Abstract
Purpose
Fertility is a quality of life outcome adversely affected by cancer therapy. Many childhood cancer patients, however, are not offered options to preserve their fertility. Providers acknowledge difficulty discussing impaired fertility to patients due to lack of knowledge of available options. Our objective was to review the impact of a pediatric multidisciplinary fertility preservation program on providers’ fertility preservation counseling and discussion of options.
Methods
A retrospective medical chart review was conducted for pediatric cancer patients prior to and following program establishment. Fertility preservation discussions, consults, and incidence were noted. Following filtering and stratification, 198 and 237 patients were seen prior to and following program establishment, respectively.
Results
Following program establishment, provider–patient discussions of impaired fertility (p = 0.007), fertility preservation consults (p = 0.01), and incidence of fertility preservation procedures (p < 0.001) increased among patients. Furthermore, the number of patients who received fertility preservation consults after receiving gonadotoxic treatment decreased (p < 0.001). This trend was particularly noted in pre-pubertal and female patients, for whom fertility preservation options are limited without an established program.
Conclusion
The establishment of a formal program greatly improved access to fertility preservation consults and procedures in children with cancer.
Keywords: Childhood cancer, Infertility, Gonadotoxic treatment, Pediatrics, Urology, Gynecology
Introduction
The survival rate for childhood cancer is now a remarkable 85% [1]. However, due to cancer treatments such as chemotherapy and radiation, survivors are vulnerable to health and quality of life limitations in their subsequent adulthood [2, 3]. Fertility, in both males [4] and females [5], is a quality of life outcome that can be diminished by cancer therapy. Fertility preservation options are therefore increasing in demand for children undergoing gonadotoxic treatments.
National guidelines suggest providers universally discuss fertility with their patients undergoing gonadotoxic treatments [6–8]. However, childhood cancer patients are frequently not offered the option to preserve their future fertility prior to receiving fertility-threatening treatments. Survey-based investigations have found that between 41 and 52% of childhood cancer survivors and families do not recall conversations of fertility during their cancer care [9, 10]. A major reason cited by youth for foregoing fertility preservation is being unaware of their options [11]. From the provider perspective, approximately half of oncologists admit they do not bring up fertility preservation to patients facing fertility-threatening treatment [12, 13], and very few providers use national guidelines to support their decision-making [13].
Several barriers exist for providing comprehensive fertility preservation counseling to patients. While few providers noted a lack of fertility specialists or time constraints, many feel that they do not have adequate knowledge on fertility preservation possibilities to be able to provide this as an option [14]. One meta-analysis found that the most frequent barrier to fertility preservation in cancer patients is institutional gaps, such as inadequate facilities/funding or absences of institution-specific fertility preservation guidelines. Furthermore, poor connections to fertility specialists or ill-defined roles in multidisciplinary teams lead to providers not feeling comfortable referring patients for fertility preservation consults [15].
National organizations have implemented initiatives to improve patient education of fertility preservation. However, patients likely benefit more from personalized information by their oncology care team [15]. To address the lack of provider knowledge and improve patient fertility preservation outcomes, the implementation of a hospital-wide fertility preservation program has been suggested [16] to standardize communication and education among providers and patients. Such a program has led institutions to have higher rates of provider referrals [17, 18] and subsequent incidence of fertility preservation [19]. Furthermore, patient satisfaction with respect to receiving fertility preservation information greatly increases following the implementation of a fertility program [20].
