Abstract
While the coronavirus disease 2019 (COVID-19) pandemic has multiple devastating public health and socio-economic effects across the world, Nigeria along with other West African countries is simultaneously faced with a recurrent Lassa fever epidemic. The complicating scenario is the similarity in the clinical manifestation of COVID-19 and Lassa fever, making the misdiagnosis of the initial presentation of both diseases a significant risk with an increased likelihood of co-infection. However, the strict implementation of COVID-19 infection prevention and control measures across Nigeria after the initial outbreaks concurrently resulted in the reduction of Lassa fever cases. The abrupt change in the behaviour of Lassa fever epidemiological data, which are attributable to the implementation of COVID-19 infection prevention and control measures at the national, sub-national and community levels, requires detailed investigation during and after the COVID-19 epidemic to elucidate the interactions and evolutionary dynamics of Lassa fever cases in Nigeria.
Keywords: Coronavirus disease 2019, infection prevention and control, Lassa fever, pandemic, public health
Introduction
Coronavirus disease 2019 (COVID-19), caused by the novel severe acute respiratory syndrome coronavirus (SARS-CoV-2) that emerged from Wuhan in China, has spread across 216 countries, areas or territories of the world as a pandemic with multiple devastating public health and socio-economic implications [1]. One of the public health implications of COVID-19 in West Africa and Nigeria in particular is the continuous Lassa fever epidemic that has recurred over recent decades. The COVID-19 pandemic coincides with another Lassa fever epidemic comprising a further increase in cases. COVID-19 in Nigeria has reached 56 256 confirmed cases with 1082 deaths nationwide and a case fatality ratio of 1.9% (14 September, 2020) [2], whereas Lassa fever reached 1078 confirmed cases with 225 deaths and 20.9% case fatality ratio [3].
Lassa fever is a severe zoonotic viral haemorrhagic disease caused by Lassa virus, a single-stranded RNA virus belonging to the Arenaviridae family. Since its emergence in 1968 from Lassa, a town in northeastern Nigeria, this virus has spread across Nigeria and the West African region causing severe outbreaks annually [4]. Human transmission of this virus occurs primarily through contact with contaminated excrement or body secretions of the natural reservoir of the virus, Mastomys natalensis (the multimammate rat), or secondarily through human-to-human transmission and hospital-acquired infection through contact with blood, secretions and excretions of infected persons [5]. Out of the 36 states in Nigeria, 27, including the Federal Capital Territory, are already affected with Lassa fever with the highest number of cases regularly occurring during the dry season (November–April) [6]. Furthermore, about 300 000–500 000 Lassa fever cases occur annually in West Africa with over 5000 deaths [7]. Within the last decade, there has been a steady rise in the incidence of Lassa fever not only in Nigeria but in the entire West African sub-region.
COVID-19 and Lassa fever co-epidemics in Nigeria: epidemiological dynamics
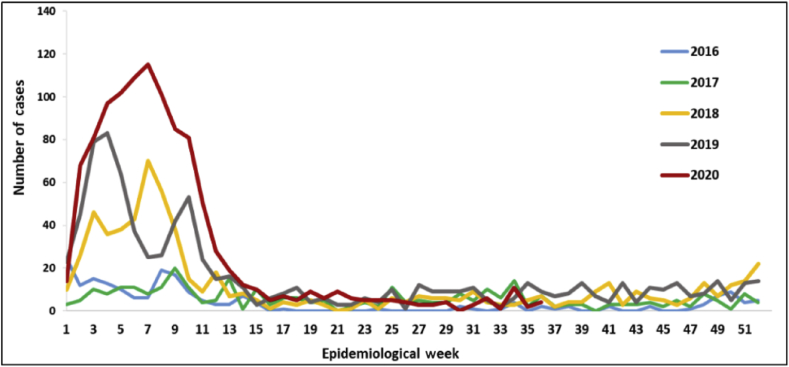
