Abstract
Background and objectives
The role of schools in the spread of SARS-CoV-2 infections in the community is still controversial. The objective of our study was to describe the epidemiology of SARS-CoV-2 infections in different pediatric age groups during the first 2 months of the fall back-to-school period, in the context of increasing viral transmission in France.
Methods
Weekly epidemiological data provided by Santé Publique France and the Ministry of National Education were analyzed according to the age groups defined by the different school levels. Weeks (W) 34–42 were considered for analysis.
Results
The PCR positivity rate and incidence rate increased in all age groups during the study period, in an age-dependent manner. At W42, with adults being considered as reference, the risk ratio for a positive PCR test was 0.46 [95% CI: 0.44–0.49] and 0.69 [0.68–0.70] for children aged 0–5 years and 6–17 years, respectively. Similarly, the incidence rate ratio was 0.09 [0.08–0.09], 0.31 [0.30–0.32], 0.64 [0.63–0.66], and 1.07 [1.05–1.10] for children aged 0–5 years, 6–10 years, 11–14 years, and 15–17 years, respectively. Children and adolescents accounted for 1.9% of the newly hospitalized patients between W34 and W42, and for 1.3% of new intensive care admissions. No death was observed. Among infected children and adolescents, the percentage of asymptomatic individuals was 57% at W34 and 48% at W42. The number of schools closed remained low, less than 1% throughout the study period. The number of confirmed cases among school staff was consistent with the data measured in the general population.
Conclusion
In the context of increasing viral transmission in the population, the spread among children and adolescents remained lower than that observed among adults, despite keeping schools open. However, the impact was age-dependent, with data in high schools close to those observed in adults.
Keywords: SARS-CoV-2, Lockdown, Children, Adolescents, PCR
1. Introduction
Children have a very unique position in the COVID-19 pandemic. Infected children rarely develop severe forms of the disease [1], [2], [3], and there is considerable epidemiological evidence in favor of reduced susceptibility to infection [4], [5] and reduced ability to transmit the infection [6], [7], [8], [9]. These data have called into question the usefulness of the school closures that accompanied the first lockdown measures in most countries in the spring of 2020. This questioning was all the more necessary since these school closures were accompanied by numerous deleterious effects on the physical and mental health of children and by increased social inequalities [10], [11], [12], [13].
As soon as the first lockdown was over, the French Pediatric Society advocated to reopen the schools. This reopening was only gradual and partial between the end of the first lockdown on May 11, 2020 and the summer vacation, but was fully completed with the start of the new school year on September 1, 2020 [14]. However, this back-to-school period took place under particular epidemiological conditions in France, since viral spread was increasing within the general population, especially among young adults. While it was accepted that reopening schools could be safe in the context of low transmission in the community [15], the epidemiological impact of keeping schools open in a context of increasing viral diffusion remained poorly documented. The objective of our study was therefore to describe the epidemiology of SARS-CoV-2 infections in different pediatric age groups during the school months of September and October 2020.
2. Methods
2.1. Population
Two sources of data were used regarding SARS-CoV-2 infections: general population data provided weekly by the National Public Health Agency, Santé Publique France (SPF), and school data provided weekly by the Ministry of National Education (MNE). General population incidence calculations were based on the number of people in each age group as recorded by the National Statistics and Economic Studies Institute (INSEE). The schools registered by MNE included all French public or private institutions, from kindergarten classes (3–5 years old) to high schools (15–17 years old). These schools accommodate 12,400,000 students, supervised by 1,162,850 adult staff, teachers or others. The students were spread over 528,400 classes in 61,500 schools. The health protocol put in place was aimed at welcoming all pupils, at all levels, and throughout school time, in compliance with the prescriptions issued by the health authorities. These are described in detail in the supplementary Appendix (Suppl. Appendix 1). In practice, guidelines for hygiene and social distancing measures were given for students and staff. Wearing a face mask, both indoors and outdoors (except for sports activities), was mandatory for staff and pupils in secondary schools (from 11 years old). School started on September 1 and continued until the vacation on October 17. The indications for polymerase chain reaction (PCR) testing in children were proposed by the French Society of Pediatrics, and included the presence of symptoms, contact with an infected person, or the presence of a person at risk of severe COVID at home [14].
2.2. Data collected
The following weekly epidemiological data were provided according to age by SPF: number of PCR tests performed, number of positive PCR tests, weekly national incidence of proven cases, number of hospitalizations, number of intensive care hospitalizations, number of deaths. SPF also gave the number of investigated clusters, defined by the presence of at least three confirmed or probable cases, within a 7-day period. We used data from week (W) 34 to W42, i.e., from August 17 to October 25, 2020, in order to take into account the resurgence of viral circulation that preceded the start of the school year in France.
For data collection, three information systems were used:
-
•
the number of daily tests for COVID-19 as well as the number of positive tests reported to SPF since May 13, 2020 by the laboratories participating in the SI-DEP system (Screening Information System). This information system includes all the biomedical analysis laboratories, whether private or public, ambulatory or hospital-based and can be considered as exhaustive, since it forms the basis for the implementation of the contact-tracing process. The data collection for this study was stopped on November 18 at 4 a.m;
-
•
the number of hospitalizations for COVID-19, including patients in intensive care (ICU) or other critical care units and deaths occurring during hospitalization, are reported by all establishments in France via the SI-VIC system (Information System for Victim Monitoring). SI-VIC was activated for the management of the COVID-19 epidemic on March 19, 2020. The data collection for this study was stopped on November 18 at 3 p.m. It is currently not possible to differentiate between hospitalizations linked to a diagnosis of COVID-19 and those during which a diagnosis of COVID-19 was made;
-
•
since May 11, 2020, the Regional Health Agencies (ARS), in conjunction with the regional SPF units and local partners, have been investigating clusters, defined by at least three confirmed or probable cases within a period of 7 days, belonging to the same community or having participated in the same gathering of people, whether they know each other or not. The SI-MONIC (Cluster Monitoring) system, developed by the SPF, gathered the data.
