Abstract
Background
The global COVID-19 pandemic has impacted on the mental health of individuals, particularly those with chronic illnesses. We aimed to quantify stress, anxiety and depression among individuals with Inflammatory bowel disease (IBD) in Australia during the pandemic.
Methods
An electronic survey was made available to IBD patients Australia-wide from 17 June to 12 July 2020. Respondents with an underlying diagnosis of IBD and over 18 years of age were included. A validated questionnaire (Depression, Anxiety, Stress Score-21, DASS21) was used to assess depression, anxiety and stress. Data on potential predictors of depression, anxiety and stress were collected.
Results
352 participated in the survey across Australia. 60.5% of respondents fulfilled DASS criteria for at least moderate depression, anxiety or stress. 45% reported a pre-existing diagnosis of depression and/or anxiety. Over 2/3 of these respondents reported worsening of their pre-existing depression/anxiety due to the current pandemic. Of those without a pre-existing diagnosis of anxiety or depression, high rates of at least moderate to severe depression (34.9%), anxiety (32.0%) and stress (29.7%) were noted. Younger age (OR 0.96, 95% CI 0.94 to 0.98, p<0.001), lack of access to an IBD nurse (OR 1.81, 95% CI 1.03 to 3.19, p=0.04) and lack of education on reducing infection risk (OR 1.99, 95% CI 1.13 to 3.50, p=0.017) were associated with significant stress, anxiety and/or depression.
Conclusion
High prevalence of undiagnosed depression, anxiety and stress was identified among respondents. Improved access to IBD nurse support and greater attention to education are modifiable factors that may reduce depression, anxiety and/or stress among patients with IBD during the pandemic.
Keywords: inflammatory bowel disease, COVID-19, psychological stress, ulcerative colitis, crohn's disease
Summary box.
What is already known about this subject?
People with inflammatory bowel disease (IBD) have higher background rates of depression and anxiety than the general population, and may be more susceptible to the negative mental health impact of the COVID-19 pandemic.
There are no prior Western country studies that have quantified depression and anxiety rates among patients with IBD during the pandemic.
What are the new findings?
High rates of depression, anxiety and stress were noted in respondents. Even those without a prior diagnosis of depression or anxiety had high rates of significant depression (34.9%), anxiety (32.0%) and stress (29.7%).
Predictors for at least moderate depression, anxiety or stress included younger age, symptomatic disease, lack of access to an IBD nurse, lack of advice from medical practitioner regarding reducing COVID-19 infection and perceived increased susceptibility to COVID-19 compared with the general population.
How might it impact on clinical practice in the foreseeable future?
This study highlights the need to support the mental health of patients with IBD during the global pandemic.
Improved access to subspecialty nurses and medical practitioner advice on reducing infection risk are two modifiable factors that may reduce depression, anxiety and stress among patients with IBD.
Introduction
The COVID-19 outbreak has caused fears of morbidity and mortality from potential infection, and the impact of social distancing on financial well-being, relationships and mental health worldwide. High rates of depression, anxiety and stress have been documented in countries with high rates of COVID-19, such as China and Italy.1 2 Factors such as female gender, negative affect, detachment and having an infected acquaintance have been found to be associated with increased levels of depression, anxiety and/or stress.
Inflammatory bowel disease (IBD) is a chronic autoinflammatory condition that affects the gastrointestinal tract. Peak onset is typically in young adults, however, IBD affects individuals from the entire age spectrum. IBD is well known to have a substantial impact on quality of life: individuals with IBD have comparatively higher rates of anxiety and depression than the general population.3 In addition, immunosuppressive medications may heighten individual fears of infection during the present COVID-19 pandemic. Individuals with IBD may hence be more susceptible to the negative mental health impact of the COVID-19 pandemic compared with the general population.
To date, there has been scarce data on the impact of the COVID-19 pandemic on the mental health of people living with IBD. The aim of our study was to assess the impact of the COVID-19 pandemic on the mental health of individuals with IBD living in Australia. Australian states introduced social distancing rules in March 2020 to combat the spread of COVID-19. In addition, we seek to find factors that are associated with increased depression, anxiety and stress, to allow for future interventional studies.
