Abstract
Objective
Diabetes self-management (DSM) education, social support, and information technology interventions can improve patient engagement and health. A major challenge is animating, integrating, and accessing resources in under-resourced, rural communities. Set in an island community in Hawai‘i, this study piloted a program that integrated friend-and-family support, community health services, telehealth-enabled DSM education, and mobile technologies by activating the community’s social capital to support the program.
Materials and Methods
An action research approach informed the design and implementation of a community-based DSM program that included: friends and family support, telehealth classes, personalized consultations, Bluetooth-enabled blood glucose monitors, and text messaging support. Outcomes were evaluated using biometric data, surveys, interviews, and participant observations.
Results
The study spanned 9 months with 7 dyads, each with 1 individual with type 2 diabetes and a friend or family member. Six of the 7 participants with diabetes experienced reduced hemoglobin A1c percentages, with 3 reducing by more than 1%. The seventh participant maintained a hemoglobin A1c level within American Diabetes Association recommended ranges. DSM knowledge and self-care behaviors improved overall. Interviews and participant observations highlighted program strengths and social challenges associated with the interpersonal relationships between the members of the dyads.
Conclusions
A community-centric diabetes program can enhance understanding of diabetes etiology, DSM activities, and communication skills for effective disease management support in under-resourced rural communities. Social capital among community members, leveraged with health information technology, can catalyze and integrate limited health system resources for DSM and social support as a cost-effective strategy to develop community-centric chronic healthcare management initiatives.
Keywords: diabetes self-management, social support, telehealth, health information technology intervention, action research
INTRODUCTION
Diabetes self-management (DSM) involves understanding, monitoring, and balancing interrelated effects such as blood glucose (BG) levels, nutrition, exercise, and medication. Support resources include education from healthcare providers with knowledge of the etiology and treatment of diabetes, family and friends (F&F) who can encourage and assist the person with diabetes (the patient), and information technologies (ITs) that assist in self-monitoring, on-going support, and education. These resources are limited in rural and low socioeconomic status communities,1–3 which tend to have high incidences of diabetes.4 This study looked beyond what such communities lack to consider whether social capital, which often characterizes these communities, might catalyze and integrate limited health system and health IT resources (HITs) to better support DSM behaviors and improve health outcomes.
DSM education and health IT
Education on the etiology of diabetes is essential for understanding why DSM activities are helpful and also contributes to patient self-efficacy and the belief that diabetes can be managed.5–7 DSM education programs can help patients improve clinical outcomes and behaviors.5,6 However, sustaining patient engagement and reducing dropout rates due to cost, inconvenience, and dwindling interest are persistent barriers to effective deployment.1–3 Moreover, access to specialized healthcare services that can improve patient understanding is limited in rural or remote communities.2,4 Previous research supports the use of telehealth for medically underserved patients to address these issues.6 Through video teleconferencing, patients and families can gain access to certified diabetes educators, dieticians, endocrinologists, and psychologists who may not be available in their communities. In these ways, telehealth technologies can be key resources to improve chronic care management,8,9 reduce healthcare spending, and improve clinical outcomes.9
Health organizations, such as the U.S. Health and Medicine Division and the Agency for Healthcare Research and Quality, recommend the use of HITs to support self-management of chronic conditions.10 The American Diabetes Association’s recommendations for self-care include medication adherence, foot care, and BG monitoring. Bluetooth-enabled BG monitors (glucometers) enable patients to check blood levels and transmit results to an online database accessible by patients and supporting stakeholders. Automatic data transfer from glucometers to clinical databases are easier to use and more accurate than traditional paper logging and self-reports based on recall.11 Such remote monitoring can enable more efficient support, such as reminders to take BG readings or to check in with patients with high or low BG reports.12
Text messaging is another channel for communicating with patients between visits by allowing for more frequent and targeted communication. Text messaging systems have been associated with increased self-efficacy in DSM,13–15 improved clinical measures,15,16 significantly reduced hemoglobin A1c (A1c) levels,6,12,17–20 and improvements in self-health behaviors such as increasing medication adherence and foot care.6,13,18 Text messaging interventions may also increase self-awareness and control of diabetes, reinforce feelings of success for staying on track with DSM activities, enhance awareness and acceptance of the seriousness of diabetes, and foster a feeling that someone cares.7,13,21
F&F support
Because F&F play critical social-support roles, scholars have argued that diabetes should be considered a family, rather than an individual, disease.22 F&F participate in patient routines and may assist with medication adherence, BG monitoring, and meal planning.22–28 Diabetes is a generational disease, and someone who observes family member complications may incorrectly believe that amputations, blindness, and renal failure are unavoidable outcomes.29 With proper education and training, F&F can contribute to improvements in patient self-efficacy, perceived social support, diabetes knowledge, and self-care activities.23,28,30 Integrating F&F into DSM education has been associated with reductions of A1c and improvements in DSM activities.31–34 However, it is not yet fully understood how to involve F&F in opportunities for engagement via HIT, particularly in the specific roles, activities, quality and extent of support, and interaction styles, which may contribute to positive outcomes.20,23,27,28,31
Social capital
Though under-resourced and rural communities have limited access to DSM-enhancing services and resources that can improve health outcomes, they may have high levels of social capital.35,36 Lin37 defined social capital in terms of “resources embedded in a social structure which are accessed and/or mobilized in purposive actions” and highlighted the community structures of the embedded resources, the opportunities for access through individuals’ purposive actions, and the action-oriented mobilization by individuals.37 Social capital includes a sense of community, formal and informal relationships, trust, and reciprocity.38–41 It influences the information flow and community members’ social credentials and reinforces relationships through common value perspectives and social support.37,40,41
The World Health Organization identifies social capital as a key element for creating health equity and well-being of individuals and communities, while studies suggest social capital can be an important factor in improved health outcomes.42 Of note, a culturally adapted family-model DSM education intervention in a Marshallese community resulted in significant reductions in A1c levels up to 1 year after the study.43 The family approach in may have been effective because of the collectivist nature of the Marshallese culture.44 However, research is needed to assess in what circumstances and in what ways social capital in under-resourced, rural communities might mobilize limited resources to promote DSM.
MATERIALS AND METHODS
Although research findings on HIT interventions for DSM support are promising, access to formal DSM education and support resources remains low in rural and underserved communities, while gaining and sustaining patient engagement with interventions can be problematic.1–3,6 Focusing on these challenges, this study developed a community-centric DSM approach utilizing F&F support, telehealth, remote glucose monitoring, and text messaging that drew on social capital to activate and integrate DSM resources and evaluated the approach in a pilot program in an under-resourced rural community.