In 2016, Mayo Clinic established a hospital-wide pediatric fertility preservation program. The program is multidisciplinary in nature and involves pediatric gynecology, pediatric urology, pediatric surgery reproductive endocrinology, and laboratory medicine, among others. The program supports all clinically established fertility preservation options for boys and girls [21], such as oocyte/embryo cryopreservation, sperm banking, and ovarian/testicular shielding. Experimental procedures, such as testicular (and formerly ovarian) tissue cryopreservation, are offered through IRB-approved protocols (Mayo Clinic Institutional Review Board # 15-004891 and 14-010037). Briefly, the workflow is as follows: Patients undergoing moderate to severe gonadotoxic treatment are referred to the program by their oncologist for a formal fertility preservation consult when they are presumed to have moderate to highly gonadotoxic treatment. Fertility preservation counseling is provided by a multidisciplinary team, and all options are presented to patients. From here, a research coordinator presents the research protocol (if patients are interested in ovarian/testicular tissue cryopreservation), including risks and benefits of participation. The procedure (if required) is scheduled at the same time as another required procedure, to lessen both anesthesia risks and out-of-pocket costs for patients. Post-procedure, a protocol is in place for patient follow-up and tissue/specimen handling. Patients’ insurance typically covers procedures, and patients are responsible for annual tissue storage fees. Here, we present the clinical outcomes following the establishment of a hospital-wide fertility preservation program.
Methods
Study subjects
Patients were identified using Mayo Clinic’s Advanced Cohort Explorer. We conducted a medical record review of children admitted to Pediatric Hematology/Oncology at or under 17 years of age at our institution (Table 1) from January of 2014 to January of 2020. Patients were stratified by admission prior to or after program establishment in August of 2016. Patients were filtered for oncology cases that had most or all of oncology care provided by our institution and had potentially gonadotoxic treatment as part of their care (i.e., radiation and/or chemotherapy).
Table 1.
Filtering and stratification for study subjects
| Filter | Pre-program | Post-program |
|---|---|---|
| Initial patients identified from search | 350 | 467 |
| Removed for non-cancer diagnosis | 135 | 210 |
| Removed for non-gonadotoxic treatment (i.e., surgery only) | 17 | 20 |
| Final number of patients included in analysis | 198 | 237 |
Data abstraction
Basic and clinical demographics including Tanner staging were collected for each patient as well as information regarding their cancer diagnosis. Discussions of impaired fertility, fertility preservation consults, and fertility preservation incidence were recorded for each patient.
Statistical analysis
Fisher’s exact tests with a significant p value of 0.05 were conducted to compare proportions between pre- and post-program factors. All statistical analyses were conducted in RStudio version 1.1383.
Results
Case series demographics
Of 435 children studied, 198 were admitted prior to the establishment of a fertility preservation program, and 237 were seen after (Table 2). Demographics between each group did not statistically differ. Ages between groups ranged from 0 to 17 years (median = 8 years). Approximately 12% of all patients were deceased as of February 2020. Patients consisted of marginally more males than females. The majority of patients self-identified as White and not of Hispanic or Latinx ethnicity.
Table 2.
Demographics of pre- and post-program study subjects
| All patients (N = 483) | Pre-program (N = 198) | Post-program (N = 237) | |
|---|---|---|---|
| Dates | 2014–2019 | Jan 2014–Aug 2016 | Aug 2016–Dec 2019 |
| Age in years (mean) | 0–17 (8.3) | 0–17 (8.3) | 0–17 (8.3) |
| Deceased patients (%) | 12% | 17% | 8% |
| Male:female ratio | 1.34 | 1.22 | 1.44 |
| Race (%) | |||
| American Indian/Alaskan Native | 0% | 1% | 0% |
| Asian | 2% | 2% | 2% |
| Black/African American | 4% | 5% | 3% |
| Native Hawai’ian/Pacific Islander | 1% | 1% | 1% |
| White | 81% | 81% | 81% |
| Other/unknown | 13% | 11% | 14% |
| Ethnicity (%) | |||
| Hispanic/Latinx | 6% | 5% | 6% |
| Not Hispanic or Latinx | 90% | 94% | 87% |
| Unknown | 4% | 2% | 7% |
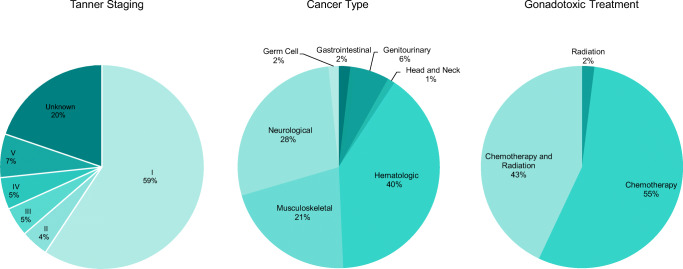
Clinical characteristics of patients were well-distributed (Fig. 1). Tanner stages ranged from I to V. Fifty-nine percent of patients were pre-pubertal (Tanner I) and 7% were post-pubertal (Tanner V). Eighty-nine percent of patients had either a hematologic, musculoskeletal, or neurological cancer type. Gonadotoxic treatment consisted of chemotherapy only in 55% of patients, radiation only in 2%, and both chemotherapy and radiation in 43%. Among all patients who underwent a fertility preservation option (both prior to and after a fertility preservation program), 58% consisted of ovarian or testicular tissue cryopreservation and 42% consisted of oocyte or sperm banking.