Together with other nations of the world, Nigeria is currently facing a COVID-19 epidemic, with the index case reported on 27 February 2020 [2]. Annually, the incidence of Lassa fever tends to increase from the later months of the rainy season and then peaks between March and May. This recurrent temporal pattern associated with Lassa fever means that the COVID-19 epidemic began shortly before Lassa fever reached its seasonal peak in Nigeria, resulting in COVID-19 and Lassa fever co-epidemics [8]. During epidemiological week 9 of 2020, when the first confirmed case of COVID-19 was reported in Nigeria, there was already an increase in the number of confirmed Lassa fever cases reportedly affecting 27 states, exceeding the number of cases reported in 2019 during the corresponding week [3]. The increased number of cases from the 2019 Lassa fever epidemic could have possibly resulted in a higher number of cases and the early rise of Lassa fever in 2020, with higher notifications than the average in the preceding year. Epidemiological data obtained from week 9 of 2020 showed Edo, Ondo and Taraba states to be the epicentres of Lassa fever, having the highest number of cases (Fig. 1; Table 1). Edo and Ondo states are coincidentally among the states worse stricken with the COVID-19 epidemic in Nigeria, however, curiously, after epidemiological week 36 of 2020, there was a significant decrease in the number of Lassa fever cases (Fig. 1, Table 2), coinciding with the implementation and intensification of the COVID-19 prevention and control measures by the states and federal governments, respectively. The decrease in Lassa fever cases in the above-mentioned states became noticeable in late April 2020 (Fig. 1; Table 3), the peak of recurrent Lassa fever outbreaks in Nigeria [3].
Fig. 1.
Comparative trend of confirmed Lassa fever cases by epidemiological weeks between 2016 and 2020.
Table 1.
Weekly and cumulative number of suspected and confirmed Lassa fever cases for weeks 1 to 9, 2020 (week 9, 24 February to 1 March 2020)
| States | Current week (Week 9) |
Deaths (confirmed cases) | Cumulative (Weeks 1–9) |
Deaths (confirmed cases) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases |
Cases |
|||||||||||
| Suspected | Confirmed | Trend | Probable | HCW | Suspected | Confirmed | Probable | HCW | ||||
| 1 | Abia | 4 | 32 | 2 | 2 | |||||||
| 2 | Adamawa | 11 | 3 | 1 | ||||||||
| 3 | Akwa Ibom | 1 | 8 | |||||||||
| 4 | Anambra | 1 | 17 | 1 | ||||||||
| 5 | Bauchi | 35 | 3 | 124 | 33 | 2 | 8 | |||||
| 6 | Bayelsa | 4 | ||||||||||
| 7 | Benue | 1 | 1 | 20 | 7 | 1 | ||||||
| 8 | Borno | 4 | 27 | 4 | 1 | 1 | ||||||
| 9 | Cross River | 6 | ||||||||||
| 10 | Delta | 9 | 69 | 13 | 3 | 1 | ||||||
| 11 | Ebonyi | 20 | 8 | 1 | 158 | 55 | 1 | 10 | ||||
| 12 | Edo | 176 | 31 | 1 | 1 | 1196 | 263 | 1 | 9 | 28 | ||
| 13 | Ekiti | 11 | ||||||||||
| 14 | Enugu | 2 | 30 | 7 | 1 | |||||||
| 15 | FCT | 4 | 32 | 1 | ||||||||
| 16 | Gombe | 2 | 27 | 5 | 1 | 1 | ||||||
| 17 | Imo | 2 | 15 | |||||||||
| 18 | Jigawa | 1 | 22 | 1 | ||||||||
| 19 | Kaduna | 13 | 96 | 6 | 1 | 1 | 3 | |||||
| 20 | Kano | 12 | 5 | 2 | 3 | 1 | ||||||
| 21 | Katsina | 35 | 5 | 1 | 1 | 2 | ||||||
| 22 | Kebbi | 4 | 1 | 20 | 3 | 2 | ||||||
| 23 | Kogi | 13 | 6 | 1 | 71 | 27 | 1 | 8 | ||||
| 24 | Kwara | 6 | ||||||||||
| 25 | Lagos | 6 | 23 | 1 | ||||||||
| 26 | Nasarawa | 4 | 28 | 6 | 3 | |||||||
| 27 | Niger | 1 | 8 | |||||||||
| 28 | Ogun | 2 | 30 | 1 | ||||||||
| 29 | Ondo | 83 | 25 | 3 | 603 | 246 | 4 | 34 | ||||
| 30 | Osun | 2 | 29 | 2 | ||||||||
| 31 | Oyo | 10 | 1 | |||||||||
| 32 | Plateau | 9 | 1 | 2 | 85 | 26 | 4 | |||||
| 33 | Rivers | 1 | 16 | 9 | 3 | |||||||
| 34 | Sokoto | 5 | 20 | 4 | 1 | |||||||
| 35 | Taraba | 16 | 9 | 3 | 82 | 42 | 2 | 1 | 17 | |||
| 36 | Yobe | 3 | ||||||||||
| 37 | Zamfara | 15 | ||||||||||
| Total | 421 | 85 | 0 | 1 | 11 | 3054 | 775 | 9 | 27 | 132 | ||
Abbreviation: FCT, Federal Capital Territory; HCW, health-care worker.