From W38, the MNE provided the following weekly data: number of confirmed cases among students and staff, number of classes closed, number of schools closed. The confirmed cases of students were those reported by families to their establishment. Initially, class closures were considered as soon as the first case was confirmed in a class. The rules for class closures were loosened on September 22. From this date, class closures were only considered when three students tested positive for COVID-19, not coming from the same family or not living in the same household. However, variations may have occurred in the decisions to close classes, which were ultimately made by the regional health agencies.
2.3. Data analysis
For the analysis, age groups were defined according to school levels: 0–2 years (nursery school or home childcare), 3–5 years (kindergarten), 6–10 years (primary school), 11–14 years (middle school), 15–17 years (high school). We also analyzed epidemic data from the upper age groups in the general population: 18–29, 30–49, and 50 years and over. The relative risk of having a positive PCR test result by age was calculated for each age group, with the 30–49 age group in the general population considered as the reference. Children and adolescents were then grouped into two categories, 0–5 years and 6–17 years, and compared with adults 18 years and older. Similarly, the ratio of incidence per week was calculated for each age group in comparison with the incidence measured in the 30–-49-year-old age group, which was used as reference. Results are given with 95% confidence intervals. STATA software was used for the analysis.
3. Results
3.1. Confirmed cases
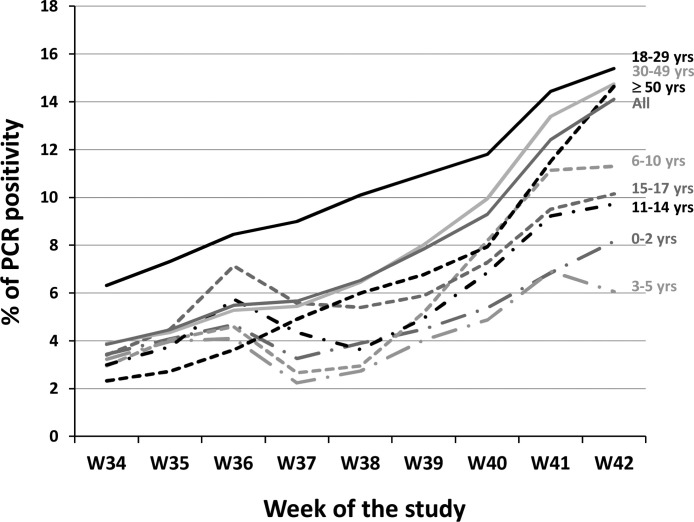
The period from W34 to W42 was marked by an increase in the number of cases identified by PCR (Table 1 ). Within the overall French population, the number of weekly new cases was 28,009 and 174,141 in W34 and W42, respectively. This increase may be partly related to the increase in the number of tests performed, which rose from 727,551 to 1,234,761 in W34 and W42, respectively. This increase was, however, mainly linked to an increase in viral spread in the population, as demonstrated by the sustained and large rise in the percentage of positivity among the tests performed, from 3.8% to 14.1% in W34 and W42, respectively (Fig. 1 ).
Table 1.
New SARS-CoV2 proven cases in each age range. The number of tests performed each week (N) and the number of positive tests (n) are given. The weekly incidence is expressed per 100,000 persons of the corresponding age range.
| Age range | W34 | W35 | W36 | W37 | W38 | W39 | W40 | W41 | W42 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 0–2 years |
N n (%) |
6627 228 (3.4) |
7396 302 (4.1) |
9303 436 (4.7) |
16,440 537 (3.3) |
11,539 451 (3.9) |
7020 315 (4.5) |
5,488 296 (5.4) |
5,705 391 (6.8) |
6,754 552 (8.2) |
| Incidence | 10.6 | 14.0 | 20.2 | 24.9 | 20.9 | 14.6 | 13.7 | 18.2 | 25.6 | |
| 3–5 years |
N n (%) |
7164 232 (3.2) |
8562 341 (4.0) |
13,859 569 (4.1) |
37,740 847 (2.2) |
22,013 604 (2.7) |
9016 365 (4.0) |
6,735 329 (4.9) |
7,772 537 (6.9) |
9,929 601 (6.0) |
| Incidence | 10.0 | 14.7 | 24.6 | 36.5 | 26.1 | 15.8 | 14.2 | 23.2 | 25.9 | |
| 6–10 years |
N n (%) |
16,097 478 (3.0) |
19,995 811 (4.1) |
26,634 1,225 (4.6) |
80,433 2,145 (2.7) |
78,334 2,311 (2.9) |
29,548 1,536 (5.2) |
