Abstract
Objective
To elicit novel ideas for informatics solutions to support individuals through the menopausal transition. (Note: We use “individuals experiencing menopause” and “experiences” rather than “symptoms” when possible to counter typical framing of menopause as a cisgender women’s medical problem.)
Methods
A participatory design study was conducted 2015–2017 in the Western US. Two sessions were held with individuals experiencing menopause recruited from the general public; and 3 sessions with healthcare practitioners (HCPs) including nurses, physicians, and complementary and integrative health (CIH) practitioners were held. Participants designed technologies addressing informational needs and burdensome experiences. HCPs reflected on designs from participants experiencing menopause. Directed content analysis was used to analyze transcripts.
Results
Eight individuals experiencing menopause (n = 4 each session) and 18 HCPs (n = 10 CIH, n = 3 nurses, n = 5 physicians) participated. All participants provided ideas for solution purpose, hardware, software, features and functions, and data types. Individuals experiencing menopause designed technologies to help understand and prevent burdensome menopause experiences. HCPs designed technologies for tracking and facilitating communication. Compared to nurses and physicians, CIH practitioners suggested designs reframing menopause as a positive experience and accounted for the complex lives of individuals experiencing menopause, including stigma; these ideas corresponded to comments made by participants experiencing menopause. Participants from both populations were concerned about data confidentiality and technology accessibility.
Conclusions
Participant generated design ideas included novel ideas and incorporated existing technologies. This study can inform the development of new technologies or repurposing of existing technologies to support individuals through the menopausal transition.
Keywords: gynecologic health, informatics, menopause, participatory design, user-centered design
INTRODUCTION
In the United States (US), about 6000 people reach menopause daily.1 This marks a 2–7-year journey2–4 for menstruating individuals who are cisgender women, non-binary, gender fluid, and other gender identities. Physiological changes impact daily life and health management,5–8 requiring individuals to relearn their changing bodies, adjust their behaviors to mitigate disruptive experiences, and manage new health risks. See Supplementary Table S1 for more information about the menopausal transition including biopsychosocial factors, common experiences, current treatments, and resources.
Information technologies have the potential to support individuals through this menopausal transition (MT).9 Considering that MT is dynamic, the current landscape of menopause related technologies is limited, dominated by apps for mobile devices (eg, Caria [https://joincaria.com]) and some wearables (eg, Grace Cooling,10 Embr Wave11) Apps mainly focus on tracking common menopause experiences, like hot flashes (eg, MenoPro).12 Less attention has been paid to facilitating behavioral strategies to support biopsychosocial and health risk changes, mitigating disruptive menopausal experiences, and addressing informational needs.
Currently, few articles exist on menopause informatics development and evaluation, with more work published in the human computer interaction (HCI) than biomedical literature. We were unable to identify any publications describing the evaluation of menopause technologies in the biomedical or HCI literature. Among the few publications available, studies have investigated the reliability of information provided on menopause websites,13,14 design requirements for menopause mHealth applications,15–17 and evidence-based development of menopause-related interventions.15 To investigate users’ menopause-related needs, researchers have analyzed posts to online communities or forums18 and conducted interviews,19 both individually and via focus groups,16,17 or held participatory design (PD) sessions.15,20 Studies only included women experiencing menopause; their perspectives have not explicitly compared with those of healthcare practitioners (HCPs), which could help design technologies supporting person–provider collaboration and addressing stigma faced by individuals experiencing menopause when seeking medical care.21,22
Menopause informatics can be considered part of the broader context of gynecologic health informatics that has primarily focused on menstruation tracking. However, it is unclear how well these apps support users’ needs, menstrual health, or health literacy. A 2016 review of 108 free menstrual tracking apps found only 20 were accurate in predicting average cycle lengths, ovulation prediction, and contained no misinformation.23 Also, an evaluation of popular menstrual tracking apps found that most did not support menstrual literacy well, assumed users wanted to track fertility, and were biased towards heteronormative and cisgender conceptualizations of menstruation.24 Comparatively fewer informatics solutions have been developed within the space of gynecologic disease. For example, endometriosis, which occurs when endometrial tissue is found outside the uterus,25,26 is a condition affecting at least 11% of women.27,28 Phendo, an app utilizing citizen science to help researchers better characterize the disease and provide social support for those with endometriosis,29 is 1 of a few apps systematically approaching the development and evaluation of the solution, engaging potential end users, and being built by scholars who conducted research to understand design requirements within this space.30 Overall, there is little rigorous informatics work within gynecologic health that could inform menopause informatics solution development.
Based on the current menopause and gynecologic health technology landscape, we need to revisit the MT informatics space to understand how technology can support the changing experiences and needs through MT. HCI researchers have called for technologies to support menopause holistically, celebrate it, and consider the individual body, interactions with others, and physical spaces in which individuals experience menopause.18,31,32 Therefore, the objective of this study was to elicit expansive ideas of technologies to support individuals experiencing menopause that provide developers with new ideas extending beyond mobile apps and tracking. While MT is traditionally framed within cisgender women’s health, there are people who do not identify as cisgender women and experience menopause.33,34 Therefore, in this article we use variants of “individuals experiencing menopause,” using “experiences” rather than “symptoms” because of stigma associated with menopause.21,22 Also, individuals do not necessarily use the term “symptoms” or have medical perspectives on MT, contrary to the medical model that pathologizes/medicalizes menopause.35–37 We acknowledge that clinicians commonly use “symptoms” which we consider within the broader concept of “experiences.”
MATERIALS AND METHODS
Study design, sample, timeframe, and setting
This PD study was conducted September 2015–June 2017 in urban centers across the Western US. PD is often used when designing informatics solutions with marginalized populations.38,39 We recruited 2 populations: individuals who have experienced menopause and HCPs. HCPs included nurses, physicians, and complementary and integrative health (CIH) practitioners, the latter from whom individuals experiencing menopause often seek integrative health solutions (eg, acupuncture) to address burdensome experiences.40–42
Sessions for individuals experiencing menopause took place in private rooms in a community center because it was an accessible, nonmedical space on a bus line, close to a major highway, and with ample free parking. HCP sessions were held in private rooms within buildings where the HCPs held regular staff meetings. The study was approved by the University of Washington Institutional Review Board.
Participant recruitment
Individuals who experienced menopause were recruited from the general population. We designed our recruitment strategy to reach potential participants regardless of access to or engagement with healthcare, socioeconomic status (SES), or access to the Internet or other technologies. Paper fliers were posted in publicly accessible locations (eg, libraries). Fliers were not explicitly inclusive of individuals of all genders, using the term “women.” HCPs were recruited through snowball sampling. Electronic invitations were sent to professional networks and HCPs known to our team.
Inclusion criteria for participants were: not having health problems that would interfere with taking part in the session (eg, glaucoma), ability to speak English, ability to travel to study locations, and ability to write. Individuals who experienced menopause needed to be 40–64 years old (span during which menopause and early post-menopause can occur).2,43–47 HCPs needed to have practiced supporting individuals experiencing menopause; they were not required to be female.
Study procedures
Two PD sessions lasting approximately 4.5 hours were held with individuals experiencing menopause. Three 0.5–2.5-hour PD sessions were held with HCPs. We held sessions separately by population to minimize potential perceived power imbalances or stigma22 and provide a safe space for individuals who experienced menopause to freely design technologies. The goal of the sessions was for participants to generate multiple ideas, not to generate a single unified technology.
Participants were given writing and crafting materials (eg crayons, colored paper, pipe-cleaners, stickers). For the individuals’ sessions, 3 facilitators guided participants through activities to generate design ideas for solutions they could use themselves. For HCP sessions, 1–3 facilitators guided HCPs in designing solutions used by individuals experiencing menopause. Artifacts generated included design ideas generated by participants working individually and in pairs. HCPs engaged in an additional activity to reflect on exemplar design artifacts generated by individuals who have experienced menopause. See Table 1 for PD session tasks.