Note: Red triangle, increased; green triangle, decreased.
Table 2.
Weekly and cumulative number of suspected and confirmed Lassa fever cases for weeks 1 to 36, 2020 (31 August to 6 September 2020)
| States | Current week (Week 36) |
Deaths (confirmed cases) | Cumulative (Weeks 1–36) |
Deaths (confirmed cases) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases |
Cases |
|||||||||||
| Suspects | Confirmed | Trend | Probable | HCW | Suspected | Confirmed | Probable | HCW | ||||
| 1 | Abia | 59 | 5 | 2 | ||||||||
| 2 | Adamawa | 18 | 4 | 1 | ||||||||
| 3 | Akwa Ibom | 12 | ||||||||||
| 4 | Anambra | 32 | 2 | 1 | ||||||||
| 5 | Bauchi | 333 | 44 | 3 | 7 | 20 | ||||||
| 6 | Bayelsa | 6 | ||||||||||
| 7 | Benue | 47 | 9 | 1 | 4 | |||||||
| 8 | Borno | 31 | 4 | 1 | 1 | |||||||
| 9 | Cross River | 14 | ||||||||||
| 10 | Delta | 1 | 135 | 16 | 3 | 3 | ||||||
| 11 | Ebonyi | 4 | 324 | 76 | 1 | 22 | ||||||
| 12 | Edo | 26 | 2 | 2264 | 344 | 1 | 10 | 39 | ||||
| 13 | Ekiti | 14 | ||||||||||
| 14 | Enugu | 69 | 10 | 2 | ||||||||
| 15 | FCT | 71 | 3 | 2 | ||||||||
| 16 | Gombe | 50 | 9 | 1 | 1 | 2 | ||||||
| 17 | Imo | 20 | ||||||||||
| 18 | Jigawa | 29 | 1 | |||||||||
| 19 | Kaduna | 1 | 129 | 7 | 2 | 1 | 5 | |||||
| 20 | Kano | 14 | 5 | 2 | 3 | 1 | ||||||
| 21 | Katsina | 47 | 6 | 1 | 1 | 2 | ||||||
| 22 | Kebbi | 31 | 4 | 2 | ||||||||
| 23 | Kogi | 1 | 1 | 114 | 39 | 1 | 8 | |||||
| 24 | Kwara | 15 | ||||||||||
| 25 | Lagos | 32 | 1 | |||||||||
| 26 | Nasarawa | 46 | 9 | |||||||||
| 27 | Niger | 10 | 4 | |||||||||
| 28 | Ogun | 36 | 1 | |||||||||
| 29 | Ondo | 10 | 1 | 1223 | 374 | 1 | 13 | 68 | ||||
| 30 | Osun | 32 | 2 | |||||||||
| 31 | Oyo | 13 | 1 | |||||||||
| 32 | Plateau | 3 | 163 | 32 | 8 | |||||||
| 33 | Rivers | 21 | 9 | 3 | ||||||||
| 34 | Sokoto | 24 | 5 | 3 | ||||||||
| 35 | Taraba | 146 | 57 | 2 | 1 | 22 | ||||||
| 36 | Yobe | 5 | ||||||||||
| 37 | Zamfara | 18 | ||||||||||
| Total | 46 | 4 | 0 | 0 | 0 | 5647 | 1078 | 14 | 44 | 225 | ||
Abbreviation: FCT, Federal Capital Territory; HCW, health-care worker.
