Abstract
Rationale: Implementation of the Hospital Readmissions Reduction Program (HRRP) following discharge of patients with chronic obstructive pulmonary disease (COPD) has led to a reduction in 30-day readmissions with unknown effects on postdischarge mortality.
Objectives: To examine the association of HRRP with 30-day hospital readmission and 30-day postdischarge mortality rate in patients after discharge from COPD hospitalization.
Methods: Retrospective cohort study of readmission and mortality rates in a national cohort (N = 4,587,542) of admissions of Medicare fee-for-service beneficiaries 65 years or older with COPD from 2006 to 2017.
Measurements and Main Results: Data were analyzed for three nonoverlapping periods based on implementation of the HRRP specific to COPD: 1) preannouncement (December 2006 to March 2010), 2) announcement (April 2010 to August 2014), and 3) implementation (October 2014 to November 2017). The 30-day readmission rate decreased from 20.54% in the preannouncement period (December 2006 to July 2008) to 18.74% in the implementation period (May 2016 to November 2017). The 30-day risk-standardized postdischarge mortality rates were 6.91%, 6.59%, and 7.30% for the preannouncement, announcement, and implementation periods, respectively. Generalized estimating equations analyses estimated an additional 1,196 deaths (October 2014 to April 2016) and 3,858 deaths (May 2016 to November 2017) during the HRRP implementation period.
Conclusions: We found a reduction in 30-day all-cause readmission rate during the implementation period compared with the preannouncement phase. HRRP implementation was also associated with a significant increase in 30-day mortality after discharge from COPD hospitalization. Additional research is necessary to confirm our findings and understand the factors contributing to increased mortality in patients with COPD in the HRRP implementation period.
Keywords: hospital readmissions, obstructive lung diseases, Medicare, hospitalization, mortality
At a Glance Commentary
Scientific Knowledge on the Subject
Evidence suggests that the Hospital Readmission Reduction Program (HRRP) developed by the Centers for Medicare and Medicaid Services is associated with a reduction in 30-day readmissions. It is also suspected that HRRP may be associated with an increase in the 30-day risk-standardized postdischarge mortality rates for some groups of patients currently participating in the program.
What This Study Adds to the Field
We studied 4,587,542 Medicare fee-for-service beneficiaries with chronic obstructive pulmonary disease (COPD) who were 65 years and older. The study period from 2006 to 2017 covers the creation of HRRP and the introduction of COPD to the program. We found statistically significant increases in the risk-standardized 30-day postdischarge mortality rates across the nation for patients with COPD. Teaching hospitals and hospitals with a >1 nurse-per-bed ratio had a lower 30-day postdischarge mortality rate during the latter part of the HRRP implementation period.
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death in the United States (1). COPD affects 12.7 million Americans, and annually, about 800,000 patients are hospitalized with COPD (2). Of these, one in five patients are readmitted, mostly for non–COPD-related conditions (3–5). Readmissions after discharge from a COPD hospitalization cost ∼$13 billion and are associated with poor outcomes (6, 7).
To improve clinical outcomes and control rising healthcare costs, the Patient Protection and Affordable Care Act created the Hospital Readmissions Reduction Program (HRRP) in March 2010 (8). Penalties for target conditions were announced and became effective in October 2012. HRRP began penalizing hospitals for higher-than-expected 30-day readmissions rates for non-COPD conditions (4). Penalties for COPD were added in October 2014. Payment reductions to hospitals treating Medicare beneficiaries are capped at 3%. The penalties apply to all Medicare fee-for-service beneficiaries in relevant diagnosis-related groups, including COPD. The penalties are calculated based on a 3-year rolling average.
Since the creation of the HRRP, hospitals have reduced their readmission rates (9–15). This reduction started before the implementation of penalties by the HRRP for COPD (11, 12) and non-COPD conditions (10, 14, 15). This suggests that hospitals started implementing strategies to reduce readmission rates and to avoid future payment reductions during the announcement period (penalty-free) of the HRRP. During the implementation phase of the HRRP, there was a paucity of evidence-based strategies to guide hospitals in how to reduce hospital readmissions after COPD hospitalization. Over time, patient and system factors that contribute to readmission after hospitalization for COPD have been identified (3–5, 16–21). However, the early interventions applied to reduce COPD readmissions demonstrated variable impacts on readmission rates (22–28), and some may have resulted in higher mortality (29).
The purpose of our study was to examine the relationship between 30-day risk-standardized all-cause hospital readmission rates and 30-day risk standardized all-cause postdischarge mortality for Medicare beneficiaries with COPD during three time periods: 1) a 4-year baseline period before the official start of the HRRP program; 2) a 4-year period of announcement for COPD; and 3) a 3-year period of the established HRRP for COPD. We hypothesized that differences would exist in the relationship between 30-day all-cause hospital readmission rates and 30-day all-cause postdischarge mortality rates for Medicare beneficiaries with COPD across the three time periods. Our hypothesis is based on prior evidence suggesting a relationship between risk-standardized readmission rates and risk-standardized mortality rates for COPD (12). The strengths of our study include a large national cohort of Medicare fee-for-service beneficiaries studied from 2006 to 2017. The large cohort and longitudinal data allowed us to examine trends in patient characteristics and hospitals factors not possible in previous studies. The study findings will expand our knowledge of the relationships between the HRRP and 30-day postdischarge mortality rates in patients with COPD. Some of the results of this research have been previously reported as an abstract (30).
Methods
Study Cohort
We conducted a hospital-level retrospective study of all-cause 30-day readmissions (hereafter referred to as 30-day readmission rates) and 30-day postdischarge mortality (hereafter referred to as 30-day mortality rates) involving patients with COPD, using 100% Medicare files from 2006 to 2017. The study was approved by the institutional review board of the University of Texas Medical Branch and complies with the Centers for Medicare and Medicaid Services (CMS) Data Use Agreement requirements. Acute admission patients with COPD as the principal discharge diagnosis were identified using the Medicare Provider Analysis and Review files following the CMS published algorithm (31–33). We selected patients with acute COPD admission, aged 65 years or older, and enrolled in Medicare Part A for at least 12 months before admission and at least 1 month after discharge (including those who died within 1 mo of discharge). We excluded admissions in which the patient died during the hospital stay, had another COPD hospitalization discharge in the 30 days before admittance, was discharged against medical advice, or was transferred from hospice. Transfer admissions were bundled to the first hospital (Figure 1).
Figure 1.
