structure–activity relationship study, 33 was discovered to inhibit the BoNT/A LC with an IC50 of 21 nM. X-ray crystallography analysis of 30 and 33 revealed that the dipeptides inhibit through a competitive mechanism and identified several key intermolecular interactions.
Keywords: Dipeptide, botulinum neurotoxin, protease inhibitor, hydroxamic acid
The botulinum neurotoxin (BoNT) is a metabolic byproduct of the Clostridium botulinum bacteria and causes the paralytic disease botulism. In humans, botulism is commonly caused by the consumption of improperly processed foods (i.e., meats and canned food) contaminated with the BoNT or by the consumption of the bacteria, which grows in the intestinal tract and releases the toxin.1,2 There are seven serotypes of the toxin categorized A–G, with BoNT/A being the most toxic, with an LD50 of 1.3 ng/kg in humans, making it the most lethal toxin known to man.3,4 It is estimated that ∼1 g of BoNT/A can kill 1 million people.5,6 This has elevated BoNT as a potential bioterrorism weapon7,8 due to the high toxicity and ease of producing the toxin. BoNT has several clinical applications to treat neuromuscular and neuronal diseases;1 however, overexposure can lead to intoxication, even when using controlled clinical doses. The current countermeasures available for BoNT intoxication are antitoxins, but they have many drawbacks, such as a limited treatment window (>48 h post exposure)9 once infected. In addition, the dangerous side effects9 and the high cost of producing the antitoxins highlight their issues and demonstrate that they would not be an ideal treatment during a widespread biological attack.7,8 Therefore, new therapeutics, specifically small molecules that are more cost effective and can enter cells to increase the treatment window, are urgently needed to counter the deadly effects of a potential large-scale BoNT outbreak.
The neurotoxin is composed of a 100 kDa heavy chain (HC) and 50 kDa light chain (LC) linked by a single disulfide bond.1,10,11 The HC is composed of two active domains, a translocation domain at the N-terminus and a binding domain at the C-terminus.1 The binding domain recognizes neurons by binding to a ganglioside and a protein receptor.1,11 The translocation domain inserts the LC, a Zn2+-dependent metalloprotease, into the cytosol of neurons and is a critical step for intoxication.12 Upon internalization into the neuron cytosol, BoNT/A LC cleaves the synaptosome-associated protein (SNAP-25).1 SNAP-25, vesicle-associated membrane protein (VAMP), and syntaxin make up the SNARE protein complex that is required for docking of synaptic vesicles to the nerve terminal for the controlled release of acetylcholine into the neuromuscular junction for normal neuromuscular and autonomic functions.12 The cleavage of a single SNARE protein by the BoNT inhibits the formation of the SNARE complex and halts the release of acetylcholine, leading to flaccid muscle paralysis.1,10,11,13 Severe cases of intoxication lead to cardiac and respiratory failure and eventually death.
Small-molecule therapeutics are advantageous for the treatment of BoNT intoxication on a large scale and would provide relief for BoNT intoxication even after the neurotoxin has entered the cell.14,15 A promising small-molecule therapeutic target for BoNT/A intoxication is the LC.14,16,17 A variety of molecules have been reported to bind and inhibit the proteolytic activity of the LC.15,18
Our laboratory previously discovered a novel molecular scaffold for BoNT/A LC inhibition,19 with our best inhibitor having an IC50 value of 0.54 μM against the BoNT/A LC.20 In the present study we have expanded on our amino scaffold by incorporating a second amino acid. The dipeptide includes a hydroxamic acid at the C-terminus, two amino acids with hydrophobic side chains, and a sulfonamide at the N-terminus connecting an aromatic. Reported peptide BoNT/A LC inhibitors are composed of polar amino acid sequences, such as arginine, to interact with zinc and other polar residues in the active site.21−24 The dipeptides in this work include a hydroxamic acid at the C-terminus to chelate with zinc. The hydroxamic acid is a known metal chelator25 and a common chemical warhead for BoNT/A LC inhibitors.14,18,26,27 The hydroxamic acid and N-terminus sulfonamide in our dipeptides will provide the polar contacts. We propose that the hydrophobic amino acid side chains are better suited for BoNT/A LC inhibitors, as they can maximize the interactions with the large hydrophobic active site.24,27 In addition, the aromatic group attached to the sulfonamide will be available for pi-stacking and additional hydrophobic interactions.