Note: Red triangle, increased; green triangle, decreased.
Table 3.
Weekly and cumulative number of suspected and confirmed Lassa fever cases for weeks 1 to 17, 2020 (week 7, 20–26 April 2020)
| States | Current week: (Week 17) |
Deaths (confirmed cases) | Cumulative (Weeks 1–17) |
Deaths (confirmed cases) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases |
Cases |
|||||||||||
| Suspects | Confirmed | Trend | Probable | HCW | Suspected | Confirmed | Probable | HCW | ||||
| 1 | Abia | 50 | 5 | 2 | ||||||||
| 2 | Adamawa | 17 | 4 | 1 | ||||||||
| 3 | Akwa Ibom | 1 | 12 | |||||||||
| 4 | Anambra | 26 | 2 | 1 | ||||||||
| 5 | Bauchi | 309 | 43 | 3 | 7 | 18 | ||||||
| 6 | Bayelsa | 1 | 6 | |||||||||
| 7 | Benue | 32 | 8 | 1 | 3 | |||||||
| 8 | Borno | 30 | 4 | 1 | 1 | |||||||
| 9 | Cross River | 12 | ||||||||||
| 10 | Delta | 4 | 109 | 16 | 3 | 3 | ||||||
| 11 | Ebonyi | 3 | 259 | 73 | 1 | 16 | ||||||
| 12 | Edo | 33 | 1 | 1761 | 321 | 1 | 10 | 39 | ||||
| 13 | Ekiti | 14 | ||||||||||
| 14 | Enugu | 6 | 59 | 10 | 2 | |||||||
| 15 | FCT | 68 | 3 | 2 | ||||||||
| 16 | Gombe | 2 | 1 | 44 | 9 | 1 | 1 | 2 | ||||
| 17 | Imo | 18 | ||||||||||
| 18 | Jigawa | 1 | 27 | 1 | ||||||||
| 19 | Kaduna | 126 | 7 | 2 | 1 | 5 | ||||||
| 20 | Kano | 13 | 5 | 2 | 3 | 1 | ||||||
| 21 | Katsina | 46 | 6 | 1 | 1 | 2 | ||||||
| 22 | Kebbi | 29 | 4 | 2 | ||||||||
| 23 | Kogi | 2 | 1 | 104 | 36 | 1 | 8 | |||||
| 24 | Kwara | |||||||||||
| 25 | Lagos | 31 | 1 | |||||||||
| 26 | Nasarawa | 44 | 8 | 3 | ||||||||
| 27 | Niger | 9 | ||||||||||
| 28 | Ogun | 36 | 1 | |||||||||
| 29 | Ondo | 30 | 5 | 891 | 318 | 1 | 6 | 44 | ||||
| 30 | Osun | 30 | 2 | |||||||||
| 31 | Oyo | 12 | 1 | |||||||||
| 32 | Plateau | 1 | 120 | 29 | 6 | |||||||
| 33 | Rivers | 1 | 21 | 9 | 3 | |||||||
| 34 | Sokoto | 23 | 5 | 3 | ||||||||
| 35 | Taraba | 134 | 56 | 2 | 1 | 21 | ||||||
| 36 | Yobe | 5 | ||||||||||
| 37 | Zamfara | 18 | ||||||||||
| Total | 85 | 8 | 0 | 0 | 0 | 4545 | 987 | 14 | 37 | 188 | ||
Abbreviation: FCT, Federal Capital Territory; HCW, health-care worker.
Note: Red triangle, increased; green triangle, decreased.
Long before the emergence of COVID-19, the WHO stated that because of the weakened infection prevention and control (IPC) measures at the sub-national level, Nigeria's capacity to effectively manage and control Lassa fever remains suboptimal [6]. However, to effectively mitigate the spread of COVID-19, strict implementation of COVID-19 control and prevention measures including social distancing, national lockdown, improved personal hygiene, avoidance of person-to-person contact, use of face masks, and the prohibition of public transport and inter-state travel were implemented across the country [9]. The science of the relationship between the intensification, implementation and community adherence to COVID-19 IPC measures and the decrease in Lassa fever cases require further detailed epidemiological studies to fully comprehend such epidemiological relationships and dynamics.
