Abstract
Background: The COVID-19 pandemic led to changes in the way that healthcare was accessed and delivered in the United Kingdom (UK), particularly during the peak of the first lockdown period (the “first wave”) beginning in March 2020. In some patients, COVID-19 is associated with acute neuropsychiatric manifestations, and there is suggestion that there may also be longer term neuropsychiatric complications. Despite this, at the time of writing there are only emerging data on the direct effects of the COVID-19 pandemic on psychiatric care.
Methods: In this retrospective study we analyzed referrals to an inpatient liaison psychiatry department of a large acute teaching hospital during the first wave of covid-19 in the UK and compared this data to the same period in 2019.
Results: We saw a 40% reduction in the number of referrals in 2020, with an increase in the proportion of referrals for both psychosis or mania and delirium. Almost one third (28%) of referred patients tested positive for COVID-19 at some point during their admission, with 40% of these presenting with delirium as a consequence of their COVID-19 illness. Save delirium, we did not find evidence for high prevalence of new-onset acute mental illness in COVID-19 positive patients.
Conclusion: Our data indicate decreased clinical activity in our inpatient psychiatry liaison department during the first wave of the COVID-19 pandemic, although a relative increase in relative increase in referrals for psychosis or mania, suggesting less of a relative decrease in more severe cases of mental illness. The reasons for this are likely multifactorial, including structural changes in the NHS and patient reluctance to present to emergency departments (ED) due to infection fears and Government advice. Our data also supports the literature suggesting the high relative prevalence of delirium in COVID-19, and we support integration of psychiatry liaison teams in acute general hospital wards to optimize delirium management. Finally, consideration should be given to adequate staffing of community and crisis mental health teams to safely manage the mental health of people reluctant to visit EDs.
Keywords: COVID-19, SARS-CoV-2, liaison psychiatry, delirium, pandemic
Introduction
COVID-19 is the clinical syndrome caused by the novel coronavirus SARS-CoV-2. The first documented case of COVID-19 in the United Kingdom (UK) was confirmed in January 2020 (1). Since then, a number of measures have been implemented to reduce the spread of the virus, including a UK-wide lockdown on March 23rd 2020 (2). Although at the time of writing the lockdown has not been fully lifted, on May 10th 2020 the prime minister announced the introduction of the five-tiered COVID-19 alert system, heralding the end of the “first wave” of COVID-19 in the UK (3). In anticipation of a rise in COVID-19 related inpatient admissions during this first wave, acute hospitals within the National Health Service (NHS) reframed their priorities, shifting focus to safe management and treatment of COVID-19 and its complications. While justified, experts pointed out the necessity for the mental health needs of the hospitalized population to be treated with equal urgency and vigor (4).
Liaison psychiatry is a hospital-based multidisciplinary specialty which provides psychiatric input for inpatients admitted to general hospitals. Broadly, patients seen by a liaison department are those with a history of mental illness who have physical complaints, or those in whom physical illness has precipitated a change in mental state. To this end, many liaison psychiatry departments across the NHS were braced for a surge in referrals due to the effects of the COVID-19 pandemic and associated lockdown on the mental health of the population.
Many patients with COVID-19 experience mild symptoms which are confined to the respiratory tract, however COVID-19 is now understood to have broader systemic effects, including on the central nervous system (5, 6). There are data suggesting the neurotropic potential of SARS-CoV-2 in preclinical studies (7), although this has not consistently translated to clinical populations and is not generally supported by clinical studies (8). Instead, it is increasingly understood that the link between COVID-19 infections and neuropsychiatric presentations may be indirect, mediated for example through an inflammatory response (9, 10).
Neuropsychiatric consequences of previous coronavirus outbreaks showed high rates of psychiatric outcomes in infected patients. Confusion, low mood, anxiety, and impaired memory were noted in the acute stage of the illness in around a third of patients, whilst follow-up data indicated a high prevalence of post-traumatic stress disorder, depression, and anxiety (11). Currently, data are emerging on the neuropsychiatric complications associated with COVID-19 infections, which have shown similar prevalences (12, 13). There have been some data to suggest that COVID-19 is associated with new-onset psychiatric disorders such as psychosis (14, 15), however at the time of writing there is insufficient evidence to confirm this association (10, 16).
At the time of writing, an increase in psychiatric admissions in response to the COVID-19 pandemic has not been noted across Europe (17, 18). Furthermore, centrally collected data revealed a steep fall in overall Emergency Department (ED) presentations for the months following the imposition of lockdown, though details for the various patient groups remain unclear (19). Data is emerging from international studies on the specific effects of COVID-19 on psychiatric presentations; one study reported a 21% reduction in psychiatric presentations to ED in Ireland during the initial 8-week COVID-19 restrictions (20), with a similar study finding a 3-fold decrease in mental health presentations in New Zealand in comparison to previous years (21).
Despite this, there are indications that we may expect the burden on mental health services to increase in future; specifically, the longer-term effects of COVID-19 infection and the associated lockdown are yet to be established, but longer-term neuropsychiatric illnesses arising a result of COVID-19 (22, 23) are likely to add to the already significant burden that psychiatric patients and services are experiencing (24).