Table 1. Tasks included in participatory design sessions with individuals and health care practitioners to elicit ideas of informatics solutions to support individuals experiencing menopause.
INDIVIDUALS EXPERIENCING MENOPAUSE
Introduction, Overview, & Icebreaker: Personal introductions. Participants introduce themselves, and researchers introduce themselves and the topic, as well as the plan for the day. Next, participants participate in an icebreaker exercise in which they discuss a fantasy solution to a problem to address a menopause-related issue they have experienced.
Brainstorming & Selection: Utilizing some motivating statements and questions, the participants generate ideas designed to address the need for tracking women’s health in everyday living. The goal is to first generate many, wide ranging ideas to these challenges. Participants spend the first 10 minutes working individually, generating ideas related to the positive and negative experiences they have had through menopause, and recording them on individual sticky notes. Afterwards, the session takes an “all-in” approach with each participant sharing their ideas with the group. After sharing all of the ideas and topics, the entire group led by the facilitators attempts to classify and organize the individual topics into higher category groupings (affinity diagramming) which are used in the next section of the focus group: prototyping.
Prototyping: Participants work on constructing prototypes. Participants are divided into groups of 3-4. Initially, participants in each group sketch 2-3 different concepts that incorporate the ideas and topics from the brainstorming session. Participants are encouraged to explore different designs for each of their sketches. As a team, participants then create low fidelity prototypes that address the original question: “How can a mobile tool help women track health in everyday living?” The goal is for each group to come up with a prototype created from a variety of office and art supplies. Researchers act as facilitators and visit each group periodically to help with the prototyping activity. At some point during this phase, the groups break for lunch.
Prototype Presentation & Discussion: The groups present their work to the other groups. Participants ask each other questions and offer constructive feedback.
Debriefing & thanks: The researchers summarize the day’s work and give thanks to the participants for engaging in the session.
HEALTHCARE PRACTITIONERS
Introduction: Personal introductions.
Brainstorming & Selection: Participants generate ideas that begin to address the question “How can a mobile tool help women track health in everyday living?” and are instructed not to discuss specific patients but instead think about the population of women experiencing menopause as a whole. The goal is to first generate many, wide ranging ideas to these challenges. Participants spend the first 5-10 minutes working individually, generating ideas, and recording them on individual sticky notes. Afterwards, the session takes an “all-in” approach with each participant sharing their ideas with the group. After sharing all of the ideas and topics, the entire group led by the facilitators attempts to classify and organize the individual topics into higher category groupings (affinity diagramming) which are used in the next section of the focus group: prototyping.
Prototyping: Initially, participants work individually again and sketch 2-3 different concepts that incorporate the ideas and topics from the brainstorming session. Participants are encouraged to explore different designs for each of their sketches (5-10 minutes). The participants are then divided into groups of 2-4. Participants share their ideas from sketching and then, as a team, create low fidelity prototypes that address the original question: “How can a mobile tool help women track health in everyday living?” The goal is for each group to come up with a prototype created from a variety of office and art supplies. Researchers act as facilitators and visit each group periodically to help with the prototyping activity.
Prototype Presentation & Discussion: The groups present their work to the other groups. Other participants ask questions and offer constructive feedback. After this discussion, the researchers describe the women’s designs and lead a discussion with the healthcare providers about their benefits and challenges, as well as their similarities and differences from the designs created by the providers. Researchers do not disclose women’s names or other identifying information to clinicians and may redact portions of the designs in order to preserve participants’ confidentiality. Healthcare providers offer additional feedback on the design of a women’s health tracking tool based on the discussion, again without discussing any specific patients.
Debriefing & thanks: The researchers summarize the day’s work and give thanks to the providers for engaging in the session.
At the end of the sessions, participants completed a demographic questionnaire. Individuals experiencing menopause selected their age and education level; they self-reported their gender and race/ethnicity, providing their own responses rather than choosing options from a predetermined list. Race and gender data were collected because they are indicators of systemic racism and sexism faced by people of color in healthcare.21,22,34,48–51 We included age and education, indicators of ageism and classism, respectively, because of how they intersect with racism and sexism to create distinct forms of discrimination in everyday life, work, and healthcare.49,52–59 HCPs selected their age and self-reported their gender; and job titles and years of practice supporting individuals experiencing menopause. Participants received a VISA gift card: US$50 for individuals who have experienced menopause and US$20 for HCPs. Free food and beverages were provided. A HIPAA-compliant service transcribed the audio recordings.
Analyses
Codebook development
Two researchers analyzed transcripts using directed content analysis.60 The initial codebook was based on session prompts for design specifications (Table 1). Initial codes included: purpose of the technology, hardware and software, technology features and functions, data elements, and concerns.
Initial coding
To identify additional codes and achieve coding consistency, 2 researchers completed 3 rounds of coding using randomly selected sections of PD session transcripts (1 transcript per round; 2 from sessions for individuals experiencing menopause and 1 from an HCP session). During each round of coding, each researcher independently coded the same section of text using the same codebook and added new codes when they identified new themes. The unit of analysis was a distinct idea or comment provided by study participants.
Next, the 2 researchers compared the coded text and which codes were applied. They discussed new codes and came to agreement on which new codes to integrate into the codebook. This process was repeated until no new codes were identified and interrater reliability of the 2 researchers’ coding was greater than 80%.61 Percent agreement between the 2 researchers on occurrence and nonoccurrence of coded text during the third round was 84.6%. The researchers came to consensus during the third round of coding for a final interrater agreement of 100%.
Final coding
Researchers independently coded the remaining transcripts using the finalized codebook, excluding HCP session text describing reactions to designs by individuals who experienced menopause. After all transcripts were coded, researchers reviewed the coded text within each participant population, developing broader themes in order to capture similarities and differences in design ideas between the 2 populations.
Researchers lastly coded text regarding HCP reactions to designs created by individuals experiencing menopause. The codebook for this text was based on information we sought from HCPs during the sessions (Table 1). Codes included similarities in designs and differences in designs.
Statistical analyses
Demographic data was analyzed using descriptive statistics including counts and percentages for categorical variables and means and standard deviations (SDs) for continuous variables.
RESULTS
Description of study participants
Eight people attended 2 sessions for individuals who have experienced menopause (Session A n = 4, Session B n = 4). They were heterogeneous regarding race/ethnicity and educational attainment (Table 2).
Table 2.
Demographic characteristics of individuals who have experienced menopause by participatory design session (n = 4,4)
| Characteristic |
Session A
(n = 4) |
Session B
(n = 4) |
|---|---|---|
|
Age, n (%) 45–49 50–54 55–59 |
1 (25) 2 (50) 1 (25) |
0 (0) 2 (50) 2 (50) |
| Gender, a n (%) | 4 “Female” (100%) | 4 “Female” (100%) |
| Race/ethnicity (alphabetical order) |
“Black” “Islander” “White” “White” |
“Asian, non-Hispanic” “Black” “multi-racial (Asian/Hispanic)” “South American (not the US)” |
|
Education, n (%) Did not finish high school Finished high school/GED Associate’s degree Bachelor’s degree Graduate or professional degree |
1 (25) 1 (25) 0 (0) 2 (50) 0 (0) |
0 (0) 0 (0) 1 (25) 2 (50) 1 (25) |
Gender and race/ethnicity were reported by participants via open-ended responses. Quotation marks indicate verbatim what the participants wrote on their surveys.