Research setting
The Moloka‘i ‘Ohana Diabetes Program (MOD-P) was conducted on the island of Moloka‘i in the state of Hawai‘i. Moloka‘i has a population of approximately 7,400, with 21% of families falling below the poverty line, compared with 11% statewide.45,46 Moloka‘i also has a high prevalence of residents with diabetes (17.5% of its population, compared with 10.9% in the state and 10.5% nationwide), and adults suffer disproportionately from other chronic conditions, such as kidney disease, cancers, asthma, obesity, and heart disease.47 Health services on the island are limited due to population size and the remote location. Many patients must fly to Honolulu for specialty health care. A community strength is the shared sense of ohana (family) among residents, who support one another as an extended family: “[Social] capital is rooted in traditional Hawaiian values, which stress cooperation and unity (lōkahi), a family sense of belonging (‘ohana), and love and care for the land (malama ‘aina, aloha ‘aina).”48
Research design and methodology
The research aimed to assess how community members’ social capital resources might activate and integrate scarce health service resources to better support community members’ DSM practices. Research questions included (1) Did the MOD-P impact participants’ understanding of diabetes, patient self-management activities, and health outcomes? (2) In what ways did MOD-P influence participants’ access to and engagement with DSM support resources? and (3) In what ways did social capital in the community influence observed outcomes of the MOD-P?
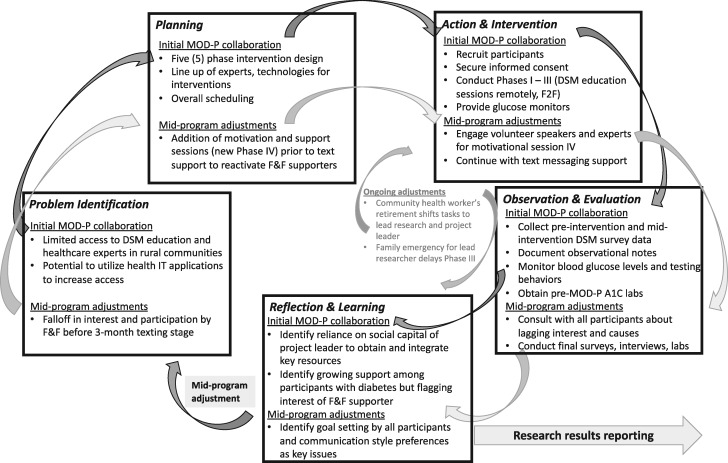
Action research (AR) methodologies are appropriate when research goals include acting to improve a problematic situation and generating general knowledge.49,50 Our research interest in how social capital resources in the community might mobilize DSM resources required stakeholder participation and learning, which are hallmarks of AR.50–52 Thus, this study utilized an AR methodology49–55 to design the MOD-P, guided by social capital theory37 and empirical research on DSM interventions, to develop action plans along with key stakeholders in the community, to implement and monitor the program over 9 months, and to evaluate outcomes to generate new knowledge and insights.49,56 See Supplementary Appendix SA for an extended discussion of AR in this project. Figure 1 depicts the MOD-P’s AR cycles. Table 1 outlines each step of the MOD-P.
Figure 1.
Action research cycles in the Moloka‘i ‘Ohana Diabetes Program (MOD-P). A1c: hemoglobin A1c; DSM: diabetes self-management; F&F: family and friends; IT: information technology.
Table 1.
MOD-P design
| Program phase | Actions and interventions | Data collected |
|---|---|---|
| Phase I: Recruitment and orientation | Recruit participants |
Baseline health surveya A1c levelb |
| Orientation |
Baseline support surveyc Baseline diabetes knowledged |
|
| Phase II: Telehealth classes—DSM education (funded through participant health insurance) | Telehealth class #1: DSM education | Video teleconference evaluatione |
| Telehealth class #2: DSM education | Participant observation of sessions | |
| Telehealth class #3: DSM education |
Telehealth class evaluatione Participant observation of sessions Second diabetes knowledge checkd |
|
| Phase III: Consultation with health care providers—goal setting (funded through participant health insurance) | In-person diabetes educator consultations (goal setting) | DSM general goalsf |
| Online telehealth consultations: dietician/nutritionist | DSM nutrition goalsf | |
| Phase IV: Telehealth session—motivation and support (modified and refocused in second AR cycle) |
Telehealth session #4: Patient-to-patient talk story and motivational interview training Technology overview: BG monitors |
Participants’ reflections about session Participation observation by researchers |
|
Telehealth session #5: Chronic kidney disease/motivational patient-to-patient talk story |
Patient and F&F life goals DSM support evaluationc Third diabetes knowledge checkg |
|
| Phase V: Text message support over 3 mo | Text message support 2× week: (1) check-in, (2) informational |
Qualitative data from text messages; BG levelsh and frequency of blood testsh Participant observation by researcher |
| Phase VI: Participant reflection and learning | Final interviews and surveys |
Post health surveya A1c levelb Post support surveyc Fourth diabetes knowledge checkg Qualitative data from interviews |
A1c: hemoglobin A1c; BG: blood glucose; CHW: community health worker; DSM: diabetes self-management; F&F: family and friends; MOD-P: Moloka‘i ‘Ohana Diabetes Program; PHQ-9: Patient Health Questionnaire; SKILLD: Spoken Knowledge in Low Literacy in Diabetes; SME: subject matter expert.
Lab results provided by participant.
Diabetes Social Support Questionnaire.59
SKILLD Knowledge Assessment Scale.60
Researcher-provided feedback surveys.
Patient logs from diabetes management system database.
Modified SKILLD Knowledge Assessment Scale.
Readings from BG monitor’s diabetes management system and database.
Problem identification and planning (MOD-P phase I)
The MOD-P design resulted from discussions among a long-term healthcare provider in the community (who became the program manager), researchers from one of the state’s universities, and expert health services providers (diabetes educator, pharmacist, primary care physician, nephrologist). The University’s Office of Research Compliance Human Studies Program authorized study protocols and qualified it for expedited review under CRF 46.110 and 21 CRF 56.110, Category 5, 6, 7a, and 7b. Study participants (dyads of persons with type 2 diabetes plus 1 F&F supporter) and health services experts contributed to refinements and adjustments in the program. The 6 phases were identified in the initial MOD-P collaboration cycle. Following evaluation and reflection of phase III, phase IV was redesigned and refocused to address emerging issues with F&F participation and support.
Actions and interventions (MOD-P phases II-V)
The first 6 months of the project focused on scheduling and telehealth sessions and the last 3 months focused on text messaging and support. DSM education and support sessions were given by subject matter experts (SMEs) located in Honolulu and delivered via video teleconference. SMEs included a diabetes educator and pharmacist, a dietitian/nutritionist, a nephrologist, a psychologist, and a peer lecturer. Three DSM classes were held in phase II. Phase III included 2 individual consultations, one in-person with the patient, F&F, and the diabetes educator; and one through video teleconference with the patient, F&F, and a dietician/nutritionist. The purpose was to tailor general information from group classes to individual patients. In phase IV, participants were given Bluetooth-enabled glucometers with access to the system’s database and training on use. A mid-program adjustment cycle added teleconferencing classes focused on general life goals and motivational interview techniques to assist F&F in developing effective support skills and patients’ and community members’ testimonies about their challenges and successes with managing diabetes and chronic kidney disease as it relates to uncontrolled diabetes. Phase V included a 3-month period of text message support in which participants received 2 texts per week: one checking in and one with health-related information.
