Abstract
Nearly all families in the United States were exposed to varying degrees of stress related to the COVID-19 pandemic during the spring of 2020. Building on previous research documenting the pernicious effects of stress on youth mental health, we aimed to test the effects of exposure to COVID-19-related stress on youth symptomatology. Further, in light of evidence suggesting that parents play an important role in buffering children from environmental stress, we assessed how specific parental behaviors (i.e., parental emotion socialization, maintenance of home routines, and availability to discuss the pandemic with child) contributed to effective parental buffering of the impact of pandemic-related stress on children’s symptomatology. Conversely, we tested whether parental anxiety-related symptomatology and parenting stress exacerbated the effect of children’s exposure to pandemic-related stress on children’s symptomatology. Results suggest that parents who engaged in relatively higher levels of emotion coaching of children’s negative emotions and who maintained more stable home routines during the pandemic were more effectively able to buffer the effects of pandemic-related stress on children’s symptomatology. Parents who reported higher levels of parenting stress and anxiety-related symptomatology were less likely to effectively buffer stress. Though interpretation of the findings is limited due to sole reliance on parental report and the cross-sectional study design due to the constraints of collecting data during a global pandemic, findings underscore the importance of assessing family-level factors when considering the impact of stressors on children’s symptomatology and highlight the need to support parents during global events that place families under significant stress.
Keywords: Emotion socialization, Parental buffering, COVID-19, Stress, Parenting
Introduction
The global COVID-19 pandemic represents a major stressor for nearly all families in the United States (Liu and Doan, 2020). Given widespread governmental directives enforcing social distancing and pervasive isolation, nearly all aspects of family life were disrupted during the spring of 2020. Parents were required to work remotely without access to childcare or to work in essential roles while risking disease transmission for themselves and their families. Children transitioned to online schooling, with an increased burden for managing learning falling on parents. Many families faced additional concerns related to job loss and food and housing insecurity, as well as long-term effects of isolation on family members’ mental and physical health. Additional family-level challenges included securing medical care for individuals with chronic conditions, having inadequate supplies or access to technological resources at home, and dealing with the monotony and uncertainty inherent in indefinite quarantine (Pfefferbaum and North, 2020).
Recent meta-analyses and reviews examining psychological impacts of the pandemic have documented its widespread behavioral and emotional effects, including increased stress and symptomatology (Brooks et al., 2020; Rajkumar, 2020; Torales et al., 2020). Though the effects of the COVID-19 pandemic on youth mental health in the United States have yet to be investigated, initial evidence from studies of Chinese children exposed to COVID-19-related stress suggests significant psychological distress among youth in response to the pandemic (Jiao et al., 2020; Liang et al., 2020; Xie et al., 2020; see Racine et al., 2020 for a review of literature to date). Further, experts have highlighted the need for attention to the potentially detrimental effects of the pandemic on youth mental health (Fegert et al., 2020; Gruber et al., 2020; Holmes et al., 2020), in part due to the restriction of access to mental health services typically provided in school settings (Golberstein et al., 2020; Masonbrink & Hurley, 2020). Previous research examining the impacts of exposure to early life stress on the development of youth symptomatology also sheds light on the mental health implications of youth exposure to stress, underscoring risk for development of internalizing and externalizing problems (McLaughlin et al., 2012).
Despite the potential negative effects of stress exposure on youth mental health, stress exposure does not affect all children equally, perhaps, in part, due to variation in social support resources available (Compas et al., 2001). A growing body of research highlights that parents can effectively buffer children from the deleterious effects of stress. In addition to providing offspring with the safety and security necessary for survival, a central role of caregivers is to provide external regulation for their children’s emotions (Eisenberg et al.,1998) and to support development of children’s intrinsic capacity for self-regulation (Hofer, 1978), which is particularly relevant during and following exposure to stress. The potent buffering effect of parental presence on children’s reactivity to stress is also visible at the physiological level. Specifically, parental presence can buffer the effect of stress by dampening children’s cortisol reactivity (Gunnar & Donzella, 2002) and amygdala reactivity (Gee et al., 2014). However, there is substantial variability in the degree to which parents buffer children from the deleterious effects of stress, and specific parental factors may moderate the degree to which parental presence during a child’s experience of stress buffers children from the negative effects of stress exposure (Williamson et al., 2017).
Although American families were exposed to COVID-19-related stress to varying degrees, depending on factors such as the severity of the outbreak in a family’s geographical area, family SES, and racial/ethnic identity (Hooper et al., 2020), the COVID-19 pandemic represents a universal stressor for all families. Therefore, the COVID-19 pandemic represents a naturalistic opportunity to investigate how caregivers may effectively buffer or exacerbate the effects of stress on children’s mental health. Further, widespread shelter-in-place orders and voluntary quarantine across the United States meant that children and adolescents were more reliant on parents to provide support and assistance, without access to broader social resources for support, which may amplify buffering processes in the parent–child relationship.
The Present Study
The present study aimed to delineate the impacts of family-level COVID-19-related stress on child functioning. Specifically, we aimed to 1) assess associations between family-level stress directly related to the COVID-19 pandemic and child symptomatology; 2) assess parental factors that may promote effective parental buffering (i.e., parental emotion socialization, parental availability to discuss COVID-19, and parental maintenance of routines) of the effect of pandemic-related stressors on child symptomatology, and 3) assess parental factors that may exacerbate the effect of pandemic-related stressors on child symptomatology (i.e., parenting stress, parental symptomatology). Here we briefly review relevant factors that may promote effective parental buffering or exacerbation of pandemic-related stress on children’s symptomatology.
Parental Emotion Socialization
Parental emotion coaching, defined as the degree to which parents assist their children in identifying their emotions, show respect for their children’s emotional expression, and play an active role in situations that trigger emotions, has been found to be a protective factor for children exposed to a range of stressors (Cohodes et al., 2017; Greene et al., 2020). Parents who report engaging in higher levels of emotion coaching tend to report that they view their children’s negative emotions as opportunities to scaffold children’s development of effective emotion regulation strategies, build intimacy with their children, and help their children think of strategies to cope with emotions (Gottman et al., 1996).
Parental Availability for Discussion of Stressful Events
Highly related to parental emotion socialization, previous studies have identified that parental availability to discuss stressors may mitigate the negative effects of stress-exposure on children’s symptomatology (Carpenter et al., 2017; Stallard et al., 2001). Parents who provide opportunities for children to engage in discussions about their reactions to stressful events may be able to prevent children’s development of symptomatology by helping children to reframe negative appraisals of stressful events and to co-create a narrative about a stressor (Goodman et al., 1997; Williamson et al., 2018). Relatedly, parental discussion of stressful events with children has been proposed as one mechanism by which parents may be able to affect the content of children’s narratives about stress exposure (Fivush et al., 2003), ultimately buffering the potentially harmful effects of exposure to stress on children’s development of symptomatology (Kilmer and Gil‐Rivas, 2010).
