Beneath top-down national and state directives and recommendations, communities must respond to the many phases of coronavirus disease 2019 (COVID-19). The pandemic has unfolded differently across those communities with outcomes dependent on context, infrastructure, capacity, and how assets are organized, linked, and deployed. Achieving control requires real-time multisector data sharing, learning, and adaptation. Leaders from health care, public health, congregate care, elected offices, neighborhoods, schools, and businesses must work together to create systems that can respond to a pathogen that does not respect geographic, jurisdictional, or disciplinary boundaries.1
Response capabilities have been compromised by limited cross-sector coordination and decades-long disinvestment in public health.2, 3, 4 The Pandemic All-Hazards Preparedness Act of 2006 was passed to overcome these limitations by establishing an “electronic nationwide public health situational awareness capability through an interoperable network of systems to share data and information.”5 This goal has not been achieved,6 and communities continue to rely on insights pieced together, often manually, from multiple isolated sources.7 Data are often at too large a scale (ie, national or state) or too incomplete (ie, single sector or jurisdiction) to be useful for decision-making.
As severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) found its way to Greater Cincinnati, it became clear that we, like many communities, lacked processes and infrastructure to optimize pandemic control. We were confronted with difficult, urgent decisions without up-to-date data and coordination capabilities.8, 9, 10, 11 We sought to catalyze an agile and adaptive regional response using a learning health system (LHS) lens. Much as a hurricane disrupts travel, utilities, and access to needed services, so too has COVID-19 wreaked havoc across regions. One sector cannot respond to a hurricane; neither can one sector respond to COVID-19. Here, we describe how we used LHS principles to lower boundaries across sectors, promote collaborative sense-making, and grow coordinated infrastructure.
Developing a Learning Health System for a Regional COVID-19 Response
Design Principles
Our pre-existing regional emergency preparedness coalition defined Greater Cincinnati as including 14 counties in three states, with 22 hospitals and 17 local health departments serving more than 2 million people. Although response plans existed across jurisdictions and institutions, they were insufficiently linked. Thus, we quickly saw a need to use design and change management strategies, and a network organizational model,12 to catalyze an LHS “team of teams” to empower stakeholders to act with shared purpose. We applied the following guiding principles:
Engage Stakeholders to Co-Design Goals, Measures of Effectiveness, and Theory of Action
Initial discussions focused on pressing problems of hospital surge capacity and personal protective equipment availability. By delineating scope, scale, and boundaries that made sense epidemiologically and pragmatically, decision-makers came to understand cross-sector interconnections. The result was goals, measures, and a recognition of critical stakeholders not yet connected to the response (eg, congregate care leaders).
Integrate Data Streams to Create a Single Source for Measures
Widely available data streams provided the foundation for a complete, holistic, and accurate regional picture, beyond its component parts. By bringing together data into a single community-wide report, stakeholders developed a more holistic view of the pandemic. For instance, they were able to observe the relationship of community incidence to hospital and congregate care facility admission, not one or the other.
Use Data to Build Shared Purpose and Overcome Competition
In normal circumstances, stakeholders compete — hospitals for patients, social service agencies and universities for grant dollars. System-level measures revealed opportunities for learning, catalyzing alignment, and collective action.
Unleash Community Members’ Inherent Motivation, Insight, and Expertise
The pandemic resulted in a spontaneous outpouring of contributions by scientists, organizations, and citizens. Harnessing such expertise added capacity and accelerated innovation (eg, voluntary participation of media companies in developing communication strategies).
Facilitate Rapid Learning
What was appropriate on day 1 was not on day 30. Structured improvement methods facilitated adaptation to rapidly changing context and identification of answers to emerging questions (eg, how to establish outdoor testing sites in cold weather, where to locate sites to optimize equitable access, and how to communicate to diverse populations). Small-scale testing and cross-sector learning generated the know-how needed to identify and scale up solutions.
Developing an Aim and a Theory for Action
Aims and theory emerged from these principles. In mid-March 2020, a coalition of health care, public health, and community leaders came together, convened by the Regional Health Information Organization that serves as the hub for health information exchange and emergency preparedness. A team with expertise in design, change management, improvement, epidemiology, analytics, and community health was recruited from local academic medical centers to help assembled stakeholders create regional situational awareness and strategy. Initial participants were hospital leaders, but participation evolved and grew over time, ultimately becoming a regional multi-agency coalition (MAC) composed of leaders from stakeholder organizations and sectors.
