Abstract
This study aimed to identify Brazilian dietary patterns and their associations with health, lifestyle and sociodemographic characteristics. Data from the Brazilian National Health Survey conducted in 2013 were used. A questionnaire was applied containing 22 items related to dietary consumption. Dietary patterns were determined through factor analysis (FA). Poisson regression models, with robust variance, were used to identify associations between dietary patterns and independents variables. Statistical significance was defined as p-value<0.05. Data were analysed for 60,202 adults (estimated population size: 146,308,458). FA identified three dietary patterns: healthy, protein, and western. The younger age group (18–24 years) had a lower adherence to the healthy pattern (PR:0.53; 95%CI:0.49–0.58) and greater adherence to the protein (PR:1.52; 95%CI:1.42–1.62) and western (PR:1.80; 95%CI:1.68–1.93) patterns compared to the elderly (≥60 years). Women had a greater association with the healthy pattern (PR:1.32; 95%CI:1.28–1.38) and lower association with the protein pattern (PR:0.80; 95%CI:0.77–0.82) compared to men. Illiterate participants showed lower adherence to the healthy (PR:0.58; 95%CI:0.53–0.63) and western (PR:0.54; 95%CI:0.48–0.62) patterns compared to those with higher educational levels. Smokers had lower adherence to the healthy (PR:0.76; 95%CI:0.71–0.81) and higher adherence to the protein (PR:1.14; 95%CI:1.11–1.19) patterns compared to non-smokers. Participants with poor/very poor self-rated health status had a lower adherence to the healthy (PR:0.79; 95%CI:0.73–0.86) and western (PR:0.81; 95%CI:0.73–0.89) patterns compared to those in a very good/good self-rated health status. Multimorbidity was positively associated with the healthy pattern (PR:1.18; 95%CI:1.11–1.26) and inversely associated with the protein pattern (PR:0.88; 95%CI:0.80–0.96) compared to participants without comorbidities. We suggest that strategies to promote healthy eating should consider health, lifestyle and sociodemographic characteristics in the Brazilian population.
Introduction
Dietary patterns have changed throughout human history. Food industry modernization contributes to continuous and abundant access to energy-dense food rich in lipids, sugar, and additives [1]. On the other hand, fruit, vegetable, and fish production and consumption are dependent on season, region, climate, and food system sophistication [1]. Changes in dietary patterns associated with government initiatives have contributed to reducing disease prevalence related to nutritional deficiencies [1]. However, this has created space for non-communicable diseases (NCDs) [1]. These changes in diet and disease patterns are known as the nutritional and epidemiological transition [1]. In Brazil, NCDs are responsible for 70% of deaths. One third of these deaths occur in people under the age of 60 [2]. Vulnerable people—especially those with lower income and education—are the most affected by NCDs. Social inequality is thus a key factor in the NCD burden [2].
Studies associating dietary patterns, sociodemographic characteristics and lifestyle factors are of particular interest in the nutritional epidemiology field [3]. Most studies consider food intake or nutrient effects in isolation, disregarding the complex interactions between them [3,4]. However, a typical diet is composed of foods combined in meals and snacks with a high degree of interactions between nutritional compounds [4]. Thus, dietary patterns have been proposed as an alternative to fill this methodological gap [3].
Most studies that evaluated dietary patterns have focused on countries in North America, Europe, and Asia [5]. Few Brazilian studies are available, and the ones that are focus on specific areas or specific population groups [6–14]. Moreover, the most recent studies evaluating national dietary patterns are relatively old, having used data from 2002/2003 [10,15].
Therefore, studies using recent data representing the Brazilian population are needed to monitor the ongoing changes in Brazilian dietary patterns. New evidences will contribute to the development and improvement of public policies aiming to reduce NCDs. This study aims to identify the main Brazilian dietary patterns and associated health, lifestyle and sociodemographic characteristics.
Materials and methods
Design and study population
This cross-sectional study used data from the Brazilian National Health Survey—BNHS (in Portuguese: Pesquisa Nacional de Saúde—PNS), 2013 [16]. BNHS is a five-year household survey with a complex sample design, representative of the Brazilian population in macro-regions, states, urban, rural, and metropolitan areas [17]. The Brazilian Ministry of Health and the Brazilian Institute of Geography and Statistics (IBGE) developed and carried out the BNHS. It is the largest national survey conducted to date on Brazilian public health [18]. The sample design used conglomerates in three levels: primary units of sampling (first stage), household (second stage), and selection of the household adult resident (third stage) [19]. Indigenous villages, barracks, military bases, housing camps, boats, penitentiaries, penal colonies, prisons, asylums, orphanages, convents, and hospitals were not included in the sampling design [17].
The questionnaire consisted of three parts: (i) housing and neighbourhood; (ii) household, and (iii) individual head-of-household (applied to a randomly selected resident older than 18) [17]. The National Commission of Ethics in Research for Human Beings approved the survey under number 328.159. All participants gave free and informed written consent [19]. More details about BNHS methods are available in a previous publication [19].
Variables
The following independent variables were selected for analysis: age, sex, colour/race, marital status, education, area of residence, macro-regions, socioeconomic status, physical activity, tobacco use, alcohol intake, self-rated health status and multimorbidity.
Age was categorized into four groups: 18–24 years; 25–39 years; 40–59 years; 60 years and older. Skin colour was self-declared as white, black, east asians, brown or indigenous and then categorised into "white or east asians" and "other". In Brazil, whites and east asians have similar socioeconomic characteristics [20]. Education was categorised as illiterate, elementary school, high school and university.
Socioeconomic status was defined based on availability of household items and the provision of home services and correspondent scores. The method used is described in greater detail in a previous publication [21]. The cut-off criteria for each socioeconomic class were as follows: Class A (45–100 points); B (29–44 points); C (17–28 points); D and E (0–16 points) [21].
Physical activity level included activities practised during leisure time, work, domestic activities, and commuting. This variable was categorised as sufficient (≥ 150 minutes per week), insufficient (>0 and <150 minutes per week), and sedentary (no physical activity) [22].
Tobacco use was categorised into non-smokers, ex-smokers, or smokers, and was based on self-reported consumption. Alcohol intake was categorised as abstainer, moderate, or binge drinker according to the Brazilian Ministry of Health [18,23].
The presence of two or more NCDs in the same person was defined as multimorbidity [24]. The following diseases were considered chronic conditions: systemic arterial hypertension, diabetes mellitus, hypercholesterolaemia, cardiovascular disease, asthma, arthritis or rheumatism, vertebral problems, work-related musculoskeletal disorder, depression, mental illness, lung disease, cancer (all types) and chronic kidney disease. The variable was classified into four categories (none or 1, 2, 3, and 4 conditions or more). Physical and mental health were also self-assessed according to the question: in general, how do you assess your health? Possible answers were very good/good, regular, bad/very bad.
Statistical analysis
The food consumption questionnaire was composed of 22 food items. Factor Analysis (FA) was performed to identify dietary patterns. FA allows the reduction of a large number of variables to a few factors that are not correlated with each other, explaining patterns underlying the original data.
The Bartlett test and Kaiser–Mayer–Olkin (KMO) coefficient were applied to verify the method applicability. KMO≥0.6 was considered acceptable in the partial correlation between diet variables [25,26]. For the Bartlett test, we assumed a Type I error rate of 5% [27,28].
Each dietary pattern was composed of food items with factor loads ≤-0.35 and ≥0.35. The total variances explained by each factor were also considered to determine the number of factors to be retained. Cattell’s scree plots and Eigenvalue >1 were also considered to select the patterns [28]. Orthogonal varimax transformation was applied to facilitate the interpretation of factor results [28]. Internal consistency between diet items and their respective factors was evaluated using Cronbach’s alpha test [29]. Participants received a factorial score for each identified pattern. Dietary patterns were categorized into quartiles (Q1-Q4). We assumed the first quartile as the reference quartile and compared it with the others. Thereby, we sought to observe associations with independents variables according by higher or lower adherence to each dietary pattern.
