Abstract
Objective
Hiring medical scribes to document in the electronic health record (EHR) on behalf of providers could pose patient safety risks because scribes often have no clinical training. The aim of this study was to investigate the effect of scribes on patient safety. This included identification of best practices to assure that scribe use of the EHR is not a patient safety risk.
Materials and Methods
Using a sociotechnical framework and the Rapid Assessment Process, we conducted ethnographic data gathering at 5 purposively selected sites. Data were analyzed using a grounded inductive/hermeneutic approach.
Results
We conducted site visits at 12 clinics and emergency departments within 5 organizations in the US between 2017 and 2019. We did 76 interviews with 81 people and spent 80 person-hours observing scribes working with providers. Interviewees believe and observations indicate that scribes decrease patient safety risks. Analysis of the data yielded 12 themes within a 4-dimension sociotechnical framework. Results about the “technical” dimension indicated that the EHR is not considered overly problematic by either scribes or providers. The “environmental” dimension included the changing scribe industry and need for standards. Within the “personal” dimension, themes included the need for provider diligence and training when using scribes. Finally, the “organizational” dimension highlighted the positive effect scribes have on documentation efficiency, quality, and safety.
Conclusion
Participants perceived risks related to the EHR can be less with scribes. If healthcare organizations and scribe companies follow best practices and if providers as well as scribes receive training, safety can actually improve.
Keywords: patient safety, electronic health records, sociotechnical systems, medical scribes, qualitative research
INTRODUCTION
Medical scribes
The often-onerous burden of clinical documentation and the ubiquitous utilization of the electronic health record (EHR) can generate physician dissatisfaction and burnout.1,2 Medical scribes, defined as “paraprofessionals who transcribe clinic visit information into the EHRs in real time under physician (provider) supervision,”3 are consequently being utilized at an increasing pace. In the United States, many are preprofessional students aiming for careers in medicine, but with no clinical training.4 There are no licensing requirements for preprofessional scribes. Research results about scribe use are largely positive, but the safety of this unregulated new industry has not been assessed.
In 2019, Bossen et al published the results of a comprehensive literature review about medical scribes, highlighting 60 papers that describe primarily positive impacts.5 Fifty were based in the United States, 9 in Australia, and 1 in Canada. The authors explain that medical scribes do not exist in Scandinavian and other countries, or they may be called something else, so their search did not find more non-US studies. They also note that the United States might be unique in fostering the emergence of new professions such as scribing. Most cited studies reported productivity and satisfaction gains for providers along with more accurate and therefore increased billing.6–16 Several studies that measured patient satisfaction have shown either increased satisfaction or no change.3,6–10,14,16 Since their review included only papers published through 2017 and a good deal of research has been done since then, we updated their literature search, finding additional relevant papers with results similar to those in prior studies: The increase in provider satisfaction and productivity has been further verified.17–28 In addition, studies of scribes have found other positive outcomes, such as increasing the joy of practicing.24 It is therefore reasonable, after reviewing these studies, to conclude that the use of medical scribes can have a positive impact on provider workflow, provider and patient satisfaction, and on organizational finances.
There has, however, also been debate about the unintended consequences of scribes, which might include stifled EHR innovation because using scribes is a workaround indicative of problems inherent in EHRs.29–31 A second unintended consequence might be decreased note quality.32 Finally, expansion of the scribe role has also been cited as a concern.30 Scribes often do more than documentation, so there may be risks having unlicensed individuals with a broader set of duties. We found in a prior survey of clinic and risk managers that, especially in rural areas and small clinics, scribe roles go beyond documentation; risk managers are especially uneasy about assigning expanded roles to scribes.20 Guidelines by The Joint Commission suggest a much more limited scope than respondents reported to us.33 Clinical scribes, those who are licensed as MAs or nurses, are expected to keep their scribe roles separate and narrow within these guidelines. The level of risk having nonclinical scribes expanding their roles is not known.
Sociotechnical model for EHR safety
As Diana Forsythe noted in her seminal publications, information technology should not be studied within a narrow technology-oriented focus.34 Because scribes often play an integral role as part of a healthcare team embedded within the larger clinic ecosystem,35 they are part of a complex and dynamic sociotechnical workflow. An 8-dimensional sociotechnical model has been developed specifically to address EHR-related patient safety.36 The SAFER guides, a set of tools available through the US Office of the Coordinator for Health Information Technology, which can assist organizations in planning for and assessing the safety of their systems, include reference to the risks of scribe use,37 and were developed using this sociotechnical model. We selected this framework as a guide for this study to assure that we captured a complete picture. The 8 dimensions include personnel, hardware and software, interfaces, content, environment/rules and regulations, workflow, monitoring, and organizational characteristics. All aspects are dynamic, interrelated, and change over time.