Dipeptides have the potential to be developed into therapeutic treatments. There are several current drugs that contain a dipeptide scaffold, such as enalapril, lisinopril, and spriapril, which are angiotensin-converting enzyme (ACE) inhibitors. The pharmacokinetics of dipeptides are better than those of larger peptides due to intestinal cellular transporters that are specific for di- and tripeptides and have been shown to be responsible for the absorption of several dipeptide drugs.28−30 Furthermore, dipeptides have been shown to cross the blood–brain barrier,31 which would be advantageous for botulism therapeutics. Dipeptides are an untapped source of BoNT/A LC inhibitors; therefore, our goal of this current work is to evaluate dipeptides as inhibitors.
Dipeptides were synthesized on hydroxylamine Wang resin using Fmoc-protected amino acids and following standard coupling and deprotection strategies. The dipeptide was deprotected, and the N-terminus reacted with various sulfonyl chlorides under basic conditions to give the completed dipeptide on resin. The resin was treated with acid to release the dipeptide from the resin and reveal the hydroxamic acid (Scheme 1). The crude product was purified by prep-HPLC and freeze-dried to give pure dipeptides (1–33), as confirmed by analytical HPLC. Compounds 30–33 were further confirmed by NMR and HRMS. The dipeptides were studied via a commercial FRET-based BoNT/A LC enzymatic assay (List Laboratories, CA) to determine the percent inhibition or IC50 values. Additionally, two crystal structures of the BoNT/A LC bound to dipeptides (30 and 33) were solved and analyzed to determine specific intermolecular interactions between the dipeptide and the BoNT/A LC.
Scheme 1. Synthesis of Dipeptides.
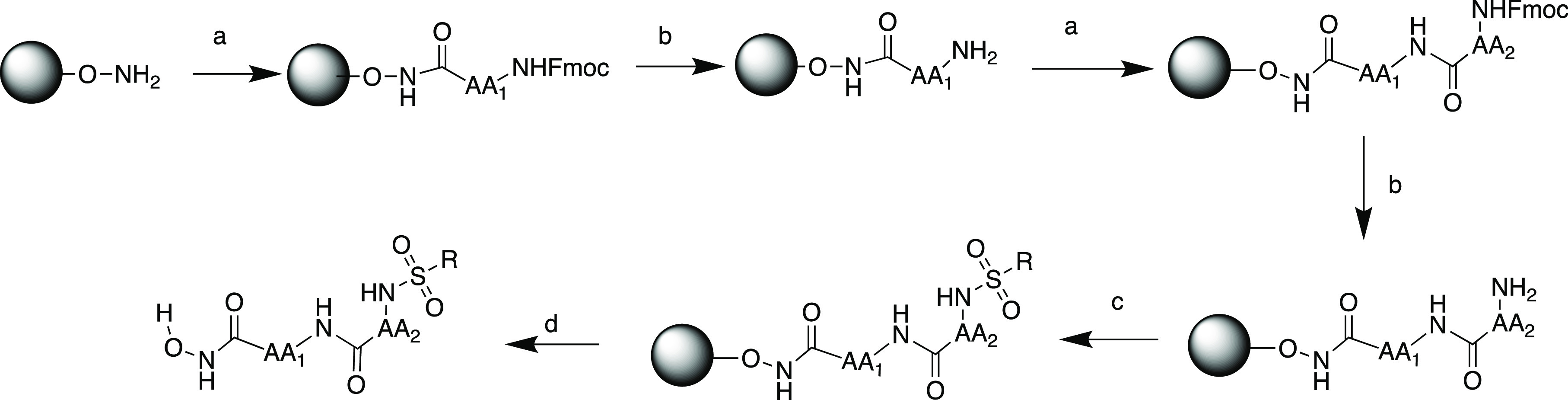
Reagents and conditions: (a) Fmoc-protected amino acid, HOBt, DIC, DMF; (b) 25% PIP in DMF; (c) sulfonyl chloride, 2,6-lutidine, DCM; (d) 50% TFA in DCM.
A dipeptide amino acid profile study was performed to determine the optimal amino acid sequence for binding and inhibition. We focused on amino acids with nonpolar side chains because the BoNT/A LC active site is large and predominantly hydrophobic24,32 and thus focused on optimizing the nonpolar binding interactions. Both the hydroxamic acid and sulfonamide were constant throughout this entire study.
