Abstract
Introduction
Reducing cigarette use is a major public health goal in the United States. Questions remain, however, about the potential for the social environment in the adult years—particularly in the 30s and beyond—to influence cigarette use. This study tested pathways hypothesized by the social development model to understand the extent to which social environmental factors at age 33 (eg, involvement with smokers or with physically active people) contribute to changes in cigarette use from age 30 to age 39. Both combustible and electronic cigarette use were investigated.
Methods
Data were from the Seattle Social Development Project, a longitudinal study of 808 diverse participants with high retention. Self-reports assessed social developmental constructs, combustible and electronic cigarette use, and demographic measures across survey waves.
Results
At age 30, 32% of the sample reported past-month cigarette use. Using structural equation modeling, results showed high stability in cigarette use from age 30 to 39. After accounting for this stability, cigarette-using social environments at age 33 predicted personal beliefs or norms about smoking (eg, acceptability and social costs), which in turn predicted combustible cigarette use at age 39. Cigarette-using environments, however, directly predicted electronic cigarette use at age 39, with no significant role for beliefs about smoking.
Conclusions
Cigarette use was highly stable across the 30s, but social environmental factors provided significant partial mediation of this stability. Pathways were different for combustible and electronic cigarette use, however, with personal smoking norms playing an important role for the former but not the latter.
Implications
This study addresses the need for longitudinal investigation of social mechanisms and cigarette use in the 30s. Findings reinforce efforts to prevent the uptake of cigarettes prior to the 30s because, once started, smoking is highly stable. But social environmental factors remain viable intervention targets in the 30s to disrupt this stability. Addressing personal norms about smoking’s acceptability and social costs is likely a promising approach for combustible cigarette use. Electronic cigarettes, however, present a new challenge in that many perceived social costs of cigarette use do not readily translate to this relatively recent technology.
Introduction
Cigarette use remains the leading cause of preventable disease, disability, and death in the United States. Although rates of smoking have decreased, 14% of adults (34 million) in the United States smoked cigarettes in 2017.1,2 Nicotine is known to be among the most addictive substances and it is estimated that only 6% of smokers who attempt to quit each year are successful.3,4 Better understanding of social factors that can contribute to reductions in adult cigarette use is of ongoing importance to public health campaigns and intervention development.2 The 30s may be an important but underexamined age period for intervention because smokers who quit successfully typically do so in the 30s,5 whereas quitting after the 30s and early 40s is relatively rare.6,7 The 30s is also often a transitional time that includes longer term considerations of one’s own health and functioning (eg, consequences of health risks, career development, and parenting)8–10 that may bolster efforts to change.
The social environment has been shown to play an important role in the etiology of substance use, including cigarette use, in adolescence and young adulthood.11,12 Major social risk factors for tobacco initiation include family members or peers who smoke, neighborhood exposure to and availability of tobacco products, lower socioeconomic status of family or neighborhood, and personal educational attainment.11,13 Studies have also found that gender, ethnicity, social skills, and perceived norms or beliefs about the acceptability of and harm from smoking can be significant risk or protective factors for youth and early adult tobacco use.11,14,15
Less research has examined social environmental factors later into adulthood and their possible effects on cigarette use. Exceptions include some recent studies of smoking cessation among participants age 30 and older indicating that reduced cigarette use was related to having a nonsmoking and supportive partner; fewer friends who smoke; and family, peer, and community norms that support nonsmoking.16–18 Legislation banning smoking in public places has also been associated with a downward trend in smoking behavior overall.19 There remains a need, however, for a more systematic, theory-guided approach that incorporates multiple risk and protective factors into a single model and identifies specific social mechanisms and pathways associated with smoking. More longitudinal studies that reach into adulthood are especially needed to examine the lagged relationships between social mechanisms and smoking.20,21 The advantage of this approach, compared with more exploratory or cross-sectional studies with younger cohorts, is that it can help to identify how predictive factors are interrelated and potentially guide interventions to improve effectiveness and efficiency in reducing cigarette use in the 30s and beyond.
New questions are also raised by the advent of electronic cigarettes (e-cigs), which first became commercially available in the United States in 2007. E-cigs are typically battery-powered devices that deliver nicotine by heating a nicotine-containing liquid which is then inhaled as an aerosol. Although e-cigs contain potentially toxic substances including fine particulate matter and metals, current research suggests that major brands (not containing vitamin-E acetate) are less harmful than conventional or combustible cigarettes (c-cigs).22,23 Many adult smokers believe that e-cigs can help them reduce or quit c-cig use and use them for this purpose—although there is debate about the effectiveness of this strategy.23–25 In 2016, 3% of the total adult U.S. population and 11% of current c-cig smokers reported using e-cigs every day or some days. Among e-cig users, 29% reported being a former smoker, suggesting that e-cigs had replaced their prior combustible cigarette use. Two thirds (66%) of adult e-cig users, however, reported using both e-cigs and c-cigs, and only 4% were not regular c-cig users before using e-cigarettes (adapted from Bao et al.26). Since 2016, data show a slight dip and rebound in overall adult e-cig use prevalence (at 3.2%, 2.8%, and 3.2% across years from 2016 to 2018).27 Given their association and overlap, it is important to consider the role of social environmental factors for e-cig use as well as c-cig use. We are aware of no research focusing on social environmental factors that predict e-cig use in the 30s or compare that use with c-cig use. The current investigation addresses these research needs.