Participants in 3 HCP sessions (Session 1 n = 10, Session 2 n = 3, Session 3 n = 5) included registered nurses (RNs), advanced registered nurse practitioners (ARNPs), medical doctors (MDs), and CIM practitioners (Table 3).
Table 3.
Demographic characteristics for healthcare practitioners
| Characteristic |
Session 1
a
n = 10 |
Session 2
n = 3 |
Session 3
a
n = 5 |
|---|---|---|---|
|
Age, n (%) 30–39 40–49 50–59 60–69 70–79 |
0 (0) 2 (28.6) 4 (57.1) 1 (14.3) 0 (0) |
0 (0) 0 (0) 1 (33) 1 (33) 1 (33) |
3 (75) 0 (0) 1 (25) 0 (0) 0 (0) |
| Genderc, n (%) | 7 “F” or “female” (100) | 3 “F” or “female” (100) |
3 “F” or “female” (75) 1 “Male” (25) |
| Race/ethnicity b,c |
“African American” “Caucasian” “Caucasian” “caucasian” “White” “White” “White” |
“Caucasian” “Caucasian” “White, non-Hispanic” |
“Asian/Caucasian” “Caucasian” “White” “White” |
| Job title b,c |
“Clinic director and Academic Dean” “Counselor” “Licensed acupuncturist” “LMP” “Mental health counselor/owner” Naturopathic doctor and acupuncturist “Owner of business” Psychotherapist “Yoga professional instructor” |
“Clinical Professor” “Postdoc RN” “Student and clinician (NP)” |
“ARNP” “assoc. prof” “MD” “Physician” Internal medicine physician |
|
Years practicing supporting individuals experiencing menopause, Mean (SD) Range |
11.2 (5.9) 3–17 |
30.0 (17.6) 10–43 |
9.3 (12.0) 1.5–27 |
Abbreviations: ARNP, advanced registered nurse practitioner; LMP, licensed massage practitioner; MD, medical doctor; NP, nurse practitioner; RN, registered nurse; SD, standard deviation.
Three of the 10 participants in Session 1 and 1 of the 5 participants in Session 3 did not return a completed demographic form. Complete information was obtained only about their job title (not enclosed in quotes) except for 1 participant in session 1.
Listed in alphabetical order.
Gender, race/ethnicity, and job title were reported by participants via open-ended responses. Quotation marks indicate verbatim what the participants wrote on their surveys.
Table 4 provides a list of specific design solutions (initial codes) suggested by participants—they were within the context of the broad themes we identified and are provided below as section subheadings.
Table 4. Examples of designs suggested by participants
Purpose of technology
Track and monitor: experiences, moods, physiology, and behaviors
Understand: symptoms, relationships between different symptoms, relationships between symptoms and behaviors or moods, the impact of physiology on experiences
Access: informational and community support, lab results
Hardware
Wearable device
Sensor
Chip
Patch
Software
App or website for individuals experiencing menopause, healthcare practitioners (HCPs), or both
Visualization of data
Hologram
Dictation
Mode to support vision impaired individuals
Features and functionalities
Connectivity between devices
Access to medical records
Passive and active data collection
Communication between women and HCPs, women and other women
Compare their experiences with other women
Decision-support system to provide self-care suggestions based on collected data
Deliver an intervention to treat or prevent a burdensome experience
Can download and print data
Alerts that are generated by the technology or from HCPs
Alerts for those experiencing menopause and HCPs
Journaling ability
Learn about the user over time with increased data input
Data elements
Basic information about menopause
Information about self-care strategies
Perspectives of individuals experiencing the menopausal transition
Tracking experiences and identifying solutions
Some participants designed technologies to track behaviors, moods or feelings, and experiences (Table 4; purpose of technology). Because participants had a sense that experiences were related to each other in some way, they wanted ways to capture, analyze, and learn from data to identify potential relationships. Participant 3 (P3) in Session B stated, “So if you’re waking up in the middle of the night, and you’re only awake for 15 minutes, are you drippin’? What’s the sever[ity], is it from the hot flash? Or is it from something else?… How often are you waking up in the night? From what? What’s the result of waking up? Is it a hot flash? How long does it last? And then how long does it take for you to go back to sleep? And then, when you go back to sleep, is it an REM [rapid eye movement] sleep? What kind of sleep pattern is it?”
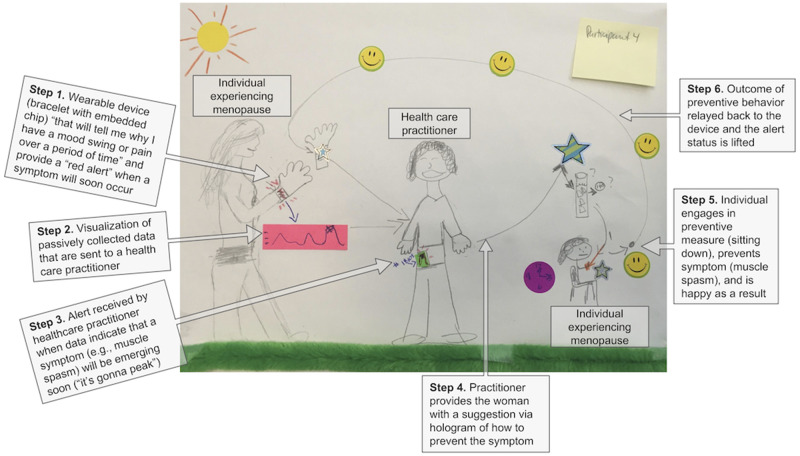
Participants wanted technologies to go beyond merely tracking data to using data to predict, prevent, and minimize burdensome menopause experiences (Table 4; features and functionalities). As P4 in Session B stated, “Well, there’s a problem, now what’s the solution?” One participant designed a system that used tracked data to alert the user of an upcoming burdensome experience, such as a hot flash or leg cramp (Figure 1). The device could then support the user, through automated suggestions, or communications from an HCP, on what to do to prevent or minimize that experience. P1 in Session A stated, “I’d like a little alarm thing that would go off… to signal that to me before I actually was feeling the symptoms, and so then I could take the preventative measure before I had to feel the impact of the hot flash or the cold flash.”
Figure 1.
Solution designed by an individual experiencing menopause (P4 from Session 1). Example solution ideas (and related design examples described in Table 4 in parentheses) are provided by steps. Step 1: Wearable with chip (hardware) enables passive data collection and alerts (features and functionalities) in order to track symptoms (purpose of technology). Step 2: The wearable provides visualizations of collected data (software) and facilitates communication with healthcare practitioner (HCP) (features and functionalities). Step 3: Alerts are sent to an HCP (features and functionalities). Step 4: Alerts are sent from the HCP to the user with a suggestion on how to manage a symptom (features and functionalities) to prevent the symptom (purpose of technology). Step 5 and Step 6: The symptom is prevented (purpose of technology).
Individuals in Sessions A and B noted the importance for technologies to minimize impact and burden of menopause experiences because of their busy lives. It was important for solutions to prevent, mitigate, or eliminate burdensome experiences (Table 4; features and functionalities). P1 in Session B designed a device to manage hot flashes that “lets you know: OK, some hot flash is coming up in the next 5 minutes… And then you prepare to receive it. Because, for me, it’s important to know when it’s coming because… before it comes, I [take action] to… minimize it or cool it down.”
Managing lived experiences
Participants wanted technologies to support their menopause experiences within their busy work schedules and responsibilities. P3 in Session B noted difficulties in managing care and work commitments while experiencing menopause: “I was taking care of my mother and she was dying, and so I needed to be on the HRT [hormone replacement therapy] in order to function and still keep a full-time job.”