18,753 1,537 (8.2) |
23,253 2,591 (11.1) |
33,040 3,737 (11.3) |
| Incidence | 11.6 | 19.6 | 29.7 | 51.9 | 56.0 | 37.2 | 37.2 | 62.7 | 90.5 | |
| 11–14 years |
N n (%) |
21,540 646 (3.0) |
25,658 963 (3.7) |
24,760 1,422 (5.7) |
48,319 2,107 (4.4) |
71,985 2,621 (3.6) |
53,651 2,656 (4.9) |
41,733 2,865 (6.9) |
49,261 4,548 (9.2) |
65,429 6,366 (9.7) |
| Incidence | 19.3 | 28.7 | 42.4 | 62.8 | 78.1 | 79.2 | 85.4 | 135.6 | 189.8 | |
| 15–17 years |
N n (%) |
25,087 856 (3.4) |
30,016 1,350 (4.5) |
29,254 2,089 (7.1) |
44,865 2,504 (5.6) |
64,383 3,475 (5.4) |
56,919 3,355 (5.9) |
50,957 3,716 (7.3) |
60,382 5,746 (9.5) |
77,108 7,828 (10.1) |
| Incidence | 34.5 | 54.4 | 84.2 | 101.0 | 140.1 | 135.3 | 149.8 | 231.7 | 315.6 | |
| 18–29 years |
N n (%) |
174,809 11,026 (6.3) |
211,059 15,456 (7.3) |
22,6136 19,103 (8.4) |
237,970 21,382 (9.0) |
244,301 24,669 (10.1) |
217,824 23,865 (11.0) |
200,177 23,621 (11.8) |
219,686 31,711 (14.4) |
25,9916 39,999 (15.4) |
| Incidence | 120.6 | 169.1 | 209.0 | 233.9 | 269.9 | 261.1 | 258.4 | 346.9 | 437.6 | |
| 30–49 years |
N n (%) |
220,321 8580 (3.9) |
275,463 11,969 (4.3) |
299867 15,808 (5.3) |
344,246 18,715 (5.4) |
337,958 21,818 (6.5) |
267,480 21,435 (8.0) |
243,487 24,226 (9.9) |
291,514 39,041(13.4) |
37,8818 55,841(14.7) |
| Incidence | 50.8 | 70.9 | 93.6 | 110.8 | 129.2 | 126.9 | 143.4 | 231.2 | 330.6 | |
| ≥ 50 years |
N n (%) |
255,906 5963 (2.3) |
310,782 8474 (2.7) |
331,814 12,024 (3.6) |
331,420 16,287 (4.9) |
325,922 19,558 (6.0) |
299,107 20,275 (6.8) |
291,142 23,115 (7.9) |
330,780 38,120 (11.5) |
403,767 59,217 (14.7) |
| Incidence | 22.4 | 31.8 | 45.1 | 61.1 | 73.4 | 76.1 | 86.7 | 143.0 | 222.2 | |
| All |
N n (%) |
727,551 28,009 (3.8) |
888,931 39,666 (4.5) |
961,627 52,676 (5.5) |
1,141,433 64,524 (5.6) |
1,156,435 75,507 (6.5) |
940,565 73,802 (7.8) |
858,472 79,705 (9.3) |
988,353 122,685 (12 .4) |
1,234,761 174,141 (14.1) |
| Incidence | 41.7 | 59.1 | 78.5 | 96.1 | 112.5 | 110.0 | 118.8 | 182.8 | 259.5 |
Fig. 1.
Weekly PCR test positivity rates for different age groups. For clarity, the references for each age group are noted in the figure next to the corresponding curve.
Analysis by age group identified different epidemiological profiles according to age category during the study period. The beginning of the study period (W34) was marked by a predominant viral circulation in the 18–29 age group, with a positive PCR rate of 6.3%, contrasting with rates of less than 4% in all other age groups (Fig. 1), and with an incidence rate of 120.6/100,000 persons, 3 times higher than that measured in the general population (Table 1).
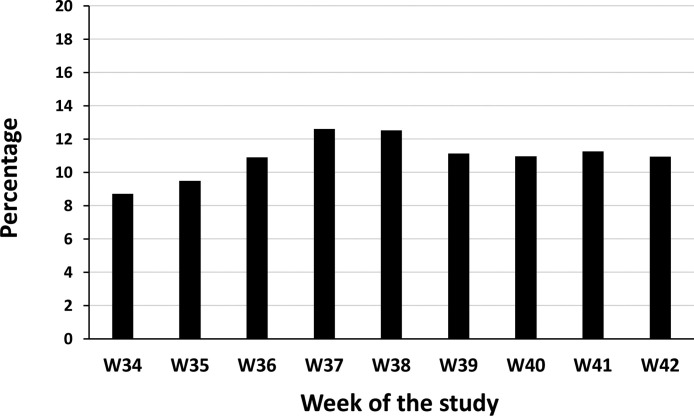
Between W34 and W42, an increase in the number of cases was observed in all age groups (Table 1), but children and adolescents under 18 years of age only contributed to less than 13% of the cases identified (Fig. 2 ), while they represent 22% of the total population. The increase was particularly marked among adults over 30 years of age, unrelated to variations in the number of tests performed (Suppl. Fig. 1). Interestingly, an increase in the number of tests performed in children around W37 and W38 was not accompanied by a parallel increase in the number of positive cases (Suppl. Fig. 1).
Fig. 2.
Percentage of children and adolescents between 0 and 18 years of age among newly confirmed COVID-19 cases each week.