The Social Development Model in the 30s
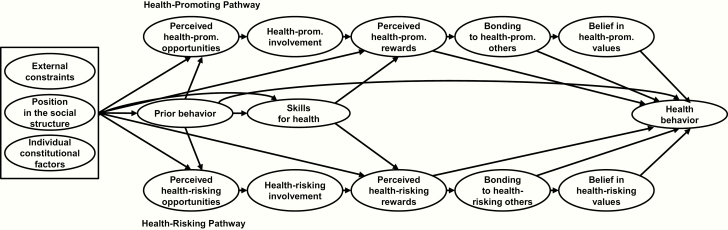
The social development model (SDM)28,29 is used in the present study to investigate the role of social environmental factors in the mid-30s for cigarette use from age 30 to 39. As shown in Figure 1, the SDM posits that an individual develops health-related behaviors through a process that begins with opportunities for interaction with others (both health-promoting and health-risking) in the various social environments in which he or she is embedded (eg, family, peers, school, and workplace). Through involvement in interactions with others, and skills relevant to the interactions and behaviors, an individual is rewarded by approval and success, leading to a social bond of attachment and commitment to the person or group with whom one is involved. Bonding, in turn, motivates an individual to adopt the beliefs and values of the respective social environments. The extent to which this process leads to health-promoting behavior (eg, physically active; upper pathway in Figure 1) or health-risking behavior (eg, smoking; lower pathway) depends on the predominant values and behaviors of the social environments and the degree to which an individual is involved, rewarded, and bonded in that environment.
Figure 1.
The social development model for health behavior. Prom. = promoting.
To illustrate with respect to cigarette use, an individual’s risk for smoking would be predicted in part by the extent to which friends and other peers smoke (opportunities), how often the individual is involved with smoking peers, the rewards and reinforcements received from smoking peers, the strength of bonds with these peers, and the extent to which the individual adopts similar norms and beliefs about smoking as these peers. The parallel health-promoting pathway includes the same general constructs but references the extent to which peers engage in healthy activities (running, biking, etc.). In addition, the SDM accounts for the effects of prior behavior both directly and indirectly (through social developmental processes) on later health behavior, as well as the influence of external social constraints (societal norms, rules, and laws), one’s position in the social structure (gender, ethnicity, and socioeconomic status), and individual characteristics (such as temperament) (shown as exogenous factors in Figure 1).
We and others have applied the SDM across diverse samples to successfully predict a range of health-related outcomes including substance use and misuse and other problem behaviors, as well as positive outcomes.29–35 No tests of the SDM specific to tobacco use, however, have been conducted. The SDM is well suited to the 30s because it captures diverse sources of social influence reflecting the variation in life paths at this age (eg, for a single person who is dating and attending school, or for a married parent who is working full time). For the prediction of cigarette use in the 30s in the present study, we included factors along the health-risking pathway that were specific to cigarette-using environments (perceived opportunities with others who smoke cigarettes, etc.), and factors along the health-promoting pathway specific to environments that promote good physical health, largely focused on the extent to which others across different social environments engaged in physical activities to improve health.
Study Aims
The goal of this study was to better understand the degree to which social environmental factors in the 30s help explain continuity in cigarette use from age 30 to 39. To do this, we addressed three main study aims. First, we specified measures of the social environment in the mid-30s to investigate the cigarette-using and health-promoting environmental pathways consistent with the SDM. Second, we aimed to model the continuity of cigarette use from age 30 to 39 and test the hypothesis that environmental and attitudinal mechanisms specified by the SDM mediate this continuity. To the extent mediated pathways are confirmed, these can inform intervention development seeking to reduce cigarette use during the 30s. Third, use of electronic cigarettes was included in the model in order to test the hypothesis that similar environmental factors played a significant role in predicting this emerging behavior when considered jointly with combustible cigarette use. Given growing interest in e-cigs, it is important to investigate similarities and differences in environmental factors contributing to their use compared with c-cigs. If different pathways emerge, the possibility of use-specific intervention implications should be considered.
Methods
Sample
Data are from the Seattle Social Development Project, a longitudinal study of health behavior and health outcomes. The longitudinal panel was established in 1985 from a population of all students (N = 1053) entering Grade 5 in 18 public schools serving higher crime neighborhoods in Seattle, Washington. Of these students, 808 (77%) youth and their parents consented to participate in the longitudinal study. Data for analyses reported here were collected in the spring of 2005, when most participants were 30 years old (M = 30.51, SD = .55), and again at ages 33 (2008) and 39 (2014). Retention of still-living participants from the original panel averaged 90% from age 30 to 39 (37 participants were deceased by age 39). Over the course of the study, retention was not consistently related to gender, ethnicity, childhood poverty, or adolescent substance use. The sample was 51% male; 47% were European American, 26% African American, 22% Asian American, and 5% Native American. Of these, 5% were Hispanic. Over half (52%) had experienced childhood poverty as evidenced by participation in the National School Lunch/Breakfast Program between the ages of 10 and 12. Participants were interviewed in person and completed password-protected web-based surveys lasting 2–3 hours in total, after which they received $100 compensation. The study was approved by the Human Subjects Review Committee at the University of Washington.