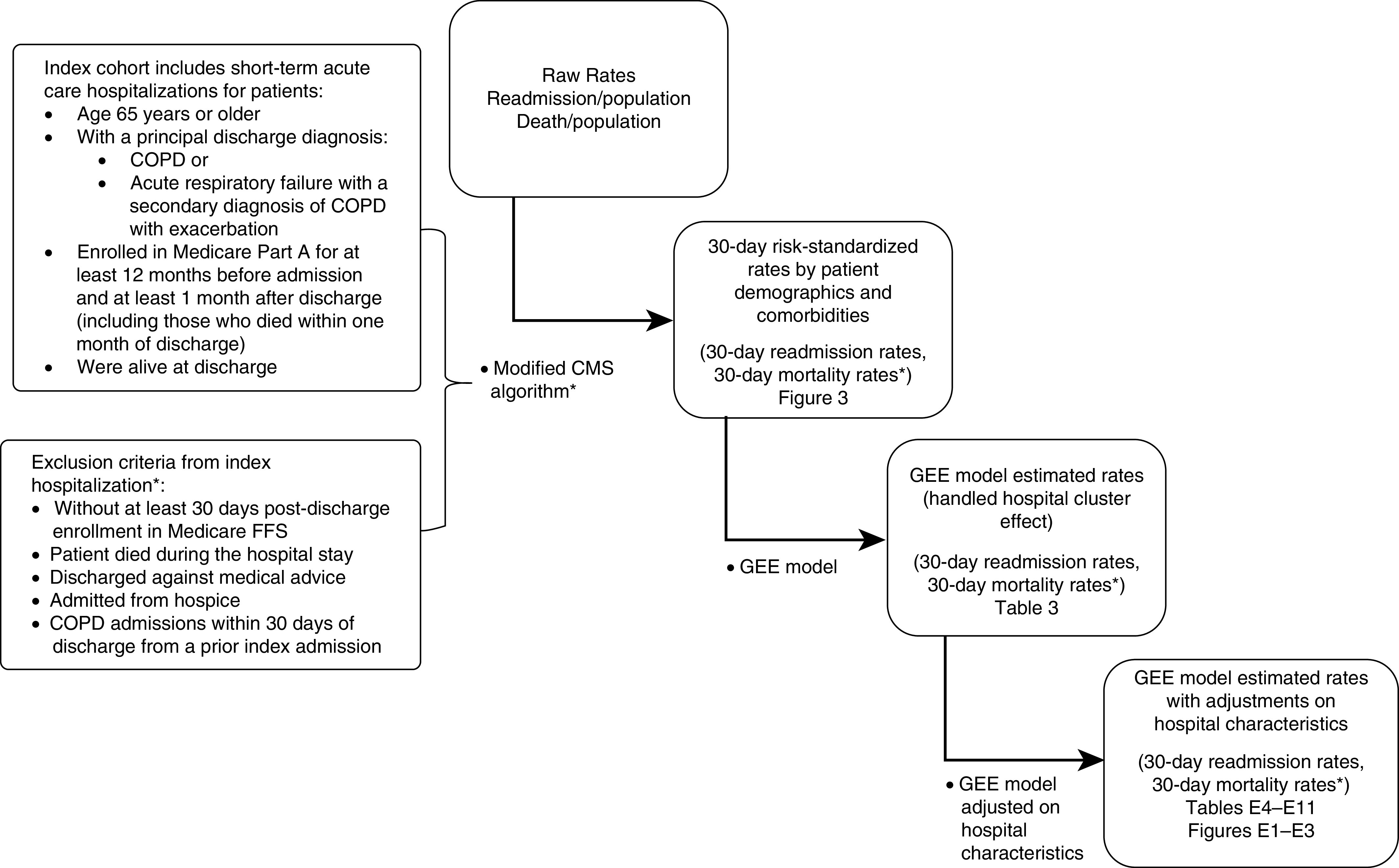
Flowchart of study methodology. *Our 30-day postdischarge mortality outcome was obtained by excluding patients who died during hospitalization (before hospital discharge). This is contrary to how CMS calculates 30-day mortality rates (mortality within a 30-d period from the date of the index admission). Other differences from the CMS algorithm are caused by limitations in our data sources; please see Methods section. ‡Tables and figures available in the online supplement. CMS = Centers for Medicare and Medicaid Services; COPD = chronic obstructive pulmonary disease; FFS = fee-for-service; GEE = generalized estimating equation.
Study Periods
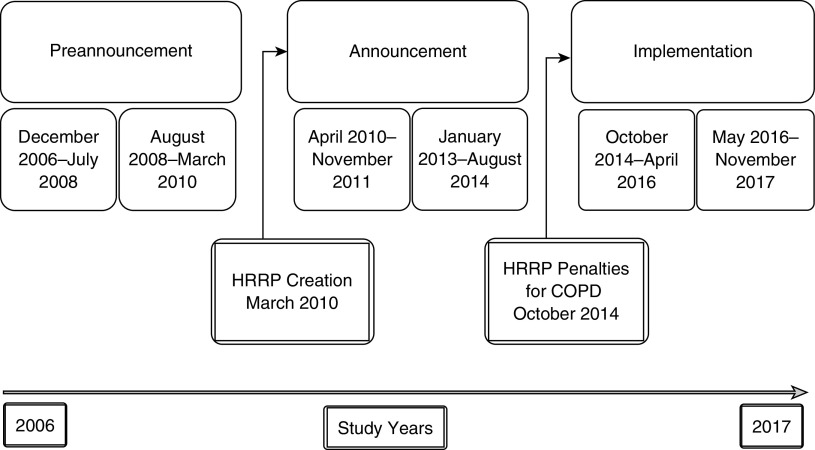
We split the study years into three nonoverlapping periods (preannouncement, announcement, and implementation), based on the HRRP announcement date (April 2010) and the implementation of penalties specific for COPD (October 2014). We excluded admissions in the year 2012 owing to limitations in linking beneficiary identification. Because of the same limitation, our announcement period, which covers 2012, was split into two 20-month subperiods. Our periods were divided as follows: preannouncement, December 2006 to July 2008 and August 2008 to March 2010; announcement, April 2010 to November 2011 and January 2013 to August 2014; implementation, October 2014 to April 2016 and May 2016 to November 2017. The announcement period of April 2010 to November 2011 was used as a pivot for comparisons among periods (Figure 2).
Figure 2.
Study periods in relationship to the HRRP announcement and implementation of penalties for COPD. The study years were divided into three nonoverlapping periods (preannouncement, announcement, and implementation), based on the HRRP announcement date (April 2010) and the implementation of penalties specific for COPD (October 2014). We excluded admissions in the year of 2012 owing to limitations in linking beneficiary identification. COPD = chronic obstructive pulmonary disease; HRRP = Hospital Readmissions Reduction Program.
Outcomes
The 30-day readmission rates and 30-day mortality rates were calculated at the hospital level following the CMS Condition-Specific Measures Updates and Specifications Report (32–34).
We collected hospital characteristics, including medical school affiliation, number of full-time nurses, organ transplant service, number of Medicare-certified beds, geographical region (35), type of ownership (36), and hospital ratings from a survey of patients’ experiences (Hospital Consumer Assessment of Healthcare Providers and Systems) (37, 38).
Statistical Analysis
Hospital characteristics, 30-day readmission rates, and 30-day mortality rates for each of the three periods were summarized. The generalized estimating equation (GEE) model was used to compare differences in readmission rates and mortality rates among periods while accounting for the cluster effect in hospitals (Table 1). We compared readmission and mortality rates for different hospital characteristics in each period; change in readmission and mortality rates across periods; and the slope of changes among hospital types. The Bonferroni procedure was used to correct for the family-wise error. We estimated additional deaths during the HRRP implementation period based on parameters from the GEE model. Additional detail on the methods used to make these measurements is provided in an online supplement. All analyses were performed using SAS version 9.4 (SAS Inc.). All reported P values were two-sided with P < 0.05.
