Abstract
Objective:
Cinnamon effect on blood pressure remains controversial. The present pilot study assessed cinnamon effect on blood pressure, and metabolic profile of stage 1 hypertension patients (S1HTN).
Materials and Methods:
This double-blind placebo-controlled randomized trial was conducted between June and October 2019, in Mashhad, Iran. Study inclusion criteria comprised S1HTN diagnosis, based on 24-hour ambulatory blood pressure monitoring (ABPM). Subjects were randomly assigned to two groups: cinnamon group (capsule, 1500 mg/day, 90 days) and placebo group. On days 0 and 90, ABPM derived systolic and diastolic blood pressure (SBP and DBP, respectively), blood lipid profile, and fasting blood sugar (FBS) were recorded.
Results:
The two groups did not differ significantly regarding vascular risk factors, educational status, lipid profile and blood pressure at baseline, except for lower HDL-c in cinnamon group (p=0.03). On day 90, there was no significant difference between two study groups for lipid profile and blood pressure. A statistically significant decrease in mean 24-hr SBP and mean day SBP was observed in the cinnamon group, while mean night SBP and mean night DBP were decreased significantly in the placebo group after 90 days. A statistically significant decrease in mean change of day value of SBP was found in the cinnamon group, compared to the placebo. On day 90, FBS remained practically unchanged but a significant increase in HDL-c (5.8 unit; p=0.01) and a significant decrease in LDL-c levels (17.7 unit; p=0.009) were observed in the cinnamon group compared to placebo group.
Conclusion:
Cinnamon caused a statistically significant decrease in mean ambulatory SBP but in a clinically moderate way, and lipid profile was significantly improved. Therefore, cinnamon might be considered a complementary treatment in subjects with S1HTN.
Key Words: Cinnamon, Hypertension, Cholesterol, HDL, LDL
Introduction
Several studies have shown the continuous relationship of blood pressure and cardiovascular disease (Lewington et al. 2002). This relationship seems to pertain to mild hypertension as well. For patients with stage 1 hypertension (S1HTN) defined by systolic blood pressure (SBP) of 140–159 mm Hg or diastolic blood pressure (DBP) of 90–99 mm Hg (Brook and Rajagopalan 2018; Whelton et al., 2018), evidence accumulates that treated patients with controlled blood pressure levels have significant lower rates of mortality and stroke (Thomopoulos et al. 2014). At the same time, ambulatory blood pressure measurements were found to be satisfactory correlated to all-cause mortality and vascular events in hypertensive African Americans while ambulatory measurements of SBP and DBP added to the identification of patients at risk beyond clinic blood pressure measurements (Yano et al. 2019).
In different corners of the world, cinnamon has been used by various cultures since long ago. The genus Cinnamon with nearly 250 species, contains trees of 10-17 m high that grow in Southern America, Southeastern Asia and Australia (Mousavi et al. 2019a). Cinnamon has been also traditionally used in cuisine as a flavoring/coloring agent (IM et al. 2014; Ranasinghe et al. 2013). Two main species of Cinnamomum, Cinnamomum zeylanicum and Cinnamomum cassia, exert antitumoral and antioxidant properties (Kawatra and Rajagopalan 2015). These two species mainly differ in terms of coumarin (1, 2-benzopyrone) level (Archer 1988). Nevertheless, both plant species contain phytochemicals such as eugenol, cinnamaldehyde, and camphor (Gruenwald et al. 2010). Generally, major chemicals reported to be present in cinnamon include coumarin, cinnamic acid, eugenol, and cinnamaldehyde that contribute to its pharmacological properties (e.g. anti-inflammatory, anti-oxidant, anti-diabetic, and anti-obesity) (Jayaprakasha and Rao 2011; Khan et al. 2003; Mousavi et al. 2019b). With respect to the blood lipid profile, cinnamon could decrease LDL-c but improve HDL-c (Allen et al. 2013; Askari et al. 2014; Khan et al. 2003). In a randomized double -blind control trial, 16-week administration of 3 g cinnamon per day to subjects with metabolic syndrome, led to significant decreases in fasting blood sugar (FBS), glycosylated haemoglobin (HbA1C) and body mass index (BMI) as well as marked improvements of blood pressure, serum total cholesterol, low-density lipoprotein (LDL-c) cholesterol, serum triglycerides (TG), and high-density lipoprotein (HDL-c) cholesterol (Jain et al. 2017).
Effect of cinnamon on blood pressure is a controversial issue as besides trials that reported its blood-pressure lowering effect, there are reports that found cinnamon ineffective in this context (Azimi et al. 2016; Vafa et al. 2012; Wainstein et al. 2011; Ziegenfuss et al. 2006). In 2013, Akilen et al. showed that based on data reported by three randomized clinical trials, administration of cinnamon (at doses ranging 0.5 to 2.4 g/day for 12 weeks) results in remarkable decrement of SBP and DBP in patients with prediabetes and diabetes type II (Akilen et al. 2013).
