Abstract
Objective
Characterize sinonasal complications associated with endoscopic orbital decompression for thyroid eye disease (TED).
Methods
Retrospective analysis of patients who underwent endoscopic orbital decompression at Houston Methodist Hospital by two otolaryngologists and one ophthalmologist between May 2016 and February 2020 for TED. Patient ethnicity, age, laterality, operative approach (middle turbinectomy vs middle turbinate sparing), and history of prior sinusitis were collected.
Results
One hundred and forty‐five orbital decompressions met the inclusion criteria. Postoperative obstructive sinusitis where herniated orbital fat caused obstruction of the sinus ostium occurred in 5.5% of operations. Patients who had a prior history of sinusitis were more likely to develop postoperative obstructive sinusitis (P = .02). The middle turbinectomy approach was more likely to show a reduced incidence of postoperative sinusitis (P = .014).
Conclusion
Given the increased difficulty of managing sinonasal complications in the context of a decompressed orbit, efforts should be made to identify factors that might reduce the incidence of postoperative endonasal complications. The current study suggests that resection of the middle turbinate may allow for increased space for orbital fat herniation and lead to a decreased incidence of postoperative obstructive sinusitis.
Level of Evidence
IV.
Keywords: adult rhinology, Graves' disease, orbital decompression, outcomes/cost effectiveness, scholarly databases, sinusitis, statistics, thyroid eye disease
.
Sinonasal complications related to endoscopic orbital decompression and the factors that predict them are not well established in the literature. The current manuscript is a retrospective review identifying the rate/predictive factors of postoperative sinusitis following endoscopic orbital decompression for Thyroid Eye Disease.
1. INTRODUCTION
Thyroid eye disease (TED) refers to group of autoimmune disorders affecting the eyes, often but not always in the presence of thyroid hormone level abnormalities, as found in Graves' disease or Hashimoto's thyroiditis. 1 Taken as a whole, autoimmune thyroid disorders (ATDs) are among the most common autoimmune disorders in the United States with thyroid hormone replacement ranking among the most frequently prescribed medications in the country. 2 , 3 Nearly half of patients with ATDs develop some manifestations of TED, which may include dry eye, tearing, conjunctival hyperemia, eyelid retraction, chronic eyelid edema, ocular hypertension, periocular and ocular pains, uveitis, proptosis, exposure keratopathy, and diplopia, 4 and up to 5% may develop vision‐threatening complications such as corneal ulceration, recalcitrant glaucoma, and stretch or compressive optic neuropathy. 5 , 6
Among other changes in the orbit, TED often causes inflammation and scarring of the extraocular muscles, sometimes leading to massive enlargement, and the transformation of orbital fibroblasts into new and expanding adipocytes. 7 The increase in orbital tissue volume and the conical shape of the bony orbit may lead to apical compression of the optic nerve. 8 While nonsteroidal therapies, external beam irradiation, and corticosteroids and other immunomodulators may modify the active, progressive phase of TED, 9 once anatomic changes have occurred, surgical correction may be necessary to manage sight‐threatening complications.
Several strategies exist to manage the tight orbit through orbital decompression, including transcranial, transfacial, transconjunctival, and transnasal approaches. 10 Dual approach transconjunctival and endonasal endoscopic decompressions is often performed due to enhanced visualization of both intraorbital structures and the skull base with no skin incision. 10 While several studies have examined the ophthalmologic outcomes following endoscopic endonasal decompression, few studies have examined the sinonasal complications. 11
The purpose of the current study is to characterize sinonasal complications in a cohort of patients that underwent combined transconjunctival and endonasal endoscopic orbital decompression for TED, assess the impact of a prior history of sinusitis, examine the causes of postoperative sinusitis, and explore the impact of removing or preserving the middle turbinate.
2. METHODS
The study was a retrospective analysis of all patients who underwent endoscopic endonasal orbital decompression by two otolaryngologists and one ophthalmologist at Houston Methodist Hospital between May 30th, 2016, and February 28th, 2020 for TED. The study was performed in compliance with the Institutional Review Board at Houston Methodist Hospital. Patient ethnicity and age, side of operation (right or left), and type of sinus surgery performed (removal or sparing of the middle turbinate) were collected.
