Abstract
Older age and cardiovascular comorbidities are well-known risk factors for all-cause mortality in patients with coronavirus disease 2019 (COVID-19). Hypertension and age are the 2 principal determinants of arterial stiffness (AS). This study aimed to estimate AS in patients with COVID-19 requiring hospitalization and analyze its association with all-cause in-hospital mortality. This observational, retrospective, multicenter cohort study analyzed 12 170 patients admitted to 150 Spanish centers included in the SEMI-COVID-19 Network. We compared AS, defined as pulse pressure ≥60 mm Hg, and clinical characteristics between survivors and nonsurvivors. Mean age was 67.5 (±16.1) years and 42.5% were women. Overall, 2606 (21.4%) subjects died. Admission systolic blood pressure (BP) <120 and ≥140 mm Hg was a predictor of higher all-cause mortality (23.5% and 22.8%, respectively, P<0.001), compared with systolic BP between 120 and 140 mm Hg (18.6%). The 4379 patients with AS (36.0%) were older and had higher systolic and lower diastolic BP. Multivariate analysis showed that AS and systolic BP <120 mm Hg significantly and independently predicted all-cause in-hospital mortality (adjusted odds ratio [ORadj]: 1.27, P=0.0001; ORadj: 1.48, P=0.0001, respectively) after adjusting for sex (males, ORadj: 1.6, P=0.0001), age tertiles (second and third tertiles, ORadj: 2.0 and 4.7, P=0.0001), Charlson Comorbidity Index (second and third tertiles, ORadj: 4.8 and 8.6, P=0.0001), heart failure, and previous and in-hospital antihypertensive treatment. Our data show that AS and admission systolic BP <120 mm Hg had independent prognostic value for all-cause mortality in patients with COVID-19 requiring hospitalization.
Keywords: arterial stiffness, blood pressure, COVID-19, heart failure, hypertension, pulse pressure
The coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 has emerged as a worldwide pandemic of unexpected severity. Initial symptoms usually affect the respiratory system and include fever, cough, and hypoxia. However, there is growing evidence that COVID-19 is actually a classic multisystem disease with a plethora of different signs and symptoms, among which cardiovascular manifestations predominate.1
Of the epidemiological connections between COVID-19 and the arterial system, 3 are the most notable. First, hypertension invariably ranks in first place among baseline comorbidities in patients with COVID-19.2 Second, although data are scarce and controversial,3 hypertension seems to represent an independent and significant determinant of all-cause mortality in patients hospitalized with COVID-19.4 Third, age is indisputably the risk factor most strongly associated with worse outcomes in patients with COVID-19.5 Long before the COVID-19 pandemic began, arterial stiffness (AS) was a concept that unified the long-term impact of these 2 components on the cardiovascular system: hypertension and aging. It was originally interpreted as a marker of changes in the aortic wall and was thought to reflect underlying arteriosclerosis on multiple levels.6 Obesity, diabetes, smoking, and especially subclinical inflammation have been linked to pathological AS, but the 2 main determinants of AS are blood pressure (BP) and age, leading to the assertion that AS should be recognized as the best marker of vascular aging.7 Current guidelines for the management of hypertension include AS among the many tools for assessing hypertension-mediated organ damage because it has shown independent prognostic value beyond the commonly used risk tables.8
Carotid-femoral pulse wave velocity by applanation tonometry is the gold standard for measuring large-artery stiffness.9 Although several techniques have been developed in recent years to estimate AS on a population scale,10 daily use of pulse wave velocity measurement requires training and time and is, therefore, not recommended for routine practice. A practical, simple, and proven alternative approach to estimate the burden of AS in large populations is the calculation of pulse pressure (PP; systolic BP−diastolic BP). Values above 60 mm Hg have been shown to correlate significantly with AS, especially in older people, and its use as marker of AS is widely endorsed in the literature.11,12
We hypothesize that AS would be pathologically increased in patients with COVID-19 because they share the 2 principal risk factors: old age and hypertension. The objective of this study is to estimate AS by calculating the PP of patients with COVID-19 requiring hospital admission and analyze its association with all-cause mortality. The secondary objective is to characterize patients with AS who are included in the Spanish Society of Internal Medicine (SEMI)-COVID-19 Network database.
Material and Methods
Study Design and Population
Our study is based on the SEMI-COVID-19 Registry, an ongoing multicenter, nationwide, observational cohort database in which 150 hospitals in all 17 regions of Spain participate. Further information on the registry and its data collection methods can be found in the source article.13 The data that support the findings of this study are available from the corresponding author upon reasonable request. Inclusion criteria for the registry were age ≥18 years and first admission to a hospital in Spain with diagnosis of COVID-19 confirmed microbiologically by reverse transcription polymerase chain reaction testing of a nasopharyngeal sample, following the recommendations of the World Health Organization. The exclusion criteria were declining to participate, withdrawal of informed consent, or subsequent admissions of the same patient. Patients were admitted and treated according to the clinical judgment of the attending physicians, following local protocols and the recommendations of the Spanish Ministry of Health. Personal data management strictly complied with Spanish Law 14/2007, of July 3, on Biomedical Research and Regulation (EU) 2016/679 of the European Parliament and with the Council of April 27, 2016, on the protection of natural persons with regard to the processing of personal data and on the free movement of such data. The SEMI-COVID-19 Registry has been approved by the Provincial Research Ethics Committee of Malaga (Spain), following the recommendation of the Spanish Agency of Medicines and Medical Products (AEMPS, for its initials in Spanish). All the patients gave informed consent. From March 1 to June 24, 2020, when the last patient was included in this substudy, 13 121 consecutive patients aged between 18 and 106 years were recruited.
Hypertension was included among the list of variables recorded, along with previous and in-hospital use of ACE (angiotensin-converting enzyme) inhibitors and ARBs (angiotensin receptor blockers).
Procedures
At least one physician from the internal medicine department in each hospital is voluntarily in charge of collecting and entering patients’ data from their medical record in an online electronic data capture system developed by the Spanish Society of Internal Medicine (SEMI, for its initials in Spanish). A database manager (Dr Ramos Rincón) centrally verifies procedures and incoming data from all hospitals. An independent external agency together with the study’s scientific steering committee is responsible for database monitoring. Dissociated patient identifiable data are pseudo-anonymized to avoid direct identifiers. All information is fully encrypted through a valid Transport Layer Security certificate and hosted on a secure server.
The database includes almost 300 variables under the following headings: (1) inclusion criteria; (2) epidemiological data; (3) reverse transcription polymerase chain reaction and serology data; (4) personal medical and medication history, including antihypertensive treatment, categorized as ACEIs, ARBs, or others; (5) symptoms and physical examination findings at admission; (6) laboratory (blood gases, metabolic panel, complete blood count, coagulation) and diagnostic imaging tests; (7) additional data at seven days after admission or at admission to the intensive care unit; (8) pharmacological treatment during the hospitalization and ventilator support; (9) complications during the hospitalization; and (10) progress after discharge and 30 days from diagnosis. The age-adjusted Charlson Comorbidity Index was calculated from the data collected.14 A complete list of variables can be found in the source article.13 The primary end point was all-cause in-hospital mortality versus hospital discharge. The time of follow-up was defined as the period from admission to discharge or death. Mortality is expressed as the case fatality rate.
Statistical Analysis
Continuous variables were tested for normal distribution using Kolmogorov-Smirnov test. Results are shown as means (SD) or medians (25th–75th percentile) for continuous variables and absolute values (%) for categorical variables.
To compare baseline demographic and clinical characteristics among the different groups, we used ANOVA or the Kruskal–Wallis test for continuous variables. Differences in proportion were analyzed using the χ2 test. Systolic BP (SBP) was divided into 3 categories: SBP <120 mm Hg, SBP ≥120 and simultaneously SBP <140 mm Hg, and SBP ≥140 mm Hg. The middle range group will be noted as 120≤ SBP <140. Hypertension was categorized as absent or present, and the latter was further subcategorized into 3 groups based on treatment received: (1) no ACEIs/ARBs, (2) ACEIs, and (3) ARBs. AS was defined as present when PP (systolic minus diastolic BP) was ≥60 mm Hg. The association between AS and death was analyzed using Kaplan-Meier survival curves; the log-rank test was calculated from baseline to time of death according to the presence or absence of AS. We used a logistic regression to evaluate the relationship between significant variables found on the univariate analysis and all-cause mortality; variables with P<0.1 on the univariate analysis were included. All statistical analyses were performed using SPSS software (IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp). A 2-tailed P<0.05 was considered statistically significant.
