Abstract
Objective
Assess the quality of a new disposable nasopharyngolaryngoscope (NPL) through resident feedback at multiple academic institutions and provide a cost analysis of reusable and disposable NPLs at a single academic center.
Study Design
An online survey was distributed to residents at institutions throughout the United States that have implemented use of a disposable NPL (Ambu aScope 4 Rhinolaryngo).
Setting
Cost analysis performed at a single academic center. Resident survey distributed to multiple residency programs throughout the United States.
Subjects and Methods
The survey collected demographic information and asked residents to rate the new disposable NPL and other reusable NPLs using a 5‐point Likert scale. A cost analysis was performed of both reusable and disposable NPLs using information obtained at a single academic center.
Results
The survey was distributed to 109 residents throughout the country and 37 were completed for a response rate of 33.9%. The disposable NPL was comparable to reusable NPLs based on ergonomics and maneuverability, inferior in imaging quality (P < .001), and superior in setup (P < .001), convenience (P < .001), and rated better overall (P < .04). The disposable NPL was found to be cheaper per use than reusable NPLs at $171.82 and $170.36 compared to $238.17 and $197.88 per use for the reusable NPL if the life span is 1 year and 5 years respectively.
Conclusion
Disposable NPLs may offer an alternative option and initial feedback obtained from resident physicians is favorable. Cost analysis favors disposable NPLs as the cost‐effective option.
Level of Evidence
NA.
Keywords: cost analysis, cost effectiveness, endoscopy
Nasopharyngolaryngoscopes are universally used by otolaryngologists in the diagnosis and treatment of various conditions of the upper aerodigestive tract. This study sought to compare a novel disposable version of the endoscope to the widely used reusable nasopharyngolaryngoscope through cost analysis and survey of residents at institutions who have employed the novel device.
1. INTRODUCTION
Nasopharyngolaryngoscopy (NPL) is widely used within the field of otolaryngology and allows the operator the ability to fully evaluate the upper aerodigestive tract. It is an essential tool in the diagnosis of voice disorders, locating foreign bodies, diagnosis of head and neck cancers, evaluation of the acute airway, and evaluation of many other disorders of the upper aerodigestive tract. 1 , 2 NPL also has therapeutic uses including aiding in removal of foreign bodies, vocal cord injections, and use of laser to remove vocal cord lesions. 3
NPLs are used both in the clinic setting and within the hospital for inpatient and emergency department consultations. In between uses, the reusable NPL requires reprocessing given their exposure to blood, body fluids, and microorganisms to avoid cross‐contamination and this process requires time and resources. 4
Similar to NPLs, bronchoscopes also require reprocessing between uses. In recent years, a single‐use or disposable version of the bronchoscope has been introduced and is widely used in a variety of clinical settings, negating the need for reprocessing. Several studies have compared the cost of reusable bronchoscopes to disposable bronchoscopes. These studies have shown that the disposable bronchoscopes are comparable in cost to reusable bronchoscopes and that cost of reusable bronchoscopes depends on the initial purchasing cost of the bronchoscopes, cost of maintenance and repairs, the cost of reprocessing, and the number of uses of the bronchoscopes. 5 , 6 , 7 , 8
Within the past year, a single‐use or disposable version of the NPL has been produced and implemented at several institutions within the United States. Currently there is no study in the literature evaluating the cost of reusable NPLs compared to disposable NPLs. In addition, there is no published literature that evaluates resident feedback on the use of disposable NPLs. This study sought to provide a cost analysis of reusable NPLs at an academic center to be compared to the cost of disposable NPLs as well as obtain initial feedback from residents at institutions regarding disposable NPLs in comparison to reusable NPLs.
2. MATERIALS AND METHODS
2.1. Resident survey
A list of institutions with otolaryngology residency programs that had instituted use of the Ambu aScope 4 Rhinolaryngo was obtained from the Ambu Incorporation. The Ambu aScope 4 Rhinolaryngo is a disposable version of an NPL intended for single use and requires connection to an Ambu monitor for viewing with the capability to record and still‐capture images during the procedure. The list included a total of nine institutions with otolaryngology residency programs. One of the institutions has residents from two separate residency programs rotate at the hospital.
