Abstract
Cardiovascular diseases have been recognized as the main cause of death all over the world. Recently, the established cardio-ankle vascular index (CAVI) has become known as an index of arterial stiffness of the arterial tree from the origin of the aorta to the ankle. CAVI reflects the progress of arteriosclerosis, and a rapid rise in CAVI indicates arterial smooth muscle cell contraction. Considering the vasculature of the atheroma where vasa vasorum penetrates the smooth muscle cell layer and supplies blood to the intimal atheromatous lesion, a rapid rise of CAVI means “choked” atheroma. Thus, we proposed a “smooth muscle cell contraction” hypothesis of plaque rupture.
Keywords: arterial stiffness, atherosclerosis, smooth muscle cell contraction, CAVI
Introduction
Atherosclerosis is the basic pathological condition of cerebro-cardiovascular diseases, and several risk factors such as hypertension, diabetes mellitus, dyslipidemia, and obesity, especially visceral fat accumulation are known. Although the mechanism of its progression has been proposed,1,2 to date, valuable indicators for impending cardiovascular events remain insufficient.
Sometimes, we met several cases who were attacked by cerebro-cardiovascular event just after a mental shock and/or acute onset of poor control of the above risks. Considering the predicting factors of those impending events, it is necessary to assess the structure and vasculature of the atheromatous lesion. The intimal atheromatous lesion is supplied by vasa vasorum via the adventitia. Namely, new microvessels penetrate the medial smooth muscle layer to enter the intimal atherosclerotic lesion and supply the blood. Considering this structural feature, it can be supposed that rapid contraction of the smooth muscle cells may squeeze the vasa vasorum and consequently block the blood supply into the intimal atheromatous lesion. The “choked” atheroma subsequently causes necrosis, leading to plaque rupture. Thus, we proposed the “smooth muscle cell contraction” hypothesis of plaque rupture.
Cardio-Ankle Vascular Index (CAVI) as an Evaluation Index of Atherosclerosis Progression
Atherosclerosis has been recognized as the major cause of vascular disease and its related death. However, there are still no sufficient indices that are viable means of forecasting impending cerebro-cardiovascular events. Traditionally, arterial stiffness evaluated by pulse wave velocity (PWV) has been regarded as a marker of atherosclerosis, and its value has been recognized as a predictor of cardiovascular events in prospective tests.3–9 However, PWV is intrinsically dependent on blood pressure at the measuring time; PWV increases or decreases in accordance with blood pressures.10,11 Therefore, PWV, as an analysis of arterial stiffness, is not worthy for forecasting impending cardiovascular events. Cardio-ankle vascular index (CAVI), which reflects arterial stiffness from the origin of the aorta to the ankle, was developed in 2004.12 CAVI is derived from stiffness parameter beta proposed by Hayashi et al, and the equation has been modified using Bramwell-Hill’s equation.13–15 The feature of CAVI is its independency from blood pressure at the time of measurement.10,11 Prospective studies have already been reported, and the role of CAVI as a long-term prognosis predictor of cardiovascular events is well established.16–22
The usefulness of CAVI in clinical medicine is widely accepted by many researchers. Increased CAVI has been reported to be related to aging (men > women),23 coronary artery diseases (CAD),24 chronic kidney diseases,25 cerebral infarction,26 metabolic syndrome,27 diabetes mellitus,28 dyslipidemia,29 smoking,30 obstructive sleep apnea syndrome (OSA),31 hypertension,32 cognitive decline33 and emotional stress.34 Decreased CAVI has been reported to be related to weight reduction,35 blood glucose control,28 administration of antihypertensive agents (angiotensin II receptor blocker > calcium antagonist),32 lipid-lowering agents like statin,36 stop smoking37 and continuous pulmonary assistance for OSA.38 Matsushita reported the association of CAVI and CVD outcomes in the systematic review.39 They concluded that CAVI was higher in patients with CVD than those without. In terms of the prospective prognostic value of CAVI, they found a limited number of studies, but they indicated a modest association between CAVI and CVD risks. The relationship between stroke and CAVI was also reported in several small studies.40–42 CAVI has been established as an index of atherosclerosis, and a high CAVI value has been shown to indicate that the atheromatous lesion is already in an advanced state.
Examples of a Rapid Rise in CAVI and Cerebro-Cardiovascular Events
It has been reported that the frequency of cardiovascular events increases just after a huge earthquake.43–48 Several influential factors have been reported, such as hypertension, mental stress, and sympathetic nerve activation.49–55 But the precise mechanisms have not been fully clarified.
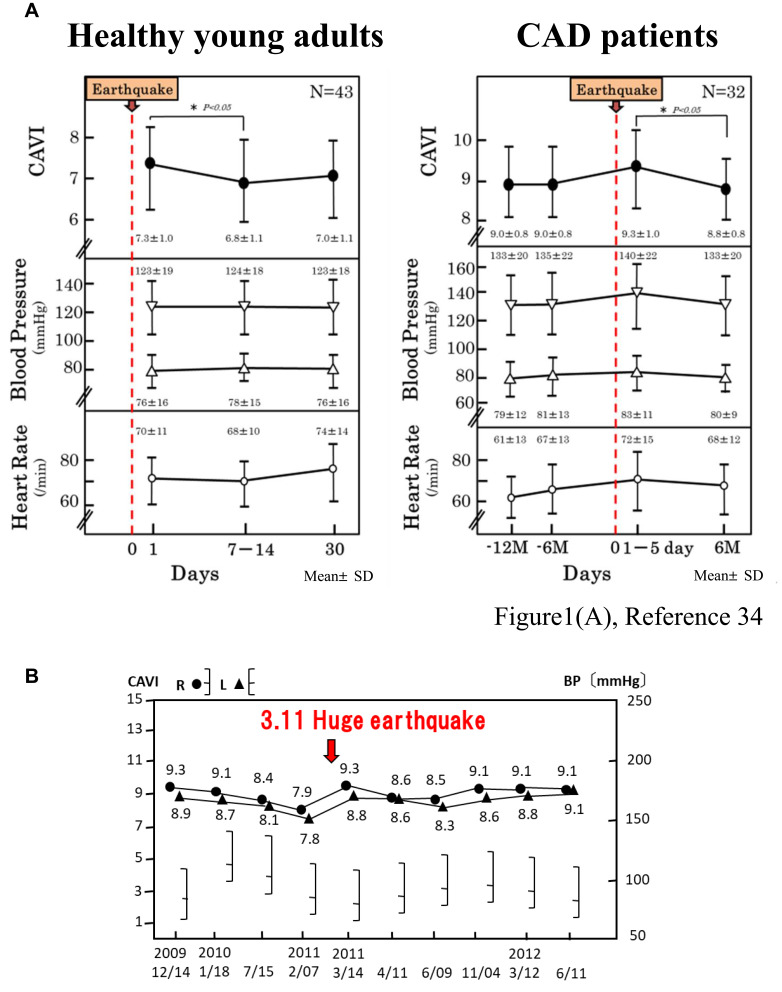
We encountered cases of transiently enhanced arterial stiffness as evaluated by CAVI after a huge earthquake; On March 11, 2011, an earthquake of magnitude 9.0 occurred on the Pacific coast of Tohoku, Honshu Island, Japan, at 14:46 local time (the Great East Japan Earthquake). It was followed by a series of powerful aftershocks, with 31 earthquakes of magnitude larger than 6 over 3 days. Our institute (Toho University Sakura Medical Center Hospital) was situated about 300 km away from the epicenter. The building was strongly shaken and part of a wall collapsed. An unusual crisis occurred in our town. The number of patients who suffered from cerebral bleeding increased by two-fold compared to the several years before the earthquake. Furthermore, the number of deaths in our town increased in the year 2011 compared to 2009, 2010 and 2012.34 We thought this increase in mortality in 2011 was primarily due to psychological stress caused by the huge earthquake. As shown in Figure 1A, Shimizu et al reported that CAVI was enhanced transiently just after the earthquake in healthy people and in CAD patients. Particularly in healthy people, CAVI increased even though blood pressure was not raised significantly.34 Figure 1B shows the one case with the metabolic disorder who had psychological damage by the huge earthquake and increased CAVI. He had been treated for diabetes mellitus, hypertension and dyslipidemia in our hospital. Because his hometown was damaged by the huge earthquake and subsequent nuclear power plant troubles caused by the ensuing tsunami, he felt deep stress and his CAVI increased considerably.