In an animal study done in normotensive (NR) rats, salt-loaded hypertensive rats (SLHR), L-NAME hypertensive rats (LNHR) and spontaneously hypertensive rats (SHR), effects of C. zeylanicum extract on the blood pressure were assessed. Intravenous administration of the extract led to a significant decrease in blood pressure in all animals (Nyadjeu et al. 2011). Similarly, a hypotensive effect was found for this extract in NTR and SLHR; also, authors suggested that the extract’s vasorelaxant activity in the rat thoracic aortic ring segments, is probably mediated through modulation of L-type voltage-sensitive calcium channels (Wansi et al. 2007).
To shed light on possible effects of cinnamon on blood glucose/lipid profile as well as blood pressure, in the present trial, we administered cinnamon to S1HTN patients for 90 days and evaluated the above-noted parameters.
Materials and Methods
General description of the study
The present study is a double-blind randomized placebo-controlled trial. The Ethics committee of Mashhad University of Medical Sciences approved the study protocol (approval No. IR.MUMS.MEDICAL.REC.1397.577). Also, the trial was registered at https://www.irct.ir/ (registration No.IRCT20191204045605N1). Before being enrolled, all participants received and signed a consent form. Trial registration, baseline/eligibility testing, allocation, and follow-up were all conducted in accordance with Consolidated Standards of Reporting Trials guidelines (Schulz et al. 2010).
Preparation of cinnamon/placebo capsules
Dried cinnamon )from Cinnamomum zeylanicum) was purchased from local market in Mashhad, Iran in June 2019. Cinnamon capsules (containing 500 mg of dried cinnamon powder) and placebo capsules (containing 500 mg lactose powder) were prepared at School of Pharmacy, Mashhad University of Medical Sciences. The capsules were identical in appearance.
Study subjects
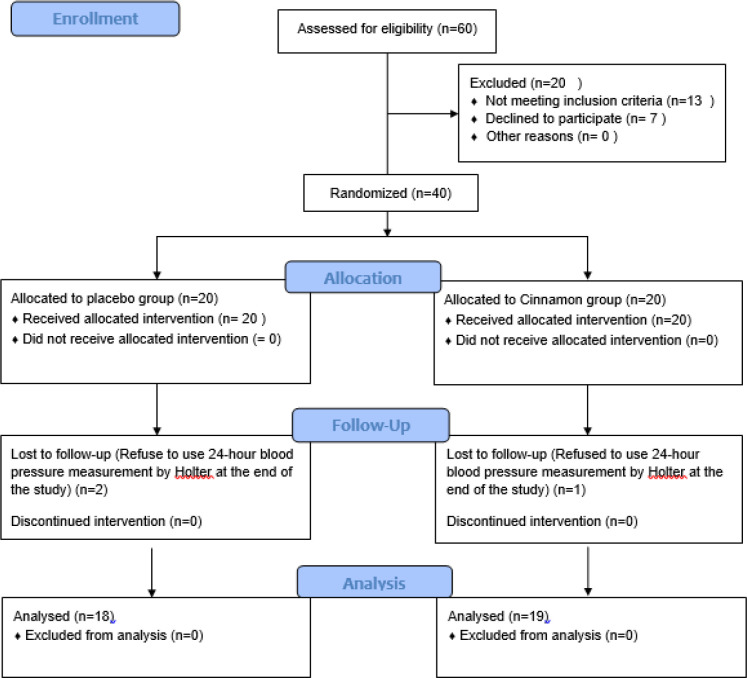
In the present trial, 40 individuals (age range 40-75 years old) of both sexes who referred to cardiology clinic of Imam Reza hospital, Mashhad University of Medical Sciences, during the “Iranian National Campaign for Blood Pressure Control”, between June and October 2019 and diagnosed with S1HTN (office clinic visits SBP>140mmHg and/or DBP>90mmHg, 24h ambulatory mean SBP>130 mmHg and DBP>80 mmHg) were enrolled in the study (Consort flowchart is provided in Figure 1).
Figure 1.
Consort flowchart of the present trial
Blood pressure was measured with the use of calibrated mercury sphygmomanometers, with the patient resting in the seated position for 2 minutes. A mean of two clinic blood pressure readings was selected. 24-hour ambulatory blood pressure monitoring was performed with the use of validated, automatic instruments (ABP-700, AVECINNA Co.) that were programmed to measure patients’ blood pressure at 30 minute intervals during the day and 60 minute intervals during the night and the relevant readings were evaluated by a certified cardiologist. Study subjects were non-diabetic, had no history of liver disease, and were not receiving any blood pressure lowering treatment at the time of enrollment; also, subjects had a 10-year cardiovascular disease risk <10%, based on heart risk assessment scoring see page http://www.cvriskcalculator.com/. Exclusion criteria were presence of end-organ damage including heart/renal failure, presence of causes of secondary hypertension (e.g. Cushing’s syndrome, acromegaly, hypo/hyperthyroidism and hyperaldosteronism), or pregnancy and breast-feeding. In this pilot study, 20 individuals in each group, were included. Power analysis was done at the end of the study to determine the effect size with 20 individual per group; by considering type I error=0.05, and type II error=0.2, the estimated effect size was 20% compared to the control group.