To our knowledge, this is the first study to report on the clinical activity of an inpatient liaison psychiatry service during the first wave of the COVID-19 pandemic and to compare it with the activity of previous periods. The study had three aims: (1) to characterize referrals made to inpatient liaison psychiatry services in terms of demographics, reasons for referral, duration of admission, diagnoses, and outcomes; (2) to compare the findings with the same period in 2019; and (3) to characterize the SARS-CoV-2 positive cohort of patients referred to liaison psychiatry, including whether COVID-19 was associated with new-onset psychiatric disorders in patients without a history of psychiatric disorders.
Methods
Setting
King's College Hospital (KCH) is a 950-bed capacity general acute hospital and major trauma, liver and hematology center located in Lambeth, London, one of the most ethnically diverse areas in UK. The liaison psychiatry service is a multidisciplinary team providing assessment and treatment of mental health disorders for adult (18–65 years of age) and older adult (older than 65) patients who are admitted via the emergency department (ED), or electively. The liaison psychiatry service is embedded wholly within KCH, however clinicians in the service are employed by South London and Maudsley NHS Foundation Trust (SLaM).
Inpatient referrals are received electronically through a secure NHS email address and follow a standard template. The referrals are triaged by the duty doctor and consultant during working hours and if they are accepted, the patient is reviewed face to face. At all points patients remain under the primary responsibility of the referring medical or surgical (or similar) team, with liaison psychiatry input in addition if necessary. After review by liaison psychiatry, the impression and recommendations are discussed with the referring team and the reviews are recorded on the electronic patient notes system; the patients then either remain on the liaison psychiatry caseload whilst an inpatient with ongoing input until discharge or are discharged from the caseload back to the referring team.
Study Design
This is a retrospective inpatient electronic referrals and records review covering a 10-week period (2nd March 2020–10th May 2020, inclusive), the end of which coincides with the initial loosening of the lockdown restrictions in the UK. Data from the same 10-week period in 2019 were also extracted and anonymised and served as a comparator group. Follow-up period in 2020 was until 10th June (one month). Information was derived directly from electronic referrals. Missing information was sourced or corroborated by reviewing patient hospital records.
Data was analyzed using IBM SPSS Statistics 26. Means were compared used Student's T-test. Frequencies were compared using Chi-squared analysis. Alpha was set at 0.05. Z-scores were calculated using adjusted residuals from Chi-squared contingency tables and were deemed significant if ≥2.0 or ≤−2.0. Due to the descriptive and exploratory nature of the study, significance levels were not corrected for multiple comparisons.
Data Extraction
Demographic data were obtained from the patient's records, and if not recorded, coded as Unknown. Patients were coded as either White, Asian, Black, Mixed, or Other as per the Harmonized Concepts and Questions for Social Data Sources guidance produced by the Office for National Statistics (25). Referring team details were obtained from the electronic referrals, when available. Self-referrals are those in which it is recorded that psychiatric input was explicitly requested by the patient. “Adult” patients were those aged 18–64, and “older adult” those aged >64 years. Reasons for referral were clustered in mutually agreed categories by the research team, based on the clinical question posed by the referrer.
Reasons for rejection were obtained from reviewing patient notes and were as follows: primary substance misuse issues (these were directly handled by our alcohol care team), duplicate referral, uncomplicated delirium with an obvious precipitating and treatable cause, unclear role for psychiatric input, the patient was already discharged, the patient already had outpatient (OPD) follow-up or OPD follow-up alone was appropriate, and patients with safeguarding issues without psychiatric aspects.
Legal status was coded as “informal” (referring to the default position of the patient not being subject to compulsory detention to hospital for treatment), unless at any point during the admission the patient was placed under legal frameworks of the Mental Capacity Act (more specifically a Deprivation of Liberty Safeguards, DoLS), or a Section of the Mental Health Act (1983), which mandated their detention in hospital for the period of treatment.
Characterization of patients with COVID-19 was based on hospital records at the time of obtaining a laboratory-confirmed positive SARS-CoV-2 infection using a reverse-transcriptase polymerase chain reaction assay for SARS-CoV-2 ribonucleic acid on nasopharyngeal swab or on admission if the patient was admitted for presumed COVID-19 infection. Delirium was identified based on identifying diagnoses through record review, a method which is widely used and validated (26), with high inter-rater reliability (27). First psychiatric presentation was transposed into a binary yes/no based on whether the patient had previously had one or more assessments by any clinician in any department of SLaM mental health services, based on review of their electronic notes.
Results
Study Population (Demographics)
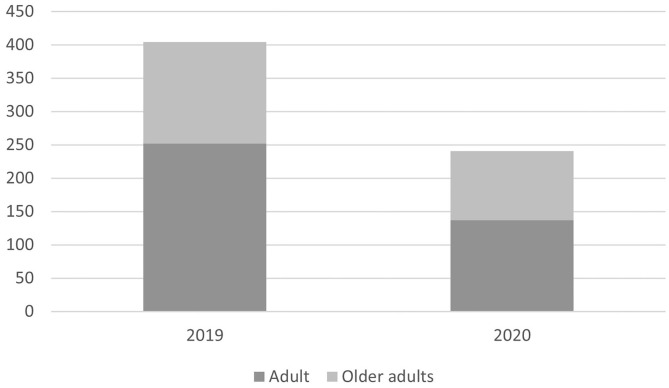
Between March 2nd and May 10th 2019 the KCH inpatient Liaison Psychiatry Team received a total of 404 referrals. In the same 10-week period in 2020 the referral number was 241, representing a decrease of 40.3%. The number of older adults referred decreased from 152 to 104 in 2020 in comparison to 2019 (31.6% decrease), with Adult referrals decreasing from 252 to 137 (45.6% decrease) (Figure 1). Table 1 shows demographic information of referrals by year.