We applied a Poisson regression model with robust variance to estimate the association between dietary patterns, health and sociodemographic characteristics. Robust Poisson regression models allow correction for overestimation of associations when outcomes are not rare (>10% prevalence). Associations were presented as Prevalence Ratios (PR) with 95% confidence intervals (95% CI). Taking into account the cross-sectional desing of the study, we considered one as a constant time at risk to estimate the prevalence ratios [30].
The independents variables were age, sex, colour/race, marital status, educational level, area of residence (urban/rural), physical activity, smoking, alcohol intake, self-rated health, multimorbidity and socioeconomic status. Wald tests were used to evaluate the significance of variables in the bivariate analyses; values with p≤0.20 were retained for the multivariate model. Only variables with significant associations (Wald test p<0.05) to the dietary patterns were kept in the final model. All analyses were stratified by Brazilian macro-regions and performed with Stata software, version 14 [31].
Results
Health, sociodemographic and lifestyle characteristics
Data from 60,202 participants were analysed (participation rate 93.6%), representing 146,308,458 Brazilian adults according to the complex sample design.
Table 1 shows the study population characteristics. The average age was 41.3 years (SD: ± 16.6) and 53.0% were women. Thirty four percent of the population attended at least high school and 37.9% primary school only. Approximately 86% of the population lived in urban areas, and 43.8% lived in the southeast region. More than half (54%) reported practicing enough physical activity. The prevalence of non–smokers was 67.8% and smokers 14.7%. The prevalence of binge drinking was 13.6%. Approximately 66% of the sample self-reported very good or good health. Those reporting none or one NCD were 76.4%.
Table 1. Estimated population size (N = 146,308,458), prevalence (% per column), and confidence intervals (95% CI) of helath, lifestyle and sociodemographic characteristics in Brazilian adults.
| Variables | N | % (95%CI) |
|---|---|---|
| Age group (years) | ||
| Mean | 41.3 | |
| SD | 16.6 | |
| 18–24 | 23,306,033 | 16.0 (15.0–16.5) |
| 25–39 | 46,494,908 | 31.7 (31.1–32.5) |
| 40–59 | 50,099,686 | 34.3 (33.6–35.0) |
| 60+ | 26,407,831 | 18.0 (14.5–18.7) |
| Gender | ||
| Men | 68,916,470 | 47.0 (46.3–47.9) |
| Women | 77,391,988 | 53.0 (52.0–53.6) |
| Skin Colour/Race | ||
| White/East Asian | 70,813,082 | 48.5 (47.6–49.3) |
| Other a | 75,495,376 | 51.5 (50.8–52.4) |
| Marital status | ||
| Married | 89,537,328 | 61.2 (60.5–61.2) |
| Other b | 56,771,130 | 38.8 (38.0–39.5) |
| Education | ||
| University | 26,958,232 | 19.3 (18.5–20.2) |
| High School | 50,173,018 | 34.3 (33.6–35.0) |
| Elementary School | 54,004,400 | 37.9 (37.0–38.7) |
| Illiterate | 11,948,795 | 8.6 (8.2–9.0) |
| Area of residence | ||
| Urban | 126,132,422 | 86.2 (85.7–86.6) |
| Rural | 20,176,036 | 13.8 (13.3–14.2) |
| Economic status | ||
| A-B | 36,633,476 | 25.0 (24.5–25.6) |
| C | 57,463,271 | 39.3 (38.6–40.0) |
| D-E | 52,211,711 | 35.7 (35.1–36.3) |
| Physical Activity | ||
| Sufficient | 78,933,914 | 54.0 (53.1–54.7) |
| Insufficient | 26,540,646 | 18.0 (17.5–18.7) |
| None | 40,833,898 | 28.0 (27.1–28.6) |
| Smoking | ||
| Never | 99,248,243 | 67.8 (67.1–68.5) |
| Ex-smokers | 25,540,840 | 17.5 (16.8–18.0) |
| Current | 21,519,375 | 14.7 (14.2–15.2) |
| Alcohol intake | ||
| Abstainer | 87,183,278 | 59.6 (58.7–60.4) |
| Moderate | 39,152,545 | 26.8 (26.0–27.5) |
| Binge drinker | 19,972,635 | 13.6 (13.1–14.2) |
| Self-Rated Health | ||
| Very good/Good | 96,748,777 | 66.1 (65.4–66.8) |
| Fair | 41,039,237 | 28.0 (27.4–28.7) |
| Poor/Very poor | 8,520,444 | 5.9 (5.5–6.1) |
| Multimorbidity | ||
| 0 or 1 | 111,769,410 | 76.4 (75.7–77.0) |
| 2 | 18,245,024 | 12.5 (12.0–13.0) |
| 3 | 8,901,041 | 6.9 (5.7–6.5) |
| 4+ | 7,392,983 | 5.2 (4.7–5.4) |
N, Absolute frequency of estimated population. CI, confidence interval. SD, standard deviation.
a Black(a), brown(a), indigenous.
b single, divorced, separated, widowed.
Factor analysis
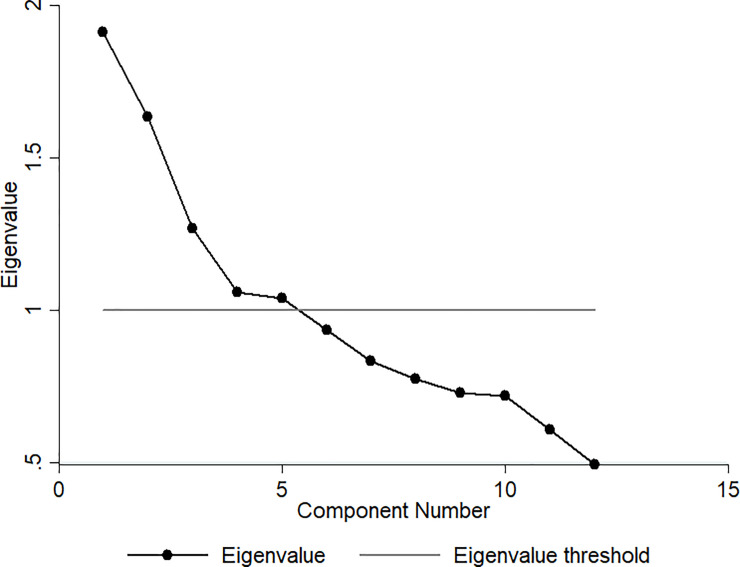
Table 2 presents the results of the FA, which identified three main dietary patterns: healthy, protein, and western. Fig 1 shows the scree plot revealed three main dietary patterns with eigenvalues greater than one (see Table 2 for details). The healthy pattern was composed of raw salads, vegetables, cooked vegetables, fruits, and fresh fruit juice. The protein pattern was composed of beans, red meat, fish, and chicken. The western pattern was composed of processed and ultra-processed foods: snacks, pizzas, sweets, and soft drinks. The three main patterns explained 40% of diet variability. The overall KMO was 0.61. The p-value for the Bartlett test was 0.001. The highest p-value for the Cronbach Alpha test was 0.55. Milk was not included in any of the dietary patterns due to a low factorial load.
Table 2. Brazilian dietary patterns components identified by Factor Analysis (FA).
| Dietary Patterns | Food Items/Food Group | Factor Load | KMO | Eigenvalue | Variance (%) a | CronbachAlpha test |
|---|---|---|---|---|---|---|
| Healthy | Lettuce and tomato salad or other vegetable or raw legumes | 0.75 | 0.60 | 1.91 | 15.60 | 0.55 |
| Cooked vegetables and legumes b | 0.73 | 0.60 | ||||
| Natural fruit juice | 0.42 | 0.63 | ||||
| Fruits | 0.59 | 0.72 | ||||
| Protein | Beans | 0.54 | 0.56 | 1.64 | 12.80 | 0.39 |
| Red meat | 0.68 | 0.58 | ||||
| Fish | -0.62 | 0.61 | ||||
| Poultry | -0.38 | 0.52 | ||||
| Western | Soft drinks | 0.60 | 0.60 | 1.26 | 11.80 | 0.41 |
| Sweets c | 0.65 | 0.60 | ||||
| Sandwiches, snacks or pizza | 0.70 | 0.59 |
KMO, Kaiser-Meyer-Olkin.