Table 1.
GEE Model* Estimated 30-Day Readmission Rates and 30-Day Mortality Rates at the Hospital Level after Patients’ Discharge from COPD Hospitalization by the HRRP from December 2006 to November 2017 in the United States
| HRRP Periods | Period minus Announcement Period*† [% (95% CI)] | P Value‡ | ||
|---|---|---|---|---|
| 30-d readmission rate | Preannouncement | December 2006 to July 2008 | 0.46 (0.41 to 0.5) | <0.0001 |
| August 2008 to March 2010 | 0.32 (0.28 to 0.36) | <0.0001 | ||
| Announcement | January 2013 to August 2014 | −1.75 (−1.8 to 1.71) | <0.0001 | |
| Implementation | October 2014 to April 2016 | −1.53 (−1.58 to 1.48) | <0.0001 | |
| May 2016 to November 2017 | −1.34 (−1.39 to 1.29) | <0.0001 | ||
| 30-d mortality rate | Preannouncement | December 2006 to July 2008 | 0.33 (0.29 to 0.36) | <0.0001 |
| August 2008 to March 2010 | 0.1 (0.07 to 0.13) | <0.0001 | ||
| Announcement | January 2013 to August 2014 | 0.12 (0.09 to 0.16) | <0.0001 | |
| Implementation | October 2014 to April 2016 | 0.22 (0.18 to 0.26) | <0.0001 | |
| May 2016 to November 2017 | 0.71 (0.67 to 0.75) | <0.0001 | ||
Definition of abbreviations: CI = confidence interval; COPD = chronic obstructive pulmonary disease; GEE = generalized estimating equation; HRRP = Hospital Readmissions Reduction Program.
GEE model was used to account for the hospital cluster effect among multiple periods. We compared each periods’ mortality rate with that of the announcement period (each period minus the announcement period).
Announcement period from April 2010 to November 2011 was used as a pivot for comparisons among periods.
P value shows the significance of the differences. The P value was corrected by the Bonferroni procedure to account for family-wise error.
Results
Between December 2006 and November 2017, there were 4,587,542 admissions of Medicare fee-for-service beneficiaries 65 years or older with COPD. Among these, 4,450,933 (97.0%) were discharged alive. Of these discharges, there were 236,748 (5.3%) deaths within 30 days. The 30-day readmission rate decreased from 20.54% in the preannouncement period (December 2006 to July 2008) to 18.74% in the implementation period (May 2016 to November 2017). The 30-day mortality rates were 6.91%, 6.59%, and 7.30% for the preannouncement, announcement, and implementation periods, respectively (Figure 3).
Figure 3.
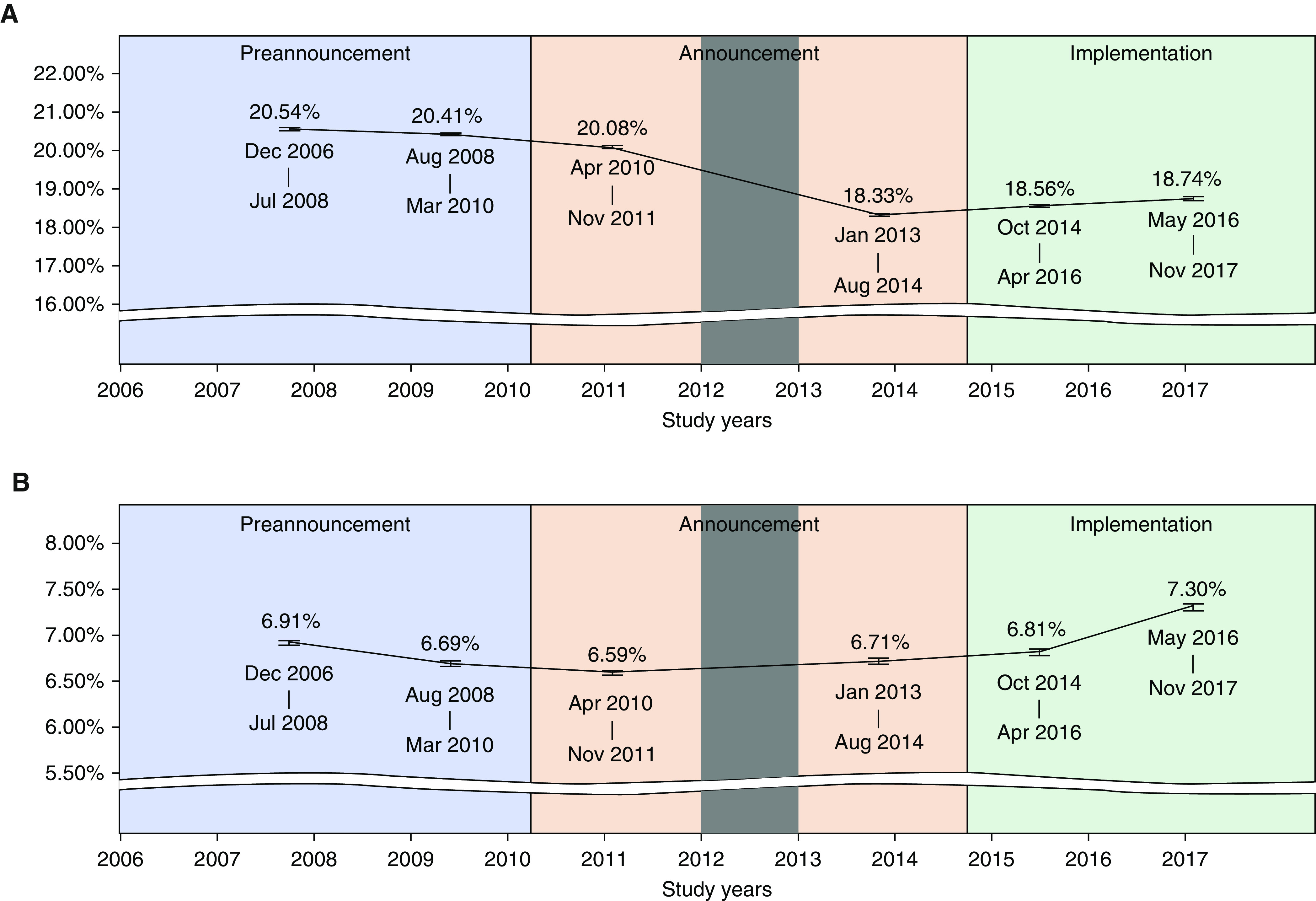
(A and B) Thirty-day readmission rate (A) and 30-day mortality rate (B) at the hospital level after patients’ discharge from COPD hospitalization during periods of the HRRP from December 2006 to November 2017 in the United States. We excluded admissions in the year of 2012 (grayed-out area) owing to limitations in linking beneficiary identification. COPD = chronic obstructive pulmonary disease; HRRP = Hospital Readmissions Reduction Program.
Patient Characteristics
About 57% of patients were male; the mean age was 77 (±SD 7) years; 86% were white, 8.9% were black, and 2% were Hispanic. About 12% of patients had a COPD admission in the previous year. The majority of patients in the study received no mechanical ventilation (79–85%) during the index hospitalization. Some 7–15% of patients had sleep apnea. Except for during the preannouncement period, the majority of patients had more than five chronic conditions (Table 2).