All countries of the world are presently battling against COVID-19. Therefore, the further epidemic of Lassa fever in Nigeria will pose tremendous challenges for the effective containment of COVID-19. The coexistence of SARS-CoV-2 and Lassa fever virus in countries where Lassa fever is endemic, like Nigeria, could result in co-infections with these two viruses. Although no study has examined the incidence of SARS-CoV-2 and Lassa fever virus co-infection in Nigeria, reports from dengue-endemic countries have reported increasing SARS-CoV-2–dengue virus co-infections in Bangladesh, Brazil, Colombia, Ecuador, India, Malaysia, Pakistan, Singapore and Thailand [[10], [11], [12], [13]].
More importantly, the clinical similarities in the presentation of patients with COVID-19 and Lassa fever—including fever, headache, general weakness, malaise, sore throat and cough from the onset of both infections to pneumonia, breathing difficulty, diarrhoea, disorientation, abdominal pain, low blood pressure, tremor, seizures, coma and multiple organ dysfunction at the later or severe stage [5,14,15]—complicate things further. Although some clinical signs and symptoms in a case series may initially point to COVID-19 or Lassa fever, this predictive and initial clinical variability should not be misplaced for validly guaranteed laboratory diagnosis. In some instances, the initial clinical manifestation of COVID-19 presents as fever together with joint and muscle pains, and general weakness without respiratory symptoms [[16], [17], [18]], which mimics the presentation of Lassa fever. Therefore, patients reporting to hospitals must be properly examined and explored for both diseases.
COVID-19-Lassa fever co-epidemics in Nigeria: contextual hypotheses
Given the abrupt change in the behaviour of Lassa fever epidemiological data, which is a departure from the recurring annual trend of Lassa fever outbreaks in Nigeria, some major hypotheses can be urgently raised. The first and most obvious is the underreporting or under-notification of Lassa fever cases, as we observed in our previous work [8]. This sudden decrease of Lassa fever cases could be attributable to the swift change in focus and disease surveillance by the government in mobilizing resources, agencies and personnel to urgently respond to the emergence of COVID-19 after the confirmation of the initial cases in Nigeria. These immediate steps taken by the governments at all levels could have led to delay or underreporting of Lassa fever cases at both national and sub-national levels. Furthermore, because Lassa fever and COVID-19 share similar clinical features, most of the febrile Lassa fever cases might have overlapped with COVID-19 cases in health centres [5,14]. As these two viral infections have similar diagnoses including RT-PCR, ELISA and other rapid serological detection assays, the possibility of misdiagnosis of these infections cannot be overemphasized. Pseudo-serological laboratory results for Lassa fever in individuals with COVID-19, and the converse, could further have led to severe public health implications. There is a need for health professionals to report suspected cases of both outbreaks side by side. An emerging challenge within the Nigerian health-care system is the proper understanding of the progression of the ‘masked’ or ‘underestimated’ Lassa fever epidemic with the simultaneous occurrence of ‘overhyped’ COVID-19 epidemic.
Another hypothesis is the reduction of Lassa fever morbidity as a result of the implementation of strict COVID-19 IPC measures, including social distancing, national lockdown, improved personal hygiene, avoidance of person-to-person contact, use of face masks and prohibition of inter-state travel [9]. This could have helped to reduce the true incidence of Lassa fever in Nigeria, and so mitigating the 2020 epidemic. Population movements, social interactions and personal hygiene are known to be major drivers of epidemics [19]. The recurrent Lassa fever outbreaks are often mediated by poor community hygiene, which supports rodent infestation of homes, inadequate personal hygiene, travel to epicentres and Lassa fever-prone areas, contact with infected persons, and nosocomially, mostly involving health-care workers [5]. The decrease in the incidence of Lassa fever after epidemiological week 36 of 2020, especially from states previously worse stricken, may be attributed to decreased Lassa fever morbidity resulting from the COVID-19 IPC measures being strictly implemented at the national, sub-national and community levels. The general adoption of these COVID-19 IPC measures across Nigeria may have significantly altered the epidemiological patterns of transmission of the Lassa fever virus, hence reducing the number of cases. At the community and population levels, social distancing has been reported to greatly reduce pathogen transmission [20]. The current social distancing scenario provides the opportunity of testing this hypothesis, which may be used to improve Lassa fever IPC measures at the national, sub-national and community levels. However, in-depth studies during and after the COVID-19 epidemic are necessary to consider the impact of population mobility and interactions data and evolution of the frequencies of Lassa fever cases in Nigeria.