Figure 1.
Bart chart showing decrease in number of referrals in 2020 in comparison to 2019 with total number of referrals on the y axis. The darker bars represent the proportion of referrals for adult patients, with the lighter bars representing older adults.
Table 1.
Demographic information of referrals by year.
| 2019 | 2020 | p | |
|---|---|---|---|
| Mean age (years) | 60.2 | 57.0 | 0.043 |
| Gender (%) | |||
| Females | 188 (46.7) | 114 (47.3) | n.s. |
| Males | 216 (53.3) | 127 (52.7) | n.s. |
| Ethnicity (%) | |||
| Asian | 13 (3.2) | 13 (5.4) | n.s. |
| Black | 88 (21.8) | 63 (26.1) | n.s. |
| White | 249 (61.6) | 143 (59.3) | n.s. |
| Mixed | 8 (2.0) | 5 (2.1) | n.s. |
| Unknown | 46 (11.4) | 17 (7.1) | n.s. |
N.S, non-significant. P-value for age was calculated using T-test for means. Gender and ethnicity were compared with Chi-square.
Referral Details
Table 2 displays a breakdown of primary reasons for referral; proportionately, referrals for psychosis or mania increased by 85.1% in 2020 in comparison to 2019, and referrals for cognitive impairment increased by 71.3%, although these were only approaching significance. Although the proportions were different between the years (X2 21.8, d.f. 11, p = 0.026), the differences were non-significant when stratified by adult and older adult. Standardized residuals (z-scores) for each referral reason were calculated for the overall data, none of which reached significance, although psychosis referrals in 2020 were approaching significance (z = 1.8), as were referrals for cognitive impairment (z = 1.6).
Table 2.
Primary reasons for referral by year.
| 2019 | 2020 | |||||
|---|---|---|---|---|---|---|
| Adults | Older adults | Total (%) [z] | Adults | Older adults | Total (%) [z] | |
| Low mood | 71 (28.2%) | 65 (42.85) | 136 (33.7%) [0.0] | 39 (28.5%) | 42 (40.4%) | 81 (33.6%) [0.0] |
| Challenging behavior | 23 (9.1%) | 28 (18.4%) | 51 (12.6%) [−0.1] | 10 (7.3%) | 21 (20.2%) | 31 (12.9%) [0.1] |
| Anxiety | 25 (9.9%) | 11 (7.2%) | 36 (8.9%) [0.4] | 11 (8.0%) | 7 (6.7%) | 18 (7.5%) [−0.5] |
| Self-harm | 28 (11.1%) | 8 (5.3%) | 36 (8.9%) [−0.1] | 18 (13.1%) | 4 (3.8%) | 22 (9.1%) [0.1] |
| Psychosis or mania | 27 (10.7%) | 8 (5.3%) | 35 (8.7%) [−1.4] | 26 (19.0%) | 10 (9.6%) | 36 (14.9%) [1.8] |
| Substance misuse | 21 (8.3%) | 1 (0.7%) | 22 (5.4%) [1.2] | 5 (3.6%) | 0 (0.0%) | 5 (2.1%) [−1.6] |
| Medication advice | 13 (5.2%) | 7 (4.6%) | 20 (5.0%) [0.6] | 7 (5.1%) | 1 (1.0%) | 8 (3.3%) [-0.8] |
| Cognitive impairment | 6 (2.4%) | 13 (8.6%) | 19 (4.7%) [−1.2] | 8 (5.8%) | 13 (12.5%) | 21 (8.7%) [1.6] |
| Somatoform | 16 (6.3%) | 0 (0.0%) | 16 (4.0%) [0.4] | 7 (5.1%) | 0 (0.0%) | 7 (2.9%) [−0.5] |
| Capacity | 11 (4.4%) | 4 (2.6%) | 15 (3.7%) [1.3] | 2 (1.5%) | 0 (0.0%) | 2 (0.8%) [−1.7] |
| Other | 8 (3.2%) | 7 (4.6%) | 15 (3.7%) [0.5] | 0 (0.0%) | 6 (5.8%) | 6 (2.5%) [−0.7] |
| Psychiatric transfer | 3 (1.2%) | 0 (0.0%) | 3 (0.7%) [−0.7] | 4 (2.9%) | 0 (0.0%) | 4 (1.7%) [0.9] |
| Total | 252 | 152 | 404 | 137 | 104 | 241 |
Data were compared using Chi-square with z-scores calculated from standardized residuals.
Table 3 shows the number of referrals to liaison psychiatry by specialty teams in the hospital. There were significantly fewer referrals from neurology in 2020 (z = −2.5). Referrals from acute medicine increased by 28.0% in 2020. Although not significant, referrals from ITU increased by 79.6% in 2020. Overall, the proportions of referrals by team was different (X2 32.9, d.f. 10, p < 0.001) between the years.