Results
Demographic Characteristics of the Study Population
A total of 13 121 records were collected in the SEMI-COVID-19 Registry at June 24, 2020, of which 951 were excluded due to missing information on certain key variables. A total of 12 170 (92.8%) subjects were included in this substudy, as can be seen in the patient flowchart in Figure 1. Table 1 includes the baseline demographic and clinical features of all participants and according to the presence or absence of AS. The mean age of the total group was 67.5±16.1 years and 42.5% were women. The vast majority of patients were White (90.0%), followed by patients of Latin American origin (8.2%). The data presented only include patients who were hospitalized and either discharged or died: 72.7% were discharged home, 5.9% continued their recovery in health care institutions outside the hospitals, and 21.4% died. This proportion of deaths is consistent with official data from the Spanish Ministry of Health as of May 29, 2020 (20 534 deaths among 99 808 hospitalized patients, 20.6%).15 The most prevalent terminal complications of patients with COVID-19 with fatal outcome was adult respiratory distress syndrome (76.8%), followed at a considerable distance by acute renal failure (36.0%), multiorgan failure (26.6%), secondary bacterial pneumonia (22.1%), sepsis (20.1%), shock (15.9%), heart failure (HF, 14.7%), and cardiac arrhythmia (9.3%). Disseminated intravascular (3.4%), myocarditis (2.5%), acute coronary disease (2.3%), pulmonary embolism (1.9%), and stroke (1.7%) were also present but far more rare.
Figure 1.
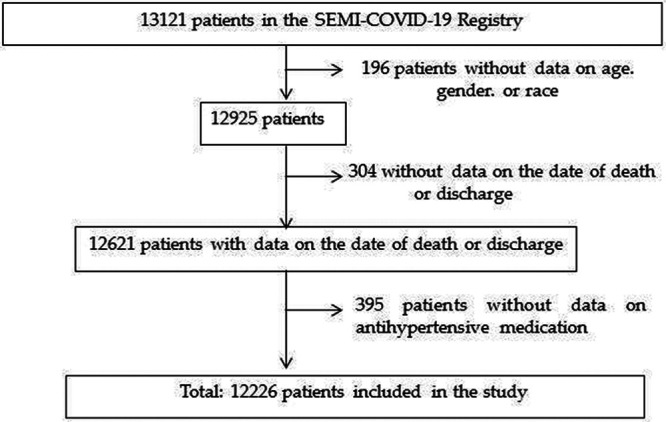
Patient inclusion flow chart. COVID-19 indicates coronavirus disease 2019.
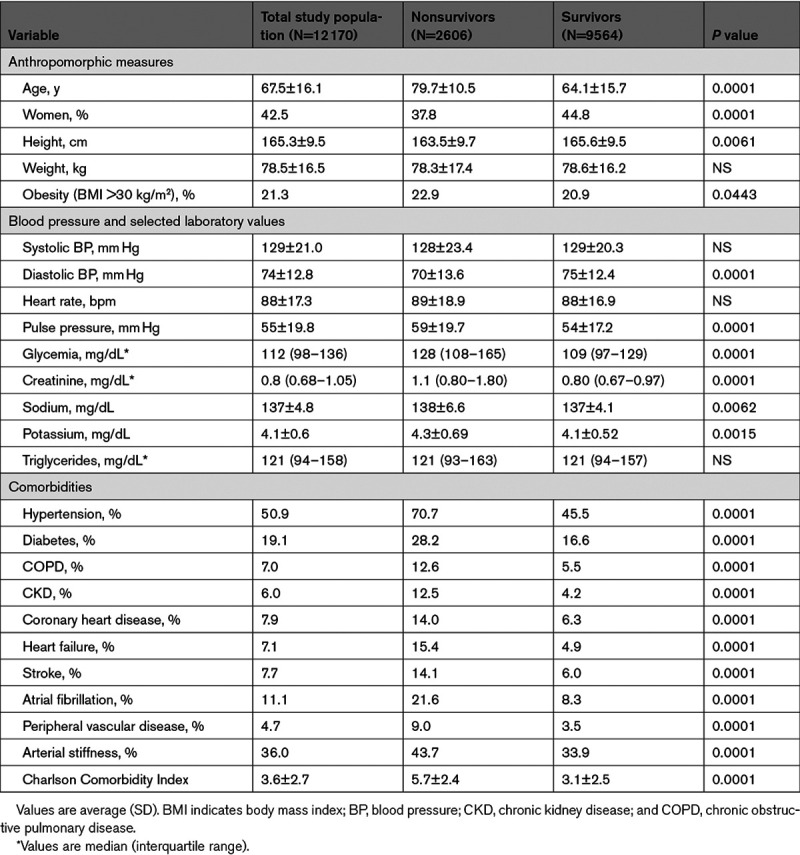
Table 1.
Demographic and Baseline Clinical Features of the Study Population in General and According to the Presence or Absence of Arterial Stiffness
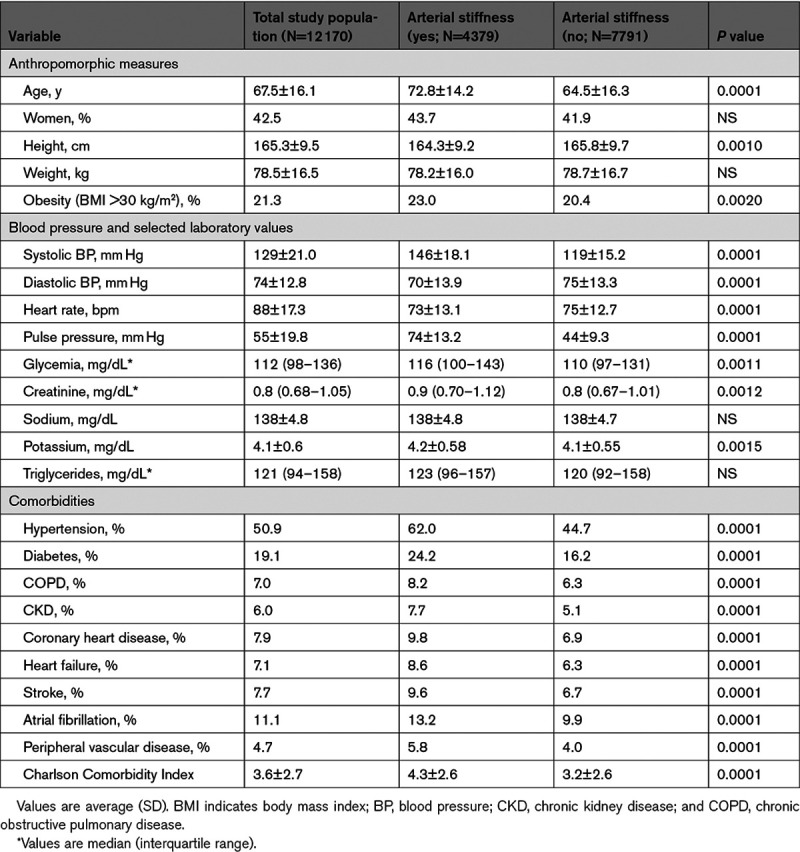
As shown in Table 1, hypertension was the most frequent comorbidity (50.9%) in patients with COVID-19, followed by diabetes (19.1%), atrial fibrillation (11.1%), coronary heart disease (7.9%), stroke (7.7%), heart failure (HF; 7.1%), chronic obstructive pulmonary disease (COPD; 7.0%), chronic kidney disease (CKD; 6.0%), and peripheral arterial disease (4.7%). After sorting the population by presence or absence of AS, the data show that age, SBP and the Charlson Comorbidity Index score were markedly higher and diastolic BP lower in the former group compared with the latter. All the comorbidities analyzed were, without exception, far more frequent in patients with AS. We found small albeit significant differences in certain laboratory parameters.
Outcomes
Kaplan-Meier survival curves (Figure 2) according to presence or absence of AS confirm increased all-cause mortality in subjects with AS compared with those without AS (log-rank P<0.001). A noteworthy finding is that the difference in survival can be detected from the very beginning, and the rate shows a tendency to converge at the end of the observation period.
Figure 2.
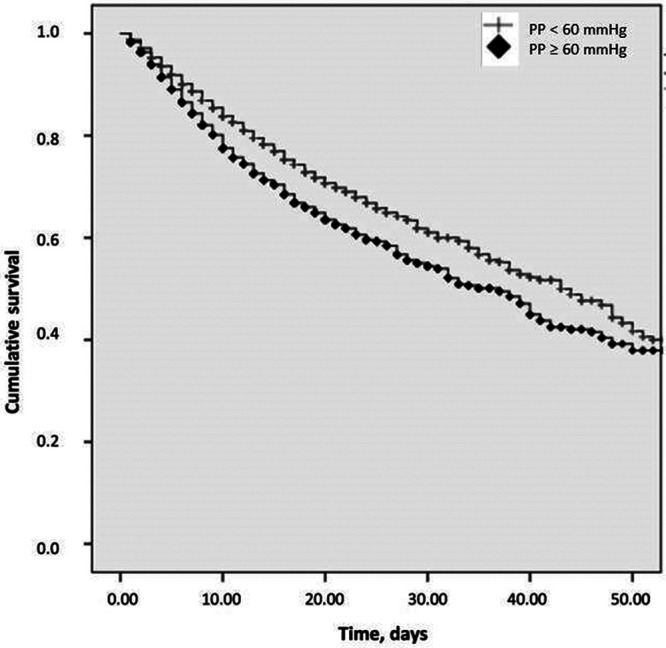
Kaplan-Meier curves in patients with/without arterial stiffness (AS). Log rank P<0.001. PP indicates pulse pressure.
