Abstract
Effective communication between members of the multidisciplinary team is imperative for patient safety. Within the Medicine for the Elderly wards at Royal Victoria Hospital (RVH) in Dundee, we identified an inefficient process of information-sharing between the orthopaedics outpatient department (OPD) at the main teaching hospital and our hospital’s rehabilitation teams, and sought to improve this by introducing several changes to the work system. Our aim was for all patients who attended the OPD clinic to have a plan communicated to the RVH team within 24 hours.
Before our intervention, clinic letters containing important instructions for ongoing rehabilitation were dictated by the OPD team, transcribed and uploaded to an electronic system before the RVH team could access them. We analysed clinic attendances over a 4-week period and found that it took 15 days on average for letters to be shared with the RVH teams. We worked with both teams to develop a clinical communication tool and new processes, aiming to expedite the sharing of key information. Patients attended the OPD with this form, the clinician completed it at the time of their appointment and the form returned with the patient to RVH on the same day.
We completed multiple Plan–Do–Study–Act cycles; before our project was curtailed by the COVID-19 pandemic. During our study period, seven patients attended the OPD with a form, with all seven returning to RVH with a completed treatment plan documented by the OPD clinician. This allowed rehabilitation teams to have access to clinic instructions generated by orthopaedic surgeons almost immediately after a patient attended the clinic, essentially eliminating the delay in information-sharing.
The introduction of a simple communication tool and processes to ensure reliable transfer of information can expedite information-sharing between secondary care teams and can potentially reduce delays in rehabilitation.
Keywords: geriatrics, communication, rehabilitation, quality improvement, teamwork
Problem
Royal Victoria Hospital (RVH) is a subacute rehabilitation hospital located in Dundee, Scotland. The hospital provides care predominantly to patients over the age of 65 years from across the National Health Service (NHS) Tayside health board area, with a focus on rehabilitation and discharge planning after acute illness or injury which has resulted in functional decline. Admissions are accepted as a ‘stepdown’ from a variety of inpatient specialties within the main Ninewells Hospital site which include general medicine, Medicine for the Elderly (MFE), general surgery, and trauma and orthopaedics.
Patients are admitted to any of three MFE rehabilitation wards. A multidisciplinary team (MDT) approach is integral to the hospital’s ethos, in order to facilitate holistic care and safe discharge. Each ward’s team is led by a medical consultant, with other team members including nurses, foundation doctors, physiotherapists, occupational therapists, speech and language therapists, dietitians and social workers.
Orthopaedic patients represent a significant proportion of admissions to the hospital. Although the vast majority do not require routine follow-up, a number of patients from this cohort require prolonged rehabilitation due to the nature of their injury (usually lower limb fractures) and need formal follow-up by the orthopaedics team at Ninewells Hospital. A key part of these specialist reviews is to allow the rehabilitation teams in RVH to formulate safe and effective care plans while taking into account specific instructions, such as weight-bearing status.
Before our intervention, a key challenge was the delay in information-sharing between the outpatient department (OPD) and RVH rehabilitation teams. Typically, clinic notes would be dictated by a surgeon at the time of consultation, which would then be transcribed by secretarial staff before being ‘signed off’ by a clinician. Ultimately, these would be uploaded to the clinical communication platform, Clinical Portal, where the RVH teams could read and act on the clinic encounter.
Over a 4-week period, we analysed the time taken from a patient’s OPD attendance to their clinic letters being made available electronically. Nine patients attended the OPD during this period; the mean time taken for clinic letters to be made available was 15 days, with a range of 4–27 days. The rehabilitation teams believed that this period of time potentially represented ‘lost rehabilitation days’, as there was no other formal pathway for relevant information to be provisionally shared. Thus, therapists were unable to make progress with care plans, for example, allowing patients to progress onto less restrictive mobility aids.
Although difficult to quantify, a significant task burden was placed on members of both teams in order to overcome this delay. Members of the RVH team would contact the OPD secretaries to clarify plans based on dictations that were not yet available electronically, leading to an inefficient interface between the departments. For example, a physiotherapist emailed the orthopaedic surgeon directly to enquire about a patient’s weight-bearing status after they had attended the OPD. Main concerns included the impact this pathway had on clinical and administrative staff in both teams, as well as the potential impact this delay had on patient journey.
