Abstract
Low rates of preterm birth were observed during the coronavirus disease 2019 (COVID-19) lockdown in Melbourne, Australia.
INTRODUCTION
Preliminary international data suggest a decrease in prematurity during the coronavirus disease 2019 (COVID-19) pandemic,1–3 potentially due to the effect of lockdown. Others could not confirm this observation.4 The lockdown implemented in metropolitan Melbourne, Australia, has been one of the longest and strictest in the world. We aimed to investigate its effect on prematurity rates.
METHODS
We investigated the rates of prematurity in women who gave birth at Monash Health's three maternity hospitals serving a large geographic area in Melbourne, Australia, between January 1, 2018, and September 30, 2020. Ethical approval was obtained from the Monash Health Human Research Ethics Committee (approval number QA/69113/MonH-2020-235157).
We conducted interrupted time-series analysis of the monthly rates of prematurity before 28 weeks of gestation, comparing trends before and after July 2020 with an ARIMA (auto-regressive integrated moving average) model. Rates of prematurity at less than 28 weeks of gestation, less than 34 weeks, and less than 37 weeks among women who gave birth in July–September 2020 were compared with those giving birth July–September 2019, excluding pregnancy terminations and stillbirths. Analyses were conducted in Stata 16.0, and a .05 statistical significance threshold was used.
RESULTS
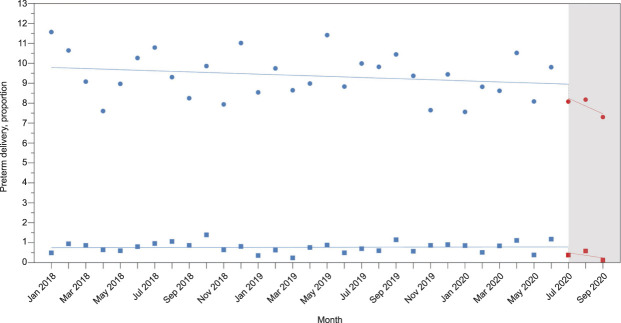
Between January 2018 and September 2020, 27,164 women gave birth to 27,760 neonates, including 26,578 (97.8%) singleton and 586 (2.2%) multiple pregnancies. Interrupted time-series analysis showed a significantly lower rate of prematurity after July 2020 (Fig. 1, P=.007 for births at less than 37 weeks of gestation).
Fig. 1. Interrupted time-series analysis between January 2018 and September 2020. The blue and red circles represent the monthly rates of preterm birth at less than 37 weeks of gestation before and after July 2020, respectively. The blue and red squares represent the monthly rates of preterm birth at less than 28 weeks of gestation before and after July 2020, respectively. The shaded area represents the lockdown period (n=26,895, excluding 269 pregnancies that did not result in a liveborn neonate, P=.007 for the difference in trends of preterm birth at less than 37 weeks of gestation).
Matheson. Prematurity During Lockdown. Obstet Gynecol 2021.
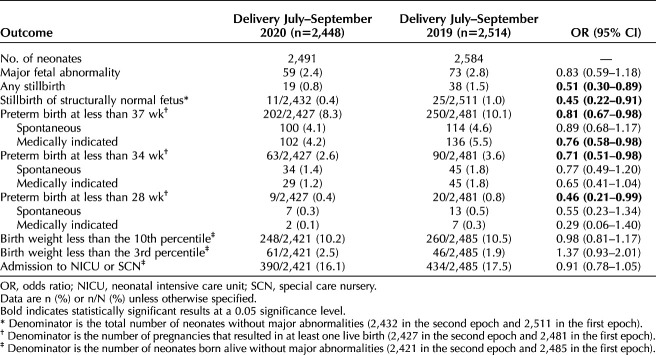
In total, there were 2,448 births in July–September 2020 and 2,514 births in July–September 2019. Comparing women who gave birth in July–September 2020 with those in the same period in 2019, there were no differences in demographic or baseline characteristics (age, weight, height, region of birth, smoking, marital status, and parity). Women giving birth during lockdown had a lower rate of multiple pregnancies (1.8% vs 2.8%, P=.015). We observed significantly lower rates of prematurity before 28 weeks of gestation (0.4% vs 0.8%, odds ratio [OR] 0.46, 95% CI 0.21–0.99, P=.047), before 34 weeks (2.6% vs 3.6%, OR 0.71, 95% CI 0.51–0.98, P=.038), and before 37 weeks (8.3% vs 10.1%, OR 0.81, 95% CI 0.67–0.98, P=.034).
