Robert L. Goldenberg, MD.

Elizabeth M. McClure, PhD.

Conditions associated with preterm birth are responsible for more than half of childhood mortality before 5 years of age and a significant portion of long-term developmental disabilities.1 Despite many attempts, few interventions have substantially reduced the rate of neonates born preterm.2 Bedrest, antibiotics, progestins, pessaries, and numerous other strategies have not consistently reduced preterm birth. Despite some fluctuations, the preterm birth rate does not appear to have changed substantially over the past half century.1
One challenge in analyzing the effect of various interventions on preterm birth is that the rates have not been measured consistently either over time or across locations. Combinations of last menstrual period, fundal height, quickening, and, in recent decades, ultrasonography, have been used to determine gestational age. This variation in methodology contributes to challenges in evaluating changes in gestational age over time and in comparing preterm birth rates among various groups, especially outside of randomized trials.3 Therefore, any study assessing preterm birth should describe the methodology used to determine gestational age. Given the limitations of gestational age ascertainment, birth weight should be used to confirm study findings. In addition, other confirmatory data should be reported when possible, such as the percentage of neonatal intensive care unit admissions.
Preterm births have many apparent risk factors and etiologies but often are divided into two major categories: 1) spontaneous preterm births, usually defined as those occurring after spontaneous onset of labor or membrane rupture; and 2) medically indicated preterm births, usually defined as those occurring after a prelabor cesarean birth or induction of labor.1,4 Studies claiming a reduction in preterm birth should describe the proportion of the reduction attributed to each group. Preterm births also are frequently classified by gestational age, ranging from extremely preterm (less than 28 weeks of gestation) to late preterm (34–37 weeks). Studies claiming a reduction in preterm birth should be able to determine the gestational age groups in which reductions occurred. Finally, because stillbirth is a competing outcome, the effect of the intervention on stillbirth rates should be presented as well.
The observation of a potential reduction in preterm birth in some locations during the coronavirus disease 2019 (COVID-19) pandemic has aroused interest, likely in part due to previous failures to reduce preterm birth rates. In most reports, this potential reduction is attributed to indirect effects of a lockdown rather than to the infection itself. Early in the pandemic, multiple reports showed an increase in preterm birth associated with maternal COVID-19 infection, which, in retrospect, appeared to be related to an increase in medically indicated prelabor cesarean births.5,6 More recently, while the effect of maternal COVID-19 infection on preterm birth has become less clear, no evidence suggests that maternal infection with COVID-19 reduces preterm birth.5
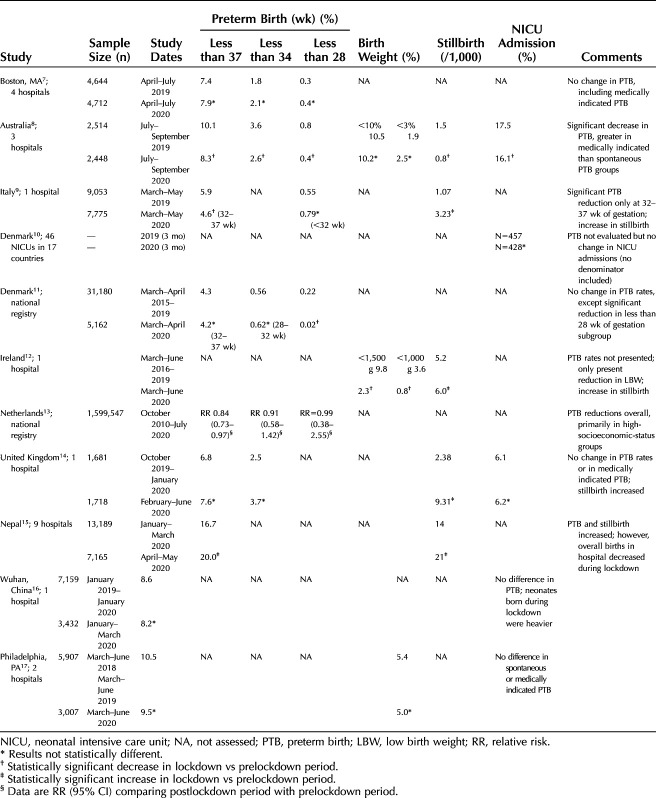
In this month's issue of Obstetrics & Gynecology, two Research Letters (see pages 403 and 405) present preterm birth rates associated with COVID-19 lockdown compared with an earlier period.7,8 We are aware of 11 studies,7–17 mostly originating from high-income countries, including the two in this issue,7,8 that explore the association of lockdowns implemented in response to the COVID-19 pandemic and rates of preterm birth or low birth weight. We have summarized these studies (Table 1), focusing not only on their results but also on their adherence to some of the quality metrics. As with this issues' two studies, when all are considered, there is essentially an even split between those suggesting that lockdown was associated with reduced rates of preterm birth or low birth weight and those that conclude it was not. We suspect that investigators who did not see a reduction in preterm birth would be less likely to publish their results. Thus, negative findings may be underrepresented in publications.