Two operative approaches were compared—the middle turbinectomy approach and the middle turbinate sparing approach. In the middle turbinate‐sparing approach, the middle turbinate was medially fractured to gain access to the maxillary ostium, but was not resected. In the middle turbinectomy approach, the middle turbinate was either partially or completely resected at the time of the operation. The choice of whether to resect or keep the middle turbinate was based on surgeon preference. Operative reports for each orbital decompression operation were reviewed to determine whether the middle turbinate was taken in the operation. Furthermore, the patient's medical records (preoperative history and physical examination or operative notes) were reviewed to determine whether the patient had a history of sinusitis prior to their orbital decompression. All patients who stated that they had a prior history of sinusitis were included, and the extent of sinusitis was not investigated (frequent antibiotic use, duration, etc). Patients were generally expected to follow up with the otolaryngologist 1 week and 1 month following their operation.
Complications following the procedure were also collected from the medical record. Importantly, patient complications could only be noted if they returned to the original hospital for further management.
2.1. Statistics
One‐tailed two proportion z‐test was used to perform comparisons of proportions. Binary logistic regression analysis was used to further evaluate middle turbinate preservation and prior history of sinusitis as predictors of postoperative obstructive sinusitis. All statistical analyses were carried out using SPSS (IBM SPSS Statistics for Windows, Version 25.0; IBM Corp, Armonk, New York).
3. RESULTS
A total of 145 endoscopic endonasal orbital decompressions were performed in the study time period on 93 patients. Fifty patients (53.8%) received bilateral orbital decompressions. Of these procedures, 41 were middle turbinate sparing (28.3%), while 104 (71.7%) middle turbinectomies were performed. Ethnicity and age were not significantly different between the two groups (Table 1).
TABLE 1.
Characteristics of patients that underwent endoscopic orbital decompression
| Middle turbinectomy (n = 104) | Middle turbinate sparing (n = 41) | |||
|---|---|---|---|---|
| Ethnicity | Caucasian | 78 (71.6%) | 31 (28.4%) | P = 1.0 |
| African American | 15 (71.4%) | 6 (28.6%) | ||
| Asian/Pacific Islander | 6 (75.0%) | 2 (25.0%) | ||
| Hispanic | 5 (71.4%) | 2 (28.6%) | ||
| Age | 55.76 | 54.66 | P = .61 | |
| Laterality | Right | 42 (40.4%) | 18 (43.9%) | P = .84 |
| Left | 62 (59.6%) | 23 (56.1%) | ||
| Preoperative sinusitis | 13 (12.5%) | 4 (9.8%) | P = .32 |
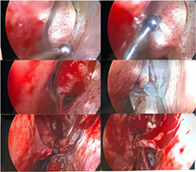
Seven patients (8 total sides) were noticed to have herniated orbital contents that blocked the osteomeatal complex (OMC) and developed obstructive sinusitis. Figure 1 shows an example of such a patient in which the middle turbinate became scarred against the opening of the maxillary sinus in a manner that caused obstructive sinusitis. Upon removing the middle turbinate, it became clear that herniated orbital fat contents were responsible for the obstruction of the OMC. The overall rate of sinusitis requiring reoperation in the current cohort was 5.5%.
FIGURE 1.

Middle turbinate scarred against the opening of the maxillary sinus due to herniated orbital fat. A middle turbinectomy is performed and the opening of the maxillary sinus is widened
3.1. History of prior sinusitis
First, we evaluated whether a preoperative history of sinusitis would increase the likelihood of developing obstructive sinusitis postoperatively (Figure 2). A significantly higher percentage of patients who developed postoperative obstructive sinusitis had a prior history of sinusitis (37.5%), compared to only 10.2% of patients who had no sinusitis complications following surgery (P = .02). In the binary logistic regression model, a prior history of sinusitis was found to be a significant predictor of postoperative obstructive sinusitis (odds ratio (OR) = 6.99, P = .02, Table 2).
FIGURE 2.

Incidence of preoperative sinusitis based on postoperative complications—a comparison of the percentage of patients that had a prior history of sinusitis based on development of postoperative obstructive sinusitis (P = .02)
TABLE 2.
