Abstract
Introduction: The spread of the SARS-CoV-2 virus has caused chaos around the world. At the onset of the virus’ detection in the State of Qatar, a free-testing system was rapidly established to invite individuals who had recently returned from countries with a COVID-19 disease travel warning to avoid putting other people at risk. The testing site needed to be accessible to individuals without requiring them to enter the hospital and congregate in a waiting area. The aim of this article is to share our experience with the early implementation of a drive-through testing clinic using the invited person's vehicle as an isolation compartment during screening to minimize person-to-person contamination.
Methods: A Hamad Medical Corporation site was selected to stage a drive-through testing facility to avoid congestion and offer space to facilitate the process. A process was rapidly agreed upon, and staff received the required training regarding infection control measures and documentation. At the testing site, individuals were subjected to the following steps: registration and history taking, temperature measurement, swabbing, and receipt of a sick leave certificate and a flyer about self-quarantine.
Results: Over the first six days of implementation, the relevant authorities determined that 687 individuals had to be contacted, 103 attended their testing appointment in that period, and an additional 327 people (close relations of the individuals contacted or individuals contacted but without a health card) also subjected themselves to the testing process, which took a median time of 11 minutes 39 seconds. No individual exhibited symptoms that warranted immediate isolation while they were at the drive-through testing clinic. However, four individuals were diagnosed with COVID-19 following laboratory analysis of the swab taken and followed up. The median time between swab collection and laboratory testing was 13 hours 41 minutes 59 seconds.
Conclusions: Collaboration among various key health, governmental, and travel industry partners was essential to the successful and rapid implementation of a COVID-19 drive-through testing clinic in the early days of the pandemic in Qatar. The general public reacted well to this process. Communication, coordination, and planning were identified as critical factors at every step of the process. It started from the initial call to the travelers who had recently returned from a country with a newly instituted travel warning and concluded by them leaving with their sick leave certificate and an information flyer with reminders about preventative infection control measures and encouraging them to self-quarantine after having been swabbed.
Keywords: drive-through testing, COVID-19, pandemic, infectious disease, quarantine
Introduction
Upon China reporting to the World Health Organization (WHO) cases of a new coronavirus (SARS-CoV-2) on December 31, 2019, all continents observed a relatively rapid spread of the associated COVID-19 disease. The spread of this potentially lethal disease occurred despite China's best efforts to prevent a global outbreak by imposing a quarantine zone in Wuhan.1 As the death toll linked to COVID-19 across the globe was rising, the WHO recommended that all countries be prepared for a potential pandemic.2 Although of questionable effectiveness in terms of preventing disease spread,3 safety measures concerning the testing of travelers, having a 14-day quarantine period when returning from countries where the disease is widespread, not permitting the return from certain affected countries, or even closing borders have been adopted by several countries, including Qatar.1,4–6
Qatar is a peninsula that extends into the Persian Gulf from the Arabian Peninsula with a mostly expatriate population of nearly three million inhabitants but is in a geopolitical situation that gives it the characteristics of an island given the current blockade imposed by its neighboring countries since June 2017.7,8 Although it has caused several inconveniences, in the current situation, it may contribute to an easier containment and control of the spread of COVID-19. The only points of entry into Qatar are via its two international airports and its few seaports. From a healthcare services viewpoint, Qatar is on par with all developed countries with very modern facilities, high standards of care, and offers heavily subsidized care to everyone.9
Identified issue and initial response
As soon as the situation with the spread of SARS-CoV-2 in other countries gained momentum, the Ministry of Public Health (MoPH) in Qatar put measures in place to repatriate its citizens from the most affected countries at the time. It put them in quarantine to avoid potential cross-contamination of other people in the local community. Figure 1 shows the timeline of critical events for Qatar, leading to the implementation of the first drive-through testing clinic.
Figure 1.