A survey was then designed to obtain feedback from residents including demographic information and feedback for both the disposable NPL and other reusable NPLs. The survey utilized a 3‐point Likert scale rating to assess resident feedback on the ease of learning to use the NPLs. The survey utilized a 5‐point Likert scale to assess resident feedback on imaging quality, maneuverability, ergonomics, setup, convenience, and overall ratings. Imaging was explained as the visual quality seen on screen or through the NPL. Maneuverability was described as the ease with which the NPL was passed through the upper aerodigestive tract and includes size and tip bending of the NPL. Ergonomics was described as feel of the NPL in the hands including weight, shape, and texture. Setup was described as the ease of setting up the NPL for use including connecting to a screen, focusing the NPL, and aligning the camera. Convenience was described as the ease of obtaining the NPL within the hospital along with necessary equipment, transporting the NPL and necessary equipment, and disposing of the NPL and necessary equipment following the procedure.
A Web‐based anonymous survey (www.surveymonkey.com) was created. IRB exemption was obtained from SUNY Upstate Institutional Review Board given that no patient information would be used. The survey was designed to be anonymous. A link to the survey was then sent to program directors of the listed institutions and asked to be forwarded to the residents. Residents were chosen to complete the survey because, similar to the study institution, they are likely performing the majority of inpatient NPLs and more likely to have used the disposable NPL. Emails of individual residents were obtained from residency websites and a link to the survey sent to residents from six of the institutions.
The survey was available for response from February 2nd, 2020 until March 18th, 2020. The mean response rating was calculated for each category based on responses and a t test was then performed to compare responses for the disposable NPL to responses for all other reusable NPLs. The Karl Storz NPL was the most commonly cited other NPL and a t test was performed to compare responses for the disposable NPL to responses for the Karl Storz NPL. A t test was performed to compare responses regarding the ease of learning to use the disposable NPL to other NPLs. A P‐value of <.05 was considered significant.
2.2. Cost analysis
Information was obtained from the study institution for cost analysis of the reusable NPLs including the cost of the initial purchase of the NPLs and necessary equipment, number and cost of repairs in a year‐long span from October 1st, 2018 until September 30, 2019. In addition, the costs associated with reprocessing of the NPLs including staff wages, time, and materials were obtained. The cost of the disposable NPL and associated monitor was also obtained.
To ascertain the number of uses of the NPLs, the medical record was queried utilizing keywords including nasopharyngolaryngoscopy and nasopharyngo‐laryngoscopy from October 1st, 2018 until March 31st, 2019. These keywords were chosen based on medical record templates used for documenting the procedure. Next, the resulting list was cross‐referenced with the patient charts to confirm the procedure was performed. This included only procedures performed within the hospital as consults or on admitted patients. It did not include outpatient procedures. The time frame was prior to implementation of the disposable NPL and therefore all procedures were performed using reusable Karl Storz NPLs. Information was then used to calculate the cost of an individual use of the reusable NPLs.
The calculations are based in part on a similar study that compared the per‐use cost of reusable and disposable bronchoscopes. 9 The initial cost, maintenance, and repair fees were totaled and a per‐use cost was calculated based on the annual uses of scopes. First, the purchasing prices of the reusable scopes were divided by the annual number of uses and a lifespan of 1 and 5 years. The Karl Storz online catalog does not list a specific life span for their NPL; it says “superior life span due to robust mechanical design.” Therefore the cost analysis evaluated the NPL's based on 1 and 5 years as outpatient clinics at the study institution have observed life spans of the endoscopes up to 5 years. Next, this cost was added to the annual repair fee, again divided by the annual number of uses. Finally, maintenance and labor fees for each reprocessing were then added to determine the per‐use cost of the reusable NPLs.
3. RESULTS
3.1. Resident survey
After emails were sent to 10 program directors and directly emailed to 99 residents at six institutions, the survey was distributed to a total of 109 residents and a total of 37 (33.9%) responses were collected. Six of the respondents indicated within the survey that they do not use the disposable NPL and did not complete the remainder of the survey. Therefore, 31 responses were included in data analysis.