The amino acid profile study (Table 1) indicated that the isoleucine at AA1 is the preferred C-terminal amino acid. As Ile was replaced with a smaller amino acid, Ala (5), β-Ala (15), or Gly (16) inhibition decreased. The substitution of Ile for a larger side chain such as Phe (6) also decreased the inhibition. These results are consistent with a small hydrophobic pocket in proximity to the catalytic zinc ion. The sec-butyl of Ile fits well in this pocket, as smaller side chains could have fewer interactions, leading to decreased binding. The larger side chain of Phe would not fit in this small pocket and would thereby sterically disrupt zinc chelation and significantly limit binding and inhibition, which was observed for 6. The incorporation of Aib into the dipeptide also decreased binding. This is most likely due to Aib altering the conformation of the dipeptide, as Aib is known to have drastic effects on the secondary structure of peptides.33 This result is consistent with our previous study that revealed Ile to be the optimal amino acid at the C-terminus.20
Table 1. Dipeptide Amino Acid Sequence Study.
| compd. | AA1 | AA2 | % inhibitiona |
|---|---|---|---|
| 1 | Ile | Leu | 100 |
| 2 | Ile | Phe | 100 |
| 3 | Ile | Ile | 85 |
| 4 | Ile | Aib | 84 |
| 5 | Ala | Ile | 55 |
| 6 | Phe | Ile | 44 |
| 7 | Ile | Ala | 31 |
| 8 | Aib | Ile | 11 |
| 9 | Ile* | Ile* | 48 |
| 10 | Ile* | Ile | 57 |
| 11 | Ile | Ile* | 69 |
| 12 | Ile* | Phe* | 63 |
| 13 | Phe | Ile* | 62 |
| 14 | Ile | Phe* | 41 |
| 15 | β-Ala | Ile | 62 |
| 16 | Gly | Ile | 18 |
Dipeptides were evaluated at 15 μM with 20 nM BoNT/A LC and 8 μM SNAPtide substrate. Enzyme reactions were performed in triplicate, and the percent inhibition reported is the average. *d-amino acid.
Amino acids with large side chains can be accommodated at AA2, as this position is farther away from the zinc chelation event (Table 1). The AA2 position is less sensitive to amino acid substitution, as Aib (4) resulted in moderate inhibition. In addition, the hydrophobic side chains of AA2 are in an ideal position to interact with the large hydrophobic cavity. Phe is well suited at AA2 because the group can participate in π-stacking or other hydrophobic interactions, which is confirmed by the strong inhibition observed for 2. Leu and Ile at AA2 (1 and 3, respectively) also displayed strong inhibition, as the branched side chains can form more hydrophobic contacts than Ala (7), which showed poor inhibition. This result was expected because AA2 is farther away from zinc binding and in an excellent position to interact with the hydrophobic wall of the active site; therefore, aromatic and branched alkyl side chains would reinforce binding.
The stereochemistry of the amino acids was also evaluated for inhibition (Table 1). As expected, dipeptides containing l-amino acids resulted in better inhibition than d-amino acid dipeptides. This result is not surprising because native amino acids would interact better with the peptide backbone of the active site. It is worth noting that 13 had slightly better inhibition than the l-dipeptide counterpart (6). The combination of l-Phe and d-Ile (AA1 and AA2, respectively) could result in an alternate binding mode for 13, leading to the improved inhibition. In our previous amino acid scaffold, we discovered that d-isoleucine was essential for strong inhibition, as the d-amino acid was thought to position the sulfonamide biphenyl into a favorable binding site.20 Overall, dipeptides containing l-amino acids provided the best inhibition, and this stereochemistry was maintained throughout the study.
The initial dipeptide contained a biphenyl with a chlorine at C-4′, modeled after our previous lead structure.19,20 We hypothesize that at least one phenyl ring and polar substituent(s) would be essential for inhibition. As observed in other inhibitor studies,24,32 there are few polar contacts, and these opportunities should be utilized for tight binding to the predominately hydrophobic BoNT/A LC active site. We varied both the phenyl and polar substituents to identify intermolecular interactions (Table 2). Chlorine has been shown to be involved in key interactions, specifically with Arg363,27,32,34 and as expected, without chlorine on the biphenyl, the inhibition decreased. Furthermore, substitution of the biphenyl for 4-cyclohexylphenyl (18) or phenyl (19) resulted in decreased inhibition, as the cyclohexyl most likely contributed to steric clashes and diminished hydrophobic interactions in regards to 18. Interestingly, when a halide was added to the phenyl (22 or 23), inhibition increased. This supports a key polar interaction that is essential for binding.
Table 2. Probing the Aromatic System on the Dipeptide N-Terminus.

