Abstract
Purpose: adolescence is a time of change and it generally entails a greater family vulnerability thus; the aim of this study was to identify the risk factors for poor emotional adjustment to COVID among parents of adolescents. Design and methods: 94 parents of adolescents (11–18 years old, M = 13.90, SD = 1.85) participated at different times during the state of alert in Spain. 91.5% were mothers. Their ages ranged from 35 to 63 years (M = 46.54; SD = 5.09). The variables assessed were anxiety, depression and stress (DASS), moods (MOOD), somatization (SCL) and resilience (CD-RISC). Descriptive analyses, t-tests, ANOVAs, correlations, and hierarchical regressions were performed. All this by means of a cross-sectional and longitudinal study design. Results: at the beginning of the confinement parents showed low levels of emotional distress and moderate levels of positive emotionality and resilience. However, those with a prior psychological problem, who had lost their job, or had lost someone to the pandemic, showed worse emotional adjustment. Resilience was relevant in predicting anxiety-depressive symptoms, and a low level of happiness was relevant in predicting stress. Emotional symptoms improved over time, and resilience remained stable. Conclusions: the emotional impact of COVID over time is influenced by mood, mental health, and resilience. In addition, parents who had a previous health problem, had lost their job or a loved one, had a worse adjustment. Practical implications: it is important to carry out intervention programs that increase resilience, treating parents who require it, since their emotional adjustment has repercussions on the emotional adjustment of family system.
Keywords: Family caregiver, COVID-19, Psychological adjustment, Resilience, Adolescence
Purpose
The emergence and rapid expansion of COVID-19 in early 2020 has led to multiple infections and deaths worldwide. By mid-January 2021, COVID-19 had already caused 100,998,542 infections worldwide, and 2,670,102 of those were in Spain (data extracted on 01/28/2021, (Ministerio de Sanidad, 2020)). Faced with this situation, governments around the world had to decree social distancing measures, ranging from some social limitations to mandatory state of alert (European Centre for Disease Prevention and Control, 2020; Orgilés et al., 2020) The pandemic has claimed the lives of 2,177,819 people, of whom 57,291 were in Spain (data extracted on 01/28/2020, Coronavirus Resource Center, 2021).
The COVID-19 pandemic has been characterized by the continuous losses that society has had to face (Zhai & Du, 2020a). In this context, many families have had to isolate themselves, losing social, family, school and work support—having to telework or even losing their jobs (United Nations New York: Intergovernmental Organization, 2020). After the loss of freedom that it entailed, this new situation has meant that parents have had to face difficult circumstances at home, while having to deal with the needs of their children (Campbell, 2020). Moreover, some families had added stressors to handle, including some as disturbing as a member of their family having to be in isolation (due to suffering from or suspected of having COVID-19) or even, in some cases, having suffered the loss of a loved one (in the most extreme situations, without even being able to say goodbye to them). Under these circumstances, the absence of rituals such as funerals (which provide support and help to accommodate assimilate/psychologically the experience) tends to diminish the social support received and/or perceived at these times. These factors mean that people who have lost a family member during this pandemic are at greater risk of experiencing psychological complications (Zhai & Du, 2020b).
This pandemic can pose a threat to the mental health of the general population (Brooks et al., 2020; Goldschmidt, 2020) but particularly to the parents of adolescents. Adolescence is a time of social, emotional and identity changes that can cause a disturbance in the daily lives of adolescents and their families (Andrews, Foulkes, & Blakemore, 2020; Orkaizagirre-Gómara et al., 2020). Adolescents and their families are particularly vulnerable at this time, their needs being very different from those of children. Although in general, the pediatric population has been the most affected by this pandemic on an emotional level, the impact on adolescents has been particularly significant, as they have lost the possibility of socializing with their peers for a long time. This aspect is fundamental for psycho-emotional development throughout life, and is particularly important in adolescence (Orte et al., 2020). During this stage it is common for more conflicts to occur between members of the family system, thus deteriorating the family climate, which can have a significant impact on the mental health of the members of the system (Alavi et al., 2020). Parents, in addition to sustaining their own process, have to deal with the emotional needs of their children at this difficult stage of development (Cameron et al., 2020).