Parental Maintenance of Family Routines and Practices
Parental maintenance of family routines and practices following children’s exposure to stress is associated with reduced child symptomatology (Boyce, 1981; Foy, 1992). More broadly, familial commitment to routines has been found to buffer the psychological effects of exposure to trauma (Greeff & Wentworth, 2009) and has therefore been hypothesized to be a key family-level mechanism by which parents can promote children’s resilience following stress exposure (Williamson et al., 2018).
Parental Stress and Symptomatology
A recent meta-analysis examining psychiatric effects of exposure to the COVID-19 pandemic identified anxiety- and depression-related symptomatology as a common response to the stressors imposed by the pandemic among adults (Rajkumar, 2020). Parents’ own levels of stress and symptomatology may have profound effects on children’s coping (Kerns & Brumariu, 2017). Representing one possible mechanism by which higher levels of parental stress and symptomatology inhibit effective parental buffering of child exposure to stress, previous studies have documented that parents experiencing high levels of symptomatology may be less available to support children in managing their own stress-related responses, model effective coping, and engage in familial communication about stressors (Lyons-Ruth et al., 2002; Ponnet et al., 2012; Radke-Yarrow et al., 1993).
Hypotheses
We hypothesized that there would be a positive association between family-level COVID-19-related stress and children’s internalizing and externalizing symptomatology. Furthermore, we hypothesized that parental emotion coaching, availability to discuss COVID-19, and maintenance of family routines during the pandemic would moderate the association between child exposure to pandemic-related stress and symptomatology, such that children of parents who engaged in high levels of emotion coaching, who were more available to discuss COVID-19, and who maintained family routines to a greater degree during the pandemic would be less symptomatic in response to pandemic-related stress. Conversely, we hypothesized that parental stress and anxiety-related symptomatology would exacerbate the effects of pandemic-related stress on children, such that children of parents who reported higher levels of parenting stress and anxiety-related symptomatology would exhibit higher levels of internalizing and externalizing symptomatology.
Method
Pre-Registration
We pre-registered exploratory study hypotheses, detailed methods and procedures, and a preliminary data analysis plan for the present study (including exclusion criteria and data-stopping rules) using the Open Science Framework repository (https://osf.io). The pre-registration was submitted prior to analysis of the data and was embargoed in order to prevent modification.
Participants
Table 1 provides descriptive statistics for all demographic variables. N = 247 English-speaking participants were recruited in response to an Amazon TurkPrime posting advertising a study for parents of children under 18 years of age (Litman et al., 2017). Participants were excluded for admitting to answering randomly and for failing attention checks (n = 47), yielding a final sample of N = 200. 94% of the sample were biological parents (n = 188) and 6% were adoptive parents (n = 12). 54% of the sample were mothers (n = 108). Parents were between the ages of 25–61 (Mage = 38.27). Parents with multiple children (mean number of children = 2.07) were asked to select one child to use as the reference for the survey (henceforth referred to as the target child). Target children were 52.5% female (n = 105) and were between the ages of 10 months to 17 years (Mage = 8.84). Parents were 74% white/Caucasian (n = 148), 13% Asian (n = 26), 4.5% Latino/a (n = 9), 4% African American (n = 8), 2.5% Native American (n = 5), 1.5% bi/multiracial (n = 3), and .5% of participants reported that they preferred not to state their race/ethnicity (n = 1). 85.5% of parents reported co-parenting with a spouse or partner (n = 171), 9.5% reported being single parents (n = 19), 3.5% reported co-parenting with a former partner (n = 7), 1% of respondents reported co-parenting with another adult (n = 2), and .5% reported another type of parenting arrangement (n = 1). 85.5% of parents reported being married (n = 171), 7% reported being single (n = 14), 5.5% reported being separated or divorced (n = 11), and 1.5% reported being in a non-marital partnership (n = 3). Parents had completed an average of 16.41 years of education (range 4–24 years). The majority of parents reported working full-time (59.5%; n = 119) and 18.5% reported being stay-at-home parents (n = 37).
Table 1.
Descriptive Statistics for all Demographic Variables
| Parent Demographic Variables | |||
| Age | |||
| Mean ± SD | 38.27 ± 7.32 | ||
| Min-Max | 25-61 | ||
| Median (IQR) | 11 | ||
| Sex | |||
| Male | 108 (54%) | ||
| Female | 92 (46%) | ||
| Missing | |||
| Race/Ethnicity | |||
| Non-Hispanic White/Caucasian | 148 (74%) | ||
| Asian | 26 (13%) | ||
| Hispanic/Latino | 9 (4.5%) | ||
| Black/African American | 8 (4%) | ||
| Native American | 5 (2.5%) | ||
| Other | 3 (.5%) | ||
| Prefer not to answer | 1 (.5%) | ||
| Years of education | |||
| Mean ± SD | 16.41 ± 2.91 | ||
| Min-Max | 4-24 | ||
| Median (IQR) | 4 | ||
| Parent’s relationship to target child | |||
| Biological | 188 (94%) | ||
| Adoptive | 12 (6%) | ||
| Parent marital status | |||
| Married | 171 (85.5%) | ||
| Single | 14 (7%) | ||
| Separated/divorced | 11 (5.5%) | ||
| Partnered | 1 (.5) | ||
| Widowed | 0 (0%) | ||
| Parenting arrangement | |||
| Co-parent with spouse/live-in partner | 171 (85.5%) | ||
| Single parent | 19 (9.5%) | ||
| Co-parent with former spouse/partner | 7 (3.5%) | ||
| Other | 3 (1.5%) | ||
| Co-parent with other adult | 2 (1%) | ||
| Other | 1 (.5%) | ||
| Parent employment status | |||
| Full-time | 119 (59.5%) | ||
| Stay at home parent | 37 (18.5%) | ||
| Part-time | 32 (16%) | ||
| Unemployed | 12 (6%) | ||
| Other | 6 (3%) | ||
| Student | 4 (2%) | ||
| Looking for a job | 4 (2%) | ||
| Retired | 1 (.5%) | ||
| On disability | --- | ||
| Child Demographic Variables | |||
| Target child age | |||
| Mean ± SD | 8.84 ± 4.78 | ||
| Min-Max | 10 months-17 years | ||
| Median (IQR) | 8 | ||
| Target child sex | |||
| Female | 105 (52.5%) | ||
| Male | 95 (47.5%) | ||
| Number of children in family | |||
| Mean ± SD | 2.07 ± 1.37 | ||
| Min-Max | 1-10 | ||
| Median (IQR) | 1 | ||
| Sex of children in family | |||
| Both female and male | 93 (46.5%) | ||
| Female only | 54 (27%) | ||
| Male only | 53 (26.5%) | ||
Employment percentages do not sum to 100 percent because more than one item could be selected. Percentages do not always sum to 100 due to rounding
TurkPrime Participant Selection Parameters
Recent methodological reviews have emphasized the importance of excluding low-reputation, inattentive workers from MTurk samples to maintain data quality (Hauser & Schwarz, 2016). Therefore, several TurkPrime features were used to ensure the highest possible data quality, including automatic verification of worker country location, automatic blocking of suspicious geocode locations and duplicate IP addresses, and automatic blocking of workers who had previously completed any pilot studies related to the present study. In addition, all workers were prescreened using the Prime Panels feature such that the study was only advertised to participants who were verified to be the parent of at least one child under age 19. In addition, only participants who had successfully completed at least 90% of past studies that they had signed up for (i.e., who had an approval rating over 90) were selected for the study.
