Abstract
This is a rare case report of two filamentous fungi in a patient with contact lens related keratitis. An early corneal scrape may be useful in detecting multiple causative pathogens and aiding management. The main learning point is to consider fungal infections in patients with atypical ulcer appearances, as prompt diagnosis may reduce the morbidity burden.
Keywords: ophthalmology, visual pathway
Background
Infectious keratitis is a condition in which the cornea becomes infected by a variety of microbial agents. These can be bacterial, viral, parasitic or fungal. Fungal keratitis is estimated to account for between 1% and 5% of all infectious keratitis in temperate climates,1 and within the UK, the incidence has been estimated at 0.32 cases per million individuals per year.2 The causative fungal organisms can be further subdivided into filamentous, yeasts and dimorphic fungi. Within temperate climates yeasts are thought to account for roughly 30%–52% of all fungal keratitis.1 In the literature, the main risk factors are; corneal trauma contaminated with organic matter, contact lens wear and corneal surgery.1 The prompt identification and treatment of fungal keratitis is essential in reducing morbidity. In the literature, it is estimated that fungal keratitis can result in the loss of the globe in 10%–25% of cases.1 In this article, a case of fungal keratitis due to unusual fungi is presented and discussed.
Case presentation
We present a case of a woman in her fifties who attended the emergency eye clinic with a 24-hour history of an uncomfortable, photophobic left eye following contact lens removal. She reported being a monthly soft contact lens wearer, who did not sleep or shower with her contact lenses in situ. She had no preceding history of trauma and the only medical history of note was episcleritis.
At the initial consultation her visual acuity was 6/6 OD and 6/9 OS. Examination of the left cornea demonstrated a 1.5 × 1.2 mm superficial corneal ulcer with a single 0.5 mm satellite lesion (figure 1). Both ulcers were located outside the visual axis along the horizontal meridian.
Figure 1.
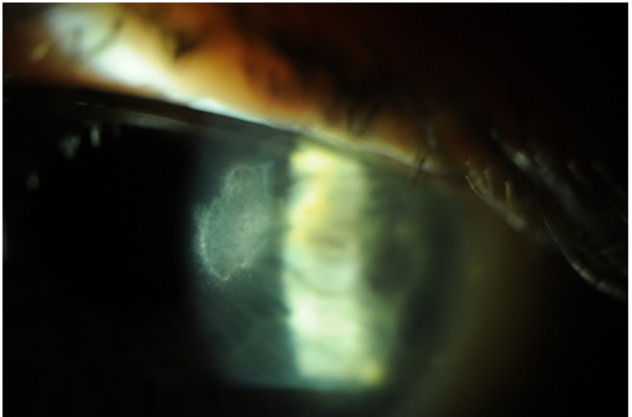
Location of the main corneal ulcer—5 days after treatment was commenced and after corneal scrapping.
Investigations
Initial empiric treatment comprised topical ofloxacin hourly. After 4 days, the eye was more comfortable but vision had reduced to 6/24, with little change in the ulcer size. Given the clinical deterioration, a potential fungal infection was entertained and a corneal scrape was performed. As the corneal scrape was taken at the time of her review appointment, the initial empiric treatment of ofloxacin had not been discontinued prior to the scraping. Corneal scrape samples were sent to the microbiology lab for microscopy, gram staining and calcofluor white staining. Further corneal scrape samples were plated onto blood agar, chocolate agar and Sabouraud’s agar. After our local laboratory found the presence of fungi in her samples, these were sent to the reference laboratory in Manchester where microscopy with further staining using Lactophenol blue was performed to highlight the morphological features of the organism.
Differential diagnosis
Our initial differential diagnosis was of a bacterial keratitis as this is the most common cause of a corneal ulcer in the UK in contact lens wearers.1 The other differential we considered was of a fungal keratitis, mainly because of the satellite lesion and the drop in vision despite treatment.
