Abstract
Objectives
Little is known about the mental health outcomes of hospitalized COVID-19 patients. The aims of the study were: (1) to examine the trajectories of anxiety, depression, and pandemic-related stress factors (PRSF) of COVID-19 hospitalized patients one-month following hospitalization; (2) to assess the presence of post-traumatic stress symptoms (PTSS) a month after hospitalization; (3) to identify baseline risk and protective factors that would predict PTSS one month after hospitalization.
Methods
We contacted hospitalized COVID-19 patients (n = 64) by phone, at three time-points: during the first days after admission to the hospital (T1); after ~two weeks from the beginning of hospitalization (T2), and one month after hospitalization (T3). At all time-points we assessed the levels of anxiety and depression symptoms, as well as PRSF. At T3, PTSS were assessed.
Results
The levels of depressive and anxiety symptoms decreased one-month following hospitalization. Moreover, higher levels of anxiety (standardized β = 1.15, 95% CI = 0.81–1.49, p < 0.001) and depression (β = 0.97, 95% CI = 0.63–1.31 p < 0.001) symptoms during the first week of hospitalization, feeling socially disconnected (β = 0.59, 95% CI = 0.37–0.81 p < 0.001) and experiencing a longer hospitalization period (β = 0.25, 95% CI = 0.03–0.47 p = 0.026) predicted higher PTSS scores a month post-hospitalization.
Conclusions
We identified early hospitalization risk factors for the development of PTSS one month after hospitalization that should be targeted to reduce the risk for PTSS.
Keywords: Anxiety, COVID-19, Depression, Mental health, Patients, PTSS
1. Introduction
The mental health outcomes associated with COVID-19 have been studied mainly among the general population and medical workforce [1,2]. However, evidence regarding mental health consequences of hospitalized patients with COVID-19 are largely understudied [2]. The majority of existing studies are cross-sectional, and showed high rates of depression, anxiety and post-traumatic stress symptoms (PTSS; [[3], [4], [5], [6]]). We recently described cross-sectional data, showing that immediately after hospitalization, COVID-19 patients reported high levels of anxiety symptoms and related pandemic worries [7]. Furthermore, patients who felt socially isolated experienced increased anxiety. While important, these studies did not examine the course of mental health outcomes of COVID-19 patients beyond a single assessment, and following discharge from the hospital. Research on previous pandemics showed that infected hospitalized patients reported increased psychological distress [8], and high rates of PTSS [9,10]. Extending these prior findings, the current study examined COVID-19 patients' mental health status during a one-month period following hospitalization. In addition, we aimed to identify baseline risk and protective factors that would predict PTSS one month following hospitalization.
2. Materials and methods
2.1. Participants
Participants were COVID-19 patients hospitalized at Sheba Medical Center, Israel, recruited between March 12th-May 4th 2020. Patients were contacted by phone and screened at three time points: T1–1-5 days following their admission to the hospital (M = 1.9, SD = 1.1); T2–6-18 days from admission (M = 9.2, SD = 2.0); and T3–30-45 days from admission (M = 33.8, SD = 2.7), while no longer in the hospital. The minimum number of days between T1 and T2 assessments were 6, and between T2 to T3 were 23. Patients who were younger than 18 or who had cognitive or language barriers, were excluded from the study. The study was approved by the Institutional Review Board of Sheba Medical Center, Israel (IRS#SMC-7182-20).
2.2. Measures
We employed the Hebrew versions of the Anxiety and Depression modules of the Patient-Reported Outcomes Measurement Information System (PROMIS; see www.nihpromis.org) Adult version [[11], [12], [13]]. We also examined pandemic-related stress factors (PRSF) using a 4-point Likert-type scale (from 0 = never, to 3 = always, see [7,13]). At T3, according to the PTSD criteria in the DSM-5 [14], PTSS were assessed using the Hebrew version of the Primary-Care PTSD Screen (PC-PTSD-5; [15]). Patients were asked five “yes”/"“no” questions regarding traumatic symptoms, specifically in relation to the COVID-19 pandemic.