Figure 1.
Increase in cardio-ankle vascular index (CAVI) just after the Great East Japan Earthquake (M9; March 11, 2011). The immediate increase was seen in both healthy young adults and in coronary artery disease (CAD) patients, despite their relatively stable blood pressure (A). Some patients showed a marked increase in CAVI following the earthquake, such as in the CAVI results of the diabetic hypertense patient shown here (B) who suffered psychological stress.
Ethics and Statistical Analysis
The institutional review board of Toho University Sakura Medical Center approved the study (NO. 2011–004). Each participant gave written informed consent after receiving a detailed description of the procedures in accordance with the Declaration of Helsinki.
One-way ANOVA was performed to determine whether the differences among groups were statically significant and the Tukey’s test was used for post hoc comparisons. A P-value of <0.05 was considered significant. Statistical analysis was performed using SPSS software package (PASW Statistics 18, Chicago, IL, USA) (Figure 1A).34
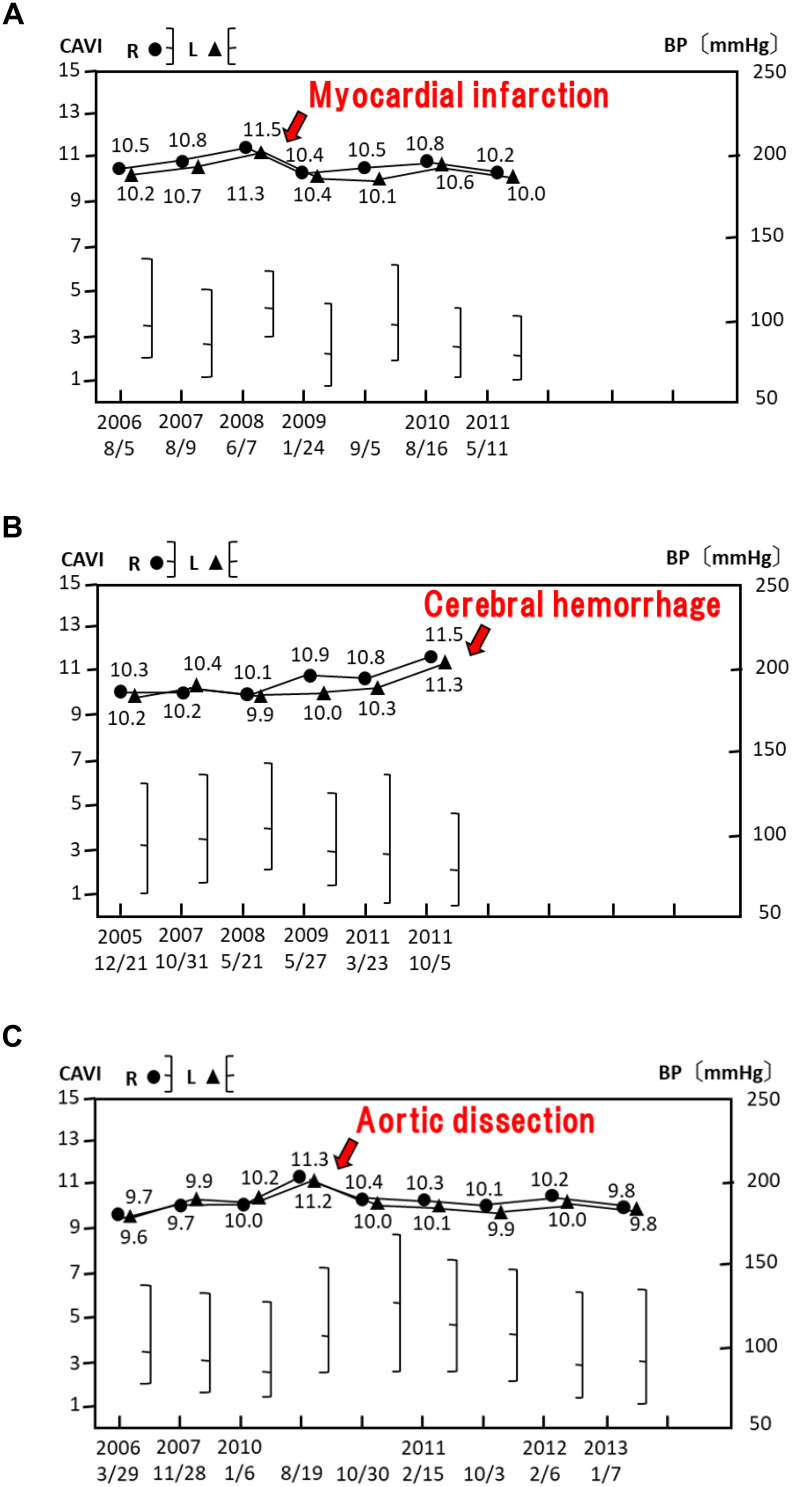
Other cases are shown in Figure 2; we have observed the CAVI changes in several patients who suffered from myocardial infarction, cerebral hemorrhage and aortic dissection. These cases showed a rapid rise in CAVI by Δ0.5–Δ1.0 with a high baseline CAVI (>10) at 2 weeks before or several months before their cardiac events. The case shown in Figure 2A had an acute myocardial infarction 4 months after a rapid rise in CAVI. Figure 2B shows a case who suffered from cerebral hemorrhage 7 days after a rapid rise in CAVI and that in Figure 2C suffered from an aortic dissection 2 weeks after a rapid rise in CAVI.