Fig. 1.
Patient demographics. Tanner stage, cancer type, and gonadotoxic treatment distributions of patient cohort. Patients were predominantly (59%) Tanner stage I. Majority (89%) of patients had a hematologic, musculoskeletal, or neurological malignancy. About half of patients (55%) had chemotherapy only as gonadotoxic therapy, 2% had radiation only, and 43% had both chemotherapy and radiation
Fertility preservation program outcomes
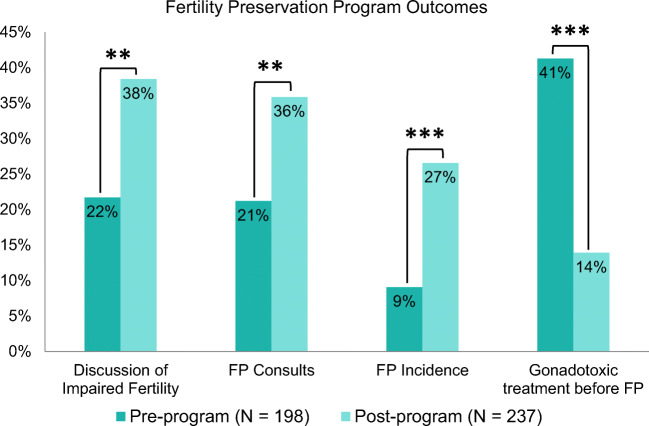
Following the establishment of a fertility preservation program, there was an increase in the proportion of patient discussions with any of provider involved in their cancer care of impaired fertility (22 to 38%, p = 0.007), fertility preservation consults (21 to 36%, p = 0.01), and incidence of fertility-preserving options such as sperm, oocyte, or tissue cryopreservation (9 to 27%, p < 0.001). The proportion of patients who received fertility preservation consults after receiving gonadotoxic treatment decreased from 41 to 14% following program establishment (p < 0.001; Fig. 2).
Fig. 2.
Fertility preservation program outcomes. Proportion of patients who had discussions of impaired fertility with their oncologist, had a fertility preservation consult, or underwent fertility preservation significantly increased between pre-program (blue bars) and post-program (orange). The proportion of those who had gonadotoxic treatment before their FP consults significantly decreased. Statistical comparisons shown are between pre- and post-program patients. Asterisks represent significance level (* p < 0.05, ** p < 0.01, *** p < 0.001)
Of post-program patients who underwent fertility preservation, ovarian or testicular cryopreservation was performed in 74% of patients (46/62). When ovarian and testicular tissue cryopreservation was removed from analysis, incidence of fertility preservation did not differ following program establishment (9 to 7%, p = 0.476).