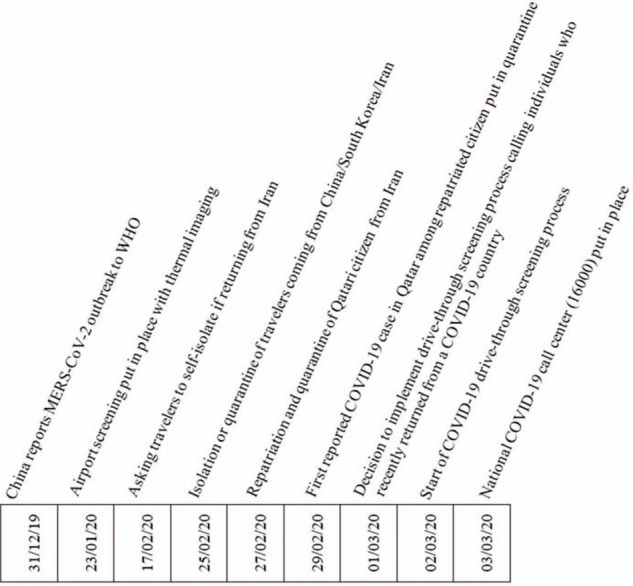
Timeline of significant events in Qatar in relation to the COVID-19 outbreak leading to the opening of a drive-through testing clinic.
In addition to infrared thermal image scanners being deployed at airports to screen arrival passengers from an early stage (Figure 1), the Qatar National Pandemic Preparedness Committee also identified the need to put a system in place rapidly to invite travelers for swab testing retrospectively. Since it was then believed that individuals may not show any symptoms during the first 14 days of being contaminated and yet already be infectious,1 it was decided to contact anyone who had returned to Qatar (n = 2891) between February 16, 2020, and February 23, 2020, from specific affected countries so they could be given a free COVID-19 testing appointment. They would be requested to self-quarantine for 14 days from their return date into the country. They were also asked to extend this testing invitation to anyone they had been in close contact with over a prolonged period of time, such as other members of their household.
Approach adopted to test travelers returning from countries significantly affected by COVID-19
Gathering individuals potentially infected with the SARS-CoV-2 virus in a hospital facility waiting room carries the inherent risk of contaminating other people and requires regular and more stringent decontamination of that environment after each patient encounter. On the other hand, finding these individuals in the community is logistically challenging to orchestrate and highly resource-intensive. Different strategies were rapidly developed and implemented to contact and test the 2891 targeted individuals. Our team decided to adopt a drive-through testing (DTT) approach, which had already proved effective when tested as an exercise by another team in the United States.9 An action plan was immediately instituted. In addition, the required physical and human resources were made available at a suitable location to handle 687 of the targeted individuals (citizens, residents, and visitors), as determined by the relevant authorities. These individuals included people who had recently returned from a SARS-CoV-2 infected country and their immediate relatives or household members.
Process and implementation
The DTT process avoids tests being performed in an emergency or outpatient department or within a primary care center and uses the vehicle of the persons invited to be tested as an isolation compartment.10 The individuals coming by car for testing need a spacious area for staging without causing traffic disruptions. A new tertiary hospital just outside Doha was identified as the most appropriate facility to set up the COVID-19 DTT clinic (Figure 2). It has ample parking space. Some of its unused facilities along the car park area could be converted into a registration desk and a room to receive, label, and store the swab specimens until they were brought to a laboratory for testing.
Figure 2.