The third hypothesis is the media overhype of the COVID-19 epidemic and the associated misinformation, misconception and rumours, which encourage stigmatization against individuals suspected of having COVID-19. Recently, reports emerging from Lagos, Nigeria's epicentre for COVID-19, indicated that numerous individuals flee isolation centres after testing positive for COVID-19 [21]. Similar reports have also emerged across Nigeria showing COVID-19-positive patients or individuals with suspected infections absconding from isolation centres, fleeing their homes or switching off their cell phones to avoid contact tracing [22]. As the initial clinical manifestation of Lassa fever is similar to COVID-19, individuals with unsuspected Lassa fever become afraid of been stigmatized, so refrain from seeking immediate medical attention. Furthermore, as the result of safety concerns regarding the handling and management of COVID-19 cases, non-urgent febrile individuals suspected of having COVID-19 are often referred to limited Nigeria Centre of Disease Control approved centres for testing, where strict precautions are observed. This disruption in health-care organization, which allows further diagnoses and explorations only after receiving COVID-19-negative results after several days, often leads to potentially dangerous delays in Lassa fever diagnosis and notification. The concurrent occurrence of COVID-19–Lassa fever co-epidemics in Nigeria necessitates simultaneous diagnoses of both infections for individuals suspected of having either of the diseases.
From our previous epidemiological study assessing knowledge, attitudes and practices regarding COVID-19 in Nigeria, 45.3% of the respondents held that prayer is also a potent measure for COVID-19 control and prevention [23]. In a similar study, Olapegba et al. [24] reported how the majority of the respondents maintained that prayer and religious beliefs could mitigate the COVID-19 epidemic in Nigeria. This agrees with the stern religious adherence and beliefs in the vast majority of the Nigerian population, making them resort to religious rituals and prayers without reporting suspected cases of disease or seeking medical attention. The observation and reports reinforced the hypothesis indicating a relationship between religious beliefs and the reduction of disease notification and/or reportage. This behavioural pattern in the Nigerian population transcends the COVID-19 epidemic but could be exhibited in other epidemics, including the recurrent Lassa fever epidemics.
Conclusion
Countries where Lassa fever is endemic, including Nigeria, are at high risk of increasing cases of co-infection and prolonged co-epidemics so long as SARS-CoV-2 and Lassa virus coexist and actively circulate within the population. Mitigating these viral diseases requires concerted and effective public health campaigns and strict implementation of IPC measures with the population eliminating Multimammate rat infestations of homes, improving community and personal hygiene, using face masks and practicing social distancing. Nigerian health-care systems should be organized to provide quality care including concurrent diagnoses of both COVID-19 and Lassa fever for individuals suspected of having either of these diseases or febrile patients without unnecessary delays due to constraints emanating from the COVID-19 pandemic.
Conflict of interest
None exist.
