Abstract
Objective
To use medical claims data to determine patterns of healthcare utilization in children with intellectual and developmental disabilities, including frequency of service utilization, conditions that require hospital care, and costs.
Study design
Medicaid administrative claims from 4 states (Iowa, Massachusetts, New York, and South Carolina) from years 2008-2013 were analyzed, including 108 789 children (75 417 male; 33 372 female) under age 18 years with intellectual and developmental disabilities. Diagnoses included cerebral palsy, autism, fetal alcohol syndrome, Down syndrome/trisomy/autosomal deletions, other genetic conditions, and intellectual disability. Utilization of emergency department (ED) and inpatient hospital services were analyzed for 2012.
Results
Children with intellectual and developmental disabilities used both inpatient and ED care at 1.8 times that of the general population. Epilepsy/convulsions was the most frequent reason for hospitalization at 20 times the relative risk of the general population. Other frequent diagnoses requiring hospitalization were mood disorders, pneumonia, paralysis, and asthma. Annual per capita expenses for hospitalization and ED care were 100% higher for children with intellectual and developmental disabilities, compared with the general population ($153 348 562 and $76 654 361, respectively).
Conclusions
Children with intellectual and developmental disabilities utilize significantly more ED and inpatient care than other children, which results in higher annual costs. Recognizing chronic conditions that increase risk for hospital care can provide guidance for developing outpatient care strategies that anticipate common clinical problems in intellectual and developmental disabilities and ensure responsive management before hospital care is needed.
Over $233 billion is spent annually on healthcare for children in the US,1 but little is known about specific patterns of healthcare utilization for children with intellectual and developmental disabilities. Although there is evidence that children and adults with intellectual and developmental disabilities show high overall healthcare needs and associated costs,2,3 accurate data based on systematic surveillance of the health of people with intellectual and developmental disabilities are lacking.4 Obtaining critical information that can guide management of complex conditions outside of hospital settings may enable many children with intellectual and developmental disabilities to avoid expensive emergency care or hospitalization.
Evidence to date suggests that people with intellectual and developmental disabilities use substantially more healthcare services2,5 with evidence that some subgroups may present with more urgent care needs6 while others may be less likely to present with urgent needs.7 Despite the increased utilization, people with intellectual and developmental disabilities experience poorer health outcomes,2,8,9 poorer quality of care,10,11 and potentially avoidable gaps or excesses in utilization patterns.12 In addition, evidence for adults suggests they experience limited access to key components of primary healthcare13 including preventive healthcare14 and management of chronic conditions,14 and timely ambulatory care.12,13
Developmental disabilities affect 3 or more areas of major life activity: self-care, receptive or expressive language, learning, mobility, self-direction, capacity for independent living, and economic self-sufficiency.15 Children with developmental disabilities are expected to need supports and services of extended duration, often including individualized planning and care coordination.15 The most common conditions or subtypes associated with developmental disabilities include intellectual disability, cerebral palsy, autism spectrum disorder (ASD), fetal alcohol syndrome/spectrum, and Down syndrome and other genetic conditions.16 Using a broad definition of developmental disabilities, the prevalence was estimated at 7% in 2016.17
Intellectual disability involves significant limitations in both intellectual functioning and adaptive behavior, which includes many social and practical skills that manifest before the age of 18 years.18 Intellectual functioning includes capabilities in reasoning, learning, and problem solving. Adaptive behavior refers to the conceptual, practical, and social skills that are learned and performed by people in their daily lives. An estimate of the prevalence of intellectual disability in US children from birth through age 17 years is 1.2%.17 The prevalence of intellectual and developmental disabilities in the current study, which used a definition based on the most common developmental disabilities including intellectual disability, autism spectrum disorder, cerebral palsy, fetal alcohol syndrome, Down syndrome, and other genetic conditions, is estimated to be 2.3%-4.2% in the total Medicaid population.16
Because limited data are available with which to conduct systematic surveillance of the health of people with intellectual and developmental disabilities, this study used Medicaid claims data on children in 4 states as 1 source of secondary data available to states to describe patterns of hospitalization and emergency department (ED) use of patients with intellectual and developmental disabilities, and the costs associated with this care. We hypothesized that Medicaid members with intellectual and developmental disabilities would use both ED and inpatient hospital care at higher rates than the general population and that many of the most frequent medical conditions that result in hospital care for this population are ones that could potentially to be managed effectively on an outpatient basis (eg, ambulatory care sensitive conditions). This hypothesis was informed in part by the nature of the functional limitations frequently observed in people with intellectual and developmental disabilities that may limit their ability to report signs and symptoms ofillness and a dependence on others to seek and successfully access medical care.