Methods
Study design and study population
We conducted a cross-sectional survey of individuals living with IBD in Australia. The survey content was developed by a group consisting of three gastroenterologists, a clinical psychologist, an IBD clinical nurse consultant and a gastroenterology trainee. The final content was approved by consensus. The study was conducted between 17 June and 12 July 2020. The electronic survey was uploaded on an online platform (Survey Monkey) and was advertised using the social media platforms of Crohn’s and Colitis Australia and the Western Sydney Local Health District. Efforts were made to advertise the survey widely. Potential participants could access the survey via an online link.
A validated questionnaire (Depression, Anxiety, Stress Score-21, DASS21) was used to assess depression, anxiety and stress in respondents.4 The DASS-21 is a self-report questionnaire consisting of 21 items with 7 items per subscale domain: depression, anxiety and stress. Respondents score each item from 0 to 3, and item scores are added together and multiplied by 2 for each domain to generate three subscale scores. Depression subscale scores corresponds to normal population (0–9), mild (10–13), moderate (14–20) and severe symptoms (21–27). Anxiety subscale scores correspond to normal population (0–7) mild, (8–9) moderate (10–14) and severe symptoms (15–19). Similarly, stress subscale scores corresponded to normal population (0–14), mild (15–18), moderate (19–25) or severe symptoms (26-33). Significant depression, anxiety and/or stress in our study was defined as at least moderate DASS21 subscores for depression, anxiety and/or stress. We also collected data on demographics, IBD phenotype and disease activity, other medical history and potential predictors of depression, anxiety and stress (see online supplemental table 1 for full questionnaire).
bmjgast-2020-000581supp001.pdf (84KB, pdf)
Study participants
All respondents living in Australia, with an underlying diagnosis of IBD, and over 18 years of age were included. IP address restrictions meant each participant could fill out the survey only once. The survey was anonymous, and no personal data were collected at any stage.
Patient and public involvement
A survey draft was trialled on 10 patients with IBD who attend the IBD service at Blacktown hospital. Qualitative feedback was obtained on time taken to complete the survey, its content and its clarity. The survey was edited based on this.
Statistical analysis
Descriptive statistics were used to analyse response to questions. Univariate and multivariate logistic regression analyses were used to determine if associations exist between respondent characteristics and stress, depression and anxiety. Results were expressed as ORs with 95% CI. A p<0.05 was considered as statistically significant. Statistical analyses were conducted using IBM SPSS statistics V.26.
Completion of the questionnaire was considered as implied consent for participation in the study.
Results
There were 352 respondents to the survey (table 1). The mean age of respondents was 40 years (SD 14 years), and majority were female (79%). Most respondents were from New South Wales (NSW) (54%) and Victoria (23%). University-level education was completed by 48% of the respondents and 44% were in full time employment. A diagnosis of Crohn’s disease (CD) was reported by 59%, ulcerative colitis by 36% and indeterminate colitis by 5%. Thirty-nine per cent of CD respondents reported perianal involvement. Severe, moderately severe and mild symptoms were reported by 14%, 20% and 43% of respondents, respectively, while 23% reported to be in clinical remission without symptoms.
Table 1.
Characteristics of respondents
| Characteristic (no of responders) | Criteria | Frequency (%) |
| Gender (n=351) | Male | 20.5 |
| Female | 78.8 | |
| Other | 0.6 | |
| Age (n=352) | Median 38 (IQR 29–49) |
|
| State (n=352) | New South Wales | 54.3 |
| Victoria | 22.7 | |
| Queensland | 11.1 | |
| South Australia | 2.0 | |
| Northern territory | 0.6 | |
| Tasmania | 3.1 | |
| Western Australia | 6.3 | |
| Education (n=353) | Primary or secondary school | 9.1 |
| Completed high school | 25.2 | |
| University education | 47.9 | |
| Vocational education and training | 17.8 | |
| Employment status (n=351) | Employed—full time | 43.9 |
| Employed—part time | 17.9 | |
| Self employed | 6.3 | |
| Temporary/casual | 7.7 | |
| Unemployed | 21.1 | |
| Student | 3.1 | |
| IBD diagnosis (n=354) | Ulcerative colitis | 35.9 |
| Crohn’s disease | 59.3 | |
| IBD unspecified | 4.8 | |
| Peri-anal Crohn’s (n=201) | Yes | 39.3 |
| Age at IBD diagnosis | Median 26 (IQR 20–34) |
|
| Current Clinical Status of Disease (n=337) | No symptoms | 22.8 |
| Mild symptoms | 43.0 | |
| Moderate symptoms | 20.2 | |
| Severe symptoms | 13.9 | |
| Chronic medical conditions apart from IBD | Diabetes | 4.8 |
| Heart disease | 3.7 | |
| Lung disease (asthma, COPD) | 9.9 | |
| Previous stroke | 1.1 | |
| Hypertension | 9.3 | |
| Kidney disease | 0.8 | |
| Nil other medical condition | 71.8 |
COPD, Chronic obstructive pulmonary disease; IBD, inflammatory bowel disease.