Patient safety and best practices
There remain a number of gaps in our knowledge about scribes, especially related to EHRs. No studies have been done about the scribe perspective and, again noted by Diana Forsythe, such gaps in knowledge about perspectives, especially the views of those without power, can severely limit the usefulness of health information technology.34 We found only 2 studies related to the quality of documentation done by scribes. One, based on chart reviews comparing scribe and provider notes against a validated instrument for assessing note quality, found that scribe notes were superior to provider notes.38 The other, a simulation study by our team, showed large variations in the quality of scribe notes.32 A related question is whether there is a risk to patient safety when a scribe rather than a provider does documentation. Only 2 studies have been published addressing this: 1 was by our team39 and the other, conducted in Australia, found there is no difference in harms.26 Unfortunately, there is no set of best practices for scribes using EHRs that organizations and providers can rely on when making decisions about safety when implementing a scribe program.
Goals of this study
Our goal was to discover how much providers, scribes, and managers believe scribes affect documentation quality and EHR-related patient safety. We also aimed to identify best practices for scribes using the EHR safely.
MATERIALS AND METHODS
Site and participant selection
We used the Rapid Assessment Process (RAP) previously described in detail40–43 and the 8-dimensional sociotechnical framework36 for studying organizations that differ in their approaches to using scribes. RAP is a novel ethnographic approach that depends on a multidisciplinary team to expeditiously gather and analyze primarily qualitative data using carefully developed tools.
We selected sites in the United States so that all organizations were following the same federal guidelines. Sites were purposively selected for differences in geography, size, type of organization (academic vs community), and in model of scribe use (internal program vs scribe company). We selected 4 sites using the same product (Epic Systems) to minimize the variability of the technology dimension, plus 1 using AllScripts for comparison purposes. We selected participants based on their roles as scribes, providers, or others involved in scribe programs like clinic managers, quality improvement specialists, and scribe program managers (within both healthcare organizations and the vendor community).
Adaptation of the sociotechnical model throughout the process
As outlined in the previously mentioned SAFER guides,37 EHR safety is multidimensional, and it depends on factors that go well beyond technical aspects. Therefore, the sociotechnical model, which encompasses the entire landscape of safety, guided each phase of our research, from selection of participants, to development of interview questions, and to interpretation and presentation of results. However, we first modified it by collapsing it into 4 dimensions and, as in Figure 1, clarified the expectation that there would be more overlap, intersection, and synchrony among dimensions than is illustrated in the original framework. The 4 dimensions of hardware and software, content, user interface, and measurement and monitoring became our Technical dimension. We have renamed the personnel dimension the Personal dimension so that we could broaden it beyond manpower issues, the external rules and regulations dimension has become the Environmental dimension because we wanted to include all pressures from outside the organization. Finally, the organizational policies, procedures, and culture dimension has been shortened to the Organizational dimension.
Figure 1.
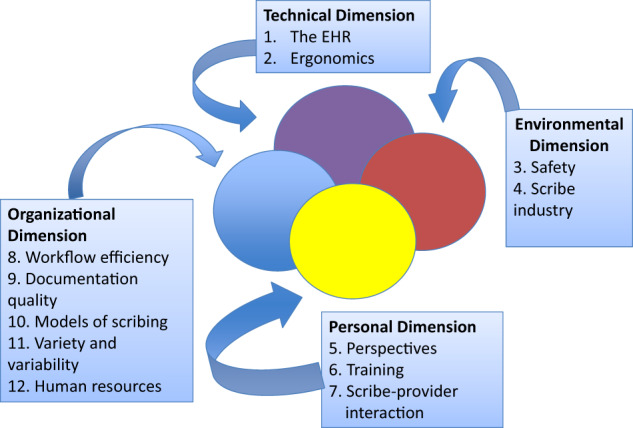
The 12 themes related to the use of scribes.
Ethical review
The institutional review boards (IRB) at OHSU and the 1 other site, which had an IRB, approved the study, as did the relevant oversight groups at the other sites. We followed informed consent procedures according to requirements of each site. Most sites allowed verbal consent after the participant read and discussed with researchers an information sheet about the study; 1 site required paper consent forms signed in the presence of a local staff member.
Data collection methods
We adapted the RAP40–43 to appropriately and accurately collect data from the study sites. A multidisciplinary research team of informaticians with varying backgrounds in healthcare, social sciences, and scribe management (former scribes who now train and manage scribe programs or clinic or scribe company managers), all with training in informatics and qualitative methods, collected and analyzed the data. Before each visit, we developed a field manual of tools consisting of 1) information about each site supplied by internal site sponsors who had helped us with arrangements, 2) different interview guides for providers, scribes, and managers, 3) observation guides with notes about foci for each visit, and 4) schedules for each site visitor. Triangulation was achieved via differing backgrounds of researchers and subjects, site variance, multiple methods, and differing analytical techniques. This rigorous triangulation strategy and iterative reflexivity (sharing one’s preconceived ideas to help researchers guard against bias) exercises were designed to assure high-quality data gathering and analysis. Member checking to assure trustworthiness of the results was done by means of site visit team meetings with internal site sponsors while on site and written reports of our findings after each visit.
