COVID-19 has plagued the world since it was first identified in December 2019. Previous systematic reviews and meta-analysis were limited by various factors such as the usage of non-peer reviewed data and were also limited by the lack of clinical data on a global scale.
KEYWORDS: COVID-19, comorbidity, SARS-CoV-2
ABSTRACT
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has rapidly spread across the globe at unprecedented speed and is showing no signs of slowing down. The outbreak of coronavirus disease 2019 (COVID-19) has led to significant health burden in infected patients especially in those with underlying comorbidities. The aim of this study was to evaluate the correlation between comorbidities and their role in the exacerbation of disease in COVID-19 patients leading to fatal outcomes. A systematic review was conducted using data from MEDLINE, Scopus, Web of Science, and EMBASE databases published from 1 December 2019 to 15 September 2020. Fifty-three articles were included in the systematic review. Of those 53 articles, 8 articles were eligible for meta-analysis. Hypertension, obesity, and diabetes mellitus were identified to be the most prevalent comorbidities in COVID-19 patients. Our meta-analysis showed that cancer, chronic kidney diseases, diabetes mellitus, and hypertension were independently associated with mortality in COVID-19 patients. Chronic kidney disease was statistically the most prominent comorbidity leading to death. However, despite having high prevalence, obesity was not associated with mortality in COVID-19 patients.
INTRODUCTION
Coronaviruses (CoVs) are RNA viruses with a large nonsegmented genome and can infect both animals and humans (1). CoV infections can cause respiratory distress, gastrointestinal and hepatic diseases, and neurological complications (2). With the recent emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), responsible for the current coronavirus disease 2019 (COVID-19) pandemic, there are now seven coronaviruses known to infect humans (3–5). First identified in Wuhan, China, SARS-CoV-2 has since spread rapidly around the globe with over 210 countries and territories reporting infections. The global new COVID-19 cases and deaths are soaring. Increasing numbers of cases and deaths are being reported weekly since early October 2020. The numbers peaked in the second week of November 2020 with almost 4 million new cases and 60,000 new deaths recorded. As of 13 December 2020, SARS-CoV-2 is known to have infected over 70.4 million individuals with more than 1.5 million associated deaths reported (6). Fortunately, through a global effort, COVID-19 vaccines are now entering the market to slow the spread of COVID-19, with the vaccines developed by Pfizer-BioNTech and Moderna both reporting greater than 94% efficacy in clinical trials (7). The Pfizer-BioNTech COVID-19 vaccine has been approved for use in the United States, Canada, and United Kingdom, and priority is being given to people over 80 years of age and health care workers (8). On 18 December 2020, the U.S. Food and Drug Administration issued an emergency use authorization for Moderna’s vaccine (7, 9, 10). However, caution is still warranted, as it is still unknown whether these vaccines will provide long-term protection.
There are multiple risk factors that are associated with COVID‐19. For example, the male population has a higher rate of SARS-CoV-2 infection compared to females (11, 12). Studies have shown that a higher incidence of severe and fatal COVID-19 is observed with increasing age (13), and it is speculated that this phenomenon is partly attributed to preexisting comorbid conditions (14). To date, there are several systematic reviews being published regarding the effect of comorbidities on prognosis of COVID-19 patients. However, much of the previous data analysis is limited by factors such as incomplete prevalence reporting due to the use of non-peer reviewed data and only using data from China (15, 16). This limits the conclusions that can be drawn from these early studies, particularly given the global reach of the SARS-CoV-2 pandemic.
As the pandemic has progressed, an increasing amount of clinical data has been made available from around the world. The aim of this study is to present an updated systematic review on the influence of comorbidities on the exacerbation of COVID-19. Here we analyze the most recent data available in the literature to gain better insights into the development of COVID-19 and severe forms of the disease resulting in death to aid the development of strategies to better manage SARS-CoV-2-infected patients.
RESULTS
Study selection.
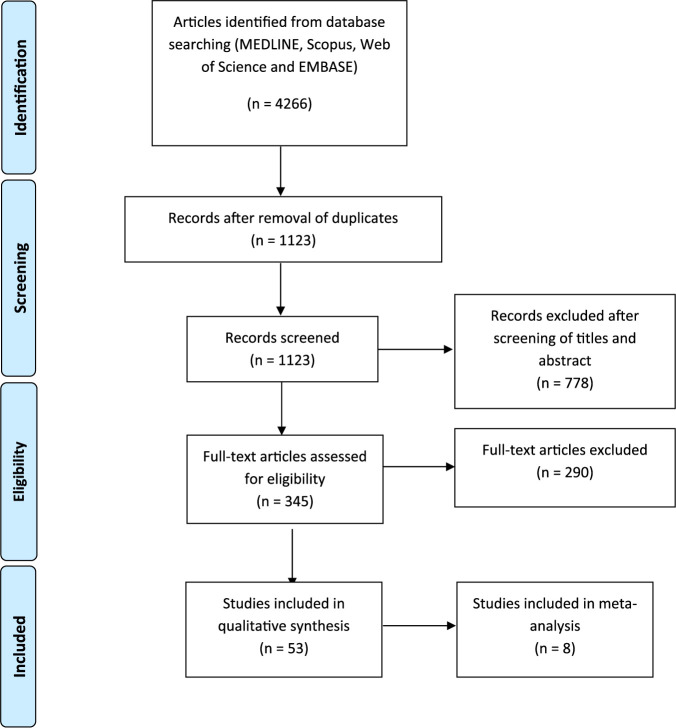
A total of 4,266 articles were identified using the search strategy employed in MEDLINE, Scopus, Web of Science, and EMBASE databases. A total number of 3,143 duplicates and irrelevant articles were removed, bringing the number of articles screened for title and abstract to 1,123. Subsequently, 778 articles were excluded after title and abstract screening, resulting in 345 studies which were subjected to full-text screening. Fifty-three studies matched our predetermined inclusion and exclusion criteria. These studies included a total number of 375,859 participants from 14 countries, namely, Brazil, China, India, Iran, Italy, Mexico, Oman, Saudi Arabia, South Korea, Spain, Turkey, Uganda, United Kingdom, and United States (see Table S1 in the supplemental material).
Characteristics of included studies. Data included in this table, when available, included the title, country, age, number of participants, and the type of analysis applied. Download Table S1, DOCX file, 0.05 MB (55.4KB, docx) .
Copyright © 2021 Ng et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.
Among the selected articles, two articles specifically studied adult patients (17, 18), while three articles focused on pediatric patients (19–21). The remaining 49 articles did not impose any age limitations in their respective studies. However, despite SARS-CoV-2 testing in all patients, these studies did not identify positive samples in patients with a mean age of <18 years, which aligns with previous observations suggesting age plays a role in the severity of SARS-CoV-2 infection (13, 14, 22, 23). The three most prevalent comorbidities were hypertension, obesity, and diabetes amounting to 80,093 (21.3%), 68,935 (18.3%), and 67,954 (18.1%) patients, respectively. The comorbidities were reported as defined, respectively, from extracted studies.
Clinical outcomes reported in study participants included mortality, severe disease, hospitalization, length of hospitalization, the need for intubation, and development of acute respiratory distress syndrome. In one study, the final clinical outcome of patients was not reported (24).
The majority of studies included in the analysis did not report the status of the comorbidities in patients. Two articles investigated the role of cancer in COVID-19 patients. One study included 12 participants of which 7 had received anticancer treatments a month prior to the study (25), while in another Italian cohort, active cancer independently predicted mortality in COVID-19 patients (26). Chronic kidney disease stage was reported in two studies (27, 28), and later disease stages were not associated with a worse prognosis in study participants from Iran (27), while the effect of higher chronic kidney disease states on prognosis was not evaluated in a Spanish study (28). In a cohort of COVID-19 patients with chronic kidney and end-stage renal diseases, only the former was reported as an independent predictor of the requirement of intensive care unit (ICU) level care (29).