Design
To test study aims, we sought to utilize available measures across data waves in the 30s to best represent all model constructs and outcomes and hypothesized temporal relationships, as well as to retain relative model parsimony for analytic execution and interpretability. To achieve this, continuity and mediation of cigarette use was examined by modeling the direct association of cigarette use at age 30 with cigarette use at age 39 as well as the indirect association mediated through SDM constructs modeled at age 33. All SDM constructs at age 33 were linked by pathways consistent with SDM hypotheses. To limit model complexity, exogenous covariates were confined to key demographic measures shown to be associated with cigarette use, modeled as “position in the social structure” as specified by the SDM.11,14
Measures
Social Development Model
SDM measurement has been developed and validated in prior reports.29–31,34 SDM constructs used in this analysis were assessed with self-reports of past-year behavior at age 33. For each construct, items similar to those shown illustratively in Table 1 were assessed across multiple life domains (spouse/partner, dating, peers, and coworkers) and combined into mean scales. Because items were combined across different domains into a formative index, internal consistency estimates are not appropriate (eg, the level of opportunities for involvement with partner were not necessarily expected to be associated with the level of opportunities for involvement with peers), with the exception of skills for health (α = .81) and cigarette beliefs (α = .60).36 To define opportunities, involvement, rewards, and bonding as health promoting or health risking, these measures were weighted by the degree to which others in the social environment were engaged in health-promoting activities or cigarette use. For example, to indicate a health-promoting social influence, frequency of involvement with three closest friends was weighted by the degree to which each friend was engaged in healthy activities (eg, running or biking) such that involvement with a relatively active friend would obtain a higher score but equivalent involvement with a relatively inactive friend would obtain a lower score. Similarly, to indicate a health-risking social influence, the frequency of involvement with closest friends was weighted by the extent to which each friend used cigarettes.31,37 After weighting, measures of each SDM construct were created by combining items into mean scores and then recoding the range from 0 to 1 to provide consistency in range across scales. Higher scores indicated a higher level of the construct as labeled.
Table 1.
Social Development Model Measures
| Construct | Description | Number of items | Example |
|---|---|---|---|
| Perceived opportunities with active people | Perceived opportunities for involvement with others who engage in activities to improve health | 7 | I have lots of chances to do things with my partner. [weighted by partner’s engagement in activities to improve physical health] |
| Involvement with active people | Actual involvement with others who engage in activities to improve health | 12 | Overall, how often do you interact, hang out, or talk with the friend closest to you? [weighted by his or her engagement in activities to improve physical health] |
| Perceived rewards from active people | Perceived rewards for involvement with others who engage in activities to improve health | 15 | How much support and encouragement do you receive from your partner? [weighted by partner’s engagement in activities to improve physical health] |
| Bonding to active people | Attachment and commitment to others who engage in activities to improve health | 13 | How close is your relationship with the friend closest to you? [weighted by his or her engagement in activities to improve physical health] |
| Belief in importance of being active | Value of active leisure activities to participant | 1 | How important are active leisure activities to you personally? |
| Perceived opportunities with smokers | Perceived opportunities for involvement with others who smoke cigarettes | 9 | I have a lot of chances to do things with my coworker(s). [weighted by coworkers’ use of cigarettes] |
| Involvement with smokers | Actual involvement with others who smoke cigarettes | 14 | How often do you interact or talk with your partner? [weighted by partner’s use of cigarettes] |
| Perceived rewards from smokers | Perceived rewards for involvement with others who smoke cigarettes | 15 | How much can you really count on the friend closest to you to help you feel better when you are feeling generally upset or down in the dumps? [weighted by his or her use of cigarettes] |
| Bonding to smokers | Attachment and commitment to others who smoke cigarettes | 13 | I would stick by my partner no matter what. [weighted by partner’s use of cigarettes] |
| Belief that cigarette use is ok with few social costs | Values accepting of others who smoke cigarettes | 4 | Do you think it is okay for adults to smoke cigarettes? |
| Skills for health-related involvement | Proactive involvement in managing health (adequate sleep, control stress, and daily routines) | 4 | How often to you get adequate sleep every day? |
Cigarette Use
Frequency of c-cig use in the past month was included in the models at ages 30 and 39, self-reported on a 5-point scale for typical daily use from “not at all,” “less than one cigarette a day,” and so forth, up to “about a pack a day or more.” Frequency of e-cig use was also included at age 39, self-reported as number of times used in the past month (coded 0–30 to limit outliers). Because e-cigs were new to the market and still rare, e-cig use was not assessed at age 33 (in 2008) or prior. All cigarette-use measures were log-transformed to reduce skewness.
Covariates
Demographic covariates included gender (coded 1 if male, 0 if female), ethnicity (dummy coded for African American, Asian American, and Native American, with European American as reference category), childhood poverty (coded 1 if participated in the school lunch/breakfast program between ages 10 and 12, 0 otherwise), and educational attainment (years of schooling by age 21).
Analyses
Models were examined with Mplus 7.4 using the MLR estimator (maximum likelihood with robust standard errors) and full-information maximum likelihood missing data estimation.38 Standardized path coefficients are presented, using two-tailed tests of significance. The comparative fit index (CFI)39 and root mean squared error of approximation (RMSEA)40 are reported for model fit. Part of the sample was exposed to a multicomponent preventive intervention in the elementary grades, consisting of teacher training, parenting classes, and social competence training for children.41 It is possible that the intervention led to differences in the covariances among study variables. To investigate this, we conducted a multiple-group structural equation model test comparing a model where covariances were constrained to be equal across the full intervention (those receiving all intervention components, where intervention effects have been found to be strongest in prior reports) and control groups, to a model in which these parameters were freely estimated.38 This test showed no significant reduction in the overall fit of the constrained model (Δχ 2(46) = 49.00, p = .35), suggesting no substantial group differences in the relationships of interest and supporting full-sample analyses. Thus, consistent with prior analyses that have shown few differences in the covariance structures of the intervention and control groups,30,42 analyses shown here were based on the full sample.