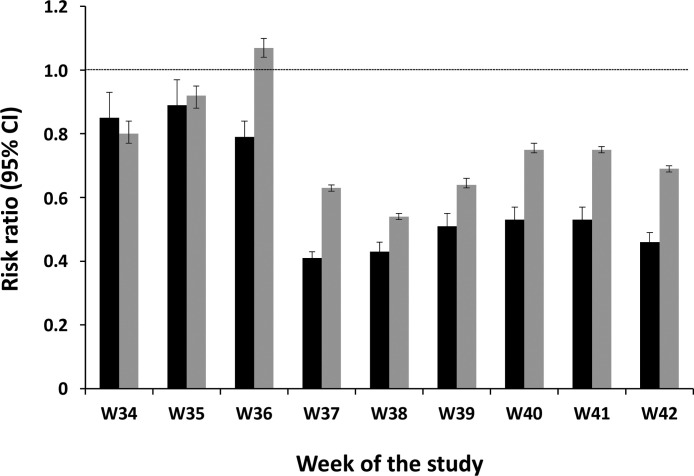
At the end of the study period, in W41 and W42, there were three groups that could be identified according to their PCR positive rate (Fig. 1). Children between 0 and 5 years old had the lowest rates of positive PCR results, between 6 and 8%. Children and adolescents between 6 and 17 years old had intermediate rates of positivity, between 9 and 11%. Adults over the age of 18 exceeded the 14% positivity rate. Compared with adults, the relative risk of having a positive PCR test result was significantly lower in all pediatric age groups from W38 onward (Fig. 3 and Suppl. Table 1).
Fig. 3.
Risk ratio for positive test according to age and by week. Children are grouped into two age groups: 0–5 years (black columns) and 6–17 years (grey columns). The reference group consists of all adults aged 18 and over, indicated by the hatched line (RR = 1). Error bars are 95% confidence intervals.
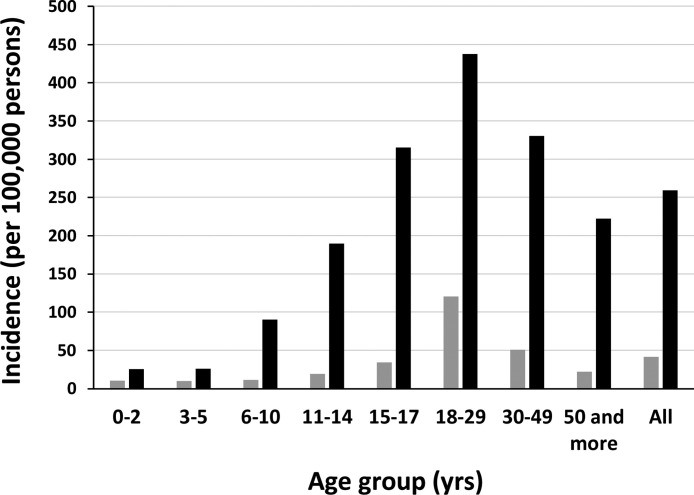
The changes in weekly incidences were also clearly age-dependent (Fig. 4 ). Children between 0 and 5 years of age continued to have a low incidence, with a modest increase between W34 and W42. In the group of children between 6 and 17 years old, the increase in weekly incidence between W34 and W42 was even greater the older the child was. At W42, the incidence in adolescents aged 15–17 years was 316/100,000, higher than that measured in the general population (259/100,000). Compared with adults, the incidence rate ratio was significantly lower in all pediatric age groups between 0 and 14 years of age throughout the study. There was no longer a significant difference in the incidence rate ratio in 5–17-yearolds from W39 onward (Suppl. Table S2).
Fig. 4.
Weekly incidence of proven cases of COVID-19 in different age groups in week 34 (grey columns) and week 42 (black columns).
3.2. Hospitalizations
Of the newly hospitalized patients with a positive sample for SARS-CoV-2 between W34 and W42, children and adolescents younger than 18 years of age accounted for 1.9% of these hospitalizations (Table 2 ). They accounted for 1.3% of new hospitalizations in intensive care. No deaths were observed in children or adolescents. Infants between 0 and 2 years of age represented 48% of all pediatric hospitalizations and 43% of intensive care admissions.
Table 2.
Weekly number of new hospital admissions (H) and new intensive care admissions (ICU) among children and adolescents by age group, and numbers observed in the French population as a whole.
| 0–2 years |
3–5 years |
6–10 years |
11–14 years |
15–17 years |
Total population |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| H | ICU | H | ICU | H | ICU | H | ICU | H | ICU | H | ICU | |
| W34 | 19 | 2 | 3 | 0 | 4 | 0 | 5 | 0 | 5 | 1 | 1084 | 174 |
| W35 | 21 | 4 | 3 | 1 | 6 | 1 | 3 | 0 | 11 | 1 | 1337 | 210 |
| W36 | 23 | 2 | 6 | 1 | 8 | 2 | 7 | 2 | 10 | 1 | 1704 | 288 |
| W37 | 20 | 1 | 5 | 1 | 7 | 0 | 11 | 1 | 10 | 0 | 2464 | 427 |
| W38 | 32 | 5 | 4 | 2 | 13 | 0 | 15 | 1 | 12 | 3 | 3657 | 599 |
| W39 | 22 | 2 | 3 | 1 | 2 | 0 | 12 | 1 | 12 | 1 | 4204 | 786 |
| W40 | 28 | 4 | 6 | 0 | 5 | 0 | 11 | 1 | 16 | 2 | 4264 | 893 |
| W41 | 26 | 1 | 4 | 1 | 6 | 1 | 10 | 3 | 20 | 3 | 5084 | 910 |
| W42 | 93 | 12 | 5 | 2 | 13 | 6 | 15 | 2 | 19 | 2 | 7530 | 1343 |
| Total | 284 | 33 | 39 | 9 | 64 | 10 | 89 | 11 | 115 | 14 | 31,328 | 5630 |
3.3. Proportion of asymptomatic cases
Of those with a positive PCR test result, the percentage of asymptomatic individuals varied little over the 9 weeks, but differed by age group (Suppl. Fig. 2). Among children and adolescents under 18 years of age, the percentage of asymptomatic individuals was 57% at W34 and 48% at W42. In adults 18 years and older, the proportion of asymptomatic individuals among those testing positive was much lower, measured at 39% and 31% at W34 and W42, respectively.