Demographic information of resident respondents can be seen in Table 1. None of the institutions that have implemented the disposable NPL were from the Pacific Coast/Northwest. Most respondents, 96.77%, indicated that the disposable NPL is used for consults within the hospital. The Karl Storz reusable NPL was most commonly cited as another NPL that respondents were most familiar with at 87.5% (27 of 31 respondents) and this was commonly used for both consults within the hospital (93.75%) as well as in outpatient clinics (87.5%).
TABLE 1.
Respondent demographic information
| Age | 25‐30 | 31‐35 | |||
| 26 (70.27%) | 11 (29.73%) | ||||
| Gender | Male | Female | |||
| 24 (64.86%) | 13 (35.14%) | ||||
| PGY level | PGY‐1 | PGY‐2 | PGY‐3 | PGY‐4 | PGY‐5 |
| 6 (16.22%) | 8 (21.62%) | 7 (18.92%) | 9 (24.32%) | 7 (18.92%) | |
| Residency location | Northeast | Southeast | Midwest | Southwest | Pacific Coast/Northwest |
| 18 (48.65%) | 6 (16.22%) | 11 (29.73%) | 2 (5.41%) | 0 (0.00%) |
Note: Demographic information of the resident respondents to the survey.
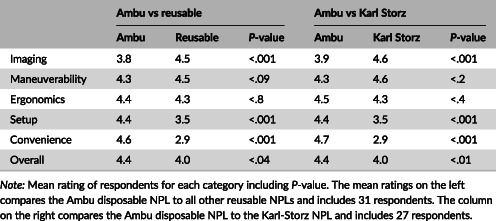
The ratings of the disposable NPL against all other reusable NPLs and the ratings of the disposable NPL against the Karl Storz reusable NPL are summarized in Table 2. Respondents felt that the disposable NPL was inferior in imaging quality to both all reusable NPLs as well as the Karl Storz NPL. Respondents felt that the disposable NPL was comparable in both maneuverability and ergonomics compared to all reusable NPLs as well as the Karl Storz NPL. Respondents felt that the disposable NPL was superior to other reusable NPLs and the Karl Storz NPL in terms of setup and convenience. Respondents rated the disposable NPL more highly overall than all reusable NPLs and more highly than the Karl Storz reusable NPL. Respondents rated the disposable NPL as easier to learn with average response of 2.9 compared to 2.7 for all reusable NPLs (P < .04).
TABLE 2.
Respondent rating averages
| Ambu vs reusable | Ambu vs Karl Storz | |||||
|---|---|---|---|---|---|---|
| Ambu | Reusable | P‐value | Ambu | Karl Storz | P‐value | |
| Imaging | 3.8 | 4.5 | <.001 | 3.9 | 4.6 | <.001 |
| Maneuverability | 4.3 | 4.5 | <.09 | 4.3 | 4.6 | <.2 |
| Ergonomics | 4.4 | 4.3 | <.8 | 4.5 | 4.3 | <.4 |
| Setup | 4.4 | 3.5 | <.001 | 4.4 | 3.5 | <.001 |
| Convenience | 4.6 | 2.9 | <.001 | 4.7 | 2.9 | <.001 |
| Overall | 4.4 | 4.0 | <.04 | 4.4 | 4.0 | <.01 |
Note: Mean rating of respondents for each category including P‐value. The mean ratings on the left compares the Ambu disposable NPL to all other reusable NPLs and includes 31 respondents. The column on the right compares the Ambu disposable NPL to the Karl‐Storz NPL and includes 27 respondents.
3.2. Cost analysis
The cost analysis for both the reusable and disposable NPL was constructed and calculated to produce a per‐use cost for each. The otolaryngology department at the study institution performed 330 NPLs from October 1st, 2018 through March 31st, 2019 using reusable NPLs. Extrapolated to 1 year, the otolaryngology department would perform approximately 660 NPLs. Table 3 summarizes the cost of purchase of the six NPLs utilized by the otolaryngology department and the cost of necessary equipment including two light sources for the NPL, a charger for the light sources, the C‐MAC monitor for viewing, and the VIP Pole which is a cart that allows transport of the monitor. The total cost for this equipment was $33 240.69.
TABLE 3.