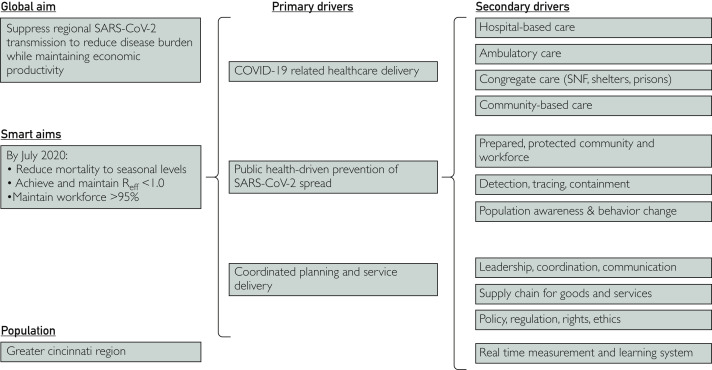
Within ∼10 days of Greater Cincinnati’s first SARS-CoV-2 case, our situational awareness and strategy team worked with the growing MAC to 1) develop and agree on a shared aim — to suppress regional SARS-CoV-2 transmission to reduce disease burden while maintaining economic productivity; 2) delineate scope of activities by defining populations, geographies, and partners; and 3) identify drivers of a successfully networked system comprised of effective health care delivery, public health-driven prevention, and coordinated cross-sector planning and service delivery (Figure 1 ).
Figure 1.
Simplified early iteration of system-level key driver diagram showing the aim and theory for action for the regional response to coronavirus disease 2019 (COVID-19). Our global and SMART aims are listed on the left. Primary and secondary drivers extend on the middle and right side of the figure, respectively. Reff, effective reproductive ratio; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; SMART, specific, measurable, achievable, realistic, timebound; SNF, skilled nursing facility.
Focusing on Shared Measurement
We then defined measures related to our aim, drawing on practices from around the world. Officials in Wuhan, China, used municipal public health measures such as daily case incidence and effective reproductive ratios to inform and evaluate effectiveness of nonpharmaceutical interventions over time.11 Taiwan demonstrated how integrated “timely, accurate, and transparent” data meaningfully informed responses.13
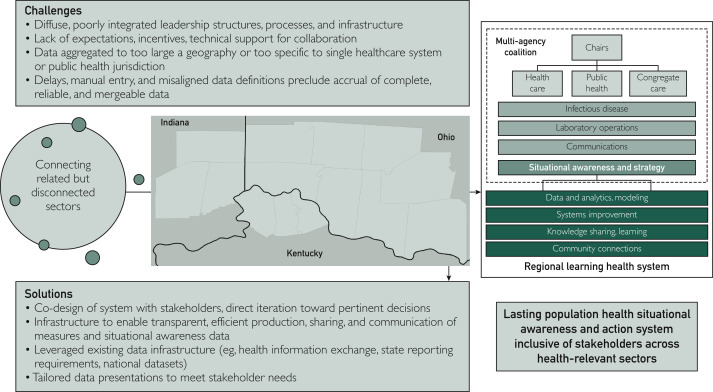
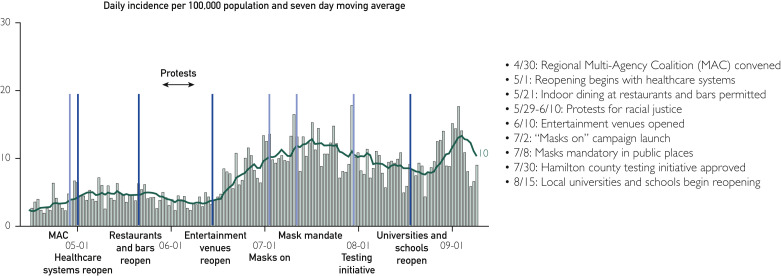
By early April, we were producing a shared dashboard daily for MAC members — leaders from area hospitals, public health jurisdictions, and congregate care facilities alongside subject matter experts and support teams like ours (Figure 2 ). The process of agreeing upon and then using measures built shared commitment and deepening understanding of the interdependent components of the system these leaders were seeking to manage. We related incidence and spread to downstream pandemic effects: health care system impact (ie, hospital occupancy, ventilator use, personal protective equipment availability, and death) and community capability (ie, access to testing, test turnaround time, participation in contact tracing, and time-lags from symptom to isolation).14 We depicted measures at different levels of aggregation — entire region, county, neighborhood, health care system, and hospital — and across vulnerable subpopulations (those residing in congregate care facilities, living in impoverished neighborhoods, and of minority race or ethnicity). We used statistical process control methods to differentiate significant change from random variation.15 Geospatial approaches identified case clusters and enhanced awareness of background context.16 Annotations on charts and maps helped the MAC relate changes in intervention strategies to changes in measures (Figure 3 ).