At W42, the rate of positive PCR test results was identical in children between 0 and 10 years of age, tested while symptomatic or asymptomatic (Fig. 5 ). From the age of 11 onward, the rate of positivity became higher in symptomatic individuals than in asymptomatic ones, and this difference increased with age group to be very marked in adults.
Fig. 5.
Percentage of positive PCR tests during week 42 in individuals tested without symptoms (gray columns) or with symptoms (black columns), by age group.
3.4. Class closures
The number of confirmed cases in children in primary, middle, or high schools, reported by their families at their establishment and listed by the MNE, was lower than the number of cases identified by the exhaustive collection of SPF (Table 3 ). The underestimation varies according to the week, from 36% at W39 to 59% at W41 (Suppl. Fig. 3).
Table 3.
Number of cases reported to the Ministry of National Education.
| W38 | W39 | W40 | W41 | W42 | |
|---|---|---|---|---|---|
| Confirmed cases among students, n (% of total) | 5056 (0.04) | 5612 (0.05) | 4636 (0.04) | 5279 (0.04) | 8223 (0.07) |
| Confirmed cases among staff, n (% of total) | 1307 (0.11) | 1153 (0.1) | 1031 (0.09) | 1276 (0.11) | 2063 (0.18) |
| Classes closed, n (% of total) | NA | 1152 (0.2) | 290 (0.05) | 199 (0.04) | 293 (0.06) |
| Schools closed, n (% of total) | 89 (0.14) | 19 (0.03) | 14 (0.02) | 24 (0.04) | 27 (0.04) |
On the other hand, the number of confirmed cases among school staff was consistent with the data measured in the total general population (Table 3). The increase in the number of cases observed at the end of the study period was shifted by 1 week compared with that observed in the general population (Suppl. Fig. 4).
The number of class closures was high during W39, and then stabilized at less than 300 per week with less stringent closure rules (Table 3). The number of schools closed remained low throughout the study period. Overall, the number of classes closed from W40 onward was higher than the number of clusters analyzed by SPF in primary, middle, and high schools (Table 4 ). Clusters reported in nurseries and kindergarten represented less than 3% of all clusters analyzed in France during the study period. Clusters were most numerous in middle and high schools, representing 10% of all clusters analyzed.
Table 4.
Clusters registered within the SI-MONIC system (Santé Publique France).
| All (n) | Nurseries |
Kindergarten |
Primary |
Middle and high |
University |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||
| W34 | 222 | 0 | 0 | 0 | 0 | 1 | 0.5 | 0 | 0 | 1 | 0.5 |
| W35 | 229 | 1 | 0.4 | 1 | 0.4 | 0 | 0 | 1 | 0.4 | 1 | 0.4 |
| W36 | 360 | 6 | 1.7 | 3 | 0.8 | 3 | 0.8 | 11 | 3.1 | 3 | 0.8 |
| W37 | 502 | 10 | 2.0 | 12 | 2.4 | 24 | 4.8 | 56 | 11.2 | 42 | 8.4 |
| W38 | 495 | 13 | 2.6 | 7 | 1.4 | 26 | 5.3 | 78 | 15.8 | 59 | 11.9 |
| W39 | 526 | 7 | 1.3 | 10 | 1.9 | 13 | 2.5 | 88 | 16.7 | 72 | 13.7 |
| W40 | 503 | 13 | 2.6 | 4 | 0.8 | 10 | 2.0 | 66 | 13.1 | 52 | 10.3 |
| W41 | 580 | 16 | 2.8 | 3 | 0.5 | 10 | 1.7 | 50 | 8.6 | 60 | 10.3 |
| W42 | 799 | 13 | 1.6 | 2 | 0.3 | 9 | 1.1 | 71 | 8.9 | 41 | 5.1 |
| Total | 4216 | 79 | 1.9 | 42 | 1.0 | 96 | 2.3 | 421 | 10.0 | 331 | 7.9 |
4. Discussion
Our study assessed the trends of pediatric COVID-19 cases in France in September and October 2020, in the particular context of the permanent and full opening of schools, despite a national context of increasing viral diffusion within the general population.