Work, life, and sleep difficulties were mentioned by participants in both sessions. P3 in Session B recalled a particular experience with a colleague at work when, “all of a sudden… I had a hot flash and my back is dripping. And I’m turning… pink and the woman in the office is going: Do I need to call 9-1-1? ‘Cuz she thought I was having like a heart attack or something. And I said: Hold that thought… And I had to wait a minute, 2 minutes go by. And then I totally forgot what she said.” P2 in Session A also noted the disruptive nature of hot flashes: “I was kind of surprised that when I was younger and people complained about the hot flashes, I was just like: Big deal—you sweat a little. You’re hot. But it really does interfere with your life for those few minutes of your life, over and over again.”
The need for a technology to address the disruptive and potentially embarrassing aspects of MT were also raised by individuals whose concerns were not taken seriously by HCPs. P1 in Session A had an experience with a doctor during which she felt the doctor was dismissive of her experiences, leading her to minimize and put up with the experiences: “I was real cold like every day and things and I thought I was really sick but, you know, the doctor’s like: No, uh-uh [negative]… you’re gonna be, you know, fine … and they didn’t give me anything for it… even the negative experiences I’ve had, they just don’t really seem that bad. I guess I just accept it—it is part of life.”
To address difficulties of managing menopausal experiences without the support of HCPs, participants designed wearables with sensors in the form of watches, jewelry, headbands, and clothing to predict and prevent burdensome symptoms (Table 4; hardware, features, and functionalities). After a long group discussion about the burden of hot flashes, P1 in Session B suggested a sensor-embedded shirt that could sense temperature changes and adjust a person’s temperature: “[it automatically] adjusts the temperature immediately… a chip or something that it attach[es] to parts of the clothing… [that could] sense it [the hot flash] and then it automatically… adjusted the temperature of the clothing to cool you off immediately.”
Fostering independence and empowerment
Individuals experiencing menopause wanted informatics solutions that provide information about what to expect during MT, such as changing health risks, to help “understand the process and maybe give ‘em tools” (P4 Session B) (Table 4; purpose of technology and data elements). Participants also wanted information about behaviors like exercises, food intake, and regular exams to support their health and manage burdensome menopause experiences, such as sitting down to prevent a leg cramp (Figure 1). Participants also wanted information about ways to engage in self-care and nonpharmaceutical options (eg, herbs) to manage menopause experiences.
Other ideas included websites that provide information on MT, including common experiences, that was empowering (Table 4; purpose of technology and software). Individuals in Session B discussed the negative and disempowering presentation of menopause, leading 1 participant to suggest that an information website should be positive. This included reframing how experiences are described online. P3 stated, “Why are you connecting [negative expereinces of]… women’s change of life [during menopause], instead of celebrating her change of life?… I call them power surges when I have my hot flashes. It’s like: Oh, I’m having a power surge moment… I find it a better empowerment kind of thing if I call them power surges… I find that a better term than [hot flash].”
Perspectives of healthcare providers (HCPs)
There were similarities across HCP types in their designs of technologies to support individuals experiencing menopause. This included tracking menopause experiences and using tracking data to understand patterns which could then inform decision-making (Table 4; purpose of technology, features, and functionalities).
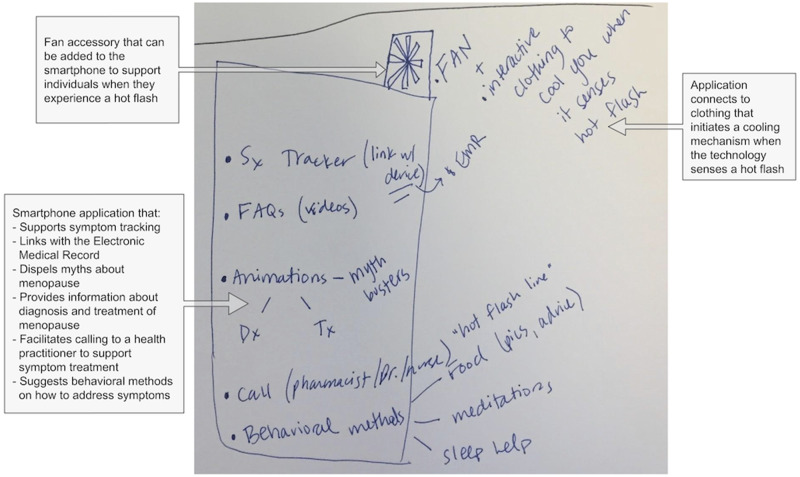
Tracking menopause experiences
HCPs designed technologies enabling individuals to track their MT experiences, including moods, feelings, behaviors, and physiology (Figure 2; Table 4; purpose of technology). HCPs designed technologies to decrease or eliminate burdensome menopausal experiences. In congruence with individuals experiencing menopause, HCPs designed technologies that provide information about menopause and self-care (Table 4; data elements). An HCP in Session 1 described a design that provided “positive encouragement to take absolute care of self. To make it rewarding through tracking devices and apps. So, like keeping track of, you know, what I’ve done right and well and then something that says: You deserve a break. Go do something fun.”
Figure 2.
Solution designed by 2 healthcare practitioners (HCP Session 3). Example solution ideas (and related design examples described in Table 4 in parentheses) included: A fan accessory for a smartphone (hardware), connects to clothing that can cool the wearer (hardware) symptom tracking (purpose of technology), provide information about menopause (data element), sends data to and connects users to healthcare practitioners (features and functionalities), and suggests behaviors in which users can engage (features and functionalities).
In contrast to individuals wanting a preventative solution, HCPs wanted to understand relationships between behaviors and menopausal experiences or between psychological and physiological experiences (Table 4; purpose of technology). For example, HCP1 in Session 2 stated that during diaphoresis (excessive sweating), “what is happening to her mood state? And if she could be measuring or indicating her mood and this device is measuring the physiology and putting the 2 together.” HCP3 in Session 2 designed a solution to track “mood and mood states and irritability and temper… to see, oh, I didn’t get much sleep the night before. Now, I’m really irritable.”
Understanding patterns and making adjustments
HCPs designed wearables for individuals experiencing menopause to support changes with aging in vision, mobility, and cognition, which individuals experiencing menopause did not include in their designs (Table 4; hardware and software). HCP designs also included websites about menopause, visualizations of menopause-related data and information (video or graphs), and ways to connect the technology to a computer and then download the information onto a computer with a more readable screen (Table 4; data elements, software, features, and functionalities). HCP1 in Session 2 described a desire for visualizations of data, stating “it would be fascinating to have a comparison across days… [to] see how well I’m doing.”
HCPs’ designs of solutions for individuals experiencing menopause had features and functionalities (Table 4) including passive data collection and artificial intelligence that learns about an individual over time based on what they actively reported. Other features and functionalities included ways to facilitate communication, provide direct intervention (eg, automatic cooling device), or deliver self-care advice (Figure 2). For example, HCP5 in Session 3 designed a “symptom tracker that can kind of learn over time… if you’re having more hot flashes like in the morning time, it would learn… [and] maybe remind you to go somewhere cool or do something that will cool you down. Also, something that will track interventions you’re trying. So, it might suggest… try walking this week. And so, you’ll track your walking and it’ll track the number of hot flashes… [and] you can track the different interventions over time and see what’s working.” HCPs in the session also designed solutions to facilitate collaboration with HCPs. For example, 2 physician participants in Session 3 independently designed solutions that shared tracked information with HCPs. Nurse participants in Session 2 had a discussion about having a solution that could “relay to a provider… who could respond” especially when the solution was able to indicate if the user was in crisis.