Methods
Administrative data from the Medicaid Management Information System (MMIS) was used in this analysis from each of four states with expertise in analysis of intellectual and developmental disabilities: Iowa, Massachusetts, New York, and South Carolina. MMIS data included Medicaid enrollment and service claims, including both fee-for-service claims and managed care encounters containing International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes.19 Data usage approvals were obtained according to the procedures for each state MMIS system. When required, protection procedures for human subjects were reviewed and approved by Institutional Review Boards. Only aggregate results were shared among states. SAS v 9.4 (SAS Institute Inc, Cary, North Carolina) or Oracle SQL Developer (Oracle Corporation, Redwood Shores, California) was used to conduct analyses.
Identification of Medicaid Members with Intellectual and Developmental Disabilities
MMIS data from a prestudy case-finding period of 2008-2013 were used to identify cohorts of children (ages 0-17 years) with intellectual and developmental disabilities. Because Medicaid programs and MMIS data elements can vary by state, state teams identified coding methods that resulted in comparable cross-state cohorts. A standardized algorithm was applied to each state’s MMIS data to define the cohort.16 Children enrolled at least 11 months out of 1 or more calendar years between 2008 and 2013 were included. Children with commercial insurance coverage in addition to Medicaid were excluded. To be eligible for this analysis, children needed to have service utilization (inpatient, ED, outpatient, etc) associated with ICD-9-CM diagnostic codes that matched the list of intellectual and developmental disabilities diagnoses generated for this project, selected because of their close association with functional limitations that define developmental disability.16 Filtering criteria requiring multiple service claims were used to rule out utilization related to suspected but unconfirmed diagnoses; claims data were bundled at the claim level to prevent duplicate counting of a single visit.
Because most members of the identified cohort had more than 1 intellectual and developmental disability-related ICD-9-CM code during the 5-year study period, a hierarchy was used to assign each child to a single diagnostic subgroup beginning with the most specific diagnosis (eg, genetic causes) to the least specific diagnosis (unspecified intellectual disability).16 Eight mutually exclusive diagnostic subgroups were identified: Down syndrome/trisomy/autosomal deletions; other genetic conditions, such as Lesch-Nyhan, tuberous sclerosis, fragile X syndrome, and Prader-Willi syndrome; fetal alcohol syndrome; cerebral palsy; autism or pervasive developmental disorder; mild intellectual disability; moderate-to-profound intellectual disability; and unspecified intellectual disability.
Demographic Variables
The following variables were used to describe the sample of children with intellectual and developmental disabilities: first age recorded during the study period, sex (male/female), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other, unknown), and mean number of years enrolled in Medicaid during the study period. Complete information regarding race/ethnicity could not be documented consistently across all 4 states because race/ethnicity is an optional variable in reporting Medicaid administrative data.
Hospital Utilization
The study analyzed encounters during the calendar year of 2012 for both inpatient hospital admissions and outpatient ED visits. Inpatient admissions to extended-stay psychiatric facilities were excluded, as well as encounters with lengths of stay over 25 days, to ensure that inpatient stays were focused on acute care. Maternal and neonatal inpatient stays were also excluded. Encounters where a child was admitted from an ED visit were considered primarily inpatient admissions and were not counted in the outpatient ED utilization rates.
The primary ICD-9-CM codes for inpatient admission and outpatient ED utilization were categorized utilizing the Clinical Classifications Software (CCS), a system of standardized, clinically meaningful categories used to organize diagnoses and procedures in ICD-9-CM developed by the Agency for Healthcare Research and Quality as part of the Healthcare Cost and Utilization Project (HCUP).20 Multilevel CCS hierarchical categories were used to organize the diagnoses given in the inpatient and ED settings into larger aggregations of clinically relevant groups.
Benchmarks for Comparisons of Relative Risk
Two sources of benchmarks were used to compare the patterns of utilization in the intellectual and developmental disability child cohort to children in the general US population. For inpatient admissions, discharge data from the 2012 HCUP National Inpatient Sample (NIS)21 provided the benchmark. To maintain consistent methodology with the intellectual and developmental disability cohort, maternal and neonatal inpatient stays were excluded. For ED visits, outpatient ED discharges in the 2012 HCUP Nationwide Emergency Department Sample (NEDS)13 provided a benchmark. Both the NIS and NEDS use the same CCS hierarchical categories for organization of ICD-9-CM codes, permitting direct comparison of diagnostic groups between the intellectual and developmental disability cohort and the general population of US children.