Program outcomes by pubertal status
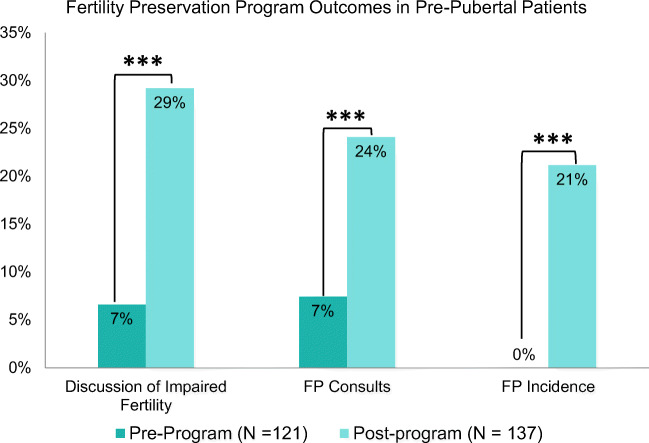
This trend was particularly noted among pre-pubertal children (Tanner I). Discussions of impaired fertility (7 to 29%, p < 0.001) and fertility preservation consults (7 to 24%, p = 0.002) increased after the establishment of a fertility preservation program. Consequently, fertility preservation procedures among pre-pubertal children increased from none to 21% with the establishment of a fertility preservation program (Fig. 3).
Fig. 3.
Program outcomes in subset of pre-pubertal patients. Proportion of pre-pubertal (Tanner I) patients who had discussions of impaired fertility with their oncologist, had a fertility preservation (FP) consult, or underwent fertility preservation significantly increased between pre-program (blue bars) and post-program (orange bars). Statistical comparisons shown are between pre- and post-program patients. Asterisks represent significance level (* p < 0.05, ** p < 0.01, *** p < 0.001)
Among pubertal and post-pubertal patients (Tanner II–V), there were no statistical differences between pre- and post-program patients in fertility impairment discussions (57 to 67%, p = 0.734), fertility preservation consults (55 to 65%, p = 0.731), or fertility preservation incidence (33 to 41%, p = 0.689).
Program outcomes by patient gender
In male patients, fertility preservation incidence more than doubled (14 to 30%, p = 0.017). Female patients saw a more dramatic effect: fertility preservation increased more than seven-fold (3 to 22%, p < 0.001; Fig. 4).
Fig. 4.
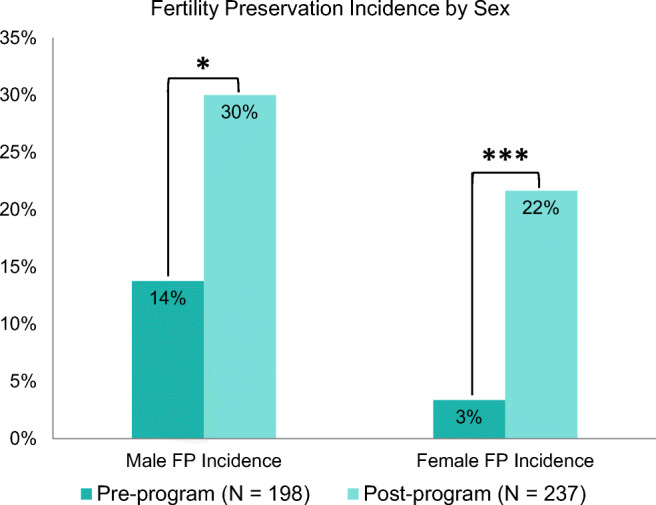
Patient gender differences in program outcomes. Proportion of male and female patients who underwent fertility preservation significantly increased between pre-program (blue bars) and post-program (orange bars). Statistical comparisons shown are between pre- and post-program patients. Asterisks represent significance level (* p < 0.05, ** p < 0.01, *** p < 0.001)
Provider discussions of fertility
When patients were not physician-referred for fertility preservation (FP), only 1% underwent a FP procedure through self-referral (3/299). In contrast, when patients were referred for an FP consult, 84% (115/137) received an FP consult and 64% (88/137) underwent an FP procedure (p < 0.001).