Figure 2.
Increase in the cardio-ankle vascular index (CAVI) prior to cerebro-cardiovascular events. Cases with a rapid rise in CAVI who had acute myocardial infarction 4 months later (A), cerebral hemorrhage 7 days later (B), and aortic dissection 2 weeks later (C).
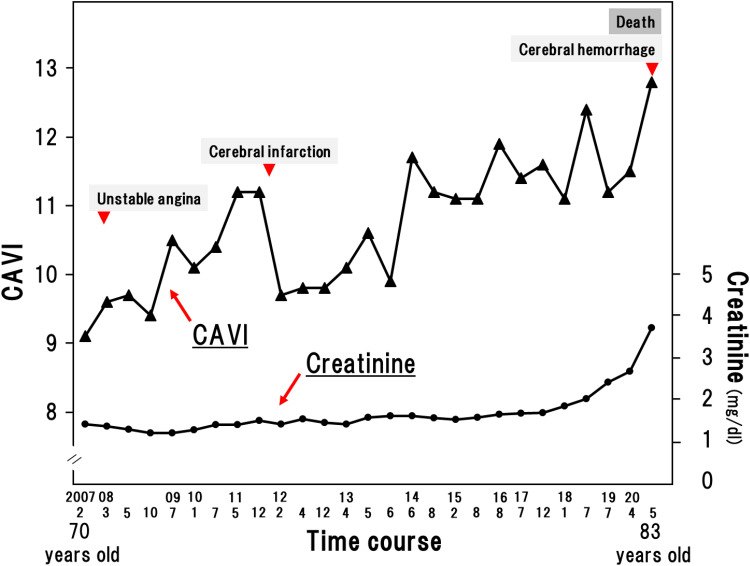
Figure 3 shows the CAVI over 13 years in an atherosclerotic patient who came to our hospital. In the beginning, his baseline CAVI was already above nine. He developed unstable angina and cerebral infarction when his work was busy as a chef of his restaurant, and finally died of cerebral hemorrhage after a rapid rise in CAVI (11.5 to 12.8 in the last month). This case shows the gradual increase in CAVI with aging and the development of atherosclerotic diseases.
Figure 3.
Increase in cardio-ankle vascular index (CAVI) over 13 years in an atherosclerosis patient with a high baseline CAVI. This patient showed a rapid rise in CAVI (to 11.5) a few months before cerebral infarction and a high rapid rise to 12.8 just prior to cerebral hemorrhage.
The above-mentioned observations cannot be considered to be due simply to chance. We encountered these cases incidentally, and proving these phenomena by a prospective study is not easy. However, these are facts in our daily practice, and we could not deny the possibility that a rapid rise in CAVI might be a prodrome of impending cerebro-cardiovascular events. Based on our experience, it might be said that patients with advanced atherosclerosis should receive particular attention when CAVI rises suddenly.
CAVI Reflects the Contraction and Relaxation of Vascular Smooth Muscle Cells (VSMCs)
CAVI has been shown to be elevated or decreased with the administration of various vasoactive agents. It is known that the arterial wall deforms largely and nonlinearly, which are characteristics unique to soft biological tissues. The key which controls arterial elasticity is the function of VSMCs. We consider that CAVI reflects the contraction and relaxation of VSMCs in arteries based on the available evidence.
Shirai et al reported that CAVI values are not affected by blood pressure when blood pressure was reduced with the administration of the β1 blocker, metoprolol. The β1 blocker decreases blood pressure by reduction of heart muscle contraction, and therefore, arterial stiffness measured as CAVI is not changed even though blood pressure changes.10 Furthermore, when the α1 blocker, doxazosin, is administered, CAVI decreases as blood pressure decreases; the α1 blocker reduces blood pressure by reduction of vascular smooth muscle contraction.10 This reduction of vascular smooth muscle contraction induces a decrease in CAVI. This result might imply that CAVI reflects the arterial stiffness based on vascular smooth muscle contraction.
Shimizu et al56 and Yamamoto et al57 reported the effect of nitroglycerin administration on CAVI. After administration of nitroglycerin, the stiffness of the arteries from the origin of the aorta to the ankle as measured by CAVI decreased in both the healthy volunteers and CAD patients. The function of VSMCs was even present in CAD patients. It is difficult to strictly distinguish this organic stiffness and functional stiffness. We might be able to guess the organic stiffness as the baseline CAVI, and functional stiffness as the rapidly changed CAVI due to nitroglycerin. These findings demonstrate that CAVI reflects organic and functional arterial stiffness.
As a practical clinical example, we have already reported that CAVI is affected by obstructive sleep apnea, blood glucose control, and body weight.58 On the other hand, Lim J reported on the influence of the cold pressor test on changes in CAVI.59 It is well known that “winter peak” of CVD-related hospitalizations and mortality is due to cold stress.60 Coronary spasms are also more likely to be triggered by exposure to cold and stress in winter.61–64 Taken together, it can be said that CAVI reflects the contraction and relaxation of VSMCs.
Vasculature of the Atheromatous Lesion
To understand the meaning of rapidly raised CAVI as a prodrome of cardiovascular event, the structure of an atheromatous lesion and its vasculature need to be reviewed. Arteries consist of three morphologically distinct layers: innermost layer, the intima; the middle layer, the media; and the external layer, the adventitia. The intima is bounded on the lumen by a continuous layer of endothelial cells that form a protective barrier between the blood and artery walls.
Atheromatous lesions are subdivided into three stages: fatty streak, fibrous plaque, and complicated lesions.65 The fatty streak is characterized by the accumulation of lipid-laden macrophages surrounded by lipid extracellularly in the intima.66 Fibrous plaques consist of an intimal accumulation of proliferated smooth muscle cells surrounded by a large amount of connective tissue, which appears to form a “cap” that covers a deeper accumulation of both intra- and extracellular lipids. Necrosis and cell debris are usually associated with this lipid accumulation. The advanced or so-called complicated lesion appears to be a fibrous plaque that has been altered as a result of hemorrhage, calcification, necrosis, thrombosis, and further cell degenerative change mixed with cell proliferation, and advanced lesions are called vulnerable plaque.67 Thus, the lesions of atherosclerosis contain newly migrated proliferative smooth muscle cells (synthetic type), together with newly formed connective tissue, and deposits of lipid. These pathological changes are usually limited in the intima, and medial smooth muscle cell (contractile type) layer remains.