Relative risks (RRs) and 95% CIs were calculated as rate ratios using rates per 1000 of utilization in the intellectual and developmental disability cohort as numerators and utilization in the general US child population as the denominators, based on the appropriate HCUP benchmarks for the year 2012. RRs were used as a measure of association in this study because of their robust ability to estimate association regardless of the frequency of the outcome.
Results
Identifying Children with Intellectual and Developmental Disabilities
A total of 4 373 694 children (ages 0-17 years) met Medicaid enrollment criteria in the 4 participating states for during the prestudy case-finding period of 2008-2013. Using the hierarchy of subgroups for intellectual and developmental disabilities, we identified a cohort of 108 789 children with intellectual and developmental disabilities, which represents an intellectual and developmental disabilities child prevalence of 2.49%. Table I includes descriptive characteristics of the cohort of children with intellectual and developmental disabilities. The cohort had 15 417 inpatient admissions in the study year of 2012, with 5.1% of children having one admission, 1.4% having 2 admissions, and 1.1% having three admissions during this period; most children (92.4%) did not have any admissions. The cohort’s outpatient ED utilization in 2012 included 71 231 visits, with 65.7% of children having no outpatient ED visits, 19.5% having 1 visit, 7.7% having 2 visits, 3.5% having 3 visits, 1.7% having 4 visits, and 2.0% having 5 or more visits during the year.
Table I.
Descriptive characteristics of children with intellectual and developmental disabilities and medical claims paid by Medicaid in 4 US states
| Categories | n | % of Sample |
|---|---|---|
| Age (y) | ||
| <1 | 1825 | 1.7 |
| 1-2 | 10 137 | 9.3 |
| 3-6 | 29 947 | 27.5 |
| 7-12 | 40 220 | 37.0 |
| 13-17 | 26 660 | 24.5 |
| Sex | ||
| Male | 75 417 | 69.3 |
| Female | 33 371 | 30.7 |
| Race | ||
| White | 40 269 | 37.0 |
| Black | 20 665 | 19.0 |
| Hispanic | 20 638 | 19.0 |
| Other | 5929 | 5.4 |
| Unknown | 21 288 | 19.6 |
| Intellectual and developmental disability condition (using group hierarchy) | ||
| Down syndrome/trisomy/autosomal deletions | 8099 | 7.4 |
| Other genetic causes | 2045 | 1.9 |
| Fetal alcohol syndrome | 964 | 0.9 |
| Cerebral palsy | 12 301 | 11.3 |
| Autism spectrum disorders | 51 121 | 47.0 |
| Intellectual disability (all levels) | 34 259 | 31.5 |
Medical Conditions Frequently Associated with Hospitalization
Table II shows the 15 medical conditions that accounted for over one-half (8145) of the intellectual and developmental disability cohort’s total admissions in 2012. Epilepsy/convulsions was the most common admission-related diagnosis, followed by mood disorders, pneumonia, paralysis, and asthma. Both pediatric asthma and bacterial pneumonia are considered ambulatory care-sensitive conditions (ACSCs)23,24 that should be responsive to community-based care and should not require hospitalization when managed well.25 When compared with utilization rates in the general population of US children, all 15 conditions representing the most frequent reasons for hospital admissions in children with intellectual and developmental disabilities were associated with RRs of hospitalization significantly higher than 1.0 (P < .0001). Hospitalizations related to epilepsy/convulsions, paralysis, behavior disorders, hereditary central nervous system (CNS) disorders, or aspiration pneumonitis were each >19 times more likely to occur in children with intellectual and developmental disabilities than for children in the general US population. In some cases, a diagnosis that was used to select the intellectual and developmental disabilities cohort (eg, cerebral palsy) was also closely associated with a condition that was a frequent reason for hospitalization (eg, paralysis), which meant that the reason for hospitalization was not always independent of the original intellectual and developmental disabilities diagnosis.
Table II.
