Abstract
Objective
To determine interest in and barriers to video visits in safety-net patients with diverse age, racial/ethnic, or linguistic background.
Materials and Methods
We surveyed patients in an urban safety-net system to assess: interest in video visits; ability to successfully complete test video visits; and barriers to successful completion of test video visits.
Results
Among 202 participants, of which 177 (87.6%) were persons of color and 113 (55.9%) preferred non-English languages, 132 (65.3%) were interested in and 109 (54.0%) successfully completed a test video visit. Younger age, non-English preference, and prior smartphone application use were associated with interest. Over half (n = 112) reported barriers to video visits; Internet/data access was the most common barrier (n = 50, 24.8%).
Conclusion
Safety-net patients are interested in video visits and able to successfully complete test visits. Internet or mobile data access is a common barrier in even urban safety-net settings and may impact equitable telemedicine access.
Keywords: telemedicine, digital divide, healthcare disparities, safety-net providers, vulnerable populations
INTRODUCTION
Before the COVID-19 pandemic, telemedicine video visits were uncommon, especially within safety-net settings. A 2018 survey found only 44% of community health centers used any telehealth. In the health centers that used telehealth, only half of the use was for patient-facing encounters instead of clinician-to-clinician encounters and < 30% of use was for primary care.1COVID-19-related physical distancing recommendations and changes in reimbursement policies2 triggered wide scale conversion to telemedicine encounters.3 Prior studies on interest in video visits focused on the subset of patients who had already completed a video visit, representing early adopters who are likely different from the general population.4,5
As telemedicine becomes a standard modality for healthcare, little is known about the interest in or challenges to video visits among low-income, diverse racial/ethnic, or non-English speaking populations. These populations already face disparities accessing healthcare and are already less likely to use digital health tools due to disparities in device ownership, broadband access, and digital literacy.6–8 To understand the interest and accessibility of video visits among safety-net patients, we conducted an in-depth survey in a public healthcare system to inform strategies to ensure equitable access.
MATERIALS AND METHODS
Design, setting, and participants
Cross-sectional phone survey of all patients scheduled with approximately 20 clinicians for a telephone visit during a 2-week period at the women’s health or general medicine clinic in an urban safety-net system, where most patients are uninsured or Medicaid-insured.9
Protocol
Participants were called by trained research analysts or medical student volunteers in their preferred language (with an interpreter, if needed) before their telephone appointment and asked about their interest in video visits. All participants were asked about access to a digital device with video capability, access to mobile data/Internet, and prior use of smartphone applications. If participants were not interested, they were asked to identify reason(s) why. (Call script and survey in Supplementary eMethods). If patients were interested, the caller offered to provide instructions for downloading the video application and conduct a simulated video visit. We focused on downloading the video application used in our health system for telemedicine video visits during the time of this study; this application is accessible through a computer web browser, desktop client, or as a mobile application on the Apple App Store, Google Play App Store, and Amazon Appstore. Sociodemographic characteristics (age, gender, race/ethnicity, and preferred language) and patient portal enrollment were collected from chart review. We also noted if the participant required help from a household member during the call to successfully complete a simulated video visit. This study protocol was reviewed by an institutional review board and determined to be quality improvement. Patient completion of the phone survey was used to indicate consent.
Outcomes
The primary outcome was interest in video visits. The secondary outcome was success downloading the video application and completing a simulated video visit. We also describe barriers to interest in video visits or successful completion of a simulated video visit.
Analysis
We report the bivariate relationship between sociodemographic characteristics and technology experience with outcomes. We conducted a multivariable logistic regression analysis of the primary outcome, adjusting for age, language, and smartphone application use.
RESULTS
Of 298 patients called, 202 were reached. The majority identified as persons of color (87.6%) and/or preferred a non-English language (55.9%). Reached participants were more likely to be Latinx and speak Spanish than those not reached.