Results
Descriptive statistics and zero-order correlations among study variables are shown in Table 2. At ages 30 and 39, 230 (32%) and 159 (24%) participants reported past-month c-cig use, respectively, and 130 (20%) reported c-cig use at both ages. Mean c-cig use at age 39 was almost half a pack a day (interpolated as 9.04 cigarettes/day from the 5-point scale, SD = 6.55) among users; 60 participants (9%) reported past-month e-cig use with a mean frequency of 8.62 times in the past month (SD = 10.60) among users; 45 participants (7%) reported both past-month c-cig and e-cig use (Table 2 shows means of the logged scores used in the analysis). It is noteworthy that the magnitude of correlations of cigarette use in the 30s with gender, ethnicity, and childhood poverty was relatively low. The only correlations above .10 in magnitude were the association of gender (male; r = .11) and Asian American ethnicity (vs. European American) (−.11) with c-cig use at age 39. Educational attainment was an exception, with strong associations with less c-cig use at both ages 30 (−.36) and 39 (−.33). E-cig use had almost no association with these demographic measures, including education (r = −.05).
Table 2.
Correlations Between Measures
| Construct | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | M (SD) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender (male) | .01 | .04 | −.08 | −.08 | −.14* | .04 | −.06 | −.02 | −.02 | −.05 | .09 | .04 | .03 | .04 | .20* | .02 | .09* | .11* | .05 | −.01 | .05 | .51 (.50) |
| 2. Afr Am (vs. Eur Am) | — | — | .45* | −.10* | −.13* | −.09* | −.11* | −.07 | −.09* | −.01 | .01 | −.03 | −.01 | .07 | .01 | −.03 | −.03 | .02 | −.10* | −.01 | .26 (.44) | |
| 3. Asn Am (vs. Eur Am) | — | .35* | .12* | .04 | .02 | .04 | .06 | −.04 | −.08 | −.07 | −.05 | −.06 | −.02 | −.04 | −.08 | −.11* | −.03 | .04 | −.07 | .22 (.41) | ||
| 4. Nat Am (vs. Eur Am) | .17* | −.14* | −.14* | −.12* | −.11* | −.13* | −.07* | .08* | .04 | .08* | .06 | .06 | −.03 | .07 | .08* | .00 | −.13* | .07 | .05 (.22) | |||
| 5. Childhood poverty | −.31* | −.19* | −.12* | −.16* | −.13* | −.12* | .14* | .15* | .11* | .12* | .04 | −.01 | .08 | .05 | .02 | −.16* | .13* | .52 (.50) | ||||
| 6. Educ. Attainment | .27* | .22* | .25* | .23* | .22* | −.32* | −.31* | −.27* | −.27* | −.20* | .08* | −.36* | −.33* | −.05 | .25* | −.30* | 12.23 (1.41) | |||||
| 7. Health opportunities | .89* | .93* | .94* | .29* | −.30* | −.27* | −.25* | −.26* | −.21* | .18* | −.27* | −.27* | −.07* | — | — | .75 (.21) | ||||||
| 8. Health involvement | .90* | .91* | .29* | −.26* | −.18* | −.20* | −.20* | −.16* | .19* | −.22* | −.21* | −.08* | — | — | .63 (.17) | |||||||
| 9. Health reward | .94* | .28* | −.30* | −.25* | −.21* | −.24* | −.19* | .18* | −.23* | −.21* | −.08* | — | — | .68 (.20) | ||||||||
| 10. Health bonding | .27* | −.26* | −.21* | −.19* | −.18* | −.16* | .17* | −.22* | −.21* | −.06 | — | — | .66 (.18) | |||||||||
| 11. Health belief | −.13* | −.13* | −.10* | −.11* | −.20* | .26* | −.18* | −.18* | −.02 | .30* | −.12* | .73 (.31) | ||||||||||
| 12. Cig. opportunities | .95* | .95* | .96* | .42* | −.17* | .43* | .33* | .24* | — | — | .23 (.18) | |||||||||||
| 13. Cig. involvement | .94* | .94* | .42* | −.17* | .44* | .35* | .21* | — | — | .21 (.16) | ||||||||||||
| 14. Cig. rewards | .98* | .40* | −.12* | .42* | .32* | .21* | — | — | .20 (.19) | |||||||||||||
| 15. Cig. bonding | .40* | −.14* | .42* | .32* | .23* | — | — | .20 (.19) | ||||||||||||||
| 16. Cig. belief | −.12* | .35* | .34* | .14* | −.19* | .42* | .43 (.20) | |||||||||||||||
| 17. Skills for health | −.16* | −.09* | −.03 | .18* | −.15* | .60 (.21) | ||||||||||||||||
| 18. C-cig use (age 30) | .68* | .35* | −.24* | .44* | .67 (1.11)+ | |||||||||||||||||
| 19. C-cig use (age 39) | .30* | −.23* | .34* | .56 (1.09)+ | ||||||||||||||||||
| 20. E-cig use (age 39) | −.07* | .23* | .15 (.57)+ | |||||||||||||||||||
| 21. Health-prom. env. | −.25* | .28 (.20) | ||||||||||||||||||||
| 22. Cig.-using env. | −.22 (.18) |
Afr Am = African American; Asn = Asian; Nat = Native; Eur = European; Educ. = Educational; Cig. = cigarette; C-cig = combustible-cigarette; E-cig = electronic-cigarette; prom. = promoting; env. = environment.