| compd. | R | % inhibitiona |
|---|---|---|
| 17 | biphenyl | 77 |
| 18 | 4-cyclohexylphenyl | 57 |
| 19 | phenyl | 52 |
| 20 | 3,5-dichlorophenyl | 100 |
| 21 | meta-tert-butylphenyl | 93 |
| 22 | para-bromophenyl | 87 |
| 23 | para-chlorophenyl | 77 |
| 24 | meta-chlorophenyl | 79 |
| 25 | 3,4-diethoxyphenyl | 22 |
| 26 | 2,6-dichlorophenyl | 83 |
Dipeptides were evaluated at 15 μM with 20 nM BoNT/A LC and 8 μM SNAPtide substrate. Enzyme reactions were performed in triplicate, and the percent inhibition reported is the average.
The position or type of halide on the phenyl was not crucial for inhibition, as a halide at the para (23) or meta (24) position did not greatly alter the inhibition. However, the addition of a second chlorine to the phenyl (20) drastically improved inhibition, indicating strong polar intermolecular interactions. Another explanation for the strong inhibition of 20 is the electron-withdrawing ability of the chlorines, which would increase the phenyl’s π-stacking interactions, leading to tight binding. The position of the chlorines affected the inhibition, as the 2,6-dichlorophenyl analog (26) had lower inhibition compared with 20, indicating that chlorine is involved in a favorable interaction in the meta position, or the ortho position is causing a steric repulsion. This evidence points to the chlorines involved in specific interactions within the active site rather than an electron effect that is strengthening the π-stacking. The addition of ethoxy groups (25) also caused the inhibition to significantly decrease. This could be due to a steric effect or the electron-donating nature of the ethoxy groups disrupting the π-stacking. The strong inhibition observed for 21 was surprising because this dipeptide does not follow a clear trend with the other dipeptides in this study. The BoNT/A LC has been reported to bind large hydrophobic groups such as adamantane through an induced fit model.34 The BoNT/A LC active site is known to be highly flexible32 and could accommodate the hydrophobic tert-butyl group of 21 via an induced fit. On the basis of the results of this study, the 3,5-dichrolophenyl contributed to potent inhibition and will be included in second-generation dipeptides.
Second-generation dipeptides were synthesized based on the previous results, and their IC50 values for the BoNT/A LC were determined (Table 3). The library focused on branched side chains at both AA1 and AA2 in addition to Phe at AA2. The AA1 position is more sensitive to branched side chains, as this amino acid is adjacent to the hydroxamic acid. Substituting Ile (20) with Val (33) resulted in a 7.5-fold decrease in the IC50 value. The removal of a methyl group drastically changed the IC50 value, indicating a well-defined small hydrophobic pocket in close proximity to the catalytic zinc. The isopropyl of valine fits better in the pocket than the sec-butyl of Ile, which demonstrates the sensitivity of the AA1 position. Poor binding in this pocket disrupts zinc chelation, causing decreased inhibition. This trend is consistent with 32, as the propyl side chain of Nva would be too long for the pocket, resulting in a two times higher IC50 compared with 33. The second-generation library confirmed our pervious results that a small hydrophobic pocket is in close proximity to the catalytic zinc.
Table 3. Second-Generation Dipeptides.
| compd. | AA1 | AA2 | R | IC50 (μM)a |
|---|---|---|---|---|
| 27 | Nva | Ile | biphenyl-4-chloro | 1.0 |
| 2 | Ile | Phe | biphenyl-4-chloro | 2.4 |
| 28 | Ile | Val | biphenyl-4-chloro | 2.9 |
| 20 | Ile | Phe | 3,5-dichlorophenyl | 0.15 |
| 29 | Leu | Ile | 3,5-dichlorophenyl | 0.15 |
| 30 | Nva | Ile | 3,5-dichlorophenyl | 0.089 |
| 31 | Ile | Val | 3,5-dichlorophenyl | 0.069 |
| 32 | Nva | Phe | 3,5-dichlorophenyl | 0.043 |
| 33 | Val | Phe | 3,5-dichlorophenyl | 0.021 |
Dipeptides were evaluated using 20 nM BoNT/A LC, 8 μM SNAPtide substrate, and a range of dipeptide concentrations to determine IC50 values.