Medical conditions most frequently associated with health service utilization in children with intellectual and developmental disabilities
| Inpatient hospitalizations | ||||||
|---|---|---|---|---|---|---|
| Rank for intellectual and developmental disabilities cohort | CCS code | CCS description | Total admissions | Rate per 1000 | RR* | 95% CI |
| 1 | 83 | Epilepsy/convulsions | 1879 | 17.3 | 19.43 | 18.56-20.34 |
| 2 | 657 | Mood disorders | 941 | 8.6 | 6.19 | 5.80-6.60 |
| 3 | 122 | Pneumonia | 791 | 7.3 | 4.59 | 4.28-4.92 |
| 4 | 82 | Paralysis | 615 | 5.7 | 224.02 | 204.50-245.41 |
| 5 | 128 | Asthma | 608 | 5.6 | 3.60 | 3.33-3.90 |
| 6 | 55 | Fluid/electrolyte disorder | 436 | 4.0 | 6.57 | 5.98-7.22 |
| 7 | 217 | Other congenital anomaly | 430 | 4.0 | 9.56 | 8.69-10.52 |
| 8 | 652 | Behavior disorders | 395 | 3.6 | 23.51 | 21.26-25.99 |
| 9 | 58 | Other nutrition disorder | 378 | 3.5 | 16.86 | 15.22-18.67 |
| 10 | 125 | Bronchitis | 355 | 3.3 | 2.08 | 1.87-2.31 |
| 11 | 237 | Implant/graft complication | 322 | 3.0 | 9.15 | 8.20-10.22 |
| 12 | 126 | Upper respiratory infection | 259 | 2.4 | 4.87 | 4.31-5.51 |
| 13 | 81 | Other hereditary CNS | 254 | 2.3 | 37.70 | 33.22-42.78 |
| 14 | 129 | Aspiration pneumonitis | 247 | 2.3 | 34.12 | 30.02-38.77 |
| 15 | 155 | Other GI disorder | 235 | 2.2 | 8.48 | 7.45-9.64 |
| Outpatient ED care | ||||||
| Rank for intellectual and developmental disabilities cohort | CCS code | CCS description | Total ED visits | Rate per 1000 | RR† | 95% CI |
| 1 | 126 | Other upper respiratory infection | 7114 | 65.4 | 1.51 | 1.47-1.54 |
| 2 | 239 | Superficial injury/contusion | 3787 | 34.8 | 1.51 | 1.47-1.56 |
| 3 | 92 | Otitis media | 3542 | 32.6 | 1.58 | 1.52-1.63 |
| 4 | 246 | Unknown origin fever | 3201 | 29.4 | 1.77 | 1.71-1.83 |
| 5 | 244 | Other injury/condition | 2824 | 26.0 | 1.67 | 1.61-1.73 |
| 6 | 7 | Viral infection | 2727 | 25.1 | 2.09 | 2.02-2.17 |
| 7 | 83 | Epilepsy/convulsions | 2658 | 24.4 | 7.58 | 7.29-7.87 |
| 8 | 128 | Asthma | 2473 | 22.7 | 2.44 | 2.34-2.54 |
| 9 | 235 | Open wound head/trunk | 2171 | 20.0 | 1.32 | 1.27-1.38 |
| 10 | 250 | Nausea/vomiting | 2127 | 19.6 | 2.00 | 1.92-2.09 |
| 11 | 155 | Other GI disorder | 2114 | 19.4 | 2.84 | 2.72-2.96 |
| 12 | 133 | Other lower respiratory disease | 1734 | 15.9 | 2.36 | 2.25-2.47 |
| 13 | 232 | Sprain/strain | 1571 | 14.4 | 0.95‡ | 0.91-1.00 |
| 14 | 652 | Behavior disorders | 1485 | 13.7 | 14.95 | 14.20-15.74 |
| 15 | 253 | Allergic reaction | 1443 | 13.3 | 1.37 | 1.30-1.44 |
GI, gastrointestinal.
All 15 diagnoses were associated with significantly higher RR of hospitalization (P < .0001) in the cohort with intellectual and developmental disabilities than in the benchmark population of US children (HCUP NIS21).
All diagnoses except sprain/strain were associated with significantly higher RR of ED care (P < .0001) in the cohort with intellectual and developmental disabilities than in the benchmark population of US children (HCUP NEDS22).
P = .06.
The 15 most frequent diagnoses resulting in hospitalization for children with intellectual and developmental disabilities were also grouped according to the domains of the ICD-9-CM.20 The Figure shows that 50% of these admissions were related to either CNS dysfunction or mental health conditions. Admissions associated with respiratory system diagnoses were also frequent (28%).
Figure.