Observations, evaluation, and reflection (MOD-P phases II-VI)
We collected data and evaluated progress throughout phases I-V. The focus in phase VI was to gather post–MOD-P observational data and participants’ reflections. Patients provided A1c lab results at the start and completion of the program (9 months’ duration). We received the BG levels, frequency, date, and time of patients’ blood tests from the glucometer’s Diabetes Management Web-Based System, which provided summary reports that calculated averages and a comparison of results to patients’ stated goals. We used standard American Diabetes Association measures and scales to collect DSM outcome data. Patients were given pre- and postprogram health surveys. Dyads were given diabetes knowledge assessment and diabetic support surveys pre- and postinterventions (at 4 time periods). All participants completed questionnaires asking for feedback about the program, telehealth technology, and telehealth sessions.
To understand participants’ experiences with the MOD-P and to assess the influence of social capital in integrating resources through this program, we collected qualitative data from audio-recorded interviews with participants (patients, F&F, program manager), open-ended survey questions, the lead researcher’s participant observations, and field notes from group meetings, telehealth sessions, and informal interactions with participants, text messages, emails, and other field notes. The qualitative data were analyzed using applied thematic analysis methods, with categories derived from the research questions, social capital theory concepts, and emerging themes related to F&F support dynamics.61,62Table 2 provides a summary of key themes and categories. See Supplementary Appendix SB for an extended discussion of data analysis methods.
Table 2.
Examples of analytic coding categories
| Analytic theme/category | Examples from MOD-P data |
|---|---|
|
Theme: Integrating formal and informal health services within the community Ways in which resources were integrated to facilitate access and support DSM, as well as issues or limitations encountered. Formal structural resources: Pre-existing in the healthcare system to support DSM programs; may not be activated, utilized, or readily accessed. Informal community resources: Became available to support DSM programs through participants’ actions. |
|
|
Theme: Integrating HIT resources with DSM services and support Ways in which IT facilitated integrating support resources or maximizing effects of resources. Designed/intended HIT use: Intended/observed ways that participants utilized project-supplied HIT (ie, telehealth sessions, Bluetooth glucometers, DSM website, mobile phone texting). Issues/limits with HIT use: Unexpected or unintended ways in which HIT was used/not used. |
|
|
Theme: Integrating F&F support Intended/observed ways that F&F provided engage in DSM and support partner with diabetes. Dynamics of F&F support: Unexpected or unintended outcomes of engaging F&F as DSM supporter. |
|
|
Theme: Integrating social capital and F&F support resources Ways in which social capital facilitated engagement, activation, integration, and leveraging of other resources. Social capital resources: Resources embedded in the social structure of the community accessed or mobilized for purposeful actions. Issues/limits of social capital: Unexpected or unintended outcomes of relying on social capital to activate and integrate resources. |
|
|
Lessons learned: Situated, practical knowledge about designing and implementing community-based DSM programs developed through reflection and learning in AR cycles. |
|
AR: action research; BG: blood glucose; CHW: community health worker; DSM: diabetes self-management; F&F: family and friends; HIT: health information technology; MOD-P: Moloka‘i ‘Ohana Diabetes Program; PCP: primary care physician; SME: subject matter expert.
RESULTS
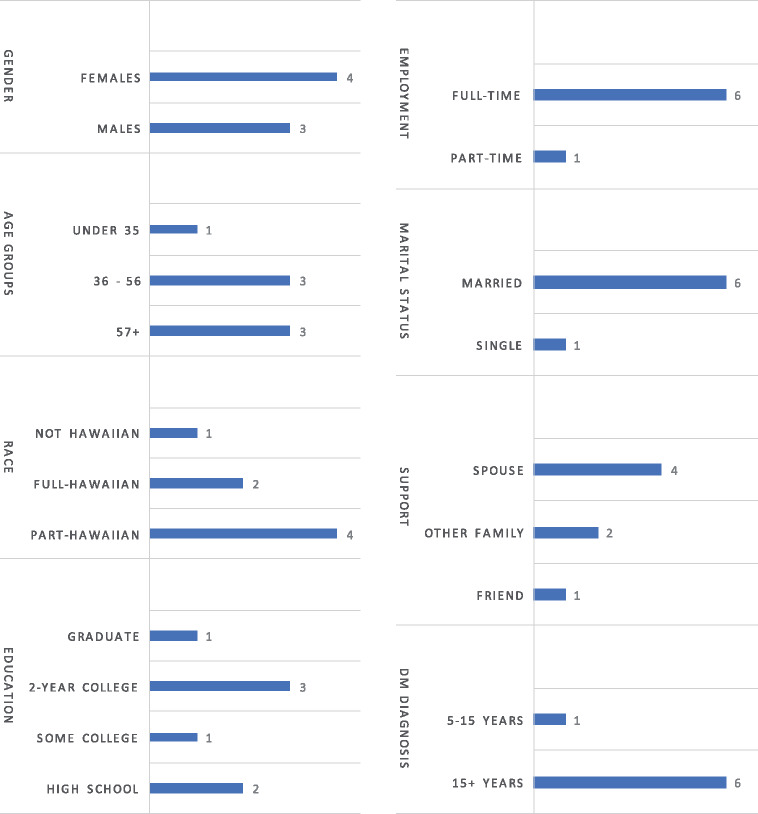
Participants were recruited via word-of-mouth and flyers posted in a local pharmacy and physician offices. Screening criteria included being 18 years of age or older, having a diagnosis of type 2 diabetes, having accompanying adult friend/family member to participate with the patient, owning a smartphone and agreeing to receive text messages, and having health insurance to cover cost of glucometer and DSM education sessions. All participants received a detailed description of the study and data management plan as part the informed consent protocol in phase I. Seven participants with diabetes, each accompanied by an F&F, agreed to join the project. This small pilot group was not statistically representative of the community in terms of demographic characteristics. However, all participants were longtime community members, and the cohort was similar in ethnic diversity to Moloka‘i’s population. Figure 2 highlights relevant demographic characteristics.
Figure 2.
Demographic characteristics of participants with diabetes. DM: diabetes mellitus.