Table 1.
Summary of Studies Evaluating Preterm Birth Before and After the Coronavirus Disease 2019 (COVID-19) Lockdown
In terms of quality, none of the studies describe methods to determine gestational age; for those estimating a reduction in preterm birth, only one found a similar reduction in birth weight. The study from Australia,8 which demonstrated a reduction in preterm birth during the lockdown, did not show a corresponding decrease in birth weight during the same time-period. In this study, the reduction in preterm birth appeared to be greater among medically indicated deliveries. Several studies found that the reduction in preterm birth rate was confined to extremely low-birth-weight or very-low-birth-weight preterm neonates; on the other hand, one study showed a significant reduction only in near-term births. Although many addressed overall cesarean birth rates, few7,8,14,17 addressed whether the preterm births averted were spontaneous or medically indicated. Of the studies that provided data on medically indicated preterm birth, the three that showed no changes also observed no change in the overall preterm birth rates.7,14,17 The most recently published study, from Philadelphia, Pennsylvania, which included data on medically indicated preterm births, found no change in preterm birth or stillbirths associated with the lockdown.17
Although unavoidable because of the range of governmental actions, different study dates, and lengths of time defined the lockdown periods, but of concern, many studies used different lengths of time for the historic control sample. In addition, the numbers were often small, especially in the studies that evaluated subgroups of extremely preterm neonates. Because many potential pregnancy outcomes could have been reported in these studies (eg, various gestational age and birth weight ranges, neonatal intensive care unit admission), it is unsurprising that a few of these, by chance, would be positive. Importantly, among the six publications that presented data on stillbirth in the lockdown period, four of them reported significant increases.
With the methodologic issues noted, the discrepancies in results, and the likelihood of time-period selection and publication bias, we believe that there is not sufficient evidence to conclude that there was a consistent reduction in preterm birth associated with COVID-19 lockdowns. Thus, although the two articles presented in this issue add to the overall body of literature, there remain concerns that make the direction of the findings difficult to interpret. Certainly, it is far too early to consider potential mechanisms for a reduction in preterm birth associated with COVID-19 lockdowns.
Footnotes
Financial Disclosure The authors did not report any potential conflicts of interest.