Figure 2.
Schematic pathway from disconnected sectors to an integrated regional population health situational awareness and action system, using Greater Cincinnati’s coronavirus disease 2019 (COVID-19) Multi-Agency Coalition (MAC) as an example. The left side shows the oft-separate, siloed sectors. To connect these related but disconnected sectors for a region such as Greater Cincinnati (map in the center), there are a series of challenges (middle-top) that can be met through the identified solutions (middle-bottom). For the current pandemic, this resulted in the MAC depicted on the right. The MAC is co-chaired by the chief executive officer (CEO) of a large adult health care system and the CEO of the organization serving as both the convener of the regional disaster preparedness coalition and the Regional Health Information Organization. The MAC includes appointed representatives of regional health care systems, two public health commissioners representing regional public health jurisdictions, and a leader of the Council on Aging and CEO of a long-term care facility representing congregate care facilities (including skilled nursing facilities, jails, halfway houses, shelters, etc). Support teams include representation of infectious disease specialists, a chair of pathology representing laboratory operations, communications (linked to the Chamber of Commerce and business community), and our situational awareness and strategy team. Since the formation of the MAC, additional sectors and their representatives have been added, including those from schools and universities. Together, the MAC and teams that support the MAC focus on aims relating to disease containment, testing and tracing, nonpharmaceutical interventions, communications across sectors and with the public, and supply chain (eg, hospital beds, ventilators, and personal protective equipment). Such a structure could have lasting ramifications as we seek population health situational awareness and action to outlast COVID-19.
Figure 3.
Annotated chart depicting daily case incidence, measured per 100,000 population, with a 7-day moving average. Each line indicates an event or change expanded upon with the list on the right side. Light blue lines indicate mitigation-oriented interventions. Dark blue lines indicate background changes likely influencing viral transmission.
By early May, we were producing a subset of dashboard measures to share publicly.17 This enhanced transparency extended the reach of the LHS, further enabling real-time learning and action across still more sectors (eg, schools, universities, and businesses).9 , 10 , 18 , 19 These measures continue to provide the single trusted regional COVID-19 picture looked to by those in health-relevant sectors, the media, and public alike. Data within the dashboard have evolved over time, changing because of needs identified and feedback obtained.
The discussions data generate inform important decisions and expedite structured, continuous improvement processes. In the pandemic’s initial surge phase, data about stable hospital capacity informed a decision to not open Cincinnati’s convention center as a field hospital, saving tens of millions of dollars. Identification of increasing case incidence following reopening in May and June directly stimulated community-wide “mask on” communication campaigns supported by the regional Chamber of Commerce and business community. Granular depictions of geographic case clusters helped detect outbreaks in congregate care facilities and emergent racial or ethnic inequities. Geospatial analytics informed decisions about locations for community testing. Networked leaders also began using the data to drive improvement. Health departments reduced lags in contact tracing. Community testing teams worked with partnered organizations and community centers to increase demand for and accessibility of tests. Schools brought data to decisions about re-opening and improvement methods to efforts to maximize students reached while on virtual instruction.20 Regular use of available data also mitigated data shortcomings (eg, inaccurate or incomplete data or inconsistent operational definitions). A local health care leader commented that routinely reflecting on and critically evaluating data “allowed [stakeholders] to look outside [their] span of control, toward bigger community issues” reflective of the broader regional system.
Moving From COVID-19 Toward Lasting Infrastructure
Despite the presence of the Regional Health Information Organization and preparedness infrastructure, we encountered several important challenges (Figure 2). First, regional health care institutions are active competitors, historically reluctant to share data. Second, like in many regions, our health information exchanges tend to be siloed, excluding public health, congregate care, and social services data.21 , 22 Third, the sheer number of jurisdictions, organizations, and sectors creates immense alignment, measurement, and improvement challenges. Finally, delays in data entry, manual entry, and unclear data definitions make interpretation difficult.