Discussion
The establishment of a hospital- and clinic-wide fertility preservation program significantly increased the number of fertility consults and subsequently fertility preservation procedures undergone by patients. Implementing fertility preservation programs at other institutions has similarly increased fertility preservation consultations and incidence of fertility preservation procedures [17–19, 22, 23].
Unfortunately, many patients have already undergone gonadotoxic treatment at the time of their first fertility preservation consult and therefore may have already experienced some gonadotoxicity. Of note, this study found that the proportion of patients who received fertility preservation consults after gonadotoxic treatment decreased after program establishment, inferring that the existence of a formal program results in earlier consults and provides more benefit to patients facing gonadotoxic treatments.
This study found the most significant increase in fertility preservation consults among pre-pubertal patients, leading to one in five pre-pubertal patients undergoing fertility preservation following program establishment. Many barriers exist for pre-pubertal patients to receive fertility preservation [24, 25], including the experimental nature of particular fertility preservation options for this population. The establishment of a formal fertility preservation program, including the introduction of experimental procedures such as ovarian/testicular tissue cryopreservation, therefore provides significant benefit to childhood cancer patients that otherwise would have no access to fertility preservation options.
The establishment of a fertility preservation program introduced ovarian and testicular tissue cryopreservation. This proved to be a popular option: almost 3 of 4 children who underwent any fertility preservation option post-program chose to undergo these procedures. While post-pubertal youth have the option of undergoing egg or sperm freezing, these options are patient-specific and may not always be plausible. Sperm freezing may be an uncomfortable option for youth, and egg freezing often delays cancer treatment by weeks. For both pre-pubertal and post-pubertal patients, ovarian/testicular tissue cryopreservation is a popular option.
In our cohort, there was a greater increase in fertility preservation incidence for females than males following program establishment. Generally, male patients more frequently have discussions of fertility preservation prior to cancer treatment compared to females [11]. Such gender-based differences are likely due to the options available to each. Pubertal males are often able to provide semen samples for cryopreservation quickly and easily, prior to initiation of cancer treatment. However, options available to females, such as oocyte cryopreservation, can be costly and delay treatment [26]. In December of 2019, the American Society of Reproductive Medicine (ASRM) deemed ovarian tissue cryopreservation as non-experimental and an acceptable method for fertility preservation as clinical care for both pre- and post-pubertal girls [6]. This has been predicted by national associations [27, 28], as many live births and ongoing pregnancies have been achieved through this method of fertility preservation since 2004 [27]. Ovarian tissue cryopreservation as standard of care will provide patients with more established fertility preservation choices that will not delay cancer treatment, as well as potentially ease the financial burden that is associated with the surgery and storage of tissue.
This study demonstrated that when patients discussed fertility with a provider in their cancer care, they were much more likely to undergo a fertility preservation option. Those without medical oncologists are less likely to be told that their cancer treatment may affect fertility, compared to those with a medical oncologist [11]. This indicates a need for further provider knowledge of fertility preservation options. When providers are provided with an educational program regarding fertility preservation options, they are more likely to educate both coworkers and patients on the topic [29]. While establishing a multidisciplinary program offers more provider awareness, there is still room to improve through further education of providers.
There are some limitations to the current study. The current study reviewed the outcomes of pediatric cancer patients only. However, many children face diagnoses that affect their fertility outside of oncology, including certain endocrine, genetic, neurologic, rheumatologic, and metabolic diseases. Furthermore, transgender youth would be eligible for fertility preservation prior to starting hormone blockers. There remains a need for pediatric fertility preservation in the non-oncological setting [30]. Our program extends fertility preservation options beyond cancer. Further studies are recommended to examine the clinical outcomes from fertility program establishment in this patient population. Of note, all cancer patients were included in this study, with no exclusion for those who were too ill to be offered fertility preservation. Furthermore, gonadotoxic treatment was presumed as chemotherapy and/or radiation in cancer treatment, but there are several chemotherapy/radiation regimens that are not gonadotoxic. Had these patients been excluded, it is presumed that a much higher proportion of patients would be offered fertility preservation.