Predictors of interest in video visits and successful completion of test video visits
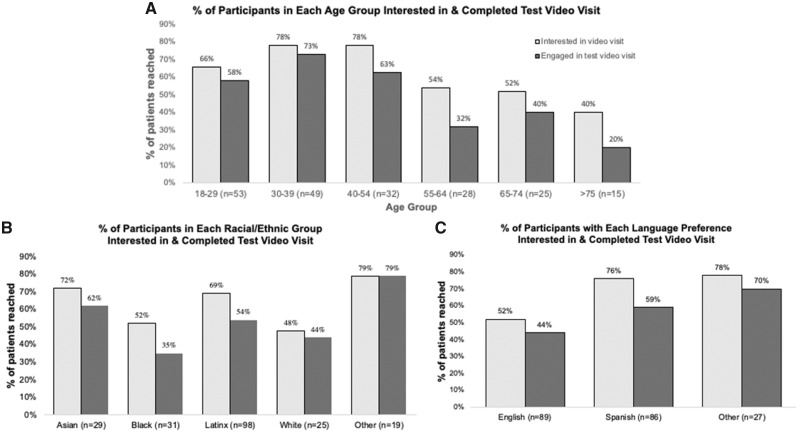
Among the 202 surveyed participants, 132 (65.3%) were interested and 109 (54.0%) successfully completed a simulated video visit (Table 1). Neither race/ethnicity nor gender were associated with outcomes. Younger age was associated with interest in video visits and completion of a simulated video visit. Nearly two-thirds of participants < 55 years old completed a simulated video visit in comparison to one-third of participants 55+ years old. Non-English-speakers were more likely to be interested in video visits (76% vs 51%). In several groups (≥ 40 years old, Black, Latinx, or Spanish-speaking), ≥ 15% patients interested in video visits could not download the video application during the call. (Figure 1)
Table 1.
Sociodemographic characteristics of participants (N = 202)
| Characteristic | Respondents, No (%) |
||
|---|---|---|---|
| All Participants (N = 202) | Interested in video visit (N = 132) | Completed test video visit (N = 109) | |
| Age, y b, c | |||
| 18–29 | 53 (26.2%) | 35 (26.5%) | 31 (28.4%) |
| 30–39 | 49 (24.3%) | 38 (28.8%) | 36 (33.0%) |
| 40–54 | 32 (15.8%) | 25 (18.9%) | 20 (18.4%) |
| 55–64 | 28 (13.9%) | 15 (11.4%) | 9 (8.3%) |
| 65–74 | 25 (12.4%) | 13 (9.9%) | 10 (9.2%) |
| > 75 | 15 (7.4%) | 6 (4.6%) | 3 (2.8%) |
| Gender | |||
| Male | 53 (26.2%) | 31 (23.5%) | 23 (21.1%) |
| Female | 149 (75.2%) | 101 (76.5%) | 86 (78.9%) |
| Language preference a, b | |||
| English | 89 (44.1%) | 46 (34.9%) | 39 (35.8%) |
| Spanish | 86 (42.6%) | 65 (49.2%) | 51 (46.8%) |
| Other | 27 (13.4%) | 21 (15.9%) | 19 (17.4%) |
| Race/ethnicity a | |||
| Asian | 29 (14.4%) | 21 (15.9%) | 18 (16.5%) |
| Black | 31 (15.4%) | 16 (12.1%) | 11 (10.1%) |
| Latinx | 98 (48.5%) | 68 (51.5%) | 54 (49.5%) |
| White | 25 (12.4%) | 12 (9.1%) | 11 (10.1%) |
| Other | 19 (9.4%) | 15 (11.4%) | 15 (13.8%) |
P < .05 for patients reached.
P < .05 for patients interested in video.
P < .05 for patients that completed test video visit.
Figure 1.
Percentage of patients reached in each (A) age range, (B) racial/ethnic group, or (C) language preference group that expressed interest in having a video visit and successfully completed a test video visit.
In our sample, 42 patients (20.8%) were enrolled in the online patient portal, and 149 (73.8%) had experience using smartphone applications. Patient portal enrollment was not associated with interest in video visits, but every interested portal user successfully completed a simulated video visit. Prior smartphone application use was associated with both interest in video visits and success in completing a simulated video visit (Supplementary eTable 1, P < .001).