In the French context where the indications for PCR tests were limited in children, targeting those actually at risk of infection, while tests were freely available to adults regardless of the notion of symptoms or contact, our first study result was that viral spread as assessed via the positive PCR rate remained lower in children and adolescents than in adults. While a high positivity rate was observed in the 18–29-year-olds at the start of the study, the highest positivity rates at the end of the study were observed not only in the 18–29-year-olds, but also in the 30–49-year-olds and the over 50-year-olds, this last age group being the one with the greatest increase in the rate of positivity during the course of the study. Among children and adolescents, we identified an effect of age on the PCR positivity rate in the different school grades. During the course of the study, the PCR positivity rate increased slightly in children in nursery or kindergarten, while for those in primary, secondary, or high school it increased more, but without reaching the rates observed in adults. Nevertheless, the relative risk of positive PCR results remained significantly lower in children and adolescents, regardless of their educational level, than that of adults throughout the study, suggesting that the increase in the number of cases in adults had only a delayed impact on children. These results support studies suggesting that children were less susceptible to infection and weaker transmitters of COVID-19, and they justify a posteriori the continued opening of schools in the French context of the study period. In a model based on multinational data, children's susceptibility to infection was estimated to be half that of adults [4]. A recent systematic review with meta-analysis including 18 contact-tracing studies confirmed the lower susceptibility to infection of children under 12–14 years of age compared with adults, while the susceptibility of adolescents did not appear to be different [5]. In a large SARS-CoV-2 prevalence study focusing on children in southwest Germany during a period of lockdown, the estimated seroprevalence was particularly low in children aged 1–10 years, and threefold lower than in their parents, suggesting that children were unlikely to have boosted the pandemic [16]. Very similar to our study, the recent analysis of pediatric infections observed in the United States between March and December 2020 showed that among persons aged 0–24 years, the weekly incidence was higher in each successively increasing age group, and that the weekly incidence among adults aged 25 years and over exceeded that among children and adolescents aged 0–13 years throughout the review period [17]. Concerning more specifically intra-school transmission, it is interesting to compare our study with the experience of Baden-Wurttemberg and their reopening of schools in May 2020 [18]. This reopening in this German region was done with reinforced hygiene and social distancing measures, but no masks were worn in class, even at secondary school. During the 11 weeks of the study, pediatric cases between 0 and 19 years of age accounted for 17.9% of all cases reported in this region, compared with the maximum value of 12.6% at W37 in our study. Among the individuals that had attended school during their infectious period, secondary cases within the school were observed for only 4% of them. Similarly in Italy, based on the estimated post-lockdown transmissibility, it was concluded that reopening educational levels up to secondary schools might have influenced SARS-CoV-2 transmissibility only marginally [19]. However, some models underline the need to accompany the reopening of schools with reinforced measures of hygiene and social distancing [20]. It was previously admitted that schools could open safely when community transmission was low [15]. Based on the evidence from contact tracing in schools, and on observational data from a number of EU countries, a survey of the European Center for Disease Prevention and Control (ECDC) suggested that reopening schools has not been associated with significant increases in community transmission after the first lockdown [21]. Interestingly, a French modeling study can be compared with what really happened [22]. In this model, the progressive or immediate return to school for some or all students was shown to significantly influence the dynamics of ICU hospitalizations for COVID-19. In the actual situation, and despite a progressive and complete opening of schools after the first lockdown in France, the ICU admissions observed were those corresponding to the curve of the model constructed with the continued closure of schools, suggesting that the reopening of schools did not have an impact on viral spread in the population: The actual number of hospitalizations in ICU in Ile de France was 181 in W31, compared with around 250 predicted by the model with maintained school closure and 1500 in the case of full reopening, even considering a very low transmissibility among young children.
However, in the specific context of increasing community transmission during the study period, a significant increase in the weekly incidence was measured among middle school students, and more so among high school students, despite the mandatory wearing of masks for these age groups within their schools. It is likely that festive behavior at school-leaving or at weekends, which is itself age-dependent, contributed to this result. It is also possible that this result in fact illustrated a physiologically intermediate behavior of these age groups with regard to viral infection and transmission. Several studies had already noted this age-dependent susceptibility to infection. In the Korean experience, home transmission from an index case was 3 times lower in 0–9-year-olds than in 10–19-year-olds [8]. In an analysis of 58 clusters within the same household, the secondary attack rate was twice as high among 13–17-year-olds than among those under 12 years of age [6]. At the end of our study period, adolescents between 15 and 17 years of age was one of the age groups with a very high weekly incidence, suggesting that the hygiene and social distancing measures taken in high schools, or adherence to these measures, were not sufficient to prevent transmission of the infection in this age group. Mostly, the absence of a full lockdown allowed these adolescents to maintain social activities that are more sources of contamination than the school itself [18]. However, these results raise the question of which attitude to have toward high schools, but also middle schools, in the context of high viral transmission within the general population. It should be noted, however, that the positive PCR rate in this age group remained lower than in the older age groups, while hygiene and social distancing measures were potentially insufficiently respected. Further, the fact that the positivity rate in 6–10-year-olds increased rapidly during the study and was higher at W42 than that observed in 11–17-year-olds is an indirect argument to justify the wearing of masks from the age of 6 years, which was effective in France from November 2020.
Despite the increasing incidence of infections among children, especially in high and middle schools, an important finding of our study was the low number of intra-school outbreaks, and the absence of arguments for the transmission from students to school staff. The number of classes closed due to multiple cases within the class represented less than 1% of the total number of classes, and the number of clusters investigated in the different school levels (between 3 and 17 years old) by the regional health agencies represented less than 15% of the total number of clusters investigated at the national level. However, these numbers may have been underestimated due to under-reporting of cases of infected children by families to school directors. Nevertheless, even considering that a factor of 2 must be taken into account due to this under-reporting, the number of closed classes would have remained very low. These results are very similar to those observed in Italy during the first month of school in September 2020 [23]. Cases of infection in students or professionals were reported in only 1.8% of schools. Less than 0.02% of students were infected. Similarly, the German study showed the very low participation of schools in all of the epidemics identified [24]. The reported number of infected school staff was most likely more reliable than the number of infected students, because absenteeism for staff was inevitably recorded by school directors. Moreover, the complete correlation at the beginning of the study between the incidence observed among staff and the general population reinforced the credibility of these numbers. There was clearly no over-representation of infection among school staff, and even a later increase in infection among these individuals compared with the increase in the general population. It is possible that the many precautions taken within schools may have contributed to a better protection of these persons. Consistently, a US study found no difference in the rates of infection or hospitalization during the first 3 months of the pandemic between people who continued to care for children and those who stopped that activity [25].