Binary logistic regression evaluating postoperative sinusitis
| Evaluated risk factor | Odds ratio | 95% Confidence interval | P value |
|---|---|---|---|
| Middle turbinate sparing approach | 5.48 | (1.16, 25.90) | .032 |
| History of sinusitis | 6.99 | (1.36, 36.16) | .020 |
3.2. Middle turbinate removal
Given that removal of the middle turbinate allows more space for herniated orbital contents following decompression of the orbit, we hypothesized that a middle turbinectomy approach would lower the incidence of sinusitis. Postoperative obstructive sinusitis due to orbital fat herniation was found to be significantly lower in the middle turbinectomy groups (2.88%) compared to the group in which the middle turbinate remained (12.20%) (P = .013, Figure 3). Furthermore, between these two groups, the rates of preoperative sinusitis were not significantly different between the middle turbinectomy (12.5%) and middle turbinate sparing (9.8%) groups (P = .32, Table 1). In the binary logistic regression model, the use of a middle turbinate sparing approach was associated with an increased risk of developing postoperative sinusitis (OR = 5.48, P = .032, Table 2).
FIGURE 3.

Middle turbinectomy vs turbinate sparing—incidence of postoperative sinusitis based on either a middle turbinectomy or middle turbinate sparing approach (P = .014)
3.3. Management of sinusitis complications
The sinusitis caused by orbital fat herniation was most frequently maxillary sinusitis (87.5%), with one case being caused by frontal sinusitis (12.5%) (Table 3). When the middle turbinate remained, most patients (80%) received a middle turbinectomy and a maxillary antrostomy to open up the maxillary sinus, while one patient required only a maxillary antrostomy (20%). The patient that developed frontal sinusitis required a nasofrontal duct dilation in addition to a middle turbinectomy. In the patients who developed sinusitis following an orbital decompression with a middle turbinectomy, one patient developed orbital fat related sinusitis bilaterally and required bilateral maxillary antrostomy to improve the drainage of the maxillary sinus. Finally, the last patient that developed maxillary sinusitis following a middle turbinectomy had an endoscopic middle meatus maxillary antrostomy followed by a partial inferior turbinectomy (Table 3).
TABLE 3.
Characteristics of patients with sinusitis complications due to orbital fat herniation
| Patient | Middle turbinate | Preoperative sinusitis | Emergent | Reason | Procedure | Days to reoperation |
|---|---|---|---|---|---|---|
| 1 | Spared | No | Yes | OC; MS | MA; MT | 176 |
| 2 | Spared | Yes | No | MS | MA; MT | 118 |
| 3 | Spared | No | No | MS | MA | 357 |
| 4 | Spared | No | No | FS | NFD; MT | 42 |
| 5 | Spared | No | No | MS | MA; MT | 47 |
| 6 | Taken | Yes | No | MS | MA | 272 |
| 6 | Taken | Yes | No | MS | MA | 265 |
| 7 | Taken | No | No | OC; MS | MA; PIT | 38 |
Abbreviations: FS, frontal sinusitis; MA, maxillary antrostomy; MS, maxillary sinusitis; MT, middle turbinectomy; NFD, nasal frontal duct dilation; OC, orbital cellulitis; PIT, partial inferior turbinectomy.
The average time to reoperation for orbital content related sinusitis was slightly longer in the middle turbinectomy group (164 days) compared to the middle turbinate sparing group (148 days); however, this difference was not significant (P = .66). In two cases, patients presented with orbital cellulitis along with maxillary sinusitis (Table 3). Only one patient required reoperation emergently.
4. DISCUSSION
4.1. Sinusitis following endoscopic orbital decompression
Endonasal sinusitis complications following endoscopic orbital decompression are not well described in the literature. While the incidence of these complications is fairly rare, management of these issues becomes significantly more challenging in the context of a decompressed orbit. The incidence of common endonasal complications (sinusitis and bleeding) have been explored previously, 11 but the factors that specifically lead to reoperation have not been thoroughly studied.
It is important to note that most studies in the literature do not specifically differentiate between sinusitis caused by OMC obstruction by orbital fat and chronic sinusitis that occurs outside of the context of Graves' disease. 11 , 12 The current study specifically focuses on the development of obstructive sinusitis secondary to orbital fat herniation and OMC obstruction, which is uniquely related to the procedure. 13
Previously, the incidence of sinusitis secondary to maxillary/frontal sinusitis following endoscopic orbital decompression was noted to be as high as 20%. 10 , 14 The rate of sinusitis described in this cohort (5.5%) is fairly low; however, this complication can still require reoperation and can threaten a patient's vision. Therefore, special effort should be made to identify factors that might lead to a reduction in rates of sinusitis and subsequent reintervention.