One study categorized obese participants into two groups, having a body mass index (BMI) of 30 to 40 kg/m2 or BMI of ≥40 kg/m2. Having a BMI above 40 kg/m2 and being younger than 50 years was independently associated with mortality (30). A study by Docherty et al. (31) grouped diabetic patients into those with and without complications. However, the individual effect of each of the groups on patient outcome was not reported. None of the studies included in the analysis evaluated the role of antidiabetic therapy on SARS-CoV-2 outcome in patients.
Mortality.
Thirty studies reported mortality as a clinical outcome in COVID-19 patients (17, 18, 26–28, 30–54). Independent risk factors for mortality were reported in 22 studies, and these risk factors included hypertension, obesity, diabetes, renal disease, chronic obstructive pulmonary disease (COPD), neurological disease, and cardiovascular disease (18, 26, 30–37, 40, 42–52). Eight studies were selected for meta-analysis of cancer (36, 39), chronic kidney diseases (26, 28, 39), diabetes (26, 28, 32, 53), hypertension (26, 32, 53), and obesity (28, 37) as comorbidities. Meta-analysis results for comorbidities in which three or more studies were included in the analysis are shown in Fig. 1 and 2. By virtue of having larger sample sizes, we believe meta-analysis results for diabetes and hypertension are more reliable.
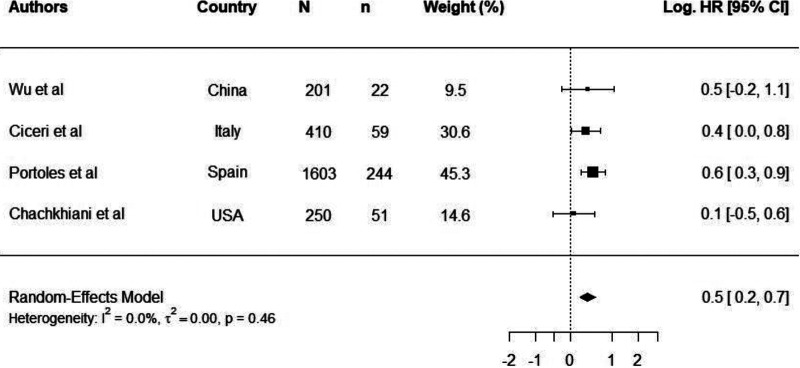
FIG 1.
Log hazards ratios of COVID-19-related mortality in patients with diabetes. Log.HR was calculated from four independent studies (Wu et al. [53], Ciceri et al. [26], Portoles et al. [28], and Chachkhiani et al. [32]). N is the study size, n is the number of participants with comorbidity, and Log.HR is the natural logarithm of hazard ratio.
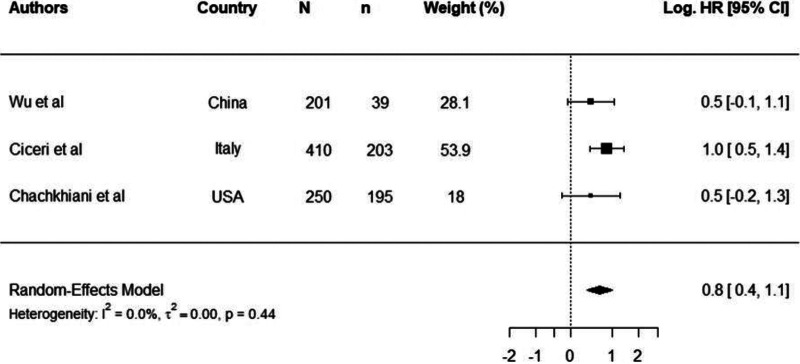
FIG 2.
Log hazards ratios of COVID-19-related mortality in patients with hypertension. Log.HR was calculated from three independent studies (Wu et al. [53], Ciceri et al. [26], and Chachkhiani et al. [32]). N is the study size, n is the number of participants with comorbidity, and Log.HR is the natural logarithm of hazard ratio.
The overall natural logarithm of odds ratio (log.OR) of mortality in cancer patients was 0.49 (95% confidence interval [95% CI], 0.01 to 0.97), which translates to an OR of 1.63 (95% CI, 1.01 to 2.00). The results indicate a significant 63% increased odds of COVID-19-related mortality in patients with cancer.
The overall natural logarithm of hazard ratio (log.HR) of mortality in patients with chronic kidney diseases was 1.28 (95% CI, 0.89 to 1.67), which translates to an HR of 3.61 (95% CI, 2.45 to 5.32). The results indicate a significant 3.6 times increased hazard of COVID-19-related mortality in patients with chronic kidney diseases.
The overall log.HR of mortality in patients with diabetes was 0.46 (95% CI, 0.24 to 0.67), which translates to an HR of 1.94 (95% CI, 1.54 to 2.46) (Fig. 1). The results indicate a significant 94% increased hazard of COVID-19-related mortality in patients with diabetes.
The overall log.HR of mortality among patients with hypertension and nonhypertensive patients was log.HR 0.8 (95% CI, 0.40 to 1.10) (Fig. 2), which translates to a HR of 2.10 (95% CI, 1.50 to 2.90). The results imply that the hazard of COVID-19 mortality was increased 2.1 times in patients with hypertension, indicating a significant effect on mortality in COVID-19 patients.
The overall log.HR of COVID-19 mortality among obese patients was 0.45 (95% CI, −0.03 to 0.94) which translates to an HR of 1.58 (95% CI, 0.96 to 2.57). The results indicate a nonsignificant 58% increased hazard of COVID-19 mortality in patients with obesity. Overall, there was low heterogeneity in all meta-analyses, which implied that performing a random-effects meta-analysis was unnecessary.
Severe disease.
Ten studies reported severe disease as an outcome in COVID-19 patients (19, 54–62). The definition of severe disease, however, varied among studies. Independent predictors of severe infection were described in three studies, and these predictors included neurological disease, neoplastic disease, arterial hypertension (59), obesity (55), and diabetes mellitus (57). One study reporting severe disease as an outcome specifically targeted pediatric patients with a median age of 16 years and a total of 407 patients. Critical illness was linked with increasing age, longer duration of symptoms, and lower oxygen saturation on presentation. Twenty-four of the children tested positive for SARS-CoV-2, and 19 of them required hospitalization. Of those 19 patients, 7 were critically ill, with 4 requiring intubations. Comorbidities were present in two out of the four intubated patients, and one of them died from a sudden cardiac arrest (19).
Severe outcome.
A composite severe outcome in COVID-19 patients was reported in three studies (25, 63, 64). Of the three studies, only cancer with an OR of 6.51 (95% CI, 1.72 to 24.64; P = 0.006) was reported as an independent risk factor for a severe outcome in a study with participants from China (25). In a Spanish cohort of 456 SARS-CoV-2-positive rheumatic and nonrheumatic patients, connective tissue disorder with an OR of 1.64 (95% CI, 1.02 to 2.66; P = 0.042), obesity with an OR of 1.78 (95% CI, 1.13 to 2.81; P = 0.013), diabetes with an OR of 1.81 (95% CI, 1.11 to 2.95; P = 0.018), hypertension with an OR of 2.60 (95% CI, 1.72 to 3.94; P < 0.001), heart failure with an OR of 3.49 (95% CI, 2.21 to 5.51; P < 0.001), and lung disease with an OR of 2.15 (95% CI, 1.34 to 3.45; P = 0.001) could be reported as risk factors for a severe outcome only in bivariate analysis.
Hospitalization.
