Clinical Implications.
-
•
The District of Columbia did not experience the “September asthma epidemic” of exacerbations during the current novel coronavirus pandemic. Emergency department visits, hospitalizations, and intensive care unit admissions for asthma during the fall season were significantly reduced compared with previous years. Careful monitoring is necessary to recognize and prepare for childhood asthma morbidity to return to its prepandemic levels.
In the United States, pediatric asthma exacerbations peak during the fall season because of several specific seasonal factors including increased spread of common respiratory viruses (especially human rhinovirus) associated with schools reopening, increased exposure to indoor aeroallergens, changing outdoor aeroallergen exposures, and colder weather.1 , 2 In early 2020, social distancing, quarantines, and school closures enacted to reduce coronavirus disease 2019 (COVID-19) also reduced pediatric respiratory illnesses and asthma morbidity.3, 4, 5 Two studies demonstrated fewer emergency department (ED) visits for pediatric asthma during the spring of 2020 as compared with previous years,3 , 5 but it remained uncertain whether 2020 would have the typical fall seasonal peak. In addition, overall health care utilization declined early during the pandemic in part because of fear of exposure to COVID-19,6 meaning that patients might present to EDs with more severe asthma exacerbations due to delays in seeking care. We therefore sought to determine, among children with asthma residing in the District of Columbia (DC), whether there was (1) a decrease in asthma-related ED visits and hospitalizations and (2) an increase in the acuity of asthma exacerbations presenting to our hospital during the 2020 fall season as compared with previous fall seasons.
Population-based demographic and health care utilization data for children and adolescents with asthma aged 2 to 17 years residing in DC between January 2016 and November 2020 were assembled from an existing electronic data warehouse maintained at Children's National Hospital (CNH). This warehouse uses hospital electronic health records to identify children with current asthma and track their asthma-related utilization at CNH. Of note, a large majority of all ED visits and hospitalizations by DC youth aged 2 to 17 years are made to CNH (>90% in 2018).7
Current asthma is strictly defined as having an International Classification of Diseases, Ninth Revision or International Classification of Diseases, Tenth Revision asthma diagnosis with at least 1 asthma-related visit (ED, hospitalization, or outpatient) in the preceding 24 months. An ED visit, hospitalization, or pediatric intensive care unit (PICU) admission is defined as asthma-related if 1 or both of the top 2 discharge diagnoses are from a predetermined list of asthma-related codes. For each month, we calculated (1) the total number of asthma-related ED visits, hospitalizations, and PICU admissions, (2) the ratio of asthma-related hospitalizations to ED visits, and (3) the ratio of asthma-related PICU admissions to ED visits. These ratios allow us to approximate the overall acuity of asthma exacerbations by month. We defined the fall season as September through November. t tests were used to compare the means of each outcome variable between the 2020 fall season (pandemic) and combined previous fall seasons (prepandemic, 2016-2019). This study was approved by CNH's Institutional Review Board.
Between 2016 and 2020, children and adolescents with asthma experienced 17,423 asthma-related ED visits, 3,413 asthma-related hospitalizations, and 530 asthma-related PICU admissions. Of these, 5422 ED visits (31.1%), 1056 hospitalizations (30.9%), and 175 PICU admissions (33.0%) occurred during the fall season.