As a team, we recognised the potential benefit of introducing a clinical communication tool to expedite information-sharing before a clinic dictation could be made available, with the aim of facilitating the sharing of key clinical information between departments within 24 hours for all patients attending the OPD from RVH.
Background
The majority of our orthopaedics rehabilitation patients are admitted with fragility fractures, which account for around 300 000 hospital attendances each year in the UK.1 These fractures occur as a result of low-energy trauma2 which would not normally result in injury. Osteoporosis is a significant risk factor for these fractures, the incidence of which increases with age.3
As the elderly population grows, the number of people affected by fragility fractures is expected to rise,4 representing a potential increase in the need for fracture management and post-fracture rehabilitation services among the elderly population. Thus, the need for effective information-sharing between orthopaedics and rehabilitation teams will become increasingly important to ensure a streamlined patient journey through the acute and rehabilitation care pathways.
Geriatric rehabilitation is ‘a multidimensional approach of diagnostic and therapeutic interventions, the purpose of which is to optimise functional capacity, promote activity, and preserve functional reserve and social participation in older people with disabling impairments’.5 Rehabilitation is person centred and should involve professionals from across healthcare disciplines. An organised MDT approach to the care of older adults with fractures can reduce the risk of complications and length of hospital stay in the acute setting,6 and specialist geriatric rehabilitation after hip fractures has been associated with reduced need for institutional care.7 Optimising the ability of teams to formulate collaborative multiprofessional care plans is therefore of clear benefit to patients.
Several barriers may exist to effective MDT working in the geriatric rehabilitation setting. Despite a shift towards the delivery of healthcare by teams rather than individuals, the complex healthcare work system has been slow to adapt to promote interdisciplinary communication.8 This was perhaps the case in our ‘pre-intervention’ work system as exemplified by our baseline data. It is widely accepted that good communication and team working are central to positive patient outcomes,9 while poor communication contributes to healthcare errors with associated morbidity and mortality.10
Information-sharing between teams and individuals can be problematic, and sub-optimal communication commonly occurs at the interface between wards or departments.11 Indeed, longer term rehabilitation after a fracture is likely to take place in a different environment from the orthopaedics ward to which the person was initially admitted, as is the case for patients in RVH. Additionally, information-sharing between individuals from different professional backgrounds can be inadequate,11 potentially stemming from a variation in preferred communication styles between healthcare disciplines and the way different healthcare professionals are taught to communicate.12 We sought to explore this factor during the design, and introduction of our communication tool as the main interface between the OPD and RVH teams during the clinic appointment is between the orthopaedic surgeon and healthcare support worker (HCSW), and this will be explored in more detail later. Other factors such as power gradient, hierarchy and organisational culture can also contribute to communication errors in healthcare.12
There are important strategies for improving communication between teams and individuals in healthcare settings. These strategies should ideally ‘take little time and effort to complete, deliver comprehensive information efficiently, encourage interprofessional collaboration and limit the probability of error’,13 with a widely used example being the ‘situation, background, assessment and recommendation’ handover tool. The benefits of structured handover tools have been well described; however the introduction of such clinical communication tools into an already complex work system such as hospitals and OPDs should be done in collaboration with the wider team.
Handover is an integral and regular task within the NHS Tayside work system; indeed, the importance of clear handover is emphasised during induction sessions for newly qualified doctors. However, there are a number of patient areas where handover of patient information is informal, with no structured communication tool to facilitate efficient and safe transfer of key information. Clinical communication tools have been introduced within the same health board to promote information-sharing between ward teams with positive results.14 We sought to demonstrate that similar methods could be effective in facilitating information-sharing between acute and rehabilitation settings.