4.2. Factors leading to increased risk of postoperative obstructive sinusitis
In the current study, we first explored whether a history of preoperative sinusitis would lead to a higher incidence of postoperative obstructive sinusitis. A patient's preoperative history of sinusitis is relevant to understanding the overall health of the sinonasal cilia that exist in a patient's nose. Having a history of chronic rhinosinusitis was found to be associated with increased likelihood of developing obstructive sinusitis complications postoperatively. These findings are consistent with the study performed by Antisdel et al, which found that a history of chronic rhinosinusitis significantly correlated to postoperative obstructive sinusitis. 11 Given the increased difficulty of operating on patients that already have a decompressed orbit, it is critical to identify factors that might prevent reoperation in these patients. Our finding that a prior history of sinusitis leads to an increased risk of postoperative sinusitis suggests the possible need to be more aggressive during the initial surgery in improving sinus drainage.
We also found that resection of the middle turbinate was associated with a reduced incidence of postoperative obstructive sinusitis when compared to a middle turbinate sparing approach. This is possibly due to the fact that leaving the middle turbinate when performing the decompression would limit the space necessary for orbital fat to herniate appropriately. The removal of the middle turbinate during endoscopic sinus surgery is often performed with minimal adverse consequences with regards to quality of life status or olfactory function. 15 In the literature, operative approaches with regards to the middle turbinate vary in endoscopic orbital decompression. Antisdel et al reported in a study utilizing a partial middle turbinectomy approach that the incidence of patients with sinusitis requiring lysis reported was 1.2%, similar to the 2.9% found in the current study for the middle turbinectomy approach. 11 However, in a cohort of 62 patients of middle turbinate sparing endoscopic orbital decompressions, Kasperbauer and Hinkley found that only two patients (3.4%) had obstructive sinusitis. 12 Therefore, future study is warranted to reconcile the differences seen between these techniques.
Performing an endoscopic orbital decompression is a relatively unique procedure in that sinonasal anatomy is altered usually in the absence of active sinus disease. Therefore, it may be appealing to avoid relatively aggressive measures such as resection of the middle turbinate. In some instances, the turbinate sparing approach may be an appropriate option. For example, in predominately posterior orbital decompressions for optic nerve compression, significant globe recession is neither required nor desirable for management of the TED pathology. Furthermore, if the anteromedial bone strut between the orbital floor and orbital medial wall are left intact anteriorly to prevent inferior and medial globe displacement, middle turbinate resection may be unnecessary. However, in the absence of these features, the results of the current study point to the possible need for more aggressive management in patients at high risk of postoperative complications, such as those with a preoperative history of sinusitis.
Finally, the results of this study point to the need for consistent follow‐up of patients who undergo orbital decompressions for several months following the procedure. While the exact time frame for developing sinusitis complications is unknown, following up patients who undergo endoscopic orbital decompression for several months can ensure that proper reintervention is performed if deemed necessary.
4.3. Study limitations
There are several limitations to this study. First, the total number of patients with orbital fat leading to obstructive sinusitis in the current study is low, limiting the overall power of the conclusions. However, this is has been noted to be a problem noted in many other studies performed on endoscopic orbital decompression as well, and remains an issue in evaluating complications associated with the procedure. 10 , 11
Furthermore, the current study only evaluates the sinusitis complications of the patients that returned to the original hospital for management of their complications. Patients in the current cohort traveled long distances to receive their orbital decompressions, and may have elected to manage postoperative complications locally. Therefore, the actual rate of sinonasal complications following endoscopic orbital decompressions is likely higher than what is reported in the current cohort and in the literature.
The retrospective nature of the study also increases the risk of having confounding variables that affect the conclusions drawn, especially when considering resection of the middle turbinate. In the current study, the demographic characteristics and incidence of prior sinusitis was not significantly different between middle turbinectomy and middle turbinate sparing groups. However, other confounding variables have the potential to affect the conclusions drawn. Ideally, a prospective study should be done, randomly assigning patients to either a middle turbinate sparing or middle turbinectomy approach to ensure that the results of the current study are applicable in general clinical practice.
Furthermore, while the current study evaluated two hypothesis for the potential causes of sinusitis following endoscopic orbital decompression (previous history of sinusitis/sparing the middle turbinate), there are several others that likely should be evaluated in future studies. First, our study does not explicitly address the size of the decompression performed or the size of the maxillary ostium when considering complications. It stands to reason that larger decompressions with more fat herniation along with a smaller maxillary ostium would lead to increased incidence of obstructive sinusitis. The current study lacks objective measurement of the volume of fat prolapsed from the orbit into the sinus following orbital decompression, which is something that should be evaluated in future studies. Features such as these are important in reviewing ways to reduce postoperative sinusitis following endoscopic orbital decompression.