Allocation, treatment and measurements
Using a computer-based random-number generator, participants were randomly and equally allocated to cinnamon or placebo groups. In each group, the subjects received 500 mg capsules three times a day for 90 days (cinnamon dose was chosen based on previous reports (Allen et al. 2013; Mousavi et al. 2019a; Zare et al. 2019). At two time points (i.e. days 0 (considered baseline) and 90), BMI, blood lipid profile (in terms of LDL-c, HDL-c, cholesterol and triglycerides (TG) levels) and blood sugar profile (i.e. FBS level) were measured. On the same days, patients were evaluated with the use of 24-hour ambulatory blood pressure monitoring. In the present trial, participants and clinical assessor were blinded to the study groups.
Statistical analysis
Data is presented as mean±SD or percentages. SPSS Ver. 18 (SPSS, Inc., Chicago, IL, USA) was used for the statistical analysis. The Kolmogorov–Smirnov test was used to evaluate the normal distribution of variables analyzed. Independent t-test was used (in case of non-parametric data, Mann-Whiney U test was done) to compare cinnamon’s and placebo effects. Wilcoxon sign test was employed to compare the before-after changes of the studied variables in each study group. We also calculated changes of variables by subtracting values on day 90 from those of day 0 and compared this difference between the two study groups by Mann-Whiney U test. Chi square test or Fisher exact test was used to compare categorical variables between groups. Statistical difference was set at p<0.05.
Results
In this trial, three subjects (1 from cinnamon group and 2 from placebo group) early discontinued treatment and were excluded from final analysis. The demographics of the study population are summarized in Table 1.
Table 1.
Demographic records of the participants randomly allocated to the two groups
| Cinnamon group | Placebo group | p | |
|---|---|---|---|
| Age (years old), mean±sd | 54.4±10.2 | 49.8±9.07 | 0.227¥ |
| Sex (Male) (%) | 14 ( (73.7 | 11 (61.1 ) | 0.414* |
| Family history of IHD (%) | 4 (21.1) | 3 (16.7) | 0.734* |
| Family history of HTN (%) | 12 (63.2) | 5 (27.8) | 0.031* |
| Family history of DM (%) | 7 (36.8) | 6 (33.3) | 0.823* |
| Smoking (%) | 4 (21.1) | 4 (22.2) | 0.931* |
| Job Employed (%) | 16 (84.2) | 14 (77.8) | 0 .878* |
| University education (%) | 12 (63.2) | 9 (50.0) | 0.528* |
¥Independent T test, *Chi square test
The two study groups were matched in terms of mean age, sex, BMI, education status, job, familial history of diabetes and CVD; however, familial history of hypertension differ significantly between the two groups. On day 0 (i.e. before initiation of the intervention), 24-hr SBP and DBP, as well as BMI, were recorded and blood samples were collected (for assessment of lipid and FBS levels) (Tables 2 and 3). No significant differences between the groups were recorded.
Table 2.
Systolic and diastolic blood pressure as well as BMI, measured before initiation of the trial (day 0) and after the completion of the trial (day 90). BMI: body mass index; DBP: diastolic blood pressure
| Day 0 | Day 90 | |||||||
|---|---|---|---|---|---|---|---|---|
| Cinnamon | Placebo | p value* | Cinnamon | Placebo | p value** | p value # | p value ## | |
| Mean±sd 24-hr SBP (mmHg) | 131±4.44 | 131±4.59 | 0.648 | 130±4.58 | 130 ±5.45 | 0.994 | 0.03 | 0.1 |
| Mean±sd 24-hr DBP (mmHg) | 79.1±6.28 | 79.1±5.67 | 0.985 | 78.4±5.45 | 78.8±5.61 | 0.715 | 0.1 | 0.5 |
| Mean±sd day SBP (mmHg) | 133±4.53 | 132±4.38 | 0.444 | 132±4.31 | 132±5.15 | 0.848 | 0.004 | 0.8 |
| Mean±sd night SBP (mmHg) | 107±5.54 | 109±4.34 | 0.140 | 106±5.49 | 108±4.61 | 0.167 | 0.2 | 0.01 |
| Mean±sd day DBP (mmHg) | 80.2±6.09 | 80.5±5.70 | 0.906 | 79.5±5.63 | 80.8±5.84 | 0.480 | 0.09 | 0.4 |
| Mean±sd night DBP (mmHg) | 75.5±6.14 | 76.6±5.87 | 0.577 | 76.6±4.92 | 77.8±5.63 | 0.362 | 0.1 | 0.03 |
| BMI (kg/m2),Mean±sd | 28.4±3.52 | 26.4±3.02 | 0.073 | 28.2±3.34 | 26.0±2.71 | 0.036 | 0.3 | 0.01 |
*Comparison between Cinnamon and placebo groups on day 0, by Mann-Whitney U test.