Measurement
We analysed the time taken for clinic letters to be made available following a patient’s attendance at the orthopaedics OPD clinic between December 2019 and January 2020. All patients who attended the clinic from the MFE rehabilitation wards were included. We compared the clinic attendance date with the date of letter authorisation (which is the date on which letters are shared on the Clinical Portal system). This was the only formal route of communication between the OPD and rehabilitation teams before our intervention. Nine patients attended the OPD. The mean time between attendance and authorisation was 15 days, with a range from 4 to 27 days. One patient did not have a formal dictated letter available as of mid-March 2020.
We intended to promote near-immediate information-sharing between teams (ie, less than 24 hours), resulting in elimination of the need for plans to be ‘chased up’ by the ward doctors or therapists. In turn, we intended for this to improve the patient journey.
Our primary outcome measure was to improve the patient journey, although this proved difficult to measure. Our primary process measure was the time taken for information to be shared between the OPD and RVH therapy teams, as well as completion of our communication tool. We recognised the need to have balancing measures, and intended to gather information regarding the time burden placed on clinicians filling out the form, as well as measuring potential duplication of work as a result of the form’s introduction (since the clinicians would still ultimately dictate a letter for Clinical Portal). The intervention period was from February 2020 to April 2020. We intended to re-evaluate our strategy after each clinic attendance, to review the effectiveness of our interventions, and this would inform our ongoing Plan–Do–Study–Act (PDSA) cycles.
Design
The primary members of our improvement team were two Foundation Year 2 doctors completing an MFE rotation at RVH. The expertise of the wider ward teams was sought to inform the direction of the project, with particular guidance from physiotherapists and MFE consultants. As a result of an MDT discussion, the introduction of a clinical communication tool (the pro forma) was identified as a potentially beneficial addition to the work system which could allow easy and effective interdepartmental communication. The form was designed to prompt sharing of salient rehabilitation-focused information without being an additional burden for OPD staff.
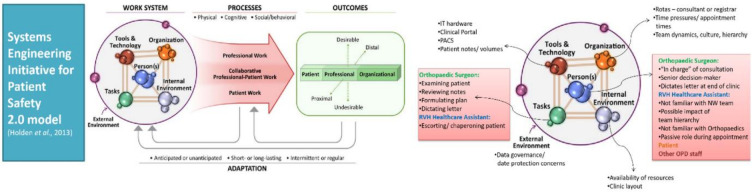
Before introducing a tool into the work system, we sought to understand the work system in more detail by discussing the current pathway with staff from both departments. We used the Systems Engineering Initiative for Patient Safety (SEIPS) 2.0 model to structure this work system analysis.15 In doing so, we recognised that the NHS is a complex sociotechnical work system. One of the authors had previous experience of work system analysis and quality improvement (QI) design using the SEIPS 2.0 model from their undergraduate training, and we used the worksheet available from the NHS Education for Scotland’s Knowledge Network webpage on ‘Systems Thinking’ to provide a basic structure to our work system analysis.16 The Teaching Lead for Patient Safety at our institution supported us in applying this human factors knowledge to our project design.
We identified that the key OPD-RVH interface during clinic attendances was between the orthopaedic surgeon and the HCSW who accompanies patients to the appointment from RVH (figure 1). We identified that this interaction would be central to the successful implementation of the new tool, so we sought the views of HCSWs. We recognised there could be a reluctance for the HCSW to prompt the orthopaedic surgeon to complete this form due to organisational culture, hierarchy and team dynamics, and these concerns were echoed by the HCSWs. Thus, we moved to an approach to involve members of both departments in the design and implementation of the pro forma to empower and enable all members of the team to feel able to contribute to this QI intervention. In doing so, we gained a wider perspective of the issues. By capitalising on the expertise of the MDT at both sites and promoting a collaborative approach to improvement, we sought to ensure our intervention was sustainable.
Figure 1.
Diagram showing the application of the SEIPS 2.0 model into our work systems analysis. IT, information technology; OPD, outpatient department; PACS, picture archiving and communication system; RVH, Royal Victoria Hospital. Figure reproduced by permission of Taylor & Francis Ltd (www.tandfonline.com).