As previously indicated, the AA2 position is less sensitive to amino acid substitutions and has the potential for numerous hydrophobic interactions. The optimal amino acid at the AA2 position is Phe, with a potent IC50 value of 21 nM for 33. The phenyl side chain is most likely participating in π-stacking. As expected, the sulfonamide biphenyl analogs (2, 27, and 28) resulted in modest IC50 values ranging from 1 to 3 μM. Replacing the biphenyl with 3,5-dicholorphenyl drastically improved the IC50 values to <1 μM. The results confirm that the biphenyl is too large for the dipeptide scaffold. Also, the chlorines on the phenyl are vital for inhibition due to the formation of polar contacts or by effecting the electronics of the phenyl, leading to improved binding.
We solved the crystal structure of the apo BoNT/A LC (PDB 7KY2) and the cocrystal structures of the BoNT/A LC bound to 30 (PDB 7KYF) and 33 (PDB 7KYH) to gain structural insight into dipeptide binding (Table S1 and Figures 1 and 2). Compounds 30 and 33 both displayed the predicted hydroxamate chelation to the active-site zinc. This evidence signifies that the dipeptide scaffolds in this study participate in a competitive mode of inhibition, as observed with other hydroxamate-based inhibitors.14 In addition, the 3,5-dicholorophenyl sulfonamide of both compounds occupies a similar area between Phe369 and Val70 in the crystal structure. There is no apparent π-stacking observed in this area of the crystal structure for both compounds. The chlorines are involved in polar interactions with the peptide backbone, establishing the chlorines as a key element for binding. Halogen bonding has been observed in many protein ligand complexes, indicating the importance of this interaction in drug discovery.35 Overall, the dipeptides occupy the same region within the BoNT/A LC active site. The sulfonamide of 30 participates in contacts with Arg363 and Tyr366 (Figure 1). In our previous molecular modeling study, we proposed that the sulfonamide interacts with Arg363 and acts as the hinge to guide the molecule into the binding sites.20 The crystal structure validates this theory and also demonstrates the potential for Tyr366 to be involved in this interaction. The polar interaction anchors the molecule in the active site and orientates the Ile side chain toward the opening of the active site. The propyl side chain of Nva is positioned into the previously discovered small hydrophobic pocket formed by Thr220 and Glu224 and adjacent to the catalytic zinc.
Figure 1.
X-ray crystal structure of 30 bound to the BoNT/A LC active site (PDB 7KYF). Green dashed lines represent intermolecular contacts generated with ChimeraX.36
Figure 2.
X-ray crystal structure of 33 bound to the BoNT/A LC active site (PDB 7KYH). Green dashed lines represent intermolecular contacts generated with ChimeraX.36
In the crystal structures, the side chains of 33 occupy different regions in the BoNT/A LC active site (Figure 2) compared with 30. The phenyl of Phe is π-stacking with Tyr366, which blocks Arg363 from interacting with the sulfonamide or any other elements of the molecule. The π-stacking is a key interaction for this dipeptide, leading to the low IC50 value. The sulfonamide is pointing into the active site but is not involved in any interactions within the active site. The valine side chain is in the small hydrophobic pocket formed by Phe163, Phe194, and Thr220.
Dipeptides with hydrophobic side chains have been shown to be potent inhibitors for the BoNT/A LC. Through a structure–activity relationship study of the dipeptide sequence and sulfonamide aromatic, dipeptide 33 was synthesized and had an IC50 of 21 nM. A crystal structure of this dipeptide bound to the BoNT/A LC revealed the hydroxamic acid chelating to the zinc, supporting a competitive mode of inhibition. The side chains of 33 are involved in numerous hydrophobic interactions within the active site, including π-stacking. A well-defined small hydrophobic pocket adjacent to the catalytic zinc was also discovered in this study. In addition, the crystal structure of 30 displays polar interactions between the chlorines and the peptide backbone and between the sulfonamide and Arg363. The inhibition data along with the crystal structures provide a foundation for the future development of dipeptides as potent inhibitors for the BoNT/A LC. These novel BoNT/A LC inhibitors have enormous potential for future optimization as the dipeptide core is amenable to rapid structural changes to improve inhibition. Furthermore, future studies will evaluate the physiochemical properties and investigate the dipeptides in cellular and in vivo experiments.