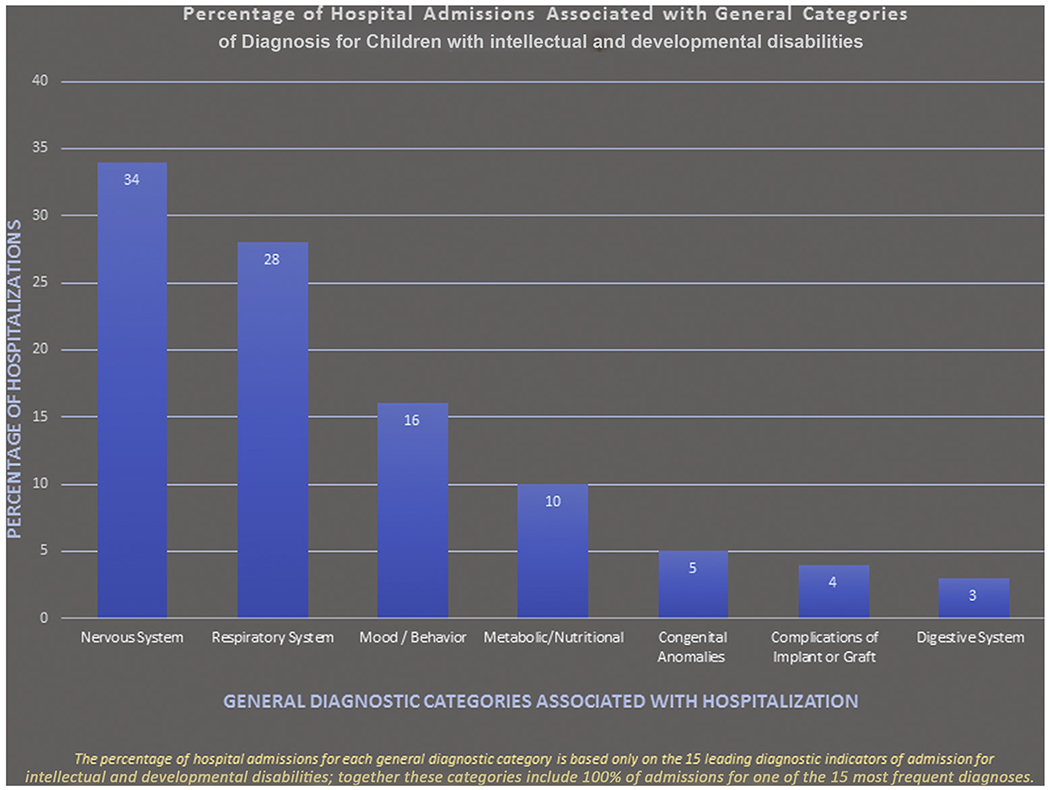
Percentage of hospital admissions associated with general categories of diagnosis for children with intellectual and developmental disabilities
Medical Conditions Frequently Associated with Outpatient Emergency Care
The conditions most frequently associated with outpatient ED utilization for children with intellectual and developmental disabilities are listed in Table II. These 15 diagnoses accounted for 58% of the cohort’s annual outpatient ED visits (40 971 out of 71231 visits). The 5 most frequent conditions leading to outpatient ED care were upper respiratory infections, superficial injury/contusions, otitis media, fevers, or other injuries/conditions. All but one of the top 15 conditions associated with outpatient ED services were present at a significantly higher RR (P < .0001) compared with the general population. Two conditions, epilepsy/convulsions and behavior disorders, were more than 7 times as likely to require outpatient ED care for children with intellectual and developmental disabilities compared with the general population.
Costs of Hospital Inpatient and Outpatient ED Care
Table III shows the costs of outpatient ED care and inpatient hospitalization for children with intellectual and developmental disabilities compared with national benchmarks for hospital costs in HCUP NIS21 and HCUP NEDS.22 These comparisons show that the pediatric intellectual and developmental disability cohort utilizes inpatient care at 1.8 times the rate (ie, 80% more utilization) of the US general population of children. Hospitalization for children with intellectual and developmental disabilities is also associated with higher costs per hospital stay, with average claims per admission costing 35% more than the HCUP benchmarks for children in the general population ($8690 vs $6415). The total inpatient costs paid by Medicaid in 2012 for the 108 789 children with intellectual and developmental disabilities in the 4-state sample in this analysis was $133 973 730, which is $78 841 097 (143%) higher than the estimated expenditures for inpatient care provided to a comparable number of children from the general population.
Table III.
Costs of outpatient emergency and inpatient hospitalization in children with intellectual and developmental disabilities
| Cohort with intellectual and developmental disabilities |
General child population |
||||
|---|---|---|---|---|---|
| Type of care | Number of visits | Visit rate per child | Cost per visit | Benchmark visit rate per child | Benchmark cost per visit |
| Inpatient hospitalization | 15 417 | 0.142 | $8690 | 0.079 | $6415 |
| Outpatient ED care | 71 231 | 0.655 | $272 | 0.365 | $542 |
Benchmarks are based on 2012 data for the US population ages 0-17 years from the HCUP NIS21 and the HCUP NEDS.22 The cost per visit benchmark for ED care is based on data from the Agency for Healthcare Research and Quality, Center for Financing, Access, and Cost Trends, Medical Expenditure Panel Survey.26
With respect to outpatient ED care, the pediatric intellectual and developmental disability cohort’s utilization rate was also 1.8 times that of the general population of children in the US; there were 655 annual outpatient ED visits per thousand children with intellectual and developmental disabilities compared with 365 annual visits per thousand for children in the general population. Paid claims for children with intellectual and developmental disabilities cost 50% less on average ($272 vs $542) compared with benchmarks. Annual ED costs were $19 374 832 for the intellectual and developmental disability cohort and an estimated $21 521 728 for a same-size sample from the benchmark population. Combined annual costs of ED plus inpatient care for the intellectual and developmental disability cohort were 100% higher than costs for the general population ($153 348 562 and $76 654 361, respectively).