Health and behavioral outcomes
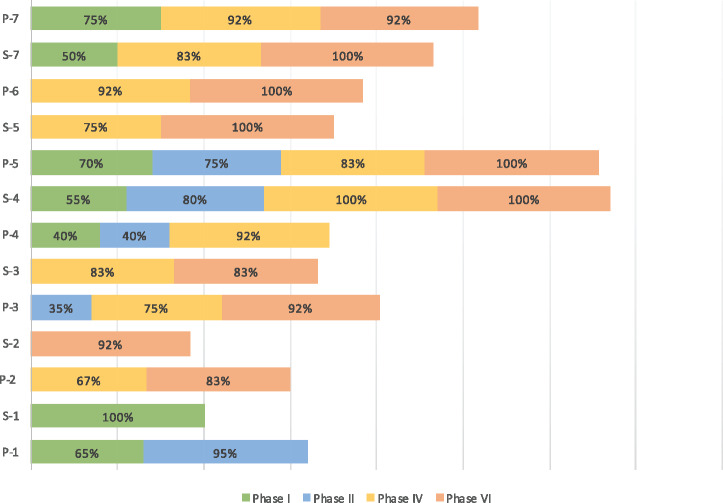
Descriptive, quantitative data collected throughout the course of the project pre- and postinterventions (Table 1) pointed to positive changes in diabetes knowledge, DSM behavior, and health outcomes over the 9-month program. Figure 3 displays results from the diabetes knowledge check scores before and after the DSM classes (phases I/II) and before and after the text message support (phases IV/VI) for patients and F&F. In instances in which participants responded to pretest and posttest questionnaires, scores improved. Improvements were most evident among F&F who had not participated in formal DSM education prior to this project.
Figure 3.
Diabetes Knowledge Test scores before, during, and after the Moloka‘i ‘Ohana Diabetes Program. Percent of correct answers from the Spoken Knowledge in Low Literacy in Diabetes Knowledge Assessment Scale; administered to patients with diabetes and family and friends support P: participant with diabetes; S: family and friends support.
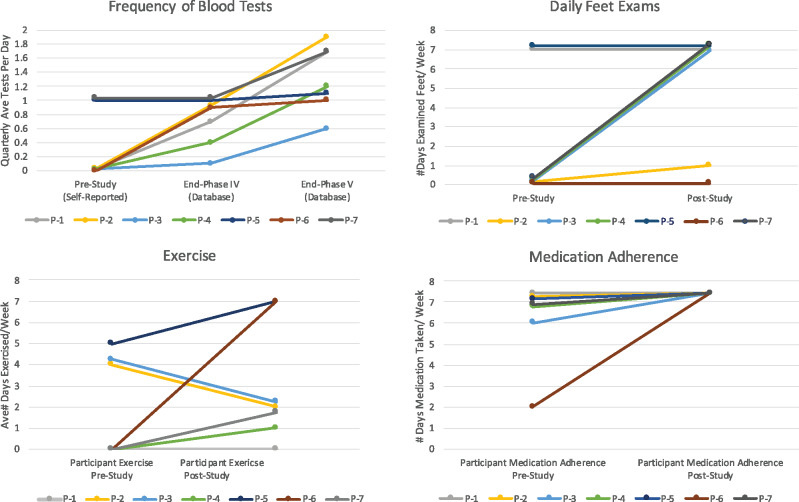
Figure 4 displays changes in pre- and postintervention DSM behaviors among patients. Increased BG monitoring frequency was the most consistent DSM behavior change for patients. Four of 7 also reported increased exercise or increases in daily foot exams, while 2 of 7 increased daily medication adherence and others maintained high adherence levels.
Figure 4.
Changes in diabetes self-management activities. P: participant with diabetes.
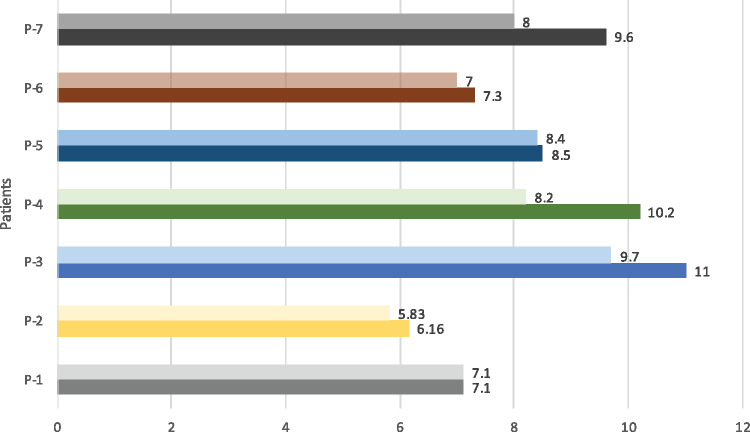
Health status outcomes were assessed based on A1c levels pre– and post–MOD-P (9 months’ duration). Figure 5 displays changes in A1c. Six of the 7 patient participants had improved A1c scores, and 1 had no change (mean decrease of -0.804 ± 0.809).
Figure 5.
Pre and post hemoglobin A1c percentage levels. P: participant with diabetes.
Enhancing access and engagement with DSM support
Qualitative analysis highlighted 3 themes related to integration of formal and informal health services, HIT resources, and F&F support.
Theme 1: Integrating formal and informal health services within the community
The patients’ primary care physician (PCP) initially referred patients to DSM education. The diabetes resource center partner in Honolulu provided formal educational services funded through patients’ health insurance. The resource center provided group DSM classes via video teleconference and individual consultations with the patient and F&F in-person (one-time) and through telehealth sessions in the home. By agreement with the resource center, F&F could attend without additional charges. Receiving this DSM education was a novel situation on Moloka‘i, as one F&F participant commented: “We never had classes together. So, once we found he [spouse] was diabetic we never had this kind education… The doctor would just say you take this kind of medication, but we never had classes to go to.”
A community health champion, community SMEs, and organizations with meeting facilities on Moloka‘i provided informal health services and resources. The community health champion, a retired community health provider living on the island, volunteered as the program manager. She drew on her social network among other professionals on Moloka‘i and in Honolulu to secure additional resources for the MOD-P at little or no cost, for instance, engaging the nephrologist and psychologist to volunteer telehealth sessions with the participants. Integrating informal community resources as customized sessions in phases III and IV with formal resources from the diabetes resource center (reimbursed via patients’ health insurance) in phases II and III amplified standard DSM education. Participants reflected that blending these services and in-person and video-conferencing delivery channels reinforced the DSM information, allowing better information absorption into self-care practices. This was valuable even for long-term patients. One participant noted, “I thought I knew everything, but I don’t. I learned new stuff.” However, questions about patient’s own medication or about how the classes aligned with the PCP’s goals for them could not be addressed, indicating integration of formal clinical care support would be valuable.
Theme 2: Integrating HIT resources with DSM services and support
The MOD-P used HITs to increase access to and patient engagement with DSM support by integrating HITs and social support interventions. Table 3 summarizes HIT resources and participants’ experiences with them.
Table 3.
Assessment of information technologies in MOD-P
| HIT application in interventions | Learning and reflection regarding HIT uses |
|---|---|
| Video teleconferencing: Zoom video communications | |
|
|
| Bluetooth-enabled BG monitor: OneTouch Verio Flex (and mobile phone) | |
|
|
| Diabetes management web-based system: OneTouch Reveal | |
|
|
| Mobile phone text messaging | |
|
|
BG: blood glucose; CHW: community health worker; DSM: diabetes self-management; F&F: family and friends; HIT: health information technology; MOD-P: Moloka‘i ‘Ohana Diabetes Program; PCP: primary care physician; SME: subject matter expert.