A Priori Power Calculations
We used the software program G*Power to conduct a power analysis (Faul et al., 2009). Our goal was to obtain 80% power to detect a medium effect size of f = .25 at the standard .05 alpha error probability for linear multiple regression tests examining whether buffering and exacerbating factors moderate the effect of COVID-19-related stress on child symptomatology, which yielded a recommended sample size of N = 200 for the present study.
Procedure
All study procedures were executed via distribution of a Qualtrics survey on Amazon TurkPrime. Participants provided informed consent prior to completing a compiled survey consisting of measures assessing parental emotion socialization and child and parental symptomatology (presented in randomized order), followed by a separate survey of family-level exposure to pandemic-related stressors. Participants completed data quality and attention checks, and were thanked, debriefed, and compensated $8 at the end of the study. All consent and assessment procedures were approved by the institutional review board at Yale University.
Study Timing
Data were collected between April 24th and April 26th, 2020. Based on several metrics of evaluation of the severity of the pandemic including daily deaths, daily infections and testing, and overall hospital resource use, the current peak in COVID-19 in the United States (at time of publication) occurred between April 14th and April 19th 2020, suggesting that data for the current study were collected immediately following this peak (IHME | COVID-19 Projections, 2020). In addition, data aggregated from state governments, executive orders, and local news reports show that nearly 90% of Americans were quarantined during the study period (in 38 out of 50 states; Lee et al., 2020).
Materials
Demographics
Participants were asked to report on their sex and age, the target child’s age and sex, their relationship to the target child, the number of children in their family, the sex and age of each child in their family, their marital and parenting (e.g., single) status, and years of education. In addition, parents were asked to report their race and ethnicity, their annual household income and the number of individuals relying on this income, and the number of hours that they spent parenting during waking hours.
Child Symptomatology
Child Behavioral Checklist (CBCL 1.5–5; CBCL 6–18; Achenbach & Rescorla, 2001). The CBCL 1.5–5 and 6–18 are 99-item parent-report measures of children’s behavioral problems. Parents rated items describing children’s behavior on a 3-point Likert scale of 0 (Not true) to 2 (Very or often true). The internalizing and externalizing scales of the CBCL have demonstrated high internal consistency, with alphas ranging from .89 to .92 (Achenbach & Rescorla, 2001). The CBCL has also shown excellent stability over an 8-day period, and high external validity in the form of high correlations between CBCL scores and teacher reports of behavior problems as well as clinician assessment of child psychopathology (Gross et al., 2006). Because we were unable to monitor clinical risk in the context of an online survey, the following items assessing self-harm and suicidality were omitted from the study protocol: “18. Deliberately harms self or attempts suicide.” and “91. Talks about killing self.” The externalizing (24 items; Cronbach’s α = .91 for CBCL 1.5–5; 32 items; Cronbach’s α = .94 for CBCL 6–18) and internalizing problems (36 items, Cronbach’s α = .95 for CBCL 1.5–5; 31 items, Cronbach’s α = .93 for CBCL 6–18) scales were used in the present study for both age versions of the measure. Since two age versions of the measure were used (1.5–5 and 6–18), standardized raw scores for both internalizing and externalizing composites were used in order to compare across the two different versions.
COVID-19-Related Family Stressors and COVID-19 Exposure
Epidemic-Pandemic Impacts Inventory (EPII; Ford et al., 2020). The EPII is a recently developed measure designed to assess the impact of public health emergencies on multiple aspects of personal and family life, ranging from impacts on work and employment to emotional health and well-being. As the EPII was developed in response to the recent COVID-19 outbreak, psychometric information is not yet available. At the end of each list of questions specifically assessing each domain of personal or family life (e.g., work and employment), we added a single question assessing the degree of distress participants felt with regard to this specific domain (e.g., “In general, what is the level of distress you have experienced relating to employment and financial impacts due to the COVID-19 outbreak?”), which participants answered using a 7-point Likert scale ranging from 1 (Mildly distressing) to 7 (Highly distressing), which was modeled after a line of questions included in the COVID-19 and Perinatal Experiences (COPE) study (Thomason & Graham, 2020). A composite score representing family-level exposure to COVID-19-related stressors (henceforth referred to as “COVID-19-related family stress”) was calculated by summing the eight items assessing parental distress in response to the impact of COVID-19 on the following domains of family life: work and employment, education and training, home life, social activities, economic wellbeing, emotional health and wellbeing, physical health problems, and physical distancing and quarantine.
Parental Emotion Socialization and Response to Children’s Pandemic-Related Reactions
Emotion-Related Parenting Styles Self-Test-Likert (ERPSST-Likert; Lee et al., 2000). Based on Gottman’s meta-emotion philosophy (Gottman et al., 1997), the ERPSST-Likert is an 81-item parent-report measure designed to assess parents’ thoughts and feelings about their own, as well as their child’s, experience of anger and sadness. Parents rated the degree to which they agreed with statements about their children’s negative emotions (e.g., “When my child is sad, it’s a time to problem solve.”) on a 5-point Likert scale, from 1 (Always false) to 5 (Always true). The ERPSST yields four scores representing predominant emotions socialization styles: dismissive, disapproving, laissez-faire, and emotion coaching, and has been shown to have good construct validity (Lee et al., 2000). The emotion coaching (5 items; Cronbach’s α = .80) scale was used in the present study.
Parental Response to Trauma Questionnaire (PRTQ; Williamson et al., 2018). The PRTQ is a 50-item parent-report measure designed to assess parental reactions to children’s traumatic exposures and related symptomatology. The PRTQ systematically assesses parents’ thoughts about their child’s coping following child exposure to trauma (appraisal-related questions), as well as trauma-related alterations in parental behavior (support-related questions). Parents rated the degree to which they engaged in specific thought patterns (e.g., “My child might go to pieces if I don’t protect him/her from his/her fears.”) or behaviors (e.g., “I warn my child about possible dangers whenever I can.”) on a 4-point Likert scale from 0 (Don’t agree at all/Not at all) to 3 (Agree completely/A lot). The PRTQ has been shown to have good convergent validity and test–retest reliability (Williamson et al., 2018).
We modified a subset of PRTQ items to specifically query parents’ beliefs and responses to children’s pandemic-related stress exposure. Questionnaire instructions and items were modified, as necessary, to specifically reference COVID-19 (e.g., “My child will not be able to deal with being reminded of the pandemic.”). Two composite scores were created for use in the present study: 1) a composite score created by summing all items related to the degree to which parents reported talking with their child about their COVID-19-related reactions (e.g., “I talk about the frightening pandemic with my child just like I do with anything else.”; 5 items; Cronbach’s α = .83) and 2) a composite score created by summing all items related to the degree to which parents reported trying to maintain routines during COVID-19 (e.g., “I’ve tried not to change my child’s usual routine.”; 3 items; Cronbach’s α = .66).