*p < .05.
+Logged scores; other scales (other than educ. attainment) ranged from 0 to 1.
Social Development Model for Combustible and Electronic Cigarette Use
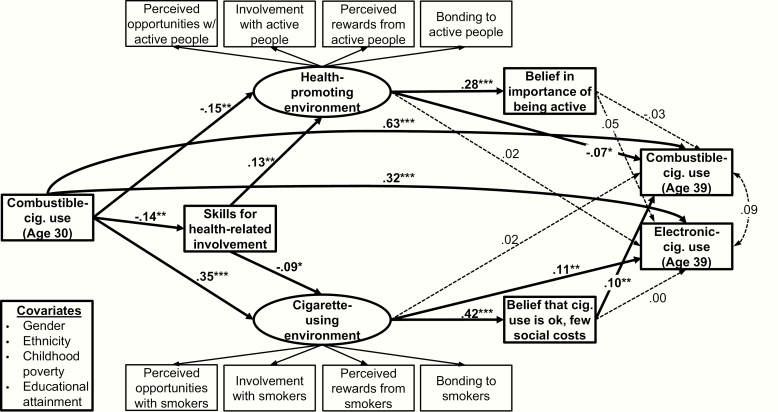
Table 2 shows that the measures of opportunities, involvement, rewards, and bonding were highly correlated. In line with the approach taken in prior tests of the SDM,30,31 these findings motivated the creation of two latent variables to capture the common variance in these constructs: one factor for the health-promoting environment (indicated by opportunities, involvement, rewards, and bonding with active people), and one factor for the cigarette-using environment (indicated by opportunities, involvement, rewards, and bonding with smokers). A model including these latent variables and structural relationships consistent with the hypothesized pathways of the SDM is shown in Figure 2. This model included c-cig use at age 30 as prior behavior and both c-cig and e-cig use at age 39 as correlated health behavior outcomes, as well as demographic covariates predicting prior behavior, skills, and environmental factors as specified by the SDM. Covariances among significantly correlated residuals of all corresponding health-promoting and cigarette-using constructs (eg, bonding to active people with bonding to smokers) were also included in the model. For clarity, pathways for demographic covariates and correlated residuals are not shown in Figure 2; all other significant and nonsignificant pathways depicted were included in the final model. Factor loadings on the two latent environment variables all exceeded .92 and the measurement model fit the data moderately well: χ 2(115) = 681.03, CFI = .94, RMSEA = .08.
Figure 2.
Latent variable model predicting combustible and electronic cigarette use at age 39 with pathways hypothesized by the social development model; predictors were assessed at age 33 except prior cigarette use. Significantly correlated residuals of indicator variables and corresponding model factors were included but not shown for clarity. cig. = cigarette. N = 788. χ2(116) = 328.52, CFI = .98, RMSEA = .05. Indirect effects: c-cig to c-cig = .03, p < .05; c-cig to e-cig = .04, p < .05. *p < .05, **p < .01, ***p < .001.
Results of the structural model indicated that the largest effects by far on both c-cig and e-cig use at age 39 were the direct paths from prior cigarette use at age 30 (Figure 2). The standardized path coefficients indicate an effect size of a one standard deviation change in prior cigarette use, which is equivalent to 1.88 c-cigs used per day or using e-cigs 1.38 times per month at age 39 for every 3.02 c-cigs used per day at age 30. It is noteworthy, however, that the structural relationships among SDM constructs at age 33 are consistent with SDM hypotheses and that, after accounting for the strong stability in cigarette use over time, social environmental factors in the intervening years still played a significant role for later cigarette use. The indirect effects demonstrated significant partial mediation of the effects of prior c-cig use on both c-cig and e-cig use at age 39 (β = .03, p < .05, and β = .04, p < .05, respectively). Prediction of c-cig use was primarily through the cigarette-using environment and, in turn, personal cigarette norms (beliefs that cigarette use is okay and has few social costs) at age 33. But e-cig use was predicted only through the cigarette-using environment, with little role for personal cigarette beliefs for this behavior.
The model also indicated a smaller though significant role for the health-promoting environment on less c-cig use at age 39, but no role on later e-cig use either directly or indirectly through health beliefs. Among demographic variables (not shown), educational attainment demonstrated significant associations with both health-promoting (β = .14, p < .01) and cigarette-using environments (β = −.14, p < .01), as well as less c-cig use at age 30 (β = −.36, p < .001). Childhood poverty was also associated with cigarette-using environments at age 33 (β = .08, p < .05). Direct effects of skills for health-related involvement on c-cig and e-cig use were also tested but were not significant and not added to the model. This model fit the data well: χ 2(116) = 328.52, CFI = .98, RMSEA = .05.