The effect was stronger in medically indicated prematurity, but a smaller nonsignificant decrease in spontaneous preterm birth was observed. These findings were not associated with increased rates of stillbirth or birth of small-for-gestational-neonates. The effect was also independent of multiple pregnancies (adjusted OR for birth at less than 34 weeks of gestation 0.71, 95% CI 0.53–0.96, P=.026). Pregnancy outcomes are summarized in Table 1.
Table 1.
Pregnancy Outcomes of Women Who Delivered Between July and September 2020 and Those Who Delivered Between July and September 2019
DISCUSSION
Australia adopted strict mitigation measures, reaching a score of 80 in a 1–100 stringency scale after July 2020,5 and the lockdown was stricter still in Melbourne. Between July 8 and September 28, 2020, leaving the house was permitted only for “essential” workers, seeking health care, 1 hour a day of exercise, or shopping for necessities while staying within 5 km from home. Gatherings between more than two people were prohibited. A daily curfew was introduced from 8:00 pm, and mask wearing outside of the home became mandatory.
We confirm an association between lockdown and reduced preterm birth rates.1–3 The reduction that occurred was stronger in medically indicated than in spontaneous prematurity and, reassuringly, without increases in stillbirth or undetected small-for-gestational-age neonates. Conversely, we also found a decrease in stillbirth rates during lockdown. The effect persisted after adjustment for twin pregnancies. Lockdown may reduce prematurity rates through lifestyle changes including cessation of work, increased hygiene measures, social distancing resulting in fewer infections by common pathogens, less air pollution, or perhaps other factors not yet delineated. Although most interventions to reduce the risk of prematurity apply to high-risk populations and have limited effect, lockdown affected the entire population.
A limitation of our study is that women and children who qualify for our cohorts do so conditional on delivery, which, together with possible unmeasured confounding by differences in maternal demographics and clinical characteristics, may affect the comparability and likely explains the difference in multiple pregnancy rates between the two groups. Comparability might be further affected by the milder restrictions that occurred in Melbourne in April–May 2020. Future studies are needed to better quantify the effect of lockdown in relation to gestational age, subgroup effects, and to establish potential causative factors.
Footnotes
Financial Disclosure Kirsten R. Palmer reports that money was paid to her institution from GlaxoSmithKline, the Cerebral Palsy Alliance, and the National Health & Medical Research Council. Ben W. Mol reports that he is supported by a NHMRC Investigator grant (GNT1176437), and has been a consultant for ObsEva, Merck, Merck KGaA, iGenomix and Guerbet. He has received research support from Merck and Guerbet. The other authors did not report any potential conflicts of interest.
Presented at the Society for Maternal-Fetal Medicine's 41st Annual Pregnancy Meeting, held virtually, January 25–30, 2021.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/C186.
REFERENCES
- 1.Hedermann G, Hedley PL, Bækvad-Hansen M, Hjalgrim H, Rostgaard K, Poorisrisak P, et al. Danish premature birth rates during the COVID-19 lockdown. Arch Dis Child Fetal Neonatal Ed 2021;106:93–5. doi: 10.1136/archdischild-2020-319990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Philip RK, Purtill H, Reidy E, Daly M, Imcha M, McGrath D, et al. Unprecedented reduction in births of very low birthweight (VLBW) and extremely low birthweight (ELBW) infants during the COVID-19 lockdown in Ireland: a ‘natural experiment’ allowing analysis of data from the prior two decades. BMJ Glob Health 2020;5:e003075. doi: 10.1136/bmjgh-2020-003075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Been JV, Ochoa LB, Bertens LCM, Schoenmakers S, Steegers EAP, Reiss IKM. Impact of COVID-19 mitigation measures on the incidence of preterm birth: a national quasi-experimental study. Lancet Public Health 2020;5:e604–11. doi: 10.1016/S2468-2667(20)30223-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rasmussen MI, Hansen ML, Pichler G, Dempsey E, Pellicer A, El-Khuffash A, et al. Extremely preterm infant admissions within the SafeBoosC-III consortium during the COVID-19 lockdown. medRxiv 2020:2020.10.02.20204578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hale T, Angrist N, Cameron-Blake E, Hallas L, Kira B, Majumdar S, et al. Oxford COVID-19 government response tracker, Blavatnik School of Government. Accessed October 14, 2020. https://www.bsg.ox.ac.uk/research/research-projects/coronavirus-government-response-tracker [DOI] [PubMed] [Google Scholar]