Strategy
In order to improve communication between both teams, our aim was for all patients attending the orthopaedics OPD for review to return to RVH with a completed written care plan which could be reviewed by therapists within 24 hours. We used the Model for Improvement to identify key issues and design our intervention.17 We completed two full PDSA cycles over a 2-month period, curtailed by local service redesign as a result of the COVID-19 pandemic.
PDSA cycle 1: designing and introducing a pro forma, raising awareness and dealing with staff concerns
During our first full PDSA cycle, we aimed to design and introduce our pro forma into the work system. We identified two patients who were due to attend the OPD over a 3-week period and intended to trial the pro forma during this time. We worked with members of the MDT to design a tool which would prompt clinicians to provide succinct and relevant clinical information, using the principles described earlier. We predicted that the introduction of a pro forma would reduce the time taken for key details to be shared between the OPD and inpatient teams.
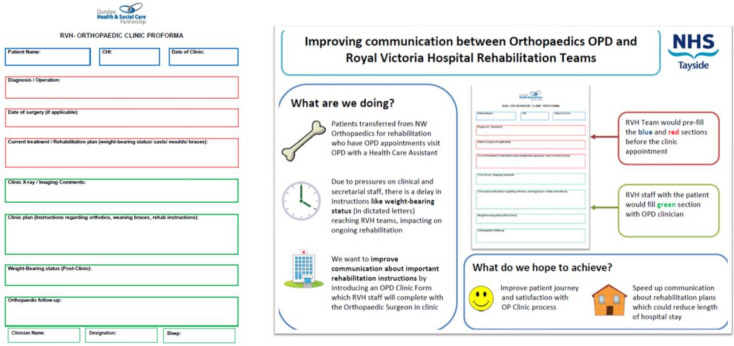
The pro forma was colour-coded, separating the document into three key sections to promote ease of completion. The first two sections, comprising blue and red text boxes, were intended to be prepopulated by the RVH team prior to clinic attendance. Blue boxes were designated for patient demographics, such as their name, Community Health Index (NHS) number and clinic date. Red boxes were designated for providing key information about diagnosis, the procedure performed (if applicable) and current therapy instructions. The third section, which had green text boxes, was designated for OPD clinicians’ comments on the clinic encounter itself, prompting for information about X-ray imaging, the clinic plan (including weight-bearing status) and future follow-up.
The form was presented at a local staff meeting, where we also highlighted our project to the wider RVH team. Senior medical and allied health clinicians felt the form was easy to use, and would provide the right amount of information without being burdensome for the OPD staff. The trial of our communication tool was communicated to senior OPD medical and nursing staff by email.
We printed several forms and filed them with other important documentation in the ward doctors’ rooms. On the day of the appointment, ward doctors prepopulated the form and filed it at the front of the patients’ medical notes, as these notes would accompany the patient to their appointment. A verbal reminder was provided to HCSWs that the form was at the front of the notes, and they were asked to make the OPD team aware of the form on their arrival to the OPD clinic.
Both patients attended the OPD on the same date. Although both forms were successfully completed in full, we received feedback from HCSWs that they felt reluctant to ask the surgeon to complete the pro forma, as they perceived there to be a lack of awareness about our project. It was also noted that there was no section for the OPD consultant to provide their contact details, meaning the RVH team were not able to ascertain who had led the consultation, and would have been unable to contact them to clarify any details if needed. Thus, we sought to take measures to enable the HCSW to prompt the OPD clinician, by reinforcing to them that the project was a collaborative project between RVH and the OPD, and explaining that the form had been accepted as a formal part of the work system. Additionally, we sought to amend the pro forma to reflect the form as it was being used in the real clinical setting, by adding text boxes for OPD clinician contact details.
During the first full PDSA cycle, an additional patient attended the OPD but was not accompanied with a form due to lack of awareness among the ward team about the project.