**Comparison between Cinnamon and placebo groups on day 90, by Mann-Whitney U test.
#Comparison between data of day 0 and 90 in Cinnamon group, by Wilcoxon Signed rank test.
##Comparison between data of day 0 and 90 in placebo group, by Wilcoxon Signed rank test.
Table 3.
Biochemical parameters measured before initiation of the trial (day 0) and after the completion of the trial (day 90). FBS: fasting blood sugar; HDL-c: high-density lipoprotein cholesterol; LDL-c: low-density lipoprotein cholesterol; and TG: triglyceride
| Day 0 | Day 90 | |||||||
|---|---|---|---|---|---|---|---|---|
| Cinnamon | Placebo | p value* | Cinnamon | Placebo | p value** | p value # | p value ## | |
| LDL-c (mg/dl), mean±sd | 100±32.83 | 95.4±21.49 | 0.619 | 80.8±6.70 | 93.9±5.25 | 0.137 | 0.001 | 0.96 |
| HDL-c (mg/dl), mean±sd | 42.3±9.67 | 50.9±13.4 | 0.032 | 47.0±1.90 | 49.8±2.26 | 0.352 | 0.002 | 0.5 |
| TG (mg/dl), mean±sd | 123±55.20 | 106±54.6 | 0.261 | 122±55.9 | 107±55.0 | 0.354 | 0.4 | 0.6 |
| Cholesterol (mg/dl), mean±sd | 162±34.72 | 168±29.6 | 0.511 | 152±30.6 | 164±24.4 | 0.097 | 0.001 | 0.6 |
| FBS (mg/dl), mean±sd | 94.3±7.05 | 93.4±5.59 | 0.964 | 93.7±5.42 | 92.6±5.28 | 0.593 | 0.8 | 0.1 |
*Comparison between Cinnamon and placebo groups on day 0, by Mann-Whitney U test.
**Comparison between Cinnamon and placebo groups on day 90, by Mann-Whitney U test.
#Comparison between data of day 0 and 90 in Cinnamon group, by Wilcoxon Signed rank test.
##Comparison between data of day 0 and 90 in placebo group, by Wilcoxon Signed rank test.
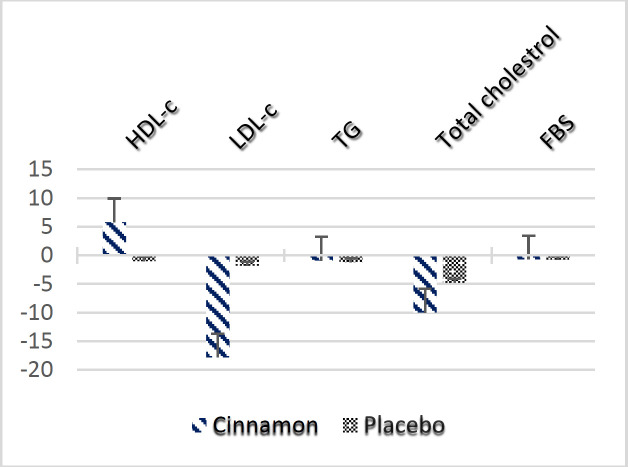
Cinnamon and placebo groups presented different patterns of blood pressure changes over time. A statistically significant decrease in mean 24-hr SBP and mean day SBP was observed in the cinnamon group, while mean night SBP and mean night DBP were decreased significantly in the placebo group after 90 days. At the end of the study, blood pressure values were not significantly different between the 2 groups (p>0.05) (Table 2). Mean changes in blood pressure were not significantly different between the two study groups (Figure 2), while mean change of day value of SBP was significantly decreased in the cinnamon group compared to the placebo (p=0.03). At baseline, although BMI was higher in cinnamon-administered subjects compared to placebo group, the said difference was not statistically significant. Comparison of the mean changes of BMI before and after the intervention did not show significant differences between the groups.
Figure 2.