Next, it is important to define the blood supply of atheromatous lesions. It was previously thought that the nutrients and oxygen are supplied by diffusion through the intimal endothelial cell layer from the lumen. As the stage of atherosclerosis advances, hypoxic conditions of the lesion promote the growth of microvessels derived from the vasa vasorum. Newly developed microvessels supply nutrients and oxygen to the outer medial layer and intimal atheromatous lesions.68,69 It is known that the advanced stage of intimal atheromatous lesions is rich in microvessels.70 The notable point is that the vasa vasorum penetrates the medial smooth muscle cell layer from the adventitia to the intimal layer. The medial smooth muscle cells of the arterial wall are able to contract and relax, even at the advanced stage of arteriosclerosis. These conclusions are supported by the observation that CAVI is decreased by the administration of nitroglycerin among both healthy people and patients with CAD. Therefore, when medial smooth muscle cells contract, the penetrating microvessels are “choked”. Resultantly, the downstream area of intima atheromatous lesions would become ischemic. Furthermore, prolonged ischemia would cause necrosis in the core of atheromatous lesions. Around the necrotic core, inflammatory reactions are augmented; macrophages accumulate, digest the surrounding matrix components and cause the atheromatous lesion to rupture.71 Such a rupture causes thrombus formation in the arterial wall cavity and cardiovascular events ensue.
To support this hypothesis, it must be proven that blood supply into the intimal atheromatous lesion comes from the vasa vasorum via the adventitia, and that this blood flow can be stopped by contraction of smooth muscle cells.
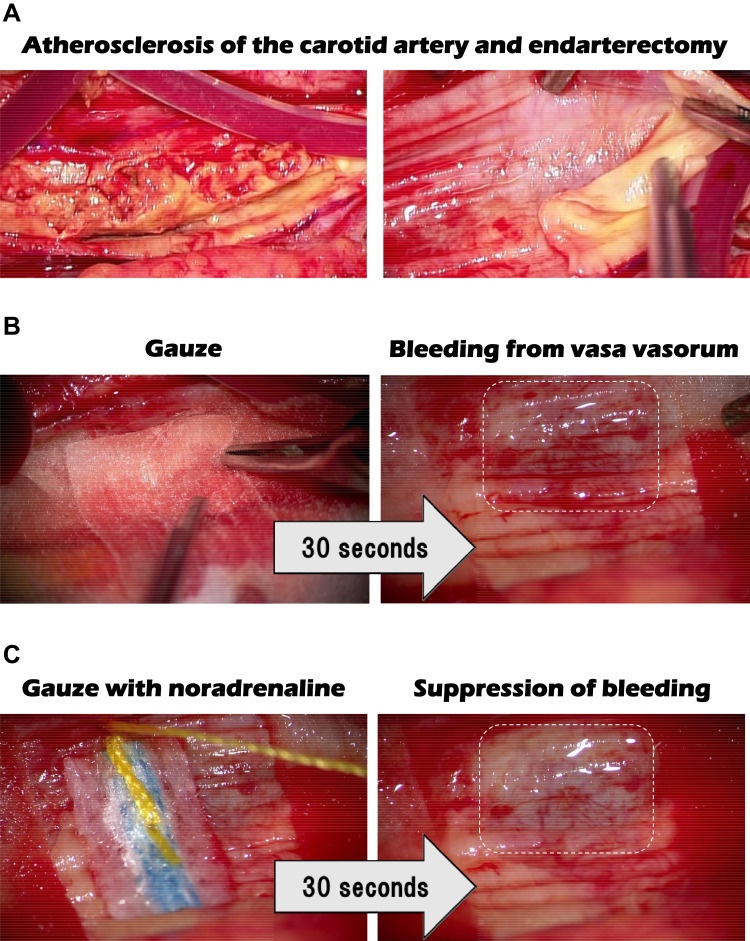
We undertook carotid endarterectomy of the patient whose cervical artery had more than 90% stenosis by an atheromatous lesion (Figure 4). At this operation, the intimal atheromatous layer of the carotid artery was peeled off, and the medial smooth muscle layer was denuded. Just after peeling off the intimal layer, bleeding was immediately observed on the surface of the medial smooth muscle cell layer. However, when the surface of this medial smooth muscle layer was covered with gauze dipped in the noradrenaline, bleeding was inhibited. Such procedures are routinely performed by brain surgeons. This phenomenon indicated that the blood supply of the intimal atheromatous lesion was mediated by the vasa vasorum, and this blood flow was stopped by contraction of the medial smooth muscle cells.
Figure 4.
Carotid endarterectomy of a patient with 90% stenosis of the cervical artery. (A) Atherosclerosis of the carotid artery and endarterectomy; (B) Gauze was applied for the bleeding which occurred after peeling off the intimal atheromatous layer of the carotid artery; (C) Gauze, dipped in the catecholamine noradrenaline, was applied and inhibited the bleeding, indicating that the blood supply of the intimal atheromatous lesion was from the vasa vasorum and that it was stopped by contraction of the medial smooth muscle cells.
Decreasing the blood flow, intimal atheroma might cause necrosis of the plaque core, leading to rupture. Osada et al reported that most aortic dissections initially developed in the outer third of the media alongside the vasa vasorum. They suggested that dysfunction of the vasa vasorum might play a key role in long-standing ischemia or malnutrition of the aortic media, and that the resultant necrotic layer would provoke dissecting aneurysm.72
It is also mentioned that spasms caused by smooth muscle contraction can play a key role in acute coronary events.
Smooth Muscle Cell Contraction Hypothesis for Plaque Rupture
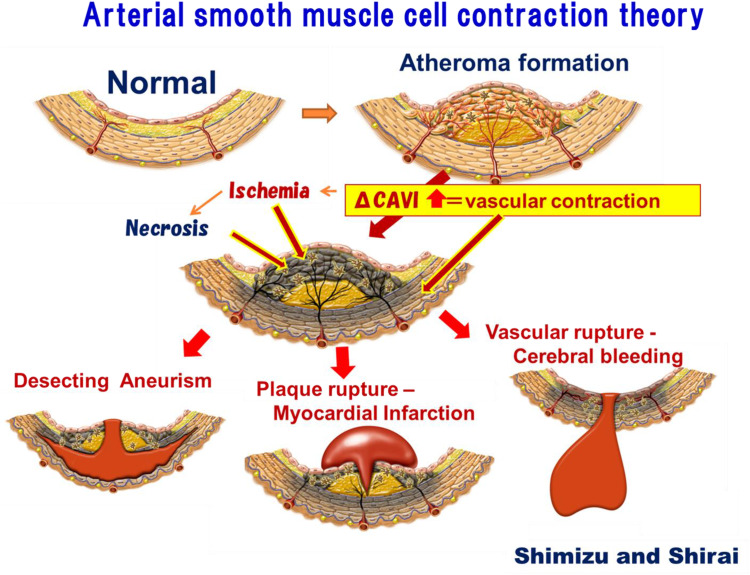
On the basis of the data and features of the vasculature of atheromatous lesions described above, we proposed “the smooth muscle contraction” hypothesis for cardiovascular events. This process is shown in Figure 5. Myocardial infarction due to plaque rupture, dissecting aneurism and brain hemorrhage might be explained as follows:
Figure 5.