PDSA cycle 2: adapting the pro forma and gaining ‘buy-in’ from both teams
The pro forma was updated to include the consulting clinician’s details in the green section (figure 2). We also sent further correspondence about the QI project via email to the clinical lead for orthopaedics, which was cascaded to members of the wider team via a senior nurse, this included an updated proforma. The RVH physiotherapy team also liaised with their counterparts in the OPD. An infographic to draw attention to the pro forma was developed, outlining the key aims of our project and was distributed to both teams. We predicted that these changes would help to address the concerns raised by HCSWs about the effect of professional dynamics (and ‘power gradient’), promoting better completion of the pro forma.
Figure 2.
Example of clinical pro forma and quality improvement information poster. CHI, Community Health Index; NHS, National Health Service; OPD, outpatient department.
Over a 7-week period, five patients attended the OPD. The pro forma was received positively, with feedback from the HCSW and orthopaedic surgeons indicating that the form was becoming integrated into the OPD review process. HCSWs felt more empowered to ask the surgeon to complete, as we were able to reinforce to them that the form was a collaborative venture between the RVH and OPD teams. All five patients returned to RVH with fully completed forms.
Results
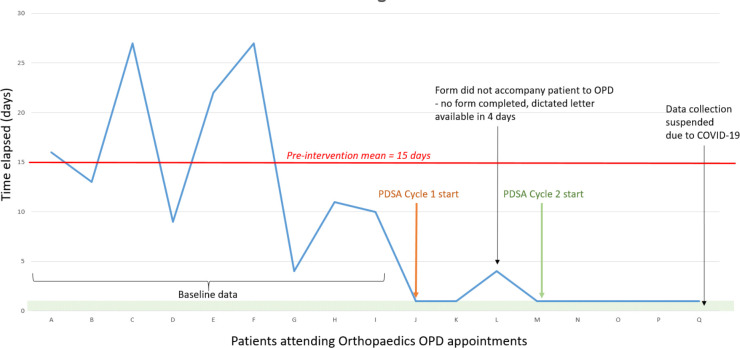
After two full PDSA cycles carried out over a 2-month period, we were able to demonstrate a marked improvement in the time taken to communicate key rehabilitation-focused clinical details to RVH therapy teams from the OPD. Our key aim was for all patients who attended the OPD to have a clinic plan available to therapists within 24 hours of their clinic attendance by the end of our project period. Although during our first PDSA cycle, one of three patients did not return to RVH with a completed form, all five patients thereafter returned from the OPD with completed forms (figure 3). A mixture of staff groups completed these forms, including the HCSW escorting the patient, outpatient clinic staff nurse and orthopaedic surgeons.
Figure 3.
Run chart demonstrating time elapsed (days) from OPD appointment to information-sharing with RVH team. OPD, outpatient department; PDSA, Plan–Do–Study–Act; RVH, Royal Victoria Hospital.
Specific feedback from the physiotherapists stated “the information was perfect for what we needed—not too detailed and all the information we need to progress safely with rehab”, and “anecdotally we are able to more quickly proceed with rehab with improved communication; this has reduced our need to chase orthopaedics for information they have already provided. We would have seen these patients on day 1 prior to the form but it now means we can more quickly progress and work on mobility.”
We consider the previously measured 15-day average period from clinic attendance to letters being available on Clinical Portal to represent potential ‘rehabilitation days lost’. Our interventions have resulted in a much prompter channel for information-sharing with minimal delay. Thus, although difficult to quantify, the introduction of this tool has the potential to reduce overall duration of hospital stay and improve the patient journey for those requiring specialist rehabilitation in RVH following acute orthopaedic admission.
The NHS comprises a complex sociotechnical work system where there is a need for multiprofessional and interdisciplinary approaches to patient care, delivered across a range of high and low acuity specialties. The addition of a clinical communication tool could add to this complexity by representing a burdensome task which busy teams are expected to complete. We were careful to design a form which was easy to complete and only asked for essential information. However, our pro forma did not replace dictated letters as the formal communication channel between both teams; instead, it was an interim communication tool to expedite the sharing of key information. The completion of the pro forma by the orthopaedics team could therefore result in duplication of work, since the OPD clinicians would ultimately go on to dictate a letter which would have to be transcribed. We initially intended to gather information about this as one of our balancing measures but were unable to do so. We would intend to do this in the future as part of further PDSA cycles.