Discussion
Consistent with the study’s main hypothesis, Medicaid members with intellectual and developmental disabilities used hospital care at significantly higher rates compared with benchmarks for the general population. Annual per capita inpatient expenses for children with intellectual and developmental disabilities exceeded expenses for the general population by 143%. Epilepsy/convulsions was the single most frequent reason for hospitalization of children with intellectual and developmental disabilities, with the annual risk for children needing hospitalization for epilepsy being nearly 20 times as high (RR = 19.43) as for children in the general population. RR for several other conditions was even higher, including risks for hospitalization related to paralysis (RR = 224.02), behavior disorders (RR = 23.51), hereditary CNS conditions (RR = 37.70), and aspiration pneumonitis (RR = 34.12). A subset of the codes most frequently associated with inpatient utilization include conditions that are associated with intellectual and developmental disabilities or comorbid conditions found at increased frequencies in children with intellectual and developmental disabilities. In some cases, it was not clear whether coding for a condition such as paralysis represents the immediate and specific condition being treated in the admission, or whether it is a condition that contributes additional complexity to the encounter. As the primary purpose of Medicaid claims data is to facilitate payment for services, the inclusion of paralysis as a primary reason for the visit may be an artifact observed when this data is used for the secondary purpose of surveillance.
This marked difference in hospital utilization and cost need not be inevitable as several of the most frequent reasons for hospital admission in the population with intellectual and developmental disabilities are ACSCs (eg, asthma, pneumonia) thatrespondpositivelyto appropriate outpatient management. Even in the case of conditions that have not been identified specifically as ACSCs (eg, epilepsy, mood disorders), there are community-based services and management strategies that can support effective outpatient care to prevent hospitalization. In fact, over 90% of children with intellectual and developmental disabilities did not require an admission during a year of tracking in the current study, which means that many of the complications associated with disabling conditions are being managed on an outpatient basis.
Similar to the findings for inpatient hospitalization, the RR for outpatient ED care was significantly higher for children with intellectual and developmental disabilities across a range of medical conditions. However, the RR levels tended to be less marked than was seen for the risk of hospital admissions, with only 2 conditions (behavior disorders and epilepsy/convulsions) exceeding a RR of 3.00 for ED care. Regarding the cost of ED care per visit, paid claims for Medicaid members with intellectual and developmental disabilities were approximately 50% lower when compared with benchmarks for the general population of children receiving ED care. It is likely that this finding reflects the lower payments typically provided by Medicaid to hospitals and care providers when compared with commercial insurance. In contrast, costs per inpatient visit were significantly higher for children with intellectual and developmental disabilities, which suggests that the complexity and duration of inpatient care can result in increased total costs even if Medicaid reimbursement rates are lower.
The use of data based on a large, multistate patient sample is a significant strength of the study; however, several potential limitations must be recognized in interpreting the findings. First, not all states currently have the infrastructure to perform this type of analysis, which places some limits on access to the full range of data needed to assess the generalizability of findings across all US states. Therefore, the findings may not be fully generalizable to environments in all US states. Second, even in states that are currently able to analyze Medicaid administrative data, some variations in data collection and coding procedures exist, which limited access to data that would allow comparisons with children without intellectual and developmental disabilities. Third, our focus on a Medicaid-only intellectual and developmental disability cohort limits the ability to examine utilization for all children with intellectual and developmental disabilities regardless of insurance coverage, although many children with intellectual and developmental disabilities have access to Medicaid coverage through a disability-related pathway rather than through income-based eligibility.27 We were also limited in benchmarking in that comparable data could not be disaggregated into a Medicaid population without intellectual and developmental disabilities vs those with coverage from other payers. Fourth, some children were excluded from our intellectual and developmental disability cohort because they did not receive any care during the inclusion period of 2008-2013, or because none of the care they received included a diagnostic code related to intellectual and developmental disabilities. Although our multiyear methods of cohort identification were selected to attempt to minimize this limitation, if present, this issue could contribute to greater differences in rates of hospital care for the intellectual and developmental disability cohort compared with the benchmark population. Fifth, although the identification of differences in service utilization is an important first step in changing clinical practice to prevent unnecessary hospitalizations, developing effective strategies for intervention is challenging. In addition, it is difficult to disentangle the influences of ineffective outpatient management from the effects of having a condition (eg, paralysis) associated with specific medical problems that may lead to higher hospitalization rates even when reasonable outpatient care is provided.