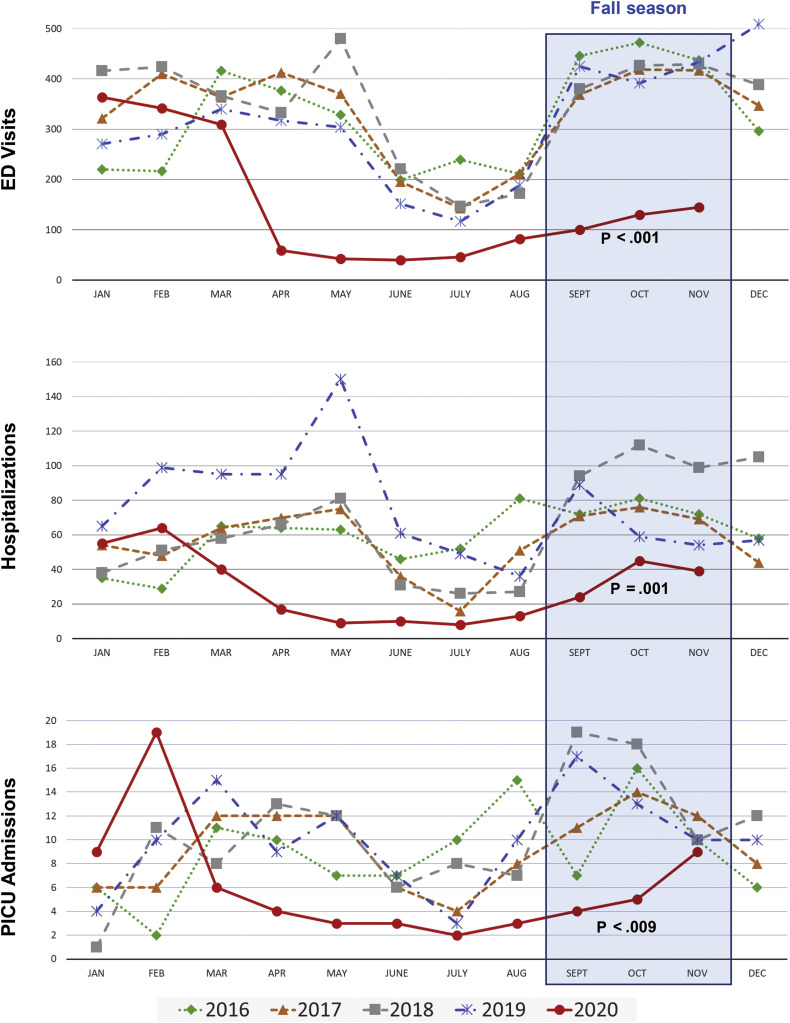
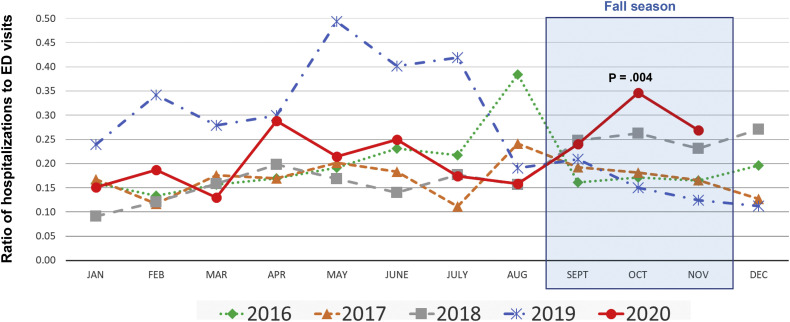
Asthma-related ED visits, hospitalizations, and PICU admissions fell in April 2020 shortly after the pandemic began and remained lower than previous years through the summer and fall (Figure 1 ). The monthly mean number of these events in fall 2020 was significantly less than in previous fall seasons (mean ± SD, 125 ± 23 vs 421 ± 29 ED visits/mo, P < .001; 36 ± 11 vs 79 ± 17 hospitalizations/mo, P = .001; 6 ± 3 vs 13 ± 4 PICU admissions/mo, P = .009). However, the ratio of hospitalizations to ED visits (Figure 2 ) was higher during the pandemic fall season as compared with prepandemic years (monthly means ± SD, 0.29 ± 0.06 vs 0.19 ± 0.04; P = .004). A similar significant increase was seen for the ratio of PICU admissions to ED visits (monthly means ± SD, 0.05 ± 0.01 vs 0.03 ± 0.01; P = .035).
Figure 1.
Asthma-related health care utilization by month (2016-2020). Asthma-related ED visits, hospitalizations, and PICU admissions over time by month between 2016 and 2020. The P values are for comparisons of mean monthly numbers for fall seasons of 2016-2019 to fall season of 2020.
Figure 2.
Ratio of asthma-related hospitalizations to ED visits by month (2016-2020). Ratio of asthma-related hospitalizations to ED visits by month between 2016 and 2020. The P value is for a comparison of mean monthly numbers for fall seasons 2016-2019 to fall season of 2020.
Consistent with earlier studies, we noted a reduction in asthma-related ED visits during the 2020 spring season shortly after the pandemic began.3 , 5 Our study extends this observation through fall 2020 and also demonstrates a significant decrease in asthma-related hospitalizations and PICU admissions. This continued reduction in pediatric asthma morbidity likely stems from various factors including mask-wearing, social distancing, and online school learning.