Video teleconferencing (zoom.us) in phases II-IV allowed participants to attend classes on island and in some instances, from their homes. This enabled one participant to attend sessions despite childcare responsibilities. It also allowed the dietician to help participants assess food in their homes.
Patients, F&F, and MOD-P staff interacted using Bluetooth-enabled glucometers and the monitor’s online database. Patients found Bluetooth-enabled glucometers more convenient compared with traditional paper logs and noted that color codes/graphs were easy to use and informative. This encouraged more frequent BG monitoring. One participant reflected, “During the study, I did more blood testing than I ever did in my whole life.” Several participants noted more frequent testing helped them understand their body’s response to different foods, which reinforced and personalized DSM education. Contrary to expectations, patients and F&F did not share test results via the database. Patients preferred viewing data on their mobile phones vs the online database, as not all participants had easy access to a computer. F&F did not use the online database but viewed the glucometer’s application on the patient’s mobile phone or received results via text messages from the patient.
For the MOD-P staff, the online database enabled remote data viewing, which allowed the community health worker (CHW) to personalize check-ins, reinforce DSM education, and maintain communication with participants via text messages over 3 months in phase V. We monitored the glucometer database to view the patients’ BG levels, frequency of tests, and notes on food, exercise, and medication. We then tailored text messages and support for each dyad. For example, when we saw a low BG result, we sent a summary and web link to articles explaining the signs, dangers, tips on how to increase glucose, and protocols for checking blood after a low reading. Patients reported that text message check-ins improved accountability, as they knew that CHWs were checking their numbers. Several commented this made them feel that CHWs “cared.” Reflecting on these experiences, one participant said, “Thanks to you guys, it (testing) is like a habit now.”
Although the texting phase helped maintain patients’ and F&F’s engagement with MOD-P (only 2 F&F dropped out), some participants found the timing of scheduled texts inconvenient, and group texting conversations burdensome. As one participant commented, “Sometimes there were too many texts…and sometimes the time when it comes…it’s towards the end of the day already, so I’m so tired!” Some F&F felt that they could be more honest about their partner’s status and behavior if their partner were not included on the text, for instance, when seeking advice on motivating the patient to exercise. Therefore, we adjusted how we sent text messages and used judgment about when to send to the whole group, to a dyad, or to an individual.
Theme 3: Integrating F&F support resources
A key objective of the MOD-P was to build the capacity of F&F to support partners by including them in the DSM education, providing ongoing information (eg, diet and menu hints), and facilitating F&F support from external resources (SMEs and CHWs) via HIT interventions (Table 3). The MOD-P formalized the previously informal support role by adding structure to the relationship. Generally, the F&F support role may include emotional, informational, or instrumental (task-based) support, feedback, and appraisal. This structure helped to define the support person’s responsibilities and expectations about the patient’s DSM behaviors. For instance, one F&F member said, “I came to support her. If I tried to find out what she learned from the meetings it would have been hard, by being part of this I can learn too. I can help prepare meals. I do most of the cooking.”
However, dyad relationships were varied and dynamic, requiring fine-tuning and adjustment in MOD-P activities. The 7 dyads each had different relationships, communication styles, interests in participating, and goals for managing diabetes. For instance, although some participants found that there were merits to having a relative as their support person, others reported that choosing a nonrelative might be preferable, as friends could help with stress reduction when the source of that stress was family related. Participants also noted that support comes from individuals other than designated F&F, such as several participants walking with one another or with fellow employees for exercise during lunch breaks when friends learned about their participation in MOD-P.
All dyads found that discussing the type of support the F&F should offer their partner, and specifically how to communicate support, was important to address stress and conflict that arose. For instance, one participant reported that the F&F provided information, exercise suggestions, and nutritional insights, but she felt that the F&F’s communication tone came off as scolding. Conversely, the F&F reported taking extra effort to provide information and then felt frustrated because the partner seemed to ignore the advice. To address communication issues and to reengage participants, we added group telehealth sessions to phase IV to address life goal-setting and dyad communication styles. One session (with a remote SME) focused explicitly on the F&Fs’ goals for engaging in the program and their own hopes for outcomes. Some patients found that they benefited from strict, relentless communication, while others preferred nurturing and encouraging suggestions. Overall, patients reported that there is a fine line between caring and nagging. As one F&F remarked, “Actually, (from) doing this class, well because they talked about what the support person should be like … cause I thought I was being caring…right? And then when he said something to me about nagging, I said - okay so I going just step back little bit.”
Activating and amplifying DSM support via social capital
The MOD-P relied on nominal funding for program staff and travel and had no allocated budget or paid staff. The program instead relied primarily on the social capital of stakeholders to activate latent DSM support resources, both formal (insurance funding for DSM education, glucose monitors) and informal (F&F, volunteer SMEs, community members), which were not being actively employed in the community prior to MOD-P. Table 4 summarizes sources of social capital critical to the development and implementation of the program and contributions to program outcomes.
Table 4.
Sources and uses of social capital by MOD-P participants
| Stakeholder | Sources of social capital in community | Implications for project outcome |
|---|---|---|
| Patient | Formal and informal relationships with F&F, PCP, program manager, staff, and other participants |
• Shared information • Asked for assistance and clarification • Reserved meeting venues • Supported other participants |
| F&F | Sense of community, trust, and reciprocity with patient, program manager, staff, and other participants |
• Emotional support • Informational support • Instrumental support • Companionship |
| Program manager | Reciprocal relationships with researcher, SMEs, participants, and MOD-P staff; access to pharmacy and staff; cultural and healthcare system knowledge |
• Design, implementation and modification of program • Researcher and SME coordination • Participant support • Informational support • Instrumental support |
| Community health worker | Trusting and reinforcing relationship with program manager; sense of community with personal connections with participants |
• Program operations (participant recruitment, organization and coordination of telehealth sessions, scheduling meeting venues) • Dyad support • Informational support • Instrumental support • Emotional support • Educational follow-up |
| Lead researcher | Reciprocal relationships with program manager and SMEs |
• Program development, coordination, and implementation (with program manager) • Dyad support • Informational support • Instrumental support • Technical training and SME coordination • Emotional support |
| Primary care provider | Formal relationship with patients; trust; central role in information diffusion |
• Authorized patient clinical eligibility • Provided patient referral to DSM education classes for insurance coverage • Oversaw patient clinical care |
| SMEs | Credentials, specialized knowledge, reciprocal relationship with program manager and researcher |
• Conducted telehealth classes • Coordinated with MOD-P staff • Provided input to MOD-P program design and redesign |
| Pharmacy staff | Credentials, specialized knowledge, formal relationships with program manager and health information technology vendors |
• Facilitated access to blood glucose monitor vendor and associated training • Assisted with clarification on medical coverage for DSM supplies |
| Telehealth resource center staff | Formal relationship with researcher | Technical assistance for teleconference arrangements and technical troubleshooting |
| Other community partners | Reciprocal and trusting relationships with facilities operators | Venues for meetings, interviews, and class sessions |
DSM: diabetes self-management; F&F: family and friends; MOD-P: Moloka‘i ‘Ohana Diabetes Program; PCP: primary care physician; SME: subject matter expert.