The closure of education centers means that parents have had to live under the same roof as their children for longer, increasing the number of tasks, functions and responsibilities involved in the daily care of their children. This scenario might have caused major psycho-emotional impact on many parents (Collins, Landivar, Ruppanner, & Scarborough, 2020), in addition to the stress that the teenager's relatives may already be experiencing (Prime, Wade, & Browne, 2020).
During the pandemic, many parents have therefore suffered emotional symptoms such as anxiety, depression and stress, and problems of somatization (Liu et al., 2020; Qiu et al., 2020). This clinical profile has been most likely to occur in people who suffered from physical or mental health problems prior to the pandemic (Yao et al., 2020) or who presented socio-economic difficulties.
However, the role of psychological symptoms in this pandemic has yet to be clarified. Most studies are cross-sectional and when longitudinal studies were conducted, the data showed controversial results: symptomatology signs remains the same or even increases (Brooks et al., 2020; Wang et al., 2020a, Wang et al., 2020b). If the progression of emotional symptomatology during confinement has not been studied extensively in the general population, as far as we know, this issue has not been addressed in parents of adolescents either. Studies have pointed to factors such as adequate pre-pandemic mental health (Brailovskaia & Margraf, 2020); higher positive emotionality and lower negative emotionality, as well as high resilience, which might be helpful in the adaptation to isolation (El-Masri et al., 2020). It should be borne in mind that the mental health of parents can have a significant impact on that of their children. Children of parents with poorer mental health show lower levels of adjustment to adversity, and have poorer physical and mental health (Silva et al., 2018). The families with the most positive emotionality, most positive family relationships and healthier parental styles may have been better adapted to the pandemic and its associated stressors, and may have presented greater resilience (Prime, Wade, & Browne, 2020).
At the family level, among other things, resilience involves the family's ability to create meaning out of adversity and to confer/construct meaning to their experiences, and this factor can be modified by their experiences (Prime, Wade, & Browne, 2020). Nevertheless, for people who have faced relatively little adversity in their lives, living through the pandemic may now be a sensitizing situation that further reduces their tolerance to subsequent stress, leading to a possible increased psychopathology. All the above is even more important bearing in mind that stressful events associated with COVID-19 may occur again in the future and require us to join forces and employ new strategies to mitigate the disease. Longitudinal studies are therefore needed to evaluate the impact of COVID-19 on adults with adolescents, since the effects of exposure to continuous stress will be seen over time in some cases (Prime, Wade, & Browne, 2020).
For all the reasons listed above, this study aims to determine the psycho-emotional impact of the COVID-19 pandemic (studied through anxiety-depressive symptomatology, emotionality, stress, and somatization) on parents of adolescents. To that end, it combines both a cross-sectional and a longitudinal analysis, while also attempting to ascertain the role that resilience plays in the adjustment of these families to the extraordinary situation created by COVID-19.
Design and methods
Participants
The participants were 94 family caregivers of teenagers (11–18 years old, M = 13.90; SD = 1.85) assessed at the beginning of COVID-19 (2–3 weeks after the state of alert was declared in Spain). The age of the caregivers ranged from 35 to 63 years, with a mean age of 46.54 (SD = 5.09), and 91.5% were mothers. The caregivers reported having a chronic illness prior to the onset of the pandemic was 22.5%. The most prevalent of these illnesses were allergic diseases (rhino conjunctivitis and bronchial asthma). Furthermore, 20.2% stated that they presented a psychological problem prior to the pandemic, especially anxiety disorders and depression. The most common number of children in the family was two (60.4%), followed by one child (28.6%). During the pandemic, 31.9% of caregivers teleworked in their normal employment in the home. 27.5% were able to work in the workplace, but 15.4% were subject to a temporary or permanent layoff. The remaining subjects were unable to carry out their work due to being temporarily incapacitated for work or because they did not have paid work at the beginning of the COVID-19 pandemic. Parents reported having a family member with symptoms of COVID-19 was 13.5%, but only 3.4% of those family members had a confirmed diagnosis.