To overcome challenges and connect disconnected sectors, our situational awareness and strategy team used data, analytics, and modeling to identify solutions and meet decision-making needs of stakeholders. We routinely identified data sources and developed prototype measures relevant to immediate needs. Reviewing data relative to regional goals was the first topic on the agenda of every MAC and subgroup meeting (often multiple times weekly). During these meetings, we elicited feedback on measure utility and presentation23 and responded with revisions and new analyses as needed (often within 24 hours). As possible, we used existing infrastructure. Continuous measure reviews helped identify and mitigate reporting errors and unearth immediate needs.
In parallel, we provided coaching in systems improvement, knowledge sharing, and community connection. We facilitated rapid learning cycles where stakeholder organizations learned from small-scale tests of changes and from one another. We continuously identified best practices from other regions, sharing knowledge back with regional partners. We identified contextual realities within neighborhoods and on the front lines, facilitating the co-design of tailored solutions. Transparent data sharing, learning from variation, sharing best practices, and connecting with community members deepened trust, stimulated action, and enabled participants to see themselves as part of one LHS with common objectives.24 This approach, built from the bottom-up, facilitated the identification, contextualization, and alignment of responses to new challenges or top-down directives.
There is now an opportunity to build better national infrastructure by learning from hundreds of small-scale responses like ours. Future phases of this pandemic, other pandemics, climate events, and economic disasters all could benefit from such infrastructure and learning. Complex challenges demand coordinated, integrated, and adaptive functionalities across relevant sectors. Recognizing the power of LHS approaches like ours has the potential to inform policy and support better systems for emergency preparedness and for population health. Indeed, COVID-19 highlights the urgency to achieve data interoperability and trustworthy integration of data, programs, and ideas.6 Building a national system by capturing regional innovations (and learning from failures) may seem daunting, but it is a tractable problem. There are fewer than 400 metropolitan statistical areas similar to Greater Cincinnati across the United States. It is possible to gather and curate the best of what is taking place in such regions, share it broadly, and provide mechanisms to access not just technical experts, but also peers who have solved similar problems.25
Regions must also have the resources and supports necessary to optimize existing capabilities and then extend them. Policies and incentives should promote cross-jurisdictional and cross-sector alignment. Learning health system development will require support for technical assistance to learn and apply new methods of system change and collaborative learning. It will also require investments in educating the next generation of LHS improvers, and researching how LHS design, technology, and data and digital governance shape communities’ ability to respond at the speed and scale of epidemics.
Conclusion
To enhance likelihood of success, health care systems, public health jurisdictions, congregate care facilities, elected officials, neighborhood leaders, schools, and businesses must work together to pursue solutions to complex problems such as COVID-19. Learning health system approaches and principles facilitate broad community alignment and dynamic, collaborative action. An enduring, dynamic, adaptive population health situational awareness and action LHS, built from the bottom-up, can help us to emerge stronger, enabling swift, comprehensive responses to future phases of this pandemic and to other epidemics sure to follow.
Acknowledgments
This work, and broader efforts to manage this once-in-a-lifetime pandemic, would not have been possible without the efforts of countless individuals, teams, and organizations across Greater Cincinnati. We explicitly thank those within our health care systems, our public health departments, and our community who have been at the front lines during our regional COVID-19 experience.
We would also like to thank Mr Ben Dawson, Mr Jason Bubenhofer, Mr Perry Ellington, Mr Alex Vaillancourt, and Ms Esther Cleary for their efforts in support of population health situational awareness. We thank Dr Stephen Davis, Dr Evaline A. Alessandrini, Dr Rick Lofgren, Dr Dustin Calhoun, Mr Craig Brammer, and Ms Tiffany Mattingly for their leadership and for their review of this manuscript.
Footnotes
Ms Saeed’s current affiliation is Boston Children’s Hospital, Boston, MA.
Potential Competing Interests: The authors report no potential competing interests.