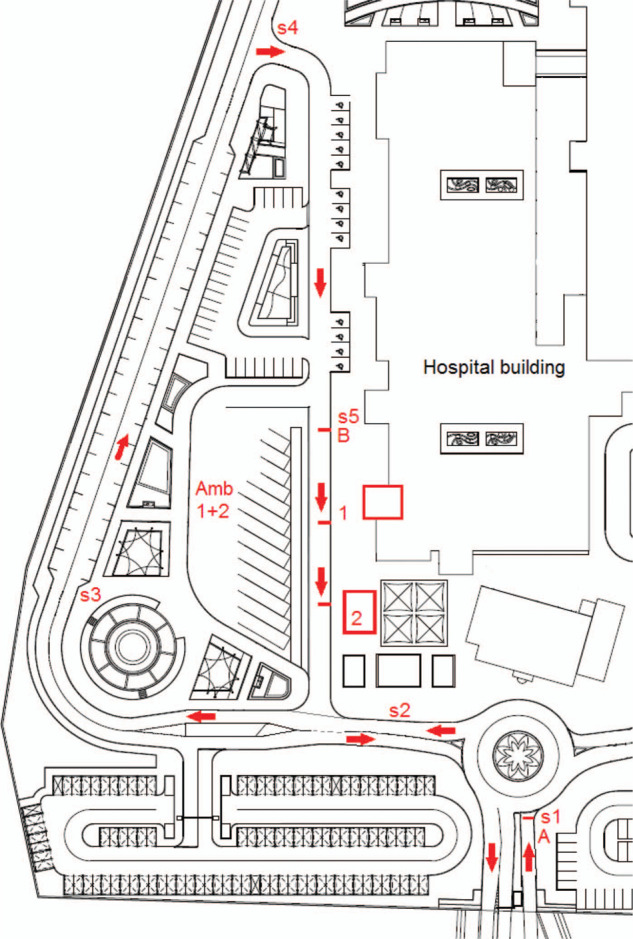
COVID-19 drive-through testing clinic established at a general hospital outside Doha. (Key: S1-5: Security officers directing COVID-19 DTT traffic; A: Stop point to direct all hospital visitors in the right direction; B: Start of screening queue; 1: Greeting, collection of identification documents, temperature check, and questioning of individual about travel history and presentation of symptoms; 2: Swabbing, handing over a sick leave certificate and information flyer, and swab labeling and storage laboratory.
Overnight, the team established a free DTT clinic that was open daily from 8 am to 8 pm. Also, individuals who had recently returned from a country with a new COVID-19 travel warning would be called. The free DTT clinic was arranged and ready for operation the next day in the parking facility at Hamad Medical Corporation (HMC) Hazm Mebaireek General Hospital (HMGH). This goal was achieved thanks to the smooth mobilization, rapid planning, and exemplary collaboration of the various entities involved. The key partners were multiple departments from the HMC Ambulance Service (HMCAS) and HMGH, and the MoPH directly liaising with the Immigration Section of the Ministry of Interior (MOI). Daily multidisciplinary team meetings were held at HMGH to review and improve the process and discuss its challenges. In addition, a secure electronic communication group was created to facilitate communication and provide regular updates throughout the day.
The day before the opening of the DTT clinic, the team from the Hamad Patient Contact Center called individuals on the list provided by the MOI through the MoPH to coordinate the appointments. They explained that patients had to subject themselves to COVID-19 testing at HMGH and remain in self-quarantine, even if they had no symptoms. Patients were also asked to bring other members of their household so that they could also be tested.
Upon arrival at the entrance of HMGH, every car was stopped by a security officer. This security officer had been briefed to direct people coming for their appointment to follow the road leading to the testing area. Several other security officers were posted on this road to direct the traffic (Figure 2). Other hospital visitors were informed to proceed as they would normally to a different car parking area.
All security, registration, and clinical staff involved in the process received training on the appropriate ways to wear and handle personal protective equipment (PPE) and any document given by the vehicle passengers using infection control measures to avoid any possible cross-contamination. A final security stop occurred ahead of the testing line to ensure that no more than two vehicles were at each of the next two stages simultaneously. Each stage had a signpost indicating where the driver had to stop and requesting the driver to place the vehicle's transmission gear in the park position. The first stage was to register each passenger on the online hospital patient record system, determine travel dates and potential exposure, ask symptomatic questions, and perform temperature measurements. The second stage was to swab each passenger's nose and mouth and provide a 14-day sick leave certificate issued from the day of returning to Qatar and an information flyer advising the individuals to self-quarantine and adopt proper infection control measures (Appendix 1). The clinicians involved in this swabbing process wore a disposable N95 mask with eye protection, a gown, and disposable gloves that were changed between each complete swab test.
The parallel two-stage testing process was managed by two teams of nine staff members working in parallel. Each team comprised two porters (greeting and taking identification details and transporting swabs), three nurses (measuring temperature, asking travel, exposure, and symptomatic questions, and taking swabs), a registration clerk, a physician (dispensing sick leave certificates), a laboratory technician (labeling and managing collected swabs), and a driver (transporting swabs to the laboratory every two hours). In addition, two ambulances and their crew remained on standby near the testing lane (Figure 2) to transport individuals with a fever or with breathing difficulty immediately to the Communicable Disease Center for isolation and further testing. An Ambulance Service supervisor and a senior hospital administrator were also onsite, and another one was on call.