Private gastroenterologists managed 50% of patients and 26% were managed in dedicated public IBD clinics (table 2). An IBD nurse was accessible by 46% of respondents. Current systemic steroids use was reported by 11% of respondents, with 45% reported being on an immunomodulator and 55% on a biologic. Only 1.8% and 3.4% of patients stopped their medications during COVID-19 pandemic on their own accord and based on advice by a health professional, respectively. Access to telehealth was available to majority of the respondents (67.5%). COVID-19-specific health education was only received by 53% of respondents, with 97.2% of those who receive education agreeing that the information provided was useful.
Table 2.
IBD Medication and management, questionnaire responses
| Question (no of responders) | Responses | Frequency (%) |
| Current medications for treatment of IBD | Prednisolone | 10.5 |
| Topical steroids | 4.2 | |
| 5 ASA | 41 | |
| Thiopurines | 35.9 | |
| Methotrexate | 6.8 | |
| Anti-TNF | 32.8 | |
| Ustekinumab | 7.6 | |
| Vedolizumab | 13 | |
| Tofacitinib | 0.3 | |
| Study drugs (clinical trials) | 0.8 | |
| Symptom control medication | 21.5 | |
| IBD medication knowledge (n=336) | Very high level | 11.9 |
| High Level | 39.9 | |
| Intermediate | 36.6 | |
| Low level | 9.5 | |
| Very low level | 2.1 | |
| IBD medication adherence pre-COVID-19 pandemic (n=328) | Rarely missed a dose | 79.3 |
| Occasionally missed a dose | 17.4 | |
| Frequently missed a dose | 3.4 | |
| IBD follow-up (n=334) | Public IBD Clinic | 26.3 |
| Public gastroenterology clinic | 15.3 | |
| Public surgical clinic | 1.2 | |
| Private gastroenterologist | 50 | |
| Private surgeon | 0.3 | |
| General practitioner | 6.9 | |
| Access to IBD nurse (n=335) | Yes | 46.9 |
| Access to phone based gastroenterology service (n=335) | Yes | 67.5 |
| Advice received on reducing COVID-19 infection risk (n=335) | Yes | 53.1 |
| Perceived usefulness of the advice (n=177) | Extremely useful | 27.7 |
| Very useful | 43.5 | |
| Somewhat useful | 26.0 | |
| Not so useful | 2.8 | |
| Not at all useful | 0 | |
| Place of presentation in event of significant IBD flare assuming no pandemic (n=328) | Emergency department | 20.7 |
| Gastroenterologist | 43.9 | |
| General practitioner | 18.6 | |
| Self-medicate | 5.2 | |
| IBD helpline/IBD nurse | 11.6 | |
| Place of presentation in event of significant IBD flare during COVID-19 pandemic (n=326) | Emergency department | 19.3 |
| Gastroenterologist | 44.2 | |
| General practitioner | 14.7 | |
| Self-medicate | 7.4 | |
| IBD helpline/IBD nurse | 14.4 | |
| Ceased IBD medications due to COVID-19 pandemic (n=326) | Yes, on own accord | 1.8 |
| Yes, on health professional advice | 3.4 | |
| No | 94.8 | |
| Advised by a health provider to stop IBD medication due to COVID-19 | Gastroenterologist | 4.0 |
| Surgeon | 0.6 | |
| GP | 3.1 | |
| Allied health professional | 0.6 | |
| Alternative therapy practitioner | 2.3 |
ASA, Aminosalicylic acid; GP, general practitioner; IBD, inflammatory bowel disease; TNF, tumour necrosis factor.