“Smooth muscle cell contraction” hypothesis for plaque rupture.
First step:
Atheromatous lesions consist of an intimal thickness composed of proliferated synthetic type of smooth muscle cells, and fibrous components, such as collagen and elastin. This stage is called the fibrous cap, which involves the enhancement of CAVI. In this stage, the vasa vasorum develops and microvessels begin to penetrate the medial smooth muscle cell layer and supply blood to the intimal atheromatous lesion.
Second step:
When a person is subjected to a stressful environment such as a huge earthquake or other natural disasters, various types of personal mental shock become a burden with advanced stages of atheromatous lesions (high basal CAVI >10); the medial smooth muscle cells begin to contract and then a rapid rise in CAVI would occur. The contracted smooth muscle cells “choke” microvessels from the vasa vasorum, stopping the blood flow into the intimal area, and then vulnerable plaque becomes ischemic and subsequently necrotic. Around the formed necrotic core, macrophages gather and dissolve the necrotic tissues. Then, the vulnerable plaque would be ruptured. In the case of the coronary artery, plaque rupture causes thrombus formation at the surface of the artery, causing myocardial infarction. In the case of the aorta, a necrotic core develops in the wall and causes dissecting aneurysm. In the case of a brain artery, the thin arterial wall is easily ruptured by necrosis of the smooth muscle cell layer, causing brain hemorrhage. These are the processes in which smooth muscle contraction causes cardiovascular events. To predict the looming vascular events, CAVI which detects rapid contraction of smooth muscle cells would be a distinctive indicator warning of conditions leading to such events. Thus, it is recommended to measure arterial stiffness with CAVI in short intervals (ie every week or every morning) when possible. Furthermore, we tentatively propose that a high basal value of CAVI is over 10 and enhanced ΔCAVI is over 0.7 for the sign of a looming cardiovascular event. Tentative basal value CAVI (= 10) was nearly mean CAVI (7.84) in Japanese + 2 x standard deviation (2x1.07).73 ΔCAVI (0.7) was correspondent to two times of coefficient variation (3.8%) of CAVI measurement12 These values are just tentative and might be changed in the future by the accumulation of abundant data. Sato Y reported that CAVI ≥ 10 contributed more to the occurrence of CV events than CAVI < 10 in the prospective study. Basal CAVI value 10 is corresponding to the upper 1/4 value for CVD event.20 In addition, Otsuka et al revealed that ⊿CAVI ≥ 0.5 during 6 months of observation period was associated with the high risk of CV event.74
How to Prevent Impending Cardiovascular Events by Monitoring CAVI
In the case that CAVI is measured continuously and the value is rapidly increased, what should be done? According to the smooth muscle cell contraction hypothesis, a rapid rise in CAVI is due to smooth muscle cell contraction by various types of stress. Therefore, in order to decrease CAVI, many therapeutic treatments should be attempted to relax the arterial smooth muscle cell contraction.
Available methods include light exercise, taking a bath and some medications that have been reported to decrease CAVI, such as administration of antihypertensive agents like olmesartan,32 lipid-lowering agents like pitavastatin,36 controlling diabetes mellitus,28 decrease body weight (in cases of metabolic syndrome),35 stop smoking37 and CPAP installation for OSA.38 In addition, the elimination of stress might be the most important. A comprehensive therapy plan should be considered case by case through monitoring of CAVI.
Conclusion and Future Perspectives
A rapid rise in CAVI in persons with a high basal CAVI might be a prodrome of serious cardiovascular events. This might be due to smooth muscle contraction induced by very stressful situations. Although this hypothesis has not been fully proven yet, it might be useful to provide an alert to let the patient try to relieve stress in order to relax the arterial smooth muscle cells and to avoid serious subsequent cardiovascular events. To monitor arterial stiffness, we now currently use CAVI; however, more easy and available instruments are expected in the future. Further studies are necessary to clarify which arterial stiffness might be well reflecting the coronary artery to verify this hypothesis.
Ethics
Everyone who participated in our past study gave written informed consent after receiving a detailed description of the procedures in accordance with the Declaration of Helsinki; the study was reviewed and approved by the Ethics Committee of Toho University or Toho University Sakura Medical Center.
Acknowledgments
We deeply appreciated the clinical physiology staff in Toho University Sakura Medical Center and Mrs. Fusako Watanabe.
Disclosure
The authors report no conflicts of interest related to this work.