Parent Symptomatology
Beck Anxiety Inventory (BAI; Beck & Steer, 1990). The BAI is a 21-item self-report measure of anxiety symptoms. Parents rated items describing symptoms of anxiety (e.g., “Unable to relax”) on a 4-point Likert scale from 0 (Not at all) to 3 (Severely—it bothered me a lot). The BAI has demonstrated high internal consistency, with alphas ranging from .92 to .94, high one-week test–retest reliability, and excellent convergent validity with other indices of psychopathology such as the State-Trait Anxiety Inventory (Beck & Steer, 1988; Fydrich et al., 1992). The total score (21 items; Cronbach’s α = .95) was used in the present study.
Parenting Stress
Parenting Stress Index (PSI-4 SF; Abidin, 2012). The PSI-4th Edition Short Form is a 36-item self-report measure of parental stress in the context of the parent–child relationship. Parents rated items (e.g., “I find myself giving up more of my life to meet my children’s needs than I ever expected.”) on a 5-point Likert scale from 1 (Strongly disagree) to 5 (Strongly agree). The PSI-4 has demonstrated high internal consistency, with alphas ranging from .71 to .96 across subscales and across specific populations (e.g., high-risk vs. low-risk samples) and excellent one to three-month test–retest validity (Barroso et al., 2016; Johnson, 2015; Reitman et al., 2002). The total score (36 items; Cronbach’s α = .96) was used in the present study.
Analytic Plan
Hierarchical multiple linear regression analyses, controlling for child age, were used to test the hypothesis that exposure to COVID-19-related stress would be associated with children’s internalizing and externalizing symptomatology. In addition, hierarchical multiple linear regression was used to test whether parental emotion coaching, parental availability for discussion of COVID-19 with child, parental maintenance of routines during pandemic, parenting stress, and parent anxiety-related symptomatology moderated this association. All models were run with age included as a covariate given age-related changes in parental buffering (Gee et al., 2014; Hostinar et al., 2015). In total, five regression models were run to test each of the interaction terms (created by multiplying each hypothesized moderator by family-level COVID-19-related stress) as predictors of child internalizing and externalizing symptomatology, respectively. Predictor and product terms were centered-standardized (Aiken et al., 1991). To better assess for R2, analyses were conducted as hierarchical multiple linear regression in which the covariate (child age) was entered into the first block, the centered predictor variables (family-level COVID-19-related stress, moderator of interest) were entered into the second block, and the centered moderator term (family-level COVID-19-related stress x moderator of interest) was entered into the third block. Standardized beta coefficients were used as an estimate of effect size. In addition, given the variability in parental years of education in the present sample, all analyses were re-run with parental years of education included as a covariate, in addition to child age; results presented below did not change with this inclusion.
Results
Association Between COVID-19-Related Family Stress and Child Symptomatology
As hypothesized, controlling for child age, there was a significant positive association between COVID-19-related family stress and child internalizing problems (B = .35, t(198) = 5.70, p < .001) and externalizing problems (B = .33, t(198) = 5.89, p < .001). There was no significant interaction between COVID-19-related family stress and child age associated with either children’s internalizing problems (B = −.02, t(198) = − 1.65, ns) nor externalizing problems (B = −.01, t(198) = − .70, ns). In addition, there was no significant interaction between COVID-19 related family stress and child sex associated with either children’s internalizing problems (B = 07, t(198) = .50, ns) nor externalizing problems (B = .02, t(198) = .16, ns).
Buffering Factors
Related to family-level factors that were hypothesized to buffer the effect of COVID-19-related family stress on children’s symptomatology, consistent with hypotheses, controlling for child age, the interaction between parental emotion coaching and COVID-19-related family stress was significantly associated with both children’s internalizing problems (B = −.06, t(198) = −3.77, p < .001) and externalizing problems (B = −.03, t(198) = −2.05, p = .041). The interaction between parental maintenance of home routines during the COVID-19 pandemic and COVID-19-related family stress was significantly associated with children’s internalizing problems (B = −.05, t(198) = −2.04, p = .043), but not with children’s externalizing problems (B = −.01, t(198) = −.295, ns). Contrary to hypotheses, controlling for child age, the interaction between parental discussion of children’s COVID-19-related reactions and COVID-19-related family stress was not significantly associated with either children’s internalizing problems (B = −.01, t(198) = −.60, ns) nor externalizing problems (B = .01, t(198) = −.70, ns).
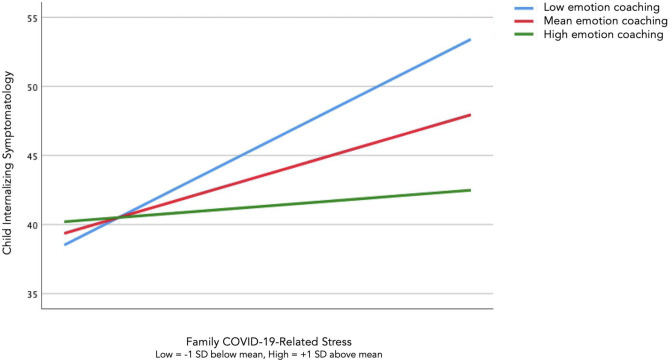
Simple slopes analyses were used to probe all significant interaction effects (Aiken et al., 1991; Dawson, 2014). Among parents who reported engaging in high levels of emotion coaching, there was no significant association between COVID-19-related family stress and either child internalizing (t = 1.04; ns) and externalizing problems (t = 1.20; ns). In contrast, among parents who reported engaging in low levels of emotion coaching with regard to their children’s negative emotions, higher levels of COVID-19-related family stress were significantly associated with higher child internalizing (t = 6.67; p < .001; Fig. 1) and externalizing problems (t = 4.65, p < .001). Though interpretation is limited due to the cross-sectional nature of the study, this pattern of results suggests that parents who report engaging in higher levels of emotion coaching of children’s negative emotions may more effectively buffer the relation between COVID-19-related family stress and children’s symptomatology.
Fig. 1.
Parental emotion coaching moderates association between pandemic-related stress and child internalizing symptomatology
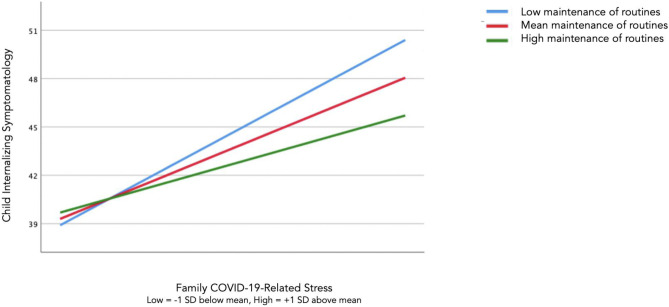
Although there was a significant association between COVID-19-related family stress and child internalizing problems among children of parents who reported both low and high levels of maintenance of the child’s home routine during the COVID-19 pandemic, the slope of the association between COVID-19 family-related stress and child internalizing problems was less steep for parents who reported a higher degree of routine maintenance (t = 2.62, p = .01) relative to parents who reported a lower degree of routine maintenance (t = 4.63, p < .001; Fig. 2), suggesting that parental commitment to maintenance of home routines during times stress may buffer the effect of stress on child symptomatology.