When designing solutions, HCPs described data elements integrated into technologies for individuals experiencing menopause (Figure 2; Table 4). In Session 1, HCPs designed technologies with information on “breathing techniques, meditation… bedtime and wake time health, food, supplements.” In contrast to the individuals’ designs of technologies that translated their tracked data into predictive and preventative solutions, HCPs’ designs focused more on understanding patterns of tracked data and delivering just-in-time information about menopause.
Design perspectives based on HCP type
There were differences across HCP types of designs for solutions to support individuals experiencing menopause. Nurses and physicians designed technologies for tracking experiences and behaviors as well as providing informational support (Table 4; purpose of technology). CHI medical professionals created similar solutions but included a more diverse set of design ideas that reframed menopause as a positive experience and time of empowerment. They also wanted solutions to accommodate the busy lives and multiple roles of individuals experiencing menopause. Acknowledging the stigma some face when seeing HCPs for menopause, CIM practitioners suggested a solution to help individuals find HCPs who provide positive and supportive MT care.
Concerns about menopause technologies
Participants from both populations discussed concerns about technologies, defined as issues brought up about the usability, accessibility, security, and privacy of technologies used to support MT. Individuals experiencing MT brought up several concerns about technologies to support them through MT, including confidentiality of data and information collected by the technology (P4 Session A) and accessibility for those with low SES or technology experience. P2 in Session B stated, “only those who can afford cell phones or computers or who are tech savvy could take advantage of it.”
HCPs expressed concerns about the credibility of online information integrated into a solution and accessibility of the solution. HCPs in Session 3 discussed wanting a web resource with validated information; HCP4 raised a concern about online communities or forums because “they can literally be so anecdotal… If it’s not moderated [by a professional], then it can become misinformation.” HCP1 in Session 2 wanted large format technology to accommodate accessibility issues for older individuals: “being cognizant of failing eyesight in aging women, starts in and around menopause when you start needing magnification and things like that.”
HCP reactions to designs created by individuals experiencing menopause
HCPs in all sessions reacted positively to designs created by individuals experiencing menopause. An HCP in Session 1 stated, “I love that they wanted to ‘nip it in the bud’…I think that idea of these electronic devices or with technology triangulate data points… [to] predict, it’s gonna happen.” HCPs from Sessions 2 and 3 noted that participants experiencing menopause included in their designs the technology’s ability to predict menopause experiences and learn about the individual over time.
HCPs noted differences comparing their designs to those by individuals who had experienced menopause. These included symptom tracking using wearable devices. HCP2 from Session 2 noted a difference in that individuals experiencing menopause do not always want HCP-mediated interventions: “…often we [HCPs] jump to intervention… it sounds like they don’t want a phone call every time they experience a hot flash. They don’t want a text message. They want it to be managed. So, that’s an ‘ah ha’ moment for me, that they want it to be automatic… They’re busy. They don’t need another thing to add into their day. But it’s something that’s automatic or that they can choose to pursue.”
DISCUSSION
In this PD study, we gathered novel ideas for technologies to support individuals experiencing MT. Participants designed a variety of technologies to address informational needs, burdensome menopause experiences (eg, hot flashes), and changing health needs. Individuals experiencing menopause focused on technologies to help understand, prevent, and positively reframe their menopause experiences; HCPs’ designs focused on tracking and patient–provider communication. Notably, several ideas from participants did not rely on engaging with an HCP to address burdensome menopause experience.
Based on our findings and the current landscape of informatics, we suggest broadening the scope of menopause technologies. Prior research on the needs, design, and use of menopause technologies has predominantly focused on self-tracking symptoms data via mobile applications or wearable devices with limited use of those tracked data for predictions or prevention of burdensome experiences (eg, 15–17). This limited scope and use is also present in technologies for other gynecologic phenomena, including menstruation23,24 and endometriosis,29,30 that could be used to inform the development of menopause solutions. However, self-tracking technologies risk trivializing nonmedical experiences and emphasizing menopause as a negative health condition.32 Our findings support the view of going beyond tracking to look at MT holistically.18,31,32 Individuals experiencing menopause in our study expressed a desire for technologies to provide interventions or guidance that could minimize burdensome experiences on their busy lives. This view is concordant with current efforts to develop a plethora of menopause solutions as exemplified by the current “Hacking Menopause” initiative from the American Association for Retired Persons (AARP); it calls for “managing the symptoms of menopause through AI, sensors, temperature management, and insight” (https://www.hackster.io/contests/aarpmenopause). Therefore, we suggest that the scope of menopause technologies go beyond merely tracking to use those tracked data to support prediction and prevention, and positively reframe the MT experience.
Prediction and prevention
Several designs from individuals experiencing menopause included the use of tracked data to predict the onset of burdensome menopause experiences (eg, hot flashes) that could prevent the disruptive nature of these experiences in day-to-day life by directly providing a technological intervention (eg, cooling mechanism) or directing the user to engage in a behavior (eg, find a cool place to sit). Predictive analytics has been used to identify age of menopause onset62,63 and timing of menstrual cycles during menopause.64 Most methods focus on collecting specific health data to tailor treatment options for a particular person.65–67 As the field of predictive analytics matures, researchers could expand its application to incorporate other data types and outcomes that matter to individuals experiencing menopause. For example, having the location of the individual (eg, at work) could allow a system to provide intelligent recommendations for nearby resources or self-management strategies when it predicts a burdensome experience. Combining predictive elements with recommendations could be akin to a decision support tool, meaning individuals have more control over their menopause experiences in the real world. Such decision support would extend beyond the existing decision-support tool that primarily supports patient–provider communication around hormone therapy.12 And more can be done to foster patient–provider connections. Individuals experiencing menopause and HCPs both designed solutions to support collaboration that helps decision-making for both parties.
With the growth of commercial wearable technologies that track and provide an intervention (eg, Embr Wave11) personal health informatics researchers should consider how wearables could extend beyond tracking to prevent burdensome menopause experiences. Designers can look to advances in other domains to creatively use data-driven prevention interventions. For example, 1 participant designed a shirt with embedded sensors, which is being developed by researchers funded by the United States Department of Energy’s Advanced Research Projects Agency.68 Another participant designed a patch that cooled the skin when a hot flash was predicted or detected, mirroring work done to embed cooling systems into wrist-worn tracking devices.11,12 These novel form factors can support further development of devices that collect data to predict onset of burdensome experiences and provide an intervention to minimize or prevent those experiences.
Positive reframing of online health resources
Individuals who experienced menopause discussed wanting thorough, detailed online resources to meet their informational needs. Participants discussed the need to change how online resources describe and characterize the experience of menopause. This need connects to the idea that well-designed solutions must support individuals’ self-expression and celebrate the menopause experience.31
Therefore, online information resources—whether for the purposes of education, social support, or otherwise—must ensure that language used does not reinforce negative stereotypes and enhance stigma surrounding menopause experiences. For example, following linguistic cues and patterns regarding how individuals describe their lived menopause experiences to others (eg, using metaphors)18 and ensuring an inclusive design that does not make assumptions about who experiences menopause24 can be used to reduce uncertainty and shed light on these experiences for perimenopausal individuals. Sensitivity to the language surrounding the lived menopause experience could also be an effective way for HCPs to discuss medical concerns and self-management strategies with individuals, during online and in-person encounters. Although HCPs in our study had concerns about the quality and accuracy of content within online spaces, prior research has demonstrated that these concerns are largely unfounded because the exchange of experiential information complements the medical information that HCPs provide.69–71 However, care must be taken to support health data literacy and identifying appropriate sources of medical information on menopause.72
Implications from lessons learned
Based on lessons learned from completing this participatory design study, we identified several considerations for future research to: (a) use participatory design in menopause informatics research; (b) share the ideas designed by individuals experiencing menopause to HCPs when conducting PD studies; and (c) design inclusive and equitable menopause technologies. See Table 5.