Total variance:40.20. Total KMO: 0.61.
a The variance percentage explained by each pattern.
b cabbage, carrot, chayote, eggplant, pumpkin. Not considered: Potato, cassava, and yams–foods rich in starch.
c cakes, pies, chocolates, candies, biscuits, or sweet biscuits.
Bartlett’s sphericity test p-value<0.001.
Factor loads ≤-0.35 and ≥0.35.
Fig 1. Cattell’s scree plot.
Association of dietary patterns with independents variables
Table 3 shows the associations between the first quartile (Q1—reference quartile) and the last quartile (Q4) of each pattern in the Brazilian population. Associations between the first, second and third quartiles are presented in the supplement as are all results related to the stratified analysis by macro-regions.
Table 3. Associations between health, lifestyle, sociodemographic characteristics and countrywide Brazilian dietary patterns.
Comparison between first and fourth quartiles.
| DIETARY PATTERNS | HEALTHY | PROTEIN | WESTERN | |||
|---|---|---|---|---|---|---|
| Prevalence Ratio | Crude (95%CI) | Adjusted (95%CI) | Crude (95%CI) | Adjusted (95%CI) | Crude (95%CI) | Adjusted (95%CI) |
| Sample Size (n) | 30,101 | 30,101 | 30,101 | |||
| Estimated Population Size (N) | 72,190,359 | 72,135,995 | 75,207,779 | |||
| Age groups (years) | ||||||
| 60+ | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 18–24 | 0.59(0.55–0.64) | 0.53(0.49–0.58) | 1.38(1.30–1.47) | 1.52(1.42–1.62) | 2.37(2.21–2.54) | 1.80(1.68–1.93) |
| 25–39 | 0.75(0.72–0.79) | 0.68(0.64–0.71) | 1.33(1.26–1.41) | 1.40(1.33–1.48) | 1.90(1.77–2.05) | 1.49(1.38–1.60) |
| 40–59 | 0.87(0.83–0.91) | 0.81(0.78–0.85) | 1.22(1.16–1.29) | 1.20(1.14–1.26) | 1.34(1.25–1.45) | 1.16(1.08–1.24) |
| p-value | <0.005 | <0.005 | <0.005 | <0.005 | <0.005 | <0.005 |
| Sex | ||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | - |
| Female | 1.32(1.28–1.38) | 1.21(1.17–1.26) | 0.73(0.70–0.75) | 0.80(0.77–0.82) | 1.02(0.98–1.06) | - |
| p-value | <0.005 | <0.005 | <0.005 | <0.005 | 0.261 | - |
| Skin Color/Race | ||||||
| White/Yellow | 1.00 | 1.00 | 1.00 | - | 1.00 | 1.00 |
| Othera | 0.72(0.70–0.75) | 0.92(0.89–0.96) | 1.00(0.96–1.03) | - | 0.72(0.69–0.75) | 0.90(0.86–0.93) |
| p-value | <0.005 | <0.005 | 0.882 | - | <0.005 | <0.005 |
| Marital status | ||||||
| Otherb | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | - |
| Married | 1.10(1.06–1.15) | 1.08(1.04–1.12) | 1.09(1.06–1.13) | 1.08(1.05–1.12) | 0.86(0.83–0.89) | - |
| p-value | <0.005 | <0.005 | <0.005 | <0.005 | <0.005 | - |
| Education | ||||||
| College | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| High School | 0.78(0.75–0.82) | 0.90(0.86–0.94) | 1.37(1.29–1.45) | 1.34(1.27–1.42) | 0.88(0.85–0.91) | 0.92(0.89–0.96) |
| Elementary School | 0.69(0.65–0.72) | 0.76(0.72–0.79) | 1.46(1.38–1.55) | 1.54(1.46–1.64) | 0.54(0.52–0.57) | 0.73(0.69–0.76) |
| Illiterate | 0.49(0.44–0.54) | 0.58(0.53–0.63) | 1.20(1.11–1.30) | 1.60(1.47–1.73) | 0.30(0.27–0.34) | 0.54(0.48–0.61) |
| p-value | <0.005 | <0.005 | <0.005 | <0.005 | <0.005 | <0.005 |
| Area of residence | ||||||
| Urban area | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Rural area | 0.60(0.56–0.65) | 0.83(0.78–0.89) | 1.10(1.05–1.15) | 1.17(1.12–1.22) | 0.47(0.43–0.52) | 0.64(0.59–0.69) |
| p-value | <0.005 | <0.005 | <0.005 | <0.005 | <0.005 | <0.005 |
| Economic Status | ||||||
| A-B | 1.00 | 1.00 | 1.00 | - | 1.00 | - |
| C | 0.84(0.80–0.88) | 1.01(0.96–1.05) | 1.04(1.00–1.09) | - | 0.82(0.78–0.85) | - |
| D-E | 0.67(0.64–0.70) | 0.92(0.88–0.97) | 0.98(0.93–1.02) | - | 0.66(0.63–0.70) | - |
| p-value | <0.005 | <0.005 | <0.005 | - | <0.005 | - |
| Physical Activity | ||||||
| Sufficient | 1.00 | 1.00 | 1.00 | - | 1.00 | - |
| Insufficient | 0.89(0.84–0.94) | 0.86(0.82–0.90) | 1.01(0.97–1.06) | - | 0.95(0.91–1.00) | - |
| None | 0.86(0.82–0.90) | 0.83(0.80–0.87) | 0.99(0.95–1.03) | - | 0.86(0.82–0.90) | - |
| p-value | <0.005 | <0.005 | 0.598 | - | <0.005 | - |
| Smoking | ||||||
| Never | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | - |
| Ex-smoker | 0.92(0.88–0.97) | 0.91(0.87–0.96) | 1.05(1.01–1.10) | 1.04(1.00–1.09) | 0.77(0.73–0.81) | - |
| Current | 0.66(0.62–0.71) | 0.76(0.71–0.81) | 1.28(1.24–1.33) | 1.15(1.11–1.19) | 0.86(0.82–0.91) | - |
| p-value | <0.005 | <0.005 | <0.005 | <0.005 | <0.005 | - |
| Alcohol intake | ||||||
| Abstainer | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Moderate | 0.96(0.92–1.00) | 0.95(0.92–0.99) | 1.13(1.09–1.18) | 1.02(0.98–1.06) | 1.31(1.26–1.36) | 1.09(1.06–1.14) |
| Binge drinker | 0.72(0.67–0.77) | 0.84(0.79–0.90) | 1.29(1.24–1.34) | 1.09(1.05–1.14) | 1.31(1.25–1.38) | 1.10(1.06–1.15) |
| p-value | <0.005 | <0.005 | <0.005 | <0.005 | <0.005 | <0.005 |
| Self-Rated Health | ||||||
| Very good/Good | 1.00 | 1.00 | 1.00 | - | 1.00 | 1.00 |
| Fair | 0.85(0.81–0.89) | 0.87(0.84–0.91) | 0.92(0.88–0.95) | - | 0.66(0.63–0.69) | 0.90(0.86–0.95) |
| Poor/Very poor | 0.74(0.67–0.80) | 0.79(0.73–0.86) | 0.86(0.80–0.93) | - | 0.48(0.43–0.54) | 0.81(0.73–0.89) |
| p-value | <0.005 | <0.005 | <0.005 | - | <0.005 | <0.005 |
| Multimorbidity | ||||||
| 0 or 1 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | - |
| 2 | 1.15(1.08–1.21) | 1.03(0.98–1.08) | 0.83(0.77–0.90) | 0.96(0.91–1.01) | 0.79(0.75–0.84) | - |
| 3 | 1.31(1.24–1.39) | 1.13(1.07–1.20) | 0.77(0.71–0.85) | 0.93(0.87–1.00) | 0.72(0.66–0.79) | - |
| 4+ | 1.34(1.27–1.41) | 1.18(1.11–1.26) | 0.77(0.71–0.85) | 0.88(0.80–0.96) | 0.65(0.59–0.73) | - |
| p-value | <0.005 | <0.005 | <0.005 | 0.012 | <0.005 | - |
Wald Test: Variables not statistically significant in the model.
a Black(a), brown(a), indigenous.
b single, divorced, separated, widowed.