Given the marked differences in SBP according to the presence/absence of AS, we focused on the association between all-cause in-hospital mortality, SBP, and AS. A graphical representation of the findings can be seen in Figure 3. The lowest mortality rate was found in patients with SBP between 120 and 140 mm Hg while worse outcomes significantly increased when SBP was below 120 or exceeded 140 mm Hg (black columns), resembling a J-curve phenomenon. No significant differences were found between the group of patients with SBP <120 and SBP ≥140 mm Hg. When dividing each SBP category into 2 groups according to PP <60 mm Hg (horizontally striped bars) or PP ≥60 mm Hg (diagonally striped bars), it is observed that patients with AS constantly presented with a significantly higher all-cause mortality than those with PP <60 mm Hg across all 3 BP categories. In other words, within each BP group PP ≥60 mm Hg was always associated with higher mortality than PP <60 mm Hg.
Figure 3.
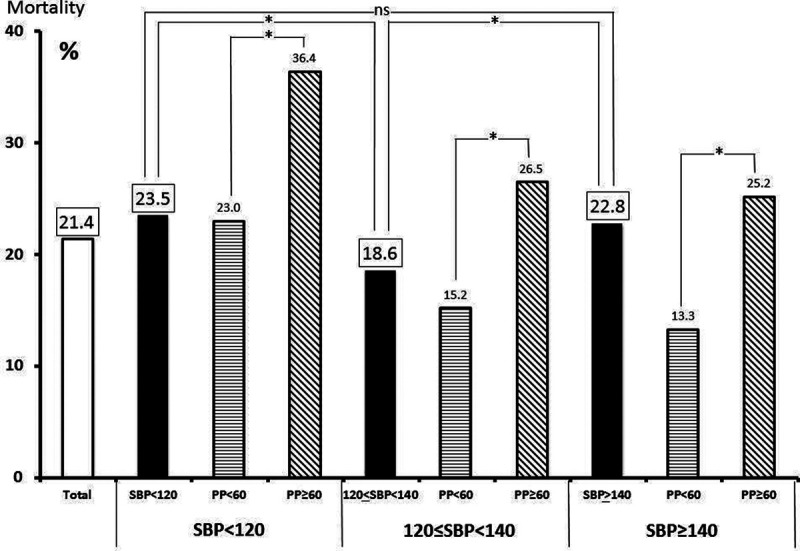
All-cause in-hospital mortality according to systolic blood pressure (SBP) at hospital admission and presence (pulse pressure [PP] ≥60 mm Hg) or absence (PP <60 mm Hg) of arterial stiffness. *P<0.0001.
All-Cause in-Hospital Mortality According to Selected Variables
Table 2 analyzes the baseline differences between survivors and nonsurvivors. It shows that nonsurvivors were older; predominantly male; more fragile; and with a higher proportion of previous chronic diseases, especially hypertension but also AS. Paradoxically, no significant difference was detected in SBP, but diastolic BP was decreased and PP increased in nonsurvivors. Again, significant differences in selected laboratory variables were observed, especially in glycemia, but they were small differences and likely of little clinical relevance.
Table 2.
Baseline Demographic and Clinical Features of the Study Population According to All-Cause Mortality
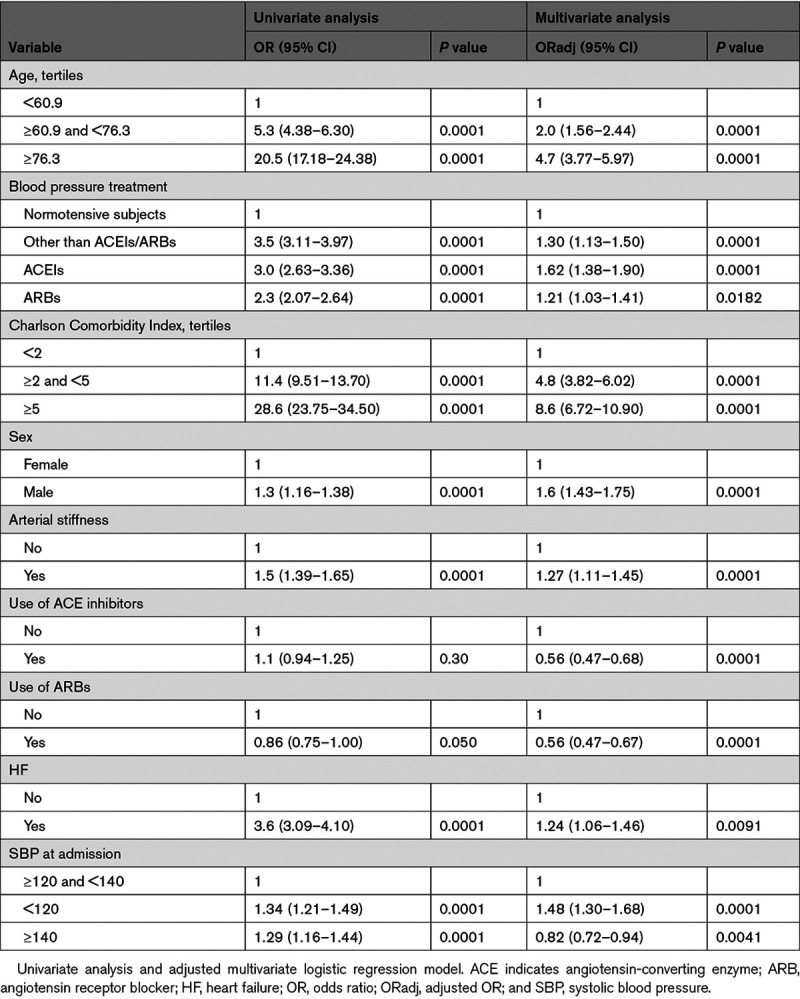
Subsequently, we performed a multivariate stepwise logistic regression analysis using all covariates with a significant (P<0.1) association with all-cause mortality as dependent variables (Table 3). The 2 main factors independently predicting death were the Charlson Comorbidity Index score and age. Male sex and HF were significant determinants; atrial fibrillation and CKD had a borderline significance (P=0.057 and P=0.070, respectively); and diabetes, COPD, and peripheral arterial disease were not significant and thus were not included in the multivariate equation. In terms of BP-related variables, treatment of preexisting hypertension continued to be an independently significant risk factor and ACEIs and ARBs as in-hospital antihypertensive treatment remained variables with a beneficial predictive value. Likewise, presence of AS and BP below 120 mm Hg, as compared with BP between 120 and 140 mm Hg, represented significant deleterious risk factors. Interestingly, BP >140 mm Hg was found to be a protective factor, in contrast to what was found on the univariate analysis. We performed 2 further sensitivity analyses. First, we defined BP either as below or above 120 mm Hg. In this case, AS (odds ratio, 1.16 [CI, 1.03–1.31], P=0.01) and BP <120 (odds ratio, 1.54 [CI, 1.36–1.75], P=0.001) continued to be significant independent predictors of poor outcomes. Second, removing AS from the equation, BP <120 continued to be as a risk factor (odds ratio, 1.36 [CI, 1.21–1.54], P=0.001) and BP >140 ceased to have any protective effect (odds ratio, 0.92 [CI, 0.81–1.03], P=0.16). In other words, SBP >140 was protective only when simultaneously adjusting for PP. BP values below 120 mm Hg were a consistent predictor of worse outcomes whereas BP values >140 mm Hg were only significant depending on the presence of AS.
Table 3.
Association of Selected Variables With All-Cause In-Hospital Mortality as Dependent Variable
Discussion
To the best of our knowledge, this retrospective, multicenter cohort study represents one of the largest analysis of hospitalized, treated, and discharged patients with COVID-19 worldwide. We analyzed data on 12 170 patients with COVID-19 in 150 hospitals across Spain, obtaining a representative sample of the pandemic in our country. The most salient conclusion that can be drawn from our analysis is that pathological AS, estimated as PP ≥60 mm Hg at admission, can be interpreted as a deleterious risk factor with predictive value for all-cause in-hospital mortality in patients with COVID-19. This risk factor acts in addition to parameters that have been previously well-established as risk factors, such as age, fragility, sex, hypertension, and HF.4 It should be underscored that previous and in-hospital antihypertensive treatments were equally and simultaneously accounted for in this analysis and did not alter the conclusions; the former would seem to indicate that preexisting hypertension does act together with AS as an independent risk factor and the latter suggesting that treatment with either ACEIs/ARBs during the hospital stay improves outcomes by significantly decreasing all-cause mortality.