Table 3.
Referring team by speciality by year.
| Referring team | 2019 (%) [z] | 2020 (%) [z] |
|---|---|---|
| Acute medicine | 117 (39.7%) [−1.3] | 121 (50.8%) [1.4] |
| Critical care unit | 6 (2.0%) [0.0] | 5 (2.1%) [0.0] |
| General surgery | 7 (2.4%) [−0.5] | 8 (3.4%) [0.5] |
| Geriatrics | 49 (16.6%) [1.0] | 28 (11.8%) [−1.1] |
| ITU | 16 (5.4%) [−1.2] | 23 (9.7%) [1.3] |
| Neurology | 20 (6.8%) [2.2] | 2 (0.8%) [−2.5] |
| Neurosurgery | 13 (4.4%) [0.2] | 9 (3.8%) [-0.3] |
| Orthopedics | 6 (2.0%) [−1.0] | 10 (4.2%) [1.1] |
| Other surgery | 14 (4.7%) [1.3] | 4 (1.7%) [−1.4] |
| Specialist medicine | 28 (12.9%) [1.5] | 16 (6.7%) [−1.7] |
| Trauma | 9 (3.1%) [−0.8] | 12 (5.0%) [0.9] |
Data were compared using Chi-square with z-scores calculated from standardized residuals.
There were significantly more referrals rejected due to uncomplicated delirium (z = 3.1), as well as safeguarding concerns as opposed to mental illness being the pertinent issue (z = 2.0), in 2020. The overall proportions of rejection reasons by year was different (X2 27.8, d.f. 6, p < 0.001), as per Table 4.
Table 4.
Breakdown of SARS-CoV-2 result by liaison team, gender, and ethnicity.
| Liaison team | Gender | Ethnicity | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Adult (%) | Older adult (%) | Male (%) | Female (%) | White (%) | Black (%) | Asian (%) | Mixed (%) | Unknown (%) | Total | |
| Positive | 26 (10.8) | 42 (40.4) | 29 (22.8) | 39 (34.2) | 35 (24.5) | 25 (39.7) | 4 (30.8) | 0 (0.0) | 4 (23.5) | 68 |
| Negative | 76 (55.5) | 56 (53.8) | 74 (58.3) | 58 (50.9) | 87 (60.8) | 28 (44.4) | 6 (46.2) | 4 (80.0) | 7 (41.2) | 132 |
| Not tested | 35 (25.5) | 6 (5.8) | 17 (18.9) | 17 (14.9) | 21 (14.7) | 10 (15.9) | 3 (23.1) | 1 (20.0) | 6 (35.3) | 41 |
| Total | 137 | 104 | 127 | 114 | 143 | 63 | 13 | 5 | 17 | |
Hospital Journey
Compared with 2019, in 2020 the proportion of patients referred to liaison psychiatry who had been conveyed to hospital by ambulance increased from 60.3% (n = 241) to 76.8% (n = 185), elective admissions reduced from 6.8% (n = 27) to 1.2% (n = 3), and the number of self-presentations (walk-ins) reduced from 22.3% (n = 89) to 14.1% (n = 34). Overall, the differences were significant (X2 28.8, d.f. 6, p < 0.001). There were no differences in the proportion of patients referred to liaison psychiatry who had been admitted to ITU at some point during their admission in 2020 (n = 47, 19.7%) than in 2019 (n = 58, 14.7%) (p = 0.102).
There was no differences between the years in the frequency of ICD-10 diagnoses at the point of discharge. There were no significant differences in proportions of discharge destinations between the years (X2 6.36, d.f. 6, p = 0.385). Despite this, there was a proportional increase in patients admitted to a psychiatric hospital compulsorily in 2020 (n = 9, 5.7% [z = 1.0]) in comparison to 2020 (n = 9, 3.2% [z = −0.7]), although a proportional decrease in patients transferred to a psychiatric hospital voluntarily in 2020 (n = 2, 1.3% [z = −1.0]) in comparison to 2019 (n = 9, 3.2% [z = 0.7]).
The COVID-19 Cohort
Regarding SARS-CoV-2 status of the accepted referrals, 54.8% (n = 132) of patients tested negative, 28.2% (n = 68) tested positive while 17.0% (n = 41) did not have a recorded test. Table 4 shows the breakdown of test results by liaison team, gender, and ethnicity.
Legal status of SARS-CoV-2 patients was different to patients without (X2 = 17.85, d.f. 8, p = 0.22). Specifically, there were more patients on DOLS (17.6%) [z = 2.6] in the SARS-CoV-2 positive group vs. the SARS-CoV-2 negative (5.4%) and not tested (2.4%) groups. Delirium was present in 39.7% (n = 27) patients at the point of COVID-19 diagnosis, and 22.0% (n = 15) had a delirium as their sole presenting symptom of COVID-19.
In total, n = 20/68 (29.4%) of SARS-CoV-2 patients had had no known past psychiatric history (i.e., no previous contact with SLaM Mental Health services prior to the current admission). Their eventual new ICD-10 diagnoses after discharge from the liaison team in this group were organic (F0) in 55.0% (n = 11), neurotic (F4) in 20.0% (n = 4), affective (F3) in 10.0% (n = 2), physiological (F5) in 5.0% (n =1), psychotic (F2) in 5.0% (n = 1), and no diagnosis in 5.0% (n = 1). One patient was diagnosed with a new-onset psychotic disorder; this was a new-onset post-natal psychosis in an otherwise asymptomatic patient.