Data collection consisted of semistructured interviews and observations in clinics. We enlisted the sociotechnical framework to ensure full coverage of important aspects of scribing. Broad areas for exploration included the 4 compressed sociotechnical dimensions. We asked questions about the following areas to elicit discussion about these dimensions: 1) motivation for using scribes, 2) the background and training of scribes, 3) the pros and cons of scribe use, 4) EHR use by scribes, and 5) the history and future of the scribe industry. All interviews were recorded and transcribed, and the investigators also took detailed field notes. Both the transcripts and the field notes were entered into the NVivo system (Burlington, MA) for qualitative data analysis.
Data analysis
Although we used the sociotechnical framework to guide our data gathering, we took a grounded hermeneutic (inductive) method for analyzing data44 to identify themes and suggestions for best practices. All authors took part in the data analysis process as part of our thorough triangulation efforts. In dyads, we coded several transcripts in a grounded fashion with no preconceived codes. Many codes related to questions we asked, but most were new concepts raised by subjects. The pairs met to compare and agree on lists of codes and develop a codebook; all contributed to analysis. We gathered data at each site until we reached saturation. Because of the amount of data gathered, our project manager used tightly controlled audit tracking, managing recordings and interview and field note documents and the analysis process using NVivo (Burlington, MA) and a secure archival mechanism.
Generation of best practices
During a member-checking process, when stakeholders within the organizations were debriefed about our findings both orally at the end of site visits and in written reports later, our research team developed a set of best practices. They are based on what we were told in interviews and debrief sessions and what we saw in the field.
RESULTS
Demographics
Between 2017 and 2019, we visited 12 clinics or emergency departments belonging to 5 organizations across the United States, with details about demographics shown in Table 1. We observed scribes working with providers for 80 person-hours and conducted 76 interviews with 81 individuals.
Table 1.
Sites, participants, and data gathered
| Site A | Site B | Site C | Site D | Site E | Total | |
|---|---|---|---|---|---|---|
|
Geographic location In US |
Northwest | Northwest | East | Midwest | Northwest | 5 sites |
| Characteristics of setting | Teaching Hospital and Clinics | Community Health System | ENT Clinic | Teaching Hospitals and EDs | Urgent Care and ENT Clinics | |
| Dates of Site Visits | Oct 2017-Jan 2018 | Jan-Feb 2018 | Aug 2018 | Oct 2018 | Dec 2018-Jan 2019 | Oct 2017-Jan2019 |
| EHR Used | Commercial (EPIC) | Commercial (EPIC) | Commercial (AllScripts) | Commercial (EPIC) | Commercial (EPIC) |
4 Commercial (EPIC) 1 Commercial (AllScripts) |
| Total Hours Interviewed | 12 | 7 | 11 | 12 | 5 | 47 hours |
| Total number of interviews | 13 interviews | 15 interviews | 18 interviews | 19 interviews | 11 interviews | 76 interviews |
| 14 people | 18 people | 18 people | 19 people | 12 people | 81 people | |
| 4 providers | 6 providers | 8 providers | 6 providers | 6 providers | 30 providers | |
| 4 scribes | 5 scribes | 6 scribes | 7 scribes | 5 scribes | 27 scribes | |
| 6 admin | 7 admin | 4 admin | 6 admin | 1 admi | 24 admin | |
| Number of clinics observed | 2 | 3 | 1 | 3 | 3 | 12 Clinics |
| Total number of people observed | 5 people: | 12 people: | 8 people: | 16 people: | 11 people: | 52 people: |
| 2 scribe/provider dyads | 6 scribe/provider dyads | 4 scribe/provider dyads | 8 scribe/provider dyads | 5 scribe/provider dyads | 25 scribe/provider dyads | |
| 1 provider (no scribe) | 1 provider (no scribe) | 2 providers (no scribes) | ||||
| Total number of hours observed | 17 hours | 20 hours | 6 hours | 25 hours | 12 hours | 80 hours |
Abbreviations: ED, emergency department; ENT, ear, nose, and throat.
Themes: insights on the use of medical scribes
Analysis of the data yielded 12 themes within our general 4-dimensional framework, depicted in Figure 1. The themes arose from the data in an inductive, hermeneutic fashion, but they naturally clustered into the 4 categories. Each theme is described below and illustrated with representative quotes from subjects.
The technical dimension
Theme 1. The EHR
Neither scribes nor providers had many complaints about the EHR. They sometimes speculated about how the systems could be improved, but they were accepting and positive about them. At times scribes were not included when notifications of changes were made, however, which caused some minor frustration.
Interviewees of all types believe that scribes are excellent users of the EHR. Scribes are generally considered EHR experts, sometimes playing formal roles as super users, offering help to others. For example, researcher field notes written during observation say “the provider asks the scribe ‘this is a right click, right?’” We were told that the EHR is so central to their workflow, and scribes use it so constantly, they quickly become adept with it. Scribes become skilled at mirroring the documentation style of individual providers, usually with the help of the EHR’s capability to build templates.