Hospitalization as an outcome was reported in nine studies (21, 48, 51, 65–70). The criteria for hospitalization are expected to vary in different countries and studies. Factors independently predicting hospitalization were identified in five studies (48, 51, 66–68), and commonly identified comorbidities included diabetes, chronic kidney diseases, obesity, smoking, and COPD. In a study by van Gerwen et al. (51), diabetes was associated with an increased risk of mechanical ventilation with an OR of 1.35 (95% CI, 1.08 to 1.69) in hospitalized patients, and an observational longitudinal study of COVID-19 patients with autoimmune inflammatory rheumatic diseases identified the presence of a systemic autoimmune condition (OR, 3.55; 95% CI, 1.30 to 9.67; P = 0.01) as a risk factor for hospitalization (66). Although the immunosuppressant medication for autoimmune patients may predispose patients to severe disease, rheumatic patients enrolled in the study were mostly elderly and presented with comorbidities (66). Despite a 14% prevalence of asthma in one study, the comorbidity was not associated with an increased risk of hospitalization with a relative risk of 0.96 (95% CI, 0.77 to 1.19; P = 0.71) (65). In a cohort of COVID-19 patients from metropolitan Detroit (MI, USA), severe obesity with an OR of 2.0 (95% CI, 1.4 to 3.6; P = 0.02) and chronic kidney disease with an OR of 2.0 (95% CI, 1.3 to 3.3; P = 0.006) were independently associated with intensive care stay in hospitalized patients (29). Additionally, severe obesity with an OR of 3.2 (95% CI, 1.7 to 6.0; P < 0.001), chronic kidney disease with an OR of 2.4 (95% CI, 1.4 to 4.2; P = 0.001), and cancer with an OR of 2.5 (95% CI, 1.2 to 5.0; P = 0.01) were independently associated with the need for mechanical ventilation (29).
In a cohort of COVID-19 patients with neurological complaints, altered mental status was identified as an independent predictor of prolonged hospital stay with an OR of 1.6 (95% CI, 1.1 to 2.5; P = 0.01) and the requirement for intubation with an OR of 4.9 (95% CI, 2.6 to 9.4; P < 0.0001) (32).
DISCUSSION
The association between comorbidities and their role in the exacerbation of COVID-19 in patients leading to death is evaluated in this study, using published results from large cohort data from across the globe. Our study identified hypertension as the most common comorbidity in COVID-19 patients followed by obesity and diabetes. This partially resonates with earlier publications on the clinical characteristic and frequency of comorbidities in SARS-CoV-2-infected patients where circulatory disease (including hypertension and coronary artery diseases) was reported to be the highest (71–73). In the meta-analysis, we demonstrated that chronic kidney disease, hypertension, and diabetes mellitus were associated with COVID-19 mortality. The latter two are among the most prevalent comorbidities in COVID-19 patients and were associated with a higher risk of fatality and often coexist as multiple comorbidities along with obesity (51). In patients with chronic kidney disease, the risk of in-hospital mortality in COVID-19 patients appears higher in cases with end-stage renal disease compared to chronic renal disease (50). However, in one study, only chronic kidney disease was associated with the requirement of ICU level care in COVID-19 patients (29). Recently, a study reported a staggering 49% of cumulative incidence of thrombotic complications in COVID-19 patients (74). COVID-19 is associated with increased clot strength, platelet fibrinogen contribution to clot strength, elevated d-dimer levels, and hyperfibrinogenemia (75). Hence, the association of severe outcomes in patients with hypertension and diabetes may be partially explained by the increased incidence of thrombotic complications as it is already established that patients with hypertension and diabetes have elevated risk of thrombotic events (76, 77).
Further investigation to explain the higher prevalence of reported comorbidities in COVID-19 patients may focus on the SARS-CoV-2 cell entry mechanism. Similarly to SARS-CoV-1, SARS-CoV-2 contains a receptor-binding domain (RBD) that recognizes angiotensin-converting enzyme 2 (ACE2) as its receptor with a higher binding affinity compared to SARS-CoV-1 (78). ACE2 receptor is commonly identified in the epithelial cells of the lungs, intestine, kidney, and blood vessel (79). Diabetic patients are frequently prescribed with thiazolidinedione, a type of oral hypoglycemic used to lower blood glucose level. Thiazolidinedione is reported to increase the expression of ACE2 (80). ACE inhibitors (ACE-I) and angiotensin II type 1 receptor blockers (ARBs) are also frequently used as a treatment strategy to treat diabetes and hypertension (81). Consequently, increased expression of ACE2 may promote the internalization of SARS-CoV-2, which in turn may increase the chances of developing COVID-19 or a severe form of the disease. However, despite clear evidence that ACE2 is the main receptor for COVID-19 (82), several studies have encouraged the continued use of ACE-I and ARB medications in patients with diabetes or circulatory diseases as use of these medications is not associated with severe COVID-19 and may even be beneficial in reducing disease severity in these patients (57, 60, 83, 84).
Chronic medical conditions, similar to infectious diseases, often present with inflammation and weakened innate immune responses in affected individuals. This may predispose those individuals to infections and disease complications (15). The high prevalence of fatal cases among COVID-19 patients with hypertension and diabetes as comorbidity could be due to the induction of cytokine storm. Cytokine storms resulting in hyperinflammation are the hallmarks of severe SARS-CoV-2 infection (85). Besides participating in host defenses against infectious agents, inflammation contributes to the pathogenesis of many chronic disorders such as diabetes mellitus, cardiovascular disease, and cancer (86). Inflammation is therefore regarded as a link between pathogens and chronic disorders. Metabolic inflammation as a consequence of hypertension and diabetes is also known to compromise the immune system, thereby weakening the host’s ability to fend off infections. Hypertension and diabetic patients are commonly reported to have weakened immunological function arising from reduced macrophage and lymphocyte activity which could predispose individuals to infections, especially those infections for which cell-mediated immunity constitute an important host defense (87). Similarly, the use of immunosuppressive drugs for the treatment of autoimmune diseases and cancer in patients also suffer from weakened immunological functions. This may explain the increased risk of hospitalization observed in these patients particularly in those that are critically ill (66, 88). Thus, patients with an underlying comorbidity, particularly cancer, hypertension, and diabetes, face a higher risk of mortality as evidenced by our findings.
Obesity was not identified as an independent predictor of mortality in our meta-analysis. However, these results should be interpreted with caution, since only two studies were included in the analysis. Obesity is unanimously accepted to be a common morbidity among critically ill patients, including its association with increased mortality (89–92). Unlike diabetes and hypertension, obesity does not directly influence the expression of ACE2. Rather, obese patients have a larger amount of ACE2-expressing adipose tissue in the body which indirectly results in an increased amount of ACE2-expressing cells (93). Other factors put forward to explain COVID-19 severity in obese individuals include abnormal cytokine and complement production leading to the reduction in the activity processes that inhibits acute inflammation (94, 95). Increased risk of blood clotting due to obesity has also been proposed to play a role (95, 96). Prolonged viral shedding is also associated with obesity in SARS-CoV-2-infected patients, which may also contribute to COVID-19 aggravation leading to mortality (97). Moreover, managing obese patients requiring intensive care presents with practical difficulties (which affect prognosis) such as the need for bariatric beds, challenging intubations, weight limitations on imaging machines impacting imaging diagnosis and the fact that obese patients are more inclined to take prone positions promoting ventilatory dysfunction (98).
There are several limitations to our findings. Our search obtained non-English articles which were excluded. In addition, many studies failed to report bivariate analysis for the investigated comorbidities leading to only eight included studies in the meta-analysis. It should also be noted that patients with chronic kidney diseases, hypertension, diabetes, and cancer are already at increased risk of mortality in the absence of COVID-19 (99–102). These limitations may contribute to the overestimation or underestimation of comorbidity and its role in the exacerbation of SARS-CoV-2 leading to fatal outcomes. We attempted to but may not have fully controlled for heterogeneity which may introduce bias into our findings, as patients included in our study are of various ages, ethnicities, and living conditions among other factors. Furthermore, some studies failed to report the type of intervention applied, such as the type of medication prescribed to affected patients, which could lead to a various number of reported casualties. In this study, data also suggested that several patients had more than one comorbidity but did not confirm whether the risk increased with the number of comorbidities. SARS-CoV-2 is claiming more lives daily, and the number of cases is still increasing. From our data, patients with comorbidities should be given prompt care to avoid complications.