Our institution increased consults and fertility preservation options undergone through the establishment of an institution-wide, multidisciplinary fertility preservation program. Pre-pubertal and female patients had particular benefit, as they had limited options outside of experimental procedures. More work to educate providers and include divisions outside of oncology is recommended to broaden the outcomes that a fertility preservation program may provide.
Acknowledgments
We thank all members of Pediatric Hematology/Oncology, Pediatric Endocrinology, Pediatric Surgery, Urology, Obstetrics and Gynecology, Pediatrics, and the In Vitro Fertilization lab at Mayo Clinic, Rochester, for their ongoing support in the success of this project.
Author contributions
SB, VBJ, RSH, and AC designed the study. SB and VBJ performed data abstraction. All authors discussed the results and contributed to the final manuscript.
Data availability
The data that support the findings of this study are available upon reasonable request from the corresponding author (AC). The data are not publicly available due to them containing information that could compromise research participant privacy/consent.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This research study was conducted retrospectively from data obtained for clinical purposes. We consulted extensively with the Mayo Clinic Institutional Review Board who determined that our study did not need ethical approval. An IRB official waiver of ethical approval was granted from the Mayo Clinic Institutional Review Board (Study # 19-006156). Methods were carried out in accordance with relevant guidelines and regulations.
Consent to participate
All patients included in this study have authorized their records to be used for research through the Minnesota Research Authorization.
Consent for publication
All patients included in this study have authorized their records to be used for research through the Minnesota Research Authorization.
Code availability
Not applicable.
Footnotes
The original online version of this article was revised: the other affiliation of Reda S. Hussein, Department of Obstetrics and Gynecology, Faculty of Medicine, Assiut University, Assiut, Egypt, should be included in the article.
Supriya Behl and Vidhu B. Joshi equally contributed to this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
2/15/2021
A Correction to this paper has been published: 10.1007/s10815-021-02091-7
References
- 1.Howlader NNA, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA. SEER cancer statistics review, 1975-2016. Bethesda: National Cancer Institute; 2019. [Google Scholar]
- 2.Hudson MM, Mertens AC, Yasui Y, Hobbie W, Chen H, Gurney JG, Yeazel M, Recklitis CJ, Marina N, Robison LR, Oeffinger KC, Childhood Cancer Survivor Study Investigators Health status of adult long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. JAMA. 2003;290(12):1583–1592. doi: 10.1001/jama.290.12.1583. [DOI] [PubMed] [Google Scholar]
- 3.Robison LL, Hudson MM. Survivors of childhood and adolescent cancer: life-long risks and responsibilities. Nat Rev Cancer. 2014;14(1):61–70. doi: 10.1038/nrc3634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vakalopoulos I, Dimou P, Anagnostou I, Zeginiadou T. Impact of cancer and cancer treatment on male fertility. Hormones (Athens) 2015;14(4):579–589. doi: 10.14310/horm.2002.1620. [DOI] [PubMed] [Google Scholar]
- 5.Lawrenz B, Mahajan N, Fatemi HM. The effects of cancer therapy on women’s fertility: what do we know now? Future Oncol. 2016;12(14):1721–1729. doi: 10.2217/fon-2015-0004. [DOI] [PubMed] [Google Scholar]