5. CONCLUSION
Postoperative sinusitis after orbital decompression commonly occurs from orbital fat herniation blocking the maxillary sinus ostium due to obstruction or scarring. Sinusitis following orbital decompression frequently occurs in the maxillary sinus, but has also been shown to involve the frontal sinus. A prior history of sinusitis is associated with an increased incidence of postoperative obstructive sinusitis. Resection of the middle turbinate may allowed for reduced incidence of postoperative sinusitis in these high‐risk patients.
CONFLICT OF INTEREST
The authors declare no potential conflicts of interest with respect to research, authorship, and/or publication of this article.
Suresh R, Soparkar CN, Alford EL. Sinonasal complications associated with endoscopic orbital decompression. Laryngoscope Investigative Otolaryngology. 2021;6:71–76. 10.1002/lio2.531
REFERENCES
- 1. Leong SC, White PS. Outcomes following surgical decompression for dysthyroid orbitopathy (Graves' disease). Curr Opin Otolaryngol Head Neck Surg. 2010;18(1):37‐43. [DOI] [PubMed] [Google Scholar]
- 2. Jacobson DL, Gange SJ, Rose NR, Graham NM. Epidemiology and estimated population burden of selected autoimmune diseases in the United States. Clin Immunol Immunopathol. 1997;84(3):223‐243. [DOI] [PubMed] [Google Scholar]
- 3. Fuentes AV, Pineda MD, Venkata KCN. Comprehension of top 200 prescribed drugs in the US as a resource for pharamcy teaching, training and practice. Pharamcy. 2018;6(2):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bahn RS. Graves' ophthalmopathy. N Engl J Med. 2010;362(8):726‐738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wiersinga WM, Bartalena L. Epidemiology and prevention of Graves' ophthalmopathy. Thyroid. 2002;12(10):855‐860. [DOI] [PubMed] [Google Scholar]
- 6. Cascone P, Rinna C, Reale G, Calvani F, Iannetti G. Compression and stretching in Graves orbitopathy: emergency orbital decompression techniques. J Craniofac Surg. 2012;23(5):1430‐1433. [DOI] [PubMed] [Google Scholar]
- 7. Weiler DL. Thyroid eye disease: a review. Clin Exp Optom. 2017;100(1):20‐25. [DOI] [PubMed] [Google Scholar]
- 8. Alford EL, Soparkar CN. Management of the 'tight orbit' and associated visual loss. Curr Opin Otolaryngol Head Neck Surg. 2013;21(4):417‐422. [DOI] [PubMed] [Google Scholar]
- 9. Strianese D. Update on Graves disease: advances in treatment of mild, moderate and severe thyroid eye disease. Curr Opin Ophthalmol. 2017;28(5):505‐513. [DOI] [PubMed] [Google Scholar]
- 10. Chu EA, Miller NR, Lane AP. Selective endoscopic decompression of the orbital apex for dysthyroid optic neuropathy. Laryngoscope. 2009;119(6):1236‐1240. [DOI] [PubMed] [Google Scholar]
- 11. Antisdel JL, Gumber D, Holmes J, Sindwani R. Management of sinonasal complications after endoscopic orbital decompression for Graves' orbitopathy. Laryngoscope. 2013;123(9):2094‐2098. [DOI] [PubMed] [Google Scholar]
- 12. Kasperbauer JL, Hinkley L. Endoscopic orbital decompression for Graves' ophthalmopathy. Am J Rhinol. 2005;19(6):603‐606. [PubMed] [Google Scholar]
- 13. Remulla HD, Gliklich RE, Metson R, Rubin PA. Delayed orbital infection after endoscopic orbital decompression for dysthyroid orbitopathy. Ophthalmology. 2000;107(5):947‐950. [DOI] [PubMed] [Google Scholar]
- 14. Gulati S, Ueland HO, Haugen OH, Danielsen A, Rodahl E. Long‐term follow‐up of patients with thyroid eye disease treated with endoscopic orbital decompression. Acta Ophthalmol. 2015;93(2):178‐183. [DOI] [PubMed] [Google Scholar]
- 15. Soler ZM, Hwang PH, Mace J, Smith TL. Outcomes after middle turbinate resection: revisiting a controversial topic. Laryngoscope. 2010;120(4):832‐837. [DOI] [PMC free article] [PubMed] [Google Scholar]