Our study identifies hypertension to have the highest prevalence as a comorbidity in COVID-19 patients. Patients with chronic kidney diseases appear to face a higher risk of fatality while hypertension, diabetes, and cancer are found to significantly exacerbate the severity of COVID-19 in patients resulting in death. Evidence presented in this study will help to determine high-risk COVID-19 patients so that appropriate measures can be taken to mitigate the number of fatalities in the COVID-19 pandemic.
MATERIALS AND METHODS
Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guidelines were used in this review (103). This study aims to report the influence of comorbidities and its role in exacerbation of COVID-19 leading to fatality in infected patients.
Ethical approval.
Ethical clearance for the study was obtained from the Health Sciences Research Ethics Committee (HSREC) (ethics number UFS-HSD2020/1150/2807/-0001) at the University of the Free State.
Search strategy.
The MEDLINE, Scopus, Web of Science, and EMBASE databases were searched for articles published from 1 December 2019 to 15 September 2020. The search strategy employed was as follows: (SARS-CoV-2 or COVID-19 or 2019-nCoV) AND (underlying or comorbid* or comorbid*) AND (prognos* or outcome*). The search was restricted to include only articles printed in English.
Study selection.
Study selection was conducted by authors, W.H.N. and T.T. independently. Identified articles were pooled together, and duplicates and irrelevant articles were removed (Fig. 3). The titles and abstracts of the studies were then screened against the inclusion and exclusion criteria below.
FIG 3.
Flow diagram outlining study selection, eligibility, and inclusion in meta-analysis.
Inclusion criteria
1. Only studies reporting comorbidities and patient’s outcome were included.
2. Only peer-reviewed journals were included.
Exclusion criteria
1. Literature and/or systematic reviews, letters, comments, case reports, and family-based studies were excluded.
2. Articles not reporting SARS-CoV-2 infections were excluded.
3. Studies not reporting the nature of comorbidity, hospital names, or regions from which study participants were drawn and the period for which the study was conducted were excluded.
Data extraction.
A data extraction form was developed in MS-Excel, and data were extracted independently by T.T. The data extracted was subjected to screening by W.H.N. and unanimity was reached on disputes after discussion. A third author was not involved, as there were no major disputes in study selection. Data extracted in this study, when available, included the title, published year, number of participants, country, patient’s age and gender, identified comorbidities, and the percentage of infected patients, type of intervention, study type, and patient outcome. In cases of studies with overlapping participants, the study with the longest sampling period was selected.
Statistical analysis.
Meta-analysis was conducted using pooled studies which reported bivariate analysis. The study aims to identify the association of comorbidity and its exacerbation of the outcome in SARS-CoV-2-infected patients resulting in death. Therefore, univariate analysis is not applicable, as it does not deal with the association. The models used for multivariate analysis, on the other hand, vary greatly in terms of the parameters used to justify its inclusion. Statistical analysis was performed using R, version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria). We performed a random-effects meta-analysis to account for between- and within-study differences across studies in the meta-analysis. For each random-effects meta-analysis, relative weight, based on the within- and between-study variances was applied. Heterogeneity was assessed based on two approaches, a scale with cutoffs at 25%, 50%, and 75% for low, intermediate, and high inconsistency, respectively, among the study findings, and level of statistical significance, where P < 0.05 shows that the true effects vary (104). A nonsignificant P value for heterogeneity implies weakness in the effect sizes but could also be related to the sample sizes across the studies analyzed. Results from the meta-analysis were summarized into either natural logarithm of odds ratio (log.OR) and 95% confidence intervals (95% CI) or natural logarithm of hazard ratio (log.HR) and 95% CI depending on the outcome considered.
Footnotes
This article is a direct contribution from Suresh Mahalingam, a Fellow of the American Academy of Microbiology, who arranged for and secured reviews by Roberto Bruzzone, HKU-Pasteur Research Pole, University of Hong Kong; Vincent Chow, National University of Singapore; and Christopher Basler, Georgia State University.
Citation Ng WH, Tipih T, Makoah NA, Vermeulen J-G, Goedhals D, Sempa JB, Burt FJ, Taylor A, Mahalingam S. 2021. Comorbidities in SARS-CoV-2 patients: a systematic review and meta-analysis. mBio 12:e03647-20. https://doi.org/10.1128/mBio.03647-20.
REFERENCES
- 1.Yang D, Leibowitz JL. 2015. The structure and functions of coronavirus genomic 3′ and 5′ ends. Virus Res 206:120–133. doi: 10.1016/j.virusres.2015.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weiss SR, Leibowitz JL. 2011. Coronavirus pathogenesis. Adv Virus Res 81:85–164. doi: 10.1016/B978-0-12-385885-6.00009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Drosten C, Günther S, Preiser W, van der Werf S, Brodt H-R, Becker S, Rabenau H, Panning M, Kolesnikova L, Fouchier RAM, Berger A, Burguière A-M, Cinatl J, Eickmann M, Escriou N, Grywna K, Kramme S, Manuguerra J-C, Müller S, Rickerts V, Stürmer M, Vieth S, Klenk H-D, Osterhaus ADME, Schmitz H, Doerr HW. 2003. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med 348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- 4.Zaki AM, Van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. 2012. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med 367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 5.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W, China Novel Coronavirus Investigating and Research Team. 2020. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. 2020. Coronavirus disease (COVID-2019) situation reports. World Health Organization, Geneva, Switzerland. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed 13 December 2020.
- 7.Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, Perez JL, Pérez Marc G, Moreira ED, Zerbini C, Bailey R, Swanson KA, Roychoudhury S, Koury K, Li P, Kalina WV, Cooper D, Frenck RW, Hammitt LL, Türeci Ö, Nell H, Schaefer A, Ünal S, Tresnan DB, Mather S, Dormitzer PR, Şahin U, Jansen KU, Gruber WC. 2020. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med 383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahase E 2020. Covid-19: Pfizer vaccine efficacy was 52% after first dose and 95% after second dose, paper shows. BMJ 371:m4826. doi: 10.1136/bmj.m4826. [DOI] [PubMed] [Google Scholar]
- 9.Moderna. 2020. Moderna announces primary efficacy analysis in phase 3 COVE study for its COVID-19 vaccine candidate and filing today with U.S. FDA for emergency use authorization. https://investors.modernatx.com/news-releases/news-release-details/moderna-announces-primary-efficacy-analysis-phase-3-cove-study. Accessed 21 December 2020.
- 10.Food and Drug Administration. 2020. Moderna COVID-19 vaccine. Food and Drug Administration, Silver Spring, MD. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/moderna-covid-19-vaccine.