Best practices related to the EHR cited by participants included keeping scribes informed about EHR updates and changes and encouraging their use of templates.
Theme 2. Ergonomics
We observed scribe-provider teams working at nursing stations, in their own workrooms, and in exam rooms. Scribes generally carry laptop computers from place to place, though in some areas they use desktop computers while providers use laptops. Many exam rooms do not accommodate scribes well. We saw hampers, sinks, trash cans, and scribes’ knees used for placement of laptops. Because the scribe needs to see the patient, he or she must sometimes keep moving around the room. Scribes take up “contorted positions depending on the set up of the room and the flexibility of the scribe,” field notes report. We observed that laptops differ within hospitals and clinics, so some are older, have small screens, or batteries that do not last long enough. At times the scribes complained that there were “no outlets in the exam room for [a] laptop.” and “the laptop would lose power every 4 hours.”
Ergonomic best practices ideally include adequate space and up-to-date equipment for scribes. These are aspirational goals: None of the sites fully met them, but all were working towards them.
Environmental dimension
We include in this dimension 2 themes that are outside the scope of an organization’s scribe program but that influence such programs immensely.
Theme 3. Scribe industry
Scribe industry representatives describe the field as new, fast-growing, and likely to change. Presently, these companies recruit, train, and place primarily preprofessional college graduates for short term (1- to 2-year) positions. We were told it usually takes 6 months before most new scribes become competent at their jobs. Companies provide human resources services to help organizations cope with the rapid turnover. They usually depend on the presence of local colleges and universities to supply recruits, so geography plays a role. Recruits usually earn minimum wages. The companies are starting to provide distant scribes as well as those on site, both because recruits are not available in more rural areas and technology is improving. One provider told us: “having it done in real time, there’s no substitute for it. Dragon doesn’t do this. You have to tell Dragon what to put in, and then you still have to go back in and edit it. And you don’t have to tell a scribe everything that needs to go in there. They’re watching and listening and putting this information in there, and then it’s getting edited in a much more truncated time frame.” The human cognitive element is important, we were told. However, there are now technologies that allow human scribes to see as well as hear the encounter from a distance. Some of our interviewees felt that if EHRs improve enough, and artificial intelligence can be included, scribes will no longer be needed. One administrator said that “scribes are a transitional strategy and as EHRs get better, Dragon gets better, tools are more built out for providers, scribes will be less utilized.” One provider mentioned having a scribe in the exam room with a patient “can be a little intrusive” whereas “remote scribing is ideal.” However, most interviewees believed the need for scribes will not evaporate because the human cognitive and interpersonal element will continue to be in demand.
Best practices include further exploration by scribe companies, organizations, and researchers to identify the best designs for scribe models for the future.
Theme 4. Compliance and risk
The main compliance concern of managers is that the organization could be legally liable if a scribe works outside the acceptable role. Most preprofessional scribes would like do more than documentation, and most providers would like them to, so the potential for role expansion is evident. One scribe said the worst part about being a scribe was “not being able to do much. [Their] goal is to be a physician… and so as a scribe there’s no real medical care you’re doing. You’re just there observing and typing in the medical record and so it can be kind of a boring job sometimes.”
On the other hand, providers believe that scribes provide legal protection for them. A provider said that the scribe is “a witness, they provide an extra layer of protection and insurance for whatever accusations come your way.” Providers also perceive that simply having a second person in the exam room is safer for patients than working alone. One noted, “It’s nice to have 2 people hear something because I’ve, you know, there are times I say ‘did they say that they were taking that med?’ you know, and you can verify what both of you heard.”
When we asked about patient safety, our interviewees often wanted to discuss provider and scribe safety as well. Especially in the emergency department environment, there are at times unruly patients. Providers mentioned that they are sometimes concerned about scribe safety, but a scribe told us: “I don’t think I’ve ever felt unsafe. Sometimes you’ll have like patients making a ruckus and the security usually gets called and it’s not too big of a deal.” Some providers noted that the mere presence of scribes offers protection for them in the emergency department: Having a third person in the room makes patients behave better.
Best practices related to compliance include avoiding inappropriate role expansion and, for certain settings, having human rather than virtual scribes in the room.
The personal dimension
Theme 5. Pros and cons of scribing from different perspectives
Providers
Providers expressed a positive perspective: They were more efficient, avoided burnout, spent less time charting, and enjoyed mentoring future healthcare professionals. They valued having more time with patients. As 1 provider put it, “[having a scribe] allows me to have better patient interaction, it makes sense financially big time. And I think the quality goes up, so what’s not to like about it?” Numerous interviewees said that having scribes can extend the careers of older providers and “we don’t have enough providers,” so this incentive to continue working is important.