Supplemental Online Material
References
- 1.Romanelli R.J., Azar K.M.J., Sudat S., Hung D., Frosch D.L., Pressman A.R. The learning health system in crisis: lessons from the novel coronavirus disease pandemic. Mayo Clin Proc Innov Qual Outcomes. 2020;5(1):171–176. doi: 10.1016/j.mayocpiqo.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Calonge N., Brown L., Downey A. Evidence-based practice for public health emergency preparedness and response: recommendations from a National Academies of Sciences, Engineering, and Medicine Report. JAMA. 2020;324(7):629–630. doi: 10.1001/jama.2020.12901. [DOI] [PubMed] [Google Scholar]
- 3.Endsley M.R. The Role of Situation Awareness in Naturalistic Decision Making. In: Zsambok C.E., Klein G., editors. Naturalistic Decision Making. Psychology Press; New York, NY: 1997. [Google Scholar]
- 4.Schneider E.C. Failing the test — the tragic data gap undermining the US pandemic response. N Engl J Med. 2020;383(4):299–302. doi: 10.1056/NEJMp2014836. [DOI] [PubMed] [Google Scholar]
- 5.Public Law 109–417—December 19, 2006 — Pandemic and All-Hazards Preparedness Act. 2006. https://www.govinfo.gov/content/pkg/PLAW-109publ417/pdf/PLAW-109publ417.pdf
- 6.Public Health Information Technology: HHS Has Made Little Progress toward Implementing Enhanced Situational Awareness Network Capabilities. 2017. https://www.gao.gov/assets/690/686971.pdf
- 7.Knieser L. The Case for A Situational Awareness Network for Emergency Response. 2020. https://www.healthitanswers.net/the-case-for-a-situational-awareness-network-for-emergency-response/
- 8.Sittig D.F., Singh H. COVID-19 and the Need for a National Health Information Technology Infrastructure. JAMA. 2020;323(23):2373–2374. doi: 10.1001/jama.2020.7239. [DOI] [PubMed] [Google Scholar]
- 9.Inglesby T.V. Public health measures and the reproduction number of SARS-CoV-2. JAMA. 2020;323(21):2186–2187. doi: 10.1001/jama.2020.7878. [DOI] [PubMed] [Google Scholar]
- 10.Hartley D.M., Perencevich E.N. Public health interventions for COVID-19: emerging evidence and implications for an evolving public health crisis. JAMA. 2020;323(19):1908–1909. doi: 10.1001/jama.2020.5910. [DOI] [PubMed] [Google Scholar]
- 11.Pan A., Liu L., Wang C. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323(19):1915–1923. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fjeldstad O.D., Snow C.C., Miles R.E., Lettl C. The architecture of collaboration. Strategic Manag J. 2012;33(6):734–750. [Google Scholar]
- 13.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020;323(14):1341–1342. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 14.Kretzschmar M.E.R.G., Bootsma M.C.J., van Boven M., van de Wijgert J.H.H.M., Bonten M.J.M. Impact of delays on effectiveness of contact tracing strategies for COVID-19: a modelling study. Lancet Public Health. 2020;5(8):e452–e459. doi: 10.1016/S2468-2667(20)30157-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Benneyan J.C., Lloyd R.C., Plsek P.E. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12(6):458–464. doi: 10.1136/qhc.12.6.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chowkwanyun M., Reed A.L., Jr. Racial health disparities and COVID-19 — Caution and Context. N Engl J Med. 2020;383(3):201–203. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- 17.The Health Collaborative Situational Dashboard. https://www.cctst.org/covid19 2020.
- 18.Krieger N., Gonsalves G., Bassett M.T., Hanage W., Krumholz H.M. The Fierce Urgency Of Now: Closing Glaring Gaps In US Surveillance Data On COVID-19. Health Affairs Blog. https://www.healthaffairs.org/do/10.1377/hblog20200414.238084/full/
- 19.Ng Y., Li Z., Chua Y.X. Evaluation of the effectiveness of surveillance and containment measures for the first 100 patients with COVID-19 in Singapore — January 2–February 29, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(11):307–311. doi: 10.15585/mmwr.mm6911e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.COVID-19. Hamilton County Public Health. 2020. https://www.hamiltoncountyhealth.org/covid19/
- 21.Kierkegaard P., Kaushal R., Vest J.R. Applications of health information exchange information to public health practice. AMIA Annu Symp Proc. 2014;2014:795–804. [PMC free article] [PubMed] [Google Scholar]
- 22.Holmgren A.J., Adler-Milstein J. Health information exchange in US Hospitals: the current landscape and a path to improved information sharing. J Hosp Med. 2017;12(3):193–198. doi: 10.12788/jhm.2704. [DOI] [PubMed] [Google Scholar]
- 23.James B. Information system concepts for quality measurement. Med Care. 2003;41(suppl 1):I71–I79. doi: 10.1097/00005650-200301001-00008. [DOI] [PubMed] [Google Scholar]
- 24.Diez Roux A.V. Population Health in the Time of COVID-19: Confirmations and Revelations. Milbank Q. 2020;98(3):629–640. doi: 10.1111/1468-0009.12474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.COVID Local. 2020. https://covid-local.org/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.