Fig. 2.
Parental maintenance of family routines moderates association between pandemic-related stress and child internalizing symptomatology
Exacerbating Factors
Consistent with hypotheses related to family-level factors that may exacerbate the association between COVID-19-related family stress and children’s symptomatology, controlling for child age, the interaction between parenting stress and COVID-19-related family stress was significantly associated with both children’s internalizing problems (B = 01, t(186) = 3.39, p =.001) and externalizing problems (B = .01, t(186) = 4.18, p < .001). The interaction between parental anxiety-related symptomatology and COVID-19-related family stress was also significantly associated with both children’s internalizing problems (B = .01, t(186) = 2.29, p = .023) and externalizing problems (B = .02, t(186) = 3.93 p < .001).
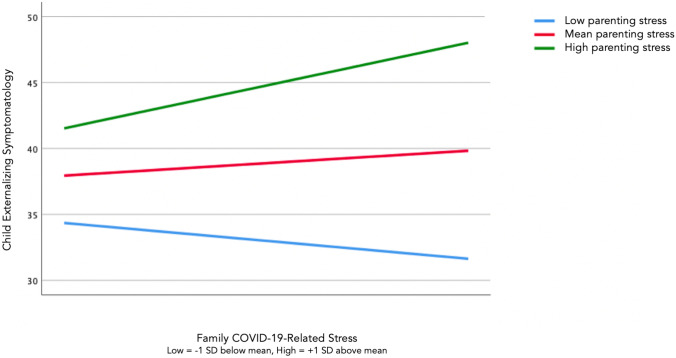
Simple slopes analyses revealed that, among parents who reported high levels of parenting stress, higher levels of COVID-19-related family stress were significantly associated with higher child internalizing (t = 3.55 p < .001) and externalizing problems (t = 2.63, p = .01; Fig. 3). In contrast, there was no significant association between COVID-19-related family stress and either child internalizing (t = −1.73; ns) and externalizing problems (t = −1.50; ns) for parents who reported relatively lower levels of parenting stress. This pattern of results suggests that, in line with hypotheses, higher levels of parenting stress may exacerbate the effect of COVID-19-related family stress on child’s symptomatology.
Fig. 3.
Parenting stress moderates association between pandemic-related stress and child externalizing symptomatology
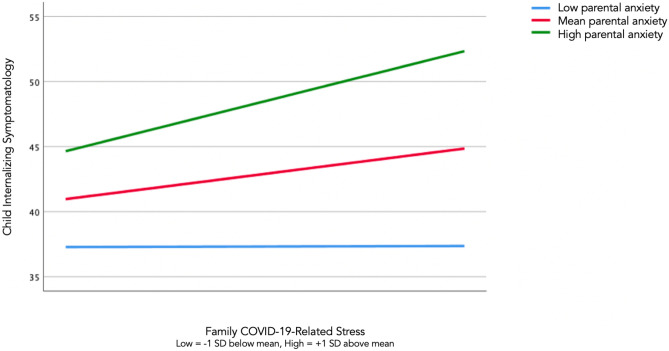
Finally, among parents who reported high levels of anxiety, higher levels of COVID-19-related family stress were significantly associated with higher child internalizing (t = 3.12; p = .002; Fig. 4) and externalizing problems (t = 2.47, p = .014). In contrast, there was no significant association between COVID-19-related family stress and either child internalizing (t = .04; ns) or externalizing problems (t = −.26; ns) for parents who reported relatively low levels of anxiety-related symptomatology. This pattern of results suggests that, as hypothesized, higher levels of parental anxiety-related symptomatology may exacerbate the effect of family-level stress on children’s symptomatology.
Fig. 4.
Parent anxiety-related symptomatology moderates association between pandemic-related stress and child internalizing symptomatology
Discussion
The present study examines possible associations between COVID-19-related stressors and children’s mental health. Though interpretation of the findings is limited given sole reliance on parental report and the cross-sectional nature of data collection due to the constraints of collecting data during a global pandemic, results provide preliminary evidence for a potential association between children’s exposure to a wide range of COVID-19-related stressors and heightened internalizing and externalizing symptomatology. Though several studies to date have highlighted the psychiatric impacts of COVID-19 on youth mental health in Chinese samples (e.g., Xie et al., 2020), and recent reviews have forecast deleterious impacts of the United States COVID-19 outbreak on child and adolescent mental health (e.g., Gruber et al., 2020; Guessoum et al., 2020), at time of submission, the present study represents the first documented evidence of associations between exposure to COVID-19-related stress and youth symptomatology. Further, we present evidence that specific parent-level factors may buffer or exacerbate the effect of pandemic-related stressors on children’s symptomatology. Specifically, parents who reported engaging in relatively higher levels of emotion coaching of children’s negative emotions and who reported that they were able to more stably maintain children’s home routines during the pandemic were more likely to effectively buffer the effects of pandemic-related stress on children’s symptomatology. Higher levels of parent-reported parenting stress and anxiety-related symptomatology was associated with less parental buffering of children from pandemic-related stressors.
Findings contribute to our understanding of the role of parents in supporting children during and following stress exposure (Williamson et al., 2018). Of note, previous studies examining parental buffering of stress have frequently examined this mechanism following child exposure to acute stressors such as terrorist attacks (e.g., Carpenter et al., 2017; Wilson et al., 2010); the present study expands upon this literature by demonstrating that specific parental behaviors moderate the effects of exposure to downstream effects of exposure to a more chronic stressor (e.g., economic effects of a global pandemic). Evidence for parental buffering and exacerbation of children’s exposure to the financial, educational, and health-related stressors associated with living through the COVID-19 pandemic underscores the importance of considering parent-level factors and parents’ potential to effectively buffer or exacerbate children’s stress when estimating the population-wide effect of exposure to stressors on children’s mental health.
Previous studies in the parental buffering literature have also focused on parental buffering or exacerbation of the effects of stress exposure on children’s development of posttraumatic stress disorder, specifically (Berkowitz et al., 2010). Here, we provide evidence for potential effective parental buffering of the impact of stress on internalizing and externalizing problems. Clinical interventions targeting children’s adverse mental health outcomes following exposure to pandemic-related stressors should also aim to target parental mental health and parenting by engaging parents in treatment (Haine-Schlagel & Walsh, 2015). Public health efforts aiming to reduce the mental health impacts of stressful events such as the pandemic should also consider the importance of targeting parental wellbeing, thereby promoting parents’ capacity to buffer children as a preventative strategy. Of note, several widely distributed guides on managing youth reactions to COVID-19 have included recommendations for parents to increase communication with children about the pandemic (Dalton et al., 2020; Jiao et al., 2020) and to continue to maintain children’s typical home routines (World Health Organization, 2020). Results of the present study represent an initial evidentiary test of these public health recommendations and form the basis for necessary subsequent research efforts investigating optimal parental and societal responses to children’s exposure to the stressors inherent in living through a global pandemic.