Table 2.
Characteristics of Fee-for-Service Medicare Patients Hospitalized for COPD during December 2006 to November 2017 in the United States
| HRRP* Periods | Preannouncement (December 2006 to March 2010) | Announcement |
Implementation (October 2014 to November 2017) | |
|---|---|---|---|---|
| April 2010 to November 2011 | January 2013 to August 2014 | |||
| Unique patients | 891,831 | 523,619 | 510,344 | 935,200 |
| All admissions | 1,911,177 | 1,025,183 | 942,435 | 1,938,060 |
| Admissions of patients ≥65 yr old | 1,523,008 | 801,033 | 745,087 | 1,518,414 |
| Unique patients, n (%) | ||||
| Sex | ||||
| M | 515,242 (57.7) | 303,216 (57.9) | 299,071 (58.6) | 536,426 (57.3) |
| F | 376,589 (42.2) | 220,403 (42.0) | 211,273 (41.4) | 398,774 (42.6) |
| Race, n (%) | ||||
| White | 781,913 (87.6) | 454,012 (86.7) | 439,385 (86.1) | 803,748 (85.9) |
| Black | 747,36 (8.3) | 482,81 (9.2) | 484,86 (9.5) | 896,04 (9.5) |
| Hispanic | 16,889 (1.8) | 9,923 (1.9) | 9,588 (1.8) | 16,073 (1.7) |
| Other | 17,557 (1.9) | 10,983 (2.1) | 11,929 (2.3) | 22,176 (2.3) |
| Unknown | 736 (0.08) | 420 (0.08) | 956 (0.19) | 3,599 (0.38) |
| Dual eligibility, n (%)† | ||||
| No | 675,864 (75.7) | 391,682 (74.8) | 381,921 (74.8) | 703,154 (75.1) |
| Yes | 215,967 (24.2) | 131,937 (25.2) | 128,423 (25.1) | 232,046 (24.8) |
| Age, yr‡ | ||||
| Mean (±SD) | 77.49 (7.4) | 77.34 (7.4) | 77.23 (7.5) | 77.24 (7.6) |
| Age range, yr, n (%) | ||||
| 65–70 | 173,541 (19.4) | 104,921 (20.04) | 103,972 (20.3) | 193,891 (20.7) |
| 70–75 | 192,603 (21.6) | 118,479 (22.6) | 119,997 (23.5) | 220,873 (23.6) |
| 75–80 | 195,443 (21.9) | 111,004 (21.2) | 106,767 (20.9) | 195,279 (20.8) |
| 80–85 | 173,427 (19.4) | 97,453 (18.6) | 88,429 (17.3) | 156,002 (16.6) |
| >85 | 156,817 (17.5) | 91,762 (17.5) | 91,179 (17.8) | 169,155 (18.09) |
| Chronic condition§ | ||||
| Mean (±SD) | 6.56 (4.4) | 7.47 (4.8) | 8.34 (5.5) | 10.23 (5.8) |
| Chronic condition range, n (%) | ||||
| ≤5 | 455,890 (51.1) | 225,481 (43.06) | 194,969 (38.2) | 209,914 (22.4) |
| 6–10 | 277,138 (31.08) | 176,353 (33.6) | 168,331 (32.9) | 343,796 (36.7) |
| >10 | 158,803 (17.8) | 121,785 (23.2) | 147,044 (28.8) | 381,490 (40.7) |
| Previous year COPD admission, n (%) | ||||
| No | 780,193 (87.4) | 458,723 (87.6) | 450,248 (88.2) | 819,971 (87.6) |
| Yes | 111,638 (12.5) | 64,896 (12.3) | 60,096 (11.7) | 115,229 (12.3) |
| History of mechanical ventilation, n (%) | ||||
| No | 765,297 (85.8) | 443,884 (84.7) | 418,597 (82.02) | 745,976 (79.7) |
| Yes | 126,534 (14.1) | 79,735 (15.2) | 91,747 (17.9) | 189,224 (20.2) |
| Obstructive sleep apnea, n (%) | ||||
| No | 825,849 (92.6) | 465,054 (88.8) | 429,831 (84.2) | 868,196 (92.8) |
| Yes | 65,982 (7.4) | 58,565 (11.1) | 80,513 (15.7) | 67,004 (7.1) |
Definition of abbreviations: COPD = chronic obstructive pulmonary disease; HRRP = Hospital Readmissions Reduction Program.
A single admission was randomly sampled for each patient, in each period.
Dual eligibility was defined as Medicare coverage in the month of admission.
Age was calculated on admission date.
Chronic conditions and previous year COPD admission looked at the 12 months before admission.
Hospital Characteristics
Table 3 presents the hospital characteristics. The percentage of hospitals with medical school affiliation increased over time (30.4% in the preannouncement period to 34.5% in the implementation period). The majority of hospitals were non–transplant centers (>77%), had ≤500 beds (88%), and were in metro areas (>70%). The percentage of hospitals that cared for patients in metro areas increased over time (70.2% in the preannouncement December 2006 to July 2008 period and 74.5% during the May 2016 to November 2017 implementation period). The majority of hospitals were nonprofit (>60%) and about 40% were in the South. The percentage of public (government-owned) hospitals decreased over time (19.3% in the preannouncement period and 16.1% in the implementation period).
Table 3.