Treatment
While awaiting the corneal scrape report the empiric treatment with ofloxacin was maintained. The results were positive for the fungi—Acremonium strictum and Fusarium dimerum. These results were somewhat unexpected and were discussed with microbiology team. The microbiologist suggested that as there was growth of the Acremonium species, compared with an isolation of the Fusarium species, the former was most likely the main culprit and advised oral voriconazole 400 mg two times per day loading dose, followed by 13 days 200 mg two times per day. Prior to commencing this regimen, we obtained blood samples for her urea and electrolytes, which were normal. We also discontinued her empiric topical treatment with ofloxacin and topically we commenced Hyloforte ocular lubricants.
Outcome and follow-up
Ten days after commencing oral voriconazole, vision in the left eye improved to 6/7.5 and the patient reported a marked improvement in her symptoms. At the time of discharge, the final visual acuity was 6/12 unaided improving to 6/6 with pinhole. Vision was reduced due to superficial anterior stromal scarring on the corneal surface inducing a degree of irregular astigmatism.
Discussion
Fungal keratitis is rarely encountered in UK clinical practice and typically follows an insidious clinical course, generally due to the delay in recognition and instigation of treatment.2 3 Acremonium is a filamentous, soil saprophyte which is linked to causing a rare form of fungal keratitis.4
The available literature describing fungal keratitis, is limited to case reports and observational studies, with the majority of cases linked to ocular trauma and particularly contamination with vegetable matter. Alfonso et al also published a case series describing Acremonium fungal keratitis following laser in situ keratomileusis.5 To our knowledge and on review of the literature, it has only been found to be implicated in cases of known trauma, ocular surgery or contamination with vegetable matter. A single case report was identified describing fungal keratitis caused by Acremonium in a patient using soft contact lenses. However, it was noted that this patient suffered from recurrent corneal erosions and used multiple courses of topical steroids for a period of 12 months prior to developing fungal keratitis.6 This is in contrast to our woman who had no other medical history and was on no medication. As fungal keratitis infections are uncommon, they are at times not considered in a prompt manner which can impact the recovery and prognosis for patients.
The most challenging aspect following identification of fungal keratitis and particularly, caused by A. striatum, is the treatment and management. The lack of consensus in the literature regarding the optimum choice of antifungal medication to use, as well as the route of administration best suited. Most clinical guidelines support empirical treatment for suspected fungal keratitis with either topical amphotericin B or topical voriconazole, with oral preparations of the latter reserved for resistant cases.7 However, multiple reports and largely published anecdotal evidence suggested that those may not provide adequate cover for Acremonium species. Kim et al published a case series consisting of five patients with Acremonium fungal keratitis, and found the majority to be resistant to first line therapy with topical fluconazole and topical amphotericin B, but reported good outcomes with the use of topical natamycin and oral voriconazole.8 Carrasco and Genesoni suggested the use of topical amphotericin B as a subconjunctival injection and oral fluconazole, however, this was based on a single patient who had complete resolution of the keratitis following the proposed treatment plan.9 Other routes of administration for voriconazole have been described, such as subconjunctival and intrastromal injection, but this remains experimental and on a case-by-case basis.10
Our patient did respond well to oral voriconazole and maintained a good visual acuity after resolution of her infection. Therefore, it is important consider rare causes of fungal keratitis and particularly, Acremonium, as identification is likely result in alteration of the management plan in order to prevent sight threatening complications.3 Taking into account the paucity in clinical guidelines to aid management in such cases, it would be reasonable to commence anti-fungal medication as available but monitor closely and consider prompt alteration if failing to respond clinically, even in the absence of classic risk factors.
Fusarium is a filamentous fungi and is considered among the most common causes of a fungal keratitis, usually associated with contact lens wear.11 Superimposed bacterial infection in fungal keratitis and vice versa is a relatively common occurrence. However, our patient’s keratitis was due to infections with two fungal species, Fusarium and Acremonium, for which there are no cases reported in the literature.12 There has in the literature been reported a single case of a filamentous fungal keratitis due to Acremonium and Penicillin species. Here, the authors found the optimal management was achieved by the use of topical amphotericin B alternated with topical natamycin and oral ketoconazole.13
Learning points.