Several limitations of the current work—in part due to the nature of data collection during a global pandemic—should be considered when interpreting findings. The present study relied exclusively on parental report and therefore it is possible that parents’ generalized perspective on family-level factors during the COVID-19 pandemic influenced reporting on both outcome and moderator variables. For example, it is possible that parents’ generalized positive outlook led to reports of both more desirable parenting qualities (i.e., high levels of optimal emotion socialization, availability for discussion of COVID-19-related topics with children), lower levels of parental stress and anxiety-related symptomatology, and lower levels of child symptomatology. In part due to documented evidence of low concordance between parents and children on children’s symptom inventories (e.g., De Los Reyes et al., 2011), sole reliance on parent-report—particularly for variables related to parenting style and child symptomatology—indicates that findings of the present study should be interpreted with caution. However, given the limitations of data collection during the height of the pandemic, we believe that these findings make an important initial contribution to a broader body of knowledge about the effects of family-level COVID-19-related stress on children’s mental health and parent-level variables that may buffer or exacerbate these effects.
Despite all efforts to ensure high-quality data collection (i.e., use of attention checks, inclusion of workers with high approval ratings), all data collection was conducted via an online convenience sample due to the quarantine and social distancing requirements inherent to collecting data about the COVID-19 pandemic. Future research that obtains children’s report of their own symptomatology and parental behaviors will be important to build upon these findings. It would have been ideal to be able to capture youth reports of all variables in the study and, further, to employ novel technologies such as ecological momentary assessment to facilitate real-time recording of the degree to which youth were affected by COVID-19-related stressors (as well as the degree to which parents engaged in behaviors likely to buffer or exacerbate the impact of stress exposure on youth mental health). However, our desire to mobilize quickly in order to assess the mental health impacts of the unfolding global pandemic in early April 2020 (and our inability to utilize typical laboratory-based assessment tools) prevented our use of these more comprehensive methodological approaches. Further, there is increasing clarity regarding the disproportionate effects of the COVID-19 pandemic on access to technological resources (Beaunoyer et al., 2020), and, in turn, the disproportionate representation of those most affected by “digital inequality” in online and phone-based study protocols (Roubinov et al., 2020), particularly among youth. Although employing more sophisticated technology to facilitate a mixed methods, multi-informant study would have enhanced the methodological rigor of the present study, we may have been additionally limited in our ability to capture a diverse sample of families affected by COVID-19 as a result.
The majority of respondents in the present study were married and reported co-parenting with a spouse or partner, suggesting that findings may not generalize to parents who are under additional stress due to increased responsibilities inherent in single-parenting or parenting in a shared custody arrangement, especially during a global pandemic when childcare resources are not widely available for many families. In addition, the majority of participants were non-Hispanic white/Caucasian; future studies should aim to recruit more diverse samples of parents, in light of growing evidence that racial and ethnic minorities have been disproportionately affected by COVID-19, as well as by the pernicious social and economic sequalae of the pandemic (Hooper et al., 2020; Shippee et al., 2020; Tai et al., 2020). Further, in line with current methodological recommendations for maximizing access to research during and following the COVID-19 pandemic (see Roubinov et al., 2020 for a review), future studies should aim to employ both online and mail-based data collection to reach families without reliable access to internet. In addition, it should be noted that the internal consistency for items in the “maintenance of routines” subscale was poor given that this subscale was created by the study authors by summing three relevant modified items from this measure (this composite score diverges from the intended subscale creation for the PRTQ). Finally, it should be noted that the examination of child age and sex as potential moderators of the association between COVID-19-related family stress and child symptomatology was not documented in our pre-registered analytical plan but was included in the manuscript in response to a recommendation that arose during the peer-review process.
In conclusion, though preliminary, this study contributes to a growing literature underscoring the need for increased attention to the effects of COVID-19-related economic, health, educational stressors on children’s mental health, and highlights the importance of considering family-level factors that may promote resilience in the face of a national crisis.
Author contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Emily Cohodes, Sarah McCauley, and Dylan Gee. Analysis was performed by Emily Cohodes, with input from Dylan Gee. Emily Cohodes created all tables and figures for the manuscript. The first draft of the manuscript was written by Emily Cohodes, and all authors made substantive contributions to manuscript revisions. All authors read and approved the final manuscript and assisted with revisions.
Funding
This work was supported by the National Institutes of Health (NIH) Director’s Early Independence Award (DP5OD021370) to D.G.G., Brain & Behavior Research Foundation (National Alliance for Research on Schizophrenia and Depression; NARSAD) Young Investigator Award to D.G.G., Jacobs Foundation Early Career Research Fellowship to D.G.G., The Society for Clinical Child and Adolescent Psychology (Division 53 of the American Psychological Association) Richard "Dick" Abidin Early Career Award and Grant to D.G.G., National Science Foundation Graduate Research Fellowship Program Award to E.M.C (NSF DGE‐1752134), The Society for Clinical Child and Adolescent Psychology (Division 53 of the American Psychological Association) Donald Routh Dissertation Grant to E.M.C., a Dissertation Funding Award from the Society for Research in Child Development to E.M.C., the Elizabeth Munsterberg Koppitz Child Psychology Graduate Fellowship from the American Psychological Foundation to E.M.C., and a Dissertation Research Award from the American Psychological Association to E.M.C.
Availability of data and material
All study code is available by request from the corresponding author.
Code availability
All study data is available by request from the corresponding author.
Compliance with ethical standards
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Review Board at Yale University.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abidin, R.R. (2012). Parenting Stress Index. 4th edn (PSI-4). Lutz, FL: Psychological Assessment Resources Inc.
- Achenbach TM, Rescorla L. Manual for the ASEBA school-age forms & profiles: An integrated system of multi-informant assessment. VT: Aseba Burlington; 2001. [Google Scholar]
- Aiken, L.S., West, S.G., Reno, R.R. (1991). Multiple regression: Testing and interpreting interactions. Sage.
- Barroso NE, Hungerford GM, Garcia D, Graziano PA, Bagner DM. Psychometric properties of the Parenting Stress Index-Short Form (PSI-SF) in a high-risk sample of mothers and their infants. Psychological Assessment. 2016;28(10):1331–1335. doi: 10.1037/pas0000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaunoyer E, Dupéré S, Guitton MJ. COVID-19 and digital inequalities: Reciprocal impacts and mitigation strategies. Computers in Human Behavior. 2020;111:106424. doi: 10.1016/j.chb.2020.106424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, A.T., & Steer, R.A. (1988). Beck anxiety inventory (BAI). Überblick Über Reliabilitäts-Und Validitätsbefunde von Klinischen Und Außerklinischen Selbst-Und Fremdbeurteilungsverfahren, 7.