Finally, our study also confirmed that infections in children and adolescents were very rarely severe. While the number of new cases represented 10–12% of the new cases identified in the general population, the number of pediatric hospitalizations represented less than 2% of the total hospitalizations, and no deaths were observed. This observation is now made in all countries [1], [2], [3]. Recently published US data for children aged 0–17 years were very similar to ours, with hospitalization and ICU admission rates of 2.3% and 0.8%, respectively [17].
Asymptomatic forms were predominant between 3 and 10 years of age. They remained even more frequent between 11 and 17 years of age than in adults. This point was consistent with other epidemiological studies [26], [27] and with models constructed from multinational data [4]. As a result of these predominantly asymptomatic infections, our study showed that PCR positivity rates were similar in symptomatic and asymptomatic children. Asymptomatic children, however, are not representative of the general pediatric population, as these children were mainly sampled in the context of contact with another infected person. The role of these asymptomatic infected children in the transmission of the virus remains poorly known, but is probably low, since the child is rarely identified as the index case of a cluster [6], [7], [8], [9]. Further, the small number of identified clusters or closed classes argue against an important role of these children in the transmission of the infection.
5. Conclusion
In the specific French context, our study confirms an age effect on the spread of SARS-CoV2, with the relative risk of a positive PCR test result being significantly lower in children and adolescents compared with adults. These results, obtained while schools were kept open in a context of increasing transmission in the general population, argue for a marginal contribution of children in the dynamics of the epidemic, and reinforce the interest of keeping schools open, especially facilities for children in the first decade of life, so as to limit the numerous deleterious effects of school closures demonstrated during the first lockdown. However, our results also show the need to strengthen policies to promote education on hygiene and social distancing measures among adolescents, and to advocate for the use of masks among 6–11-year-olds when viral transmission in the general population is high.
Disclosure of interest
The authors declare that they have no competing interest.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.arcped.2021.02.001.
Appendix A. Supplementary data
Risk ratio for positive test according to all age groups and by week.
Incidence rate ratio according to all age groups and by week.
Weekly number of PCR tests performed and cases identified in the different age groups. A: 0–2 years; B: 3–5 years; C: 6–10 years; D: 11–14 years; E: 15–17 years; F: 18–29 years; G: 30–49 years; H: 50 years and over; I: whole population. Except for graph I, the Y-axes have the same coordinates to allow for easy comparison between age groups. Left Y-axis and blue columns: number of tests with positive PCR; Right Y-axis and orange line: total number of tests.
Percentage of symptomatic (orange lines) and asymptomatic (blue lines) patients among new weekly PCR-positive cases. Different age groups were analyzed: A: 0–2 years; B: 3–5 years; C: 6–10 years; D: 11–14 years; E: 15–17 years; F: 18–29 years; G: 30–49 years; H: 50 years and over.
Comparison of the new weekly cases listed by the Ministry of National Education after declaration of the families (blue columns), and those listed by the exhaustive SI-DEP information system (orange columns) for children between 3 and 17 years old.
Comparison of the weekly incidence of confirmed cases of COVID-19 among school staff listed by the Ministry of National Education and that measured in the general population by the SI-DEP information system.
References
- 1.Gotzinger F., Santiago-Garcia B., Noguera-Julian A. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020;4:653–661. doi: 10.1016/S2352-4642(20)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim L., Whitaker M., O’Halloran A. Hospitalization rates and characteristics of children aged < 18 years hospitalized with laboratory-confirmed COVID-19 - COVID-NET, 14 States, March 1-July 25, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1081–1088. doi: 10.15585/mmwr.mm6932e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oualha M., Bendavid M., Berteloot L. Severe and fatal forms of COVID-19 in children. Arch Pediatr. 2020;27:235–238. doi: 10.1016/j.arcped.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davies N.G., Klepac P., Liu Y. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020;26:1205–1211. doi: 10.1038/s41591-020-0962-9. [DOI] [PubMed] [Google Scholar]
- 5.Viner R.M., Mytton O.T., Bonell C. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: a systematic review and meta-analysis. JAMA Pediatr. 2020;175:143–156. doi: 10.1001/jamapediatrics.2020.4573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Laws R.L., Chancey R.J., Rabold E.M. Symptoms and transmission of SARS-CoV-2 among children - Utah and Wisconsin, March-May 2020. Pediatrics. 2021;147 doi: 10.1542/peds.2020-027268. [e2020027268] [DOI] [PubMed] [Google Scholar]