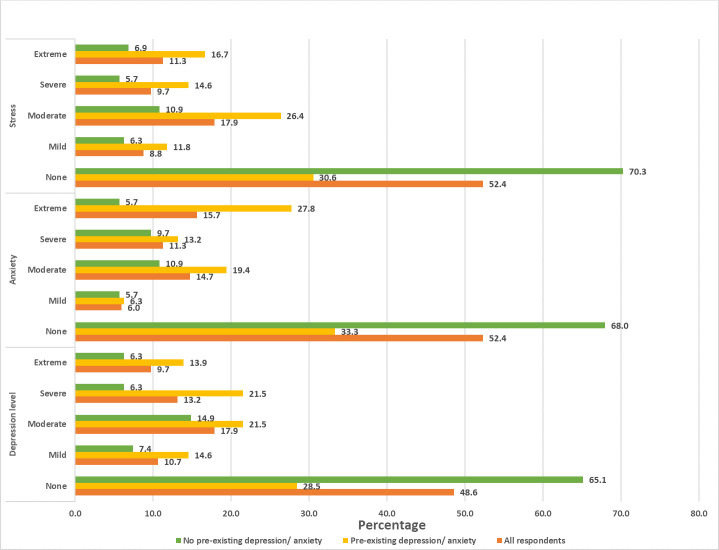
More than 90% of respondents had at least some concerns about contracting COVID-19, while 74.7% either strongly agreed or agreed that they were more susceptible to contracting the infection compared with general population (table 3). Pre-existing diagnosis of depression and/or anxiety was reported by 45% of respondents. More than 2/3 of these patients reported worsening of their diagnosis due to the psychological impact of the current pandemic (table 3). 60.5% of respondents fulfilled DASS criteria for at least moderate depression, anxiety and/or stress (figure 1). Of those without a pre-existing diagnosis of anxiety or depression, 34.9% met criteria for at least moderate depression, 32.0% met criteria for at least moderate anxiety and 29.7% met criteria for at least moderate stress.
Table 3.
Psychological impact of COVID-19 pandemic, questionnaire responses
| Question (no of responders) | Responses | Frequency (%) |
| Level of concern regarding contracting COVID-19 (n=328) | A great deal | 20.1 |
| A lot | 21.3 | |
| A moderate amount | 29.3 | |
| A little | 19.8 | |
| None at all | 9.5 | |
| Perceived greater susceptibility to COVID-19 infection than general population (n=328) | Strongly agree | 37.8 |
| Agree | 36.9 | |
| Neither agree nor disagree | 18.9 | |
| Disagree | 4.9 | |
| Strongly disagree | 1.5 | |
| Pre-existing diagnosis of anxiety/depression (n=326) | Yes | 44.8 |
| Perceived exacerbation of pre-existing anxiety/depression during pandemic (n=144) | Yes | 67.4 |
| Concerns regarding social isolation worsening mood (n=324) | Strongly agree | 12.7 |
| Agree | 35.5 | |
| Neither agree nor disagree | 25.9 | |
| Disagree | 21.0 | |
| Strongly disagree | 4.9 | |
| Exposure to COVID-19 news and information on social media (n=325) | Very often | 69.5 |
| Often | 18.5 | |
| Sometimes | 7.7 | |
| Rarely | 2.5 | |
| Never | 1.8 | |
| Perceived impact of COVID-19 coverage on mental well-being (n=324) | Negative impact | 45.1 |
| Has helped manage anxiety/depression | 23.5 | |
| Have not been affected | 31.5 |
Figure 1.
Rates of depression, anxiety and stress among survey respondents.
Univariate and multivariate analysis was performed to assess predictors of depression, anxiety and/or stress using baseline characteristics (table 4). Statistically significant predictors for at least moderate depression, anxiety or stress on multivariate analysis included: younger age, lack of immunomodulator use, symptom status, lack of access to IBD nurse, lack of advice from medical practitioner regarding reducing COVID-19 infection risk and perceived increased susceptibility to COVID-19 compared with general population With regards to current symptom status, moderate and severe disease activity was associated with increased depression, anxiety and/or stress. There was no statistically significant difference between individuals with mild symptoms compared with those who were asymptomatic. Current biological therapy or combination therapy (biological and immunomodulator) were not associated with significant depression, anxiety and/or stress. However, immunomodulator monotherapy was associated with lower depression and anxiety.
Table 4.