The program manager, a critical source of social capital, played a key role in selecting Moloka‘i as the site of the pilot program by enlisting the lead researcher to develop the program proposal. Through her community network, she recruited participants who knew her as a trusted community member, and she called on health education specialists she had worked with to volunteer their time for educational sessions. Her understanding of community needs and her wide network of contacts from years of working in health care on Moloka‘i and elsewhere in Hawai‘i catalyzed the integration of formal and informal DSM resources, activating the use of scarce resources and amplifying their effect.
The lead researcher was another key source of social capital to integrate formal and informal health services with IT support between Honolulu and Moloka‘i. Her experience managing telehealth services allowed her to orchestrate remote delivery of SME education classes on Moloka‘i. As the MOD-P progressed, she developed trusting relationships with the participants by participating in group sessions and taking on CHW tasks, such as checking on participants’ BG levels and initiating check-in texts. With growing social capital in this community, she motivated dyads’ continued active participation and engagement.
Importantly, social capital arising from the relationships among participants themselves contributed to dyad engagement and reciprocal social support. The shared cultural values of ‘ohana helped build cohesion in the cohort that facilitated information sharing and encouraged ongoing engagement with DSM activities (eg, exercise). The participants developed stronger peer-to-peer support through the common framework and language to discuss DSM information. This community awareness and commitment was evident in one F&F’s reflection: “This kind of program can help our community in general—because so many of the support people in the program were high risk for diabetes, our kids have diabetes, we all know someone with diabetes. The more we can get people to understand this the better.”
DISCUSSION
MOD-P was designed and developed as a community-centric initiative for under-resourced rural communities to facilitate community members’ access to and engagement with DSM support resources. Research provides strong evidence that DSM education,5 regular social support interactions beyond clinical encounters and settings,7,63 and a variety of HIT interventions that allow remote support for individuals’ self-care behaviors can improve health outcomes.6,12,15,16,18,19 Studies have also investigated how F&F might be engaged more effectively in DSM support generally22–24 and via text message coaching.27,28,30 Building on this evidence in an AR project, MOD-P integrated HIT interventions with social support from F&F and other community members. Although pilot data are descriptive because of the small sample size, the modest improvements observed in DSM behaviors across the cohort (Figure 4) are generally consistent with earlier studies,6,12 and reductions in A1c over the duration of the program (Figure 5) are in line with effects reported in meta-analyses of HIT interventions.6,18
The MOD-P thus provides encouraging evidence that this community-centric model has potential to be an effective, low-cost approach to increase access to and utilization of latent DSM support resources in under-resourced rural communities. Our evaluation of the project highlights key insights on how this may be accomplished.
First, integrating social support with HIT interventions reinforced DSM education for patients and F&F, and ongoing, subtle customizations of HIT interventions, tailored to individual dyads, were needed to maintain their engagement. Synergies between information in formal DSM classes, the glucometer system along with more frequent testing, and the CHWs’ check ins and educational text messages connected and reinforced DSM information and helped participants (all who had been living with diabetes for over 5 years) “learn new things” and improve some of their self-care behaviors. Customization is generally viewed as critical to reduce barriers and enhance patient engagement, particularly in underserved and minority populations.1,7,12 The small size of the MOD-P allowed customization of number, length, and content of telehealth sessions and the contents and style of text messages for dyads. Customization was key to maintaining participants’ interest over the 9 months of the program, with only 2 F&F dropping out. Our flexibility to customize MOD-P may not scale as easily to larger programs, though cafeteria-style customization may be beneficial. For instance, recent projects, which used computerized text messaging for DSM support, allowed participants to select topics of interest based on self-care goals and frequency of text message and adjusted messages for demographic characteristics (age, ethnicity, language); these studies demonstrated improvements in health outcomes and some self-care activities.7,12 However, such automated text messages may be less effective when used with rural populations, particularly among ethnic minorities, compared with urban communities.12
Second, motivational communication techniques for engaging F&F in DSM support should be addressed explicitly in program design and can be reinforced with text messaging. Effective social support does not come naturally and may even become a source of additional stress,27 as we observed. Recognizing this and a decline in F&F participation, we added group telehealth sessions to address DSM goals, life goals, and communication styles for patients and F&F. Recent research on F&F coaching suggests that text messages may be a cost-efficient communication channel to complement and reinforce F&F coaching for motivational communication.28,30 We found text messaging addressed some of the dyads’ F&F support issues, but the CHWs also had to adjust communication styles to attend closely to the dynamics of dyad relationships in text messaging interactions in phase V. Further research should examine how computer-generated coaching interactions might stimulate this type of situated, nuanced communication.
Finally, by focusing on community strengths, we found that community-led actions could activate and amplify scarce DSM resources that were previously underutilized or latent. Researchers have categorized what such communities and their members lack (eg, education, technology training, access to technology) as barriers to effective DSM education and support.1–3 However, MOD-P focused on a key strength of the Moloka‘i community: social capital that arises from close, supportive and long-term ‘ohana relationships among community members.37–42,48 The MOD-P demonstrated that community members themselves, drawing on social capital, can increase access to and engagement with DSM resources in a community-led program, with little financial support, without burdening local clinics, and that positive health and self-care behavioral outcomes can result. This approach poses some risks. The community health champion’s network of SMEs, and her experience, dedication, and trust with community members, were all instrumental to engage stakeholders (eg, lead researcher, SMEs, participants) and to activate underutilized formal resources (eg, PCP referrals, insurance reimbursement for DSM education and glucometers). Not all communities have individuals with this level of social capital, and such individuals are subject to burnout over time. An important first step with the community-centric model, therefore, is to assess social capital stocks and to identify champions who can catalyze formal and informal resources before attempting a pilot program. Program design and learning cycles should consider mechanisms to support and reinforce key stakeholders.
CONCLUSION
Substantial socioeconomic and technological barriers limit rural communities’ access to DSM programs vital to addressing the escalating challenges of diabetes in these communities.64 Nonetheless, leveraging community strengths is a viable strategy for creating chronic disease management programs. This study demonstrated how drawing on a community’s social capital to integrate formal and informal resources, with social support from F&F and HIT interventions that facilitate remote access to DSM resources, can contribute to improved health outcomes. The MOD-P provides a model for the design and implementation of community-led DSM support efforts to complement and supplement clinical efforts.
The results of this pilot are promising, but they are based on one community that exemplifies the social capital outlined here. The community-centric model should be challenged in additional studies across a diverse array of rural communities to refine its design, assess its efficacy in different contexts, and develop and document processes to implement multiple projects reliably. Future research can also assess how customized computerization of text messaging support for DSM education and F&F coaching7,20,28,30 influences patient engagement and may increase the model’s scalability to larger cohorts.