Table 5.
Implications from lessons learned while conducting our participatory design study to elicit expansive ideas of technologies to support individuals experiencing the menopausal transition
| Benefits of using participatory design (PD) in menopause informatics research |
PD allowed us to gain rich insights and design ideas that may not come from interviews or focus groups alone
|
| Insights gained from sharing individuals’ designs with HCPs |
Facilitated discussions on similarities and differences in designs
Allowed HCPs to empathize and gain and understanding of the needs of individuals experiencing menopause that they did not have before
Highlighted the importance of engaging individuals who have experienced menopause in the design process
|
| Importance of designing Inclusive and Equitable Menopause Technologies |
Participants in our study described concerns about menopause solutions including accessibility and appropriateness of the solutions
Developers can support equitable technology development through culturally-informed design 79
|
Limitations and future work
While our sample size was similar to other exploratory PD studies,85–89 it was relatively small. Our recruitment strategy was not explicitly inclusive of all genders (“woman” was used on fliers); this could have contributed to recruiting only women experiencing menopause. While we did not intentionally seek out female HCP participants, their gender composition was predominantly female. More work is needed to understand how HCP gender and technology, as well as numeracy, or graph literacy of participants impact design ideas. While we collected race, gender, and education data because of how racism, sexism, and education intersect to impact SES, we may have missed insights related to SES by not collecting other data like income. While we created sessions so each participant had turns to talk, their design ideas and willingness to express themselves might have been influenced by instances of domination vs suppression, which we did not capture. To support participants unable to express ideas in-person (or who live in dispersed geographic locations or cannot travel), future researchers could consider methods to engage participants remotely, such as sending materials to participants to complete design work, as has been done in menstrual tracking research.90
CONCLUSIONS
Our study elicited novel ideas for how technology supporting MT could track, predict, and prevent burdensome menopausal experiences. Future research can similarly apply PD methods to design technological solutions that meet the needs of the users within the broader context of their lived experiences.
FUNDING
This work was supported by the University of Washington School of Nursing, Research Intramural Funding Program. UB, ADM, and LTS were funded in part by the National Library of Medicine Biomedical and Health Informatics Training Program at the University of Washington (T15LM007442).
AUTHOR CONTRIBUTIONS
UB developed the project idea, codeveloped the methods, led the sessions, coanalyzed and interpreted data, and led writing of this manuscript. LTS facilitated a PD session, coanalyzed and interpreted data, and contributed to the manuscript. ADM codeveloped the methods, facilitated a session, and contributed to the manuscript. SHJ coanalyzed data and contributed to the manuscript. SH facilitated a PD session, interpreted findings, and contributed to the manuscript. NFW codeveloped the study idea and methods, facilitated a session, and contributed to the manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank those who participated in this study for their insights and time. We would also like to thank Judy Berg, Paula McNeil, Tyra Fainstad, and Jacob Berman for facilitating recruitment of participants. Thank you to Petra Backonja and Amanda Menking for their expertise in reviewing the article.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.American Congress of Obstetricians and Gynecologists (ACOG). Women’s Health: Stats & Facts 2011. https://www.acog.org/-/media/NewsRoom/MediaKit.pdf Accessed June 11, 2019
- 2. Gold EB, Crawford SL, Avis NE, et al. Factors related to age at natural menopause: longitudinal analyses from SWAN. Am J Epidemiol 2013; 178 (1): 70–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Harlow SD, Cain K, Crawford S, et al. Evaluation of four proposed bleeding criteria for the onset of late menopausal transition. J Clin Endocrinol Metab 2006; 91 (9): 3432–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Harlow SD, Mitchell ES, Crawford S, et al. The ReSTAGE Collaboration: defining optimal bleeding criteria for onset of early menopausal transition. Fertil Steril 2008; 89 (1): 129–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hardy C, Griffiths A, Hunter MS.. What do working menopausal women want? A qualitative investigation into women’s perspectives on employer and line manager support. Maturitas 2017; 101: 37–41. [DOI] [PubMed] [Google Scholar]
- 6. Hickey M, Riach K, Kachouie R, et al. No sweat: managing menopausal symptoms at work. J Psychosom Obstet Gynaecol 2017; 38 (3): 202–9. [DOI] [PubMed] [Google Scholar]
- 7. Hoga L, Rodolpho J, Goncalves B, et al. Women’s experience of menopause: a systematic review of qualitative evidence. JBI Database System Rev Implement Rep 2015; 13 (8): 250–337. [DOI] [PubMed] [Google Scholar]
- 8. Woods NF, Mitchell ES.. Symptoms during the perimenopause: prevalence, severity, trajectory, and significance in women’s lives. Am J Med 2005; 118 (Suppl 12): 14–24. [DOI] [PubMed] [Google Scholar]
- 9. Ismail R, Linder LA, MacPherson CF, et al. Feasibility of an iPad application for studying menopause-related symptom clusters and women’s heuristics. Inform Health Social Care 2015; 41 (3): 1–66. [DOI] [PubMed] [Google Scholar]
- 10.GRACE. n.d. https://www.gracecooling.com/ Accessed June 11, 2019
- 11.Embr. n.d. https://embrlabs.com Accessed May 19, 2020
- 12. Manson JE, Ames JM, Shapiro M, et al. Algorithm and mobile app for menopausal symptom management and hormonal/non-hormonal therapy decision making: a clinical decision-support tool from The North American Menopause Society. Menopause (New York, NY) 2015; 22 (3): 247–53. [DOI] [PubMed] [Google Scholar]
- 13. Aleksova J, Kuczynska-Burggraf M, Ranasinha S, et al. Information on early menopause: is the internet the place to search? Climacteric 2017; 20 (3): 248–55. [DOI] [PubMed] [Google Scholar]
- 14. Charbonneau DH. Readability of menopause web sites: a cross-sectional study. J Women Aging 2012; 24 (4): 280–91. [DOI] [PubMed] [Google Scholar]
- 15. Trujillo A, Buzzi MC. Towards a fuzzy rule-based systems approach for adaptive interventions in menopause self-care. In: proceedings of the 26th Conference on User Modeling, Adaptation and Personalization July 8-July 11, 2018; Singapore.
- 16. Lee M, Koo B-C, Jeong H-S, et al. Designing mHealth intervention for women in menopausal period. In: proceedings of the 9th International Conference on Pervasive Computing Technologies for Healthcare May 20-May 23, 2015; Istanbul, Turkey.
- 17. Lee M, Koo B-C, Jeong H-S, et al. Understanding women’s needs in menopause for development of mHealth. In: proceedings of the 2015 Workshop on Pervasive Wireless Healthcare 22 June, 2015; Hangzhou, China. ACM.
- 18. Lazar A, Su NM, Bardzell J, et al. Parting the Red Sea: sociotechnical systems and lived experiences of menopause. In: proceedings of the 2019 CHI Conference on Human Factors in Computing Systems May 4-May 9, 2019; Glasgow, Scotland.
- 19. Schapira MM, Gilligan MA, McAuliffe T, et al. Decision-making at menopause: a randomized controlled trial of a computer-based hormone therapy decision-aid. Patient Educ Couns 2007; 67 (1–2): 100–7. [DOI] [PubMed] [Google Scholar]
- 20. Senette C, Buzzi MC, Paratore MT, et al. Persuasive design of a mobile coaching app to encourage a healthy lifestyle during menopause. In: proceedings of the 17th International Conference on Mobile and Ubiquitous Multimedia; November 25-November 28, 2018; Cairo, Egypt. .