Mean change in blood pressure (mmHg) and body mass index after 90-day intervention in cinnamon and placebo group. BMI: body mass index; DBP: diastolic blood pressure; SBP: systolic blood pressure
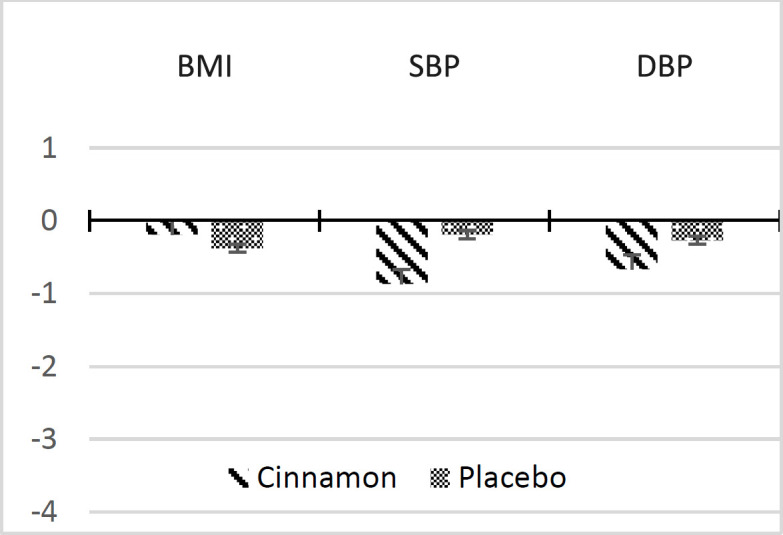
At baseline, HDL-c was significantly lower in the cinnamon compared to placebo group (42.3±9.67 vs 50.9±13.4 mg/dl; p=0.03). No significant difference in HDL-c levels was found between the 2 groups at the end of the study. This is due to the significantly higher HDL-c levels measured in the cinnamon-administered subjects, on day 90 compared to day 0 (47.0±1.9 vs 42.3±9.67 mg/dl, respectively; p=0.002), while no significant variation in HDL-c values in the placebo group was observed (49.8±2.26 vs 50.9±13.4 mg/dl, respectively; p=0.5) (Table 3). Importantly, mean change in HDL-c was significantly greater in the cinnamon group compared to the placebo group (Figure 3). At the end of the study, cinnamon supplementation led to a significant decrease of total cholesterol and LDL-c levels in treated subjects, in a magnitude of possibly high clinical value (cholesterol decrease 10.1±10 , p=0.001 and LDL decrease: 19.2± 24, p=0.001) (Figure 3).
Figure 3.
Mean change in metabolic profiles after 90-day intervention in cinnamon and placebo group. FBS: fasting blood sugar; HDL-c: high-density lipoprotein cholesterol; LDL-c: low-density lipoprotein cholesterol; and TG: triglyceride
FBS did not show significant differences between the two groups on day 90. It must be noted that no side effect was reported by the participants.
Discussion
The present study shows a considerable beneficial effect of cinnamon supplementation on S1HTN participants as reflected by a significant increase in HDL-c and a significant decrease in LDL-c and total cholesterol levels while mean ambulatory SBP levels following 90-day administration of 1.5 g/day cinnamon were moderately decreased; nevertheless, no significant effect on other metabolic parameters was observed.
Cardiovascular diseases (CVD) significantly contribute to global mortality and morbidity. Hypertension is regarded as a major risk factor for several conditions like stroke and intracranial artery stenosis (Ajebli and Eddouks 2019; Ma et al. 2019). Raised blood pressure is hold responsible for two-thirds of strokes, 50% of coronary heart disease (CHD) patients and near 9.5 million deaths/year worldwide (Pan et al. 2019); also, it is associated with premature coronary artery disease (Poorzand et al. 2019) and end-stage renal disease (Morovatdar et al. 2019).
The efficacy of herbal medicine (extracts or isolated compounds) has been widely studied and most commonly, garlic (Allium sativum), celery (Apium graveolens), Black Cumin (Nigella sativa) and Ginseng (Panax) have shown beneficial effects in lowering blood pressure (Ajebli and Eddouks 2019). Considering the positive attitude of Iranian population toward herbal medicine, in the present trial, we assessed the effect of 90-day administration of cinnamon on S1HTN and lipid profile in comparison with placebo.
Mechanistically, phytochemicals either directly relax blood vessels or indirectly suppress/activate angiotensin converting enzyme (ACE), renin angiotensin system (RAS) or the diuretic activity (Ajebli and Eddouks 2019). As a phytoconstituent of cinnamon, cinnamaldehyde was shown to lower the blood pressure in dogs and guinea pigs via induction of peripheral vasodilatation (HARADA and YANO 1975). Possibly, cinnamaldehyde hypotensive effect is mediated through inhibition of calcium influx and release (Xue et al. 2011); also, it abridged vascular contractility in diabetes type I and II (El-Bassossy et al. 2011). In the present study, cinnamon supplementation and placebo groups presented different patterns of blood pressure changes over time. Study subjects were blinded to treatment, but they were not blinded to the presence of hypertension. Thus subtle lifestyle modification changes could not be ruled out from occurring in the placebo group, explaining in part the observed changes in the said group and account at least partly for the changes in the cinnamon group.