Discussion
To our knowledge, this is the first attempt to describe the clinical activity of a UK-based liaison psychiatry service amidst the peak of the COVID-19 pandemic and the first to compare this with the corresponding period in the previous year. Results highlight a striking drop in the number of referrals in comparison to the same period in 2019, although, proportionately, referrals for psychosis or mania and cognitive impairment increased. The increased proportion of referrals for psychosis or mania plus proportional increase in patients admitted involuntarily may reflect the continuing presentation of the more severe end of mental illness over less severe cases. As well as this, there were proportionately less referrals for assistance with capacity assessments and substance abuse.
Pandemic-Related Changes
Whilst the reasons behind the overall decrease in referrals may be complex, it is probably at least in part representative of a decrease in the number of overall patients who presented and were admitted to hospital during the exponential phase of the pandemic. It is possible that the population at the time of the lockdown were less willing to present to hospital due to fear of potential infection, a phenomenon which has been reflected in ED attendances for mental illnesses in other countries (20, 21), in other medical specialities in the UK (28, 29), as well as during a previous coronavirus epidemic (30). Similarly, during the period of this study, official Government advice was to stay at home unless strictly necessary, which may have led to people choosing not to attend primary or secondary healthcare settings unless in a life-threatening emergency (31).
The lower proportion of patients admitted electively in our study likely reflects changes in the provision of NHS services during the pandemic. Specifically, data from the British Medical Association suggests that in April, May, and June 2020 in England there were between 1.3 and 1.5 million fewer elective admissions than would usually be expected (32). In our study in 2020, the increase in referrals from acute medicine, and decrease from specialist medical wards, echoes the changes in drafting specialist medical doctors into more general acute medical teams in response to the changing demands of the pandemic, as well as the closure of some specialist services (33).
Overall, however, we feel that the decrease in referrals to liaison psychiatry does not represent a genuine reflection of a reduced burden of mental illness; indeed, there are indications in the literature of worsening mental health at the population level (34). Instead, the reluctance of patients to present to hospital may have added burden onto community mental health services and primary care, which was not captured in this study. We suggest that alternative methods such as reviewing primary care records or self-reported information from surveys and apps may provide a more accurate representation of incidence of mental illness than acute hospital admissions or referrals to secondary mental health services (35, 36).
Our data showed that the total number of psychiatric admissions remained relatively unchanged at discharge from liaison psychiatry, although proportionally there was an increase in involuntary admissions. Early data has indicated that admission rates to psychiatric hospitals declined during the peak of the COVID-19 pandemic in Europe in comparison to the same period in the preceding year (17, 18). This may at least in part represent changes in severity of presentations as well as the structure of mental health services during the pandemic.
Characterizing the SARS-CoV-2 Positive Cohort
In total, 28% of referrals were SARS-CoV-2 positive; a significant proportion of which had delirium as a presenting feature, some even in the absence of other acute medical manifestations. As around 40% of SARS-CoV-2 positive patients presented with delirium as part of their COVID-19 syndrome, it is likely that referrals for COVID-19 associated delirium constituted a large proportion of this increase. Although the cause of delirium is often multifactorial, it is well-established that infections and the resultant systemic inflammatory response may lead to delirium in individuals predisposed to the condition, possibly through cytokine-induced cholinergic deficiencies (37).
Such inflammatory responses have been characterized in COVID-19 (38, 39). Data so far has indicated that the incidence of delirium in COVID-19 patients ranges from 9 to 42%, with increased incidence in those with severe infection, the elderly, and those with dementia (40–43). In many cases delirium is the sole or main presenting symptom of COVID-19 (43, 44), and, due to this, new onset of delirium has been included as a reason for clinicians to screen for COVID-19 (45).
Delirium is known to lead to stepwise worsening of cognition and may precipitate the genesis of dementia (46). Therefore, cognitive consequences in COVID-19 patients with delirium may be longstanding, a hypothesis which has been supported from early follow-up data from COVID-19 patients (47) suggesting longer-term cognitive impairment post-discharge, which is in line with evidence from longer-term follow-up from the SARS epidemic (48).
Some reports suggest that COVID-19 infection is contemporaneous with de novo psychiatric disorders such as psychosis and catatonia (5, 14, 15), although in many cases causality cannot be ascribed with confidence (10, 16). Others have also suggested high rates of post-traumatic stress symptoms, and higher odds of anxiety and depressive symptoms in COVID-19 inpatients in comparison to controls, although this has not been consistently replicated (49–51). In many cases in the literature, where psychiatric manifestations are noted, they are new diagnoses, although this data has also not always been replicated (5, 52, 53).
Aside from delirium, we did not find strong evidence of other new-onset psychiatric disorders arising in this cohort of SARS-CoV-2 positive patients; there were four new anxiety, two new affective disorder diagnoses, and one new post-natal psychosis diagnosis in the cohort. Although we did not record pharmacological agents in this study, use of certain medication in severe COVID-19, principally steroids, may lead to iatrogenic cases of mania or psychosis (54) as was the case in previous coronavirus outbreaks (11). This area requires further exploration.