Characteristics of Acute Care Hospitals* from Which Fee-for-Service Medicare Patients with COPD Were Discharged from December 2006 to November 2017 in the United States
| HRRP Periods | Preannouncement |
Announcement |
Implementation |
P Value† | |||
|---|---|---|---|---|---|---|---|
| December 2006 to July 2008 | August 2008 to March 2010 | April 2010 to November 2011 | January 2013 to August 2014 | October 2014 to April 2016 | May 2016 to November 2017 | ||
| Unique hospitals | 3,457 (100) | 3,392 (100) | 3,332 (100) | 3,296 (100) | 3,244 (100) | 3,172 (100) | — |
| Teaching hospital‡ | <0.0001 | ||||||
| Major/graduate | 601 (17.3) | 580 (17.1) | 575 (17.26) | 562 (17.05) | 562 (17.32) | 555 (17.5) | |
| Limited | 450 (13.02) | 471 (13.89) | 467 (14.02) | 501 (15.2) | 523 (16.1) | 541 (17.06) | |
| No affiliation | 2,376 (68.7) | 2,327 (68.6) | 2,289 (68.7) | 2,212 (67.1) | 2,129 (65.6) | 2,074 (65.3) | |
| Unknown | 30 (0.8) | 14 (0.4) | 1 (0.03) | 21 (0.6) | 30 (0.9) | 2 (0.06) | |
| Transplant Center | <0.0001 | ||||||
| Yes | 760 (21.9) | 748 (22.05) | 670 (20.1) | 584 (17.7) | 535 (16.4) | 528 (16.6) | |
| No | 2,667 (77.1) | 2,630 (77.5) | 2,661 (79.8) | 2,691 (81.6) | 2,679 (82.5) | 2,642 (83.2) | |
| Unknown | 30 (0.8) | 14 (0.4) | 1 (0.03) | 21 (0.6) | 30 (0.9) | 2 (0.06) | |
| Bed count | 0.0117 | ||||||
| <100 | 1,065 (30.8) | 1,057 (31.1) | 1,026 (30.7) | 988 (29.9) | 939 (28.9) | 908 (28.6) | |
| 100–250 | 1,218 (35.2) | 1,203 (35.4) | 1,183 (35.5) | 1,171 (35.5) | 1,167 (35.9) | 1,151 (36.2) | |
| 250–500 | 807 (23.3) | 780 (23) | 781 (23.4) | 771 (23.3) | 760 (23.4) | 761 (23.9) | |
| >500 | 337 (9.7) | 338 (9.9) | 341 (10.2) | 345 (10.4) | 348 (10.7) | 350 (11.03) | |
| Unknown | 30 (0.8) | 14 (0.4) | 1 (0.03) | 21 (0.6) | 30 (0.9) | 2 (0.06) | |
| Metro§ | <0.0001 | ||||||
| Metro | 2,427 (70.2) | 2,397 (70.6) | 2,369 (71.1) | 2,343 (71.0) | 2,310 (71.2) | 2,366 (74.5) | |
| Nonmetro | 921 (26.6) | 909 (26.8) | 886 (26.5) | 857 (26) | 830 (25.5) | 796 (25.09) | |
| Unknown | 109 (3.1) | 86 (2.5) | 77 (2.3) | 96 (2.9) | 104 (3.2) | 10 (0.3) | |
| Region | 0.5929 | ||||||
| Midwest | 754 (21.8) | 750 (22.1) | 745 (22.3) | 730 (22.1) | 723 (22.2) | 709 (22.3) | |
| Northeast | 544 (15.7) | 529 (15.6) | 511 (15.3) | 502 (15.2) | 489 (15.07) | 479 (15.1) | |
| South | 1,420 (41.0) | 1,408 (41.5) | 1,393 (41.8) | 1,367 (41.4) | 1,337 (41.2) | 1,319 (41.5) | |
| West | 654 (18.9) | 641 (18.9) | 630 (18.9) | 624 (18.9) | 612 (18.8) | 609 (19.2) | |
| Unknown | 85 (2.4) | 64 (1.8) | 53 (1.5) | 73 (2.2) | 83 (2.5) | 56 (1.7) | |
| Ownership|| | <0.0001 | ||||||
| Profit | 646 (18.6) | 629 (18.5) | 650 (19.5) | 671 (20.3) | 667 (20.5) | 669 (21.09) | |
| Nonprofit | 2,112 (61.0) | 2,089 (61.5) | 2,049 (61.4) | 2,009 (60.9) | 1,988 (61.2) | 1,988 (62.6) | |
| Government | 669 (19.3) | 660 (19.4) | 632 (18.9) | 595 (18.0) | 559 (17.2) | 513 (16.1) | |
| Unknown | 30 (0.87) | 14 (0.41) | 1 (0.03) | 21 (0.64) | 30 (0.92) | 2 (0.06) | |
| Full-time nurses per bed | <0.0001 | ||||||
| ≤1 | 1,944 (56.2) | 1,799 (53.0) | 1,678 (50.3) | 1,510 (45.8) | 1,407 (43.37) | 1,321 (41.6) | |
| >1 | 1,483 (42.9) | 1,579 (46.5) | 1,653 (49.6) | 1,765 (53.5) | 1,807 (55.7) | 1,849 (58.2) | |
| Unknown | 30 (0.8) | 14 (0.4) | 1 (0.03) | 21 (0.6) | 30 (0.9) | 2 (0.06) | |
| % of patients who gave high rating¶ | <0.0001 | ||||||
| <70% | 1,832 (52.9) | 2,473 (72.9) | 2,058 (61.7) | 1,656 (50.2) | 1,498 (46.1) | 1,231 (38.8) | |
| ≥70% | 450 (13.02) | 723 (21.3) | 1,121 (33.6) | 1,488 (45.1) | 1,592 (49.08) | 1,793 (56.5) | |
| Unknown | 1,175 (33.9) | 196 (5.7) | 153 (4.5) | 152 (4.6) | 154 (4.7) | 148 (4.6) | |
Definition of abbreviations: COPD = chronic obstructive pulmonary disease; HCAHPS = Hospital Consumer Assessment of Healthcare Providers and Systems; HRRP = Hospital Readmissions Reduction Program.
Data are expressed as n (%).
Hospital characteristics (except for patient rating) were collected from Centers for Medicare and Medicaid Services Provider of Service files 2007, 2009, 2011, 2013, 2015, and 2017 for the three periods.
Generalized estimating equation models were used to determine significance of trend over time for each characteristic.
Medical school affiliation involvement follows graduate > major > limited > no affiliation from most extensive to least. We grouped graduate and major in one category.
Hospital metro indicator was determined by county codes by the United States Department of Agriculture, Economic Research Service 2013 metro and nonmetro categories.
Hospital ownership categories defined in Table E3.
Patient ratings were collected from HCAHPS patient experience survey (36). We used HCAHPS: Patients’ Perspectives of Care Survey years 2008, 2009, 2011, 2013, 2015, and 2017 since the first public reporting of HCAHPS results occurred in March 2008.
Readmissions
The 30-day readmission rates after discharge from COPD hospitalization during the HRRP preannouncement, announcement, and implementation periods are presented in Figure 3 and Table 1. The 30-day readmission rate decreased from 20.54% in the preannouncement period (December 2006 to July 2008) to 18.74% in the implementation period (May 2016 to November 2017).
Readmission Adjusted by Hospital Characteristics
Overall, the 30-day readmission rate decreased from the preannouncement period (December 2006 to July 2008) to the implementation period (May 2016 to November 2017) for all hospital characteristics studied. There was a slight increase in the 30-day readmission rate during the implementation period compared with the announcement period (January 2013 to August 2014) for all hospitals irrespective of their medical school affiliation (Figure E1 in the online supplement and Tables E5 and E6), nurse-per-bed ratio (Figure E2 and Table E8), hospital rating (Figure E3 and Table E10), and hospital ownership (data not shown). However, the readmission rate was significantly lower in the nonprofit hospitals during the implementation period (May 2016 to November 2017) compared with for-profit hospitals (0.18%, P = 0.0195) (data not shown).
Mortality
The 30-day mortality rate was 6.91%, 6.59%, and 7.30% in the preannouncement (December 2006 to July 2008), announcement (April 2010 to November 2011), and implementation (May 2016 to November 2017) periods, respectively (Figure 3). The GEE model was used to account for clustering at the hospital level (Table 1) and showed a statistically significant decrease in 30-day mortality rate (0.33% decrease, P < 0.0001) between the preannouncement (December 2006 to July 2008) and announcement (April 2010 to November 2011) periods. Subsequently, the 30-day mortality rate significantly increased (0.12% increase, P < 0.0001) between the first part of the announcement period (April 2010 to November 2011) and the second part (January 2013 to August 2014). Finally, the 30-day mortality rate continued to increase during the implementation period (0.22% increase October 2014 to April 2016 and 0.71% increase May 2016 to November 2017) compared with the announcement period (April 2010 to November 2011) (Table 1).