- 21. Doubova SV, Infante-Castaneda C, Martinez-Vega I, et al. Toward healthy aging through empowering self-care during the climacteric stage. Climacteric 2012; 15 (6): 563–72. [DOI] [PubMed] [Google Scholar]
- 22. Nosek M, Kennedy HP, Gudmundsdottir M.. Silence, stigma, and shame: a postmodern analysis of distress during menopause. Adv Nurs Sci 2010; 33 (3): E24–36. [DOI] [PubMed] [Google Scholar]
- 23. Moglia ML, Nguyen HV, Chyjek K, et al. Evaluation of smartphone menstrual cycle tracking applications using an adapted applications scoring system. Obstet Gynecol 2016; 127 (6): 1153–60. [DOI] [PubMed] [Google Scholar]
- 24. Eschler J, Menking A, Fox S, et al. Defining menstrual literacy with the aim of evaluating mobile menstrual tracking applications. Comput Inform Nurs 2019; 37 (12): 638–46. [DOI] [PubMed] [Google Scholar]
- 25. Burney RO, Giudice LC.. Pathogenesis and pathophysiology of endometriosis. Fertil Steril 2012; 98 (3): 511–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rogers PAW, D’Hooghe TM, Fazleabas A, et al. Defining future directions for endometriosis research: workshop report from the 2011 World Congress of Endometriosis In Montpellier, France. Reprod Sci 2013; 20 (5): 483–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Buck Louis GM, Hediger ML, Peterson CM, et al. Incidence of endometriosis by study population and diagnostic method: the ENDO study. Fertil Steril 2011; 96 (2): 360–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Olive DL, Schwartz LB.. Endometriosis. N Engl J Med 1993; 328 (24): 1759–69. [DOI] [PubMed] [Google Scholar]
- 29.Endometriosis Foundation of America. Phendo, an App to Track and Understand Endometriosis. https://www.endofound.org/phendo-an-app-to-track-and-understand-endometriosisAccessed May 19, 2020
- 30. McKillop M, Mamykina L, Elhadad N. Designing in the Dark: Eliciting Self-tracking Dimensions for Understanding Enigmatic Disease. In: proceedings of the 2018 CHI Conference on Human Factors in Computing Systems April 21-April 26; 2018; Montreal, Quebec, Canada.
- 31. Bardzell J, Bardzell S, Lazar A, et al. (Re-) Framing Menopause Experiences for HCI and Design. In: proceedings of the 2019 CHI Conference on Human Factors in Computing Systems; 2019; Glasgow, Scotland, United Kingdom.
- 32. Homewood S. Designing for the changing body: A feminist exploration of self-tracking technologies. In: proceedings of the 2018 CHI Conference on Human Factors in Computing Systems April 21-April 26 2018; Montreal, Quebec, Canada.
- 33. Carswell JM, Roberts SA.. Induction and maintenance of amenorrhea in transmasculine and nonbinary adolescents. Transgender Health 2017; 2 (1): 195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chrisler JC, Gorman JA, Manion J, et al. Queer periods: attitudes toward and experiences with menstruation in the masculine of centre and transgender community. Culture Health Sexuality 2016; 18 (11): 1238–50. [DOI] [PubMed] [Google Scholar]
- 35. Meyer VF. The medicalization of menopause: critique and consequences. Int J Health Serv 2001; 31 (4): 769–92. [DOI] [PubMed] [Google Scholar]
- 36. Olshansky E. Feeling normal. Women's experiences of menopause after infertility. Am J Matern Child Nurs 2005; 30 (3): 195–200. [DOI] [PubMed] [Google Scholar]
- 37. Woods NF, Mitchell ES.. Anticipating menopause: observations from the Seattle Midlife Women's Health Study. Menopause (New York, NY) 1999; 6 (2): 167–73. [PubMed] [Google Scholar]
- 38. Muller MJ. Participatory design: the third space in HCI. Hum Comput Interact 2003; 4235: 165–85. [Google Scholar]
- 39. Pilemalm S, Timpka T.. Third generation participatory design in health informatics—making user participation applicable to large-scale information system projects. J Biomed Inform 2008; 41 (2): 327–39. [DOI] [PubMed] [Google Scholar]
- 40. Armitage GD, Suter E, Verhoef MJ, et al. Women's needs for CAM information to manage menopausal symptoms. Climacteric 2007; 10 (3): 215–24. [DOI] [PubMed] [Google Scholar]
- 41. Peng W, Adams J, Sibbritt DW, et al. Critical review of complementary and alternative medicine use in menopause: focus on prevalence, motivation, decision-making, and communication. Menopause (New York, NY) 2014; 21 (5): 536–48. [DOI] [PubMed] [Google Scholar]
- 42. Posadzki P, Lee MS, Moon TW, et al. Prevalence of complementary and alternative medicine (CAM) use by menopausal women: a systematic review of surveys. Maturitas 2013; 75 (1): 34–43. [DOI] [PubMed] [Google Scholar]
- 43. Harlow SD, Gass M, Hall JE, et al. ; for the Straw +10 Collaborative Group. Executive summary of the stages of reproductive aging workshop +10: addressing the unfinished agenda of staging reproductive aging. Climacteric 2012; 15 (2): 105–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Makara-Studzińśka MT, Kryś-Noszczyk KM, Jakiel G.. Epidemiology of the symptoms of menopause—an intercontinental review. PM 2014; 3 (3): 203–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sievert LL, Murphy L, Morrison LA, et al. Age at menopause and determinants of hysterectomy and menopause in a multi-ethnic community: the Hilo Women's Health Study. Maturitas 2013; 76 (4): 334–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Thomas-Teinturier C, El Fayech C, Oberlin O, et al. Age at menopause and its influencing factors in a cohort of survivors of childhood cancer: earlier but rarely premature. Hum Reprod Update 2013; 28 (2): 488–95. [DOI] [PubMed] [Google Scholar]
- 47. Woods NF, Mitchell ES.. The Seattle Midlife Women’s Health Study: a longitudinal prospective study of women during the menopausal transition and early postmenopause. Womens Midlife Health 2016; 2 (1): 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.ACOG Committee. Opinion No. 649: racial and ethnic disparities in obstetrics and gynecology. Obstet Gynecol 2015; 126 (6): e130–4. [DOI] [PubMed] [Google Scholar]
- 49. Whitehead J, Shaver J, Stephenson R.. Outness, stigma, and primary health care utilization among rural LGBT populations. PLoS One 2016; 11 (1): e0146139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ng J, Scholle SH. Disparities in Quality of Care for Midlife Adults (Ages 45–64) Versus Older Adults (Ages >65). 2010; Washington, DC: U.S. Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. Accessed December 15, 2020 from https://aspe.hhs.gov/report/disparities-quality-care-midlife-adults-ages-45%E2%80%9364-versus-older-adults-ages-65.
- 51. Bellot E, Rouse N, Hunter MS.. Reclaim the Menopause: A pilot study of an evidence-based menopause course for symptom management and resilience building. Post Reprod Health 2018; 24 (2): 79–81. [DOI] [PubMed] [Google Scholar]
- 52. Roberts D, Jesudason S.. Movement intersectionality: the case of race, gender, disability, and genetic technologies. Du Bois Rev 2013; 10 (2): 313–28. [Google Scholar]
- 53. Crenshaw K. Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. U Chi Legal F 1989; article 8, 139. [Google Scholar]
- 54. Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians' recommendations for cardiac catheterization [published correction appears in N Engl J Med 1999 Apr 8; 340(14):1130]. N Engl J Med 1999; 340 (8): 618–26. [DOI] [PubMed] [Google Scholar]
- 55. Potter L, Zawadzki MJ, Eccleston CP, et al. The intersections of race, gender, age, and socioeconomic status: Implications for reporting discrimination and attributions to discrimination. Stigma Health 2019; 4 (3): 264–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kattari SK, Hasche L.. Differences across age groups in transgender and gender non-conforming people's experiences of health care discrimination, harassment, and victimization. J Aging Health 2016; 28 (2): 285–306. [DOI] [PubMed] [Google Scholar]
- 57. Samulowitz A, Gremyr I, Eriksson E, Hensing G. “ Brave men” and “emotional women”: a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Res Manag 2018; 2018: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Assari S. Life expectancy gain due to employment status depends on race, gender, education, and their intersections. J Racial Ethnic Health Disparities 2018; 5 (2): 375–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.US Bureau of Labor Statistics. Labor Force Statistics from the Current Population Survey, 2019. https://www.bls.gov/cps/cpsaat07.htm (Accessed December 15, 2020).