Data concerning admission BP in patients with COVID-19 are very scarce and are included, at best, as minor pieces of data in larger predictive scores. Two recent studies found an association between worse outcomes and low BP16,17 and 2 others found an association between worse outcomes and high BP.18,19 However, none focused on the capital importance of BP per se. Furthermore, to date, this is the first study linking the severity of the COVID-19 pandemic to a marker of AS, namely PP ≥60 mm Hg. The limited availability of pulse wave velocity measurement capabilities in specialized centers and the acuteness of COVID-19 cases during admission might explain why associations between AS and COVID-19 are lacking in the literature. Nonetheless, there is a plethora of evidence supporting the use of increased PP as a suitable surrogate marker of AS from before the COVID-19 pandemic20 and prospective works that include measuring pulse wave velocity in patients with COVID-19 have recently been launched.21
The starting point of our analysis was the observation that the relationship between all-cause in-hospital mortality and SBP in our patients with COVID-19 resembled a J-curve phenomenon. Optimal BP targets in hypertension are a controversial matter, with some studies favoring the principle of the lower the better,22 while others support the existence of a J-curve in regards to BP and outcomes.23,24 In fact, the optimal range of admission BP observed in our study endorses the latest recommendations found in recent guidelines: a BP between 120 and 140 mm Hg.25 Our analytical approach analyzed 3 BP categories (BP <120; 120≤ BP <140, and BP ≥140 mm Hg) and a PP threshold of ≥60 mm Hg. SBP <120 and ≥140 mm Hg reflected worse outcomes when compared with 120≤ SBP <140 mm Hg. Adjusting each group according to the presence of AS revealed that higher PP was robustly associated with increased mortality across all 3 SBP groups. Due to the fact that patients with SBP ≥140 and PP <60 mm Hg, who presented the lowest mortality rate of all patients, were numerically more frequent than those with AS, SBP ≥140 was found to be a protective factor on the multivariate analysis. In other words, higher SBP values were markers of increased risk only when PP ≥60 mm Hg. This observation is not surprising and physiologically understandable, given the fact that PP includes SBP as part of its definition. The extent that the predictive value of PP exceeds that of BP alone is a long-standing unresolved controversy.26–28
Several mechanisms may account for the role of AS in the COVID-19 pandemic. Older age has been invariably shown as the principal risk factor in the COVID-19. Aging is a process characterized by quantitative and qualitative alterations of the immune system, with an increase in proinflammatory and a decrease in anti-inflammatory cytokines resulting in a state of chronic, low-grade inflammation often referred to as immunosenescence.29 Furthermore, the COVID-19-related cytokine storm has been hypothesized to be the consequence of aging, leading to the coining of the term inflame-aging.30
On the contrary, although there is no unanimous consensus on the causal association between systemic inflammation and cardiovascular events,31 several studies have fueled interest in vasculature properties and inflammatory molecules as surrogate markers of cardiovascular risk, with contradictory results.32–35 Hypertension is the strongest modifiable risk factor for cardiovascular disease worldwide, and low-grade inflammatory components have repeatedly been identified in the pathophysiology of hypertension.36,37 The characteristic features of hypertension include premature changes in vascular function and structure that can be demonstrated earlier and are more severe than those predicted as part of the normal aging process, leading to the so-called early vascular aging.38 What is more, AS has been claimed to precede incident hypertension39 and underlie the vicious circle of arteriosclerosis and hypertension.40 A variety of mechanisms may be responsible for the association between age, inflammation, hypertension, and AS, but there is a growing body of evidence that adverse remodeling through proinflammatory signaling secondary to the angiotensin II signaling cascade with aging is of paramount importance.41,42
The strengths of our study are the large number of participants, the use of a hard end point for analysis, and previous experience in handling databases by a scientific society. Nevertheless, its retrospective design, the high proportion of White participants, the unknown real spread of COVID-19 among outpatients, the strict inclusion of patients with COVID-19 requiring hospitalization, and the indirect estimation of AS mean that our results cannot be easily extrapolated to the general population.
Perspectives
In conclusion, assessment of simple hemodynamic variables such as SBP and PP at the very beginning of hospitalization of patients with COVID-19 appears to have practical consequences on outcomes.
Sources of Funding
None.
Disclosures
None.
Acknowledgements
We gratefully acknowledge all the investigators who participate in the SEMI-COVID-19 Registry. We also thank the SEMI-COVID-19 Registry Coordinating Center, S&H Medical Science Service, for their quality control data, logistic and administrative support. The authors declare that there are no conflicts of interest.
Appendix
Members of the SEMI-COVID-19 Group:
José Manuel Casas-Rojo, José Manuel Ramos-Rincón, Carlos Lumbreras-Bermejo, Jesús Millán-Núñez-Cortés, Juan Miguel Antón-Santos, Ricardo Gómez-Huelgas, Paloma Agudo-de-Blas, Coral Arévalo-Cañas, Blanca Ayuso, José Bascuñana-Morejón, Samara Campos-Escudero, María Carnevali-Frías, Santiago Cossio-Tejido, Borja de-Miguel-Campo, Carmen Díaz-Pedroche, Raquel Diaz-Simon, Ana García-Reyne, Lucia Jorge-Huerta, Antonio Lalueza-Blanco, Jaime Laureiro-Gonzalo, Jaime Lora-Tamayo, Guillermo Maestro-de-la-Calle, Barbara Otero-Perpiña, Diana Paredes-Ruiz, Marcos Sánchez-Fernández, Javier Tejada-Montes, Xavier Corbella, Narcís Homs, Abelardo Montero, Jose María Mora-Luján, Manuel Rubio-Rivas, Laura Abarca-Casas, Álvaro Alejandre-de-Oña, Rubén Alonso-Beato, Leyre Alonso-Gonzalo, Jaime Alonso-Muñoz, Crhistian Mario Amodeo-Oblitas, Cristina Ausín-García, Marta Bacete-Cebrián, Jesús Baltasar-Corral, Maria Barrientos-Guerrero, Alejandro Bendala-Estrada, María Calderón-Moreno, Paula Carrascosa-Fernández, Raquel Carrillo, Sabela Castañeda-Pérez, Eva Cervilla-Muñoz, Agustín Diego Chacón-Moreno, Maria Carmen Cuenca-Carvajal, Sergio de-Santos, Andrés Enríquez-Gómez, Eduardo Fernández-Carracedo, María Mercedes Ferreiro-Mazón-Jenaro, Francisco Galeano-Valle, Alejandra Garcia, Irene Garcia-Fernandez-Bravo, María Eugenia García-Leoni, Maria Gomez-Antunez, Candela González-San-Narciso, Anthony Alexander Gurjian, Lorena Jiménez-Ibáñez, Cristina Lavilla-Olleros, Cristina Llamazares-Mendo, Sara Luis-García, Víctor Mato-Jimeno, Clara Millán-Nohales, Sergio Moragón-Ledesma, Antonio Muiño-Miguez, Cecilia Muñoz-Delgado, Lucía Ordieres-Ortega, Susana Pardo-Sánchez, Alejandro Parra-Virto, María Teresa Pérez-Sanz, Blanca Pinilla-Llorente, Sandra Piqueras-Ruiz, Guillermo Soria-Fernández-Llamazares, María Toledano-Macías, Neera