Acknowledgments
We are grateful to the Allergan Foundation and California State University, Fullerton for financial support of this research. Instrumentation support was provided by the Department of Defense (68816-RT-REP) and the National Science Foundation MRI (CHE1726903) for the acquisition of a UPLC-HRMS apparatus. The X-ray diffraction instrument purchase was supported by the Department of Defense (DoD) Research and Education Program for Historically Black Colleges and Universities and Minority-Serving Institutions (HBCU/MI) Equipment/Instrumentation Grant to S. Chantal E. Stieber under contract no. W911NF-17-1-0537. We also thank the ALS-ENABLE beamlines for collection of X-ray diffraction data. The ALS-ENABLE beamlines are supported in part by the National Institutes of Health, National Institute of General Medical Sciences, grant P30 GM124169-01. The Advanced Light Source is a Department of Energy Office of Science User Facility under contract no. DE-AC02-05CH11231. Molecular graphics and analyses were performed with UCSF ChimeraX, developed by the Resource for Biocomputing, Visualization, and Informatics at the University of California, San Francisco, with support from the National Institutes of Health R01-GM129325 and the Office of Cyber Infrastructure and Computational Biology, National Institute of Allergy and Infectious Diseases.
Glossary
Abbreviations
- BoNT
botulinum neurotoxin
- CDC
Centers for Disease Control and Prevention
- HC
heavy chain
- LC
light chain
- SNAP-25
synaptosome-associated protein
- VAMP
vesicle-associated membrane protein
- ACE
angiotensin-converting enzyme
- FRET
fluorescence resonance energy transfer
- Fmoc
fluorenylmethoxycarbonyl
- HOBt
hydroxybenzotriazole
- DIC
N,N′-diisopropylcarbodiimide
- DMF
N,N-dimethylformamide
- PIP
piperidine
- DCM
dichloromethane
- TFA
trifluoroacetic acid
- Nva
norvaline
- Aib
2-aminoisobutyric acid
Supporting Information Available
The Supporting Information is available free of charge at https://pubs.acs.org/doi/10.1021/acsmedchemlett.0c00674.
Synthesis procedures, analytical data, and details of the enzyme assay, enzyme purification, crystallization, and structure solution (PDF)
Author Contributions
M.A., R.S.C., and A.K. synthesized dipeptides. M.A. performed inhibitor assays. W.M. expressed and purified BoNT/A LC. M.E.O. grew crystals and solved crystal structures. N.T.S. designed experiments, supervised the dipeptide synthesis and inhibitor assay, and wrote the manuscript. All authors contributed to writing the manuscript and have given approval to the final version of the manuscript.
The authors declare no competing financial interest.
Supplementary Material
References
- Pirazzini M.; Rossetto O.; Eleopra R.; Montecucco C. Botulinum Neurotoxins: Biology, Pharmacology, and Toxicology. Pharmacol. Rev. 2017, 69 (2), 200–235. 10.1124/pr.116.012658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson L. The life history of a botulinum toxin molecule. Toxicon 2013, 68, 40–59. 10.1016/j.toxicon.2013.02.014. [DOI] [PubMed] [Google Scholar]
- Gill D. M. Bacterial toxins: a table of lethal amounts. Microbiol. Rev. 1982, 46 (1), 86–94. 10.1128/MR.46.1.86-94.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossetto O.; Montecucco C. Tables of Toxicity of Botulinum and Tetanus Neurotoxins. Toxins 2019, 11 (12), 686. 10.3390/toxins11120686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnon S. S.; Schechter R.; Inglesby T. V.; et al. Botulinum toxin as a biological weapon: Medical and public health management. JAMA 2001, 285 (8), 1059–1070. 10.1001/jama.285.8.1059. [DOI] [PubMed] [Google Scholar]