The medical severity of COVID-19 illness (ranging from mild, moderate, to severe) was determined by the treating physicians (see [16]).
2.3. Statistical analysis
Anxiety and depression PROMIS scores were coded as continuous variables (T-scores) using the PROMIS coding system [13,17]. To examine differences in anxiety and depression PROMIS scores over time, and the trajectory of PRSF items, we used within-subject Friedman's Chi-Square test, with time as the independent variable. For post-hoc analysis we used Wilcoxon signed-rank tests with Bonferroni corrections.
PTSS PC-5 scores were calculated as the sum of positive replies, ranging from 0 to 5, with higher scores representing increased risk for traumatic symptoms. To evaluate the rate of patients who were at higher risk for PTSD, we chose a cut-off score of 3, which is the optimal score for screening [18]. To examine the baseline risk and protective factors associated with T3 PTSS scores, we used linear regression with PTSS PC-5 continuous scores as the dependent variable. Predictors in the model were age, sex, religiosity, number of days in hospitalization, severity of COVID-19 symptoms, PROMIS anxiety and depression scores (T1 + T2 mean), and PRSF (T1 + T2 mean). We report the regression coefficient with 95% confidence intervals. All probabilities were two-tailed, and the level of significance was 0.05.
3. Results
We approached 130 hospitalized patients. Of them, 90 met inclusion criteria and completed T1 screening (for more information, see [7]). Sixty-four patients completed all three time-points and were included in the final sample (71.1%). Twenty-six patients did not complete follow-up evaluations: 14 chose not to participate, 6 could not be reached, 4 patients experienced health deterioration, two patients died, and 1 patient's relative died. The mean age of the study population was 47.1 (SD = 15.5), 54.7% were male, and 32.8% were ultra-orthodox. There were no significant differences between the patients who completed the one-month follow-up and those who did not in age, sex, religiosity, symptom severity, T1 PROMIS anxiety and depression scores, and T1 PRSF scores. The two groups differed in length of hospitalization driven by the 4 patients with the deteriorating health condition (6.9 ± 4.3 for the patients who completed the one-month follow-up, vs. 21.2 ± 20.6 for the patients who did not, p < 0.001).
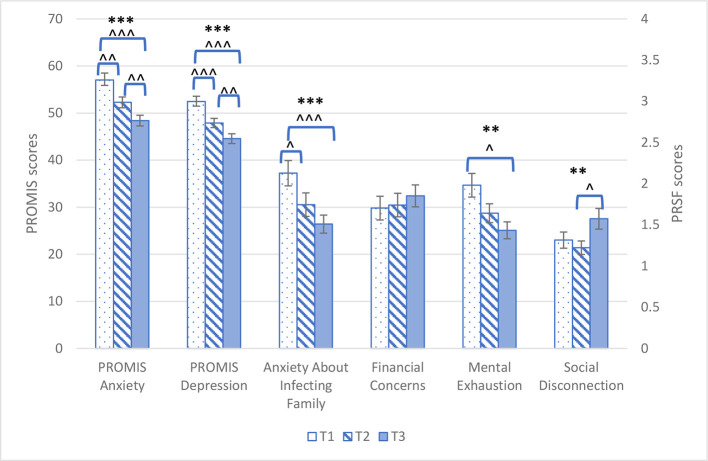
On Friedman's test, there was a significant decline in PROMIS anxiety (Friedman's χ 2(2) = 26.88, Kendall's W = 0.21, p < 0.001) and depression (Friedman's χ 2(2) = 41.09, Kendall's W = 0.32, p < 0.001) scores. On post-hoc analysis, all time differences were significant (p ≤ 0.004 for all comparisons, Fig. 1 and Table S3). Considering the PRSF, there was a significant decline in anxiety about infecting family and mental exhaustion (Friedman's χ 2(2) = 16.70, Kendall's W = 0.15, p < 0.001, Friedman's χ 2(2) = 8.51, Kendall's W = 0.08, p = 0.01, respectively). Conversely, feeling socially disconnected was higher at T3 compared to T1 and T2 (Friedman's χ 2(2) = 10.23, Kendall's W = 0.09 p = 0.01, Fig. 1). There were no significant differences in financial concerns at T3 compared to T1 and T2 (Friedman's χ 2(2) = 0.90, Kendall's W = 0.01, p = 0.64; Fig. 1 and Table S3).