References
- 1.Ross R, Glomset J. The pathogenesis of atherosclerosis. N Engl J Med. 1976;295:369–377, 420–425. doi: 10.1056/NEJM197608122950707 [DOI] [PubMed] [Google Scholar]
- 2.Bornfeldt KE. 2013 Russell Ross memorial lecture in vascular biology: cellular and molecular mechanisms of diabetes-accelerated atherosclerosis. Arterioscler Thromb Vasc Biol. 2014;34(4):705–714. doi: 10.1161/ATVBAHA.113.301928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blacher J, Asmar R, Djane S, London G, Safar M. Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension. 1999;33:1111–1117. doi: 10.1161/01.HYP.33.5.1111 [DOI] [PubMed] [Google Scholar]
- 4.Laurent S, Boutouyrie P, Asmar R, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37:1236–1241. doi: 10.1161/01.HYP.37.5.1236 [DOI] [PubMed] [Google Scholar]
- 5.Sutton-Tyrrell K, Najjar SS, Boudreau RM, et al. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation. 2005;111:3384–3390. doi: 10.1161/CIRCULATIONAHA.104.483628 [DOI] [PubMed] [Google Scholar]
- 6.Hansen TW, Staessen JA, Torp-Pedersen C, et al. Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation. 2006;113:664–670. doi: 10.1161/CIRCULATIONAHA.105.579342 [DOI] [PubMed] [Google Scholar]
- 7.Laurent S, Cockcroft J, Van Bortel L, et al. European network for non-invasive investigation of large arteries. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–2605. doi: 10.1093/eurheartj/ehl254 [DOI] [PubMed] [Google Scholar]
- 8.Mitchell GF, Hwang SJ, Vasan RS, et al. Arterial stiffness and cardiovascular events: the Framingham Heart study. Circulation. 2010;121:505–511. doi: 10.1161/CIRCULATIONAHA.109.886655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ben-Shlomo Y, Spears M, Boustred C, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014;63:636–646. doi: 10.1016/j.jacc.2013.09.063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shirai K, Song M, Suzuki J, et al. Contradictory effects of β1- and α1-adrenergic receptor blockers on cardio-ankle vascular stiffness index (CAVI): CAVI is independent of blood pressure. J Atheroscler Thromb. 2011;18(1):49–55. doi: 10.5551/jat.3582 [DOI] [PubMed] [Google Scholar]
- 11.Ibata J, Sasaki H, Kakimoto T, et al. Cardio-ankle vascular index measures arterial wall stiffness independent of blood pressure. Diabetes Res Clin Pract. 2008;80:265–270. doi: 10.1016/j.diabres.2007.12.016 [DOI] [PubMed] [Google Scholar]
- 12.Shirai K, Utino J, Otsuka K, Takata M. A noble blood pressure-independent arterial wall stiffness parameter; cardio-ankle vascular index (CAVI). J Atheroscler Thromb. 2006;13:101–107. doi: 10.5551/jat.13.101 [DOI] [PubMed] [Google Scholar]
- 13.Hayashi K, Handa H, Nagasawa S, Okumura A, Moritake K. Stiffness and elastic behavior of human intracranial and extracranial arteries. J Biomech. 1980;13:175–184. doi: 10.1016/0021-9290(80)90191-8 [DOI] [PubMed] [Google Scholar]
- 14.Bramwell JC, Hill AV. The velocity of the pulse wave in man. Proc R Soc Lond (Biol). 1922;93:298. [Google Scholar]
- 15.Hayashi K, Yamamoto T, Takahara A, Shirai K. Clinical assessment of arterial stiffness with cardio-ankle vascular index: theory and applications. J Hypertens. 2015;33:1742–1757. doi: 10.1097/HJH.0000000000000651 [DOI] [PubMed] [Google Scholar]
- 16.Kubota Y, Maebuchim D, Takei M, et al. Cardio-ankle vascular index is a predictor of cardiovascular events. Artery Res. 2011;5:91–96. doi: 10.1016/j.artres.2011.03.005 [DOI] [Google Scholar]
- 17.Yingchoncharoen T, Limpijankit T, Jongjirasiri S, Laothamatas J, Yamwong S, Sritara P. Arterial stiffness contributes to coronary artery disease risk prediction beyond the traditional risk score (RAMA-EGAT score). Heart Asia. 2012;4:77–82. doi: 10.1136/heartasia-2011-010079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Otsuka K, Fukuda S, Shimada K, et al. Serial assessment of arterial stiffness by cardio-ankle vascular index for prediction of future cardiovascular events in patients with coronary artery disease. Hypertens Res. 2014;37:1014–1020. doi: 10.1038/hr.2014.116 [DOI] [PubMed] [Google Scholar]
- 19.Satoh-Asahara N, Kotani K, Yamakage H, et al. Japan Obesity and Metabolic Syndrome Study (JOMS) Group. Cardio-ankle vascular index predicts for the incidence of cardiovascular events in obese patients: a multicenter prospective cohort study (Japan Obesity and Metabolic Syndrome Study: JOMS). Atherosclerosis. 2015;242:461–468. doi: 10.1016/j.atherosclerosis.2015.08.003 [DOI] [PubMed] [Google Scholar]
- 20.Sato Y, Nagayama D, Saiki A, et al. Cardio-ankle vascular index is independently associated with future cardiovascular events in outpatients with metabolic disorders. J Atheroscler Thromb. 2016;23:596–605. doi: 10.5551/jat.31385 [DOI] [PubMed] [Google Scholar]
- 21.Kusunose K, Sato M, Yamada H, et al. Prognostic implications of non-invasive vascular function tests in high-risk atherosclerosis patients. Circ J. 2016;80:1034–1040. doi: 10.1253/circj.CJ-15-1356 [DOI] [PubMed] [Google Scholar]
- 22.Gohbara M, Iwahashi N, Sano Y, et al. Clinical impact of the cardio-ankle vascular index for predicting cardiovascular events after acute coronary syndrome. Circ J. 2016;80:1420–1426. doi: 10.1253/circj.CJ-15-1257 [DOI] [PubMed] [Google Scholar]
- 23.Namekata T, Suzuki K, Ishizuka N, Shirai K. Establishing baseline criteria of cardio-ankle vascular index as a new indicator of arteriosclerosis: a cross-sectional study. BMC Cardiovasc Disord. 2011;11:51. doi: 10.1186/1471-2261-11-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nakamura K, Tomaru T, Yamamura S, Miyashita Y, Shirai K, Noike H. Cardio-ankle vascular index is a candidate predictor of coronary atherosclerosis. Circ J. 2008;72:598–604. doi: 10.1253/circj.72.598 [DOI] [PubMed] [Google Scholar]
- 25.Nakamura K, Iiduka T, Takahashi M, et al. Association between cardio-ankle vascular index and serum cystatin c levels in patients with cardiovascular risk factor. J Atheroscler Thromb. 2009;16:371–379. doi: 10.5551/jat.No687 [DOI] [PubMed] [Google Scholar]