- 7.Laxminarayan R., Wahl B., Dudala S.R. Epidemiology and transmission dynamics of COVID-19 in two Indian states. Science. 2020;370:691–697. doi: 10.1126/science.abd7672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park Y.J., Choe Y.J., Park O. Contact tracing during coronavirus disease outbreak, South Korea, 2020. Emerg Infect Dis. 2020;26:2465–2468. doi: 10.3201/eid2610.201315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y., Tian H., Zhang L. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob Health. 2020;5:e002794. doi: 10.1136/bmjgh-2020-002794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bignardi G., Dalmaijer E.S., Anwyl-Irvine A.L. Longitudinal increases in childhood depression symptoms during the COVID-19 lockdown. Arch Dis Child. 2020 doi: 10.1136/archdischild-2020-320372. [archdischild-2020-320372. Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garstang J., Debelle G., Anand I. Effect of COVID-19 lockdown on child protection medical assessments: a retrospective observational study in Birmingham, UK. BMJ Open. 2020;10:e042867. doi: 10.1136/bmjopen-2020-042867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leeb R.T., Bitsko R.H., Radhakrishnan L. Mental health-related emergency department visits among children aged < 18 years during the COVID-19 pandemic – United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1675–1680. doi: 10.15585/mmwr.mm6945a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levinson M., Cevik M., Lipsitch M. Reopening primary schools during the pandemic. N Engl J Med. 2020;383:981–985. doi: 10.1056/NEJMms2024920. [DOI] [PubMed] [Google Scholar]
- 14.Cohen R., Delacourt C., Gras-Le Guen C. COVID-19 and schools. Guidelines of the French Pediatric Society. Arch Pediatr. 2020;27:388–392. doi: 10.1016/j.arcped.2020.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mallapaty S. How schools can reopen safely during the pandemic. Nature. 2020;584:503–504. doi: 10.1038/d41586-020-02403-4. [DOI] [PubMed] [Google Scholar]
- 16.Tonshoff B., Muller B., Elling R. Prevalence of SARS-CoV-2 infection in children and their parents in Southwest Germany. JAMA Pediatr. 2021;22:e210001. doi: 10.1001/jamapediatrics.2021.0001. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leidman E., Duca L.M., Omura J.D. COVID-19 trends among persons aged 0–24 Years – United States, March 1-December 12, 2020. MMWR Morb Mortal Wkly Rep. 2021;70:88–94. doi: 10.15585/mmwr.mm7003e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ehrhardt J., Ekinci A., Krehl H. Transmission of SARS-CoV-2 in children aged 0 to 19 years in childcare facilities and schools after their reopening in May 2020, Baden-Wurttemberg, Germany. Euro Surveill. 2020;25:2001587. doi: 10.2807/1560-7917.ES.2020.25.36.2001587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marziano V., Guzzetta G., Rondinone B.M. Retrospective analysis of the Italian exit strategy from COVID-19 lockdown. Proc Natl Acad Sci U S A. 2021;118 doi: 10.1073/pnas.2019617118. [e2019617118] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee B., Hanley J.P., Nowak S. Modeling the impact of school reopening on SARS-CoV-2 transmission using contact structure data from Shanghai. BMC Public Health. 2020;20:1713. doi: 10.1186/s12889-020-09799-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.European Centre for Disease Prevention and Control . 2020. COVID-19 in children and the role of school settings in COVID-19 transmission. https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-schools-transmission-August%202020.pdf. [Google Scholar]
- 22.Di Domenico L., Pullano G., Sabbatini C. Can we safely reopen schools during COVID-19 epidemic? medRxiv. 2020 doi: 10.1101/2020.05.08.20095521. https://www.medrxiv.org/content/10.1101/2020.05.08.20095521v2 [05.08.20095521] [DOI] [Google Scholar]
- 23.Buonsenso D., De Rose C., Moroni R. SARS-CoV-2 infections in Italian schools: preliminary findings after 1 month of school opening during the second wave of the pandemic. Front Pediatr. 2021;8:615894. doi: 10.3389/fped.2020.615894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Otte Im Kampe E., Lehfeld A.S., Buda S. Surveillance of COVID-19 school outbreaks, Germany, March to August 2020. Euro Surveill. 2020;25:2001645. doi: 10.2807/1560-7917.ES.2020.25.38.2001645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gilliam W.S., Malik A.A., Shafiq M. COVID-19 transmission in US Child Care Programs. Pediatrics. 2021;147 doi: 10.1542/peds.2020-031971. [e2020031971] [DOI] [PubMed] [Google Scholar]
- 26.Maltezou H.C., Vorou R., Papadima K. Transmission dynamics of SARS-CoV-2 within families with children in Greece: a study of 23 clusters. J Med Virol. 2020 doi: 10.1002/jmv.26394. [10.1002/jmv.26394. Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Posfay-Barbe K.M., Wagner N., Gauthey M. COVID-19 in children and the dynamics of infection in families. Pediatrics. 2020;146:e20201576. doi: 10.1542/peds.2020-1576. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Risk ratio for positive test according to all age groups and by week.
Incidence rate ratio according to all age groups and by week.
Weekly number of PCR tests performed and cases identified in the different age groups. A: 0–2 years; B: 3–5 years; C: 6–10 years; D: 11–14 years; E: 15–17 years; F: 18–29 years; G: 30–49 years; H: 50 years and over; I: whole population. Except for graph I, the Y-axes have the same coordinates to allow for easy comparison between age groups. Left Y-axis and blue columns: number of tests with positive PCR; Right Y-axis and orange line: total number of tests.
Percentage of symptomatic (orange lines) and asymptomatic (blue lines) patients among new weekly PCR-positive cases. Different age groups were analyzed: A: 0–2 years; B: 3–5 years; C: 6–10 years; D: 11–14 years; E: 15–17 years; F: 18–29 years; G: 30–49 years; H: 50 years and over.
Comparison of the new weekly cases listed by the Ministry of National Education after declaration of the families (blue columns), and those listed by the exhaustive SI-DEP information system (orange columns) for children between 3 and 17 years old.
Comparison of the weekly incidence of confirmed cases of COVID-19 among school staff listed by the Ministry of National Education and that measured in the general population by the SI-DEP information system.