Although we recognised the potential ‘power gradient’ between HCSWs and the orthopaedic surgeon during our initial work system analysis, we only addressed this issue during our second full PDSA cycle. We took measures to make our project more visible and provided the HCSWs with confidence to prompt the OPD clinician by ensuring the team knew our pro forma had been accepted by senior clinicians as a part of the OPD process. However, the number of patients attending the OPD from RVH remains fairly small, meaning not many HCSWs will experience this process and those who do attend OPD appointments could lose the confidence to prompt the surgeons if this is an infrequent encounter. Additionally, the individual (personal) characteristics of these key members of the work system may influence future encounters, and these individual factors cannot be easily controlled. Thus, in the future, measures should be taken to minimise the impact of this professional power gradient through continued liaison between the RVH and OPD clinical teams. This is a role that could be taken on by a junior doctor or allied health professional.
A further issue which is common to many QI projects is sustainability in the longer term. The junior medical team at RVH consists of trainee doctors who rotate every 3–4 months during a typical year. Thus, measures were taken to ensure permanent staff members such as staff nurses and HCSWs are on board with the use of the pro forma. To maintain momentum and promote the use of the form, information about this project and its positive results have been included in the ‘Junior Doctor Induction Pack’ for RVH. We have also placed the infographic posters in prominent areas, such as beside nursing stations and on notice boards in staff areas.
Due to the COVID-19 pandemic, our project was interrupted and further PDSA cycles were not able to go ahead during our time at RVH. The OPD clinic structure and work environment was adapted to place an emphasis on virtual reviews, rather than in-person appointments within the OPD itself. The use of the pro forma has been suspended during this period, and its continued use may need to be reassessed depending on how the OPD functions as services return to previous ways of working in the COVID-19 recovery period.
Given this change in approach during the COVID-19 pandemic, there is a possibility that processes within the OPD may change significantly, as outpatient services are being remodelled. We anticipate there may be a longer term shift towards virtual clinics, which already take place for certain patients who attend the local emergency department with bony injuries. The costs associated with clinic attendance for RVH patients may also justify the introduction of such a virtual fracture clinic. RVH patients may be able to attend the onsite radiology department for X-ray imaging, which can then be reviewed by and commented upon by the OPD remotely. In this case, our pro forma could be adapted for electronic completion, in order to continue to facilitate prompt information-sharing.
Conclusions
Over the course of two full PDSA cycles, we have demonstrated that introducing a clinical communication tool can facilitate timely and effective information-sharing between orthopaedics and MFE rehabilitation teams working within the same NHS health board area, but across two different hospital sites.
We were able to demonstrate a significant improvement in the time taken for relevant information to be communicated by promoting the integration of the pro forma into the sociotechnical work system. In turn, this helped to ensure that the therapy teams’ care plans were aligned with the OPD clinician’s instructions, promoting a more streamlined patient journey through the rehabilitation process.
Due to the COVID-19 pandemic, our project prematurely ended and we were unable to formalise feedback from the OPD team, which would have included gathering data for our intended balancing measures. Qualitative feedback from the therapists in RVH was positive, especially from physiotherapists who were happy with the perceived improvement in time taken for patients to move forward in their rehabilitation journeys. In light of COVID-19 and a shift to virtual reviews, the current pro forma may need to be adapted to reflect changes to the OPD’s way of working.
Our project emphasises the need to ensure that key stakeholders are identified during the initial design phase when introducing a clinical communication tool, to allow steps to be taken to address potential confounding factors such as culture and hierarchy. Additionally, clear communication is vitally important to ensure professionals from a variety of backgrounds and working in different hospitals can collaborate and ‘buy in’ to an improvement project. The design and implementation of this tool was a truly multidisciplinary venture which contributed to a more streamlined process with positive outcomes for patients and the healthcare team.
Acknowledgments
Chris Taylor, lead physiotherapist, and wider multidisciplinary team at Royal Victoria Hospital, Dundee, UK; orthopaedics outpatient department team, Ninewells Hospital, Dundee, UK.