Fig. 1.
Patients' (N = 64) longitudinal trajectory of PROMIS anxiety, depression and pandemic-related stress factors (PRSF) mean scores across the three time points.
Results are presented as means and SEs.
* < 0.05; ** = 0.01; *** < 0.001. Refers to the main analyses.
^ < 0.05; ^^ ≤ 0.004; ^^^ < 0.001. Refers to post-hoc analyses.
Considering the prevalence of PTSS, 12 patients (19.4%) had a PC-5 score ≥ 3, the standard score which indicates a positive screen [18].
On a linear regression, the following early-hospitalization factors predicted increased PTSS scores: increased levels of initial anxiety (standardized β = 1.15, 95% CI = 0.81–1.49, p < 0.001) and depression (β = 0.97, 95% CI = 0.63–1.31, p < 0.001), feeling mentally exhausted (β = 0.50, 95% CI = 0.25–0.76, p < 0.001), feeling socially disconnected (β = 0.59, 95% CI = 0.37–0.81, p < 0.001) and longer hospitalization period (β = 0.25, 95% CI = 0.03–0.47, p = 0.026). The severity of COVID-19 symptoms did not predict the levels of PTSS (Table 1 ). To overcome multicollinearity, independent variables were decontaminated from common variance by regressing them out of each other and then inserting their standardized residuals into the final model [19].
Table 1.
Baseline demographic and clinical characteristics, and one-month post-admission post-traumatic stress symptoms (n=58).
| Post-Traumatic Stress Symptoms |
|||
|---|---|---|---|
| Standardized β coefficients (95% CI) | T | P-value | |
| PROMIS Anxiety scorea | 1.15 (0.81 to 1.49) | 6.853 | <0.001 |
| PROMIS Depression scorea | 0.97 (0.63 to 1.31) | 5.707 | <0.001 |
| Social disconnectiona | 0.59 (0.37 to 0.81) | 5.461 | <0.001 |
| Mental exhaustiona | 0.50 (0.25 to 0.76) | 4.006 | <0.001 |
| Number of hospital days | 0.25 (0.03 to 0.47) | 2.293 | 0.026 |
| Sex, Female | 0.16 (−0.05 to 0.37) | 1.544 | 0.13 |
| COVID-19 symptoms severity | −0.16 (−0.38 to 0.06) | −1.447 | 0.15 |
| Age, years | −0.11 (−0.33 to 0.10) | −1.066 | 0.29 |
| Anxiety about infecting familya | 0.05 (−0.18 to 0.29) | 0.464 | 0.64 |
| Financial concernsa | 0.05 (−0.19 to 0.29) | 0.419 | 0.68 |
| Religiosity, ultra-orthodox | 0.04 (−0.18 to 0.25) | 0.359 | 0.72 |
R = 0.778, Adjusted R2 = 0.511.
Results are standardized residuals adjusted for all the other factors in the model.
Score = (T1score + T2score)/2
4. Discussion
To our knowledge, this is the first study that examined mental health outcomes in hospitalized COVID-19 patients beyond a single assessment. Consistent with studies of prior pandemics and in patients hospitalized for other medical conditions [17,18], we found that both anxiety and depressive symptoms levels decreased in the month following hospitalization. Although our results present spontaneous improvement in patients' mental health, we found that 19.4% of COVID-19 patients had above cut-off PTSS scores, and that longer hospitalization periods, feeling socially disconnected, feeling mentally exhausted and high levels of anxiety and depression symptoms at baseline increased the risk of PTSS one month following hospitalization.