Results of comparing the change in 30-day mortality rate between announcement and implementation show that the mortality rate increased faster in the implementation period (Table E4). Moreover, we estimated the number of additional deaths during the implementation period (1,196 deaths during October 2014 to April 2016 and 3,858 deaths during May 2016 to November 2017) compared with the announcement period (April 2010 to November 2011).
Mortality Adjusted by Hospital Characteristics
Mortality and medical school affiliation
Table E7 presents the 30-day mortality rates by hospitals’ medical school affiliation. There was an increase in 30-day mortality rate after discharge from a COPD hospitalization during the implementation period regardless of the hospital’s medical school affiliation (Figure E1). However, the change in mortality rate in the announcement and implementation periods differed significantly by degree of medical school affiliation. For example, hospitals with no medical school affiliation had a statistically significant increase in mortality rate (0.12% increase, P < 0.0001) in the second part of the announcement period (January 2013 to August 2014) and in the implementation period (0.26% increase, P < 0.0001 October 2014 to April 2016; 0.78% increase, P < 0.0001 May 2016 to November 2017) compared with the first part of the announcement period (April 2010 to November 2011). In contrast, hospitals with major/graduate teaching status had a significant increase in 30-day mortality (0.51% increase, P < 0.0001) only during the second part of the implementation period (May 2016 to November 2017) compared with the announcement period (April 2010 to November 2011).
We also compared the slope of increase in 30-day mortality rate, and the results show that, compared with the announcement period (April 2010 to November 2011), hospitals with no medical school affiliation increased in mortality rate faster compared with major/graduate teaching hospitals during the implementation period (difference in change 0.16%, P < 0.0272 October 2014 to April 2016; difference in change 0.27%, P < 0.0001 May 2016 to November 2017) (Table E7).
Mortality rate in hospitals by nurse-per-bed
The 30-day mortality rate increased during the implementation period compared with the announcement period (April 2010 to November 2011) for all hospitals irrespective of their nurse-per-bed status (Table E9). However, the mortality rate was significantly lower (0.21% lower, P < 0.0001) for hospitals with >1 nurse-per-bed compared with hospitals with ≤1 nurses-per-bed during the second part of the implementation period (May 2016 to November 2017). Lastly, compared with hospitals with >1 nurse-per-bed, hospitals with ≤1 nurses-per-bed increased in 30-day mortality faster (difference in change −0.2%, P < 0.001) during the implementation period (May 2016 to November 2017) compared with the announcement period (April 2010 to November 2011).
Mortality and hospital rating
The 30-day mortality rate increased significantly during the implementation period compared with the announcement period (April 2010 to November 2011) for hospitals, irrespective of their patient rating (Figure E3 and Table E11).
Mortality and hospital ownership
There was an increase in 30-day mortality rate after discharge from a COPD hospitalization in all hospitals regardless of their ownership type (government, profit, or not-for-profit) during HRRP implementation (October 2014 to November 2017) compared with the announcement period (April 2010 to November 2011). However, the slope of increase in mortality rate showed that, compared with non-for-profit hospitals, the mortality rate increased faster in for-profit hospitals in the implementation period (May 2016 to November 2017) compared with the announcement period (April 2010 to November 2011) (data not shown).
Discussion
We found that, among a large national cohort of Medicare fee-for-service beneficiaries 65 years and older discharged after a COPD hospitalization, the 30-day risk-standardized readmission rate decreased during the study period. There was an increase in 30-day risk-standardized postdischarge mortality rates during the same period.
Our findings show that 30-day readmission rates were trending down before the creation of the HRRP, and even before the initiation of penalties specific for COPD by the HRRP. These findings are consistent with previous research (11) and may reflect the efforts to improve overall readmission rates taken by hospitals in advance of the penalty phase of HRRP for COPD, to minimize readmission penalties (10). The readmission rate increased slightly during the period of implementation of penalties for COPD. One potential explanation could be that there is a ceiling effect for any intervention that reduces readmissions for chronic conditions such as COPD or congestive heart failure. Another possibility is that a subset of patients with COPD are frail, poor, with multiple comorbidities, and without family support. These patients may require hospitalizations within a 30-day period of a previous discharge. Repeated hospital visits by patients in this group could contribute to increased readmissions. Individuals in this cohort of high-risk older adults are referred to as “hospital-dependent patients” and represent a vulnerable population with chronic conditions (39). Recent studies suggest that traditional resources or interventions have failed to reduce “readmissions” in this at-risk population (10, 39).
We found that the trend in hospital 30-day readmission rates during the three periods of study was similar, irrespective of the hospital’s medical school affiliation, nurse-per-bed status, patient rating, or hospital ownership. Contrary to the homogeneous findings regarding readmission rates, hospital characteristics were significantly associated with changes in 30-day mortality across the three periods of study. Specifically, hospitals with major/graduate medical school affiliations saw no increase in 30-day mortality rates for COPD until the latter part of the HRRP implementation period (May 2016 to November 2017). Teaching hospitals also had lower mortality rates for COPD, and the increases in mortality rates were slower compared with those for nonteaching hospitals.
Our findings of an association between readmission and mortality rates associated with the HRRP are consistent with prior studies (10, 13, 40, 41) following heart failure (14), pneumonia (15), and COPD hospitalization (12). Our study examined the three periods necessary to understand the interaction between the stages of the HRRP and their impact on mortality. Our 30-day risk-standardized “postdischarge” mortality outcome was obtained by excluding patients who died during hospitalization (before hospital discharge). This method is contrary to how CMS calculates 30-day mortality rates (mortality within a 30-d period from the date of the index admission) (31, 33). To compare our outcome with how CMS calculates 30-day mortality rates, we fitted an independent risk-adjusted model for mortality that includes in-hospital death and counted 30 days from admission. The results show a similar trend as in our current model (Tables E12 and E13 and Figure E4). Our findings related to the difference in 30-day mortality rates between hospitals by medical school affiliation and between teaching and nonteaching hospitals are important areas for future research, for example, whether the difference in mortality trends between teaching and nonteaching hospitals is also true for other HRRP diagnostic conditions such as stroke.
The benefits of the HRRP to improve health, prevent unnecessary hospitalizations, and control Medicare spending have been widely discussed and debated. An important concern is the impact of the HRRP on safety-net hospitals (42–44). Efforts to avoid financial penalties by reducing readmissions are often focused on minority and disadvantaged patients. Not only are these patients at higher risk for readmission, they may also be at higher risk for mortality (45, 46). CMS adjusted the formula by which penalties are assigned to safety-net hospitals beginning in fiscal year 2019. The change incorporates Medicaid eligibility as a surrogate for socioeconomic status. Although this change is a step in the right direction, balancing readmissions and mortality measures by CMS in the HRRP penalty formula may be the next step and is another area that deserves future research.
Medicare data allow us to capture a majority of patients with COPD in the nation, as this is predominantly a disease of older adults. The longitudinal nature of this study allowed us to observe the trend in hospital baseline readmission and mortality rates (after COPD discharge) before and after the development and implementation of the HRRP.