- 60. Hsieh HF, Shannon SE.. Three approaches to qualitative content analysis. Qual Health Res 2005; 15 (9): 1277–88. [DOI] [PubMed] [Google Scholar]
- 61. Topf M. Three estimates of interrater reliability for nominal data. Nurs Res 1986; 35 (4): 253–5. [DOI] [PubMed] [Google Scholar]
- 62. Depmann M, Broer SL, van der Schouw YT, et al. Can we predict age at natural menopause using ovarian reserve tests or mother's age at menopause? A systematic literature review. Menopause (New York, NY) 2016; 23 (2): 224–32. [DOI] [PubMed] [Google Scholar]
- 63. La Marca A, Sighinolfi G, Papaleo E, et al. Prediction of age at menopause from assessment of ovarian reserve may be improved by using body mass index and smoking status. PloS One 2013; 8 (3): e57005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Huang X, Elliott MR, Harlow SD.. Modeling menstrual cycle length and variability at the approach of menopause using hierarchical change point models. J R Stat Soc C 2014; 63 (3): 445–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Frey LJ, Bernstam EV, Denny JC.. Precision medicine informatics. J Am Med Inform Assoc 2016; 23 (4): 668–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.National Institutes of Health (NIH) All of Us Research Program. All of US Research Program Overview. https://allofus.nih.gov/about/about-all-us-research-program Accessed May 19, 2020
- 67. Burnham JP, Lu C, Yaeger LH, et al. Using wearable technology to predict health outcomes: a literature review. J Am Med Inform Assoc 2018; 25 (9): 1221–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Advanced Research Projects Agency [ARPA]. DELTA: Delivering Efficient Local Thermal Amenities. https://arpa-e.energy.gov/?q=arpa-e-programs/delta Accessed May 18, 2020
- 69. Huh J. Clinical Questions in Online Health Communities: The Case of “See your doctor” Threads. In: proceedings of the CSCW '15: Proceedings of the 18th ACM Conference on Computer Supported Cooperative Work & Social Computing March 14-March 18, 2015; Vancouver, Canada. [DOI] [PMC free article] [PubMed]
- 70. van Uden-Kraan CF, Drossaert CH, Taal E, et al. Coping with somatic illnesses in online support groups: do the feared disadvantages actually occur? Comput Human Behav 2008; 24 (2): 309–24. [Google Scholar]
- 71. Hartzler A, Pratt W.. Managing the personal side of health: how patient expertise differs from the expertise of clinicians. J Med Internet Res 2011; 13 (3): e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Institute of Medicine (US) Committee on Health Literacy. Health Literacy: A Prescription to End Confusion. Edited by Lynn Nielsen-Bohlman et. al., National Academies Press (US), 2004. doi:10.17226/10883. [PubMed] [Google Scholar]
- 73. Shorey S, Ng ED.. The experiences and needs of Asian women experiencing menopausal symptoms: a meta-synthesis. Menopause 2019; 26 (5): 557–69. [DOI] [PubMed] [Google Scholar]
- 74. Namazi M, Sadeghi R, Behboodi Moghadam Z.. Social determinants of health in menopause: an integrative review. Int J Womens Health 2019; 11: 637–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Chadha N, Chadha V, Ross S, et al. Experience of menopause in aboriginal women: a systematic review. Climacteric 2016; 19 (1): 17–26. [DOI] [PubMed] [Google Scholar]
- 76. Hardy C, Griffiths A, Thorne E, et al. Tackling the taboo: talking menopause-related problems at work. Int J Workplace Health Manag 2019; 12 (1): 28–38. [Google Scholar]
- 77. Parker K, Patten E. The Sandwich Generation: Rising Financial Burdens for Middle-Aged Americans. Pew Research Center. 2013. http://www.pewsocialtrends.org/2013/01/30/the-sandwich-generationAccessed May 18, 2020
- 78.United States Department of Labor. Women in the Labor Force. https://www.dol.gov/wb/stats/stats_data.htmAccessed May 18, 2020
- 79. Valdez RS, Brennan PF.. Embracing complexity: Rethinking culturally informed design in human factors/ergonomics and consumer health informatics. Int J Hum Comput Interact 2017; 33 (4): 322–32. [Google Scholar]
- 80. Veinot TC, Mitchell H, Ancker JS.. Good intentions are not enough: how informatics interventions can worsen inequality. J Am Med Inform Assoc 2018; 25 (8): 1080–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Arcia A, Suero-Tejeda N, Bales ME, et al. Sometimes more is more: iterative participatory design of infographics for engagement of community members with varying levels of health literacy. J Am Med Inform Assoc 2016; 23 (1): 174–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Lucero RJ, Sheehan B, Yen PY, et al. Developing Self-Management Tools with Vulnerable Populations for use in Personal Health Information Management Systems. In: proceedings of the11th International Congress on Nursing Informatics; June 23–27, 2012; Montreal, Canada. [PMC free article] [PubMed]
- 83. Unertl KM, Schaefbauer CL, Campbell TR, et al. Integrating community-based participatory research and informatics approaches to improve the engagement and health of underserved populations. J Am Med Inform Assoc 2016; 23 (1): 60–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Huh J, Koola J, Contreras A, et al. Consumer health informatics adoption among underserved populations: thinking beyond the digital divide. Yearb Med Inform 2018; 27 (01): 146–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Davidson JL, Jenson C. Participatory design with older adults: an analysis of creativity in the design of mobile healthcare applications. In: proceedings of the 9th ACM Conference on Creativity & Cognition. June 17- July 20, 2013. Sydney, Australia.https://dl.acm.org/doi/10.1145/2466627.2466652.
- 86. Gordon M, Henderson R, Holmes JH, Wolters MK, Bennett IM; the SPIRIT (Stress in Pregnancy: Improving Results with Interactive Technology) Group. Participatory design of ehealth solutions for women from vulnerable populations with perinatal depression. J Am Med Inform Assoc 2016; 23 (1): 105–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Jeffery AD, Novak LL, Kennedy B, Dietrich MS, Mion LC.. Participatory design of probability-based decision support tools for in-hospital nurses. J Am Med Inform Assoc 2017; 24 (6): 1102–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Miller AD, Pollack AH, Pratt W.. Bursting the information bubble: identifying opportunities for pediatric patient-centered technology. AMIA Annu Symp Proc 2016; 2016: 894–903. [PMC free article] [PubMed] [Google Scholar]
- 89. Ruland CM, Starren J, Vatne TM.. Participatory design with children in the development of a support system for patient-centered care in pediatric oncology. J Biomed Inform 2008; 41 (4): 624–35. [DOI] [PubMed] [Google Scholar]
- 90. Fox S, Menking A, Eschler J, Backonja U. Modules Over Models: Participatory Explorations of the Menstrual Tracking Application. ACM Transactions on Computer-Human Interaction (ToCHI). 2020; 27(4): article 22 (24 pages). 10.1145/3397178. [DOI]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.