At the beginning of the current pandemic, the Israeli Ministry of Health, following the World Health Organization (WHO; [20]), recommended the hospitalization of all detected patients, including those with mild and even no clinical symptoms. This recommendation might have had a negative effect in increasing the risk for PTSS at a one-month follow-up. Furthermore, in many cases of hospitalized COVID-19 patients in Israel, including in our study, patients were not allowed to be discharged from hospital until they were tested negative for COVID-19 on two consecutive tests. This situation exacerbated feelings of loss of control and uncertainty regarding the length of hospitalization, and in turn increased stress [21,22].
Our results indicate that feeling socially disconnected predicted the presence of PTSS a month after hospitalization. Furthermore, the levels of social disconnection were significantly higher at a one-month follow-up relative to baseline. Consistent with previous studies [23,24], these findings highlight the significance of social support during hospitalization of COVID-19 patients, as they are socially disconnected from their loved ones, and struggling with uncertainty regarding their health status and family concerns.
Our study has several limitations. First, we had a relatively small sample size. Second, the fact that all patients were from a single hospital in Israel, and that they were all in a stable (and overall mild) physical condition, reduced our ability to generalize the results to other countries and medical situations. Third, PTSS were assessed using a self-report screening questionnaire and not through a clinical evaluation of PTSD. Lastly, since we did not have a control group of non-hospitalized COVID-19 patients, we cannot conclude what the outcomes were in case patients were not hospitalized. Additionally, since we did not have a control group of non-COVID-19 hospitalized patients we cannot conclude which of the findings, if at all, are specific to COVID-19 patients.
In conclusion, our study indicates that ~20% of COVID-19 hospitalized patients develop significant PTSS a month after hospitalization. Previous studies using the PC-5 found that a cut-off score of 3 has a positive predictive value of 0.51 and specificity of 0.85 in indicating the presence of PTSD [18]. Therefore, COVID-19 hospitalized patients with a PC-5 score of ≥3, along with associated risk factors found in our study (i.e., high baseline depressive and anxiety symptoms, social disconnection and/or long hospitalization) should be treated to prevent the development of PTSD and other mental health sequelae.
Acknowledgements
We wish to thank Shira Bursztyn and Noy Meir for their assistance in interviewing the participants.
This work was supported by grants from Foundation Dora, Geneva, Switzerland and the Binational Science Foundation (Grant No. 2017369) and by Kirsh Foundation, New York, United States. The funding source had no role in the study design, collection, analysis, or interpretation of data, the writing of the article, or decision to submit the article for publication.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychores.2021.110399.
Appendix A. Supplementary data
Supplementary material
References
- 1.Carmassi C., Foghi C., Dell’Oste V., Cordone A., Bertelloni C.A., Bui E., Dell’Osso L. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. 2020;113312 doi: 10.1016/j.psychres.2020.113312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bo H.-X., Li W., Yang Y., Wang Y., Zhang Q., Cheung T., Wu X., Xiang Y.-T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol. Med. 2020:1–2. doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nie X.D., Wang Q., Wang M.N., Zhao S., Liu L., Zhu Y.L., Chen H. Anxiety and depression and its correlates in patients with coronavirus disease 2019 in Wuhan. Int. J. Psychiatry Clin. Pract. 2020:1–6. doi: 10.1080/13651501.2020.1791345. [DOI] [PubMed] [Google Scholar]
- 5.Zhao Q., Hu C., Feng R., Yang Y. Investigation of the mental health of patients with novel coronavirus pneumonia. Chin. J. Neurol. 2020;12 [Google Scholar]