Nationally, adherence to the healthy pattern was less common among those aged 18–24 (PR: 0.53; 95%CI: 0.49–0.58) than among those 60 and older. Associations between age and healthy pattern were similar in all Brazilian macro-regions. A dose-response relationship between age and healthy pattern was observed in all Brazilian macro-regions and at the national level. The healthy pattern was significantly more common among women compared to men in all regions and in Brazil as a whole.
The healthy pattern was significantly less frequent among illiterate participants compared to those with a university education in Brazil as a whole and all macro-regions. Likewise, the healthy pattern was significantly more common among urban residents than rural residents in the North (PR: 0.49; 95% CI: 0.37–0.66) and Northeast (PR: 0.71; 95% CI: 0.61–0.83) macro-regions. On the other hand, rural inhabitants of the South region were more likely to adopt the healthy pattern (PR: 1.15; 95% CI: 1.04–1.27) than those living in urban areas in the same region (Supplement material).
Women were more likely to adopt the healthy pattern than men (PR: 1.21; 95% CI: 1.17–1.26). Adherence to the healthy pattern was more common among married than unmarried individuals. Adherence to the healthy pattern was less common among current smokers, binge drinkers, and those with self-rated health as poor/very poor compared to non-smokers, abstainers and people with very good/good self-rated health, respectively. Individuals with four or more NCD’s were more likely to adopt the healthy pattern than those with none or one NCD.
Younger participants (18–24 years) were more likely to adopt the protein pattern (PR: 1.52; 95% CI: 1.42–1.62) than the elderly (≥60 years), with significant associations nationally and in all Brazilian macro-regions. In addition, women were significantly less likely to adopt the protein pattern than men. Married individuals were more likely to adopt the protein pattern than their unmarried counterparts. The protein pattern was more common among illiterate participants (RP: 1.60; 95% CI: 1.47–1.73) compared to those with a university degree. Current smokers and binge drinkers were more likely to adopt the protein pattern than non-smokers and abstainers. The adherence to the protein pattern was less common among those with four or more NCDs compared to those with none or one NCD. Nationally, associations between skin color, economic status, physical activity, self-rated health and the protein pattern were not significant.
Younger participants also showed higher adherence to the western pattern (PR: 1.80; 95% CI: 1.68–1.93) compared to the elderly. Adherence to the western pattern was less frequent among black, brown and indigenous participants compared to white and East Asian participants together. Overall, the western pattern was significantly less common among illiterate participants (PR: 0.54; 95% CI: 0.48–0.61) compared to those holding a university degree. In the North, rural residence was inversely associated with the western pattern compared to those living in the urban area (PR: 0.29; 95% CI: 0.21–0.40). Rural dwellers in other macro-regions also presented a weaker association with the western pattern compared to urban area residents (Supplementary Information). The western pattern was more frequent among binge drinkers than abstainers (PR: 1.10; 95% CI: 1.06–1.15). On the other hand, the western pattern was less common among those with poor/very poor self-rated health compared to those with very good/good self-rated health. Nationally, associations between sex, marital status, economic status, physical activity, smokers, multimorbidity and the western pattern were not statistically significant.
Discussion
Our study identified three main dietary patterns–healthy, protein and western–which explained 40% of the diet variability. Adherence to the healthy pattern was less common among younger participants (18–24 years old), black, brown and indigenous participants, illiterate people, people living in rural areas, physically inactive individuals, current smokers, binge drinkers and those with lower socioeconomic status and self-rated poor/very poor health. The protein pattern was more common among people who were younger, married, male, illiterate, living in rural areas, current smokers, binge drinkers and those with none or one NCD. Finally, the western pattern was more likely to be adopted by younger individuals, binge drinkers, those holding a university degree and those living in urban areas. To our knowledge, this is the first study to analyse dietary patterns using a nationally representative sample of Brazilian population.
The healthy pattern presented high factor loads for the healthy eating markers. Our findings corroborate previous studies that found similar dietary patterns [32], with high factor loads for vegetables, fruits and fresh fruit juice, poultry, low-fat cheeses, roots, tubers and fish [8,9,12,15]. The healthy pattern has also been described in other studies as vegetables [33] or prudent [9,34–44], with similar composition.
Previous studies evaluating dietary patterns in Brazilian subpopulations also identified the western pattern. High factor loads were observed for foods such as butter, margarine, added sugar, bread, pasta, fats, dairy products, sauces, pizza, processed meat, soft drinks, canned vegetables, sweets and desserts [9,13,14]. The western pattern is also described as unhealthy [34,36–38,40,41,43–51] or modern [36], presenting a high factor load for red and processed meat, eggs, refined grains, cookies, snacks, pizza, French fries and hamburgers.
Healthy and western patterns have been verified in many dietaries patterns studies and describe the extremes of a group diet. Between these patterns are intermediate dietaries patterns which characterize the differences in eating habits in different groups. Our study identified the protein pattern as the intermediate pattern. Intermediate patterns have been described in previous literature as mixed pattern presenting a high factor load for cereals, eggs, soft drinks, coffee, juice, fruit, vegetables, nuts, dairy products, butter, margarine, meat, fish, shrimp, sweets and alcohol [6]. The snacks pattern is composed of butter, cheese, meat, pork, beef, processed meats, sandwiches, eggs, dairy products, sweets, and desserts. Finally, the dual pattern [8,9,52] consists of a high factor load of dairy products, fresh fruit, tomato, vegetables, juice, fruits, green vegetables, bananas, sweets, desserts, soft drinks, processed meats, fast food, margarine, and cookies [10]. The traditional Brazilian pattern is an intermediate pattern [6–15,25,52–57] characterised by rice and beans consumption [15]. This pattern was not identified in this study because the BNHS did not evaluate rice consumption. The BNHS considered only healthy eating markers, and the rice consumption assessment was not prioritized, even though beans are usually consumed with rice in Brazil. Other intermediate country-specific patterns described in the literature are traditional Polish [42], Kimchi rice [58], Vegetarian [59], Tex–Mex [48,49], Dim Sum [60], Mediterranean [38,45], and Mchicha [61] patterns.
Sociodemographic characteristics and dietary patterns
Previous studies identified associations between dietary patterns, educational level, and income in the Brazilian population [15]. However, other sociodemographic characteristics were not considered [62]. We found that age, sex, educational level, skin colour, marital status and socioeconomic status were associated with dietary patterns.
We observed dose-response effects in the associations between age groups and dietary patterns. These dose-response effects suggest age is an important factor in food choice. Previous studies have shown that the elderly prefer healthy diets [63–66]. On the other hand, younger people prefer soft drinks and fast food [4,65,67,68]. Several factors could explain healthier eating habits in older individuals. They have more time to prepare their meals and more knowledge about healthy eating habits than young people. Moreover, they are generally more concerned about diet as part of NCD prevention and control. The high NCD prevalence observed among the elderly leads them to adopt a healthier lifestyle, including diet improvement [69,70]. Adequate diet practices require knowledge, planning time for groceries, and cooking. For young people, these aspects can be considered barriers to adopting healthy eating habits. Therefore, they tend to choose more pragmatic alternatives: eating away from home, usually high-energy density foods [15]. A study of 34,000 Brazilians reported that about 40% of participants consumed food outside home. Beetwen teenagers, fifty-one percent reported consumed food outside home. The most frequently consumed food group was the high-energy content and low nutritional quality one: alcoholic beverages, fried foods, pizza, soft drinks, and sandwiches [71]. Lack of time to prepare food, lack of access to healthy food in schools and universities, financial instability, poor culinary skills, little knowledge about food preparation, lack of cooking equipment, and easy access to processed products were indicated as the main reasons for eating unhealthily [72]. In this scenario, the provision of healthy food in school and university environments could be a strategy to promote healthy eating habits among young people.
Women presented higher adherence to the healthy pattern compared to men in all Brazilian macro-regions (S1–S5 Tables). On the other hand, women’s adherence to the protein pattern was lower compared to men. Only in the Southeast of the country, the western pattern was more common among women compared to men (S1 Table). Culturally, women are more concerned about health and body shape, which also reflects on food choices. Our findings corroborate previous studies where women showed greater adherence to healthy patterns compared to men [4,63,64,68].