It may, however, be the case that adverse psychiatric outcomes do not arise until after patients are discharged from hospital with COVID-19, with emerging studies indicating that patients can suffer with lasting fatigue and cognitive difficulties (55), as well as depression, anxiety, and post-traumatic stress disorder (56) for weeks after discharge. We may also see a rise in cases of severe mental illness such as psychosis with a time-lag of months or years, as has been described in previous respiratory viral epidemics (57).
Finally, in our study, a larger proportion of referrals for Black & Asian patients were SARS-CoV-2 positive in comparison to White patients. Data from the current pandemic has shown that Black, Asian and minority ethnic (BAME) people have been disproportionately affected by COVID-19, with poorer reported outcomes, including higher mortality (58). These structural health inequalities are also reflected in the experience of severe mental illnesses in BAME populations (59). In both cases, these poorer outcomes likely reflect social, economic and health inequalities, a complex social and political matter that needs to be urgently addressed.
Limitations
There are a few limitations to the current study. This is a retrospective electronic records review and as such causal conclusions should be avoided. The data is from a single site and may not thus be generalisable in other areas; particularly, our studied population may be reflective of the diversity of a large urban area, though not representative of rural clinical environments. We did not include referrals exclusively dealing with perinatal and substance misuse presentations, as these were dealt by the respective teams. The increase in specific referrals, for example delirium, may be ascribed, at least in part to organizational restructuring within the hospital as members of the specialist dementia and delirium team were redeployed to other parts of the hospital. We did not have access to hospital records of other organizations, hence there is the possibility some of the patients being recorded as new psychiatric presentations when in fact there was a past psychiatric history. We did not collect data on pharmacological management of either COVID-19 or mental illness. Data recording the specialty of referring team was incomplete, particularly from 2019 in which 119 referrals had these specific data missing. Finally, hospital policy on swabbing for SARS-CoV-2- reflecting governmental guidelines and the provision of resources was altered during the study period; as a result, cases of COVID-19, particularly those which were asymptomatic, may have been missed as they may not have had a swab during their admission.
Conclusions
Compared with the corresponding period in 2019, in the 10-week period during the exponential phase of the first wave of the COVID-19 pandemic in the UK, the clinical activity of our inpatient liaison psychiatry team significantly decreased, in part reflecting a change in the way people accessed health services in the UK. We saw a proportional rise in cases of cognitive impairment, which is in part explained by high rates of COVID-19 delirium. There were also proportional rises in cases of psychosis or mania, as well as patients admitted involuntarily to a psychiatric hospital at discharge, possibly suggesting less of a relative decrease in the more severe presentations. Although our results do not support the notion of consistent acute psychiatric complications of COVID-19 aside from delirium, as indicated by the low numbers of new-onset conditions, we should be mindful of potential longer-term sequelae. We would hope that adequate provision for psychiatric patients is kept at the forefront of any policy changes in response to the longer-term effects of the COVID-19 pandemic, which is ongoing at the time of writing.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
Data was collected by MB, AD, FM, SB, LP, and SG. MB drafted the manuscript, performed the statistical analyses, and oversaw submission and modifications of the manuscript. SP finalized the manuscript for submission. All authors provided input on the final draft of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Moss P, Barlow G, Easom N, Lillie P, Samson A. Lessons for managing high-consequence infections from first COVID-19 cases in the UK. Lancet. (2020) 395:e46. 10.1016/S0140-6736(20)30463-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iacobucci G. Covid-19: UK lockdown is “crucial” to saving lives, say doctors and scientists. BMJ. (2020) 368:m1204. 10.1136/bmj.m1204 [DOI] [PubMed] [Google Scholar]
- 3.BBC Coronavirus: Boris Johnson to Launch Threat Level Alert System. BBC News; (2020). Available online at: https://www.bbc.com/news/uk-52602635 (accessed December 9, 2020). [Google Scholar]
- 4.Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Varatharaj A, Thomas N, Ellul M, Davies NW, Pollak T, Tenorio EL, et al. UK-wide surveillance of neurological and neuropsychiatric complications of COVID-19: the first 153 patients. Lancet Psychiatry. (2020) 7:875–82. 10.2139/ssrn.3601761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paterson RW, Brown RL, Benjamin L, Nortley R, Wiethoff S, Bharucha T, et al. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain. (2020) 143:3104–20. 10.1093/brain/awaa240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu J, Lazartigues E. Expression of ACE2 in human neurons supports the neuro-invasive potential of COVID-19 virus. Cell Mol Neurobiol. (2020) 4:1–5. 10.1007/s10571-020-00915-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Butler M, Pollak TA, Rooney AG, Michael BD, Nicholson TR. Neuropsychiatric complications of covid-19. BMJ. (2020) 371:m3871. 10.1136/bmj.m3871 [DOI] [PubMed] [Google Scholar]