- 11.Bwire GM 2020. Coronavirus: why men are more vulnerable to Covid-19 than women? SN Compr Clin Med doi: 10.1007/s42399-020-00341-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chakravarty D, Nair SS, Hammouda N, Ratnani P, Gharib Y, Wagaskar V, Mohamed N, Lundon D, Dovey Z, Kyprianou N, Tewari AK. 2020. Sex differences in SARS-CoV-2 infection rates and the potential link to prostate cancer. Commun Biol 3:374. doi: 10.1038/s42003-020-1088-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mueller AL, McNamara MS, Sinclair DA. 2020. Why does COVID-19 disproportionately affect older people? Aging (Albany NY) 12:9959–9981. doi: 10.18632/aging.103344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steinman JB, Lum FM, Ho PP-K, Kaminski N, Steinman L. 2020. Reduced development of COVID-19 in children reveals molecular checkpoints gating pathogenesis illuminating potential therapeutics. Proc Natl Acad Sci U S A 117:24620–24626. doi: 10.1073/pnas.2012358117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, Ji R, Wang H, Wang Y, Zhou Y. 2020. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis 94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gold MS, Sehayek D, Gabrielli S, Zhang X, McCusker C, Ben-Shoshan M. 2020. COVID-19 and comorbidities: a systematic review and meta-analysis. Postgrad Med 132:749–755. doi: 10.1080/00325481.2020.1786964. [DOI] [PubMed] [Google Scholar]
- 17.Khamis F, Al-Zakwani I, Al Naamani H, Al Lawati S, Pandak N, Omar MB, Al Bahrani M, Bulushi ZA, Al Khalili H, Al Salmi I, Al Ismaili R, Al Awaidy ST. 2020. Clinical characteristics and outcomes of the first 63 adult patients hospitalized with COVID-19: an experience from Oman. J Infect Public Health 13:906–913. doi: 10.1016/j.jiph.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang Q, Zhou Y, Wang X, Gao S, Xiao Y, Zhang W, Hu Y, Wang Y. 2020. Effect of hypertension on outcomes of adult inpatients with COVID-19 in Wuhan, China: a propensity score-matching analysis. Respir Res 21:172. doi: 10.1186/s12931-020-01435-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhumbra S, Malin S, Kirkpatrick L, Khaitan A, John CC, Rowan CM, Enane LA. 2020. Clinical features of critical coronavirus disease 2019 in children. Pediatr Crit Care Med 21:e948–e953. doi: 10.1097/PCC.0000000000002511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Derespina KR, Kaushik S, Plichta A, Conway EE, Jr, Bercow A, Choi J, Eisenberg R, Gillen J, Sen AI, Hennigan CM, Zerihun LM, Doymaz S, Keenaghan MA, Jarrin S, Oulds F, Gupta M, Pierre L, Grageda M, Ushay HM, Nadkarni VM, Agus MSD, Medar SS. 2020. Clinical manifestations and outcomes of critically ill children and adolescents with coronavirus disease 2019 in New York City. J Pediatr 226:55−63.e2. doi: 10.1016/j.jpeds.2020.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garazzino S, Montagnani C, Dona D, Meini A, Felici E, Vergine G, Bernardi S, Giacchero R, Lo Vecchio A, Marchisio P, Nicolini G, Pierantoni L, Rabbone I, Banderali G, Denina M, Venturini E, Krzysztofiak A, Badolato R, Bianchini S, Galli L, Villani A, Castelli-Gattinara G, Italian SITIP-SIP Pediatric Infection Study Group, Italian SITIP-SIP SARS-CoV-2 paediatric infection study group. 2020. Multicentre Italian study of SARS-CoV-2 infection in children and adolescents, preliminary data as at 10 April 2020. Euro Surveill 25(18):2000600. doi: 10.2807/1560-7917.ES.2020.25.18.2000600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim L, Whitaker M, O’Halloran A, Kambhampati A, Chai SJ, Reingold A, Armistead I, Kawasaki B, Meek J, Yousey-Hindes K, Anderson EJ, Openo KP, Weigel A, Ryan P, Monroe ML, Fox K, Kim S, Lynfield R, Bye E, Davis S, Smelser C, Barney G, Spina NL, Bennett NM, Felsen CB, Billing LM, Shiltz J, Sutton M, West N, Talbot HK, Schaffner W, Risk I, Price A, Brammer L, Fry AM, Hall AJ, Langley GE, Garg S, COVID-NET Surveillance Team. 2020. Hospitalization rates and characteristics of children aged <18 years hospitalized with laboratory-confirmed COVID-19 - COVID-NET, 14 states, March 1-July 25, 2020. MMWR Morb Mortal Wkly Rep 69:1081–1088. doi: 10.15585/mmwr.mm6932e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parri N, Lenge M, Buonsenso D, Coronavirus Infection in Pediatric Emergency Departments Research Group. 2020. Children with Covid-19 in pediatric emergency departments in Italy. N Engl J Med 383:187–190. doi: 10.1056/NEJMc2007617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kirenga B, Muttamba W, Kayongo A, Nsereko C, Siddharthan T, Lusiba J, Mugenyi L, Byanyima RK, Worodria W, Nakwagala F, Nantanda R, Kimuli I, Katagira W, Bagaya BS, Nasinghe E, Aanyu-Tukamuhebwa H, Amuge B, Sekibira R, Buregyeya E, Kiwanuka N, Muwanga M, Kalungi S, Joloba ML, Kateete DP, Byarugaba B, Kamya MR, Mwebesa H, Bazeyo W. 2020. Characteristics and outcomes of admitted patients infected with SARS-CoV-2 in Uganda. BMJ Open Respir Res 7:e000646. doi: 10.1136/bmjresp-2020-000646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang J, Zhang J, Tu Y, Zhou X, Huang H, Shao L, Chen L, Zhao Y, Ge M. 2020. Cancer patients in SARS-CoV-2 infection: a single-center experience from Wuhan. J Cancer 11:6243–6247. doi: 10.7150/jca.47065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ciceri F, Castagna A, Rovere-Querini P, De Cobelli F, Ruggeri A, Galli L, Conte C, De Lorenzo R, Poli A, Ambrosio A, Signorelli C, Bossi E, Fazio M, Tresoldi C, Colombo S, Monti G, Fominskiy E, Franchini S, Spessot M, Martinenghi C, Carlucci M, Beretta L, Scandroglio AM, Clementi M, Locatelli M, Tresoldi M, Scarpellini P, Martino G, Bosi E, Dagna L, Lazzarin A, Landoni G, Zangrillo A. 2020. Early predictors of clinical outcomes of COVID-19 outbreak in Milan, Italy. Clin Immunol 217:108509. doi: 10.1016/j.clim.2020.108509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abrishami A, Khalili N, Dalili N, Khaleghnejad TR, Farjad R, Samavat S, Neyriz Naghadehi A, Haghighatkhah H, Nafar M, Sanei-Taheri M. 2020. Clinical and radiologic characteristics of COVID-19 in patients with CKD. Iran J Kidney Dis 14:267–277. [PubMed] [Google Scholar]
- 28.Portoles J, Marques M, Lopez-Sanchez P, de Valdenebro M, Munez E, Serrano ML, Malo R, Garcia E, Cuervas V. 2020. Chronic kidney disease and acute kidney injury in the COVID-19 Spanish outbreak. Nephrol Dial Transplant 35:1353–1361. doi: 10.1093/ndt/gfaa189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suleyman G, Fadel RA, Malette KM, Hammond C, Abdulla H, Entz A, Demertzis Z, Hanna Z, Failla A, Dagher C, Chaudhry Z, Vahia A, Abreu Lanfranco O, Ramesh M, Zervos MJ, Alangaden G, Miller J, Brar I. 2020. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan Detroit. JAMA Netw Open 3:e2012270. doi: 10.1001/jamanetworkopen.2020.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Klang E, Kassim G, Soffer S, Freeman R, Levin MA, Reich DL. 2020. Severe obesity as an independent risk factor for COVID-19 mortality in hospitalized patients younger than 50. Obesity (Silver Spring) 28:1595–1599. doi: 10.1002/oby.22913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, Holden KA, Read JM, Dondelinger F, Carson G, Merson L, Lee J, Plotkin D, Sigfrid L, Halpin S, Jackson C, Gamble C, Horby PW, Nguyen-Van-Tam JS, Ho A, Russell CD, Dunning J, Openshaw PJ, Baillie JK, Semple MG, ISARIC4C investigators. 2020. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ 369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chachkhiani D, Soliman MY, Barua D, Isakadze M, Villemarette-Pittman NR, Devier DJ, Lovera JF. 2020. Neurological complications in a predominantly African American sample of COVID-19 predict worse outcomes during hospitalization. Clin Neurol Neurosurg 197:106173. doi: 10.1016/j.clineuro.2020.106173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chaudhry ZS, Williams JD, Vahia A, Fadel R, Parraga AT, Prashar R, Shrivastava P, Khoury N, Pinto CJ, Williams C, Nagai S, Abouljoud M, Samaniego-Picota M, Abreu-Lanfranco O, Del Busto R, Ramesh MS, Patel A, Alangaden GJ. 2020. Clinical characteristics and outcomes of COVID-19 in solid organ transplant recipients: a case-control study. Am J Transplant 20:3051−3060. doi: 10.1111/ajt.16188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen L, Liu S, Tian J, Pan H, Liu Y, Hu J, Wang M, Hou X. 2020. Disease progression patterns and risk factors associated with mortality in deceased patients with COVID-19 in Hubei Province, China. Immun Inflamm Dis 8:584–594. doi: 10.1002/iid3.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ciardullo S, Zerbini F, Perra S, Muraca E, Cannistraci R, Lauriola M, Grosso P, Lattuada G, Ippoliti G, Mortara A, Manzoni G, Perseghin G. 2020. Impact of diabetes on COVID-19-related in-hospital mortality: a retrospective study from Northern Italy. J Endocrinol Invest doi: 10.1007/s40618-020-01382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garcia-Azorin D, Martinez-Pias E, Trigo J, Hernandez-Perez I, Valle-Penacoba G, Talavera B, Simon-Campo P, de Lera M, Chavarria-Miranda A, Lopez-Sanz C, Gutierrez-Sanchez M, Martinez-Velasco E, Pedraza M, Sierra A, Gomez-Vicente B, Guerrero A, Ezpeleta D, Penarrubia MJ, Gomez-Herreras JI, Bustamante-Munguira E, Abad-Molina C, Orduna-Domingo A, Ruiz-Martin G, Jimenez-Cuenca MI, Juarros S, Del Pozo-Vegas C, Duenas-Gutierrez C, de Paula JMP, Canton-Alvarez B, Vicente JM, Arenillas JF. 2020. Neurological comorbidity is a predictor of death in Covid-19 disease: a cohort study on 576 patients. Front Neurol 11:781. doi: 10.3389/fneur.2020.00781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Giacomelli A, Ridolfo AL, Milazzo L, Oreni L, Bernacchia D, Siano M, Bonazzetti C, Covizzi A, Schiuma M, Passerini M, Piscaglia M, Coen M, Gubertini G, Rizzardini G, Cogliati C, Brambilla AM, Colombo R, Castelli A, Rech R, Riva A, Torre A, Meroni L, Rusconi S, Antinori S, Galli M. 2020. 30-day mortality in patients hospitalized with COVID-19 during the first wave of the Italian epidemic: a prospective cohort study. Pharmacol Res 158:104931. doi: 10.1016/j.phrs.2020.104931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Graham NSN, Junghans C, Downes R, Sendall C, Lai H, McKirdy A, Elliott P, Howard R, Wingfield D, Priestman M, Ciechonska M, Cameron L, Storch M, Crone MA, Freemont PS, Randell P, McLaren R, Lang N, Ladhani S, Sanderson F, Sharp DJ. 2020. SARS-CoV-2 infection, clinical features and outcome of COVID-19 in United Kingdom nursing homes. J Infect 81:411–419. doi: 10.1016/j.jinf.2020.05.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gutierrez Rodriguez J, Montero MJ, Jimenez MF, Guirola G-PC, Martinez RM, Gomez AL. 2020. Variables associated with mortality in a selected sample of patients older than 80 years and with some degree of functional dependence hospitalized for COVID-19 in a Geriatrics Service. Rev Esp Geriatr Gerontol 55:317−325. (In Spanish.) doi: 10.1016/j.regg.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.He Y, Xie M, Zhao J, Liu X. 2020. Clinical characteristics and outcomes of patients with severe COVID-19 and chronic obstructive pulmonary disease (COPD). Med Sci Monit 26:e927212. doi: 10.12659/MSM.927212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li J, Xu G, Yu H, Peng X, Luo Y, Cao C. 2020. Clinical characteristics and outcomes of 74 patients with severe or critical COVID-19. Am J Med Sci 360:229–235. doi: 10.1016/j.amjms.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Martos PF, Luque Del PJ, Jimenez Garcia N, Mora RE, Asencio MC, Garcia JJ, Navarro RF, Nunez RM. 2020. Comorbidity and prognostic factors on admission in a COVID-19 cohort of a general hospital. Rev Clin Esp (In Spanish.) doi: 10.1016/j.rce.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nikpouraghdam M, Jalali Farahani A, Alishiri G, Heydari S, Ebrahimnia M, Samadinia H, Sepandi M, Jafari NJ, Izadi M, Qazvini A, Dorostkar R, Tat M, Shahriary A, Farnoosh G, Hosseini Zijoud SR, Taghdir M, Alimohamadi Y, Abbaszadeh S, Gouvarchin Ghaleh HE, Bagheri M. 2020. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in Iran: a single center study. J Clin Virol 127:104378. doi: 10.1016/j.jcv.2020.104378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Parra-Bracamonte GM, Lopez-Villalobos N, Parra-Bracamonte FE. 2020. Clinical characteristics and risk factors for mortality of patients with COVID-19 in a large data set from Mexico. Ann Epidemiol 52:93−98.e2. doi: 10.1016/j.annepidem.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Raad M, Dabbagh M, Gorgis S, Yan J, Chehab O, Dagher C, Jamoor K, Hussein IH, Cook B, Van Harn M, Singh G, McCord J, Parikh S. 2020. Cardiac injury patterns and inpatient outcomes among patients admitted with COVID-19. Am J Cardiol 133:154–161. doi: 10.1016/j.amjcard.2020.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Salacup G, Lo KB, Gul F, Peterson E, De Joy R, Bhargav R, Pelayo J, Albano J, Azmaiparashvili Z, Benzaquen S, Patarroyo-Aponte G, Rangaswami J. 2021. Characteristics and clinical outcomes of COVID-19 patients in an underserved-inner city population: a single tertiary center cohort. J Med Virol 93:416–423. doi: 10.1002/jmv.26252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smith AA, Fridling J, Ibhrahim D, Porter PS, Jr. 2020. Identifying patients at greatest risk of mortality due to COVID-19: a New England perspective. West J Emerg Med 21:785–789. doi: 10.5811/westjem.2020.6.47957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Soares RCM, Mattos LR, Raposo LM. 2020. Risk factors for hospitalization and mortality due to COVID-19 in Espirito Santo State, Brazil. Am J Trop Med Hyg 103:1184–1190. doi: 10.4269/ajtmh.20-0483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sousa GJB, Garces TS, Cestari VRF, Florencio RS, Moreira TMM, Pereira MLD. 2020. Mortality and survival of COVID-19. Epidemiol Infect 148:e123. doi: 10.1017/S0950268820001405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Twigg HL, III, Khan SH, Perkins AJ, Roberts S, Sears C, Rahman O, Smith JP, Kapoor R, Farber MO, Ellender T, Carlos G, Gilroy G, Buckley J, Bosslet G, Machado R, Gao S, Khan BA. 2020. Mortality rates in a diverse cohort of mechanically ventilated patients with novel coronavirus in the urban Midwest. Crit Care Explor 2:e0187. doi: 10.1097/CCE.0000000000000187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.van Gerwen M, Alsen M, Little C, Barlow J, Genden E, Naymagon L, Tremblay D. 2021. Risk factors and outcomes of COVID-19 in New York City; a retrospective cohort study. J Med Virol 93:907–915. doi: 10.1002/jmv.26337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vena A, Giacobbe DR, Di Biagio A, Mikulska M, Taramasso L, De Maria A, Ball L, Brunetti I, Loconte M, Patroniti NA, Robba C, Delfino E, Dentone C, Magnasco L, Nicolini L, Toscanini F, Bavastro M, Cerchiaro M, Barisione E, Giacomini M, Mora S, Baldi F, Balletto E, Berruti M, Briano F, Sepulcri C, Dettori S, Labate L, Mirabella M, Portunato F, Pincino R, Russo C, Tutino S, Pelosi P, Bassetti M, GECOVID Study Group. 