Furthermore, we found that the ratios of asthma-related hospitalizations and PICU admissions to ED visits were higher in fall 2020 as compared with prepandemic years, indicating children presenting to the ED during the pandemic were more likely to be acutely ill. Significant increases in these admission ratios are more impressive given that ED physicians may have been reluctant to place a child in a hospitalized setting during the pandemic. Perhaps, recent fear of presenting to health care facilities due to concerns over COVID-196 has kept children with mild asthma symptoms at home during the pandemic. If true, this could be a reason for a reduction in overall numbers. Before the pandemic, families from urban environments often used the ED as their first choice for exacerbations, even mild ones, that could be treated at home or in an outpatient office.8 In addition, children with more severe symptoms may have presented to the ED later and more ill, resulting in relatively higher hospitalization rates in fall 2020. There are other pandemic-triggered issues that may be related to a relative increase in the severity of asthma exacerbations presenting to the ED. Most notably, financial difficulties in an economic downturn could result in delayed refilling of controller medications, missed routine asthma care visits, and difficulties with transportation. Regardless, our findings of a significant absolute decrease in asthma-related hospitalizations and PICU admissions indicate that there has been a true reduction in exacerbations and not solely a reduction in health care utilization.
Although quarantine-associated improvement has been beneficial to the thousands of DC children and adolescents with asthma, it has detrimental effects as well. For example, not attending school may have an impact on learning and on physical and social development.9 In addition, the dramatic decline in asthma morbidity has an impact on ongoing asthma clinical intervention trials relying on exacerbations as a primary outcome. These trials will likely have to adjust power calculations and possibly increase sample sizes.
This study has limitations. Our analysis is drawn from a single metropolitan area; there may be different findings in other cities or in rural areas. In addition, states have differing social distancing guidelines with variable adherence to these guidelines. In DC, all public schools started the 2020 school year with remote learning. Replicating this study in a region where children returned to in-person school in the fall of 2020 would be an interesting comparison.
In conclusion, we demonstrated that DC did not experience its typical “September asthma epidemic” during the 2020 pandemic. This is a small silver lining in a very difficult year. As 2021 brings optimism for gradual improvements of the pandemic, careful monitoring is necessary to recognize and prepare for childhood asthma morbidity to return to prepandemic levels.
Acknowledgment
We thank Ranjodh Badh, Center for Pediatric Information at Children's National Hospital, for his effort in maintaining the electronic data warehouse.
Footnotes
This study was supported by a grant from EJF Philanthropies, Washington, DC, and by grant funding (grant no. K23AI104780) from the National Institutes of Health.
Conflicts of interest: W. J. Sheehan reports funding from the National Institutes of Health (NIH) and consulting fees from GlaxoSmithKline. S. J. Patel reports funding from the NIH and an honorarium from Pediatrics in Review journal. S. J. Teach reports funding from the NIH and EJF Philanthropies and royalty payments from UptoDate. The rest of the authors declare that they have no relevant conflicts of interest.
References
- 1.Sears M.R. Epidemiology of asthma exacerbations. J Allergy Clin Immunol. 2008;122:662–668. doi: 10.1016/j.jaci.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 2.Teach S.J., Gergen P.J., Szefler S.J., Mitchell H.E., Calatroni A., Wildfire J., et al. Seasonal risk factors for asthma exacerbations among inner-city children. J Allergy Clin Immunol. 2015;135:1465–1473.e5. doi: 10.1016/j.jaci.2014.12.1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kenyon C.C., Hill D.A., Henrickson S.E., Bryant-Stephens T.C., Zorc J.J. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allergy Clin Immunol Pract. 2020;8:2774–2776.e1. doi: 10.1016/j.jaip.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hatoun J., Correa E.T., Donahue S.M.A., Vernacchio L. Social distancing for COVID-19 and diagnoses of other infectious diseases in children. Pediatrics. 2020;146 doi: 10.1542/peds.2020-006460. e2020006460. [DOI] [PubMed] [Google Scholar]
- 5.Simoneau T., Greco K.F., Hammond A., Nelson K., Gaffin J.M. Impact of the COVID-19 pandemic on pediatric emergency department utilization for asthma. Ann Am Thorac Soc. 2021;18:717–719. doi: 10.1513/AnnalsATS.202007-765RL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Czeisler M.E., Marynak K., Clarke K.E.N., Salah Z., Shakya I., Thierry J.M., et al. Delay or avoidance of medical care because of COVID-19-related concerns—United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.District of Columbia Hospital Association (DCHA) Utilization Files. 2018. www.dcha.org Available from: Accessed December 21, 2020.
- 8.Kotwal M., Tran J., Kirby T., Krueger J., de la Torre D., Sheehan W.J. Emergency department use for non-emergent asthma-related symptoms. J Allergy Clin Immunol. 2019;143:AB223. [Google Scholar]
- 9.Black E., Ferdig R., Thompson L.A. K-12 virtual schooling, COVID-19, and student success. JAMA Pediatr. 2021;175:119–120. doi: 10.1001/jamapediatrics.2020.3800. [DOI] [PubMed] [Google Scholar]