- 9.Guilmot A, Maldonado Slootjes S, Sellimi A, Bronchain M, Hanseeuw B, Belkhir L, et al. Immune-mediated neurological syndromes in SARS-CoV-2-infected patients. J Neurol. (2020). 10.1007/s00415-020-10108-x. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ellul M, Varatharaj A, Nicholson TR, Pollak TA, Thomas N, Easton A, et al. Defining causality in COVID-19 and neurological disorders. J Neurol Neurosurg Psychiatry. (2020) 91:811–2. 10.1136/jnnp-2020-323667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parra A, Juanes A, Losada CP, Álvarez-Sesmero S, Santana VD, Martí I, et al. Psychotic symptoms in COVID-19 patients. A retrospective descriptive study. Psychiatry Res. (2020) 291:113254. 10.1016/j.psychres.2020.113254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Caan MP, Lim CT, Howard M. A case of catatonia in a man with COVID-19. Psychosomatics. (2020) 61:556–60. 10.1016/j.psym.2020.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Watson CJ, Thomas RH, Solomon T, Michael BD, Nicholson TR, Pollak TA. COVID-19 and psychosis risk: real or delusional concern? Neurosci Lett. (2021) 741:135491. 10.1016/j.neulet.2020.135491 [DOI] [PubMed] [Google Scholar]
- 14.Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:611–27. 10.1016/S2215-0366(20)30203-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, et al. Neurological associations of COVID-19. Lancet Neurol. (2020) 19:767–83. 10.1016/S1474-4422(20)30221-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cagnazzo F, Arquizan C, Derraz I, Dargazanli C, Lefevre P-H, Riquelme C, et al. Neurological manifestations of patients infected with the SARS-CoV-2: a systematic review of the literature. J Neurol. (2020). 10.1007/s00415-020-10285-9. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clerici M, Durbano F, Spinogatti F, Vita A, De Girolamo G, Micciolo R. Psychiatric hospitalization rates in Italy before and during COVID-19: did they change? An analysis of register data. Ir J Psychol Med. (2020) 37:283–90. 10.1017/ipm.2020.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoyer C, Ebert A, Szabo K, Platten M, Meyer-Lindenberg A, Kranaster L. Decreased utilization of mental health emergency service during the COVID-19 pandemic. Eur Arch Psychiatry Clin Neurosci. (2020). 10.1007/s00406-020-01151-w. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.NHS England A&E Attendances and Emergency Admissions 2020-21. NHS England and NHS Improvement; (2020). Available online at: https://www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/ae-attendances-and-emergency-admissions-2020-21/ (accessed August 3, 2020). [Google Scholar]
- 20.McAndrew J, O'Leary J, Cotter D, Cannon M, MacHale S, Murphy K, et al. Impact of initial COVID-19 restrictions on psychiatry presentations to the emergency department of a large academic teaching hospital. Ir J Psychol Med. (2020). 10.1017/ipm.2020.115. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joyce LR, Richardson SK, McCombie A, Hamilton GJ, Ardagh MW. Mental health presentations to christchurch hospital emergency department during COVID-19 lockdown. Emerg Med Australas. (2020). 10.1111/1742-6723.13667. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 22.Mandal S, Barnett J, Brill SE, Brown JS, Denneny EK, Hare SS, et al. “Long-COVID”: A cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax. (2020). 10.1136/thoraxjnl-2020-215818. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Townsend L, Dyer AH, Jones K, Dunne J, Mooney A, Gaffney F, et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS ONE. (2020) 15:e0240784. 10.1371/journal.pone.0240784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:813–24. 10.1016/S2215-0366(20)30307-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Office for National Statistics Harmonised Concepts and Questions for Social Data Sources Introduction to Harmonised Standards. Harmonised Concepts and Questions for Social Data Sources: Primary Standards. London: Office for National Statistics; (2011). [Google Scholar]
- 26.Inouye SK, Leo-Summers L, Zhang Y, Bogardus ST, Leslie DL, Agostini J V. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc. (2005) 53:312–8. 10.1111/j.1532-5415.2005.53120.x [DOI] [PubMed] [Google Scholar]
- 27.Fong TG, Jones RN, Shi P, Marcantonio ER, Yap L, Rudolph JL, et al. Delirium accelerates cognitive decline in alzheimer disease. Neurology. (2009) 72:1570–5. 10.1212/WNL.0b013e3181a4129a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M, et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. (2020) 396:381–9. 10.1016/S0140-6736(20)31356-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. (2020) 4:e10–1. 10.1016/S2352-4642(20)30108-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang HJ, Huang N, Lee CH, Hsu YJ, Hsieh CJ, Chou YJ. The Impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am J Public Health. (2004) 94:562–4. 10.2105/AJPH.94.4.562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ridsdale L. Covid-19: “protecting the NHS” encourages people with symptoms to stay at home. BMJ. (2020) 370:m3515. 10.1136/bmj.m3515 [DOI] [PubMed] [Google Scholar]
- 32.British Medical Association The Hidden Impact of COVID-19 on Patient Care in the NHS in England. BMA; (2020). Available online at: https://www.bma.org.uk/media/2841/the-hidden-impact-of-covid_web-pdf.pdf [Google Scholar]
- 33.NHS England Redeploying Your Secondary Care Medical Workforce Safely. London: NHS; (2020). 1–23p. [Google Scholar]