In multivariable analyses adjusting for age, language, and smartphone application use, non-English language preference and smartphone application use were significantly associated with higher interest in video visits. (Supplementary eTable 2)
Barriers to video visits
Among the 202 participants, over half (n = 112) reported at least 1 barrier to video visits. Nearly one-quarter (n = 50) reported concerns about data/Internet access. Barriers were more common in participants 55+ years old than <55 years old (75% vs 46%, Supplementary eTable 3). Fewer than 10% of participants reported barriers related to security, privacy, or lack of time.
Among the 93 participants who did not successfully complete a simulated video visit, >30% reported inadequate data/Internet access (n = 42); hesitancy about technology (n = 33); no access to device (n = 31); or belief that video visits were not better than telephone visits (n = 31). (Table 2) Younger participants were more likely to have devices but report video visits were not better than telephone.
Table 2.
Barriers reported to video visits by patients who did not complete a test visit (n = 93)
| At least 1 barrier | No Device | Data/Internet issues | Hesitant to use technology | Not better than phone | |
|---|---|---|---|---|---|
| Total (n, %) | 92 (99%) | 31 (33%) | 42 (45%) | 33 (36%) | 31 (33%) |
| Age, y a, b | |||||
| 18–29 (n = 22) | 22 (100%) | 0 (0%) | 6 (29%) | 5 (23%) | 12 (55%) |
| 30–39 (n = 13) | 12 (92.3%) | 0 (0%) | 3 (25%) | 3 (23%) | 7 (54%) |
| 40–54 (n = 12) | 12 (100%) | 4 (36%) | 7 (64%) | 4 (33%) | 5 (42%) |
| 55–64 (n = 19) | 19 (100%) | 9 (50%) | 9 (56%) | 9 (47%) | 4 (21%) |
| 65–74 (n = 15) | 15 (100%) | 10 (67%) | 9 (64%) | 7 (47%) | 2 (13%) |
| > 75 (n = 12) | 12 (100%) | 8 (67%) | 8 (67%) | 5 (42%) | 1 (8%) |
| Language preference | |||||
| English (n = 50) | 49 (98%) | 15 (31%) | 18 (40%) | 19 (38%) | 17 (34%) |
| Spanish (n = 35) | 35 (100%) | 11 (31%) | 19 (58%) | 11 (31%) | 14 (37%) |
| Other (n = 8) | 8 (100%) | 5 (63%) | 5 (63%) | 3 (38%) | 1 (13%) |
| Race | |||||
| Asian (n = 11) | 11 (100%) | 5 (50%) | 5 (50%) | 1 (9%) | 1 (9%) |
| Black (n = 20) | 20 (100%) | 7 (37%) | 7 (41%) | 7 (35%) | 7 (35%) |
| Latinx (n = 44) | 44 (100%) | 11 (25%) | 22 (52%) | 14 (32%) | 19 (43%) |
| White (n = 14) | 13 (93%) | 5 (36%) | 7 (50%) | 8 (57%) | 3 (21%) |
| Other (n = 4) | 4 (100%) | 3 (75%) | 1 (25%) | 3 (75%) | 1 (25%) |
P < .05 for device access.
P < .05 for perception not better than phone.
Almost 25% of participants that completed a simulated video visit (27/102) received help from a household member. Approximately half of participants with a non-English/Spanish language preference (9/18) or ≥ 55 years old (13/22) who successfully completed a simulated video visit needed help, which was higher than English/Spanish-speakers (P = .002) or participants < 55 years old (P < .001), respectively.
DISCUSSION
In this survey of over 200 safety-net clinics patients, we found high interest in video visits, particularly among younger, non-English speaking participants with experience using smartphone applications. There was no difference in interest among racial/ethnic groups. Despite interest, over half of the patients reported at least 1 barrier to a video visit. Mobile data or Internet access was the most common challenge and reported by approximately 1 in 4 participants. Our finding of broad interest in video visits as well as the importance of age and comfort with technology is consistent with prior literature on the acceptance of telemedicine and other health technology, such as patient portals.10–12 These findings suggest that device or data barriers may drive differences in health technology uptake among diverse patients more than lack of patient interest.