Toledo-Samaniego, Ana Torres-do-Rego, Maria Victoria Villalba-Garcia, Gracia Villarreal, María Zurita-Etayo, Jorge Álvarez-Troncoso, Francisco Arnalich-Fernández, Francisco Blanco-Quintana, Carmen Busca-Arenzana, Sergio Carrasco-Molina, Aranzazu Castellano-Candalija, Germán Daroca-Bengoa, Alejandro de-Gea-Grela, Alicia de-Lorenzo-Hernández, Alejandro Díez-Vidal, Carmen Fernández-Capitán, Maria Francisca García-Iglesias, Borja González-Muñoz, Carmen Rosario Herrero-Gil, Juan María Herrero-Martínez, Víctor Hontañón, Maria Jesús Jaras-Hernández, Carlos Lahoz, Cristina Marcelo-Calvo, Juan Carlos Martín-Gutiérrez, Monica Martinez-Prieto, Elena Martínez-Robles, Araceli Menéndez-Saldaña, Alberto Moreno-Fernández, Jose Maria Mostaza-Prieto, Ana Noblejas-Mozo, Carlos Manuel Oñoro-López, Esmeralda Palmier-Peláez, Marina Palomar-Pampyn, Maria Angustias Quesada-Simón, Juan Carlos Ramos-Ramos, Luis Ramos-Ruperto, Aquilino Sánchez-Purificación, Teresa Sancho-Bueso, Raquel Sorriguieta-Torre, Clara Itziar Soto-Abanedes, Yeray Untoria-Tabares, Marta Varas-Mayoral, Julia Vásquez-Manau, Jose Luis Beato-Pérez, Maria Lourdes Sáez-Méndez, María Álvarez-Bello, Ane Andrés-Eisenhofer, Ana Arias-Milla, Isolina Baños-Pérez, Laura Benítez-Gutiérrez, Javier Bilbao-Garay, Silvia Blanco-Alonso, Jorge Calderón-Parra, Alejandro Callejas-Díaz, José María Camino-Salvador, Mª Cruz Carreño-Hernández, Valentín Cuervas-Mons-Martínez, Sara de-la-Fuente-Moral, Miguel del-Pino-Jimenez, Alberto Díaz-de-Santiago, Itziar Diego-Yagüe, Ignacio Donate-Velasco, Ana María Duca, Pedro Durán-del-Campo, Gabriela Escudero-López, Esther Expósito-Palomo, Ana Fernández-Cruz, Esther Fiz-Benito, Andrea Fraile-López, Amy Galán-Gómez, Sonia García-Prieto, Claudia García-Rodríguez-Maimón, Miguel Ángel García-Viejo, Javier Gómez-Irusta, Edith Vanessa Gutiérrez-Abreu, Isabel Gutiérrez-Martín, Ángela Gutiérrez-Rojas, Andrea Gutiérrez-Villanueva, Jesús Herráiz-Jiménez, Pedro Laguna-del-Estal, Mª Carmen Máinez-Sáiz, Cristina Martín-Martín, María Martínez-Urbistondo, Fernando Martínez-Vera, Susana Mellor-Pita, Patricia Mills-Sánchez, Esther Montero-Hernández, Alberto Mora-Vargas, Cristina Moreno-López, Alfonso Ángel-Moreno-Maroto, Victor Moreno-Torres-Concha, Ignacio Morrás-De-La-Torre, Elena Múñez-Rubio, Ana Muñoz-Gómez, Rosa Muñoz-de-Benito, Alejandro Muñoz-Serrano, Jose María Palau-Fayós, Lina Marcela Parra-Ramírez, Ilduara Pintos-Pascual, Arturo José Ramos-Martín-Vegue, Antonio Ramos-Martínez, Isabel Redondo-Cánovas-del-Castillo, Alberto Roldán-Montaud, Lucía Romero-Imaz, Yolanda Romero-Pizarro, Mónica Sánchez-Santiuste, David Sánchez-Órtiz, Enrique Sánchez-Chica, Patricia Serrano-de-la-Fuente, Pablo Tutor-de-Ureta, Ángela Valencia-Alijo, Mercedes Valentín-Pastrana-Aguilar, Juan Antonio Vargas-Núñez, Jose Manuel Vázquez-Comendador, Gema Vázquez-Contreras, Carmen Vizoso-Gálvez, Gonzalo Acebes-Repiso, Uxua Asín-Samper, María Aranzazu Caudevilla-Martínez, José Miguel García-Bruñén, Rosa García-Fenoll, Jesús Javier González-Igual, Laura Letona-Giménez, Mónica Llorente-Barrio, Nicolás Alcalá-Rivera, Anxela Crestelo-Vieitez, Esther del-Corral-Beamonte, Jesús Díez-Manglano, Isabel Fiteni-Mera, Maria del Mar Garcia-Andreu, Martin Gerico-Aseguinolaza, Claudia Josa-Laorden, Raul Martínez-Murgui, Marta Teresa Matía-Sanz, Inés Armenteros-Yeguas, Javier Azaña-Gómez, Julia Barrado-Cuchillo, Irene Burruezo-López, Noemí Cabello-Clotet, Alberto E. Calvo-Elías, Elpidio Calvo-Manuel, Verónica Cano, Carmen María Cano-de-Luque, Cynthia Chocron-Benbunan, Laura Dans-Vilan, Ester Emilia Dubon-Peralta, Vicente Estrada-Pérez, Santiago Fernandez-Castelao, Marcos Oliver Fragiel-Saavedra, José Luis García-Klepzig, Maria del Rosario Iguarán-Bermúdez, Esther Jaén-Ferrer, Alejandro Maceín-Rodríguez, Rubén Ángel Martín-Sánchez, Manuel Méndez-Bailón, Sara Miguel-Álvarez, Maria José Nuñez-Orantos, Carolina Olmos-Mata, Eva Orviz-García, David Oteo-Mata, Cristina Outon-González, Juncal Perez-Somarriba, Pablo Pérez-Mateos, Maria Esther Ramos-Muñoz, Xabier Rivas-Regaira, Laura Mª Rodríguez-Gallardo, Iñigo Sagastagoitia-Fornie, Alejandro Salinas-Botrán, Miguel Suárez-Robles, Maddalena Elena Urbano, Miguel Villar-Martínez, María Aguilera-García, Ester Alonso-Monge, Jesús Álvarez-Rodríguez, Claudia Alvarez-Varela, Miquel Berniz-Gòdia, Marta Briega-Molina, Marta Bustamante-Vega, Jose Curbelo, Alicia de-las-Heras-Moreno, Ignacio Descalzo-Godoy, Alexia Constanza Espiño-Alvarez, Ignacio Fernández-Martín-Caro, Alejandra Franquet-López-Mosteiro, Gonzalo Galvez-Marquez, María J. García-Blanco, Yaiza García-del-Álamo-Hernández, Clara García-Rayo-Encina, Noemí Gilabert-González, Carolina Guillamo-Rodríguez, Nicolás Labrador-San-Martín, Manuel Molina-Báez, Carmen Muñoz-Delgado, Pedro Parra-Caballero, Javier Pérez-Serrano, Laura Rabes-Rodríguez, Pablo Rodríguez-Cortés, Carlos Rodriguez-Franco, Emilia Roy-Vallejo, Monica Rueda-Vega, Aresio Sancha-Lloret, Beatriz Sánchez-Moreno, Marta Sanz-Alba, Jorge Serrano-Ballester, Alba Somovilla, Carmen Suarez-Fernández, Macarena Vargas-Tirado, Almudena Villa-Marti, Alicia Alonso-Álvarez, Olaya Alonso-Juarros, Ariadna Arévalo-López, Carmen Casariego-Castiñeira, Ana Cerezales-Calviño, Marta Contreras-Sánchez, Ramón Fernández-Varela, Santiago J. Freire-Castro, Ana Padín-Trigo, Rafael Prieto-Jarel, Fátima Raad-Varea, Ignacio Ramil-Freán, Laura Ramos-Alonso, Francisco Javier Sanmartín-Pensado, David Vieito-Porto, Judit Aranda-Lobo, Jose Loureiro-Amigo, Isabel Oriol-Bermúdez, Melani Pestaña-Fernández, Nicolas Rhyman, Nuria Vázquez-Piqueras, Maria del Carmen Beceiro-Abad, Maria Aurora Freire-Romero, Sonia Molinos-Castro, Emilio Manuel Paez-Guillan, María Pazo-Nuñez, Paula Maria Pesqueira-Fontan, Juan Alberto Aguilera-Ayllón, Arturo Artero, María del Mar Carmona-Martín, María José Fabiá-Valls, Maria de Mar Fernández-Garcés, Ana Belén Gómez-Belda, Ian López-Cruz, Manuel Madrazo-López, Elisabeth Mateo-Sanchis, Jaume Micó-Gandia, Laura Piles-Roger, Adela Maria Pina-Belmonte, Alba Viana-García, Ana María Álvarez-Suárez, Carlos Delgado-Vergés, Rosa Fernandez-Madera-Martínez, Eva Fonseca-Aizpuru, Alejandro Gómez-Carrasco, Cristina Helguera-Amezua, Juan Francisco López-Caleya, María del Mar Martínez-López, Aleida Martínez-Zapico, Carmen Olabuenaga-Iscar, María Luisa Taboada-Martínez, Lara María Tamargo-Chamorro, Luis Fernando Abrego-Vaca, Ana Andréu-Arnanz, Octavio Arce-García, Marta Bajo-González, Pablo Borque-Sanz, Alberto Cozar-Llisto, Sonia de-Pedro-Baena, Beatriz Del-Hoyo-Cuenda, María Alejandra Gamboa-Osorio, Isabel García-Sánchez, Andrés González-García, Oscar Alberto López-Cisneros, Miguel Martínez-Lacalzada, Borja Merino-Ortiz, Jimena Rey-García, Elisa Riera-González, Cristina Sánchez-Díaz, Grisell Starita-Fajardo, Cecilia Suárez-Carantoña, Adrian Viteri-Noel, Svetlana Zhilina-Zhilina, Sonia Casallo-Blanco, Jeffrey Oskar Magallanes-Gamboa, Carlos Aldasoro-Frias, Luis Arribas-Perez, María Esther Fraile-Villarejo, Beatriz Garcia-Lopez, Victor Madrid-Romero, Emilia Martínez-Velado, Victoria Palomar-Calvo, Sara Pintos-Otero, Carlota Tuñón-de-Almeida, Ana Maria Alguacil-Muñoz, Marta Blanco-Fernández, Veronica Cano, Ricardo Crespo-Moreno, Fernando Cuadra-Garcia-Tenorio, Blanca Díaz-Tendero-Nájera, Raquel Estévez-González, María Paz