- 6.Practice Committee of the American Society for Reproductive Medicine. Electronic address aao Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112(6):1022–1033. doi: 10.1016/j.fertnstert.2019.09.013. [DOI] [PubMed] [Google Scholar]
- 7.Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, Wallace WH, Wang ET, Loren AW. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;36(19):1994–2001. doi: 10.1200/JCO.2018.78.1914. [DOI] [PubMed] [Google Scholar]
- 8.Klipstein S, Fallat ME, Savelli S, Committee On B, Section On HO, Section OS. Fertility preservation for pediatric and adolescent patients with cancer: medical and ethical considerations. Pediatrics. 2020;145(3). 10.1542/peds.2019-3994. [DOI] [PubMed]
- 9.van den Berg H, Langeveld NE. Parental knowledge of fertility in male childhood cancer survivors. Psychooncology. 2008;17(3):287–291. doi: 10.1002/pon.1248. [DOI] [PubMed] [Google Scholar]
- 10.Hohmann C, Borgmann-Staudt A, Rendtorff R, Reinmuth S, Holzhausen S, Willich SN, Henze G, Goldbeck L, Keil T. Patient counselling on the risk of infertility and its impact on childhood cancer survivors: results from a national survey. J Psychosoc Oncol. 2011;29(3):274–285. doi: 10.1080/07347332.2011.563344. [DOI] [PubMed] [Google Scholar]
- 11.Shnorhavorian M, Harlan LC, Smith AW, Keegan TH, Lynch CF, Prasad PK, et al. Fertility preservation knowledge, counseling, and actions among adolescent and young adult patients with cancer: a population-based study. Cancer. 2015;121(19):3499–3506. doi: 10.1002/cncr.29328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Oncologists’ attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol. 2002;20(7):1890–1897. doi: 10.1200/JCO.2002.07.174. [DOI] [PubMed] [Google Scholar]
- 13.Kohler TS, Kondapalli LA, Shah A, Chan S, Woodruff TK, Brannigan RE. Results from the survey for preservation of adolescent reproduction (SPARE) study: gender disparity in delivery of fertility preservation message to adolescents with cancer. J Assist Reprod Genet. 2011;28(3):269–277. doi: 10.1007/s10815-010-9504-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Panagiotopoulou N, van Delft FW, Hale JP, Stewart JA. Fertility preservation care for children and adolescents with cancer: an inquiry to quantify professionals’ barriers. J Adolesc Young Adult Oncol. 2017;6(3):422–428. doi: 10.1089/jayao.2016.0087. [DOI] [PubMed] [Google Scholar]
- 15.Panagiotopoulou N, Ghuman N, Sandher R, Herbert M, Stewart JA. Barriers and facilitators towards fertility preservation care for cancer patients: a meta-synthesis. Eur J Cancer Care (Engl). 2018;27(1). 10.1111/ecc.12428. [DOI] [PubMed]
- 16.Garvelink MM, ter Kuile MM, Bakker RM, Geense WJ, Jenninga E, Louwe LA, et al. Women’s experiences with information provision and deciding about fertility preservation in the Netherlands: ‘satisfaction in general, but unmet needs’. Health Expect. 2015;18(5):956–968. doi: 10.1111/hex.12068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carlson CA, Kolon TF, Mattei P, Hobbie W, Gracia CR, Ogle S, Ginsberg JP. Developing a hospital-wide fertility preservation service for pediatric and young adult patients. J Adolesc Health. 2017;61(5):571–576. doi: 10.1016/j.jadohealth.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 18.Ben-Aharon I, Abir R, Perl G, Stein J, Gilad G, Toledano H, Elitzur S, Avrahami G, Ben-Haroush A, Oron G, Freud E, Kravarusic D, Ben-Arush M, Herzel G, Yaniv I, Stemmer SM, Fisch B, Ash S. Optimizing the process of fertility preservation in pediatric female cancer patients-a multidisciplinary program. BMC Cancer. 2016;16:620. doi: 10.1186/s12885-016-2584-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewin J, Ma JMZ, Mitchell L, Tam S, Puri N, Stephens D, Srikanthan A, Bedard P, Razak A, Crump M, Warr D, Giuliani M, Gupta A. The positive effect of a dedicated adolescent and young adult fertility program on the rates of documentation of therapy-associated infertility risk and fertility preservation options. Support Care Cancer. 2017;25(6):1915–1922. doi: 10.1007/s00520-017-3597-8. [DOI] [PubMed] [Google Scholar]