- Bossi P.; Garin D.; Guihot A.; Gay F.; Crance J. M.; Debord T.; Autran B.; Bricaire F. Bioterrorism: management of major biological agents. Cell. Mol. Life Sci. 2006, 63 (19–20), 2196–212. 10.1007/s00018-006-6308-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cenciarelli O.; Riley P. W.; Baka A. Biosecurity Threat Posed by Botulinum Toxin. Toxins 2019, 11 (12), 681. 10.3390/toxins11120681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janik E.; Ceremuga M.; Saluk-Bijak J.; Bijak M. Biological Toxins as the Potential Tools for Bioterrorism. Int. J. Mol. Sci. 2019, 20 (5), 1181. 10.3390/ijms20051181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson J. S.; Parrera G. S.; Astacio H.; Sahota H.; Anderson D. M.; Hall C.; Babinchak T. Safety and Clinical Outcomes of an Equine-derived Heptavalent Botulinum Antitoxin Treatment for Confirmed or Suspected Botulism in the United States. Clin. Infect. Dis. 2020, 70 (9), 1950–1957. 10.1093/cid/ciz515. [DOI] [PubMed] [Google Scholar]
- Koussoulakos S. Botulinum neurotoxin: the ugly duckling. Eur. Neurol. 2009, 61 (6), 331–42. 10.1159/000210545. [DOI] [PubMed] [Google Scholar]
- Dong M.; Masuyer G.; Stenmark P. Botulinum and Tetanus Neurotoxins. Annu. Rev. Biochem. 2019, 88, 811–837. 10.1146/annurev-biochem-013118-111654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffield J. A. Botulinum neurotoxin: the neuromuscular junction revisited. Crit. Rev. Neurobiol. 2003, 15 (3–4), 175–96. 10.1615/CritRevNeurobiol.v15.i34.10. [DOI] [PubMed] [Google Scholar]
- Shukla H. D.; Sharma S. K. Clostridium botulinum: a bug with beauty and weapon. Crit. Rev. Microbiol. 2005, 31 (1), 11–8. 10.1080/10408410590912952. [DOI] [PubMed] [Google Scholar]
- Lin L.; Olson M. E.; Eubanks L. M.; Janda K. D. Strategies to Counteract Botulinum Neurotoxin A: Nature’s Deadliest Biomolecule. Acc. Chem. Res. 2019, 52 (8), 2322–2331. 10.1021/acs.accounts.9b00261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duplantier A. J.; Kane C. D.; Bavari S. Searching for Therapeutics Against Botulinum Neurotoxins: A True Challenge for Drug Discovery. Curr. Top. Med. Chem. 2016, 16 (21), 2330–2349. 10.2174/1568026616666160413135630. [DOI] [PubMed] [Google Scholar]
- Pirazzini M.; Rossetto O. Challenges in searching for therapeutics against Botulinum Neurotoxins. Expert Opin. Drug Discovery 2017, 12 (5), 497–510. 10.1080/17460441.2017.1303476. [DOI] [PubMed] [Google Scholar]
- Capkova K.; Salzameda N. T.; Janda K. D. Investigations into small molecule non-peptidic inhibitors of the botulinum neurotoxins. Toxicon 2009, 54 (5), 575–82. 10.1016/j.toxicon.2009.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar G.; Swaminathan S. Recent developments with metalloprotease inhibitor class of drug candidates for botulinum neurotoxins. Curr. Top. Med. Chem. 2015, 15 (7), 685–95. 10.2174/1568026615666150309150338. [DOI] [PubMed] [Google Scholar]
- Burtea A.; Salzameda N. T. Discovery and SAR study of a sulfonamide hydroxamic acid inhibitor for the botulinum neurotoxin serotype A light chain. MedChemComm 2014, 5 (6), 706–710. 10.1039/C4MD00053F. [DOI] [Google Scholar]
- Thompson J. C.; Dao W. T.; Ku A.; Rodriguez-Beltran S. L.; Amezcua M.; Palomino A. Y.; Lien T.; Salzameda N. T. Synthesis and activity of isoleucine sulfonamide derivatives as novel botulinum neurotoxin serotype A light chain inhibitors. Bioorg. Med. Chem. 2020, 28 (18), 115659. 10.1016/j.bmc.2020.115659. [DOI] [PubMed] [Google Scholar]
- Lai H.; Feng M.; Roxas-Duncan V.; Dakshanamurthy S.; Smith L. A.; Yang D. C. Quinolinol and peptide inhibitors of zinc protease in botulinum neurotoxin A: effects of zinc ion and peptides on inhibition. Arch. Biochem. Biophys. 2009, 491 (1–2), 75–84. 10.1016/j.abb.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Kumar G.; Kumaran D.; Ahmed S. A.; Swaminathan S. Peptide inhibitors of botulinum neurotoxin serotype A: design, inhibition, cocrystal structures, structure-activity relationship and pharmacophore modeling. Acta Crystallogr., Sect. D: Biol. Crystallogr. 2012, 68 (5), 511–520. 10.1107/S0907444912003551. [DOI] [PubMed] [Google Scholar]