REFERENCES
- 1.Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health 2019;7:e37–46. doi: 10.1016/S2214-109X(18)30451-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Piso B, Zechmeister-Koss I, Winkler R. Antenatal interventions to reduce preterm birth: an overview of Cochrane Systematic Reviews. BMC Res Notes 2014;7:265. doi: 10.1186/1756-0500-7-265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harrison MS, Goldenberg RL. Global burden of prematurity. Semin Fetal Neonatal Med 2016;21:74–9. doi: 10.1016/j.siny.2015.12.007 [DOI] [PubMed] [Google Scholar]
- 4.Papageorghiou AT, Kennedy SH, Salomon LJ, Altman DG, Ohuma EO, Stones W, et al. The INTERGROWTH-21st fetal growth standards: toward the global integration of pregnancy and pediatric care. Am J Obstet Gynecol 2018;218:S630–40. doi: 10.1016/j.ajog.2018.01.011 [DOI] [PubMed] [Google Scholar]
- 5.Yang R, Mei H, Zheng T, Fu Q, Zhang Y, Buka S, et al. Pregnant women with COVID-19 and risk of adverse birth outcomes and maternal-fetal vertical transmission: a population-based cohort study in Wuhan, China. BMC Med 2020;18:330. doi: 10.1186/s12916-020-01798-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pettirosso E, Giles M, Cole S, Rees M. COVID-19 and pregnancy: a review of clinical characteristics, obstetric outcomes and vertical transmission. Aust N Z J Obstet Gynaecol 2020;60:640–59. doi: 10.1111/ajo.13204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wood R, Sinnott C, Goldfarb I, Clapp M, McElrath T, Little S. Preterm birth during the coronavirus 2019 (COVID-19) pandemic in a large hospital system in the United States. Obstet Gynecol 2021;137:403–4. doi: 10.1097/AOG.0000000000004237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matheson A, McGannon CJ, Malhotra A, Palmer KR, Stewart AE, Wallace EM, et al. Prematurity rates during the coronavirus disease 2019 (COVID -19) pandemic lockdown in Melbourne, Australia. Obstet Gynecol 2021;137:405–7. doi: 10.1097/AOG.0000000000004236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Curtis M, Villani L, Polo A. Increase of stillbirth and decrease of late preterm infants during the COVID-19 pandemic lockdown. Arch Dis Child Fetal Neonatal Ed 2020 Oct 30. [Epub ahead of print]. doi: 10.1136/archdischild-2020-320682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rasmussen MI, Hansen ML, Pichler G, Dempsey E, Pellicer A, EL-Khuffash A, et al. Extremely preterm infant admissions within the SafeBoosC-III consortium during the COVID-19 lockdown. medRxiv 2020. doi: 10.1101/2020.10.02.20204578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hedermann G, Hedley PL, Bækvad-Hansen M, Hjalgrim H, Roostgaard K, Poorisrisak P, et al. Danish premature birth rates during the COVID-19 lockdown. Arch Dis Child Fetal Neonatal Ed 2021;106:93–5. doi: 10.1136/archdischild-2020-319990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Philip RK, Purtill H, Reidy E, Daly M, Imcha M, McGrath D, et al. Unprecedented reduction in births of very low birthweight (VLBW) and extremely low birthweight (ELBW) infants during the COVID-19 lockdown in Ireland: a 'natural experiment' allowing analysis of data from the prior two decades. BMJ Glob Health 2020;5:e003075. doi: 10.1136/bmjgh-2020-003075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Been JV, Ochoa LB, Bertens LCM, Schoenmakers S, Steegers EAP, Reiss IKM. Impact of COVID-19 mitigation measures on the incidence of preterm birth: a national quasi-experimental study. Lancet Public Health 2020;5:e604–11. doi: 10.1016/S2468-2667(20)30223-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khalil A, von Dadelszen P, Draycott T, Ugwumadu A, O'Brien P, Magee L. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA 2020;324:705–6. doi: 10.1001/jama.2020.12746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kc A, Gurung R, Kinney MV, Sunny AK, Moinuddin M, Basnet O, et al. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth and neonatal mortality outcomes in Nepal: a prospective, observational study. Lancet Glob Health 2020;8:e1273–81. doi: 10.1016/S2214-109X(20)30345-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li M, Yin H, Jin Z, Zhang H, Leng B, Luo Y, et al. Impact of Wuhan lockdown on the indications of cesarean delivery and newborn weights during the epidemic period of COVID-19. PLoS One 2020;15:e0237420. doi: 10.1371/journal.pone.0237420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Handley SC, Mullin AM, Elovitz MA, Montoya-Williams D, Lorch SA, Burris HH. Changes in preterm birth phenotypes and stillbirth at 2 Philadelphia hospitals during the SARS-CoV-2 pandemic, March-June 2020. JAMA 2020 Dec 7. [Epub ahead of print]. doi: 10.1001/jama.2020.20991 [DOI] [PMC free article] [PubMed] [Google Scholar]