This whole process is similar to airport screening and is extremely costly and resource-intensive.3 However, it was determined to be an essential measure of the containment phase of the COVID-19 outbreak in Qatar. Cost considerations included those of the staff involved in the calling process, the various aspects of testing individuals (staffing for security, registration, testing, and transporting samples, and high PPE consumption), and performing laboratory tests.
Patient and public involvement
In terms of patient and public involvement, there was a state of emergency when COVID-19 emerged and was spreading within the community. The public was neither directly involved in setting up this DTT clinic, nor were they involved in the design, implementation, reporting, or dissemination plans of this research as this is a retrospective project, which used de-identified patient information. While this DTT clinic was open, patient feedback was provided and mainly related to accelerating the process and managing expectations during the initial phone call when making the appointment.
Results
We report our findings and lessons learned regarding the first six days (March 2–7, 2020) of implementing a COVID-19 DTT process. After this, the focus of this specific DTT clinic changed.
Of the 687 individuals to be contacted to attend our DTT clinic, 292 could not be reached and were referred to the MOI for follow up. A total of 142 appointments were booked over a period of time. In contrast, the others either reported they had already been tested via another clinic, had no health card, and therefore, were asked to report without an appointment, or were identified as airline employees and therefore were directed to another testing clinic. A total of 103 individuals attended their set appointments. An additional 327 individuals were tested without appointments, as they either were travelers without health cards or were immediate relatives of travelers or household members. None exhibited symptoms (temperature >37.4°C, cough, or sore throat) that warranted their immediate transportation to the Communicable Disease Center for further testing and placement in isolation. The gender distribution of the individuals tested was highly representative of the population in Qatar.
Time was determined as an essential key performance indicator to ensure the individuals’ satisfaction and compliance called to attend this new type of clinic in Qatar. The median duration of the complete process was monitored based on the registration and discharge time from the DTT clinic as recorded in the electronic patient record system. It was 11 minutes 39 seconds (IQR: 8 min 11 sec–17 min 13 sec) (Table 1). Similarly, the median time between registering at the DTT for swabbing and laboratory results was 13 hr 41 min 59 sec (IQR: 8 hr 12 min 26 sec–20 hr 43 min 31 sec). A more detailed review of the data collected revealed that it was not normally distributed due to a few outliers. Therefore, further analysis was conducted using nonparametric tests.
Table 1.
Data of Qatar's first drive-through testing clinic at HMGH over the first six days. (SD: standard deviation)
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Total | |
|
| |||||||
| Appointments set | 8 | 33 | 37 | 24 | 15 | 25 | 142 |
|
| |||||||
| Individuals tested with an appointment | 0 | 26 | 29 | 16 | 9 | 23 | 103 |
|
| |||||||
| Individuals tested without an appointment | 41 | 86 | 73 | 70 | 11 | 46 | 327 |
|
| |||||||
| Total individuals tested | 41 | 112 | 102 | 86 | 20 | 69 | 430 |
|
| |||||||
| Males | 30 | 74 | 74 | 60 | 17 | 48 | 303 |
|
| |||||||
| Females | 11 | 38 | 28 | 26 | 3 | 21 | 127 |
|
| |||||||
| Number of individuals with symptoms while being tested | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
|
| |||||||
| Median testing time in min:sec (IQR) | 10:34 (8:02–13:17) |
13:26 (9:39–18:07) |
9:51 (6:43–17:54) |
12:20 (8:49–17:45) |
8:06 (5:51–11:16) |
12:17 (8:17–17:58) |
11:39 (8:11–17:13) |
|
| |||||||
| Confirmed COVID-19 positive test results | 0 | 0 | 0 | 0 | 0 | 4 | 4 |
|
| |||||||
| Median time between swab collection and laboratory results in hr:min:sec (IQR) | 19:47:48 (18:29:48–21:12:48) 1 sample not processed |
10:55:32 (8:08:56–18:51:31) 1 sample not processed |
14:31:57 (8:16:07–20:05:17) |
9:30:45 (3:54:02–24:14:38) 1 sample not processed |
6:10:31 (5:46:16–7:26:16) |
19:28:46 (12:49:45–23:45:56) 1 sample not processed |
13:41:59 (8:12:26–20:43:31) 4 samples not processed |
|
| |||||||
|
| |||||||
The Kruskal-Wallis H test was used to determine the differences between the DTT durations and laboratory analysis over the six days about the number of individuals tested. It revealed statistical significance (p < 0.05) for both measures (Table 2).