The chief downside was having to train new scribes when an experienced scribe left for graduate training. One provider mentioned a cognitive issue: He “finds that he sometimes can’t remember exactly what the patient had said” because he is depending on the scribe so much. Several thought that patients might not always feel comfortable with a scribe in the room.
We also heard expressions of “scribe envy” because some providers could have scribes and others could not, based on organizational priorities. Often it was the providers who most struggle with the EHR who were given scribes, which more adept providers considered unfair.
Scribes
Scribes told us the benefits of scribing include gaining experience and exposure to healthcare, improving one’s resume, being mentored, learning about medicine and the healthcare system from within, and having jobs they enjoy. However, there were negatives such as low pay, being the “low man on the totem pole,” sometimes working with a difficult provider, and being a contractor/outsider. Finding good provider–scribe matches and providing training for providers about how best to use scribes should be priorities for organizations, we were told. For example, introducing the scribe is important: When the provider does not, patients may wonder why a third person is in the room.
Managers
Managers told us they are seeking to create efficiencies so providers can see more patients and bill more accurately, while increasing provider satisfaction and preventing provider burnout. The ability to have a scribe can help with recruitment and, in addition, providers might be attracted to eventually go back to work for an organization where they had been scribes.
Theme 6. Training, knowledge, and synthesis
Typical training for becoming a preprofessional scribe with a scribe company includes about 40 hours of classroom training, online and/or in person. Prerequisites include typing ability and a minimum number of college courses. During the classroom sessions, scribes learn the basic structure of the note, professionalism, principles of coding, general EHR knowledge, terminology, body systems, HIPAA, and “being a fly on the wall.” Further instruction is given on site. The healthcare organization offers training on its EHR.
We were told that beyond basic knowledge, scribes also need to have the ability to synthesize what the provider is saying and understand the provider’s reasoning. For example, 1 scribe said: “I know where the physician is going with this and I can predict what will happen next.” A provider noted that “the scribe can just read my mind.”
Best practices include provision of classroom, on-site, and ongoing training for scribes. We asked all interviewees about scribe training, but many also emphasized that providers need training as well. Many of the safety concerns they outlined were because providers did not know how to communicate with or instruct their scribes, introduce them properly, and review their work. Some organizations provide some provider instruction, but this was felt to be insufficient and in need of updating and reinforcement over time.
Theme 7. Scribe/provider interaction
The relationship between scribe and provider should be mutually beneficial, with the scribe providing needed assistance and the provider giving mentorship. A provider needs to offer criticism and feedback to their scribe. As 1 scribe said, “I enjoy getting criticism and feedback. And so, I always try to make it a game to see like how little edits my providers have to make to my notes.”
However, there can exist negative aspects of this relationship as well. The provider and scribe may have different political views or clashing personalities. One provider said that the scribes are “all a little bit different in terms of ability, so if you have someone that is not as good that can be a challenge. Like grammar and language, which leads to more proof reading.”
The primary best practice for producing positive interactions is to assure that there is a good fit between a provider and any scribe being hired.
The organizational dimension
Theme 8. Workflow
As described earlier, the majority of scribes gather information, document the patient encounter and respond to requests for information from providers, and polish the documentation usually before the patient leaves. They may pend orders, do some coding, and complete patient instructions. The workflow is tied to the EHR and is described as very efficient by both providers and scribes. At the same time, it is tailored to the needs of the individual provider.
An important best practice is that the scribe is trained to adjust to the workflow of individual providers so that documentation can be most efficient.
Theme 9. Quality of documentation/coding
Scribes, providers, and managers feel that scribe documentation is more complete and accurate, especially if standard documentation templates are available. At all but 1 of our sites, providers were required to know how to use the EHR because, at times, they must work without scribes. When scribes are new, providers spend more time editing the notes. Often sections of the note are either dictated to the scribe or are typed or entered using voice recognition by the provider. Other sections of the note are completed by the scribe using templates. This way, the note has a mixture of free text and required field sections, so it is complete for billing and compliance and also useful for clinical purposes.
Scribe documentation is constantly monitored. Providers review the notes and orders, the scribe companies generally have an evaluation routine for scribe oversight, and billing staff in hospitals and clinics monitor quality. The quality of coding is also consistently high, we were told, with coders believing the scribes do an excellent job, better than that done by providers.
Best practices include standardization of documentation and consistent monitoring of the scribe’s work.
Theme 10. Scribe models
Each of our 5 sites used somewhat different models of scribing. Four use what we call the preprofessional model, though all had investigated clinical scribing and professional models as well. The preprofessional model depends on college students or recent graduates willing to accept minimum wages in return for healthcare-related experience that will help them get accepted into professional graduate programs. While they are highly capable and eager to learn, they do not stay long. A professional model includes scribes who are content to remain scribing, but this situation is rare. With the clinical model, medical assistants, nurses, or others with some healthcare training play the role of scribe, either instead of or in addition to the clinical duties. This model has the advantage of keeping scribes longer, but wages are higher, and it is sometimes difficult to keep tasks separated.