Predictors of at least moderate depression, anxiety and stress
| Characteristic | Univariate analysis OR (95% CI) | P value | Multivariate analysis OR (95% CI) | P value |
| Age | 1.94 (1.11 to 3.41) | 0.021 | 0.96 (0.94 to 0.98) | <0.001 |
| Gender | 0.97 (0.96 to 0.99) | 0.002 | 0.796 | |
| Education level | 0.79 | |||
| Employment status | 0.95 | |||
| IBD diagnosis | 0.20 | |||
| Age at IBD diagnosis | 0.98 (0.96 to 0.99) | 0.009 | 0.297 | |
| Current steroid use | 0.161 | |||
| Immunomodulator (IM) and biological use | ||||
| No IM or biologics | Index | 0.014 | 0.008 | |
| Combination therapy | 0.92 (0.47 to 1.83) | 0.819 | 0.69 (0.31 to 1.53) | 0.357 |
| IM monotherapy | 0.33 (0.16 to 0.69) | 0.003 | 0.26 (0.11 to 0.58) | 0.001 |
| Biologics monotherapy | 0.76 (0.39 to 1.46) | 0.408 | 0.76 (0.35 to 1.66) | 0.495 |
| IBD medication knowledge | 0.71 | |||
| IBD medication compliance | 0.16 | |||
| Symptom status: | ||||
| No symptoms | Index | Index | ||
| Mild | 2.08 (1.17 to 3.69) | 0.012 | 1.74 (0.90 to 3.36) | 0.099 |
| Moderate | 3.48 (1.69 to 7.17) | 0.001 | 3.89 (1.69 to 8.93) | 0.001 |
| Severe | 4.03 (1.77 to 9.17) | 0.001 | 3.97 (1.52 to 10.4) | 0.005 |
| Usual caregiver | ||||
| IBD clinic | Index | 0.439 | ||
| General Gastroenterology clinic | 3.28 (1.53 to 7.05) | 0.002 | ||
| Surgeon (Public & Private) | 0.77 (0.12 to 4.84) | 0.78 | ||
| Private Gastroenterologist | 2.12 (1.24 to 3.64) | 0.006 | ||
| General Physician | 1.54 (0.59 to 4.04) | 0.382 | ||
| Lack of access to IBD nurse | 1.65 (1.05 to 2.60) | 0.031 | 1.81 (1.03 to 3.19) | 0.04 |
| Access to gastroenterologist phone-based review | 0.211 | |||
| Lack of advice from medical practitioner regarding reducing COVID-19 infection risk | 1.74 (1.01 to 2.76) | 0.018 | 1.99 (1.13 to 3.50) | 0.017 |
| Perceived increased susceptibility to COVID-19 compared with general population: | ||||
| Strongly agree | Index | Index | ||
| Agree | 0.73 (0.42 to 1.27) | 0.268 | 0.71 (0.38 to 1.35) | 0.302 |
| Neither agree nor disagree | 0.32 (0.17 to 0.61) | 0.001 | 0.22 (0.10 to 0.48) | <0.001 |
| Disagree | 0.24 (0.82 to 0.72) | 0.011 | 0.15 (0.04 to 0.54) | 0.003 |
| Strongly disagree | 0.999 | 0.999 | ||
| Exposure to COVID-19 information on the news and social media | 0.88 | – |
95% CI is displayed for variables with statistically significant differences.
IBD, inflammatory bowel disease.
There was no significant association with gender, education level, employment status, IBD diagnosis, current treatment with steroids, biologics, IBD medication knowledge, IBD medication compliance, gastroenterology phone-based review access and exposure to COVID-19 information on news and social media.
Discussion
Fears of infection and the necessities of social distancing have taken a toll on the mental health of the general population during the COVID-19 pandemic.5 6 People suffering from chronic illness have been found to experience greater distress than the general population during the COVID-19 pandemic.7 Higher rates of pre-existing mental health problems and perceived increased susceptibility to infection may contribute to this. Patients with IBD can be considered in this category. Although several publications have addressed the practical side of managing patients with IBD during the COVID-19 pandemic, the impact of the COVID-19 pandemic on the mental health of patients with IBD is less well understood. Two cross-sectional survey studies have not demonstrated a significant impact of the COVID-19 pandemic or social distancing on the quality of life among adult or paediatric patients with IBD.8 9 A cross-sectional survey study of patients with IBD from Saudi Arabia demonstrated that almost half of respondents had clinical anxiety, however, no respondent reported scores consistent with depression during the pandemic.10 Particularly, this lack of depression in an IBD population is at odds with other findings and may be due to social or cultural differences or a measurement bias due the methodology employed.11 Hence, we advise caution in extrapolating these results to a Western IBD population. Further complicating this matter are differences in the local public health response in terms of social distancing, the local availability of personal protective equipment and the local dynamics of COVID-19 infections and mortality.