Cinnamon which is obtained from the inner bark of Cinnamomum trees (Lauraceae family) (Ranasinghe et al. 2013) shows pharmacological properties like antibacterial and antioxidant effects and is therefore, of great value in the Chinese medicine (IM et al. 2014). Though beneficial effects of cinnamon as a rich source of polyphenols, in regulating blood glucose were shown (Medagama 2015), its effect on blood lipid profile is controversial (Maierean et al. 2017). A recent meta-analysis showed that cinnamon significantly decreased blood TG and total cholesterol levels but did not affect blood LDL-c and HDL-c levels. Moreover, cinnamon supplementation was found to have a small effect on patients with diabetes or impaired glucose tolerance (Maierean et al. 2017).
The results of a meta-analysis study showed that cinnamon compared to placebo, did not significantly change HDL-c; however, authors found a significant increase in HDL-c following omission of one study (WMD: 0.04 mmol/l [1.54 mg/dl], 95% CI: 0.03, 0.06 [1.16, 2.32], p<0.01) (Maierean et al. 2017).
Concerning cinnamon effect on blood pressure, Mousavi et al. in a meta-analysis that included 9 trials, reported that cinnamon could markedly decrease SBP and DBP. Interestingly, greater impacts on SBP were found if the dose was below 2 g, the trial’s duration was at least 12 weeks and the participants were younger than 50 years old. Overall, authors concluded that cinnamon at lower doses and in younger subjects, has more pronounced effects on BP (Mousavi et al. 2019a). Cinnamon’s beneficial impacts on blood lipid and inflammation (Han and Parker 2017; Hong et al. 2012; Nam et al. 2019) may contribute to its hypotensive effects (Bonaa 1991).
Headache and diarrhea were reported as cinnamon’s side effects (Wiweko and Susanto 2017). Nevertheless, beside studies on pharmacological effects of cinnamon, it is of great need and importance to design studies that evaluate its possible adverse effects in humans as studies in this regard were only done in vitro and in vivo (Mousavi et al. 2019a).
Based on our results, 90-day administration of 1500 mg cinnamon/day in S1HTN patients decreased mean ambulatory SBP in a moderate clinically degree. Cinnamon’s effects however in lipid values were pronounced achieving parallel LDL decrease and HDL increase in hypertensive patients.
Performing further trials (done in larger sample size and for longer periods) on cinnamon’s effect on metabolic profile could further explore its therapeutic potential. S1HTN patients’ common lipid abnormalities make cinnamon’s an attractive therapeutic option.
Cinnamon statistically significant but clinically mildly decreased mean ambulatory SBP in S1HTN patients. A significant and clinically meaningful decrease in LDL-c and a parallel increase in HDL-c were observed in cinnamon treated hypertensive patients.
Acknowledgment
The authors would like to appreciate the assistance provided by Clinical Research Development Unit, Imam Reza Hospital, Mashhad University of Medical Sciences, Mashhad, Iran.
Conflicts of interest
The authors have declared that there is no conflict of interest.
References
- 1.Ajebli M, Eddouks M. Phytotherapy of hypertension: An updated overview. Endocr Metab Immune Disord Drug Targets. 2019 doi: 10.2174/1871530320666191227104648. doi: 10.2174/1871530320666191227104648. [DOI] [PubMed] [Google Scholar]
- 2.Akilen R, Pimlott Z, Tsiami A, Robinson N. Effect of short-term administration of cinnamon on blood pressure in patients with prediabetes and type 2 diabetes. Nutrition. 2013;29:1192–1196. doi: 10.1016/j.nut.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 3.Allen RW, Schwartzman E, Baker WL, Coleman CI, Phung OJ. Cinnamon use in type 2 diabetes: an updated systematic review and meta-analysis. Ann Fam Med. 2013;11:452–459. doi: 10.1370/afm.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Archer AW. Determination of cinnamaldehyde, coumarin and cinnamyl alcohol in cinnamon and cassia by high-performance liquid chromatography. J Chromatogr A. 1988;447:272–276. [Google Scholar]