2020. Clinical characteristics, management and in-hospital mortality of patients with coronavirus disease 2019 in Genoa, Italy. Clin Microbiol Infect 26:1537−1544. doi: 10.1016/j.cmi.2020.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Zhou X, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y. 2020. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zou L, Dai L, Zhang Y, Fu W, Gao Y, Zhang Z, Zhang Z. 2020. Clinical characteristics and risk factors for disease severity and death in patients with coronavirus disease 2019 in Wuhan, China. Front Med 7:532. doi: 10.3389/fmed.2020.00532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bartoletti M, Giannella M, Scudeller L, Tedeschi S, Rinaldi M, Bussini L, Fornaro G, Pascale R, Pancaldi L, Pasquini Z, Trapani F, Badia L, Campoli C, Tadolini M, Attard L, Puoti M, Merli M, Mussini C, Menozzi M, Meschiari M, Codeluppi M, Barchiesi F, Cristini F, Saracino A, Licci A, Rapuano S, Tonetti T, Gaibani P, Ranieri VM, Viale P, PREDICO Study Group. 2020. Development and validation of a prediction model for severe respiratory failure in hospitalized patients with SARS-CoV-2 infection: a multicentre cohort study (PREDI-CO study). Clin Microbiol Infect doi: 10.1016/j.cmi.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Choi MH, Ahn H, Ryu HS, Kim BJ, Jang J, Jung M, Kim J, Jeong SH. 2020. Clinical characteristics and disease progression in early-stage COVID-19 patients in South Korea. J Clin Med 9:1959. doi: 10.3390/jcm9061959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ebinger JE, Achamallah N, Ji H, Claggett BL, Sun N, Botting P, Nguyen TT, Luong E, Kim EH, Park E, Liu Y, Rosenberry R, Matusov Y, Zhao S, Pedraza I, Zaman T, Thompson M, Raedschelders K, Berg AH, Grein JD, Noble PW, Chugh SS, Bairey Merz CN, Marban E, Van Eyk JE, Solomon SD, Albert CM, Chen P, Cheng S. 2020. Pre-existing traits associated with Covid-19 illness severity. PLoS One 15:e0236240. doi: 10.1371/journal.pone.0236240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lee JY, Hong SW, Hyun M, Park JS, Lee JH, Suh YS, Kim DH, Han SW, Cho CH, Kim HA. 2020. Epidemiological and clinical characteristics of coronavirus disease 2019 in Daegu, South Korea. Int J Infect Dis 98:462–466. doi: 10.1016/j.ijid.2020.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Romagnolo A, Balestrino R, Imbalzano G, Ciccone G, Riccardini F, Artusi CA, Bozzali M, Ferrero B, Montalenti E, Montanaro E, Rizzone MG, Vaula G, Zibetti M, Lopiano L. 2020. Neurological comorbidity and severity of COVID-19. J Neurol doi: 10.1007/s00415-020-10123-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Şenkal N, Meral R, Medetalibeyoğlu A, Konyaoğlu H, Kose M, Tukek T. 2020. Association between chronic ACE inhibitor exposure and decreased odds of severe disease in patients with COVID-19. Anatol J Cardiol 24:21–29. doi: 10.14744/AnatolJCardiol.2020.57431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shabrawishi M, Al-Gethamy MM, Naser AY, Ghazawi MA, Alsharif GF, Obaid EF, Melebari HA, Alamri DM, Brinji AS, Al Jehani FH, Almaimani W, Ekram RA, Alkhatib KH, Alwafi H. 2020. Clinical, radiological and therapeutic characteristics of patients with COVID-19 in Saudi Arabia. PLoS One 15:e0237130. doi: 10.1371/journal.pone.0237130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang G, Zhang Q, Zhao X, Dong H, Wu C, Wu F, Yu B, Lv J, Zhang S, Wu G, Wu S, Wang X, Wu Y, Zhong Y. 2020. Low high-density lipoprotein level is correlated with the severity of COVID-19 patients: an observational study. Lipids Health Dis 19:204. doi: 10.1186/s12944-020-01382-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Aggarwal A, Shrivastava A, Kumar A, Ali A. 2020. Clinical and epidemiological features of SARS-CoV-2 patients in SARI ward of a tertiary care centre in New Delhi. J Assoc Physicians India 68:19–26. [PubMed] [Google Scholar]
- 64.Pablos JL, Galindo M, Carmona L, Lledo A, Retuerto M, Blanco R, Gonzalez-Gay MA, Martinez-Lopez D, Castrejon I, Alvaro-Gracia JM, Fernandez Fernandez D, Mera-Varela A, Manrique-Arija S, Mena Vazquez N, Fernandez-Nebro A, RIER Investigators Group. 2020. Clinical outcomes of hospitalised patients with COVID-19 and chronic inflammatory and autoimmune rheumatic diseases: a multicentric matched cohort study. Ann Rheum Dis 79:1544–1549. doi: 10.1136/annrheumdis-2020-218296. [DOI] [PubMed] [Google Scholar]
- 65.Chhiba KD, Patel GB, Vu THT, Chen MM, Guo A, Kudlaty E, Mai Q, Yeh C, Muhammad LN, Harris KE, Bochner BS, Grammer LC, Greenberger PA, Kalhan R, Kuang FL, Saltoun CA, Schleimer RP, Stevens WW, Peters AT. 2020. Prevalence and characterization of asthma in hospitalized and nonhospitalized patients with COVID-19. J Allergy Clin Immunol 146:307–314 e4. doi: 10.1016/j.jaci.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Freites Nunez DD, Leon L, Mucientes A, Rodriguez-Rodriguez L, Font Urgelles J, Madrid Garcia A, Colomer JI, Jover JA, Fernandez-Gutierrez B, Abasolo L. 2020. Risk factors for hospital admissions related to COVID-19 in patients with autoimmune inflammatory rheumatic diseases. Ann Rheum Dis 79:1393–1399. doi: 10.1136/annrheumdis-2020-217984. [DOI] [PubMed] [Google Scholar]
- 67.Giorgi Rossi P, Marino M, Formisano D, Venturelli F, Vicentini M, Grilli R, Reggio Emilia COVID-19 Working Group. 2020. Characteristics and outcomes of a cohort of COVID-19 patients in the Province of Reggio Emilia, Italy. PLoS One 15:e0238281. doi: 10.1371/journal.pone.0238281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Killerby ME, Link-Gelles R, Haight SC, Schrodt CA, England L, Gomes DJ, Shamout M, Pettrone K, O’Laughlin K, Kimball A, Blau EF, Burnett E, Ladva CN, Szablewski CM, Tobin-D’Angelo M, Oosmanally N, Drenzek C, Murphy DJ, Blum JM, Hollberg J, Lefkove B, Brown FW, Shimabukuro T, Midgley CM, Tate JE, CDC COVID-19 Response Clinical Team. 2020. Characteristics associated with hospitalization among patients with COVID-19 - metropolitan Atlanta, Georgia, March-April 2020. MMWR Morb Mortal Wkly Rep 69:790–794. doi: 10.15585/mmwr.mm6925e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sun L, Shen L, Fan J, Gu F, Hu M, An Y, Zhou Q, Fan H, Bi J. 2020. Clinical features of patients with coronavirus disease 2019 from a designated hospital in Beijing, China. J Med Virol 92:2055–2066. doi: 10.1002/jmv.25966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wu Y, Hou B, Liu J, Chen Y, Zhong P. 2020. Risk factors associated with long-term hospitalization in patients with COVID-19: a single-centered, retrospective study. Front Med 7:315. doi: 10.3389/fmed.2020.00315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. 2020. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. 2020. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tabata S, Imai K, Kawano S, Ikeda M, Kodama T, Miyoshi K, Obinata H, Mimura S, Kodera T, Kitagaki M, Sato M, Suzuki S, Ito T, Uwabe Y, Tamura K. 2020. Clinical characteristics of COVID-19 in 104 people with SARS-CoV-2 infection on the Diamond Princess cruise ship: a retrospective analysis. Lancet Infect Dis 20:1043–1050. doi: 10.1016/S1473-3099(20)30482-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. 2020. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an updated analysis. Thromb Res 191:148–150. doi: 10.1016/j.thromres.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ranucci M, Ballotta A, Di Dedda U, Bayshnikova E, Dei Poli M, Resta M, Falco M, Albano G, Menicanti L. 2020. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemost 18:1747–1751. doi: 10.1111/jth.