Cost listing for reusable NPLs
| Number of uses | 660 |
| Initial purchase of NPL | 24 008.25 |
| Initial purchase of light sources | 1590 |
| Light source charging station | 771.09 |
| C‐MAC monitor | 5858.94 |
| VIP Pole | 1012.41 |
| Total Purchase cost | 33 240.69 |
| Cost of repairs | 106 325 |
| Maintenance fees | |
| Materials | |
| Endozyme sponge (2) | 1.45 |
| Lint‐free wipes (5) | 0.31 |
| Nylon brushes (2) | 2.13 |
| Labor | |
| Staff wages (hourly) | 18 |
| Time to re‐process | 1 hour |
Note: The costs of purchasing the reusable NPLs and associated equipment, cost of repairs in a one‐year time span, number of uses in a one‐year span, costs associated with materials and labor for reprocessing of the reusable NPLs.
The total cost of repairs from October 1st, 2018 through September 30, 2019 was $106 325 for the year. There were a total of 28 repairs.
The reprocessing fees for the reusable NPL included materials and labor costs. The additional costs of the machinery for reprocessing along with detergents and acid solutions were not included as they are used to reprocess all endoscopes within the hospital. Labor fees included the hourly wages of central sterile staff which averages $18.00/hour and the time to re‐process which was reported to be approximately 2 hours, although this was calculated as an estimate for 1 hour as a portion of the reprocessing time requires disinfection and sterilization in an automated reprocessor.
The cost of the disposable NPL was reported as $170 and the monitor cost $1200. Divided over 660 uses, the cost of the monitor adds $1.82 to each procedure in 1 year. Therefore, the per‐use cost of the disposable NPLs for 1 year is $172.82 and for 5 years is $170.36.
Calculations for the per‐use cost of the reusable NPL are summarized in Table 4 and include the cost over a 1‐year and 5‐year span. The initial purchase price per use for 1 year is the initial cost divided by the number of uses (33 240.69/660 uses) and was $50.36. For a 5‐year life span, the cost per use is $10.07 (50.36/5). The annual per‐use cost of repairs was calculated to be $161.10 (106 325/660). The cost of materials for reprocessing each scope was $8.71 and included endozyme sponges (2 at $1.45 each), lint‐free wipes (5 at $0.31 each), and nylon brushes (2 at $2.13). The cost of labor was $18 for approximately 1 hour of reprocessing at an hourly wage of $18.00. These costs were added for each life span. The 1‐year life span (50.36 + 161.10 + 8.71 + 18) totaled $238.17 per use of the reusable NPL. The total cost per use for a life span of 5 years is $197.88.
TABLE 4.
Calculation of costs per‐use of a single NPL
| Reusable NPL | Disposable NPL | |||
|---|---|---|---|---|
| 1 year | 5 years | 1 year | 5 years | |
| Purchase of equipment | $33 240.69 | $6648.14 | $1200.00 | $240.00 |
| Price per use | $50.36 | $10.07 | $1.82 | $0.36 |
| Repair costs | $106 325.00 | N/A | ||
| Price per use | $161.10 | N/A | ||
| Maintenance cost per use | $8.71 | N/A | ||
| Labor cost per use | $18.00 | N/A | ||
| Total cost per use | $238.17 | $197.88 | $171.82 | $170.36 |
Note: Includes the cost of per‐use if the initial purchase cost is spread out over 1 year, 5 year, and 15 year life. Span of the NPL and includes the initial purchase cost, cost of repairs based on 1 year, cost of reprocessing each NPL, and cost of labor to reprocess each NPL.
4. DISCUSSION
Nasopharyngolaryngoscopy is a widely utilized diagnostic tool implemented globally by otolaryngologists. Within the past year, the Ambu corporation has released a disposable version of the NPL, the Ambu aScope 4 Rhinolaryngo. As novel tools, they have not yet been extensively studied as compared to reusable NPLs. This is the first known study to assess feedback from otolaryngologists, specifically residents, regarding the quality of the NPL in comparison to reusable NPLs. It is also the first study, to our knowledge, to analyze the associated costs of reusable NPLs at a single academic center.