- 5.Askari F, Rashidkhani B, Hekmatdoost A. Cinnamon may have therapeutic benefits on lipid profile, liver enzymes, insulin resistance, and high-sensitivity C-reactive protein in nonalcoholic fatty liver disease patients. Nutr Res. 2014;34:143–148. doi: 10.1016/j.nutres.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Azimi P, Ghiasvand R, Feizi A, Hosseinzadeh J, Bahreynian M, Hariri M, Khosravi-Boroujeni H. Effect of cinnamon, cardamom, saffron and ginger consumption on blood pressure and a marker of endothelial function in patients with type 2 diabetes mellitus: A randomized controlled clinical trial. Blood Press. 2016;25:133–140. doi: 10.3109/08037051.2015.1111020. [DOI] [PubMed] [Google Scholar]
- 7.Bonaa K. Association between blood pressure and serum lipids in population. The Troms ø Study. Circulation. 1991;83:1305–1314. doi: 10.1161/01.cir.83.4.1305. [DOI] [PubMed] [Google Scholar]
- 8.Brook RD, Rajagopalan S. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Soc Hypertens. 2018;12:238. doi: 10.1016/j.jash.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 9.El-Bassossy HM, Fahmy A, Badawy D. Cinnamaldehyde protects from the hypertension associated with diabetes. Food Chem Toxicol. 2011;49:3007–3012. doi: 10.1016/j.fct.2011.07.060. [DOI] [PubMed] [Google Scholar]
- 10.Gruenwald J, Freder J, Armbruester N. Cinnamon and health. Crit Rev Food Sci Nut. 2010;50:822–834. doi: 10.1080/10408390902773052. [DOI] [PubMed] [Google Scholar]
- 11.Han X, Parker TL. Antiinflammatory activity of cinnamon (Cinnamomum zeylanicum) bark essential oil in a human skin disease model. Phytother Res. 2017;31:1034–1038. doi: 10.1002/ptr.5822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harada M, Yano S. Pharmacological studies on Chinese cinnamon Effects of cinnamaldehyde on the cardiovascular and digestive systems. Chem Pharm Bull. 1975;23:941–947. doi: 10.1248/cpb.23.941. [DOI] [PubMed] [Google Scholar]
- 13.Hong J-W, Yang G-E, Kim YB, Eom SH, Lew J-H, Kang H. Anti-inflammatory activity of cinnamon water extract in vivo and in vitro LPS-induced models. BMC Complement Altern Med. 2012;12:237. doi: 10.1186/1472-6882-12-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.IM KK, Issac A, Ninan E, Kuttan R, Maliakel B. Enhanced anti-diabetic activity of polyphenol-rich de-coumarinated extracts of Cinnamomum cassia. J Funct Foods. 2014;10:54–64. [Google Scholar]
- 15.Jain SG, Puri S, Misra A, Gulati S, Mani K. Effect of oral cinnamon intervention on metabolic profile and body composition of Asian Indians with metabolic syndrome: a randomized double-blind control trial. Lipids Health Di. 2017;16:1–11. doi: 10.1186/s12944-017-0504-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jayaprakasha G, Rao LJM. Chemistry, biogenesis, and biological activities of Cinnamomum zeylanicum. Crit Rev Food Sci Nutr. 2011;51:547–562. doi: 10.1080/10408391003699550. [DOI] [PubMed] [Google Scholar]
- 17.Kawatra P, Rajagopalan R. Cinnamon: Mystic powers of a minute ingredient. Pharmacognosy Res. 2015;7(Suppl 1):S1. doi: 10.4103/0974-8490.157990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khan A, Safdar M, Khan MMA, Khattak KN, Anderson RA. Cinnamon improves glucose and lipids of people with type 2 diabetes. Diabetes care. 2003;26:3215–3218. doi: 10.2337/diacare.26.12.3215. [DOI] [PubMed] [Google Scholar]
- 19.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 20.Ma YH, Leng XY, Dong Y, Xu W, Cao XP, Ji X, Wang HF, Tan L, Yu JT. Risk factors for intracranial atherosclerosis: A systematic review and meta-analysis. Atherosclerosis. 2019;281:71–77. doi: 10.1016/j.atherosclerosis.2018.12.015. [DOI] [PubMed] [Google Scholar]
- 21.Maierean SM, Serban MC, Sahebkar A, Ursoniu S, Serban A, Penson P, Banach M. 2017. The effects of cinnamon supplementation on blood lipid concentrations: A systematic review and meta-analysis. J Clin Lipidol. Lipid and Blood Pressure Meta-analysis Collaboration (LBPMC) Group;11:1393–1406. doi: 10.1016/j.jacl.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Medagama AB. The glycaemic outcomes of Cinnamon, a review of the experimental evidence and clinical trials. Nutr J. 2015;14:108. doi: 10.1186/s12937-015-0098-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morovatdar N, Tayebi Nasrabad G, Tsarouhas K, Rezaee R. Etiology of Renal Replacement Therapy in Iran. Int J Nephrol. 2019;2019:1–5. doi: 10.1155/2019/5010293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mousavi SM, Karimi E, Hajishafiee M, Milajerdi A, Amini MR, Esmaillzadeh A. Anti-hypertensive effects of cinnamon supplementation in adults: A systematic review and dose-response Meta-analysis of randomized controlled trials. Crit Rev Food Sci Nutr. 2019a;16:1–11. doi: 10.1080/10408398.2019.1678012. [DOI] [PubMed] [Google Scholar]