García-Butenegro, Alberto Gato-Díez, Verónica Gómez-Caverzaschi, Piedad María Gómez-Pedraza, Julio González-Moraleja, Raúl Hidalgo-Carvajal, Patricia Jiménez-Aranda, Raquel Labra-González, Áxel Legua-Caparachini, Pilar Lopez-Castañeyra, Agustín Lozano-Ancin, Jose Domingo Martin-Garcia, Cristina Morata-Romero, María Jesús Moya-Saiz, Helena Moza-Moríñigo, Gemma Muñiz-Nicolás, Enriqueta Muñoz-Platon, Filomena Oliveri, Elena Ortiz-Ortiz, Raúl Perea-Rafael, Pilar Redondo-Galán, María Antonia Sepulveda-Berrocal, Vicente Serrano-Romero-de-Ávila, Pilar Toledano-Sierra, Yamilex Urbano-Aranda, Jesús Vázquez-Clemente, Carmen Yera-Bergua, Ana Belén Barbero-Barrera, Coralia Bueno-Muiño, Ruth Calderón-Hernaiz, Irene Casado-Lopez, Andrés Cortés-Troncoso, Mayte de-Guzmán-García-Monge, Francesco Deodati, Gonzalo García-Casasola-Sánchez, Elena Garcia-Guijarro, Davide Luordo, María Mateos-González, Jose A Melero-Bermejo, Lorea Roteta-García, Elena Sierra-Gonzalo, Javier Villanueva-Martínez, Mª Mar Ayala-Gutiérrez, Rosa Bernal-López, José Bueno-Fonseca, Verónica Andrea Buonaiuto, Luis Francisco Caballero-Martínez, Lidia Cobos-Palacios, Clara Costo-Muriel, Francis de-Windt, Ana Teresa Fernandez-Truchaud-Christophel, Paula García-Ocaña, Javier Gorospe-García, Maria Dolores López-Carmona, Pablo López-Quirantes, Almudena López-Sampalo, Elizabeth Lorenzo-Hernández, Juan José Mancebo-Sevilla, Jesica Martin-Carmona, Luis Miguel Pérez-Belmonte, Araceli Pineda-Cantero, Carlos Romero-Gómez, Michele Ricci, Jaime Sanz-Cánovas, Marisa Asensio-Tomás, David Balaz, David Bonet-Tur, Ruth Cañizares-Navarro, Paloma Chazarra-Pérez, Jesús Corbacho-Redondo, Leticia Espinosa-Del-Barrio, Pedro Jesús Esteve-Atiénzar, Carles García-Cervera, David Francisco García-Núñez, Vicente Giner-Galvañ, Angie Gómez-Uranga, Javier Guzmán-Martínez, Isidro Hernández-Isasi, Lourdes Lajara-Villar, Verónica Martínez-Sempere, Juan Manuel Núñez-Cruz, Sergio Palacios-Fernández, Juan Jorge Peris-García, Andrea Riaño-Pérez, José Miguel Seguí-Ripoll, Azucena Sempere-Mira, Philip Wikman-Jorgensen, Nicolás Jiménez-García, Jairo Luque-del-Pino, María Dolores Martín-Escalante, Jesús Ballano-Rodríguez-Solís, Luis Cabeza-Osorio, María del Pilar Fidalgo-Montero, Mª Isabel Fuentes-Soriano, Erika Esperanza Lozano-Rincon, Ana Martín-Hermida, Jesus Martinez-Carrilero, Jose Angel Pestaña-Santiago, Manuel Sánchez-Robledo, Patricia Sanz-Rojas, Nahum Jacobo Torres-Yebes, Vanessa Vento, Dafne Cabañero, María Calabuig-Ballester, Pascual Císcar-Fernández, Ricardo Gil-Sánchez, Marta Jiménez-Escrig, Cristina Marín-Amela, Laura Parra-Gómez, Carlos Puig-Navarro, José Antonio Todolí-Parra, Raquel Aranega-González, Ramon Boixeda, Javier Fernández-Fernández, Carlos Lopera-Mármol, Marta Parra-Navarro, Ainhoa Rex-Guzmán, Aleix Serrallonga-Fustier, Diana Alegre-González, Irene Ariño-Pérez-de-Zabalza, Sergio Arnedo-Hernández, Jorge Collado-Sáenz, Beatriz Dendariena, Marta Gómez-del-Mazo, Iratxe Martínez-de-Narvajas-Urra, Sara Martínez-Hernández, Estela Menendez-Fernández, Jose Luís Peña-Somovilla, Elisa Rabadán-Pejenaute, Raquel Fernández-González, Amara Gonzalez-Noya, Carlos Hernández-Ceron, Isabel Izuzquiza-Avanzini, Ana Latorre-Diez, Pablo López-Mato, Ana María Lorenzo-Vizcaya, Daniel Peña-Benítez, Milagros María Peña-Zemsch, Lucía Pérez-Expósito, Marta Pose-Bar, Lara Rey-González, Laura Rodrigo-Lara, Antonio Pablo Arenas-de-Larriva, Pilar Calero-Espinal, Javier Delgado-Lista, Francisco Fuentes-Jiménez, María Jesús Gómez-Vázquez, Jose Jiménez-Torres, José López-Miranda, Laura Martín-Piedra, Javier Pascual-Vinagre, Pablo Pérez-Martinez, María Elena Revelles-Vílchez, Juan Luis Romero-Cabrera, José David Torres-Peña, Francisco Javier Bejarano-Luque, Francisco Javier Carrasco-Sánchez, Mercedes de-Sousa-Baena, Jaime Díaz-Leal, Aurora Espinar-Rubio, Maria Franco-Huertas, Juan Antonio García-Bravo, Andrés Gonzalez-Macías, Encarnación Gutiérrez-Jiménez, Alicia Hidalgo-Jiménez, Constantino Lozano-Quintero, Carmen Mancilla-Reguera, Francisco Javier Martínez-Marcos, Francisco Muñoz-Beamud, Maria Perez-Aguilera, Alícia Perez-Jiménez, Virginia Rodríguez-Castaño, Alvaro Sánchez-de-Alcazar-del-Río, Leire Toscano-Ruiz, Begoña Cortés-Rodríguez, María Esther Guisado-Espartero, Lorena Montero-Rivas, Maria de la Sierra Navas-Alcántara, Raimundo Tirado-Miranda, Hortensia Alvarez-Diaz, Tamara Dalama-Lopez, Estefania Martul-Pego, Carmen Mella-Pérez, Ana Pazos-Ferro, Sabela Sánchez-Trigo, Dolores Suarez-Sambade, Maria Trigas-Ferrin, Maria del Carmen Vázquez-Friol, Laura Vilariño-Maneiro, Rosario Maria García-Diez, Manuel Martin-Regidor, Angel Luis Martínez-Gonzalez, Alberto Muela-Molinero, Raquel Rodríguez-Díez, Beatriz Vicente-Montes, Javier Ena, Jose Enrique Gómez-Segado, Luis Felipe Díez-García, Iris El-Attar-Acedo, Bárbara Hernandez-Sierra, Carmen Mar Sánchez-Cano, Yolanda Casillas-Viera, Lucía Cayuela-Rodríguez, Carmen de-Juan-Alvarez, Gema Flox-Benitez, Laura García-Escudero, Juan Martin-Torres, Patricia Moreira-Escriche, Susana Plaza-Canteli, M Carmen Romero-Pérez, Rafael Aragon-Lara, Inmaculada Cimadevilla-Fernandez, Juan Carlos Cira-García, Gema Maria García-García, Julia Gonzalez-Granados, Beatriz Guerrero-Sánchez, Francisco Javier Monreal-Periáñez, Maria Josefa Pascual-Perez, José Nicolás Alcalá-Pedrajas, Antonia Márquez-García, Inés Vargas, Ana Suarez-Lombraña, Sara Fuente-Cosío, César Manuel Gallo-Álvaro, Julia Lobo-García, Antía Pérez-Piñeiro, Anyuli Gracia-Gutiérrez, Leticia Esther Royo-Trallero, Francisco Amorós-Martínez, Erika Ascuña-Vásquez, José Carlos Escribano-Stablé, Adriana Hernández-Belmonte, Ana Maestre-Peiró, Raquel Martínez-Goñi, M.Carmen Pacheco-Castellanos, Bernardino Soldan-Belda, David Vicente-Navarro, Alba Camarena-Molina, Simona Cioaia, Anna Ferrer-Santolalia, José María Frutos-Pérez, Eva Gil-Tomás, Leyre Jorquer-Vidal, Marina Llopis-Sanchis, M Ángeles Martínez-Pascual, Alvaro Navarro-Batet, Mari Amparo Perea-Ribis, Ricardo Peris-Sanchez, José Manuel Querol-Ribelles, Silvia Rodriguez-Mercadal, Ana Ventura-Esteve, Jorge Andrés Soler, Marián Bennasar-Remolar, Alejandro Cardenal-Álvarez, Daniela Díaz-Carlotti, María José Esteve-Gimeno, Sergio Fabra-Juana, Paula García-López, María Teresa Guinot-Soler, Daniela Palomo-de-la-Sota, Guillem Pascual-Castellanos, Ignacio Pérez-Catalán, Celia Roig-Martí, Paula Rubert-Monzó, Javier Ruiz-Padilla, Nuria Tornador-Gaya, Jorge Usó-Blasco, Gloria María Alonso-Claudio, Víctor Barreales-Rodríguez, Cristina Carbonell-Muñoz, Adela Carpio-Pérez, María Victoria Coral-Orbes, Daniel Encinas-Sánchez, Sandra Inés Revuelta, Miguel Marcos-Martín, José Ignacio Martín-González, José Ángel Martín-Oterino, Leticia Moralejo-Alonso, Sonia Peña-Balbuena, María Luisa Pérez-García, Ana Ramon-Prados, Beatriz Rodríguez-Alonso, Ángela Romero-Alegría, Maria Sanchez-Ledesma, Rosa Juana Tejera-Pérez, Pablo Guisado-Vasco, Ana Roda-Santacruz, Ana Valverde-Muñoz, Jon Cabrejas-Ugartondo, Ana Belén Mancebo-Plaza, Arturo Noguerado-Asensio, Bethania Pérez-Alves, Natalia Vicente-López, Ana Alberich-Conesa, Maricruz Almendros-Rivas, Miquel Hortos-Alsina, Jorge Marchena-Romero, Anabel Martin-Urda-Diez-Canseco, Francisco Epelde, Isabel Torrente, Virginia Herrero-García, Berta Román-Bernal, Mª José Esteban-Giner, Xjoylin Teresita Egües-Torres, Sara