Our study shows that the disposable NPL compares favorably to other reusable NPLs and is preferred over reusable NPLs in terms of convenience and setup, but would benefit from improvement in imaging quality. It also was rated as easier to learn than traditional reusable NPLs; however, 100% of respondents indicated that this is not the first NPL that they have learned to use and this difference can likely be attributed to previously acquired endoscopy skills. Currently the disposable NPL is being used predominantly for consultations within the hospital. Nasopharyngolaryngoscopy is frequently required for these consultations and has been cited as necessary in up to 48% of cases with an additional 16% requiring rhinoscopy in one tertiary center. 10 Given the frequent need for endoscopy, convenience and setup are important factors for maintaining efficiency.
The findings of the cost analysis show that per‐use, the disposable NPL is cost‐effective compared to the reusable NPLs. The high per‐use cost of the reusable NPL is attributable predominantly to the high annual costs of repairs of $106 325 in the year that was used for the cost analysis. The main factor driving the higher cost of the reusable NPL is the high cost of repairs. The study institution had a total of 28 repairs in the one‐year time span with average repair cost of $3797.32, averaging $161.10 per use. The system in place at the study center involves sending in the NPL for repairs to Karl Storz. Most (54%) of the time, a repair cost of $4995 was billed in exchange for refurbished NPL to maintain an adequate supply. The clinical engineering department, in an attempt to reduce the cost of repairs, contracted a third‐party repair company. However, on multiple occasions the third‐party was unable to repair the NPL and a refurbished NPL would be charged regardless. Furthermore, these repairs and exchanges would take weeks. This delay led to multiple NPLs being out for repair at once. In fact, it was necessary at one point for the study institution to revert to older NPLs in storage to avoid lapses in patient care. As these endoscopes are utilized in emergent airway situations, this scenario was deemed unacceptable. In the search for alternative solutions, disposable NPLs were later introduced at the study institution.
Statham and Willging in 2010 assessed the cost of repairs on NPLs at an outpatient pediatric practice over a four‐year span and reported 48 major repairs with an average cost of $3815.97 and 29 minor repairs with an average cost of $326.85 on 60 NPLs with a total of 4336 procedures performed. Based on this information, the per‐use repair costs of these NPLs would be $44.43. This per‐use cost of repairs is much lower than at the study institution. However, the repair costs from Statham and Willging were evaluated at an outpatient clinic and from a total of 60 NPLs compared to the 6 NPLs used frequently at the study institution. Utilization at the hospital requires increased transport of the NPLs and handling by a wider variety of staff who reprocess the NPLs which would account for the need for more repairs. The most common reasons for repair included failed leak test, a hole at the distal end, and broken fibers. 11
Various studies have also commented that the sterilization process is often inadequate and inconsistent. 4 One alternative has been the use of disposable sheaths over the NPL. However, these are still prone to tears and do not fully eliminate the need for reprocessing of the NPL. 12 Given the current COVID‐19 pandemic, endoscopy procedures present a high risk for transmission of the SARS‐CoV‐2 virus. Studies on virucidal efficacy of chemical agents against SARS‐CoV‐2 are not available. 13 A disposable NPL would negate the need for reprocessing altogether and mitigate concern for any cross‐contamination between patients.
Limitations of the study include difficulty with distributing the survey to additional institutions. In addition it is unclear whether many of the residents that the survey was distributed to have used the disposable NPL. It was difficult to ascertain which residency programs had actually implemented and utilized the disposable NPL based on the list provided by Ambu. One of the residents responded to the email indicating that they do not use the disposable NPL within the residency program. This residency program includes 25 residents that were included with the 109 residents that received the survey. Residents were instructed to not fill out the survey if they have not used the disposable NPL and this likely falsely lowered the response rate. It was also difficult to estimate the cost of certain materials in our cost analysis of the reusable NPL including cost of detergents, acids, and the machinery required for reprocessing and for that reason it is likely that the per‐use cost of the reusable NPL was actually underestimated.
5. CONCLUSION
Disposable NPLs may offer an alternative option to traditional reusable NPLs and initial feedback from resident physicians is favorable. It was rated superior in regards to setup, convenience, and rated better overall. It was found to be comparable in regards to ergonomics and maneuverability. It was rated inferior regarding imaging quality. Implementation of the disposable NPL for use by otolaryngologists may decrease cross‐contamination of disease and given the results of the cost analysis may offer a more cost‐effective option than traditional reusable NPLs which have high associated repair costs.