- 20.Kelvin JF, Thom B, Benedict C, Carter J, Corcoran S, Dickler MN, Goodman KA, Margolies A, Matasar MJ, Noy A, Goldfarb SB. Cancer and fertility program improves patient satisfaction with information received. J Clin Oncol. 2016;34(15):1780–1786. doi: 10.1200/JCO.2015.64.5168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Javed A, Khan Z, Pittock ST, Jensen JR. Options for fertility preservation in children. Pediatr Endocrinol Rev. 2018;15(3):223–233. doi: 10.17458/per.vol15.2018.jkpj.fertilitypreservation. [DOI] [PubMed] [Google Scholar]
- 22.Ben-Aharon I, Ash S, Ben-Haroush A, Perl G, Oron G, Pinkas H, Freud N, Kravarusic D, Abir R, Sapir O, Wiznitzer A, Brenner B, Yaniv I, Stemmer S, Fisch B. Fertility preservation in young cancer patients-can we optimize the path? Harefuah. 2017;156(5):326–329. [PubMed] [Google Scholar]
- 23.Vu JV, Llarena NC, Estevez SL, Moravek MB, Jeruss JS. Oncofertility program implementation increases access to fertility preservation options and assisted reproductive procedures for breast cancer patients. J Surg Oncol. 2017;115(2):116–121. doi: 10.1002/jso.24418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jurewicz M, Hillelsohn J, Mehta S, Gilbert BR. Fertility preservation in pubertal and pre-pubertal boys with cancer. Pediatr Endocrinol Rev. 2018;15(3):234–243. doi: 10.17458/per.vol15.2018.jhmg.fertilitypubertalboys. [DOI] [PubMed] [Google Scholar]
- 25.Wallace WH, Kelsey TW, Anderson RA. Fertility preservation in pre-pubertal girls with cancer: the role of ovarian tissue cryopreservation. Fertil Steril. 2016;105(1):6–12. doi: 10.1016/j.fertnstert.2015.11.041. [DOI] [PubMed] [Google Scholar]
- 26.Nieman CL, Kinahan KE, Yount SE, Rosenbloom SK, Yost KJ, Hahn EA, et al. Fertility preservation and adolescent cancer patients: lessons from adult survivors of childhood cancer and their parents. Cancer Treat Res. 2007;138:201–217. doi: 10.1007/978-0-387-72293-1_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Christianson MS, Lindheim SR. Pediatric ovarian tissue cryopreservation: time to lift the experimental label? Fertil Steril. 2018;109(5):805–806. doi: 10.1016/j.fertnstert.2018.03.035. [DOI] [PubMed] [Google Scholar]
- 28.Forman EJ. Ovarian tissue cryopreservation: still experimental? Fertil Steril. 2018;109(3):443–444. doi: 10.1016/j.fertnstert.2017.12.031. [DOI] [PubMed] [Google Scholar]
- 29.Takeuchi E, Kato M, Miyata K, Suzuki N, Shimizu C, Okada H, Matsunaga N, Shimizu M, Moroi N, Fujisawa D, Mimura M, Miyoshi Y. The effects of an educational program for non-physician health care providers regarding fertility preservation. Support Care Cancer. 2018;26(10):3447–3452. doi: 10.1007/s00520-018-4217-y. [DOI] [PubMed] [Google Scholar]
- 30.Vakeesan B, Weidman DR, Maloney AM, Allen L, Lorenzo AJ, Gupta AA. Fertility preservation in pediatric subspecialties: a pilot needs assessment beyond oncology. J Pediatr. 2018;194:253–256. doi: 10.1016/j.jpeds.2017.10.072. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available upon reasonable request from the corresponding author (AC). The data are not publicly available due to them containing information that could compromise research participant privacy/consent.