In the Southeast and the Northeast, married people had higher adherence to the healthy pattern compared to unmarried people (S1 and S4 Tables in Suplementary Information). We verified higher adhesion to the protein pattern in married people living in Southeast, South, Midwest, and North compared to unmarried people (S1, S2, S3 and S5 Tables in Suplementary Information). Previous findings have pointed to inconsistent associations between marital status and dietary patterns [65,73]. However, married life seems to have a positive effect on changing eating habits over time [73]. A study conducted in an urban population in Lithuania revealed that married individuals were more likely to follow a diet rich in fresh and cooked vegetables, fruits, eggs, tomatoes, and meats than single individuals [66]. Married individuals tend to prepare and consume healthier foods, while single individuals tend to choose fast food options.
People with black/brown skin colour and indigenous identify lower adherence to the healthy and western patterns. On the other hand, greater adherence to the protein pattern was seen among black, brown, and indigenous participants from the Southeast and South compared to whites and East Asians (S1 and S2 Tables). Previous studies reported differences in dietary patterns between different ethnic groups [64,74]. Ethnicity is related to social inequities and income distribution in Brazil and other developing countries. Indigenous and black/and brown people generally have less access to regular education, and have lower incomes [75–77]. These factors also affect their food choices. A study in the United States found that, among white people, educational level was strongly associated with healthier patterns; however, this association was weak among black people [78].
Adherence to the healthy and western patterns was less common among the lower education group. Associations were stronger between the protein pattern and low education groups. Dietary patterns may differ between educational levels [65,66] because people with higher education tend to adopt healthier eating habits [66,68,79,80]. Our results differ, in part, from previous findings: healthy and western patterns were more common among those with higher educational levels. In this study, educational level was used as a proxy for income. People with higher educational levels tend to have higher purchasing power, which may be associated with healthier food choices. Furthermore, people with higher education are more able to understand the importance of healthy eating habits [65].
Adherence to the healthy pattern was less frequent among people with lower economic status; this group was more likely to adopt the protein and western patterns when compared to those with a higher economic status. Foods rich in saturated fat and sugar are cheaper than healthy and organic foods [15,65,66,74]. The adherence to the protein pattern among those with lower socioeconomic status could be explained by some factors: (i) among foods with high factor load in this pattern, beans are the protein source most affordable in Brazil; (ii) beans are part of a typical Brazilian meal consumed by every social classes; (iii) indigenous people cultivate and consume different species of beans in the North and Northeast regions of Brazil; (iv) the cultural high consumption of barbecue in the Midwest and South regions of Brazil; (v) fishing is common among indigenous people.
Health, lifestyle characteristics and dietary patterns
Our study also identified statistically significant associations between the three dietary patterns, health and lifestyle characteristics in the Brazilian population. People with healthy eating habits tend to adopt a healthy lifestyle. Adherence to the healthy pattern was more common among physically active individuals, abstainers and non-smokers. Many researchers have shown that people who practice regular physical activity and do not smoke are more likely to consume fruits, fishes, vegetables, legumes and less red and processed meats [67,80–83].
On the other hand, binge drinkers and smokers were more likely to adopt the protein and western patterns. The consumption of alcoholic beverages can modulate appetite and food choices [84]. The diet among alcohol consumers tends to be lower in carbohydrates, fiber, vitamins, minerals, fruits, vegetables and dairy products [84–86] and high in animal products, oils, fatty acids, bread and breakfast cereals [85]. The consumption of unhealthy food is also frequent among smokers. Nicotine can modify smokers’ sense of taste. With that, they prefer foods high in sugar and fat and processed food become more palatable [4,68,80,87].
Adherence to the healthy pattern was less frequent among individuals who reported poor/very poor self-rated heath, which corroborates a previous study [66]. Adherence to the western pattern was more frequent among those with very good/good self-rated health status in the Southeast and Midwest regions. These contradictory findings could be explained by some factors: (i) people with very good/good self-rated health are less concerned about healthy eating habits; (ii) people with NCDs tend to adopt healthier eating habits. Nationally, people with four or more NCDs were more likely to adopt the healthy pattern. Otherwise, the protein pattern was less frequent among those with four or more NCDs. We highlight as a limitation that our study is a cross-sectional study design in which reverse causality may be present. In addition, self-rated health status is a subjective variable.
We highlight as a strength of this study the fact that the BNHS is the most comprehensive, and representative health survey conducted in Brazil. Our study was able to perform dietary patterns analysis with a representative sample of the Brazilian population. In addition, we applied robust statistical methods to explore the relationship between the main dietary patterns, health, lifestyle and sociodemographic characteristics. Most previous Brazilian studies that derived dietary patterns only used samples from large urban centres [6–9,11,52,88]. This survey provided us with data from rural areas and other small towns, which enriched our findings. Lastly, FA evaluates the diet globally, considering all aspects of diet complexity.
Our study has some limitations. First, the available data in BNHS may not have captured all dietary patterns of the studied population [5]. This limitation is inherent to the instrument applied to collect food consumption data: BNHS applied a screen questionnaire of diet with only 22 food items that did not capture all foods consumed in Brazil. Second, associations between dietary patterns and independents variables presented in this study should be interpreted with caution. FA is not a mutually exclusive technique, and the same individual may have a high factor load for more than one pattern.
We identified three main dietary patterns in the Brazilian population: healthy, protein and western. We concluded that people with a healthy lifestyle were more likely to adopt healthy pattern. On the other hand, the western pattern was more common among those with an unhealthy lifestyle—smokers, binge drinkers and the physically inactive. Based on our findings, we suggest that strategies to promote healthy eating habits should consider these aspects related to health, lifestyle and sociodemographic characteristics.
Supporting information
Comparison between quartile 1 and quartile 4 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 4 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 4 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 4 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 4 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 2 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 2 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 2 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 2 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 2 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 2 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 3 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 3 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 3 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 3 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 3 for each dietary pattern.
(PDF)
Comparison between quartile 1 and quartile 3 for each dietary pattern.