- 34.Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. (2020) 7:883–92. 10.1016/S2215-0366(20)30308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Srinivasa Rao ASR, Vazquez JA. Identification of COVID-19 can be quicker through artificial intelligence framework using a mobile phone-based survey when cities and towns are under quarantine. Infect Control Hosp Epidemiol. (2020) 41:826–30. 10.1017/ice.2020.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Menni C, Valdes AM, Freidin MB, Sudre CH, Nguyen LH, Drew DA, et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat Med. (2020) 26:1037–40. 10.1038/s41591-020-0916-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Gool WA, van de Beek D, Eikelenboom P. Systemic infection and delirium: when cytokines and acetylcholine collide. Lancet. (2010) 375:773–5. 10.1016/S0140-6736(09)61158-2 [DOI] [PubMed] [Google Scholar]
- 38.Benameur K, Agarwal A, Auld SC, Butters MP, Webster AS, Ozturk T, et al. Encephalopathy and encephalitis associated with cerebrospinal fluid cytokine alterations and coronavirus disease, atlanta, georgia, usa, (2020). Emerg Infect Dis. (2020) 26:2016–21. 10.3201/eid2609.202122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang H. Delirium: a suggestive sign of COVID-19 in dementia. EClinicalMedicine. (2020) 26:100524. 10.1016/j.eclinm.2020.100524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. (2020) 395:507–13. 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mcloughlin BC, Miles A, Webb TE, Knopp P, Eyres C, Fabbri A, et al. Functional and cognitive outcomes after COVID-19 delirium. Eur Geriatr Med. (2020) 11:857–62. 10.1007/s41999-020-00353-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bianchetti A, Rozzini R, Guerini F, Boffelli S, Ranieri P, Minelli G, et al. Clinical presentation of COVID19 in dementia patients. J Nutr Heal Aging. (2020) 24:560–2. 10.1007/s12603-020-1389-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kennedy M, Helfand BKI, Gou RY, Gartaganis SL, Webb M, Moccia JM, et al. Delirium in older patients with COVID-19 presenting to the emergency department. JAMA Netw open. (2020) 3:e2029540. 10.1001/jamanetworkopen.2020.29540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ward CF, Figiel GS, McDonald WM. Altered mental status as a novel initial clinical presentation for COVID-19 infection in the elderly. Am J Geriatr Psychiatry. (2020) 28:808–11. 10.1016/j.jagp.2020.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.GOV.UK COVID-19: Investigation and Initial Clinical Management of Possible Cases. Gov.UK; (2020). Available online at: https://www.gov.uk/government/publications/wuhan-novel-coronavirus-initial-investigation-of-possible-cases [Google Scholar]
- 46.Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, Inouye SK, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. (2012) 367:30–9. 10.1056/NEJMoa1112923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C, et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. (2020) 382:2268–70. 10.1056/NEJMc2008597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hopkins RO, Weaver LK, Pope D, Orme JF, Bigler ED, Larson-Lohr V. Neuropsychological sequelae and impaired health status in survivors of severe acute respiratory distress syndrome. Am J Respir Crit Care Med. (1999) 160:50–6. 10.1164/ajrccm.160.1.9708059 [DOI] [PubMed] [Google Scholar]
- 49.Bo HX, Li W, Yang Y, Wang Y, Zhang Q, Cheung T, et al. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. (2020) 27:1–2. 10.1017/S0033291720000999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nguyen HC, Nguyen MH, Do BN, Tran CQ, Nguyen TTP, Pham KM, et al. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: the potential benefit of health literacy. J Clin Med. (2020) 9:965. 10.3390/jcm9040965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Badenoch J, Cross B, Hafeez D, Song J, Watson C, Butler M, et al. Post-traumatic symptoms after COVID-19 may (or may not) reflect disease severity. Psychol Med. (2020). 10.1017/S003329172000481X. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Iqbal Y, Al Abdulla MA, Albrahim S, Latoo J, Kumar R, Haddad PM. Psychiatric presentation of patients with acute SARS-CoV-2 infection: a retrospective review of 50 consecutive patients seen by a consultation-liaison psychiatry team. BJPsych Open. (2020) 6:e109. 10.1192/bjo.2020.85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. (2020). 10.1016/S2215-0366(20)30462-4. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brown E, Gray R, Lo Monaco S, O'Donoghue B, Nelson B, Thompson A, et al. The potential impact of COVID-19 on psychosis: a rapid review of contemporary epidemic and pandemic research. Schizophr Res. (2020) 222:79–87. 10.1016/j.schres.2020.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J Med Virol. (2021) 93:1013–22. 10.1002/jmv.26368 [DOI] [PubMed] [Google Scholar]
- 56.Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. (2020) 89:594–600. 10.1016/j.bbi.2020.07.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kepińska AP, Iyegbe CO, Vernon AC, Yolken R, Murray RM, Pollak TA. Schizophrenia and Influenza at the centenary of the 1918-1919 Spanish Influenza pandemic: mechanisms of psychosis risk. Front Psychiatry. (2020) 11:72. 10.3389/fpsyt.2020.00072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pareek M, Bangash MN, Pareek N, Pan D, Sze S, Minhas JS, et al. Ethnicity and COVID-19: an urgent public health research priority. Lancet. (2020) 395:1421–2. 10.1016/S0140-6736(20)30922-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bhui K, Halvorsrud K, Nazroo J. Making a difference: ethnic inequality and severe mental illness. Br J Psychiatry. (2018) 213:574–8. 10.1192/bjp.2018.148 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.