Health professionals who are committed to providing quality care to children with intellectual and developmental disabilities serve a population with unique and challenging needs. The complexity of serving children with disabilities can make it difficult to treat ongoing medical problems associated with a chronic condition while also focusing on providing preventive care and regular anticipatory guidance to patients and families.28 Although some of the medical problems that result in hospital admissions for children with intellectual and developmental disabilities may occur despite provision of adequate outpatient care, some of the causes of hospitalization are preventable based on the presence of ACSCs among the most frequent conditions leading to hospitalization. Identifying the conditions most likely to be associated with high rates ofhospitalization and outpatient ED care provides useful guidance to healthcare providers regarding the importance of implementing outpatient management strategies that reduce the necessity of expensive hospital care. The need for improved community-based seizure management and mental healthcare is particularly important. In addition to lowering hospital utilization rates and overall expenditures for critical medical services, improving the quality of ambulatory care for children with intellectual and developmental disabilities may lead to better overall health and more positive long-term outcomes–even for children with severe disabilities. In environments where healthcare resources are limited, proactive approaches to ensure children with developmental disabilities have access to high quality preventive and outpatient resources is of high importance to prevent unnecessary, high-cost utilization and poor outcomes for these children.
Acknowledgments
Supported by the Disability Research and Dissemination Center (DRDC) at the University of South Carolina through Cooperative Agreement (#5U01DD001007) from the Centers for Disease Control (CDC) and Prevention, and also by the Association of University Centers on Disability (AUCD) (#OT13-1302), also fromthe CDC. The contentsofthismanuscriptaresolelytheresponsibilityof the authors and do not necessarily represent the official views of the DRDC, AUCD, or the CDC. The authors declare no conflicts of interest.
We acknowledge the project oversight provided by Elizabeth Courtney-Long, employed by the CDC.
Glossary
- ACSC
Ambulatory care-sensitive conditions
- CCA
Clinical Classifications Software
- CNS
Central nervous system
- ED
Emergency department
- HCUP
Healthcare Cost and Utilization Project
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- MMIS
Medicaid Management Information System
- NEDS
Nationwide Emergency Department Sample
- NIS
National Inpatient Sample
- RR
Relative risk
Footnotes
Data Statement
Data sharing statement available at www.jpeds.com.
References
- 1.Bui AL, Dieleman JL, Hamavid H, Birger M, Chapin A, Duber HC, et al. Spending on Children’s Personal Health Care in the United States, 1996-2013. JAMA Pediatr 2017;171:181–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krahn GL, Hammond L, Turner A. A cascade of disparities: health and health care access for people with intellectual disabilities. Ment Retard Dev Disabil Res Rev 2006;12:70–82. [DOI] [PubMed] [Google Scholar]
- 3.PEW Charitable Trusts and McArthur Foundation [Internet]. State health care spending on Medicaid: a 50-state study of trends of drivers of cost. 2014, http://www.pewtrusts.org/~/media/Data-Visualizations/Interactives/2014/Medicaid/downloadables/State_Health_Care_Spending_on_Medicaid.pdf. Accessed September 5, 2018.