Gutiérrez-González, Cristina Novoa-Fernández, Pablo Tellería-Gómez, José López-Castro, Manuel Lorenzo López-Reboiro, Thamar Capel-Astrua, Paola Tatiana Garcia-Giraldo, Maria Jesús González-Juárez, Victoria Marquez-Fernandez, Ada Viviana Romero-Echevarry, Vanesa Alende-Castro, Ana María Baz-Lomba, Ruth Brea-Aparicio, Marta Fernandez-Morales, Jesús Manuel Fernández-Villar, María Teresa López-Monteagudo, Cristina Pérez-García, Lorena Rodríguez-Ferreira, Diana Sande-Llovo, Maria Begoña Valle-Feijoo, Marta Aguilar, Amparo Albert, Alberto Belda, Noemi Beltran, Sergio Canales, Amparo Carmena, Marta Catalan, Xavier Cortes, Ruben Cuesta, Maria Dolores Domenech, Monica Fernandez, Maria Amparo Fernandez, Angela Gago, Ana Garayoa, Miguel Garcia, Marta Garijo, Monica Gimenez, Jose Gonzalvo, Iratxe Jimenez, Celia Julia, Zineb Karroud-Zamrani, Amparo Lloris, Tamara Malek, Jose Mendez, Andrea Mendizabal, José Ramón Moles, Santiago Morro, Angela Nicolas, Marta Palop, Jose Maria Pascual-Izuel, Vicente Peset, Jorge Pinel, Anastasio Quesada, Marta Quilis, Sandra Reino, Bianca Ridaura, Enrique Rodilla-Sala, Alicia Roldan, Maria Carmen Saez, Inmaculada Salvador, Vanesa Sanchez, Laura Sanchis, Alberto Saura, Raquel Segovia, Julio Vicente.
Footnotes
Nonstandard Abbreviation and Acronyms
- ACE
- angiotensin-converting enzyme
- ARB
- angiotensin receptor blocker
- AS
- arterial stiffness
- BP
- blood pressure
- COVID-19
- coronavirus disease 2019
- PP
- pulse pressure
- SBP
- systolic BP
A list of all SEMI-COVID-19 Network members is given in the Appendix.
For Sources of Funding and Disclosures, see page 864.
Contributor Information
Maria Dolores López-Carmona, Email: mdlcorreo@gmail.com.
Xavi Cortes, Email: xacori@gmail.com.
Lidia Cobos-Palacios, Email: cobospalacios@gmail.com.
Sergio Canales, Email: sergiocanalesperez@hotmail.com.
Samara Campos Escudero, Email: samara.campos1990@gmail.com.
Manuel Rubio-Rivas, Email: manuel.lorenzo.lopez.reboiro@sergas.es.
Jesus Díez Manglano, Email: jdiez@aragon.es.
Santiago J. Freire Castro, Email: santiago.freire.castro@sergas.es.
Nuria Vázquez Piqueras, Email: nvazquezpiqueras@gmail.com.
Elisabeth Mateo Sanchis, Email: mateo.elisabet@gmail.com.
Paula Maria Pesqueira Fontan, Email: paulapesqueira@hotmail.com.
Jeffrey Oskar Magallanes Gamboa, Email: dr990112@hotmail.com.
Andrés González García, Email: andres_gonzalez_garcia@hotmail.com.
Victor Madrid Romero, Email: vmadridromero@gmail.com.
Lara Tamargo Chamorro, Email: laratamargo@hotmail.es.
Julio González Moraleja, Email: juliogmoraleja@gmail.com.
Javier Villanueva Martínez, Email: jvillam89@gmail.com.
Amara González Noya, Email: amara.gonzalez.noya@sergas.es.
Ana Suárez-Lombraña, Email: anasuarezlombrana@gmail.com.
Anyuli Gracia Gutiérrez, Email: agraciagut@gmail.com.
José Manuel Ramos Rincón, Email: jramosrincon@yahoo.es.
Ricardo Gómez Huelgas, Email: ricardogomezhuelgas@hotmail.com.
Novelty and Significance
What Is New?
Arterial stiffness, estimated as admission pulse pressure ≥60 mm Hg, was associated with higher risk for all-cause mortality in patients hospitalized with coronavirus disease 2019 (COVID-19).
What Is Relevant?
This association was independent of other comorbidities, gender, age, and the presence of hypertension or antihypertensive treatment.
Summary
Elevated pulse pressure and blood pressure values <120 mm Hg at admission contribute independently to the high all-cause mortality in patients with COVID-19.
References
- 1.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, Cereda D, Coluccello A, Foti G, Fumagalli R, et al. ; COVID-19 Lombardy ICU Network. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the lombardy region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang W, Liang H, Ou L, Chen B, Chen A, Li C, Li Y, Guan W, Sang L, Lu J, et al. ; China Medical Treatment Expert Group for COVID-19. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern Med. 2020;180:1081–1089. doi: 10.1001/jamainternmed.2020.2033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iaccarino G, Grassi G, Borghi C, Ferri C, Salvetti M, Volpe M; SARS-RAS Investigators. Age and multimorbidity predict death among COVID-19 patients: results of the SARS-RAS study of the Italian society of hypertension. Hypertension. 2020;76:366–372. doi: 10.1161/HYPERTENSIONAHA.120.15324 [DOI] [PubMed] [Google Scholar]
- 4.Rodilla E, Saura A, Jiménez I, Mendizábal A, Pineda-Cantero A, Lorenzo-Hernández E, Fidalgo-Montero MDP, López-Cuervo JF, Gil-Sánchez R, Rabadán-Pejenaute E, et al. Association of hypertension with all-cause mortality among hospitalized patients with COVID-19. J Clin Med. 2020;9:3136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, et al. ; China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, et al. 2007 Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2007;28:1462–1536. doi: 10.1093/eurheartj/ehm236 [DOI] [PubMed] [Google Scholar]
- 7.Olsen MH, Angell SY, Asma S, Boutouyrie P, Burger D, Chirinos JA, Damasceno A, Delles C, Gimenez-Roqueplo AP, Hering D, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the lancet commission on hypertension. Lancet. 2016;388:2665–2712. doi: 10.1016/S0140-6736(16)31134-5 [DOI] [PubMed] [Google Scholar]
- 8.Sehestedt T, Jeppesen J, Hansen TW, Wachtell K, Ibsen H, Torp-Pedersen C, Torp-Petersen C, Hildebrandt P, Olsen MH. Risk prediction is improved by adding markers of subclinical organ damage to SCORE. Eur Heart J. 2010;31:883–891. doi: 10.1093/eurheartj/ehp546 [DOI] [PubMed] [Google Scholar]
- 9.Van Bortel LM, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank JK, De Backer T, Filipovsky J, Huybrechts S, Mattace-Raso FU, Protogerou AD, et al. ; Artery Society; European Society of Hypertension Working Group on Vascular Structure and Function; European Network for Noninvasive Investigation of Large Arteries. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J Hypertens. 2012;30:445–448. doi: 10.1097/HJH.0b013e32834fa8b0 [DOI] [PubMed] [Google Scholar]
- 10.Weber T, Wassertheurer S, Rammer M, Maurer E, Hametner B, Mayer CC, Kropf J, Eber B. Validation of a brachial cuff-based method for estimating central systolic blood pressure. Hypertension. 2011;58:825–832. doi: 10.1161/HYPERTENSIONAHA.111.176313 [DOI] [PubMed] [Google Scholar]
- 11.Domanski M, Mitchell G, Pfeffer M, Neaton JD, Norman J, Svendsen K, Grimm R, Cohen J, Stamler J; MRFIT Research Group. Pulse pressure and cardiovascular disease-related mortality: follow-up study of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA. 2002;287:2677–2683. doi: 10.1001/jama.287.20.2677 [DOI] [PubMed] [Google Scholar]
- 12.Franklin SS, Lopez VA, Wong ND, Mitchell GF, Larson MG, Vasan RS, Levy D. Single versus combined blood pressure components and risk for cardiovascular disease: the framingham heart study. Circulation. 2009;119:243–250. doi: 10.1161/CIRCULATIONAHA.108.797936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casas-Rojo JM, Antón-Santos JM, Millán-Núñez-Cortés J, Lumbreras-Bermejo C, Ramos-Rincón JM, Roy-Vallejo E, Artero-Mora A, Arnalich-Fernández F, García-Bruñén JM, Vargas-Núñez JA, et al. ; en nombre del Grupo SEMI-COVID-19 Network. Clinical characteristics of patients hospitalized with COVID-19 in spain: results from the SEMI-COVID-19 registry. Rev Clin Esp. 2020;220:480–494. doi: 10.1016/j.rce.2020.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 15.Análisis de los casos de COVID-19 notificados a la RENAVE hasta el 10 de mayo en España, Informe COVID-19 n° 33. 29 de mayo de 2020. Informe n° 33. Análisis de los casos de COVID-19 notificados a la RENAVE hasta el 10 de mayo en España a 29 de mayo de 2020. Equipo COVID-19. RENAVE. CNE. CNM (ISCIII) [Google Scholar]