AUTHOR CONTRIBUTIONS
Ryan Walczak involved in the study design, data collection, data analysis, manuscript author. Mark Arnold involved in the data analysis, critical revision. Jeewanjot Grewal and Xiao Yuan involved in the data collection. Amar Suryadevara and Haidy Marzouk involved in the study conception and design, data interpretation, and critical revision.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
Walczak R, Arnold M, Grewal J, Yuan X, Suryadevara A, Marzouk H. Reusable vs disposable nasopharyngolaryngoscopes: Cost analysis and resident survey. Laryngoscope Investigative Otolaryngology. 2021;6:88–93. 10.1002/lio2.500
BIBLIOGRAPHY
- 1. Selkin SG. Routine use of office endoscopy in otolaryngology. Otolaryngology–Head and Neck Surgery. 1986;95(4):425‐428. 10.1177/019459988609500401. [DOI] [PubMed] [Google Scholar]
- 2. Silberman HD, Wilf H, Tucker JA. Flexible fiberoptic NPL. Ann Otol Rhinol Laryngol. 1976;85(5):640‐645. 10.1177/000348947608500513. [DOI] [PubMed] [Google Scholar]
- 3. Motz KM, Hillel AT. Office‐based management of recurrent respiratory papilloma. Curr Otorhinolaryngol Rep. 2016;4(2):90‐98. 10.1007/s40136-016-0118-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Muscarella LF. Prevention of disease transmission during flexible laryngoscopy. Am J Infect Control. 2007;35(8):536‐544. 10.1016/j.ajic.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 5. Terjesen CL, Kovaleva J, Ehlers L. Early assessment of the likely cost effectiveness of single‐use flexible video bronchoscopes. PharmacoEconomics – Open. 2017;1(2):133‐141. 10.1007/s41669-017-0012-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Perbet S, Blanquet M, Mourgues C, et al. Cost analysis of single‐use (Ambu® aScope™) and reusable bronchoscopes in the ICU. Ann Intensive Care. 2017;7(1). 10.1186/s13613-016-0228-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Aïssou M, Coroir M, Debes C, et al. Analyse de coût comparant les fibroscopes à usage unique (Ambu®aScope™) et les fibroscopes réutilisables pour l'intubation difficile [Cost analysis comparing single‐use (Ambu® aScope™) and conventional reusable fiberoptic flexible scopes for difficult tracheal intubation]. Ann Fr Anesth Reanim. 2013;32(5):291‐295. 10.1016/j.annfar.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 8. Tvede MF, Kristensen MS, Nyhus‐Andreasen M. A cost analysis of reusable and disposable flexible optical scopes for intubation. Acta Anaesthesiol Scand. 2012;56(5):577‐584. 10.1111/j.1399-6576.2012.02653.x. [DOI] [PubMed] [Google Scholar]
- 9. Gupta D, Wang H. Cost‐effectiveness analysis of flexible optical scopes for tracheal intubation: a descriptive comparative study of reusable and single‐use scopes. J Clin Anesth. 2011;23(8):632‐635. 10.1016/j.jclinane.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 10. Carr MM. Improving the otolaryngology consultation Service in a Teaching Hospital. Laryngoscope. 2001;111(7):1166‐1168. 10.1097/00005537-200107000-00007. [DOI] [PubMed] [Google Scholar]
- 11. Statham MM, Willging JP. Automated high‐level disinfection of nonchanneled flexible endoscopes: duty cycles and endoscope repair. Laryngoscope. 2010;120(10):1946‐1949. 10.1002/lary.21051. [DOI] [PubMed] [Google Scholar]
- 12. Silberman HD. Non‐inflatable sterile sheath for introduction of the flexible NPL. Ann Otol Rhinol Laryngol. 2001;110(4):385‐387. 10.1177/000348940111000417. [DOI] [PubMed] [Google Scholar]
- 13. Rameau A, Young VN, Amin MR, Sulica L. Flexible laryngoscopy and COVID‐19. Otolaryngology–Head Neck Surg. 2020;162:813‐815. 10.1177/0194599820921395. [DOI] [PubMed] [Google Scholar]