FUNDING
This work was supported in part by University of Hawai’i faculty research funds.
AUTHOR CONTRIBUTIONS
CH and EJD were involved with the conception, design, and data collection of the study. All authors were involved with the analysis of the study and writing and editing the manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLDEGMENTS
The authors acknowledge the MOD-P Program Manager and participants for their important contributions to this study.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Alvarado MM, Kum H-C, Coronado KG, Foster MJ, Ortega P, Lawley MA.. Barriers to remote health interventions for type 2 diabetes: a systematic review and proposed classification scheme. J Med Internet Res 2017; 19 (2): e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rutledge SA, Masalovich S, Blacher RJ, Saunders MM.. Diabetes self-management education programs in nonmetropolitan counties—United States, 2016. MMWR Surveill Summ 2017; 66 (10): 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Petersen F, Brown A, Pather S, Tucker WD.. Challenges for the adoption of ICT for diabetes self‐management in South Africa. Electron J Inf Syst Develop Countries 2019; 86 (5): e12113. [Google Scholar]
- 4. Siminerio L, Ruppert K, Huber K, Toledo FGS.. Telemedicine for reach, education, access, and treatment (TREAT): linking telemedicine with diabetes self-management education to improve care in rural communities. Diabetes Educ 2014; 40 (6): 797–805. [DOI] [PubMed] [Google Scholar]
- 5. Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes. Diabetes Educ 2017; 43 (1): 40–53. [DOI] [PubMed] [Google Scholar]
- 6. Heitkemper EM, Mamykina L, Travers J, Smaldone A.. Do health information technology self-management interventions improve glycemic control in medically underserved adults with diabetes? A systematic review and meta-analysis. J Am Med Inform Assoc 2017; 24: 1024–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mamykina L, Heitkemper EM, Smaldone AM, et al. Structured scaffolding for reflection and problem solving in diabetes self-management: qualitative study of mobile diabetes detective. J Am Med Inform Assoc 2016; 23 (1): 129–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baker LC, Johnson SJ, Macaulay D, Birnbaum H.. Integrated telehealth and care management program for Medicare beneficiaries with chronic disease linked to savings. Health Aff (Millwood) 2011; 30 (9): 1689–97. [DOI] [PubMed] [Google Scholar]
- 9. Shea S, Weinstock RS, Teresi JA, et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc 2009; 16 (4): 446–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gee PM, Greenwood DA, Paterniti DA, Ward D, Miller LMS.. The eHealth enhanced chronic care model: a theory derivation approach. J Med Internet Res 2015; 17 (4): e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Årsand E, Frøisland DH, Skrøvseth SO, et al. Mobile health applications to assist patients with diabetes: lessons learned and design implications. J Diabetes Sci Technol 2012; 6 (5): 1197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dobson R, Whittaker R, Jiang Y, et al. Effectiveness of text message based, diabetes self management support programme (SMS4BG): two arm, parallel randomised controlled trial. BMJ 2018; 361: k1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dick JJ, Nundy S, Solomon MC, Bishop KN, Chin MH, Peek ME.. Feasibility and usability of a text message-based program for diabetes self-management in an urban African-American population. J Diabetes Sci Technol 2011; 5 (5): 1246–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS.. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res 2015; 17 (2): e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Roblin DW. The potential of cellular technology to mediate social networks for support of chronic disease self-management. J Health Commun 2011; 16: 59–76. [DOI] [PubMed] [Google Scholar]
- 16. Aikens JE, Zivin K, Trivedi R, Piette JD.. Diabetes self-management support using mHealth and enhanced informal caregiving. J Diabetes Complications 2014; 28 (2): 171–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hussein WI, Hasan K, Jaradat AA.. Effectiveness of mobile phone short message service on diabetes mellitus management; the SMS-DM study. Diabetes Res Clin Pract 2011; 94 (1): e24–6. [DOI] [PubMed] [Google Scholar]
- 18. Saffari M, Ghanizadeh G, Koenig HG.. Health education via mobile text messaging for glycemic control in adults with type 2 diabetes: a systematic review and meta-analysis. Prim Care Diabetes 2014; 8 (4): 275–85. [DOI] [PubMed] [Google Scholar]
- 19. Vorderstrasse A, Lewinski A, Melkus GD, Johnson C.. Social support for diabetes self-management via eHealth interventions. Curr Diab Rep 2016; 16 (7): 56. [DOI] [PubMed] [Google Scholar]
- 20. Heitkemper EM, Mamykina L, Tobin JN, Cassells A, Smaldone A.. Baseline characteristics and technology training of underserved adults with type 2 diabetes in the Mobile Diabetes Detective (MoDD) randomized controlled trial. Diabetes Educ 2017; 43 (6): 576–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nundy S, Dick JJ, Solomon MC, Peek ME.. Developing a behavioral model for mobile phone-based diabetes interventions. Patient Educ Couns 2013; 90 (1): 125–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Denham S. A, Manoogian MM, Schuster L.. Managing family support and dietary routines: type 2 diabetes in rural Appalachian families. Fam Syst Heal 2007; 25 (1): 36–52. [Google Scholar]
- 23. Baig AA, Benitez A, Quinn MT, Burnet DL.. Family interventions to improve diabetes outcomes for adults. Ann N Y Acad Sci 2015; 1353 (1): 89–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Armour T. A, Norris SL, Jack L, Zhang X, Fisher L.. The effectiveness of family interventions in people with diabetes mellitus: a systematic review. Diabet Med 2005; 22 (10): 1295–305. [DOI] [PubMed] [Google Scholar]
- 25. Gleeson‐Kreig J, Bernal H, Woolley S.. The role of social support in the self‐management of diabetes mellitus among a Hispanic population. Public Health Nurs 2002; 19 (3): 215–22. [DOI] [PubMed] [Google Scholar]
- 26. Hu J, Amirehsani K, Wallace DC, Letvak S.. Perceptions of barriers in managing diabetes: perspectives of Hispanic immigrant patients and family members. Diabetes Educ 2013; 39 (4): 494–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lee AA, Piette JD, Heisler M, Janevic MR, Langa KM, Rosland A-M.. Family members’ experiences supporting adults with chronic illness: a national survey. Fam Syst Heal 2017; 35 (4): 463–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mayberry LS, Berg CA, Harper KJ, Osborn CY.. The design, usability, and feasibility of a family-focused diabetes self-care support mHealth intervention for diverse, low-income adults with type 2 diabetes. J Diabetes Res 2016; 2016: 7586385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Manoogian MM, Harter LM, Denham SA.. The storied nature of health legacies in the familial experience of type 2 diabetes. J Fam Commun 2010; 10 (1): 40–56. [Google Scholar]