- 26.Suzuki J, Sakakibara R, Tomaru T, et al. Stroke and cardio-ankle vascular stiffness index. J Stroke Cerebrovasc Dis. 2011;22:171–175. [DOI] [PubMed] [Google Scholar]
- 27.Topouchian J, Labat C, Gautier S, et al. Effects of metabolic syndrome on arterial function in different age groups: the advanced approach to arterial stiffness study. J Hypertens. 2018;36(4):824–833. doi: 10.1097/HJH.0000000000001631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nagayama D, Saiki A, Endo K, et al. Improvement of cardio-vascular vascular index by glimepiride in type 2 diabetic patients. Int J Clin Pract. 2010;64:1796–1801. doi: 10.1111/j.1742-1241.2010.02399.x [DOI] [PubMed] [Google Scholar]
- 29.Zhao X, Bo L, Zhao H, Li L, Zhou Y, Wang H. Cardio-ankle vascular index value in dyslipidemia patients affected by cardiovascular risk factors. Clin Exp Hypertens. 2018;40(4):312–317. doi: 10.1080/10641963.2017.1377213 [DOI] [PubMed] [Google Scholar]
- 30.Kubozono T, Miyata M, Uegama K, et al. Acute and chronic effects of smoking on arterial stiffness. Circ J. 2011;95:698–702. doi: 10.1253/circj.CJ-10-0552 [DOI] [PubMed] [Google Scholar]
- 31.Kumagai T, Kasai T, Kato M, et al. Establishment of the cardio-ankle vascular index in patients with obstructive sleep apnea. Chest. 2009;36:779–786. doi: 10.1378/chest.09-0178 [DOI] [PubMed] [Google Scholar]
- 32.Miyashita Y, Saiki A, Endo K, et al. Effects of olmesartan, an angiotensin II receptor blocker, and amlodipine, a calcium channel blocker, on cardio-ankle vascular index (CAVI) in type 2 diabetic patients with hypertension. J Atheroscler Thromb. 2009;16:621–626. doi: 10.5551/jat.497 [DOI] [PubMed] [Google Scholar]
- 33.Yukutake T, Yamada M, Fukutani N, et al. Arterial stiffness determined according to the cardio-ankle vascular index (CAVI) is associated with mild cognitive decline in community-dwelling elderly subjects. J Atheroscler Thromb. 2014;21:49–55. doi: 10.5551/jat.19992 [DOI] [PubMed] [Google Scholar]
- 34.Shimizu K, Takahashi M, Shirai K. A huge earthquake hardened arterial stiffness monitored with cardio-ankle vascular index. J Atheroscler Thromb. 2013;20:503–511. doi: 10.5551/jat.16097 [DOI] [PubMed] [Google Scholar]
- 35.Nagayama D, Endo K, Ohira M, et al. Effects of body weight reduction on cardio-ankle vascular index (CAVI). Obes Res Clin Pract. 2011;7:e139–e145. doi: 10.1016/j.orcp.2011.08.154 [DOI] [PubMed] [Google Scholar]
- 36.Miyashita Y, Endo K, Saiki A, et al. Effects of pitavastatin, a 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor, on cardio-ankle vascular index in type 2 diabetic patients. J Atheroscler Thromb. 2009;16(5):539–545. doi: 10.5551/jat.281 [DOI] [PubMed] [Google Scholar]
- 37.Noike H, Nakamura K, Sugiyama Y, et al. Changes in cardio-ankle vascular index in smoking cessation. J Atheroscler Thromb. 2010;17:517–525. doi: 10.5551/jat.3707 [DOI] [PubMed] [Google Scholar]
- 38.Kasai T, Inoue K, Kumagai T, et al. Plasma pentraxin3 and arterial stiffness in men with obstructive sleep apnea. Am J Hypertens. 2011;24:401–407. doi: 10.1038/ajh.2010.248 [DOI] [PubMed] [Google Scholar]
- 39.Matsushita K, Ding N, Kim ED, et al. Cardio‐ankle vascular index and cardiovascular disease: systematic review and meta‐analysis of prospective and cross‐sectional studies. J Clin Hypertens. 2019;21:16–24. doi: 10.1111/jch.13425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shimoyama T, Iguchi Y, Kimura K, et al. Stroke patients with cerebral microbleeds on MRI scans have arteriolosclerosis as well as systemic atherosclerosis. Hypertens Res. 2012;35(10):975–979. doi: 10.1038/hr.2012.84 [DOI] [PubMed] [Google Scholar]
- 41.Suzuki J, Sakakibara R, Tomaru T, et al. Stroke and cardio-ankle vascular stiffness index. J Stroke Cerebrovasc Dis. 2013;22(2):171–175. doi: 10.1016/j.jstrokecerebrovasdis.2011.07.010 [DOI] [PubMed] [Google Scholar]
- 42.Saji N, Kimura K, Yagita Y, Kawarai T, Shimizu H, Kita Y. Comparison of arteriosclerotic indicators in patients with ischemic stroke: ankle-brachial index, brachial-ankle pulse wave velocity and cardio-ankle vascular index. Hypertens Res. 2015;38(5):323–328. doi: 10.1038/hr.2015.8 [DOI] [PubMed] [Google Scholar]
- 43.Trichopoulos D, Zavitsanos X, Katsouyanni K, Tzonou A, Dalla-Vorgia P. Psychological stress and fatal heart attack: the Athens (1981) earthquake natural experiment. Lancet. 1983;321:441–444. doi: 10.1016/S0140-6736(83)91439-3 [DOI] [PubMed] [Google Scholar]
- 44.Dobson AJ, Alexander HM, Malcolm JA, Steele PL, Miles TA. Heart attacks and the Newcastle earthquake. Med J Aust. 1991;155:757–761. doi: 10.5694/j.1326-5377.1991.tb94029.x [DOI] [PubMed] [Google Scholar]
- 45.Leor J, Poole WK, Kloner RA. Sudden cardiac death triggered by an earthquake. N Engl J Med. 1996;334:413–419. doi: 10.1056/NEJM199602153340701 [DOI] [PubMed] [Google Scholar]
- 46.Kario K, McEwen BS, Pickering TG. Disasters and the heart: a review of the effects of earthquake-induced stress on cardiovascular disease. Hypertens Res. 2003;26:355–367. doi: 10.1291/hypres.26.355 [DOI] [PubMed] [Google Scholar]
- 47.Aoki T, Fukumoto Y, Yasuda S, et al. The Great East Japan Earthquake Disaster and cardiovascular diseases. Eur Heart J. 2012;33(22):2796–2803. doi: 10.1093/eurheartj/ehs288 [DOI] [PubMed] [Google Scholar]
- 48.Nozaki E, Nakamura A, Abe A, et al. Occurrence of cardiovascular events after the 2011 Great East Japan Earthquake and tsunami disaster. Int Heart J. 2013;54(5):247–253. doi: 10.1536/ihj.54.247 [DOI] [PubMed] [Google Scholar]
- 49.Kario K, Matsuo T, Kobayashi H, Yamamoto K, Shimada K. Earthquake-induced potentiation of acute risk factors in hypertensive elderly patients: possible triggering of cardiovascular events after a major earthquake. J Am Coll Cardiol. 1997;29:926–933. doi: 10.1016/S0735-1097(97)00002-8 [DOI] [PubMed] [Google Scholar]