The virtual scribe model, which 1 of our sites used with audio only, has the advantage of not having to find space for a third person in the exam room, but there were also downsides in that the scribe could not see what was happening during the exam. Remote video capability is available through most scribe companies now and would be especially useful, we were told, for more remote areas where human scribes are not available.
Best practices include exploration of different models to find 1 that best fits the organization’s needs.
Theme 11. Variety/variability
Scribe programs encompass a broad variety of workflows, managerial arrangements, settings, and types of providers and scribes. Several managers referred to scribing as a “wild west” industry, with a general lack of standards, since certification and licensure are not needed. Some interviewees who had worked elsewhere as scribes described places where scribes were encouraged to go far beyond normal scribe duties. Provider-specific workflow, even within the same department, differs: Some providers like more free text while others have problem-specific templates. Some providers have scribes pend orders while others do not.
Best practices include standardizing documentation and scribe duties as much as possible while still respecting provider workflow differences. At the state and national levels, more guidance should be available, along with consideration of licensing standards.
Theme 12. Human resources aspects
The human resource burden associated with recruiting, training, placing, evaluating, and scheduling scribes, because of turnover, as noted above in Theme 3 about the industry, can be considerable. Human resources are usually provided by third-party contractors, the scribe companies. While most scribes are paid minimum wage, scribe companies must be compensated for the heavy human resources burden, so they must charge healthcare organizations accordingly. Consequently, scribes feel underpaid, scribe companies feel strapped, and clinics feel overcharged.
We noted another human resource issue in that, because scribes are employees of a third- party company, they may perceive themselves as outsiders, which places a strain on the team-based culture of today’s healthcare delivery. One of the scribe companies made a concerted effort to develop social events and communication mechanisms for its scribes. As 1 scribe at this site said, “scribes support one another, they help one another…I think we have a solid community here.”
Best practices include development of communication channels for scribes so they feel connected to 1 another and to the healthcare organization within which they work.
DISCUSSION
Our goals were to assess the effect of scribes on patient safety and to identify best practices for assuring safety. Our participants strongly believe that the use of scribes is not only as safe as, but even safer than nonuse of scribes from a documentation and EHR point of view. This study is the first to use a sociotechnical framework to investigate the technical, personal, environmental, and organizational landscape surrounding scribes.
There have been some skeptical discussions in the literature about the wisdom of using scribes,29–31 and a preliminary study we conducted indicated that scribes do make errors associated with EHR documentation.32 However, in this study, subjects in all roles told us that if best practices are followed, scribes make few errors, and careful oversight avoids patient harm. Our results concerning the personal dimension of the sociotechnical model are similar to those found by Yan et al, despite their studying clinical scribes while we focused on nonclinical preprofessional scribes.14
This study’s main limitation was that we were unable to verify our participants’ responses with data from EHR use, but triangulation of different qualitative methods helped to overcome this. We did not study patients directly, nor did we do research about virtual scribes in offsite locations, including internationally. We did not include providers who do not use scribes, nor did we focus on clinical scribes or international scribe use. These are areas ripe for further investigation.
Our recommendations for best practices related to the technical dimension include improved ergonomics and better equipment for EHR use to improve usability for these heavy, constant, users. For the environmental dimension, we urge further development of guidelines, certification, and licensing of scribes to assure their work is in scope. Regarding the personal dimension, training for providers as well as scribes would help maximize the benefits of hiring scribes. Finally, related to the organizational dimension, different models of scribing should be investigated, especially those adopting new technological advances. The best practices, like the themes, are overlapping. For example, human resource elements relate to the scribe industry, the organization’s perspective, and positive interpersonal interactions between scribes and providers. The sociotechnical framework allowed us to discover nuances of relations between and among dimensions.
More research is needed to identify national oversight needs and new roles. The Joint Commission, American Hospital Association, and CMS could issue further guidance. Otherwise, scribes will continue to be asked to go beyond the boundaries of accepted practice. While the role of nonclinical unlicensed scribes needs to continue to be narrow, there could be an expanded role for individuals, whether already clinically trained or not, licensed specifically as scribes, as vital parts of a new kind of healthcare team.
CONCLUSION
Using a qualitative approach, we identified 12 themes within 4 categories of the sociotechnical framework about EHR use by medical scribes. Our interviews and observations lead us to believe that the positive aspects of scribe use described by other researchers are valid and, in fact, that safety may be enhanced. There are, however, risks of adverse, unintended consequences if best practices are not followed. While there are hazards in that the industry is unregulated and therefore models of scribe use vary greatly, there also exist methods for assuring safety, which can be described, disseminated, and hopefully adopted over time.
FUNDING
This project is supported under contract #HHSA290200810010 from the Agency for Healthcare Research and Quality (AHRQ), US Department of Health and Human Services. The findings and conclusions in this document are those of the author(s), who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the US Department of Health and Human Services. Dr. Hoekstra is supported by US NIH National Library of Medicine Training Grant T15-LM007088.