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Peng Y-H, Lin Y-S, Chen C-H, Tsai K-Y, Hung Y-C, Chen H-J, Liao W-C, Ho W-C. 2020. Type 1 diabetes is associated with an increased risk of venous thromboembolism: a retrospective population-based cohort study. PLoS One 15:e0226997. doi: 10.1371/journal.pone.0226997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mi Y, Yan S, Lu Y, Liang Y, Li C. 2016. Venous thromboembolism has the same risk factors as atherosclerosis: a PRISMA-compliant systemic review and meta-analysis. Medicine 95:e4495. doi: 10.1097/MD.0000000000004495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shang J, Ye G, Shi K, Wan Y, Luo C, Aihara H, Geng Q, Auerbach A, Li F. 2020. Structural basis of receptor recognition by SARS-CoV-2. Nature 581:221–224. doi: 10.1038/s41586-020-2179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wan Y, Shang J, Graham R, Baric RS, Li F. 2020. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol 94:e00127-20. doi: 10.1128/JVI.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhang W, Xu YZ, Liu B, Wu R, Yang YY, Xiao XQ, Zhang X. 2014. Pioglitazone upregulates angiotensin converting enzyme 2 expression in insulin-sensitive tissues in rats with high-fat diet-induced nonalcoholic steatohepatitis. ScientificWorldJournal 2014:603409. doi: 10.1155/2014/603409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Li XC, Zhang J, Zhuo JL. 2017. The vasoprotective axes of the renin-angiotensin system: physiological relevance and therapeutic implications in cardiovascular, hypertensive and kidney diseases. Pharmacol Res 125:21–38. doi: 10.1016/j.phrs.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lan J, Ge J, Yu J, Shan S, Zhou H, Fan S, Zhang Q, Shi X, Wang Q, Zhang L, Wang X. 2020. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature 581:215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 83.Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. 2020. Cardiovascular disease, drug therapy, and mortality in Covid-19. N Engl J Med 382:e102. doi: 10.1056/NEJMoa2007621. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 84.Zhang P, Zhu L, Cai J, Lei F, Qin J-J, Xie J, Liu Y-M, Zhao Y-C, Huang X, Lin L, Xia M, Chen M-M, Cheng X, Zhang X, Guo D, Peng Y, Ji Y-X, Chen J, She Z-G, Wang Y, Xu Q, Tan R, Wang H, Lin J, Luo P, Fu S, Cai H, Ye P, Xiao B, Mao W, Liu L, Yan Y, Liu M, Chen M, Zhang X-J, Wang X, Touyz RM, Xia J, Zhang B-H, Huang X, Yuan Y, Loomba R, Liu PP, Li H. 2020. Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res 126:1671–1681. doi: 10.1161/CIRCRESAHA.120.317134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sun X, Wang T, Cai D, Hu Z, Chen J, Liao H, Zhi L, Wei H, Zhang Z, Qiu Y, Wang J, Wang A. 2020. Cytokine storm intervention in the early stages of COVID-19 pneumonia. Cytokine Growth Factor Rev 53:38–42. doi: 10.1016/j.cytogfr.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Libby P 2007. Inflammatory mechanisms: the molecular basis of inflammation and disease. Nutr Rev 65:S140–S146. doi: 10.1111/j.1753-4887.2007.tb00352.x. [DOI] [PubMed] [Google Scholar]
- 87.Dooley KE, Chaisson RE. 2009. Tuberculosis and diabetes mellitus: convergence of two epidemics. Lancet Infect Dis 9:737–746. doi: 10.1016/S1473-3099(09)70282-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Orlicka K, Barnes E, Culver EL. 2013. Prevention of infection caused by immunosuppressive drugs in gastroenterology. Ther Adv Chronic Dis 4:167–185. doi: 10.1177/2040622313485275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Martinez J, Johnson CD, Sanchez-Paya J, de Madaria E, Robles-Diaz G, Perez-Mateo M. 2006. Obesity is a definitive risk factor of severity and mortality in acute pancreatitis: an updated meta-analysis. Pancreatology 6:206–209. doi: 10.1159/000092104. [DOI] [PubMed] [Google Scholar]
- 90.Al Mofleh IA 2008. Severe acute pancreatitis: pathogenetic aspects and prognostic factors. World J Gastroenterol 14:675–684. doi: 10.3748/wjg.14.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pi-Sunyer X 2009. The medical risks of obesity. Postgrad Med 121:21–33. doi: 10.3810/pgm.2009.11.2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yan LL, Daviglus ML, Liu K, Stamler J, Wang R, Pirzada A, Garside DB, Dyer AR, Van Horn L, Liao Y, Fries JF, Greenland P. 2006. Midlife body mass index and hospitalization and mortality in older age. JAMA 295:190–198. doi: 10.1001/jama.295.2.190. [DOI] [PubMed] [Google Scholar]
- 93.Al-Benna S 2020. Association of high level gene expression of ACE2 in adipose tissue with mortality of COVID-19 infection in obese patients. Obes Med 19:100283. doi: 10.1016/j.obmed.2020.100283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Krause M, Gerchman F, Friedman R. 2020. Coronavirus infection (SARS-CoV-2) in obesity and diabetes comorbidities: is heat shock response determinant for the disease complications? Diabetol Metab Syndr 12:63. doi: 10.1186/s13098-020-00572-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lockhart SM, O’Rahilly S. 2020. When two pandemics meet: why is obesity associated with increased COVID-19 mortality? Med (N Y) 1:33–42. doi: 10.1016/j.medj.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sattar N, McInnes IB, McMurray JJV. 2020. Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation 142:4–6. doi: 10.1161/CIRCULATIONAHA.120.047659. [DOI] [PubMed] [Google Scholar]
- 97.Ryan PM, Caplice NM. 2020. Is adipose tissue a reservoir for viral spread, immune activation, and cytokine amplification in coronavirus disease 2019? Obesity (Silver Spring) 28:1191–1194. doi: 10.1002/oby.22843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ryan DH, Ravussin E, Heymsfield S. 2020. COVID 19 and the patient with obesity - the editors speak out. Obesity (Silver Spring) 28:847. doi: 10.1002/oby.22808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Baena-Díez JM, Peñafiel J, Subirana I, Ramos R, Elosua R, Marín-Ibañez A, Guembe MJ, Rigo F, Tormo-Díaz MJ, Moreno-Iribas C, Cabré JJ, Segura A, García-Lareo M, Gómez de la Cámara A, Lapetra J, Quesada M, Marrugat J, Medrano MJ, Berjón J, Frontera G, Gavrila D, Barricarte A, Basora J, García JM, Pavone NC, Lora-Pablos D, Mayoral E, Franch J, Mata M, Castell C, Frances A, Grau M, FRESCO Investigators. 2016. Risk of cause-specific death in individuals with diabetes: a competing risks analysis. Diabetes Care 39:1987–1995. doi: 10.2337/dc16-0614. [DOI] [PubMed] [Google Scholar]
- 100.World Health Organization. 2018. Cancer. World Health Organization, Geneva, Switzerland https://www.who.int/news-room/fact-sheets/detail/cancer.
- 101.Arima H, Barzi F, Chalmers J. 2011. Mortality patterns in hypertension. J Hypertens 29(Suppl 1):S3–S7. doi: 10.1097/01.hjh.0000410246.59221.b1. [DOI] [PubMed] [Google Scholar]
- 102.Wang HE, Gamboa C, Warnock DG, Muntner P. 2011. Chronic kidney disease and risk of death from infection. Am J Nephrol 34:330–336. doi: 10.1159/000330673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. 2009. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Higgins JP, Thompson SG, Deeks JJ, Altman DG. 2003. Measuring inconsistency in meta-analyses. BMJ 327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Characteristics of included studies. Data included in this table, when available, included the title, country, age, number of participants, and the type of analysis applied. Download Table S1, DOCX file, 0.05 MB (55.4KB, docx) .
Copyright © 2021 Ng et al.
This content is distributed under the terms of the Creative Commons Attribution 4.0 International license.