The majority of our safety-net patients were interested in video visits regardless of language, race/ethnicity, age, or engagement with patient portals. No prior studies have documented interest or barriers to video visits in a diverse, multilingual safety-net population. Surprisingly, we found English-speakers were less interested in video visits, possibly representing concerns about privacy among English-speakers, as documented in prior studies.13,14 Alternatively, non–English-speakers may perceive language barriers as easier to overcome with visual cues, consistent with literature showing better communication outcomes with video interpreters over phone interpreters.15 Future studies should explicitly investigate both privacy concerns and patient understanding after video versus audio-only telemedicine visits for patients with communication challenges, such as patients with limited English proficiency or health literacy.
Despite the higher rates of barriers, nearly half of participants ≥ 65 years old reported interest in video visits. The greater prevalence of barriers among older patients in this study supports work documenting a digital divide in older adults, specifically with regard to device access and digital literacy.6,12,16,17 Therefore, it is crucial to support efforts to teach older individuals (and others with lower digital literacy) about how to access video visits.7 Without system workflows or payor incentives to provide support to patients, equity in telemedicine access will be impossible; in our work, two-thirds of calls lasted < 5 minutes, suggesting the feasibility of targeted support to patients who need it.
Despite only surveying urban residents, access to data/Internet was a barrier reported by one-quarter of all participants and across all sociodemographic traits. Without improved, low-cost access to data/Internet necessary for high-quality video communication, video visits will be inaccessible for many safety-net patients. This finding is consistent with literature that broadband access is associated with patient portal use.18,19 Given the growing importance of telemedicine and patient portals, our findings reinforce the need to advocate for digital infrastructure to ensure equitable telemedicine and healthcare access.6,7 Our study also highlights that digital access is a concern not only in rural populations but also for the 35 million Americans who live in poverty in urban areas.
This study is limited as a single-site survey of patient self-reported barriers. We also only surveyed patients scheduled for a visit and who answered the phone; therefore, our sample may not be fully representative of an entire safety-net population. Nonetheless, given the focus on a safety-net population with significant racial/ethnic and linguistic diversity, it provides important insights for telemedicine implementation, particularly among groups that have previously experienced inequities in health outcomes.
Future studies should explore longer-term uptake or sustained use of telemedicine among a broad population of safety-net patients to understand the generalizability of these findings, as well as whether specific interventions to address telemedicine uptake can mitigate barriers that emerged in this study (cost, Internet access, digital literacy).10,11 It will also be important to explore if there are patient, organizational, or environmental factors that may be either unique or more prominent in safety-net or lower socioeconomic status patients.11 This may help determine if current practices for patient-centered telemedicine (eg, patient training and education, mitigating privacy concerns) also adequately facilitate telemedicine access for diverse patients.
CONCLUSION
Diverse low-income patients are interested in video visits, and many are able to complete simulated video visits. However, a large portion of safety-net patients face challenges to successfully accessing video visits. To help ensure equity in telemedicine access, policies and infrastructure development are needed to address gaps in access to broadband or mobile data. Additionally, health systems and clinicians should develop plans to provide technical assistance to older patients and those with limited digital literacy to help ensure these patients can successfully access video visits. Deliberate implementation and advocacy are crucial to ensure clinicians equitably address patients’ interest in telemedicine video visits.
FUNDING
This work was supported by the Patrick and Catherine Weldon Donaghue Medical Research Foundation; the National Heart Lung and Blood Institute of the NIH under Award Number K12HL138046; and the National Center for Advancing Translational Sciences of the NIH under Award Number KL2TR001870.