Consider fungal infections in patients with atypical ulcer appearance, as prompt diagnosis may reduce the morbidity burden.
If a corneal ulcer is not improving within a few days of commencing treatment consider performing an early corneal scrape.
Early corneal scrapping is useful in identifying any causative pathogens, be they singular or multiple and in aiding management.
Footnotes
Contributors: All the authors in this work have been involved in the described case. They have all contributed to all sections of the article be it in content or reviewing the content prior to submission. CT was the main author of the article, they identified the patient and was involved in their care. BS did the primary research on the discussion points and consented the patient. JW was the clinician responsible for the patient’s care and proof read the article once it was completed.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bourcier T, Sauer A, Dory A, et al. Fungal keratitis. J Fr Ophtalmol 2017;40:e307–13. 10.1016/j.jfo.2017.08.001 [DOI] [PubMed] [Google Scholar]
- 2.Tuft SJ, Tullo AB. Fungal keratitis in the United Kingdom 2003-2005. Eye 2009;23:1308–13. 10.1038/eye.2008.298 [DOI] [PubMed] [Google Scholar]
- 3.Sahay P, Goel S, Nagpal R, et al. Infectious keratitis caused by rare and emerging micro-organisms. Curr Eye Res 2020;45:761–73. 10.1080/02713683.2019.1708407 [DOI] [PubMed] [Google Scholar]
- 4.Kumar A, Khurana A, Sharma M, et al. Causative fungi and treatment outcome of dematiaceous fungal keratitis in North India. Indian J Ophthalmol 2019;67:1048. 10.4103/ijo.IJO_1612_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alfonso JF, Baamonde MB, Santos MJ, et al. Acremonium fungal infection in 4 patients after laser in situ keratomileusis. J Cataract Refract Surg 2004;30:262–7. 10.1016/S0886-3350(03)00646-1 [DOI] [PubMed] [Google Scholar]
- 6.Yamamoto GK, Pavan-Langston D, Stowe GC, et al. Fungal invasion of a therapeutic soft contact lens and cornea. Ann Ophthalmol 1979;11:1731–5. [PubMed] [Google Scholar]
- 7.Bunya VY, Hammersmith KM, Rapuano CJ, et al. Topical and oral voriconazole in the treatment of fungal keratitis. Am J Ophthalmol 2007;143:151–3. 10.1016/j.ajo.2006.07.033 [DOI] [PubMed] [Google Scholar]
- 8.Kim S-J, Cho Y-W, Seo S-W, et al. Clinical experiences in fungal keratitis caused by Acremonium. Clin Ophthalmol 2014;8:283–7. 10.2147/OPTH.S54255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carrasco MA, Genesoni G. Treatment of severe fungal keratitis with subconjunctival amphotericin B. Cornea 2011;30:608–11. 10.1097/ICO.0b013e3181fb826d [DOI] [PubMed] [Google Scholar]
- 10.Haddad RS, El-Mollayess GM. Combination of intracameral and intrastromal voriconazole in the treatment of recalcitrant Acremonium fungal keratitis. Middle East Afr J Ophthalmol 2012;19:265. 10.4103/0974-9233.95271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun CQ, Lalitha P, Prajna NV, et al. Association between in vitro susceptibility to natamycin and voriconazole and clinical outcomes in fungal keratitis. Ophthalmology 2014;121:1495–500. 10.1016/j.ophtha.2014.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fernandes M, Vira D, Dey M, et al. Comparison between polymicrobial and fungal keratitis: clinical features, risk factors, and outcome. Am J Ophthalmol 2015;160:873–81. 10.1016/j.ajo.2015.07.028 [DOI] [PubMed] [Google Scholar]
- 13.Chen N, Lee Y-C. Mixed fungal keratitis of Penicillium species and Acremonium species. Tzu Chi Med J 2011;23:26–7. 10.1016/j.tcmj.2011.01.004 [DOI] [Google Scholar]