Table 2.
Kruskal-Wallis H test results for the DTT visit duration and time to obtaining the laboratory results for each individual by day.
| DTT visit duration | Time to laboratory results | |
|
| ||
| Total N | 430 | 426 |
|
| ||
| Chi-square | 24.572 | 81.812 |
|
| ||
| Degrees of freedom | 5 | 5 |
|
| ||
| Asymptotic sig. (2-sided test) | 0.000 | 0.000 |
|
| ||
Discussion
Fewer patients than anticipated attended the DTT clinic during the first six days as they either self-reported earlier to another clinic or attended later. It is important to note that this DTT clinic was established before the contact tracing application, Ehteraz, became compulsory in Qatar.11 We achieved much shorter DTT times than those reported in the simulation exercise conducted by a team in Stanford, CA, USA, who reported a median time of 26 minutes per screened patient for an influenza pandemic.12 The time difference in our favor can be explained by the extensive workforce involved at each station. For example, while one person captured data, someone else was performing another task with the individuals being tested, and there was no complete assessment of the individuals by a physician. However, our process median time was slightly longer than the approximate 10 minutes reported by our Korean colleagues who had developed a setup that shortened walking distances for their testing team to perform all required tasks.10 Given the pleasant climate in Qatar in early March, no temporary structure was erected to protect the testing team from the weather. They had to walk about 20 meters each way to the building with the computerized registration desk, transport swabs to the storeroom, and change PPE between patients. Our data also shows a direct impact of the number of individuals screened per day on the performance of the process. One other reason for the disparate testing times with outliers is that when there was more than one passenger in a vehicle, they were registered together. However, their testing was done sequentially, and they were then checked out separately. This disparity resulted in much longer testing periods for some individuals who appear as outliers in Figure 3. On day five (Friday—a holy day in Qatar), much fewer tests were performed, resulting in a median testing time of only eight minutes and six seconds and a median laboratory testing time of just over six hours and 10 minutes (Figure 4). For all days, the maximum median time to obtain the laboratory results was below 20 hours, which means that the individuals who tested positive could generally be informed of their test results the day after their visit at the DTT clinic. This time delay in confirming the laboratory results occurred when swab testing requests overwhelmed the then limited capacity of the laboratories. It was mitigated by the requests of all the tested individuals to remain in self-quarantine for 14 days following their return from travel.
Figure 3.
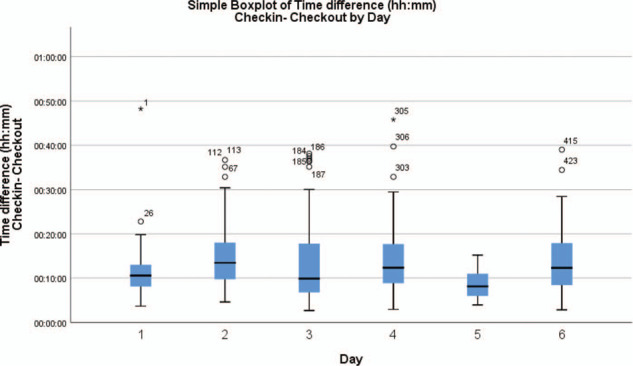
Boxplot of the DTT durations for all individuals by day.
Figure 4.
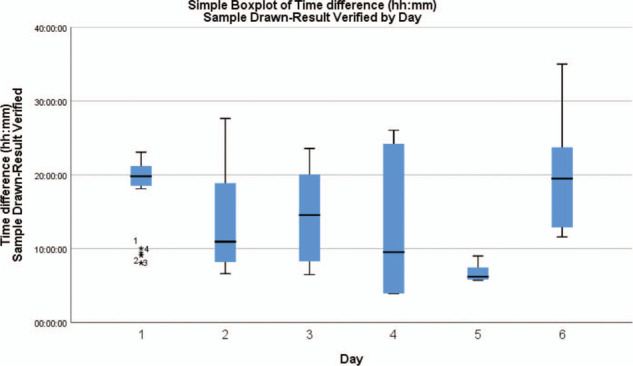
Boxplot of the time elapsed between individuals checking in the clinic each day and their swab being analyzed in the laboratory.