- 16.Mikami T, Miyashita H, Yamada T, Harrington M, Steinberg D, Dunn A, Siau E. Risk factors for mortality in patients with COVID-19 in New York city. J Gen Intern Med. 20201–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sun H, Jain A, Leone MJ, Alabsi HS, Brenner LN, Ye E, Ge W, Shao YP, Boutros CL, Wang R, et al. COVID-19 outpatient screening: a prediction score for adverse events. medRxiv. [Published ahead of print June 22, 2020]. doi: 10.1101/2020.06.17.20134262 [Google Scholar]
- 18.Vicenzi M, Di Cosola R, Ruscica M, Ratti A, Rota I, Rota F, Bollati V, Aliberti S, Blasi F. The liaison between respiratory failure and high blood pressure: evidence from COVID-19 patients. Eur Respir J. 2020;56:2001157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cao Z, Li T, Liang L, Wang H, Wei F, Meng S, Cai M, Zhang Y, Xu H, Zhang J, et al. Clinical characteristics of coronavirus disease 2019 patients in Beijing, China. PLoS One. 2020;15:e0234764. doi: 10.1371/journal.pone.0234764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H; European Network for Non-invasive Investigation of Large Arteries. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–2605. doi: 10.1093/eurheartj/ehl254 [DOI] [PubMed] [Google Scholar]
- 21.Bruno RM, Spronck B, Hametner B, Hughe AS, Lacolley P, Mayer CC, Muiesan ML, Rajkumar C, Terentes-Printzios D, Weber T, et al. , on behalf of the ARTERY Society. Covid-19 effects on ARTErial StIffness and vascular AgeiNg: CARTESIAN study rationale and protocol. Artery Research. 2020. 10.2991/artres.k.201124.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mancia G, Messerli F, Bakris G, Zhou Q, Champion A, Pepine CJ. Blood pressure control and improved cardiovascular outcomes in the international verapamil SR-trandolapril study. Hypertension. 2007;50:299–305. doi: 10.1161/HYPERTENSIONAHA.107.090290 [DOI] [PubMed] [Google Scholar]
- 23.Vidal-Petiot E, Ford I, Greenlaw N, Ferrari R, Fox KM, Tardif JC, Tendera M, Tavazzi L, Bhatt DL, Steg PG; CLARIFY Investigators. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. Lancet. 2016;388:2142–2152. doi: 10.1016/S0140-6736(16)31326-5 [DOI] [PubMed] [Google Scholar]
- 24.Böhm M, Schumacher H, Teo KK, Lonn EM, Mahfoud F, Mann JFE, Mancia G, Redon J, Schmieder RE, Sliwa K, et al. Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Lancet. 2017;389:2226–2237. doi: 10.1016/S0140-6736(17)30754-7 [DOI] [PubMed] [Google Scholar]
- 25.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement D, Coca A, De Simone G, Dominiczak A, et al. 2018 practice guidelines for the management of arterial hypertension of the European society of cardiology and the european society of hypertension. Blood Press. 2018;27:314–340. doi: 10.1080/08037051.2018.1527177 [DOI] [PubMed] [Google Scholar]
- 26.White WB. The systolic blood pressure versus pulse pressure controversy. Am J Cardiol. 2001;87:1278–1281. doi: 10.1016/s0002-9149(01)01519-3 [DOI] [PubMed] [Google Scholar]
- 27.Domanski M, Mitchell G, Pfeffer M, Neaton JD, Norman J, Svendsen K, Grimm R, Cohen J, Stamler J; MRFIT Research Group. Pulse pressure and cardiovascular disease-related mortality: follow-up study of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA. 2002;287:2677–2683. doi: 10.1001/jama.287.20.2677 [DOI] [PubMed] [Google Scholar]
- 28.Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension. 1. Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32:2285–2295. doi: 10.1097/HJH.0000000000000378 [DOI] [PubMed] [Google Scholar]
- 29.Gruver AL, Hudson LL, Sempowski GD. Immunosenescence of ageing. J Pathol. 2007;211:144–156. doi: 10.1002/path.2104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meftahi GH, Jangravi Z, Sahraei H, Bahari Z. The possible pathophysiology mechanism of cytokine storm in elderly adults with COVID-19 infection: the contribution of “inflame-aging”. Inflamm Res. 2020;69:825–839. doi: 10.1007/s00011-020-01372-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dixon DL, Wohlford GF, 4th, Abbate A. Inflammation and hypertension: causal or not? Hypertension. 2020;75:297–298. doi: 10.1161/HYPERTENSIONAHA.119.14195 [DOI] [PubMed] [Google Scholar]
- 32.Cesari M, Penninx BW, Newman AB, Kritchevsky SB, Nicklas BJ, Sutton-Tyrrell K, Rubin SM, Ding J, Simonsick EM, Harris TB, et al. Inflammatory markers and onset of cardiovascular events: results from the Health ABC study. Circulation. 2003;108:2317–2322. doi: 10.1161/01.CIR.0000097109.90783.FC [DOI] [PubMed] [Google Scholar]
- 33.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, et al. ; CANTOS Trial Group. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377:1119–1131. doi: 10.1056/NEJMoa1707914 [DOI] [PubMed] [Google Scholar]
- 34.Rothman AM, MacFadyen J, Thuren T, Webb A, Harrison DG, Guzik TJ, Libby P, Glynn RJ, Ridker PM. Effects of interleukin-1β inhibition on blood pressure, incident hypertension, and residual inflammatory risk: a secondary analysis of CANTOS. Hypertension. 2020;75:477–482. doi: 10.1161/HYPERTENSIONAHA.119.13642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ridker PM, Everett BM, Pradhan A, MacFadyen JG, Solomon DH, Zaharris E, Mam V, Hasan A, Rosenberg Y, Iturriaga E, et al. ; CIRT Investigators. Low-dose methotrexate for the prevention of atherosclerotic events. N Engl J Med. 2019;380:752–762. doi: 10.1056/NEJMoa1809798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Drummond GR, Vinh A, Guzik TJ, Sobey CG. Immune mechanisms of hypertension. Nat Rev Immunol. 2019;19:517–532. doi: 10.1038/s41577-019-0160-5 [DOI] [PubMed] [Google Scholar]
- 37.Wenzel U, Turner JE, Krebs C, Kurts C, Harrison DG, Ehmke H. Immune mechanisms in arterial hypertension. J Am Soc Nephrol. 2016;27:677–686. doi: 10.1681/ASN.2015050562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nilsson PM, Boutouyrie P, Laurent S. Vascular aging: a tale of EVA and ADAM in cardiovascular risk assessment and prevention. Hypertension. 2009;54:3–10. doi: 10.1161/HYPERTENSIONAHA.109.129114 [DOI] [PubMed] [Google Scholar]
- 39.Kaess BM, Rong J, Larson MG, Hamburg NM, Vita JA, Levy D, Benjamin EJ, Vasan RS, Mitchell GF. Aortic stiffness, blood pressure progression, and incident hypertension. JAMA. 2012;308:875–881. doi: 10.1001/2012.jama.10503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilkinson IB, McEniery CM, Cockcroft JR. Arteriosclerosis and atherosclerosis: guilty by association. Hypertension. 2009;54:1213–1215. doi: 10.1161/HYPERTENSIONAHA.109.142612 [DOI] [PubMed] [Google Scholar]
- 41.Wang M, Jiang L, Monticone RE, Lakatta EG. Proinflammation: the key to arterial aging. Trends Endocrinol Metab. 2014;25:72–79. doi: 10.1016/j.tem.2013.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Saavedra JM. Angiotensin receptor blockers and COVID-19. Pharmacol Res. 2020;156:104832. doi: 10.1016/j.phrs.2020.104832 [DOI] [PMC free article] [PubMed] [Google Scholar]