(PDF)
Data Availability
The data underlying the results presented in the study are available from https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?=&t=o-que-e.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.WCRF—World Cancer Research Fund | American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. 2007;537 Washington, DC: American Institute for Cancer Research. [Google Scholar]
- 2.Brasil. Plano de Ações Estratégicas para o Enfrentamento das Doenças Crônicas Não Transmissíveis (DCNT). Minist. Saúde. 2011. Avaliable from: http://portalms.saude.gov.br/vigilancia-em-saude/vigilancia-de-doencas-cronicas-nao-transmissiveis-dcnt/plano-de-acoes-estrategicas-para-o-enfrentamento-das-doencas-cronicas-nao-transmissiveis-dcnt. [DOI] [PubMed]
- 3.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002. February;13(1):3–9. 10.1097/00041433-200202000-00002 [DOI] [PubMed] [Google Scholar]
- 4.Beck KL, Jones B, Ullah I, McNaughton SA, Haslett SJ, Stonehouse W. Associations between dietary patterns, socio-demographic factors and anthropometric measurements in adult New Zealanders: an analysis of data from the 2008/09 New Zealand Adult Nutrition Survey. Eur J Nutr. 2018. June 1;57(4):1421–33. 10.1007/s00394-017-1421-3 [DOI] [PubMed] [Google Scholar]
- 5.Grosso G, Bella F, Godos J, Sciacca S, Del Rio D, Ray S, et al. Possible role of diet in cancer: systematic review and multiple meta-analyses of dietary patterns, lifestyle factors, and cancer risk. Nutr Rev. 2017. June 1;75(6):405–19. 10.1093/nutrit/nux012 [DOI] [PubMed] [Google Scholar]
- 6.Sichieri R. Dietary Patterns and Their Associations with Obesity in the Brazilian City of Rio de Janeiro. Obes Res. 2002. January 1;10(1):42–8. 10.1038/oby.2002.6 [DOI] [PubMed] [Google Scholar]
- 7.Sichieri R, Castro JFG, Moura AS. Fatores associados ao padrão de consumo alimentar da população brasileira urbana. Cad Saúde Pública. 2003;19:S47–53. 10.1590/s0102-311x2003000700006 [DOI] [PubMed] [Google Scholar]
- 8.Marchioni DML, Fisberg RM, Filho G, De JF, Kowalski LP, Carvalho MB de, et al. Dietary patterns and risk of oral cancer: a case-control study in São Paulo, Brazil. Rev Saúde Pública. 2007. February;41(1):19–26. 10.1590/s0034-89102007000100004 [DOI] [PubMed] [Google Scholar]
- 9.Toledo ALA de Koifman RJ, Koifman S Marchioni DML. Dietary patterns and risk of oral and pharyngeal cancer: a case-control study in Rio de Janeiro, Brazil. Cad Saúde Pública. 2010. January;26(1):135–42. 10.1590/s0102-311x2010000100014 [DOI] [PubMed] [Google Scholar]
- 10.Marchioni DM, Claro RM, Levy RB, Monteiro CA. Patterns of food acquisition in Brazilian households and associated factors: a population-based survey. Public Health Nutr. 2011. September;14(9):1586–92. 10.1017/S1368980011000486 [DOI] [PubMed] [Google Scholar]
- 11.Vilela AAF, Sichieri R, Pereira RA, Cunha DB, Rodrigues PRM, Gonçalves-Silva RMV, et al. Dietary patterns associated with anthropometric indicators of abdominal fat in adults. Cad Saúde Pública. 2014. March;30(3):502–10. 10.1590/0102-311x00167512 [DOI] [PubMed] [Google Scholar]
- 12.Santos R de O, Fisberg RM, Marchioni DM, Baltar VT. Dietary patterns for meals of Brazilian adults. Br J Nutr. 2015. September;114(5):822–8. 10.1017/S0007114515002445 [DOI] [PubMed] [Google Scholar]
- 13.Borges CA, Marchioni DML, Levy RB, Slater B. Dietary patterns associated with overweight among Brazilian adolescents. Appetite. 2018. April 1;123:402–9. 10.1016/j.appet.2018.01.001 [DOI] [PubMed] [Google Scholar]
- 14.Cunha DB, Bezerra IN, Pereira RA, Sichieri R. At-home and away-from-home dietary patterns and BMI z-scores in Brazilian adolescents. Appetite. 2018. January;120:374–80. 10.1016/j.appet.2017.09.028 [DOI] [PubMed] [Google Scholar]
- 15.Nascimento S, Barbosa FS, Sichieri R, Pereira RA. Dietary availability patterns of the brazilian macro-regions. Nutr J. 2011. July 28;10:79 10.1186/1475-2891-10-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brasil. Pesquisa Nacional de Saúde. In: Inst. Bras. Geogr. E Estat [Internet]. 2013. Available from: https://www.pns.icict.fiocruz.br/index.php?pag=proposicao.
- 17.Souza-Júnior PRB de, Freitas MPS de, Antonaci G de A, Szwarcwald CL. Desenho da amostra da Pesquisa Nacional de Saúde 2013. Epidemiol E Serviços Saúde. 2015. June;24(2):207–16. [Google Scholar]
- 18.Garcia LP, Freitas LRS de. Consumo abusivo de álcool no Brasil: resultados da Pesquisa Nacional de Saúde 2013. Epidemiol E Serviços Saúde. 2015. June;24(2):227–37. [Google Scholar]
- 19.Jaime PC, Stopa SR, Oliveira TP, Vieira ML, Szwarcwald CL, Malta DC. Prevalência e distribuição sociodemográfica de marcadores de alimentação saudável, Pesquisa Nacional de Saúde, Brasil 2013. Epidemiol E Serviços Saúde. 2015. June;24(2):267–76. [Google Scholar]
- 20.Brasil. (DIEESE). In: Departamento Intersindical de Estatística e Estudos Socioeconômmicos [Internet]. 2018 [cited 2019 Jan 21]. Available from: https://www.dieese.org.br/.
- 21.Pilli L, Ambrósio B, Suzzara B, Alves M, Reis M, Yamakava P, et al. Critério de Classificação Econômica Brasil [Internet]. Associação Brasileira de Empresas de Pesquisa. 2015. [cited 2018 Feb 21]. Available from: http://www.abep.org/criterio-brasil. [Google Scholar]
- 22.WHO. Physical Activity and Adults [Internet]. World Health Organization. 2019 [cited 2018 Feb 19]. Available from: https://www.who.int/dietphysicalactivity/factsheet_adults/en/.
- 23.Brasil. I Levantamento Nacional sobre os Padrões de Consumo de Álcool na População Brasileira [Internet]. Centro de Informações Sobre Saúde e Álcool. 2007 [cited 2019 Jan 7]. Available from: http://www.cisa.org.br/artigo/155/i-levantamento-nacional-sobre-os-padroes.php.
- 24.Carvalho JN de, Roncalli ÂG, Cancela M de C, Souza DLB de. Prevalence of multimorbidity in the Brazilian adult population according to socioeconomic and demographic characteristics. PLOS ONE. 2017. April 6;12(4):e0174322 10.1371/journal.pone.0174322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Previdelli ÁN, de Andrade SC, Fisberg RM, Marchioni DM. Using two different approaches to assess dietary patterns: hypothesis-driven and data-driven analysis. nutrients [Internet]. 2016. September 23 [cited 2018 Aug 15];8(10). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5083981/. 10.3390/nu8100593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Santos IKS dos, Conde WL. Tendência de padrões alimentares entre adultos das capitais brasileiras. Rev Bras Epidemiol. 2020;23:e200035 10.1590/1980-549720200035 [DOI] [PubMed] [Google Scholar]
- 27.Box GEP. A general distribution theory for a class of likelihood criteria. Biometrika. 1949. December 1;36(3–4):317–46. [PubMed] [Google Scholar]
- 28.Kaiser HF. An index of factorial simplicity. Psychometrika. 1974. March 1;39(1):31–6. [Google Scholar]
- 29.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951. September 1;16(3):297–334. [Google Scholar]
- 30.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003. October 20;3(1):21 10.1186/1471-2288-3-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stata: Software for Statistics and Data Science [Internet]. [cited 2020 Apr 28]. Available from: https://www.stata.com/.