- Beck, A. T., & Steer, R. A. (1990). Manual for the Beck anxiety inventory. San Antonio, TX: Psychological Corporation.
- Berkowitz S, Stover CS, Marans SR. The Child and Family Traumatic Stress Intervention: Secondary prevention for youth at risk of developing PTSD. The Journal of Child Psychology and Psychiatry. 2010;52(6):676–685. doi: 10.1111/j.1469-7610.2010.02321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyce, W.T., & WT,B. (1981). Interaction between social variables in stress research. [PubMed]
- Brooks, S.K., Webster, R.K., Smith, L.E., Woodland,L., Wessely,S., Greenberg, N., Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. [DOI] [PMC free article] [PubMed]
- Carpenter AL, Elkins RM, Kerns C, Chou T, Greif Green J, Comer JS. Event-related household discussions following the Boston Marathon Bombing and associated posttraumatic stress among area youth. Journal of Clinical Child and Adolescent Psychology. 2017;46(3):331–342. doi: 10.1080/15374416.2015.1063432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohodes E, Chen S, Lieberman A. Maternal meta-emotion philosophy moderates effect of maternal symptomatology on preschoolers exposed to domestic violence. Journal of Child and Family Studies. 2017;26(7):1831–1843. doi: 10.1007/s10826-017-0699-3. [DOI] [Google Scholar]
- Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin. 2001;127(1):87–127. doi: 10.1037/0033-2909.127.1.87. [DOI] [PubMed] [Google Scholar]
- Dalton L, Rapa E, Stein A. Protecting the psychological health of children through effective communication about COVID-19. The Lancet Child & Adolescent Health. 2020;4(5):346–347. doi: 10.1016/S2352-4642(20)30097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson JF. Moderation in management research: What, why, when, and how. Journal of Business and Psychology. 2014;29(1):1–19. doi: 10.1007/s10869-013-9308-7. [DOI] [Google Scholar]
- De Los Reyes, A. (2011). Introduction to the special section: More than measurement error: Discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. Journal of Clinical Child & Adolescent Psychology, 40(1), 1-9. [DOI] [PubMed]
- Eisenberg N, Cumberland A, Spinrad TL. Parental socialization of emotion. Psychological Inquiry. 1998;9(4):241–273. doi: 10.1207/s15327965pli0904_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul, F., Erdfelder, E., Buchner, A., Lang, A.-G. (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41(4), 1149–1160. 10.3758/BRM.41.4.1149 [DOI] [PubMed]
- Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health. 2020;14(1):20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fivush R, Hazzard A, McDermott Sales J, Sarfati D, Brown T. Creating coherence out of chaos? Children’s narratives of emotionally positive and negative events. Applied Cognitive Psychology. 2003;17(1):1–19. doi: 10.1002/acp.854. [DOI] [Google Scholar]
- Ford, J.D., Carter, A.S., Grasso, D.J., Briggs-Gowan, M.J. (2020). Epidemic – Pandemic Impacts Inventory. 3. [DOI] [PMC free article] [PubMed]
- Foy, D.W. (1992). Treating PTSD: Cognitive-behavioral Strategies. Guilford Press.
- Fydrich T, Dowdall D, Chambless DL. Reliability and validity of the Beck Anxiety Inventory. Journal of Anxiety Disorders. 1992;6(1):55–61. doi: 10.1016/0887-6185(92)90026-4. [DOI] [Google Scholar]
- Gee DG, Gabard-Durnam L, Telzer EH, Humphreys KL, Goff B, Shapiro M, Flannery J, Lumian DS, Fareri DS, Caldera C, Tottenham N. Maternal buffering of human amygdala-prefrontal circuitry during childhood but not during adolescence. Psychological Science. 2014;25(11):2067–2078. doi: 10.1177/0956797614550878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein E, Wen H, Miller BF. Coronavirus Disease 2019 (COVID-19) and Mental Health for Children and Adolescents. JAMA Pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Goodman LA, Rosenberg SD, Mueser KT, Drake RE. Physical and sexual assault history in women with serious mental illness: Prevalence, correlates, treatment, and future research directions. Schizophrenia Bulletin. 1997;23(4):685–696. doi: 10.1093/schbul/23.4.685. [DOI] [PubMed] [Google Scholar]
- Gottman, J.M., Katz, L.F., Hooven, C. (1997). Introduction to the concept of meta-emotion. Meta-Emotion. How Families Communicate Emotionally, 3–8.
- Gottman JM, Katz LF, Hooven C. Parental meta-emotion philosophy and the emotional life of families: Theoretical models and preliminary data. Journal of Family Psychology. 1996;10(3):243. doi: 10.1037/0893-3200.10.3.243. [DOI] [Google Scholar]
- Greeff AP, Wentworth A. Resilience in families that have experienced heart-related trauma. Current Psychology. 2009;28(4):302. doi: 10.1007/s12144-009-9062-1. [DOI] [Google Scholar]
- Greene CA, McCarthy KJ, Estabrook R, Wakschlag LS, Briggs-Gowan MJ, et al. Responsive parenting buffers the impact of maternal PTSD on young children. Parenting. 2020;20(2):141–165. doi: 10.1080/15295192.2019.1707623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross D, Fogg L, Young M, Ridge A, Cowell JM, Richardson R, Sivan A, et al. The equivalence of the Child Behavior Checklist/1 1/2-5 across parent race/ethnicity, income level, and language. Psychological Assessment. 2006;18(3):313. doi: 10.1037/1040-3590.18.3.313. [DOI] [PubMed] [Google Scholar]
- Gruber J, Prinstein MJ, Clark LA, Rottenberg J, Abramowitz JS, Albano AM, Aldao A, Borelli JL, Chung T, Davila J, Forbes EE, Gee DG, Hall GCN, Hallion LS, Hinshaw SP, Hofmann SG, Hollon SD, Joormann J, Kazdin AE, Weinstock LM. Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. American Psychologist. 2020 doi: 10.1037/amp0000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guessoum SB, Lachal J, Radjack R, Carretier E, Minassian S, Benoit L, Moro MR, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Research. 2020;291:113264. doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnar MR, Donzella B. Social regulation of the cortisol levels in early human development. Psychoneuroendocrinology. 2002;27(1–2):199–220. doi: 10.1016/S0306-4530(01)00045-2. [DOI] [PubMed] [Google Scholar]
- Haine-Schlagel R, Walsh NE. A review of parent participation engagement in child and family mental health treatment. Clinical Child and Family Psychology Review. 2015;18(2):133–150. doi: 10.1007/s10567-015-0182-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser DJ, Schwarz N. Attentive Turkers: MTurk participants perform better on online attention checks than do subject pool participants. Behavior Research Methods. 2016;48(1):400–407. doi: 10.3758/s13428-015-0578-z. [DOI] [PubMed] [Google Scholar]
- Hofer, M. A. (1978). Hidden regulatory processes in early social relationships. In Social Behavior (pp. 135–166). Springer.
- Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver R, Everall I, Ford T, John A, Kabir T, King K, Madan I, Michie S, Przybylski AK, Shafran R, Sweeney A, Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper MW, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020 doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar CE, Johnson AE, Gunnar MR. Parent support is less effective in buffering cortisol stress reactivity for adolescents compared to children. Developmental Science. 2015;18(2):281–297. doi: 10.1111/desc.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IHME | COVID-19 Projections. (2020). Institute for Health Metrics and Evaluation. https://covid19.healthdata.org/
- Jiao WY, Wang LN, Liu J, Fang SF, Jiao FY, Pettoello-Mantovani M, Somekh E. Behavioral and emotional disorders in children during the COVID-19 epidemic. The Journal of Pediatrics. 2020;221:264–266.e1. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson AO. Test review: Parenting stress index, (PSI-4) Los Angeles, CA: SAGE Publications Sage CA; 2015. [Google Scholar]
- Kerns, K.A., & Brumariu, L.E. (2017). Attachment in middle childhood. In Handbook of Attachment: Theory, Research, and Clinical Applications (p. 18).
- Kilmer RP, Gil-Rivas V. Exploring posttraumatic growth in children impacted by Hurricane Katrina: Correlates of the phenomenon and developmental considerations. Child Development. 2010;81(4):1211–1227. doi: 10.1111/j.1467-8624.2010.01463.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CH, Hakim-Larson J, Voelker S. The Parenting Styles Self-Test: Psychometric properties. Ottawa, Ontario: Poster Presented at the Annual Meeting of the Canadian Psychological Association; 2000. [Google Scholar]
- Lee, J.C., Mervosh, S., Avila, Y., Harvey, B., & Matthews, A.L. (2020, June 18). See How All 50 States Are Reopening (and Closing Again). The New York Times. https://www.nytimes.com/interactive/2020/us/states-reopen-map-coronavirus.html
- Liang L, Ren H, Cao R, Hu Y, Qin Z, Li C, Mei S. The Effect of COVID-19 on Youth Mental Health. Psychiatric Quarterly. 2020;91(3):841–852. doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litman, L., Robinson, J., & Abberbock, T. (2017). TurkPrime. com: A versatile crowdsourcing data acquisition platform for the behavioral sciences. Behavior Research Methods, 49(2), 433–442. [DOI] [PMC free article] [PubMed]
- Liu CH, Doan SN. Psychosocial stress contagion in children and families during the COVID-19 pandemic. Clinical Pediatrics. 2020 doi: 10.1177/0009922820927044. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth, K., Lyubchik, A., Wolfe, R., Bronfman, E. (2002). Parental depression and child attachment: Hostile and helpless profiles of parent and child behavior among families at risk. In Children of depressed parents: Mechanisms of risk and implications for treatment (pp. 89–120). American Psychological Association. 10.1037/10449-004
- Masonbrink, A.R., & Hurley, E. (2020). Advocating for Children During the COVID-19 School Closures. Pediatrics, 146(3). 10.1542/peds.2020-1440 [DOI] [PubMed]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Archives of General Psychiatry. 2012;69(11):1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B, North CS. Mental health and the COVID-19 pandemic. The New England Journal of Medicine. 2020 doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Ponnet, K., Wouters, E., Goedemé, T., & Mortelmans, D. (2012). An exploration of family-based pathways through which parents’ financial stress is associated with problem behaviour of adolescents. In Working Papers (No. 1212; Working Papers). Herman Deleeck Centre for Social Policy, University of Antwerp. https://ideas.repec.org/p/hdl/wpaper/1212.html
- Racine N, Cooke JE, Eirich R, Korczak DJ, McArthur B, Madigan S. Child and adolescent mental illness during COVID-19: A rapid review. Psychiatry Research. 2020;292:113307. doi: 10.1016/j.psychres.2020.113307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radke-Yarrow M, Nottelmann E, Belmont B, Welsh JD. Affective interactions of depressed and nondepressed mothers and their children. Journal of Abnormal Child Psychology. 1993;21(6):683–695. doi: 10.1007/BF00916450. [DOI] [PubMed] [Google Scholar]
- Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitman D, Currier RO, Stickle TR. A critical evaluation of the Parenting Stress Index-Short Form (PSI-SF) in a Head Start population. Journal of Clinical Child & Adolescent Psychology. 2002;31(3):384–392. doi: 10.1207/S15374424JCCP3103_10. [DOI] [PubMed] [Google Scholar]
- Roubinov D, Bush NR, Boyce WT. How a Pandemic Could Advance the Science of Early Adversity. JAMA Pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.2354. [DOI] [PubMed] [Google Scholar]
- Shippee TP, Akosionu O, Ng W, Woodhouse M, Duan Y, Thao MS, Bowblis JR. COVID-19 Pandemic: Exacerbating Racial/Ethnic Disparities in Long-Term Services and Supports. Journal of Aging & Social Policy. 2020;32(4–5):323–333. doi: 10.1080/08959420.2020.1772004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stallard P, Velleman R, Baldwin S. Recovery from post-traumatic stress disorder in children following road traffic accidents: The role of talking and feeling understood. Journal of Community & Applied Social Psychology. 2001;11(1):37–41. doi: 10.1002/casp.610. [DOI] [Google Scholar]
- Tai DBG, Shah A, Doubeni CA, Sia IG, Wieland ML. The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States. Clinical Infectious Diseases. 2020 doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomason, M. E., Graham, A., & Vantieghem, M. R. (2020). COPE: Coronavirus Perinatal Experiences - Impact Survey (COPE-IS). Retrieved from https://osf.io/uqhcv/
- Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Williamson V, Creswell C, Fearon P, Hiller RM, Walker J, Halligan SL. The role of parenting behaviors in childhood post-traumatic stress disorder: A meta-analytic review. Clinical Psychology Review. 2017;53:1–13. doi: 10.1016/j.cpr.2017.01.005. [DOI] [PubMed] [Google Scholar]
- Williamson V, Hiller RM, Meiser-Stedman R, Creswell C, Dalgleish T, Fearon P, Goodall B, McKinnon A, Smith P, Wright I. The parent trauma response questionnaire (PTRQ): Development and preliminary validation. European Journal of Psychotraumatology. 2018;9(1):1478583. doi: 10.1080/20008198.2018.1478583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Mental health and psychosocial considerations during the COVID-19 outbreak. https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf?sfvrsn=6d3578af_2
- Wilson AC, Lengua LJ, Meltzoff AN, Smith KA. Parenting and Temperament Prior to September 11, 2001, and Parenting Specific to 9/11 as Predictors of Children’s Posttraumatic Stress Symptoms Following 9/11. Journal of Clinical Child & Adolescent Psychology. 2010;39(4):445–459. doi: 10.1080/15374416.2010.486317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province. China: JAMA Pediatrics; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All study code is available by request from the corresponding author.
All study data is available by request from the corresponding author.