- 25.Mousavi SM, Rahmani J, Kord-Varkaneh H, Sheikhi A, Larijani B, Esmaillzadeh A. Cinnamon supplementation positively affects obesity: A systematic review and dose-response meta-analysis of randomized controlled trials. Clin Nut. 2019b;39:123–133. doi: 10.1016/j.clnu.2019.02.017. [DOI] [PubMed] [Google Scholar]
- 26.Nam J, Park Y, Kim MS, Kim JY. Anti-inflammatory Effects of Cinnamon Extracts on an Animal Model of Intestinal Inflammation, (P06-088-19) Oxford University Press. 2019 [Google Scholar]
- 27.Nyadjeu P, Dongmo A, Nguelefack TB, Kamanyi A. Antihypertensive and vasorelaxant effects of Cinnamomum zeylanicum stem bark aqueous extract in rats. J Complement Integr Med. 2011;8:1. doi: 10.2202/1553-3840.1490. [DOI] [PubMed] [Google Scholar]
- 28.Pan H, Hibino M, Kobeissi E, Aune D. Blood pressure, hypertension and the risk of sudden cardiac death: a systematic review and meta-analysis of cohort studies. Eur J Epidemiol. 2019 doi: 10.1007/s10654-019-00593-4. doi:10.1007/s10654-019-00593-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Poorzand H, Tsarouhas K, Hozhabrossadati SA, Khorrampazhouh N, Bondarsahebi Y, Bacopoulou F, Rezaee R, Jafarzadeh Esfehani R, Morovatdar N. Risk factors of premature coronary artery disease in Iran: A systematic review and meta‐analysis. Eur J Clin Invest. 2019;49:1–13. doi: 10.1111/eci.13124. [DOI] [PubMed] [Google Scholar]
- 30.Ranasinghe P, Pigera S, Premakumara GS, Galappaththy P, Constantine GR, Katulanda P. Medicinal properties of ‘true’cinnamon (Cinnamomum zeylanicum): a systematic review. BMC Complement Altern Med. 2013;13:1–10. doi: 10.1186/1472-6882-13-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension Overview, meta-analyses, and meta-regression analyses of randomized trials. J Hypertens. 2014;32:2285–2295. doi: 10.1097/HJH.0000000000000378. [DOI] [PubMed] [Google Scholar]
- 33.Vafa M, Mohammadi F, Shidfar F, Sormaghi MS, Heidari I, Golestan B, Amiri F. Effects of cinnamon consumption on glycemic status, lipid profile and body composition in type 2 diabetic patients. Int J Prev Med. 2012;3:531–536. [PMC free article] [PubMed] [Google Scholar]
- 34.Wainstein J, Stern N, Heller S, Boaz M. Dietary cinnamon supplementation and changes in systolic blood pressure in subjects with type 2 diabetes. J Med Food. 2011;14:1505–1510. doi: 10.1089/jmf.2010.0300. [DOI] [PubMed] [Google Scholar]
- 35.Wansi SL, Nyadjeu P, Ngamga D, Mbuyo E, Nguelefack T, Kamanyi A. Blood pressure lowering effect of the ethanol extract from the stembark of cinnamomum zeylanicum (lauraceae) in rats. Pharmacol online. 2007;3:166–176. [Google Scholar]
- 36.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 37.Wiweko B, Susanto CA. The effect of metformin and cinnamon on serum anti-mullerian hormone in women having PCOS: A Double-blind, randomized, controlled trial. J Hum Reprod Sci. 2017;10:31–36. doi: 10.4103/jhrs.JHRS_90_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xue Y-L, Shi H-X, Murad F, Bian K. Vasodilatory effects of cinnamaldehyde and its mechanism of action in the rat aorta. Vasc Health Risk Manag. 2011;7:273–280. doi: 10.2147/VHRM.S15429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yano Y, Tanner RM, Sakhuja S, et al. Association of daytime and nighttime blood pressure with cardiovascular disease events among African American individuals. JAMA Cardiol. 2019;4:910–917. doi: 10.1001/jamacardio.2019.2845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zare R, Nadjarzadeh A, Zarshenas MM, Shams M, Heydari M. Efficacy of cinnamon in patients with type II diabetes mellitus: A randomized controlled clinical trial. Clin Nutr. 2019;38:549–556. doi: 10.1016/j.clnu.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 41.Ziegenfuss TN, Hofheins JE, Mendel RW, Landis J, Anderson RA. Effects of a water-soluble cinnamon extract on body composition and features of the metabolic syndrome in pre-diabetic men and women. J Int Soc Sports Nutr. 2006;3:45–53. doi: 10.1186/1550-2783-3-2-45. [DOI] [PMC free article] [PubMed] [Google Scholar]