Discussion
Results indicated a significant role of the social environment for cigarette use in the 30s. The strongest predictor of cigarette use at age 39 was prior use of cigarettes at age 30, which was expected for an addictive substance such as nicotine. But social environmental factors in the mid-30s still contributed to the variance in cigarette use at age 39, even after accounting for prior cigarette use at age 30. This is itself a noteworthy result of the study because it suggests that even among smokers who are well into adulthood, their social environment in the 30s can have an influence on their cigarette use. The social environmental effects in the model indicated significant partial mediation of cigarette use for both c-cig and e-cig use at age 39. Given the strong stability in cigarette use across the 30s, this result was not obvious a priori, nor has such mediation been demonstrated in prior studies for this age period. Although the mediation was small relative to the high stability in cigarette use, the significant indirect effects can have a meaningful impact on population health given the role of cigarette use as the leading preventable cause of death in the United States.2,43
Significant mediated pathways linking prior with later cigarette use were primarily through the cigarette-using environment and beliefs about the acceptability of cigarette use, although the health-promoting environment also played a significant but smaller role. Specifically, environments characterized by opportunities, involvement, rewards, and bonding to smokers were related (directly or indirectly) to both greater c-cig and e-cig use, and environments characterized by experiences with others who engaged in healthy activities like running or biking were associated with less c-cig use. It should be noted that the cigarette-using and health-promoting environments were negatively correlated (−.25), suggesting a relative lack of health-promoting influences for those more enmeshed in cigarette-using environments and who were, therefore, less likely to have healthy social experiences counteracting those supporting cigarette use. However, results suggest that active environments may have potential to help diminish c-cig use even if cigarette-use promoting influences are present.
Findings also indicated an important difference in social environmental pathways for c-cig use versus e-cig use. Beliefs about cigarette use—whether it is okay for adults, and whether it affects a person’s social attractiveness—had a direct link to c-cig use at age 39 but not to e-cig use. This result is perhaps not surprising because public health campaigns against smoking have often stressed the social costs of smoking as a “disgusting habit” or cause for romantic rejection.44,45 With the advent of electronic cigarettes that reduce or eliminate the smoky odor, ashtrays, and cigarette butts associated with c-cig use, the beliefs and norms related to these “costs” are not salient.46,47 Hence, relationships with smokers—the cigarette-using environment—remained important for e-cig use, but the effect was direct, and norms and beliefs about the social costs of smoking did not appear to be activated.
An important limitation of the study is that there were no measures of social environments or beliefs specific to e-cigs. Future research should consider effects of relationships with others who use e-cigs and the perceived acceptability of e-cigs, as well as assessment of why participants used e-cigs. In addition to delivering nicotine in a more socially acceptable manner, research suggests that most smokers are attracted to e-cigs as a way to reduce or replace c-cig use for personal health reasons, but others may be motivated to use e-cigs by a desire to use more nicotine (eg, in areas where c-cigs are not allowed).48 In either case, these groups of e-cig users would also not be guided by their beliefs about the social costs of cigarette use, though beliefs about health effects of nicotine and other e-cig toxins could play a role.
Other limitations include a geographically limited sample that originated in Seattle. By age 30, however, much of the sample had dispersed across many different communities throughout the United States and beyond; only 30% remained in Seattle by age 39. Additionally, any differences in risk associated with the sample may affect the rates of risk behavior like smoking, but were not expected to influence the covariances that were the focus of this report. Testing the relationships reported here in other samples remains important, however. Self-report measures were used, but more than 20 years of confidential interviews with the longitudinal panel bolsters confidence in honest reporting. Cigarette use measures asked about use in the past month at ages 30 and 39, a limited timeframe that may not capture some patterns of episodic use. The study first measured e-cig use in 2014 (age 39); however, e-cigs were not widely available prior to 2008 (age 33) when measures of the SDM were assessed, thereby making it unlikely that prior e-cig use substantially influenced model variables. On the other hand, because 2014 was relatively early in the history of e-cigarettes, our measure preceded the introduction of Juul (that became the largest retail brand by 2017)49 and the identification of vaping-associated lung injury.22 Ongoing research is critical as the context and long-term consequences of e-cigarette use evolve. Important strengths of the study include longitudinal assessments enabling temporal modeling of prior behavior, social developmental mechanisms, and subsequent outcomes. The study was also theory guided from its inception, providing established measures of the SDM, as well as important demographic and socioeconomic covariates.
From a public health perspective, this study’s findings stress, first of all, the importance of preventing the uptake of smoking prior to the 30s. Consistent with the known addictive properties of nicotine, smoking behavior by age 30 was by far the strongest predictor of cigarette use 9 years later. Prior smoking also predicted the selection of cigarette-using environments at age 33. Findings also suggest, however, that the 30s may not be too late to address social influences with the potential to curb adult cigarette use. For combustible cigarettes, promoting active environments and stressing the health and social costs of cigarette use could remain a promising approach even among those who smoke beyond their 20s. Electronic cigarettes, however, present a unique challenge in that many antismoking beliefs and norms may not readily translate to this relatively new technology. Prevention programs and messages in this new era of e-cigs should consider other approaches, including limiting the availability of cigarette-using environments themselves (eg, public smoking/vaping restrictions), as well as disrupting the link between cigarette-using environments and one’s own use by stressing the risks and costs of nicotine addiction whether or not accompanied by tobacco smoke. At the same time, messages for current smokers should be mindful of the preferred goal of ending all forms of cigarette use, balanced with our current understanding that replacing c-cigs with e-cigs (with reputable branding22) will also likely have some public health benefit by reducing exposure to known carcinogens associated with combustible cigarette smoke.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Acknowledgments
The study was approved by the Human Subjects Review Committee at the University of Washington and complies with ethical standards in the treatment of human participants. We thank our funders, the study participants, and the staff of the Social Development Research Group.