- 32.Ax E, Lemming EW, Becker W, Andersson A, Lindroos AK, Cederholm T, et al. Dietary patterns in Swedish adults; results from a national dietary survey. Br J Nutr. 2016. January;115(1):95–104. 10.1017/S0007114515004110 [DOI] [PubMed] [Google Scholar]
- 33.Baglietto L, Krishnan K, Severi G, Hodge A, Brinkman M, English DR, et al. Dietary patterns and risk of breast cancer. Br J Cancer. 2011. February;104(3):524–31. 10.1038/sj.bjc.6606044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Agurs-Collins T, Rosenberg L, Makambi K, Palmer JR, Adams-Campbell L. Dietary patterns and breast cancer risk in women participating in the Black Women’s Health Study. Am J Clin Nutr. 2009. September 1;90(3):621–8. 10.3945/ajcn.2009.27666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kurotani K, Budhathoki S, Joshi AM, Yin G, Toyomura K, Kono S, et al. Dietary patterns and colorectal cancer in a Japanese population: The Fukuoka Colorectal Cancer Study. Br J Nutr. 2010. December;104(11):1703–11. 10.1017/S0007114510002606 [DOI] [PubMed] [Google Scholar]
- 36.Helen‐Ng LC, Razak IA, Ghani WMN, Marhazlinda J, Norain AT, Jallaludin R-LR, et al. Dietary pattern and oral cancer risk–a factor analysis study. Community Dent Oral Epidemiol. 2012;40(6):560–6. 10.1111/j.1600-0528.2012.00704.x [DOI] [PubMed] [Google Scholar]
- 37.Chan JM, Gong Z, Holly EA, Bracci PM. Dietary patterns and risk of pancreatic cancer in a large population-based case-control study in the San Francisco Bay Area. Nutr Cancer. 2013;65(1):157–64. 10.1080/01635581.2012.725502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Castelló A, Pollán M, Buijsse B, Ruiz A, Casas AM, Baena-Cañada JM, et al. Spanish Mediterranean diet and other dietary patterns and breast cancer risk: case–control EpiGEICAM study. Br J Cancer. 2014. September;111(7):1454–62. 10.1038/bjc.2014.434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tumas N, Niclis C, Aballay LR, Osella AR, Díaz M del P. Traditional dietary pattern of South America is linked to breast cancer: an ongoing case–control study in Argentina. Eur J Nutr. 2014. March 1;53(2):557–66. 10.1007/s00394-013-0564-0 [DOI] [PubMed] [Google Scholar]
- 40.Park Y, Lee J, Oh JH, Shin A, Kim J. Dietary patterns and colorectal cancer risk in a Korean population. Medicine (Baltimore) [Internet]. 2016. June 24 [cited 2018 Jul 3];95(25). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4998300/. 10.1200/JCO.2015.66.1181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shin S, Saito E, Inoue M, Sawada N, Ishihara J, Takachi R, et al. Dietary pattern and breast cancer risk in Japanese women: the Japan Public Health Center-based Prospective Study (JPHC Study). Br J Nutr. 2016. May;115(10):1769–79. 10.1017/S0007114516000684 [DOI] [PubMed] [Google Scholar]
- 42.Krusińska B, Hawrysz I, Słowińska MA, Wądołowska L, Biernacki M, Czerwińska A, et al. Dietary patterns and breast or lung cancer risk: A pooled analysis of 2 case-control studies in north-eastern Poland. Adv Clin Exp Med Off Organ Wroclaw Med Univ. 2017. December;26(9):1367–75. 10.17219/acem/65433 [DOI] [PubMed] [Google Scholar]
- 43.Mehta RS, Song M, Nishihara R, Drew DA, Wu K, Qian ZR, et al. Dietary Patterns and Risk of Colorectal Cancer: Analysis by Tumor Location and Molecular Subtypes. Gastroenterology. 2017. June 1;152(8):1944–1953.e1. 10.1053/j.gastro.2017.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mehta RS, Nishihara R, Cao Y, Song M, Mima K, Qian ZR, et al. Association of Dietary Patterns With Risk of Colorectal Cancer Subtypes Classified by Fusobacterium nucleatum in Tumor Tissue. JAMA Oncol. 2017. July 1;3(7):921–7. 10.1001/jamaoncol.2016.6374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cottet V, Touvier M, Fournier A, Touillaud MS, Lafay L, Clavel-Chapelon F, et al. Postmenopausal Breast Cancer Risk and Dietary Patterns in the E3N-EPIC Prospective Cohort Study. Am J Epidemiol. 2009. November 15;170(10):1257–67. 10.1093/aje/kwp257 [DOI] [PubMed] [Google Scholar]
- 46.Buck K, Vrieling A, Flesch-Janys D, Chang-Claude J. Dietary patterns and the risk of postmenopausal breast cancer in a German case–control study. Cancer Causes Control. 2011. February 1;22(2):273–82. 10.1007/s10552-010-9695-2 [DOI] [PubMed] [Google Scholar]
- 47.Safari A, Shariff ZM, Kandiah M, Rashidkhani B, Fereidooni F. Dietary patterns and risk of colorectal cancer in Tehran Province: a case–control study. BMC Public Health. 2013. March 12;13:222 10.1186/1471-2458-13-222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Melkonian SC, Daniel CR, Hildebrandt MAT, Tannir NM, Ye Y, Chow W-H, et al. Joint Association of Genome-Wide Association Study–Identified Susceptibility Loci and Dietary Patterns in Risk of Renal Cell Carcinoma Among Non-Hispanic Whites. Am J Epidemiol. 2014. September 1;180(5):499–507. 10.1093/aje/kwu158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tu H, Heymach JV, Wen C-P, Ye Y, Pierzynski JA, Roth JA, et al. Different dietary patterns and reduction of lung cancer risk: A large case-control study in the U.S. Sci Rep. 2016. 27;6:26760 10.1038/srep26760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Van Ryswyk K, Villeneuve PJ, Johnson KC, Epidemiology Research Group TCCR. Dietary patterns and the risk of female breast cancer among participants of the Canadian National Enhanced Cancer Surveillance System. Can J Public Health Rev Can Sante Publique. 2016. 27;107(1):e49–55. 10.17269/cjph.107.5230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tayyem RF, Bawadi HA, Shehadah I, Agraib LM, AbuMweis SS, Al-Jaberi T, et al. Dietary patterns and colorectal cancer. Clin Nutr. 2017. June 1;36(3):848–52. 10.1016/j.clnu.2016.04.029 [DOI] [PubMed] [Google Scholar]
- 52.Marchioni DML, Latorre M do RD de O, Eluf-Neto J, Wünsch-Filho V, Fisberg RM. Identification of dietary patterns using factor analysis in an epidemiological study in São Paulo. Sao Paulo Med J. 2005. May;123(3):124–7. 10.1590/s1516-31802005000300007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cunha DB, Almeida RMVR de, Sichieri R, Pereira RA. Association of dietary patterns with BMI and waist circumference in a low-income neighbourhood in Brazil. Br J Nutr. 2010. September;104(6):908–13. 10.1017/S0007114510001479 [DOI] [PubMed] [Google Scholar]
- 54.Cunha DB, Sichieri R, Almeida RMVR de, Pereira RA. Factors associated with dietary patterns among low-income adults. Public Health Nutr. 2011. September;14(9):1579–85. 10.1017/S136898001000354X [DOI] [PubMed] [Google Scholar]
- 55.Trindade de Castro MB. Un Patrón Dietético Mixto Se Asocia Con Un Menor Declive En El Cambio. Nutr Hosp. 2014. March 1;(3):519–23. [Google Scholar]
- 56.Massarani FA, Cunha DB, Muraro AP, Souza B da SN de, Sichieri R, Yokoo EM. Agregação familiar e padrões alimentares na população brasileira. Cad Saúde Pública. 2015. December;31(12):2535–45. 10.1590/0102-311X00090314 [DOI] [PubMed] [Google Scholar]
- 57.Castro MBT de, Vilela AAF, Oliveira ASD de, Cabral M, Souza RAG de, Kac G, et al. Sociodemographic characteristics determine dietary pattern adherence during pregnancy. Public Health Nutr. 2016. May;19(7):1245–51. 10.1017/S1368980015002700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wie G-A, Cho Y-A, Kang H -h, Ryu KA, Yoo M-K, Kim J, et al. Identification of major dietary patterns in Korean adults and their association with cancer risk in the Cancer Screening Examination Cohort. Eur J Clin Nutr. 2017. October;71(10):1223–9. 10.1038/ejcn.2017.6 [DOI] [PubMed] [Google Scholar]
- 59.Liu X, Wang X, Lin S, Lao X, Zhao J, Song Q, et al. Dietary patterns and the risk of esophageal squamous cell carcinoma: A population-based case–control study in a rural population. Clin Nutr. 2017. February 1;36(1):260–6. 10.1016/j.clnu.2015.11.009 [DOI] [PubMed] [Google Scholar]