- 6.Zhang J., Lu H., Zeng H., Zhang S., Du Q., Jiang T., Du B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immun. 2020;87:49–50. doi: 10.1016/j.bbi.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dorman Ilan S., Hertz-Palmor N., Brand Gothelf A., Hasson-Ohayon I., Matalon N., Gross R., Chen W., Abramovich A., Afek A., Ziv A., Kreiss Y., Pessach I.M., Gothelf D. Anxiety and depression symptoms in COVID-19 isolated patients and in their relatives. Front. Psychiatry. 2020 doi: 10.3389/fpsyt.2020.581598. Published in Frontiers in Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmed H., Patel K., Greenwood D.C., Halpin S., Lewthwaite P., Salawu A., Eyre L., Breen A., O'Connor R., Jones A., Sivan M. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. J. Rehabil. Med. 2020;52(5) doi: 10.2340/16501977-2694. (jrm00063) [DOI] [PubMed] [Google Scholar]
- 9.Hong X., Currier G.W., Zhao X., Jiang Y., Zhou W., Wei J. Posttraumatic stress disorder in convalescent severe acute respiratory syndrome patients: a 4-year follow-up study. Gen. Hosp. Psychiatry. 2009;31(6):546–554. doi: 10.1016/j.genhosppsych.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress after SARS. Emerg. Infect. Dis. 2005;11(8):1297–1300. doi: 10.3201/eid1108.041083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi S.W., Schalet B., Cook K.F., Cella D. Establishing a common metric for depressive symptoms: linking the BDI-II, CES-D, and PHQ-9 to PROMIS depression. Psychol. Assess. 2014;26(2):513–527. doi: 10.1037/a0035768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schalet B.D., Cook K.F., Choi S.W., Cella D. Establishing a common metric for self-reported anxiety: linking the MASQ, PANAS, and GAD-7 to PROMIS anxiety. J. Anxiety Disord. 2014;28(1):88–96. doi: 10.1016/j.janxdis.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mosheva M., Hertz-Palmor N., Dorman Ilan S., Matalon N., Pessach I.M., Afek A., Ziv A., Kreiss Y., Gross R., Gothelf D. 2020. Anxiety, Pandemic-Related Stress and Resilience among Physicians during the COVID-19 Pandemic, Depression and Anxiety. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Psychiatric Association . American Psychiatric Publishing; Washington, DC: 2013. Diagnostic and Statistical Manual of Mental Health Disorders: DSM-5. [Google Scholar]
- 15.Prins A., Bovin M., Kimerling R., Kaloupek D., Marx B., Pless Kaiser A., Schnurr P. 2015. The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5).[Measurement Instrument] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 17.PROMIS® Scoring Manuals. 2019. https://www.healthmeasures.net/promis-scoring-manuals
- 18.Prins A., Bovin M.J., Smolenski D.J., Marx B.P., Kimerling R., Jenkins-Guarnieri M.A., Kaloupek D.G., Schnurr P.P., Kaiser A.P., Leyva Y.E. The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J. Gen. Intern. Med. 2016;31(10):1206–1211. doi: 10.1007/s11606-016-3703-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garson G.D. 2019. Multilevel Modeling: Applications in STATA®, IBM® SPSS®, SAS®, R, & HLMTM, SAGE Publications. [Google Scholar]
- 20.World Health Organization . 2020. Home Care for Patients with Suspected Novel Coronavirus (nCoV) Infection Presenting with Mild Symptoms and Management of Contacts: Interim Guidance, 20 January 2020. [Google Scholar]
- 21.Abad C., Fearday A., Safdar N. Adverse effects of isolation in hospitalised patients: a systematic review. J. Hosp. Infect. 2010;76(2):97–102. doi: 10.1016/j.jhin.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guo Q., Zheng Y., Shi J., Wang J., Li G., Li C., Fromson J.A., Xu Y., Liu X., Xu H., Zhang T., Lu Y., Chen X., Hu H., Tang Y., Yang S., Zhou H., Wang X., Chen H., Wang Z., Yang Z. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav. Immun. 2020;88:17–27. doi: 10.1016/j.bbi.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maunder R.G., Lancee W.J., Rourke S., Hunter J.J., Goldbloom D., Balderson K., Petryshen P., Steinberg R., Wasylenki D., Koh D., Fones C.S. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom. Med. 2004;66(6):938–942. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- 24.Purssell E., Gould D., Chudleigh J. Impact of isolation on hospitalised patients who are infectious: systematic review with meta-analysis. BMJ Open. 2020;10(2) doi: 10.1136/bmjopen-2019-030371. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material