Statistical analysis of the data using the Kruskal-Wallis H test demonstrated that the duration of the testing process significantly varied depending on the days when the individuals attended the DTT clinic and that the primary variable between those days was the number of tests performed. Similarly, a heavier workload on the laboratory resulted in a prolonged duration for the swabs to be tested. By day six, the laboratory processing the COVID-19 swabs received many specimens from various other testing facilities, which negatively affected the time it took to obtain testing results. Based on onsite observations, the registration process of each individual on the computer and the changing of PPE between swab specimen collection are what appeared to be particularly slowing down the DTT.
In the first six days, no one met any of the criteria to be immediately taken by ambulance to the Communicable Disease Center for further assessment and care from the symptomatic screening process. Some individuals who were contacted for an appointment had already contacted the emergency number (999) or the newly established National COVID-19 contact center to be tested because of symptoms they may have exhibited, or they may have been determined to have their test performed at another venue (e.g., Airline employees). This situation cannot be investigated and reported in this article as we could only access the data of the individuals who used this DTT clinic. Over the period presented in this article, only four of the 430 individuals tested returned a positive result to the SARS-CoV-2 virus. None of them had any symptoms or complaints at the time of their visit to the DTT clinic. They were contacted and admitted to one of the isolation locations, based on the level of monitoring and treatment required.
Some unanticipated issues were that a person came by taxi, requiring the driver to be counted as a potentially contaminated individual and required follow up. Another individual walked in, entered the emergency department, and walked through the hospital building to find the DTT area. These behaviors demonstrated that these two individuals had a lack of understanding of the purpose of their visit. They could have been contagious carriers of the virus. Sufficient information might not have been communicated to them when the appointment was given to them over the phone. Clearer guidance was then provided to the individuals contacted. Security officers were also asked to question pedestrians entering the hospital grounds so they could be directed to the testing area without entering the building. In addition, the emergency department reinforced its testing process for everyone entering the facility. A similar issue has also reported by another team who presented their strategy to deal with a previous epidemic crisis.13 The team in Korea pointed out that only individuals with their own vehicles should be asked to visit a drive-through clinic. This was subsequently the case with our DTT clinic. The patients tested were of various nationalities and spoke different languages, but this did not present a significant issue to the testing process. If there had been any communication problems, the multinational DTT staff could have acted as translators.
Some minor alterations were made to the DTT process over the first few days to ensure it worked as smoothly and safely as possible for all stakeholders. These included issuing the sick leave certificate at the end of the process rather than at the beginning, requesting drivers to put their gear in park at each stage of the DTT clinic, and to pull their vehicle as close to the curb as possible since many drove large four-wheel-drive cars that sometimes restricted access making it difficult for nurses to perform the swabbing procedure. As mentioned earlier, the instructions given over the phone when inviting individuals and their immediate relatives or household members for testing were also updated to facilitate the process and encourage compliance. This information was essential as at that time, there was no mandatory use of a smartphone-based application for contact tracing, which is one of the key measures to contain the spread of the disease alongside testing, physical distancing, and self-quarantine.11,14
Conclusion
As a form of influenza, SARS-CoV-2 is difficult to detect during the incubation period, as carriers of the virus are often asymptomatic but are already infectious. In parallel with other initiatives, the elective DTT process that was rapidly established in Qatar, contributed to detecting four asymptomatic COVID-19 cases among recent travelers in six days. Thanks to the collaborative and coordinated approach adopted and constant communication between the various stakeholders, it was very rapidly implemented.