- 30. Mayberry LS, Bergner EM, Harper KJ, Laing S, Berg CA.. Text messaging to engage friends/family in diabetes self-management support: acceptability and potential to address disparities. J Am Med Inform Assoc 2019; 26 (10): 1099–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pamungkas RA, Chamroonsawasdi K, Vatanasomboon P.. A systematic review: family support integrated with diabetes self-management among uncontrolled type II diabetes mellitus patients. Behav Sci (Basel) 2017; 7 (4): 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Toobert DJ, Strycker LA, King DK, Barrera M, Osuna D, Glasgow RE.. Long-term outcomes from a multiple-risk-factor diabetes trial for Latinas: Viva Bien! Transl Behav Med 2011; 1 (3): 416–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Keogh KM, Smith SM, White P, et al. Psychological family intervention for poorly controlled type 2 diabetes. Am J Manag Care 2011; 17 (2): 105–13. [PubMed] [Google Scholar]
- 34. García-Huidobro D, Bittner M, Brahm P, Puschel K.. Family intervention to control type 2 diabetes: a controlled clinical trial. Fam Pract 2011; 28: 4–11. [DOI] [PubMed] [Google Scholar]
- 35. Hsieh C-H. A concept analysis of social capital within a health context. Nurs Forum 2008; 43 (3): 151–9. [DOI] [PubMed] [Google Scholar]
- 36. Story WT. Social capital and health in the least developed countries: a critical review of the literature and implications for a future research agenda. Glob Public Health 2013; 8 (9): 983–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lin N. Building a network theory of social capital. Connections 1999; 22: 28–51. [Google Scholar]
- 38. Adler P, Kwon S-W.. Social capital: prospects for a new concept. Acad Manag Rev 2002; 27 (1): 17–40. [Google Scholar]
- 39. Krishna A. Moving from the stock of social capital to the flow of benefits: the role of agency. World Dev 2001; 29 (6): 925–43. [Google Scholar]
- 40. Hogan MJ. Social capital: potential in family social sciences. J Socio Econ 2001; 30 (2): 151. [Google Scholar]
- 41. Putnam RD. Bowling alone: America’s declining social capital In: Crothers L, Lockhart C, eds. Culture and Politics. New York: Palgrave Macmillan; 2000: 223–4. [Google Scholar]
- 42. Agampodi TC, Agampodi SB, Glozier N, Siribaddana S.. Measurement of social capital in relation to health in low and middle income countries (LMIC): a systematic review. Soc Sci Med 2015; 128: 95–104. [DOI] [PubMed] [Google Scholar]
- 43. McElfish PA, Long CR, Kohler PO, et al. Comparative effectiveness and maintenance of diabetes self-management education interventions for Marshallese patients with type 2 diabetes: a randomized controlled trial. Diabetes Care 2019; 42 (5): 849–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hallgren EA, McElfish PA, Rubon-Chutaro J.. Barriers and opportunities. Diabetes Educ 2015; 41 (1): 86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Molokai E. Hawaii (HI) Poverty Rate Data. Hinsdale, IL: Advameg, Inc; 2020. [Google Scholar]
- 46.Molokai Community Plan Update: Planning Department/CPAC Draft.; 2015. https://www.mauicounty.gov/DocumentCenter/View/100656/Molokai-Community-Plan---Planning-Dept--CPAC-Draft-to-Planning-Commission-151112?bidId Accessed November 18, 2019.
- 47.Hawaii Health Data Warehouse, Hawaii State Department of Health, Behavioral Risk Factor Surveillance System. https://health.hawaii.gov/brfss/ Accessed November 28, 2019.
- 48. Trask HK. Native social capital: the case of Hawaiian sovereignty and Ka Lahui Hawaii. Policy Sci 2000; 33: 375–85. [Google Scholar]
- 49. Mckay J, Marshall P.. The dual imperatives of action research. Info Technol People 2001; 14 (1): 46–59. [Google Scholar]
- 50. Kemmis S, McTaggart R, Nixon R.. The Action Research Planner: Doing Critical Participatory Action Research. Singapore: Springer Science & Business Media; 2013. [Google Scholar]
- 51. Dickens L, Watkins K.. Action research: rethinking Lewin In: Gallos V, ed. Organization Development. San Francisco, CA: Jossey-Bass; 2006: 185–201. [Google Scholar]
- 52. Kemmis S, McTaggart R.. Participatory action research: communicative action and the public sphere In: Denzin NK, Lincoln YS, eds. Strategies of Qualitative Inquiry. Vol. 2 Thousand Oaks, CA: Sage; 2008: 271–330. [Google Scholar]
- 53. Greenwood D, Levin M.. Educational action research In: Introduction to Action Research. 2nd ed.Thousand Oaks, CA: Sage; 2007: 168–83. [Google Scholar]
- 54. Lau F, Hayward R.. Building a virtual network in a community health research training program. J Am Med Inform Assoc 2000; 7 (4): 361–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Day K, Kenealy TW, Sheridan NF.. Should we embed randomized controlled trials within action research: arguing from a case study of telemonitoring. BMC Med Res Methodol 2016; 16 (1): 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Davison RM, Martinsons MG, Kock N.. Principles of canonical action research. Inf Syst J 2004; 14 (1): 65–86. [Google Scholar]
- 57. Kroenke K, Spitzer RL, Williams JB.. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16 (9): 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Williams G, Freedman Z, Deci E.. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care 1998; 21 (10): 1644–51. [DOI] [PubMed] [Google Scholar]
- 59. La Greca AM, Bearman KJ.. The diabetes social support questionnaire-family version: evaluating adolescents’ diabetes-specific support from family members. J Pediatr Psychol 2002; 27 (8): 665–76. [DOI] [PubMed] [Google Scholar]
- 60. Rothman RL, Malone R, Bryant B, et al. The spoken knowledge in low literacy in diabetes scale: a diabetes knowledge scale for vulnerable patients. Diabetes Educ 2005; 31 (2): 215–24. [DOI] [PubMed] [Google Scholar]
- 61. Sandelowski M, Leeman J.. Writing usable qualitative health research findings. Qual Health Res 2012; 22 (10): 1404–13. [DOI] [PubMed] [Google Scholar]
- 62. Guest G, MacQueen KM, Namey EE.. Applied Thematic Analysis. Thousand Oaks, CA: Sage; 2011. [Google Scholar]
- 63. Rosland AM, Kieffer E, Israel B, et al. When is social support important? The association of family support and professional support with specific diabetes self-management behaviors. J Gen Intern Med 2008; 23 (12): 1992–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Center for Surveillance, Epidemiology and Laboratory Services. Policy brief: providing diabetes self-management education and support for rural Americans. 2018. https://www.cdc.gov/ruralhealth/diabetes/policybrief.html# Accessed May 27, 2019.
- 65. Padgett DK. Qualitative Methods in Social Work Research. Vol. 36 Thousand Oaks, CA: Sage; 2016. [Google Scholar]
- 66. Williamson GR, Prosser S.. Action research: politics, ethics and participation. J Adv Nurs 2002; 40 (5): 587–93. [DOI] [PubMed] [Google Scholar]
- 67. Louis MR, Bartunek JM.. Insider/outsider research teams: collaboration across diverse perspectives. J Manag Inq 1992; 1 (2): 101–10. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.