- 4.Krahn G, Fox M, Campbell V, Ramon I, Jesien G. Developing a health surveillance system for people with intellectual disabilities in the United States. J Policy Pract Intellect Disabil 2010;7:155–1566.5. [Google Scholar]
- 5.Shea LL, Xie M, Turcotte P, Marcus S, Field R, Newschaffer C, et al. Brief report: service use and associated expenditures among adolescents with autism spectrum disorder transitioning to adulthood. J Autism Dev Disord 2018;48:3223–7. [DOI] [PubMed] [Google Scholar]
- 6.Meehan E, Williams K, Reid SM, Freed GL, Babl FE, Sewell JR, et al. Comparing emergency department presentations among children with cerebral palsywith general childhood presentations: a data linkage study. Dev Med Child Neurol 2017;59:1188–95. [DOI] [PubMed] [Google Scholar]
- 7.Deavenport-Saman A, Lu Y, Smith K, Yin L. Do children with autism overutilize the emergency department? Examining visit urgency and subsequent hospital admissions. Matern Child Health J 2016;20:306–14. [DOI] [PubMed] [Google Scholar]
- 8.The Surgeon General’s call to action to improve the health and wellness of persons with disabilities. Washington, DC: US Dept of Health and Human Services, Office of the Surgeon General; 2005. [PubMed] [Google Scholar]
- 9.Krahn GL, Fox M. Health disparities of people with intellectual disabilities: what do we know? What do we do? J Appl Res Intellect Disabil 2014;27:431–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lewis MA, Lewis CE, Leake B, King BH, Lindemann R. The quality of health care for adults with developmental disabilities. Public Health Rep 2002;117:174–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Havercamp SM, Scott HM. National health surveillance of adults with disabilities, adults with intellectual and developmental disabilities, and adults with no disabilities. Disabil Health J 2015;8:165–72. [DOI] [PubMed] [Google Scholar]
- 12.McDermott S, Royer J, Mann JR, Armour BS. Factors associated with ambulatory care sensitive emergency department visits for South Carolina Medicaid members with intellectual disability. J Intellect Disabil Res 2018;62:165–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lennox NG, Van Driel ML, van Dooren K. Supporting primary healthcare professionals to care for people with intellectual disability: a research agenda. J Appl Res Dev Disabil 2015;28:33–42. [DOI] [PubMed] [Google Scholar]
- 14.Parish SL, Saville AW. Women with cognitive limitations living in the community: evidence of disability-based disparities in health care. Intellectual Disabilities 2006;44:249–59. [DOI] [PubMed] [Google Scholar]
- 15.Developmental Disabilities Assistance and Bill of Rights Act of 2000, Pub. L. No. 106-402, 114 Stat. 1677; 2000. [Google Scholar]
- 16.McDermott S, Royer J, Cope T, Lindgren S, Momany E, Lee JC, et al. Using Medicaid data to characterize persons with intellectual and developmental disabilities in five US states. Am J Intellect Dev Disabil 2018;123:371–81. [DOI] [PubMed] [Google Scholar]
- 17.Zablotsky B, Black LI, Blumberg SJ. Estimated prevalence of children with diagnosed developmental disabilities in the United States, 2014-2016. NCHS Data Brief 2017;291:1–8. [PubMed] [Google Scholar]
- 18.Schalock RL, Borthwick-Duffy SA, Bradley VJ, Buntinx WH, Coulter DL, Craig EM, et al. Intellectual disability: definition, classification, and systems of supports. 11th ed Washington, DC: American Association on Intellectual and Developmental Disabilities; 2010. [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC) [Internet]. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). 2011, http://www.cdc.gov/nchs/icd/icd9cm.html. Accessed September 5, 2018.
- 20.Elixhauser A, Steiner C, Palmer L. Clinical Classifications Software (CCS) [Software]. 2015. U.S. Agency for Healthcare Research and Quality; 2015. http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed September 5, 2018. [Google Scholar]
- 21.HCUP National Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). 2012. Rockville, MD: Agency for Healthcare Research and Quality; 2012. www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed September 5, 2018. [Google Scholar]
- 22.HCUP Nationwide Emergency Department Sample (NEDS). Healthcare Cost and Utilization Project (HCUP) [Internet]. 2012. Rockville, MD: Agency for Healthcare Research and Quality; 2012. www.hcup-us.ahrq.gov/nedsoverview.jsp. Accessed September 5, 2018. [Google Scholar]
- 23.Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood) 1993;12:162–73. [DOI] [PubMed] [Google Scholar]
- 24.AHRQ Quality Indicators—Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions. Rockville, MD: Agency for Healthcare Research and Quality; 2001. AHRQ Pub. No. 02-R0203. [Google Scholar]
- 25.Longman JM, Passey ME, Ewald DP, Rix E, Morgan GG. Admissions for chronic ambulatory care sensitive conditions - a useful measure of potentially preventable admission? BMC Health Serv Res 2015;15:472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Center for Health Statistics. Health, United States, 2012: With Special Feature on Emergency Care. Figure 29: Data from the Agency for Healthcare Research and Quality, Center for Financing, Access, and Cost Trends, Medical Expenditure Panel Survey; 2013. Hyattsville, MD. [PubMed] [Google Scholar]
- 27.Musumeci MB, Foutz J. Medicaid’s role for children with special health care needs: A look at eligibility, services, and spending. Kaiser Family Foundation Issue Brief [Internet]. 2018, https://www.kff.org/medicaid/issue-brief/medicaids-role-for-children-with-special-health-care-needs-a-look-at-eligibility-services-and-spending/. Accessed October 12, 2018.
- 28.Schor EL. Should children with special health care needs have separate preventive care visits? Arch Pediatr Adolesc Med 2007;161:1216–8. [DOI] [PubMed] [Google Scholar]