Overall, our study population had relatively high rates of depression, anxiety and stress. These were higher than reported rates in the general Australian population (depression 12-month prevalence 4.1%, anxiety 12-month prevalence 14.4%) and previous IBD studies (depression prevalence 9.9%–20.5%, anxiety disorder prevalence 4.9%–36.5%).11 12 A recent pre-COVID19 pandemic study found the prevalence of distress to be 50% among Australian patients with IBD (K10 questionnaire).13 While we did not carry out a matched survey for healthy individuals, a recent study has looked at the mental health of people in Australia in the first month of the COVID-19 restrictions.14 The estimated prevalence of clinically significant symptoms of depression in that study was 27.6% and of clinically significant anxiety at 21%. This is significantly higher than the reported rates in the Australian population in the pre COVID-19 era. Unfortunately, this or other Australian studies, have not reported on the impact of the COVID-19 pandemic on people with pre-existing depression or anxiety. In our study half of all respondents had a diagnosis of anxiety or depression prior to the COVID-19 pandemic. Of those with no prior diagnosis, about a third were found to have at least moderate depression. At least moderate anxiety and stress were also found in a third of respondents without a prior diagnosis of anxiety or depression. This could be as a result of the COVID-19 pandemic, or, alternatively, a proportion of these individuals may have had undiagnosed anxiety or depression that predates the pandemic. It is also possible that there was a degree of response bias. People with pre-existing mental health issues might have been more likely to complete the questionnaire, leading to an overestimation of symptom prevalence.
Multivariate analysis of predictors of significant depression, anxiety and stress, can provide opportunities for interventions to combat the mental health burden of the COVID-19 pandemic among the IBD population. Access to an IBD nurse and advice from medical practitioner on reducing infection risk were two modifiable factors that may protect against significant depression, anxiety and stress. Investing healthcare resources to improve access to IBD nurses and ensure patients can readily access their treating doctor during the COVID-19 pandemic may, therefore, have a positive impact on the mental health of patients with IBD, among the other obvious benefits. Moderate to severe symptomatically active disease also predicted for significant depression, anxiety and stress during the COVID-19 pandemic, as has been found in prior studies.3 Immunomodulator use was associated with lower depression, anxiety and stress. This association remained significant even on multivariate analysis, hence this observation is not only due to reduction in symptoms or reduced use of corticosteroids. Their use to control symptoms may potentially raise less concerns to patients than steroids and biologics during the pandemic. This may also explain why biological monotherapy and combination therapy did not reach statistical significance. The mental well-being of patients also needs to be considered in choosing to follow blanket recommendations for cessation of immunomodulators and biologics among patients with IBD in areas experiencing high infection rates.15 The latest European Crohn's and Colitis organisation (ECCO) guidelines take a more individualised approach and advise for continuation of medications among most uninfected patients with IBD.16
Patients with IBD have been found to have greater fears of COVID-19 infection than the general population.17 Many believe themselves to have higher than average susceptibility to COVID-19. Preliminary studies indicate that overall patients with IBD are not more susceptible to COVID-19 than the general population, and this may only be true for a proportion of patients.18–20 Active IBD has been shown to be a risk factor for severe COVID-19 infection.21 Glucocorticoids and 5-aminosalicylates have been implicated in severe cases of COVID-19 infection among patients with IBD, however, the same has not been clearly demonstrated for immunomodulators and biologics.22–24 A meta-analysis of studies found a lower incidence of COVID-19 infection among IBD populations, when compared with incidence reported in general population studies.25 This lower incidence may reflect higher precautions taken by patients with IBD on average compared with the general population. Nevertheless, the perception of increased susceptibility to COVID-19 was associated with significant depression, anxiety and stress in our study population. A survey among Italian patients with IBD found that half believed themselves to be more susceptible to severe COVID-19 infection, and this resulted in more absence from work.26 Reassurance and evidence-based advice from health providers may address this factor. Of interest, although some have found a negative association between COVID-19 news and social media exposure on mental well-being, this was not the case with our study.27
Technology can assist in ensuring patient with IBD follow-up while maintaining social distancing. In Italy, patients with IBD in the ‘red zone’ were followed up by physicians and psychiatrists using telehealth.28 Although not quantified, many patients reported anxiety and panic attacks, and the telehealth follow-up was beneficial.