References
- 1.World Health Organization (WHO) Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available from:
- 2.Nigerian Centre for Disease Control (NCDC) COVID-19 situation report: situation report 198 sunday, 13 september, 2020. https://ncdc.gov.ng/diseases/sitreps/?cat=14&name=An%20update%20of%20COVID-19%20outbreak%20in%20Nigeria Available from:
- 3.Nigerian Centre for disease control (NCDC) Lassa fever situation report. https://ncdc.gov.ng/diseases/sitreps/?cat=5&name=An%20update%20of%20Lassa%20fever%20outbreak%20in%20Nigeria Epi Week 36: 31 August–6 September 2020. Available from:
- 4.Usuwa I.S., Akpa C.O., Umeokonkwo C.D. Knowledge and risk perception towards Lassa fever infection among residents of affected communities in Ebonyi State, Nigeria: implications for risk communication. BMC Pub Health. 2020;20:217. doi: 10.1186/s12889-020-8299-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Awosanya E.J. Post-epidemic awareness and knowledge of Lassa fever among residents in affected community in Ibadan, Oyo State, Nigeria. Vet World. 2018;11:1059–1063. doi: 10.14202/vetworld.2018.1059-1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO) Lassa fever—Nigeria. 2020. https://www.who.int/csr/don/20-february-2020-lassa-fever-nigeria/en/ Available from:
- 7.Ogbu O., Ajuluchukwu E., Uneke C. Lassa fever in west African sub-region: an overview. J Vector Borne Dis. 2007;44:1–11. [PubMed] [Google Scholar]
- 8.Reuben R.C., Danladi M.M.A., Pennap G.R. Is the COVID-19 pandemic masking the deadlier Lassa fever epidemic in Nigeria? J Clin Virol. 2020;128:104434. doi: 10.1016/j.jcv.2020.104434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nigerian Centre for Disease Control (NCDC) COVID-19 guideline. https://covid19.ncdc.gov.ng/guideline/ Available from:
- 10.Ayub J. Stung by dengue, patient dies of coronavirus co-infection in Bhopal, in the Times of India. https://timesofindia.indiatimes.com/city/bhopal/stung-by-dengue-patient-dies-of-coronavirus-co-infection-inbhopal/articleshow/75330826.cms Available from:
- 11.Miah A., Husna A. Coinfection, coepidemics of COVID-19, and dengue in dengue-endemic countries: a serious health concern. J Med Virol. 2020;1–2:jmv26269. doi: 10.1002/jmv.26269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ridwan R. COVID-19 and dengue: a deadly duo. Trop Doctor. 2020;50:270–272. doi: 10.1177/0049475520936874. [DOI] [PubMed] [Google Scholar]
- 13.Yan G., Lee C.K., Lam L. Covert COVID-19 and false-positive dengue serology in Singapore. Lancet Infect Dis. 2020;20:536. doi: 10.1016/S1473-3099(20)30158-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization (WHO) Lassa fever. https://www.who.int/news-room/fact-sheets/detail/lassa-fever Available from:
- 15.World Health Organization (WHO) Coronavirus. https://www.who.int/health-topics/coronavirus#tab=tab_3 Available from:
- 16.Du W., Yu J., Wang H., Zhang X., Zhang S., Li Q. Clinical characteristics of COVID-19 in children compared with adults in Shandong Province, China. Infection. 2020;48:445–452. doi: 10.1007/s15010-020-01427-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Han C., Duan C., Zhang S., Spiegel B., Shi H., Wang W. Digestive symptoms in COVID-19 patients with mild disease severity: clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol. 2020;115:916–923. doi: 10.14309/ajg.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li L.Q., Huang T., Wang Y.Q., Wang Z.P., Liang Y., Huang T.B. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92:577–583. doi: 10.1002/jmv.25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morens D.M., Folkers G.K., Fauci A.S. Emerging infections: a perpetual challenge. Lancet Infect Dis. 2008;8:710–719. doi: 10.1016/S1473-3099(08)70256-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prem K., Liu Y., Russell T.W., Kucharski A.J., Eggo R.M., Davies N. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adediran A. COVID-19: many people on the run in Lagos after testing positive – commissioner, in premium times. https://www.premiumtimesng.com/news/headlines/391982-covid-19-many-people-on-the-run-in-lagos-after-testing-positive-commissioner.html Available from:
- 22.Onwuzoo A. Nigeria can’t beat COVID-19 with patients fleeing isolation centres in Punch. https://healthwise.punchng.com/nigeria-cant-beat-covid-19-with-patients-fleeing-isolation-centres/ Available from:
- 23.Reuben R.C., Danladi M.M.A., Saleh D.A., Knowledge Ejembi P.E. Attitudes and practices towards COVID-19: an epidemiological survey in north-central Nigeria. J Comm Health. 2020 doi: 10.1007/s10900-020-00881-1. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olapegba P.O., Ayandele O., Kolawole S.O., Oguntayo R., Gandi J.C., Dangiwa A.L. A preliminary assess-ment of novel coronavirus (COVID-19) knowledge and perceptions in Nigeria. BMJ. 2020 epub ahead of print. [Google Scholar]