- 60.Butler LM, Wu AH, Wang R, Koh W-P, Yuan J-M, Yu MC. A vegetable-fruit-soy dietary pattern protects against breast cancer among postmenopausal Singapore Chinese women. Am J Clin Nutr. 2010. April 1;91(4):1013–9. 10.3945/ajcn.2009.28572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jordan I, Hebestreit A, Swai B, Krawinkel MB. Dietary patterns and breast cancer risk among women in northern Tanzania: a case–control study. Eur J Nutr. 2013. April 1;52(3):905–15. 10.1007/s00394-012-0398-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Levy-Costa RB, Sichieri R, Pontes N dos S, Monteiro CA. Household food availability in Brazil: distribution and trends (1974–2003). Rev Saúde Pública. 2005. August;39(4):530–40. 10.1590/s0034-89102005000400003 [DOI] [PubMed] [Google Scholar]
- 63.Kearney M, Kearney JM, Dunne A, Gibney MJ. Sociodemographic determinants of perceived influences on food choice in a nationally representative sample of Irish adults. Public Health Nutr. 2000. June;3(2):219–26. 10.1017/s1368980000000252 [DOI] [PubMed] [Google Scholar]
- 64.Park S-Y, Murphy SP, Wilkens LR, Yamamoto JF, Sharma S, Hankin JH, et al. Dietary Patterns Using the Food Guide Pyramid Groups Are Associated with Sociodemographic and Lifestyle Factors: The Multiethnic Cohort Study. J Nutr. 2005. April 1;135(4):843–9. 10.1093/jn/135.4.843 [DOI] [PubMed] [Google Scholar]
- 65.Kriaucioniene V, Petkeviciene J, Klumbiene J. Dietary patterns and their association with sociodemographic factors in Lithuanian adult population. Med Kaunas Lith. 2008;44(10):799–804. [PubMed] [Google Scholar]
- 66.Luksiene DI, Baceviciene M, Tamosiunas A, Daugeliene E, Kranciukaite D. Health, alcohol and psychosocial factors in Eastern Europe study: dietary patterns and their association with socio-demographic factors in the Lithuanian urban population of Kaunas city. Int J Public Health. 2011. April;56(2):209–16. 10.1007/s00038-010-0170-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sánchez-Villegas A, Delgado-Rodríguez M, Martínez-González MÁ, de Irala-Estévez J. Gender, age, socio-demographic and lifestyle factors associated with major dietary patterns in the Spanish Project SUN (Seguimiento Universidad de Navarra). Eur J Clin Nutr. 2003. February;57(2):285–92. 10.1038/sj.ejcn.1601528 [DOI] [PubMed] [Google Scholar]
- 68.Knudsen VK, Matthiessen J, Biltoft-Jensen A, Sørensen MR, Groth MV, Trolle E, et al. Identifying dietary patterns and associated health-related lifestyle factors in the adult Danish population. Eur J Clin Nutr. 2014. June;68(6):736–40. 10.1038/ejcn.2014.38 [DOI] [PubMed] [Google Scholar]
- 69.Pala V, Sieri S, Masala G, Palli D, Panico S, Vineis P, et al. Associations between dietary pattern and lifestyle, anthropometry and other health indicators in the elderly participants of the EPIC-Italy cohort. Nutr Metab Cardiovasc Dis. 2006. April 1;16(3):186–201. 10.1016/j.numecd.2005.05.009 [DOI] [PubMed] [Google Scholar]
- 70.Mohd Shahrin FI, Omar N, Mat Daud Z‘Azuan, Zakaria NF. Factors associated with food choices among elderly: a scoping review. Malays J Nutr. 2019. November 22;25(2):185–98. [Google Scholar]
- 71.Bezerra IN, Souza A de M, Pereira RA, Sichieri R. Consumo de alimentos fora do domicílio no Brasil. Rev Saúde Pública. 2013. February;47:200s–11s. 10.1590/s0034-89102013000700006 [DOI] [PubMed] [Google Scholar]
- 72.Bernardo GL, Jomori MM, Fernandes AC, Proença RP da C. Food intake of university students. Rev Nutr. 2017. December;30(6):847–65. 10.1186/s12937-017-0305-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Thorpe MG, Milte CM, Crawford D, McNaughton SA. A comparison of the dietary patterns derived by principal component analysis and cluster analysis in older Australians. Int J Behav Nutr Phys Act. 2016. February 29;13(1):30 10.1186/s12966-016-0353-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kerver JM, Yang EJ, Bianchi L, Song WO. Dietary patterns associated with risk factors for cardiovascular disease in healthy US adults. Am J Clin Nutr. 2003. December 1;78(6):1103–10. 10.1093/ajcn/78.6.1103 [DOI] [PubMed] [Google Scholar]
- 75.Ferreira JP, Leeson G, Melhado VR, Ferreira JP, Leeson G, Melhado VR. Cartographies of aging in the rural context: race/ethnicity, gender, schooling and social class. Trab Educ E Saúde. 2019;17(1):e0017612. [Google Scholar]
- 76.Goes EF, Ramos D de O, Ferreira AJF. Racial health inequalities and the COVID-19 pandemic. Trab Educ E Saúde. 2020. May 28;18(3):e00278110. [Google Scholar]
- 77.Olinto MTA, Olinto BA. Raça e desigualdade entre as mulheres: um exemplo no sul do Brasil. Cad Saúde Pública. 2000. December;16(4):1137–42. 10.1590/s0102-311x2000000400033 [DOI] [PubMed] [Google Scholar]
- 78.Kell KP, Judd SE, Pearson KE, Shikany JM, Fernández JR. Associations between socio-economic status and dietary patterns in US black and white adults. Br J Nutr. 2015. June 14;113(11):1792–9. 10.1017/S0007114515000938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Irala-Estévez JD, Groth M, Johansson L, Oltersdorf U, Prättälä R, Martínez-González MA. A systematic review of socio-economic differences in food habits in Europe: consumption of fruit and vegetables. Eur J Clin Nutr. 2000. September;54(9):706–14. 10.1038/sj.ejcn.1601080 [DOI] [PubMed] [Google Scholar]
- 80.Mishra GD, McNaughton SA, Ball K, Brown WJ, Giles GG, Dobson AJ. Major dietary patterns of young and middle aged women: results from a prospective Australian cohort study. Eur J Clin Nutr. 2010. October;64(10):1125–33. 10.1038/ejcn.2010.121 [DOI] [PubMed] [Google Scholar]
- 81.Engeset D, Alsaker E, Ciampi A, Lund E. Dietary patterns and lifestyle factors in the Norwegian EPIC cohort: The Norwegian Women and Cancer (NOWAC) study. Eur J Clin Nutr. 2005. May;59(5):675–84. 10.1038/sj.ejcn.1602129 [DOI] [PubMed] [Google Scholar]
- 82.Oppert J-M, Thomas F, Charles M-A, Benetos A, Basdevant A, Simon C. Leisure-time and occupational physical activity in relation to cardiovascular risk factors and eating habits in French adults. Public Health Nutr. 2006. September;9(6):746–54. 10.1079/phn2005882 [DOI] [PubMed] [Google Scholar]
- 83.Charreire H, Kesse-Guyot E, Bertrais S, Simon C, Chaix B, Weber C, et al. Associations between dietary patterns, physical activity (leisure-time and occupational) and television viewing in middle-aged French adults. Br J Nutr. 2011. March;105(6):902–10. 10.1017/S000711451000440X [DOI] [PubMed] [Google Scholar]
- 84.Liangpunsakul S. Relationship between alcohol intake and dietary pattern: Findings from NHANES III. World J Gastroenterol. 2010. August 28;16(32):4055–60. 10.3748/wjg.v16.i32.4055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kesse E, Clavel-Chapelon F, Slimani N, van Liere M. Do eating habits differ according to alcohol consumption? Results of a study of the French cohort of the European Prospective Investigation into Cancer and Nutrition (E3N-EPIC). Am J Clin Nutr. 2001. September 1;74(3):322–7. 10.1093/ajcn/74.3.322 [DOI] [PubMed] [Google Scholar]
- 86.Fawehinmi TO, Ilomäki J, Voutilainen S, Kauhanen J. Alcohol Consumption and Dietary Patterns: The FinDrink Study. PLoS ONE. 2012. June 12;7(6):e38607 10.1371/journal.pone.0038607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Dallongeville J, Marécaux N, Fruchart J-C, Amouyel P. Cigarette Smoking Is Associated with Unhealthy Patterns of Nutrient Intake: a Meta-analysis. J Nutr. 1998. September 1;128(9):1450–7. 10.1093/jn/128.9.1450 [DOI] [PubMed] [Google Scholar]
- 88.Vaz J dos S, Buffarini R, Kac G, Bielemann RM, Oliveira I, Menezes AB, et al. Dietary patterns are associated with blood lipids at 18-year-olds: a cross-sectional analysis nested in the 1993 Pelotas (Brazil) birth cohort. Nutr J. 2018;17(1):1–12. 10.1186/s12937-017-0311-0 [DOI] [PMC free article] [PubMed] [Google Scholar]