Despite these strengths, our study has limitations. The data source, 100% Medicare beneficiary study files, includes only fee-for-service inpatient claims (Medicare Provider Analysis and Review) and not Medicare Part B claims. Thus, the sample was not representative of all Medicare beneficiaries and the patient comorbidities used in risk standardization were underestimated. Our data also do not include hospice claims files. In our cohort selection, we could not strictly follow the CMS mortality report to exclude patients with hospice stays in the 12 months before admission. Although recent studies have suggested an increase in hospice use in patients with COPD over time (47, 48), this increase may be related to an increase in hospital discharges of very ill patients with COPD to hospice (49). Failing to exclude hospice patients could potentially influence mortality rates. To minimize this limitation, we excluded direct transfers from hospice. Finally, our data have two separate, unlinkable Data Use Agreements for before and after 2012. Patients admitted in 2012 could not be cross-linked to the previous year and were thus excluded. However, we have data before and after this period, and our findings are directionally correct.
Conclusions
We examined the trajectory of the CMS HRRP for patients hospitalized with COPD from 2006 through 2017 using a large national cohort of Medicare fee-for-service beneficiaries. We found a reduction in the 30-day all-cause readmission rate during the implementation period compared with the preannouncement phase. HRRP implementation for COPD was also associated with a significant increase in 30-day risk-standardized postdischarge mortality. Additional research is necessary to confirm our findings and identify factors contributing to increased mortality in patients with COPD in the CMS readmission reduction program.
Supplementary Material
Acknowledgments
Acknowledgment
The authors thank Sarah Toombs Smith, Ph.D., E.L.S., Tara N. Atkins, M.L.I.S., and Matthew Lakich, M.P.H., for their assistance in the preparation of this manuscript.
Footnotes
Y.-F.K. reports grants from the University of Texas Medical Branch Claude D. Pepper Older Americans Independence Center and grants from the Agency of Healthcare Research and Quality during the conduct of the study. K.J.O. reports grants from the NIH during the conduct of the study.
Author Contributions: All authors have contributed to the current manuscript in the following manner: substantial contribution to the conception, design, data acquisition, analysis, and interpretation of the manuscript; drafted and/or revised the manuscript for important intellectual content; approved the final version to be submitted for publication; and agreed to be accountable for all aspects of the work and have ensured that questions related to the accuracy and integrity of any part of the manuscript are appropriately investigated and resolved.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.202002-0310OC on September 1, 2020
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Murphy SL, Xu J, Kochanek KD, Arias E. Mortality in the United States, 2017. NCHS Data Brief. 2018;328:1–8. [PubMed] [Google Scholar]
- 2.Wier LM, Elixhauser A, Pfuntner A, Au DH. Rockville, MD: Agency for Health Care Policy and Research; 2006. Overview of hospitalizations among patients with COPD, 2008: statistical brief# 106. In: Healthcare cost and Utilization Project (HCUP) statistical briefs. [PubMed] [Google Scholar]
- 3.Sharif R, Parekh TM, Pierson KS, Kuo YF, Sharma G. Predictors of early readmission among patients 40 to 64 years of age hospitalized for chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2014;11:685–694. doi: 10.1513/AnnalsATS.201310-358OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jacobs DM, Noyes K, Zhao J, Gibson W, Murphy TF, Sethi S, et al. Early hospital readmissions after an acute exacerbation of chronic obstructive pulmonary disease in the Nationwide Readmissions Database. Ann Am Thorac Soc. 2018;15:837–845. doi: 10.1513/AnnalsATS.201712-913OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah T, Press VG, Huisingh-Scheetz M, White SR. COPD readmissions: addressing COPD in the era of value-based health care. Chest. 2016;150:916–926. doi: 10.1016/j.chest.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lindenauer PK, Dharmarajan K, Qin L, Lin Z, Gershon AS, Krumholz HM. Risk trajectories of readmission and death in the first year after hospitalization for chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;197:1009–1017. doi: 10.1164/rccm.201709-1852OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 8.US Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP) CMS [modified Feb 2020; accessed 2020 Apr 23]. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.
- 9.US Centers for Medicare & Medicaid Services. New stratified methodology hospital-level impact file user guide: hospital readmissions reduction program. CMS [modified Nov 2019; accessed 2020 Apr 24]. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Archived-Supplemental-Data-Files/HRRP-New-Stratified-Methodology-Hospital-Level-Impact-Files.
- 10.Desai NR, Ross JS, Kwon JY, Herrin J, Dharmarajan K, Bernheim SM, et al. Association between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. JAMA. 2016;316:2647–2656. doi: 10.1001/jama.2016.18533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Myers LC, Faridi MK, Hasegawa K, Hanania NA, Camargo CA., Jr The Hospital Readmissions Reduction Program and readmissions for chronic obstructive pulmonary disease, 2006–2015. Ann Am Thorac Soc. 2020;17:450–456. doi: 10.1513/AnnalsATS.201909-672OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Samarghandi A, Qayyum R. Effect of Hospital Readmission Reduction Program on hospital readmissions and mortality rates. J Hosp Med. 2019;14:E25–E30. doi: 10.12788/jhm.3302. [DOI] [PubMed] [Google Scholar]
- 13.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374:1543–1551. doi: 10.1056/NEJMsa1513024. [DOI] [PubMed] [Google Scholar]
- 14.Gupta A, Allen LA, Bhatt DL, Cox M, DeVore AD, Heidenreich PA, et al. Association of the Hospital Readmissions Reduction Program implementation with readmission and mortality outcomes in heart failure. JAMA Cardiol. 2018;3:44–53. doi: 10.1001/jamacardio.2017.4265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the Hospital Readmissions Reduction Program with mortality among Medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. JAMA. 2018;320:2542–2552. doi: 10.1001/jama.2018.19232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Auerbach AD, Kripalani S, Vasilevskis EE, Sehgal N, Lindenauer PK, Metlay JP, et al. Preventability and causes of readmissions in a national cohort of general medicine patients. JAMA Intern Med. 2016;176:484–493. doi: 10.1001/jamainternmed.2015.7863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rinne ST, Castaneda J, Lindenauer PK, Cleary PD, Paz HL, Gomez JL. Chronic obstructive pulmonary disease readmissions and other measures of hospital quality. Am J Respir Crit Care Med. 2017;196:47–55. doi: 10.1164/rccm.201609-1944OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shah T, Churpek MM, Coca Perraillon M, Konetzka RT. Understanding why patients with COPD get readmitted: a large national study to delineate the Medicare population for the readmissions penalty expansion. Chest. 2015;147:1219–1226. doi: 10.1378/chest.14-2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh G, Zhang W, Kuo YF, Sharma G. Association of psychological disorders with 30-day readmission rates in patients with COPD. Chest. 2016;149:905–915. doi: 10.1378/chest.15-0449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buhr RG, Jackson NJ, Dubinett SM, Kominski GF, Mangione CM, Ong MK. Factors associated with differential readmission diagnoses following acute exacerbations of chronic obstructive pulmonary disease. J Hosp Med. 2020;15:219–227. doi: 10.12788/jhm.3367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buhr RG, Jackson NJ, Kominski GF, Dubinett SM, Ong MK, Mangione CM. Comorbidity and thirty-day hospital readmission odds in chronic obstructive pulmonary disease: a comparison of the Charlson and Elixhauser comorbidity indices. BMC Health Serv Res. 2019;19:701. doi: 10.1186/s12913-019-4549-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walker PP, Pompilio PP, Zanaboni P, Bergmo TS, Prikk K, Malinovschi A, et al. Telemonitoring in chronic obstructive pulmonary disease (CHROMED): a randomized clinical trial. Am J Respir Crit Care Med. 2018;198:620–628. doi: 10.1164/rccm.201712-2404OC. [DOI] [PubMed] [Google Scholar]