Several factors may have impacted our results. Although efforts were made to advertise the study as widely as possible, a degree of selection bias is unavoidable: Individuals with IBD that spend more time on the internet and social media are potentially more likely to have been made aware of this study. Similarly, those with more free time may be more likely to complete the survey. Another limitation of the study is the relatively small sample size of 352 respondents. IBD is estimated to affect around 89 000 persons in Australia, which means our survey captured less than 1% of the affected population.29 Low participation rate could be secondary to the limited time the survey was available online. The survey was run for 3 weeks to capture responses during a period of maximum lock down restrictions. Also, online surveys are less accessible to people who lack computer proficiency and hence they would be under-represented in this study. NSW as a state was over-represented in proportion of responders. NSW did have the greatest proportion of COVID-19 cases compared with other states. The COVID-19 pandemic may hence have been of greater concern on average to patients living in NSW compared with other states, potentially making them more likely to take the time to complete the survey. As the survey was anonymous and patients were not approached directly, reminders could not be sent out to individuals to complete the survey.
As this is a cross-sectional study, we cannot accurately determine how much of the mental health burden observed within our IBD population is a direct effect of the COVID-19 pandemic. Nevertheless, the high rates of depression, anxiety and stress within our study population has highlighted the need for broader studies to be carried out to confirm these findings.
The nature of the data and its analysis may also be a source of bias. Many of our survey questions use Likert scales. Inaccuracy is introduced in multivariate analysis due to an assumption of equidistance between responses, as would be the case with continuous scales.
To conclude, Australian patients with IBD appear to have high rates of mental health problems and the COVID-19 pandemic is a significant exacerbator. Interventions are needed to address this such as improving access to IBD nurses, physician advice and ongoing symptom management. Further studies to monitor rates of depression, anxiety and stress as the pandemic unfolds and to assess the effectiveness of various interventions are required.
Acknowledgments
We would like to acknowledge the help provided by the IBD patients at Blacktown Hospital in pretesting the survey. We would also like to thank Crohn’s and Colitis Australia and the Western Sydney Local Health district with their help in advertising the survey.
Footnotes
Contributors: VK: study supervision MC, NM, LH, MT, GA and VK: study concept, study design MC, NM, MT and VK: recruitment, acquisition of data. MC, NM and VK: statistical analysis, analysis and interpretation of data. MC, NM, GA, LH and VK: Manuscript drafting, critical revision
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: This project was approved by the Western Sydney Local Health District Human Research Ethics Committee (Reference: 2020/ETH01317).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as online supplemental information.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health 2020;17. 10.3390/ijerph17093165. [Epub ahead of print: 02 05 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun 2020;87:40–8. 10.1016/j.bbi.2020.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Byrne G, Rosenfeld G, Leung Y, et al. Prevalence of anxiety and depression in patients with inflammatory bowel disease. Can J of Hepatol 2017;2017:1–6. 10.1155/2017/6496727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. 2nd Ed Sydney: Psychology Foundation, 1995. [Google Scholar]
- 5.Liu CH, Zhang E, Wong GTF, et al. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res 2020;290:113172. 10.1016/j.psychres.2020.113172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.González-Sanguino C, Ausín B, Castellanos Miguel Ángel, et al. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun 2020;87:172–6. 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Louvardi M, Pelekasis P, Chrousos GP, et al. Mental health in chronic disease patients during the COVID-19 quarantine in Greece. Pall Supp Care 2020;18:394–9. 10.1017/S1478951520000528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martinelli M, Strisciuglio C, Fedele F, et al. Clinical and psychological issues in children with inflammatory bowel disease during COVID-19 pandemic. Inflamm Bowel Dis 2020;26:e95–6. 10.1093/ibd/izaa136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azzam NA, Aljebreen A, Almuhareb A, et al. Disability and quality of life before and during the COVID-19 outbreak: a cross-sectional study in inflammatory bowel disease patients. Saudi J Gastroenterol 2020;26:256. 10.4103/sjg.SJG_175_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mosli M, Alourfi M, Alamoudi A, et al. A cross-sectional survey on the psychological impact of the COVID-19 pandemic on inflammatory bowel disease patients in Saudi Arabia. Saudi J Gastroenterol 2020;26:263. 10.4103/sjg.SJG_220_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neuendorf R, Harding A, Stello N, et al. Depression and anxiety in patients with inflammatory bowel disease: a systematic review. J Psychosom Res 2016;87:70–80. 10.1016/j.jpsychores.2016.06.001 [DOI] [PubMed] [Google Scholar]
- 12.Australian Bureau of Statistics National survey of mental health and wellbeing: 2007 summary of results, 2008. Available: https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4326.0Main+Features32007?OpenDocument
- 13.Crohn’s and Colitis Australia My IBD experience: Australian inflammatory bowel disease patient experience of health care research report 2018; 2018.