AUTHOR CONTRIBUTIONS
EK, TD, MN, and CL made contributions to the design, analysis, and interpretation of the data. BB and OM acquired and interpreted the data for this work. GS contributed to analysis and interpretation of the data for this work. All authors revised the manuscript critically for important intellectual content and approved the final version to be published.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
Camilla Bykhovsky, Lauren Phinney, Marissa Silverman, Shannon Satterwhite, and Billy Zeng for helping with patient outreach.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Kim J-H, Desai E, Cole MB. How the rapid shift to telehealth leaves many community health centers behind during the COVID-19 pandemic | Health Affairs. https://www.healthaffairs.org/do/10.1377/hblog20200529.449762/full/ Accessed June 9, 2020
- 2.Centers for Medicare and Medicaid Services. Coronavirus Waivers & Flexibilities https://www.cms.gov/about-cms/emergency-preparedness-response-operations/current-emergencies/coronavirus-WaiversAccessed June 9, 2020
- 3. Mehrotra A, Ray K, Brockmeyer DM, Barnett ML, Bender JA.. Rapidly converting to “Virtual Practices”: outpatient care in the era of Covid-19. NEJM Catal 2020; 1. doi: 10.1056/CAT.20.0091. [Google Scholar]
- 4. Polinski JM, Barker T, Gagliano N, Sussman A, Brennan TA, Shrank WH.. Patients’ satisfaction with and preference for telehealth visits. J Gen Intern Med 2016; 31 (3): 269–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Slightam C, Gregory AJ, Hu J, et al. Patient perceptions of video visits using Veterans Affairs Telehealth tablets: survey study. J Med Internet Res 2020; 22 (4): e15682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rodriguez JA, Clark CR, Bates DW.. Digital health equity as a necessity in the 21st century Cures Act era. JAMA 2020; 323 (23): 2381. [DOI] [PubMed] [Google Scholar]
- 7. Nouri S, Khoong EC, Lyles CR, Karliner L.. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catal Innov Care Deliv 2020. https://catalyst.nejm.org/doi/pdf/10.1056/CAT.20.0123. [Google Scholar]
- 8. Khoong EC, Rivadeneira NA, Hiatt RA, Sarkar U.. The use of technology for communicating with clinicians or seeking health information in a multilingual urban cohort: cross-sectional survey. J Med Internet Res 2020; 22 (4): e16951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.San Francisco Department of Public Health San Francisco Department of Public Health Annual Report 2018-2019. https://www.sfdph.org/dph/files/reports/PolicyProcOfc/Full%20Report%20FY1819-%20Final%202.18.20.pdfAccessed June 15, 2020
- 10. Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M.. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare 2018; 24 (1): 4–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Or CKL, Karsh B-T.. A systematic review of patient acceptance of consumer health information technology. J. Am. Med. Inform. Assoc 2009; 16 (4): 550–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lam K, Lu AD, Shi Y, Covinsky KE. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern Med 2020; 180 (10): 1389–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Powell RE, Henstenburg JM, Cooper G, Hollander JE, Rising KL.. Patient perceptions of telehealth primary care video visits. Ann Fam Med 2017; 15 (3): 225–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tieu L, Sarkar U, Schillinger D, et al. Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: a qualitative study. J Med Internet Res 2015; 17 (12): e275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lion KC, Brown JC, Ebel BE, et al. Effect of telephone vs video interpretation on parent comprehension, communication, and utilization in the pediatric emergency department: a randomized clinical trial. JAMA Pediatr 2015; 169 (12): 1117–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Khoong EC, Le GM, Hoskote M, Rivadeneira NA, Hiatt RA, Sarkar U.. Health information-seeking behaviors and preferences of a diverse, multilingual urban cohort. Med. Care 2019; 57 (Suppl 6 Suppl 2): S176–S183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Roberts ET, Mehrotra A. Assessment of disparities in digital access among Medicare beneficiaries and implications for telemedicine. JAMA Intern Med 2020; 180 (10): 1386–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Perzynski ATRoach MJShick S, . et al. Patient portals and broadband internet inequality. J Am Med Inf Assoc 2017; 24 (5): 927–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rodriguez JA, Lipsitz SR, Lyles CR, Samal L.. Association between patient portal use and broadband access: a national evaluation. J Gen Intern Med 2020; doi: 10.1007/s11606-020-05633-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.