- 23.Press VG, Au DH, Bourbeau J, Dransfield MT, Gershon AS, Krishnan JA, et al. Reducing chronic obstructive pulmonary disease hospital readmissions: an official American Thoracic Society Workshop report. Ann Am Thorac Soc. 2019;16:161–170. doi: 10.1513/AnnalsATS.201811-755WS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McHugh MD, Berez J, Small DS. Hospitals with higher nurse staffing had lower odds of readmissions penalties than hospitals with lower staffing. Health Aff (Millwood) 2013;32:1740–1747. doi: 10.1377/hlthaff.2013.0613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhatt SP, Wells JM, Iyer AS, Kirkpatrick DP, Parekh TM, Leach LT, et al. Results of a Medicare bundled payments for care improvement initiative for chronic obstructive pulmonary disease readmissions. Ann Am Thorac Soc. 2017;14:643–648. doi: 10.1513/AnnalsATS.201610-775BC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marchetti N, Criner GJ, Albert RK. Preventing acute exacerbations and hospital admissions in COPD. Chest. 2013;143:1444–1454. doi: 10.1378/chest.12-1801. [DOI] [PubMed] [Google Scholar]
- 27.Effing T, Monninkhof EM, van der Valk PD, van der Palen J, van Herwaarden CL, Partidge MR, et al. Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2007;(4):CD002990. doi: 10.1002/14651858.CD002990.pub2. [DOI] [PubMed] [Google Scholar]
- 28.Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174:1095–1107. doi: 10.1001/jamainternmed.2014.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prieto-Centurion V, Markos MA, Ramey NI, Gussin HA, Nyenhuis SM, Joo MJ, et al. Interventions to reduce rehospitalizations after chronic obstructive pulmonary disease exacerbations: a systematic review. Ann Am Thorac Soc. 2014;11:417–424. doi: 10.1513/AnnalsATS.201308-254OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Puebla Neira D, Kuo Y, Hsu E, Sharma G. Association of the Hospital Readmissions Reduction Program implementation with 30 day mortality outcomes in patients with chronic obstructive pulmonary disease [abstract] Am J Respir Crit Care Med. 2020;201:A5952. [Google Scholar]
- 31.US Centers for Medicare & Medicaid Services. Hospital-level 30-day mortality following admission for an acute exacerbation of chronic obstructive pulmonary disease: measure methodology report, version 1 (2011) CMS [modified Feb 2020; accessed 2020 Apr 24]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.
- 32.US Centers for Medicare & Medicaid Services. Condition-specific measures updates and specifications report hospital-level 30-day risk-standardized readmission measures. 2018. [accessed 2020 Apr 24]. Available from: https://qualitynet.cms.gov/inpatient/measures/readmission/methodology.
- 33.US Centers for Medicare & Medicaid Services. Condition-specific measures updates and specifications report hospital-level 30-day risk-standardized mortality measures. 2018. [accessed 2020 Apr 24]. Available from: https://qualitynet.cms.gov/inpatient/measures/mortality/methodology.
- 34.Healthcare Cost and Utilization Project. Clinical Classifications Software (CCS) for ICD-9-CM Fact Sheet. H-CUP [modified Jan 2012; accessed 2020 Feb 11]. Available from: https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccsfactsheet.jsp.
- 35.US Centers for Medicare & Medicaid Services. Provider of services current files. CMS [last modified Jul 2020; accessed 2020 Apr 24]. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Provider-of-Services.
- 36.US Centers for Medicare & Medicaid Services. Hospital consumer assessment of healthcare providers and systems: patients’ perspectives of care survey. CMS [modified Feb 2020; accessed 2020 Apr 23]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS.
- 37.Giordano LA, Elliott MN, Goldstein E, Lehrman WG, Spencer PA. Development, implementation, and public reporting of the HCAHPS survey. Med Care Res Rev. 2010;67:27–37. doi: 10.1177/1077558709341065. [DOI] [PubMed] [Google Scholar]
- 38.United States Department of Agriculture. Rural-urban continuum codes. USDA [modified Oct 2019; accessed 2020 Apr 24]. Available from: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation/
- 39.Finkelstein A, Zhou A, Taubman S, Doyle J. Health care hotspotting - a randomized, controlled trial. N Engl J Med. 2020;382:152–162. doi: 10.1056/NEJMsa1906848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wasfy JH, Zigler CM, Choirat C, Wang Y, Dominici F, Yeh RW. Readmission rates after passage of the Hospital Readmissions Reduction Program: a pre–post analysis. Ann Intern Med. 2017;166:324–331. doi: 10.7326/M16-0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ibrahim AM, Nathan H, Thumma JR, Dimick JB. Impact of the Hospital Readmission Reduction Program on surgical readmissions among Medicare beneficiaries. Ann Surg. 2017;266:617–624. doi: 10.1097/SLA.0000000000002368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Favini N, Hockenberry JM, Gilman M, Jain S, Ong MK, Adams EK, et al. Comparative trends in payment adjustments between safety-net and other hospitals since the introduction of the hospital readmission reduction program and value-based purchasing. JAMA. 2017;317:1578–1580. doi: 10.1001/jama.2017.1469. [DOI] [PubMed] [Google Scholar]
- 43.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309:342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 44.Bazzoli GJ, Thompson MP, Waters TM. Medicare payment penalties and safety net hospital profitability: minimal impact on these vulnerable hospitals. Health Serv Res. 2018;53:3495–3506. doi: 10.1111/1475-6773.12833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Feemster LC, Au DH. Penalizing hospitals for chronic obstructive pulmonary disease readmissions. Am J Respir Crit Care Med. 2014;189:634–639. doi: 10.1164/rccm.201308-1541PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abdul-Aziz AA, Hayward RA, Aaronson KD, Hummel SL. Association between Medicare hospital readmission penalties and 30-day combined excess readmission and mortality. JAMA Cardiol. 2017;2:200–203. doi: 10.1001/jamacardio.2016.3704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Iyer AS, Goodrich CA, Dransfield MT, Alam SS, Brown CJ, Landefeld CS, et al. End-of-life spending and healthcare utilization among older adults with chronic obstructive pulmonary disease. Am J Med. 2020;137:817–824, e1. doi: 10.1016/j.amjmed.2019.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yaqoob ZJ, Al-Kindi SG, Zein JG. Trends and disparities in hospice use among patients dying of COPD in the United States. Chest. 2017;151:1183–1184. doi: 10.1016/j.chest.2017.02.030. [DOI] [PubMed] [Google Scholar]
- 49.Schorr CA, Angelo M, John G, LeCompte K, Dellinger RP. The association of increasing hospice use with decreasing hospital mortality: an analysis of the national inpatient sample. J Healthc Manag. 2020;65:107–120. doi: 10.1097/JHM-D-18-00280. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.