Identifiable information on which this report, presentation, or other form of disclosure is based is protected by federal law, section 934(c) of the public health service act, 42 USC. 299c-3(c). No identifiable information about any individuals or entities supplying the information or described in it may be knowingly used except in accordance with their prior consent. Any confidential identifiable information in this report or presentation that is knowingly disclosed is disclosed solely for the purpose for which it was provided.
AUTHOR CONTRIBUTIONS
JA, VM, and JG developed the study design. All authors created the data gathering tools. JA, SC, NS, JB, RB, BO, and CH collected the data. All authors contributed to data analysis and interpretation. Finally, all authors assisted in writing the final draft, and all have approved its submission.
ACKNOWLEDGMENTS
We would like to thank Jeremy Liu, Renee Kostrba, Peter Lundeen, and Marcia Sparling for their help at each site, as well as administrators, providers, and scribes for their participation in this project. In addition, we thank Keaton Whittaker for his assistance with analysis.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc 2019; 94 (9): 1681–94. [DOI] [PubMed] [Google Scholar]
- 2. Kroth PJ, Morioka-Douglas N, Veres S, et al. The electronic elephant in the room: physicians and the electronic health record. JAMA Network Open 2018; 1 (1): 49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mishra P, Kiang JC, Grant RW.. Association of medical scribes in primary care with physician workflow and patient experience. JAMA Intern Med 2018; 178 (11): 1467–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Heckman J, Mukamal KJ, Christensen A, et al. Medical scribes, provider and patient experience, and patient throughput: a trial in an academic general internal medicine practice. J Gen Int Med 2019; 35 (3): 770–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bossen C, Chen Y, Pine KH.. The emergence of new data work occupations in healthcare: the case of medical scribes. Int J Med Inform 2019; 123: 76–83. [DOI] [PubMed] [Google Scholar]
- 6. Addesso LC, Nimmer M, Visotcky A, et al. Impact of medical scribes on provider efficiency in the pediatric emergency department. Acad Em Med 2019; 26 (2): 174–82. [DOI] [PubMed] [Google Scholar]
- 7. Bank AJ, Obetz C, Konrardy A, et al. Impact of scribes on patient interaction, productivity, and revenue in a cardiology clinic: a prospective study. Clinicoecon Outcomes Res 2013; 5: 399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bastani A, Shaqiri B, Palomba K, et al. An ED scribe program is able to improve throughput time and patient satisfaction. Am J Emerg Med 2014; 32 (5): 399–402. [DOI] [PubMed] [Google Scholar]
- 9. Earls ST, Savageau JA, Begley S, et al. Can scribes boost FPs' efficiency and job satisfaction? J Fam Pract 2017; 66 (4): 206–14. [PubMed] [Google Scholar]
- 10. Gidwani R, Nguyen C, Kofoed A, et al. Impact of scribes on physician satisfaction, patient satisfaction, and charting efficiency: a randomized controlled trial. Ann Fam Med 2017; 15 (5): 427–33. 1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Heaton HA, Castaneda-Guarderas A, Trotter ER, et al. Effect of scribes on patient throughput, revenue, and patient and provider satisfaction: a systematic review and meta-analysis. Am J Em Med 2016; 34 (10): 2018–28. [DOI] [PubMed] [Google Scholar]
- 12. Pearson E, Frakt A.. Medical scribes, productivity, and satisfaction. JAMA 2019; 321 (7): 635–6. [DOI] [PubMed] [Google Scholar]
- 13. Shuaib W, Hilmi J, Caballero J, et al. Impact of a scribe program on patient throughput, physician productivity, and patient satisfaction in a community-based emergency department. Health Informatics J 2019; 25 (1): 216–24. [DOI] [PubMed] [Google Scholar]
- 14. Yan C, Rose S, Rothberg M, et al. Patient perspectives on clinical scribes in primary care. J Gen Intern Med 2018; 33 (11): 1859–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zallman L, Finnegan K, Roll D, et al. Impact of medical scribes in primary care on productivity, face-to-face time, and patient comfort. J Am Board Fam Med 2018; 31 (4): 612–9. [DOI] [PubMed] [Google Scholar]
- 16. Koshy S, Feustel PJ, Hong M, et al. Scribes in an ambulatory urology practice: Patient and physician satisfaction. J Urol 2010; 184 (1): 258–62. [DOI] [PubMed] [Google Scholar]
- 17. Danak SU, Guetterman TC, Plegue MA, Holmstrom HL, et al. Influence of scribes on patient-physician communication in primary care encounters: mixed methods study. JMIR Med Inform 2019; 7 (3): e14797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. DeWitt D, Harrison LE.. The potential impact of scribes on medical school applicants and medical students with the new clinical documentation guidelines. J Gen Intern Med 2018; 33 (11): 2002–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gardner RL, Cooper E, Haskell J, et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc 2018; 26 (2): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gold JA. Take note: How medical scribes are trained- and used- varies widely. The Doctors Company 2017. www.thedoctors.com Accessed August 17, 2020. [Google Scholar]