- 50.von Känel R, Mills PJ, Ziegler MG, Dimsdale JE. Effect of β2-adrenergic receptor functioning and increased norepinephrine on the hypercoagulable state with mental stress. Am Heart J. 2002;144:68–72. doi: 10.1067/mhj.2002.123146 [DOI] [PubMed] [Google Scholar]
- 51.Wilbert-Lampen U, Nickel T, Leistner D, et al. Modified serum profiles of inflammatory and vasoconstrictive factors in patients with emotional stress-induced acute coronary syndrome during world cup soccer 2006. J Am Coll Cardiol. 2010;55:637–642. doi: 10.1016/j.jacc.2009.07.073 [DOI] [PubMed] [Google Scholar]
- 52.Fukuda S, Morimoto K, Mure K, Maruyama S. Effect of the Hanshin-Awaji earthquake on posttraumatic stress, lifestyle changes, and cortisol levels of victims. Arch Environ Health. 2000;55:121–125. doi: 10.1080/00039890009603398 [DOI] [PubMed] [Google Scholar]
- 53.Muller JE, Tofler GH. Triggering and hourly variation of onset of arterial thrombosis. Ann Epidemiol. 1992;2:393–405. doi: 10.1016/1047-2797(92)90088-8 [DOI] [PubMed] [Google Scholar]
- 54.Muller JE, Abela GS, Nesto RW, Tofler GH. Triggers, acute risk factors and vulnerable plaques: the lexicon of a new frontier. J Am Coll Cardiol. 1994;23:809–813. doi: 10.1016/0735-1097(94)90772-2 [DOI] [PubMed] [Google Scholar]
- 55.Willich SN, Maclure M, Mittleman M, Arntz HR, Muller JE. Sudden cardiac death. Support for a role of triggering in causation. Circulation. 1993;87:1442–1450. doi: 10.1161/01.CIR.87.5.1442 [DOI] [PubMed] [Google Scholar]
- 56.Shimizu K, Yamamoto T, Takahashi M, Sato S, Noike H, Shirai K. Effect of nitroglycerin administration on cardio-ankle vascular index. Vasc Health Risk Manag. 2016;12:313–319. doi: 10.2147/VHRM.S106542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yamamoto T, Shimizu K, Takahashi M, Tatsuno I, Shirai K. The effect of nitroglycerin on arterial stiffness of the aorta and the femoral-tibial arteries. J Atheroscler Thromb. 2017;24(10):1048–1057. doi: 10.5551/jat.38646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shimizu K, Yamamoto T, Shirai K. Arterial stiffness, as monitored by cardio-ankle vascular index, is affected by obstructive sleep apnea, blood glucose control and body weight -a case of 8 years follow up-. Int Med Case Rep J. 2016;9:231–235. doi: 10.2147/IMCRJ.S113377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lim J, Pearman ME, Park W, Alkatan M, Machin DR, Tanaka H. Impact of blood pressure perturbations on arterial stiffness. Am J Physiol Regul Integr Comp Physiol. 2015;309:1540–1545. doi: 10.1152/ajpregu.00368.2015 [DOI] [PubMed] [Google Scholar]
- 60.Stewart S, Keates AK, Redfern A, McMurray JV. Seasonal variations in cardiovascular disease. Nat Rev Cardiol. 2017;14(11):654–664. doi: 10.1038/nrcardio.2017.76 [DOI] [PubMed] [Google Scholar]
- 61.Yasue H, Kugiyama K. Coronary spasm: clinical features and pathogenesis. Intern Med. 1997;36:760–765. doi: 10.2169/internalmedicine.36.760 [DOI] [PubMed] [Google Scholar]
- 62.Yeung AC, Vekshtein VI, Krantz DS, et al. The effect of atherosclerosis on the vasomotor response of coronary arteries to mental stress. N Engl J Med. 1991;325:1551–1556. doi: 10.1056/NEJM199111283252205 [DOI] [PubMed] [Google Scholar]
- 63.Raizner AE, Chahine RA, Ishimori T, et al. Provocation of coronary artery spasm by the cold pressor test. Hemodynamic, arteriographic and quantitative angiographic observations. Circulation. 1980;62:925–935. doi: 10.1161/01.CIR.62.5.925 [DOI] [PubMed] [Google Scholar]
- 64.Wang L, Lü S, Zhang W, Song X, Chen H, Zhang L. Coronary spasm, a pathogenic trigger of vulnerable plaque rupture. Chin Med J. 2011;124(23):4071–4078. [PubMed] [Google Scholar]
- 65.Ross R. The arterial wall and atherosclerosis. Ann Rev Med. 1979;30:1–15. doi: 10.1146/annurev.me.30.020179.000245 [DOI] [PubMed] [Google Scholar]
- 66.Sakakura K, Nakano M, Otsuka F, Ladich E, Kolodgie FD, Virmani R. Pathophysiology of atherosclerosis plaque progression. Heart Lung Circ. 2013;22(6):399–411. doi: 10.1016/j.hlc.2013.03.001 [DOI] [PubMed] [Google Scholar]
- 67.Bentzon JF, Otsuka F, Virmani R, Falk E. Mechanisms of plaque formation and rupture. Circ Res. 2014;114(12):1852–1866. doi: 10.1161/CIRCRESAHA.114.302721 [DOI] [PubMed] [Google Scholar]
- 68.Michel JB, Thaunat O, Houard X, Meilhac O, Caligiuri G, Nicoletti A. Topological determinants and consequences of adventitial responses to arterial wall injury. Arterioscler Thromb Vasc Biol. 2007;27:1259–1268. doi: 10.1161/ATVBAHA.106.137851 [DOI] [PubMed] [Google Scholar]
- 69.Boyle EC, Sedding DG, Haverich A. Targeting vasa vasorum dysfunction to prevent atherosclerosis. Vascul Pharmacol. 2017;96–98:5–10. doi: 10.1016/j.vph.2017.08.003 [DOI] [PubMed] [Google Scholar]
- 70.Doyle B, Caplice N. Plaque neovascularization and antiangiogenic therapy for atherosclerosis. J Am Coll Cardiol. 2007;49(21):2073–2080. doi: 10.1016/j.jacc.2007.01.089 [DOI] [PubMed] [Google Scholar]
- 71.Moore KJ, Tabas I. The cellular biology of macrophages in atherosclerosis. Cell. 2011;145(3):341–355. doi: 10.1016/j.cell.2011.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Osada H, Kyogoku M, Ishidou M, Morishima M, Nakajima H. Aortic dissection in the outer third of the media: what is the role of the vasa vasorum in the triggering process? Eur J Cardio Thorac Surg. 2013;43(3):e82–e88. doi: 10.1093/ejcts/ezs640 [DOI] [PubMed] [Google Scholar]
- 73.Nagayama D, Imamura H, Sato Y, et al. Inverse relationship of cardioankle vascular index with BMI in healthy Japanese subjects: a cross-sectional study. Vasc. Health Risk Manag. 2017;13:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Otsuka K, Fukuda S, Shimada K, et al. Serial assessment of arterial stiffness by cardio-ankle vascular index for prediction of future cardiovascular events in patients with coronary artery disease. Hypertens Res. 2014;37(11):1014–1020. [DOI] [PubMed] [Google Scholar]