- 14.Fisher JR, Tran TD, Hammarberg K, et al. Mental health of people in Australia in the first month of COVID-19 restrictions: a national survey. Med J Aust 2020;213:458–64. 10.5694/mja2.50831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.An P, Ji M, Ren H, et al. Prevention of COVID-19 in patients with inflammatory bowel disease in Wuhan, China. Lancet Gastroenterol Hepatol 2020;5:525–7. 10.1016/S2468-1253(20)30121-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Magro F, Rahier J-F, Abreu C, et al. Inflammatory Bowel Disease Management During the COVID-19 Outbreak: The Ten Do’s and Don’ts from the ECCO-COVID Taskforce. Journal of Crohn’s colitis 2020;14:S798–806. 10.1093/ecco-jcc/jjaa160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grunert PC, Reuken PA, Stallhofer J, et al. Inflammatory Bowel Disease in the COVID-19 Pandemic - the Patients' Perspective. J Crohns Colitis 2020 10.1093/ecco-jcc/jjaa126. [Epub ahead of print: 20 Jun 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.D'Amico F, Peyrin-Biroulet L, Danese S. Inflammatory bowel diseases and COVID-19: the invisible enemy. Gastroenterology 2020;158:2302–4. 10.1053/j.gastro.2020.04.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allocca M, Fiorino G, Zallot C, et al. Incidence and patterns of COVID-19 among inflammatory bowel disease patients from the Nancy and Milan cohorts. Clin Gastroenterol Hepatol 2020;18:2134–5. 10.1016/j.cgh.2020.04.071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh S, Khan A, Chowdhry M, et al. Risk of severe coronavirus disease 2019 in patients with inflammatory bowel disease in the United States: a multicenter research network study. Gastroenterology 2020;159:1575–8. 10.1053/j.gastro.2020.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bezzio C, Saibeni S, Variola A, et al. Outcomes of COVID-19 in 79 patients with IBD in Italy: an IG-IBD study. Gut 2020;69:1213–7. 10.1136/gutjnl-2020-321411 [DOI] [PubMed] [Google Scholar]
- 22.Neurath MF COVID-19 and immunomodulation in IBD. Gut 2020;69:1335–42. 10.1136/gutjnl-2020-321269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brenner EJ, Ungaro RC, Gearry RB, et al. Corticosteroids, but not TNF antagonists, are associated with adverse COVID-19 outcomes in patients with inflammatory bowel diseases: results from an international registry. Gastroenterology 2020;159:481–91. 10.1053/j.gastro.2020.05.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khan N, Patel D, Xie D, et al. Impact of anti-tumor necrosis factor and thiopurine medications on the development of COVID-19 in patients with inflammatory bowel disease: a nationwide Veterans administration cohort study. Gastroenterology 2020;159:1545–6. 10.1053/j.gastro.2020.05.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aziz M, Fatima R, Haghbin H, et al. The incidence and outcomes of COVID-19 in IBD patients: a rapid review and meta-analysis. Inflamm Bowel Dis 2020;26:e132–3. 10.1093/ibd/izaa170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Occhipinti V, Pastorelli L. Challenges in the Care of IBD Patients During the CoViD-19 Pandemic: Report From a "Red Zone" Area in Northern Italy. Inflamm Bowel Dis 2020;26:793–6. 10.1093/ibd/izaa084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gao J, Zheng P, Jia Y, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One 2020;15:e0231924. 10.1371/journal.pone.0231924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ciacci C, Siniscalchi M. Tips from the battlefront: psychological support of patients with a chronic illness during the COVID-19 lockdown in four steps. United European Gastroenterol J 2020;8:741–2. 10.1177/2050640620927564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu J, Kariyawasam V, Borody T. IDDF2018-ABS-0034 high age-specific prevalence of inflammatory bowel disease amongst the elderly in the city of Canada Bay area, Sydney: a metropolitan, population-based study. Gut 2018;67:A35–6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgast-2020-000581supp001.pdf (84KB, pdf)