- Kumaran D.; Adler M.; Levit M.; Krebs M.; Sweeney R.; Swaminathan S. Interactions of a potent cyclic peptide inhibitor with the light chain of botulinum neurotoxin A: Insights from X-ray crystallography. Bioorg. Med. Chem. 2015, 23 (22), 7264–73. 10.1016/j.bmc.2015.10.024. [DOI] [PubMed] [Google Scholar]
- Silvaggi N. R.; Wilson D.; Tzipori S.; Allen K. N. Catalytic features of the botulinum neurotoxin A light chain revealed by high resolution structure of an inhibitory peptide complex. Biochemistry 2008, 47 (21), 5736–45. 10.1021/bi8001067. [DOI] [PubMed] [Google Scholar]
- Muri E. M. F.; Nieto M. J.; Sindelar R. D.; Williamson J. S. Hydroxamic Acids as Pharmacological Agents. Curr. Med. Chem. 2002, 9 (17), 1631–1653. 10.2174/0929867023369402. [DOI] [PubMed] [Google Scholar]
- Dickerson T. J.; Smith G. R.; Pelletier J. C.; Reitz A. B. 8-Hydroxyquinoline and hydroxamic acid inhibitors of botulinum neurotoxin BoNT/A. Curr. Top. Med. Chem. 2014, 14 (18), 2094–102. 10.2174/1568026614666141022095114. [DOI] [PubMed] [Google Scholar]
- Thompson A. A.; Jiao G. S.; Kim S.; Thai A.; Cregar-Hernandez L.; Margosiak S. A.; Johnson A. T.; Han G. W.; O’Malley S.; Stevens R. C. Structural characterization of three novel hydroxamate-based zinc chelating inhibitors of the Clostridium botulinum serotype A neurotoxin light chain metalloprotease reveals a compact binding site resulting from 60/70 loop flexibility. Biochemistry 2011, 50 (19), 4019–28. 10.1021/bi2001483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodin B.; Nielsen C. U.; Steffansen B.; Frokjaer S. Transport of peptidomimetic drugs by the intestinal Di/tri-peptide transporter, PepT1. Pharmacol. Toxicol. 2002, 90 (6), 285–96. 10.1034/j.1600-0773.2002.900601.x. [DOI] [PubMed] [Google Scholar]
- Yang C. Y.; Dantzig A. H.; Pidgeon C. Intestinal peptide transport systems and oral drug availability. Pharm. Res. 1999, 16 (9), 1331–43. 10.1023/A:1018982505021. [DOI] [PubMed] [Google Scholar]
- Zhu T.; Chen X. Z.; Steel A.; Hediger M. A.; Smith D. E. Differential recognition of ACE inhibitors in Xenopus laevis oocytes expressing rat PEPT1 and PEPT2. Pharm. Res. 2000, 17 (5), 526–32. 10.1023/A:1007556630189. [DOI] [PubMed] [Google Scholar]
- Tanaka M.; Dohgu S.; Komabayashi G.; Kiyohara H.; Takata F.; Kataoka Y.; Nirasawa T.; Maebuchi M.; Matsui T. Brain-transportable dipeptides across the blood-brain barrier in mice. Sci. Rep. 2019, 9 (1), 5769. 10.1038/s41598-019-42099-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvaggi N. R.; Boldt G. E.; Hixon M. S.; Kennedy J. P.; Tzipori S.; Janda K. D.; Allen K. N. Structures of Clostridium botulinum Neurotoxin Serotype A Light Chain complexed with small-molecule inhibitors highlight active-site flexibility. Chem. Biol. 2007, 14 (5), 533–42. 10.1016/j.chembiol.2007.03.014. [DOI] [PubMed] [Google Scholar]
- Di Blasio B.; Pavone V.; Lombardi A.; Pedone C.; Benedetti E. Noncoded residues as building blocks in the design of specific secondary structures: Symmetrically disubstituted glycines and β-alanine. Biopolymers 1993, 33 (7), 1037–1049. 10.1002/bip.360330706. [DOI] [PubMed] [Google Scholar]
- Silhar P.; Silvaggi N. R.; Pellett S.; Capkova K.; Johnson E. A.; Allen K. N.; Janda K. D. Evaluation of adamantane hydroxamates as botulinum neurotoxin inhibitors: synthesis, crystallography, modeling, kinetic and cellular based studies. Bioorg. Med. Chem. 2013, 21 (5), 1344–8. 10.1016/j.bmc.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirimulla S.; Bailey J. B.; Vegesna R.; Narayan M. Halogen interactions in protein-ligand complexes: implications of halogen bonding for rational drug design. J. Chem. Inf. Model. 2013, 53 (11), 2781–91. 10.1021/ci400257k. [DOI] [PubMed] [Google Scholar]
- Pettersen E. F.; Goddard T. D.; Huang C. C.; Meng E. C.; Couch G. S.; Croll T. I.; Morris J. H.; Ferrin T. E. UCSF ChimeraX: Structure visualization for researchers, educators, and developers. Protein Sci. 2021, 30 (1), 70–82. 10.1002/pro.3943. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.