Footnotes
Contributors: ST and RM are joint first authors and undertook baseline data collection, designed and managed PDSA cycles, and authored the final report. VT provided advice throughout the project and critically appraised the final report.
Funding: Funding to allow publication of this work was made available through NHS Tayside Directorate of Medical Education Additional Cost of Teaching (ACT) Funds (9436849369).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon request.
References
- 1.British Orthopaedic Association Care of patients with fragility fractures. Available: https://www.bgs.org.uk/sites/default/files/content/attachment/2018-05-02/Blue%20Book%20on%20fragility%20fracture%20care.pdf [Accessed 22 Jul 2020].
- 2.Kanis JA, Oden A, Johnell O, et al. The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 2001;12:417–27. 10.1007/s001980170112 [DOI] [PubMed] [Google Scholar]
- 3.National Intitute for Health and Care Excellence Osteoporosis: assessing the risk of fragility fracture clinical guideline. Available: https://www.nice.org.uk/guidance/cg146/chapter/introduction [Accessed 22 Jul 2020]. [PubMed]
- 4.Amin S, Achenbach SJ, Atkinson EJ, et al. Trends in fracture incidence: a population-based study over 20 years. J Bone Miner Res 2014;29:581–9. 10.1002/jbmr.2072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grund S, Gordon AL, van Balen R, et al. European consensus on core principles and future priorities for geriatric rehabilitation: consensus statement. Eur Geriatr Med 2020;11:233–8. 10.1007/s41999-019-00274-1 [DOI] [PubMed] [Google Scholar]
- 6.Giusti A, Barone A, Razzano M, et al. Optimal setting and care organization in the management of older adults with hip fracture. Eur J Phys Rehabil Med 2011;47:281–96. [PubMed] [Google Scholar]
- 7.Lahtinen A, Leppilahti J, Harmainen S, et al. Geriatric and physically oriented rehabilitation improves the ability of independent living and physical rehabilitation reduces mortality: a randomised comparison of 538 patients. Clin Rehabil 2015;29:892–906. 10.1177/0269215514559423 [DOI] [PubMed] [Google Scholar]
- 8.Weller J, Boyd M, Cumin D, Teams CD. Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J 2014;90:149–54. 10.1136/postgradmedj-2012-131168 [DOI] [PubMed] [Google Scholar]
- 9.Weaver SJ, Lyons R, DiazGranados D, et al. The anatomy of health care team training and the state of practice: a critical review. Acad Med 2010;85:1746–60. 10.1097/ACM.0b013e3181f2e907 [DOI] [PubMed] [Google Scholar]
- 10.Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington (DC): National Academies Press (US), 2000. https://www.ncbi.nlm.nih.gov/books/NBK225182/ [PubMed] [Google Scholar]
- 11.Toccafondi G, Albolino S, Tartaglia R, et al. The Collaborative communication model for patient handover at the interface between high-acuity and low-acuity care. BMJ Qual Saf 2012;21 Suppl 1:i58–66. 10.1136/bmjqs-2012-001178 [DOI] [PubMed] [Google Scholar]
- 12.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care 2004;13 Suppl 1:i85–90. 10.1136/qshc.2004.010033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Müller M, Jürgens J, Redaèlli M, et al. Impact of the communication and patient hand-off tool SBAR on patient safety: a systematic review. BMJ Open 2018;8:e022202. 10.1136/bmjopen-2018-022202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramsay N, Maresca G, Tully V, et al. Does a multidisciplinary approach have a beneficial effect on the development of a structured patient handover process between acute surgical wards in one of Scotland's largest teaching hospitals? BMJ Open Qual 2018;7:e000154. 10.1136/bmjoq-2017-000154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics 2013;56:1669–86. 10.1080/00140139.2013.838643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.NHS Education for Scotland Knowledge Network Human factors for health and social care – systems thinking. Available: http://knowledge.scot.nhs.uk/hfe/systems-thinking/seips.aspx [Accessed 5 Jan 2021].
- 17.Institute for Healthcare Improvement How to improve. Available: http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx [Accessed 30 Sep 2020].