Funding
This research was supported by grants from the National Cancer Institute (R37CA225690) and the National Institute on Drug Abuse (R01DA033956 and 1R01DA09679). Content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. NCI and NIDA played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; nor in the decision to submit the article for publication.
Declaration of Interests
None declared.
References
- 1. Wang TW, Asman K, Gentzke AS, et al. Tobacco product use among adults—United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(44):1225–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 3. Nutt D, King LA, Saulsbury W, Blakemore C. Development of a rational scale to assess the harm of drugs of potential misuse. Lancet. 2007;369(9566):1047–1053. [DOI] [PubMed] [Google Scholar]
- 4. Rachid F Neurostimulation techniques in the treatment of nicotine dependence: a review. Am J Addict. 2016;25(6):436–451. [DOI] [PubMed] [Google Scholar]
- 5. Schauer GL, Malarcher AM, Asman KJ. Trends in the average age of quitting among U.S. adult cigarette smokers. Am J Prev Med. 2015;49(6):939–944. [DOI] [PubMed] [Google Scholar]
- 6. Babb S, Malarcher A, Schauer G, Asman K, Jamal A. Quitting smoking among adults—United States, 2000–2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457–1464. [DOI] [PubMed] [Google Scholar]
- 7. Gilman SE, Abrams DB, Buka SL. Life course socioeconomic status and transitions of tobacco use: event-history analyses of the age at first cigarette, daily smoking, and smoking cessation (meeting abstract). Am J Epidemiol. 2002;155(11)(suppl):S71. [Google Scholar]
- 8. Ostbye T, Malhotra R, Landerman LR. Body mass trajectories through adulthood: results from the National Longitudinal Survey of Youth 1979 Cohort (1981–2006). Int J Epidemiol. 2011;40(1):240–250. [DOI] [PubMed] [Google Scholar]
- 9. Settersten RA Age structuring and the rhythm of the life course. In: Mortimer JT, Shanahan MJ, eds. Handbook of the Life Course. Boston, MA: Springer US; 2003:81–98. [Google Scholar]
- 10. Settersten RA Jr, Ray B. What’s going on with young people today? The long and twisting path to adulthood. Future Child. 2010;20(1):19–41. [DOI] [PubMed] [Google Scholar]
- 11. U.S. Department of Health and Human Services. Preventing Tobacco Use Among Young People: A Report of the Surgeon General, 2012. Atlanta, GA: U.S. Department of Health and Human Services; 2012. [Google Scholar]
- 12. Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull. 1992;112(1):64–105. [DOI] [PubMed] [Google Scholar]
- 13. White TJ, Redner R, Bunn JY, Higgins ST. Do socioeconomic risk factors for cigarette smoking extend to smokeless tobacco use? Nicotine Tob Res. 2016;18(5):869–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dietz NA, Sly DF, Lee DJ, Arheart KL, McClure LA. Correlates of smoking among young adults: the role of lifestyle, attitudes/beliefs, demographics, and exposure to anti-tobacco media messaging. Drug Alcohol Depend. 2013;130(1–3):115–121. [DOI] [PubMed] [Google Scholar]
- 15. Rose JS, Lee CT, Dierker LC, Selya AS, Mermelstein RJ. Adolescent nicotine dependence symptom profiles and risk for future daily smoking. Addict Behav. 2012;37(10):1093–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rosenthal L, Carroll-Scott A, Earnshaw VA, et al. Targeting cessation: understanding barriers and motivations to quitting among urban adult daily tobacco smokers. Addict Behav. 2013;38(3):1639–1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Castro Y, Heck K, Forster JL, Widome R, Cubbin C. Social and environmental factors related to smoking cessation among mothers: findings from the Geographic Research on Wellbeing (GROW) Study. Am J Health Behav. 2015;39(6):809–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Georgiadou C, Lavdaniti M, Psychogiou M, Tzenalis A, Sgantzos M, Sapountzi-Krepia D. Factors affecting the decision to quit smoking of the participants of a hospital-based smoking cessation program in Greece. J Caring Sci. 2015;4(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Callinan JE, Clarke A, Doherty K, Kelleher C. Legislative smoking bans for reducing secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst Rev. 2010;2010(4):1-92. CD005992. [DOI] [PubMed] [Google Scholar]
- 20. Martin LM, Sayette MA. A review of the effects of nicotine on social functioning. Exp Clin Psychopharmacol. 2018;26(5):425–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Burgess-Hull AJ, Roberts LJ, Piper ME, Baker TB. The social networks of smokers attempting to quit: an empirically derived and validated classification. Psychol Addict Behav. 2018;32(1):64–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Centers for Disease Control & Prevention. Outbreak of Lung Injury Associated With the Use of E-cigarette, or Vaping, Products 2019. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html. Accessed December 3, 2019.