Communication with and education of travelers and the general public are critical components to preventing a disease outbreak. Although we cannot measure the effectiveness of handing out the information flyer, we hope it encouraged individuals to act accordingly until they were informed of their swab test results. Since it is impossible to test or quarantine everyone, people need to be educated to exercise self-discipline regarding hygiene, physical distancing, and adopting appropriate infection control measures. For large scale testing to be effective, the general public needs to be offered various options and be reassured concerning what will happen to them contingent on their test outcome. Aspects that limit the effectiveness of such DTT clinic for travelers are individuals who: do not have their own means of transportation; cannot be reached or speak an uncommon language; or do not understand the seriousness of the situation and how their behavior can affect the spread of a virus. The lessons learned from this DTT clinic could facilitate the implementation of similar mobile testing processes in other areas of the country to improve access and increase the number of tests being performed daily.
Acknowledgements
The authors are grateful to all staff involved in the swift implementation of this COVID-19 DTT process and wish everyone testing positive a swift recovery. Thank you to Dr Anthony Herbland from the University of Hertfordshire (UK) for performing the statistical tests.
Ethical approval
This project was approved for publication by Hamad Medical Corporation (Doha, Qatar) as a Quality Improvement project.
References
- 1. Phelan AL, Katz R and Gostin LO. The novel coronavirus originating in Wuhan, China: challenges for global health governance. Jama. 2020; 323: 709–10. [DOI] [PubMed]
- 2. WHO. WHO Director-General's opening remarks at the media briefing on COVID-19 - 9 March 2020. World Health Organization, [cited 2020 March 10] Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19–-9-march-2020.
- 3. Selvey LA, Antão C and Hall R. Evaluation of border entry screening for infectious diseases in humans. Emerging infectious diseases. 2015; 21: 197. [DOI] [PMC free article] [PubMed]
- 4. MoPH. Spread of Coronavirus Disease 2019 Remains Low in Qatar??. News Details - 8/03/2020: Ministry of Public Health, Doha, Qatar, [cited 2020 March 9] Available from: https://www.moph.gov.qa/english/mediacenter/News/Pages/NewsDetails.aspx?ItemId = 93.
- 5. WHO. Updated WHO recommendations for international traffic in relation to COVID-19 outbreak. 29 February 2020 COVID-19 Travel Advice: World Health Organization, [cited 2020 March 10] Available from: https://www.who.int/news-room/articles-detail/updated-who-recommendations-for-international-traffic-in-relation-to-covid-19-outbreak.
- 6. Tanne JH, Hayasaki E, Zastrow M, Pulla P, Smith P and Rada AG. Covid-19: how doctors and healthcare systems are tackling coronavirus worldwide. BMJ. 2020; 368. [DOI] [PubMed]
- 7. Gengler J and Al-Khelaifi B. Crisis, State Legitimacy, and Political Participation in a Non-Democracy: How Qatar Withstood the 2017 Blockade. Middle East J. 2019; 73: 397–416.
- 8. Gangaram P, Menacho AM and Alinier G. Crisis resource management in relation to empowering people to speak up in emergency medical service clinical practice settings. Journal of Paramedic Practice. 2017; 9: 60–5.
- 9. Goodman A. The development of the Qatar Healthcare System: A review of the literature. International Journal of Clinical Medicine. 2015; 6: 177–85.
- 10. Kwon KT, Ko J-H, Shin H, Sung M and Kim JY. Drive-Through Screening Center for COVID-19: a Safe and Efficient Screening System against Massive Community Outbreak. Journal of Korean Medical Science. 2020; 35. [DOI] [PMC free article] [PubMed]
- 11. El-Kassem RC, Al-Kubaisi AS, Al Naimi MM, Al-Hamadi AM and Al-Rakeb NA. Path Analytic Investigation of the Intention to Adopt E-government Services through Mobile Applications in Qatar (Tam Revisited). International Journal of Advanced Research in Engineering and Technology. 2020; 11.
- 12. Weiss EA, Ngo J, Gilbert GH and Quinn JV. Drive-through medicine: a novel proposal for rapid evaluation of patients during an influenza pandemic. Annals of emergency medicine. 2010; 55: 268–73. [DOI] [PubMed]
- 13. Caswell A. The Impact of MERS-Cov: Service and Systems Re-design: The Creation of the Caswell–Hijazi Model. American Journal of Nursing. 2019; 8: 206–15.
- 14. Kucharski AJ, Klepac P, Conlan AJK, et al. Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. The Lancet Infectious Diseases. 2020; 20: 1151–60. [DOI] [PMC free article] [PubMed]