- 21. Hafer J, Wu X, Lin S.. Impact of scribes on medical student education: a mixed-methods pilot study. Fam Med 2018; 50 (4): 283–6. [DOI] [PubMed] [Google Scholar]
- 22. Martel ML, Imdieke BH, Holm KM, et al. Developing a medical scribe program at an academic hospital: the Hennepin County Medical Center experience. Joint Comm J Qual Patient Saf 2018; 44 (5): 238–49. [DOI] [PubMed] [Google Scholar]
- 23. Nambudiri VE, Watson AJ, Buzney EA, et al. Medical scribes in an academic dermatology practice. JAMA Dermatol 2018; 154 (1): 101–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sattler A, Rydel T, Nguyen C, et al. One year of family physicians' observations on working with medical scribes. J Am Board Fam Med 2018; 31 (1): 49–56. [DOI] [PubMed] [Google Scholar]
- 25. Van Tiem JM, Stewart Steffensmeier KR, Wakefield BJ, et al. Taking note: a qualitative study of implementing a scribing practice in team-based primary care clinics. BMC Health Serv Res 2019; 19 (1): 574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Walker K, Ben-Meir M, Dunlop W, et al. Impact of scribes on emergency medicine doctors' productivity and patient throughput: multicentre randomised trial. BMJ 2019; 364: l121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Zhong CS, Mostaghimi A, Nambudiri VE.. Impact of medical scribes on dermatology trainee and attending experience. Dermatol Online J 2019; 25 (10): 2019. [PubMed] [Google Scholar]
- 28. Misra-Hebert AD, Yan C, Rothberg MB.. Physician, scribe, and patient perspectives on clinical scribes in primary care. J Gen Intern Med 2017; 32 (3): 244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bates DW, Landman AB.. Use of medical scribes to reduce documentation burden: are they where we need to go with clinical documentation? JAMA Intern Med 2018; 178 (11): 1472–3. 2018. [DOI] [PubMed] [Google Scholar]
- 30. Gellert GA, Ramirez R, Webster SL.. Medical scribes and electronic health records–reply. JAMA 2015; 314 (5): 519–20. [DOI] [PubMed] [Google Scholar]
- 31. Schiff GD, Zucker L.. Medical scribes: salvation for primary care or workaround for poor EMR usability? J Gen Intern Med 2016; 31 (9): 979–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pranaat R, Mohan V, O'Reilly M, et al. Use of simulation based on an electronic health records environment to evaluate the structure and accuracy of notes generated by medical scribes: proof-of-concept study. JMIR Med Inform 2017; 5 (3): e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.The Joint Commission, Use of unlicensed persons acting as scribes. https://www.jointcommission.org/standards/standard-faqs/ Accessed February 26, 2020
- 34. Forsythe DE. New bottles, old wine: Hidden cultural assumptions in a computerized explanation system for migraine sufferers. Med Anthrop Q 1996; 10 (4): 551–74. [DOI] [PubMed] [Google Scholar]
- 35. Sinsky CA, Bodenheimer T.. Powering-up primary care teams: Advanced team care with in-room support. Ann Fam Med 2019; 17 (4): 367–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sittig DF, Singh H.. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Heath Care 2010; 19 (Suppl 3): i68–i74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.SAFER guides. https://www.healthit.gov/topic/safety/safer-guides Accessed February 26, 2020
- 38. Misra-Hebert AD, Amah L, Rabovsky A, et al. Medical scribes: how do their notes stack up? J Fam Pract 2016; 65 (3): 155–9. [PubMed] [Google Scholar]
- 39. Woodcock DV, Pranaat R, McGrath K, et al. The evolving role of medical scribes: variation and implications for organizational effectiveness and safety. Stud Health Tech Inform 2017; 234: 382–8. [PubMed] [Google Scholar]
- 40. McMullen CK, Ash JS, Sittig DF, et al. Rapid assessment of clinical information systems in the healthcare setting: an efficient method for time-pressed evaluation. Methods Inf Med 2011; 50 (04): 299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ash JS, Chase D, Wiesen JF, Murphy EV, Marovich S.. Studying readiness for clinical decision support using the rapid assessment process and mixed methods interviews. AMIA Annu Symp Proc 2016; 2016: 285–94. [PMC free article] [PubMed] [Google Scholar]
- 42. Wright A, Ash JS, Erickson JL, et al. A qualitative study of the activities performed by people involved in clinical decision support: recommended practices for success. J Am Med Inform Assoc 2014; 21 (3): 464–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Beebe J. Rapid Assessment Process: An Introduction. Walnut Creek, CA: AltaMira Press; 2001. [Google Scholar]
- 44. Crabtree BF, Miller WL (eds.). Doing Qualitative Research. 2nd ed.Thousand Oaks, CA: SAGE; 1999. [Google Scholar]