- 23. National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-cigarettes. Washington, DC: The National Academies Press; 2018. [PubMed] [Google Scholar]
- 24. Benmarhnia T, Pierce JP, Leas E, et al. Can e-cigarettes and pharmaceutical aids increase smoking cessation and reduce cigarette consumption? Findings from a nationally representative cohort of American smokers. Am J Epidemiol. 2018;187(11):2397–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Levy DT, Yuan Z, Luo Y, Abrams DB. The relationship of e-cigarette use to cigarette quit attempts and cessation: insights from a large, nationally representative U.S. survey. Nicotine Tob Res. 2018;20(8):931–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bao W, Xu G, Lu J, Snetselaar LG, Wallace RB. Changes in electronic cigarette use among adults in the United States, 2014–2016. JAMA. 2018;319(19):2039–2041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dai H, Leventhal AM. Prevalence of e-cigarette use among adults in the United States, 2014–2018. JAMA. 2019;322(18):1824–1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Catalano RF, Hawkins JD. The social development model: a theory of antisocial behavior. In: Hawkins JD, ed. Delinquency and Crime: Current Theories. New York, NY: Cambridge University Press; 1996:149–197. [Google Scholar]
- 29. Catalano RF, Park J, Harachi TW, Haggerty KP, Abbott RD, Hawkins JD. Mediating the effects of poverty, gender, individual characteristics, and external constraints on antisocial behavior: a test of the social development model and implications for developmental life-course theory. In: Farrington DP, ed. Advances in Criminological Theory: Vol. 14. Integrated Developmental and Life-Course Theories of Offending. New Brunswick, NJ: Transaction; 2005:93–123. [Google Scholar]
- 30. Huang B, Kosterman R, Catalano RF, Hawkins JD, Abbott RD. Modeling mediation in the etiology of violent behavior in adolescence: a test of the social development model. Criminology. 2001;39(1):75–107. [Google Scholar]
- 31. Kosterman R, Hill KG, Lee JO, et al. Young adult social development as a mediator of alcohol use disorder symptoms from age 21 to 30. Psychol Addict Behav. 2014;28(2):348–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sullivan CJ, Hirschfield P. Problem behavior in the middle school years: an assessment of the social development model. J Res Crime Delinquency. 2011;48(4):566–593. [Google Scholar]
- 33. Choi Y, Harachi TW, Gillmore MR, Catalano RF. Applicability of the social development model to urban ethnic minority youth: examining the relationship between external constraints, family socialization, and problem behaviors. J Res Adolesc. 2005;15(4):505–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fleming CB, Catalano RF, Oxford ML, Harachi TW. A test of generalizability of the social development model across gender and income groups with longitudinal data from the elementary school developmental period. J Quant Criminol. 2002;18(4):423–439. [Google Scholar]
- 35. Roosa MW, Zeiders KH, Knight GP, et al. A test of the social development model during the transition to junior high with Mexican American adolescents. Dev Psychol. 2011;47(2):527–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bollen KA, Bauldry S. Three Cs in measurement models: causal indicators, composite indicators, and covariates. Psychol Methods. 2011;16(3):265–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kosterman R, Mason WA, Haggerty KP, Hawkins JD, Spoth R, Redmond C. Positive childhood experiences and positive adult functioning: prosocial continuity and the role of adolescent substance use. J Adolesc Health. 2011;49(2):180–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Muthén LK, Muthén BO. Mplus User’s Guide. Los Angeles, CA: Muthén & Muthén; 1998–2015. [Google Scholar]
- 39. Bentler PM Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238–246. [DOI] [PubMed] [Google Scholar]
- 40. Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, eds. Testing Structural Equation Models. Newbury Park, CA: Sage; 1993:136–162. [Google Scholar]
- 41. Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD. Promoting positive adult functioning through social development intervention in childhood: long-term effects from the Seattle Social Development Project. Arch Pediatr Adolesc Med. 2005;159(1):25–31. [DOI] [PubMed] [Google Scholar]
- 42. Kosterman R, Hawkins JD, Abbott RD, Hill KG, Herrenkohl TI, Catalano RF. Measures of positive adult behavior and their relationship to crime and substance use. Prev Sci. 2005;6(1):21–33. [DOI] [PubMed] [Google Scholar]
- 43. Bellinger DC Interpretation of small effect sizes in occupational and environmental neurotoxicology: individual versus population risk. Neurotoxicology. 2007;28(2):245–251. [DOI] [PubMed] [Google Scholar]
- 44. Clayton RB, Leshner G, Tomko RL, Trull TJ, Piasecki TM. Countering craving with disgust images: examining nicotine withdrawn smokers’ motivated message processing of anti-tobacco public service announcements. J Health Commun. 2017;22(3):254–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Pechmann C, Reibling ET. Anti-smoking advertising campaigns targeting youth: case studies from USA and Canada. Tob Control. 2000;9(suppl 2):18–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Case K, Crook B, Lazard A, Mackert M. Formative research to identify perceptions of e-cigarettes in college students: implications for future health communication campaigns. J Am Coll Health. 2016;64(5):380–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sangalang A, Volinsky AC, Liu J, et al. Identifying potential campaign themes to prevent youth initiation of e-cigarettes. Am J Prev Med. 2019;56(2suppl 1):S65–S75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Dockrell M, Morrison R, Bauld L, McNeill A. E-cigarettes: prevalence and attitudes in Great Britain. Nicotine Tob Res. 2013;15(10):1737–1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Huang J, Duan Z, Kwok J, et al. Vaping versus JUULing: how the extraordinary growth and marketing of JUUL transformed the US retail e-cigarette market. Tob Control. 2019;28(2):146–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.