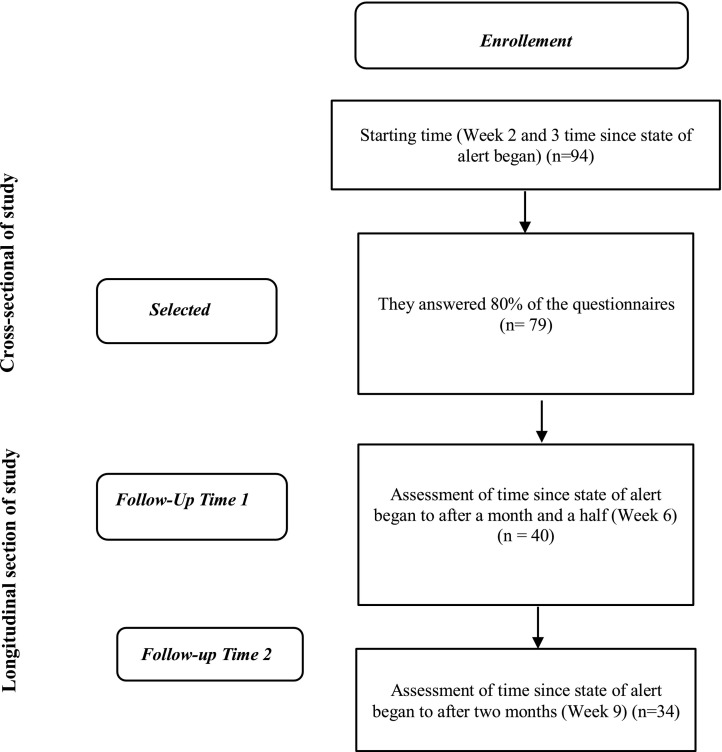
The final moment of evaluation (which is part the longitudinal analysis that we also provide) took place with a significant level of study attrition. However, this is a very important part of the analysis, which can provide very interesting data. The number of participants in this second evaluation fell from 94 subjects to 34, of whom 15.7% stated that they had a family member with COVID symptoms, but only 5.9% had a confirmed diagnosis. Thus, 2.9% of these 34 subjects had contracted COVID themselves. Finally, the percentage of caregivers who had lost someone close to them due to COVID was 23.5%. The procedure of participant selection and dropout is presented in the flowchart (Fig. 1 ).
Fig. 1.
Flowchart of study participants and dropouts.
Instruments
The Depression, Anxiety and Stress Scale (DASS) was used to assess anxiety, depression, and stress. The reduced version (DASS-21) was used (Fonseca-Pedrero et al., 2010; Lovibond & Lovibond, 1995). The DASS is a four-point Likert scale ranging from 0 (“It doesn't describe anything that happened to me or what I felt during the week”) to 3 (“Yes, this happened to me a lot, or almost always”). When responding, the subject must indicate the extent to which the sentence describes what happened or how he or she felt during the last week. This instrument has the advantage of being a self-reporting scale, short, easy to administer and respond to, and its interpretation is simple. In addition, it has presented adequate psychometric properties in previous validation studies (Clara et al., 2001; Crawford & Henry, 2003; Lovibond & Lovibond, 1995) and good psychometric adjustment in Spanish-speaking samples (Bados et al., 2005; Daza et al., 2002; Fonseca-Pedrero et al., 2010). The reliability in this study is α = 0.87 for depression, α = 0.81 for anxiety and α = 0.83 for stress.
The Connor-Davidson Resilience Scale, created by Connor and Davidson (2003) which assesses the ability to cope with stress and adversity, was used to analyze resilience. The CD-RISC-10 is a reduced version of the CD-RISC (Campbell-Sills & Stein, 2007). The Spanish version of this questionnaire has previously been used (Bobes et al., 2001). The CD-RISC-10 is composed of 10 items, which are answered considering the last month, with a Likert-type format ranging from 0 “strongly disagree” to 4 “strongly agree”. The instrument presents good psychometric properties, with adequate values of internal consistency, test-retest reliability and convergent and divergent validity (Campbell-Sills & Stein, 2007). The results obtained in the Spanish version also meet the expectations of the original study, and its internal consistency is similar to that observed in the original research (α = 0.85 in both versions) (Notario-Pacheco et al., 2011). The reliability in this study is 0.92.
The Mood Questionnaire (Rieffe et al., 2008) was used to assess mood. A Spanish version of the questionnaire was used by (Górriz et al., 2013). It evaluates the frequency of different moods (Fear, Sadness, Happiness and Anger) in the last four weeks. This questionnaire consists of 20 items with a three-point Likert scale: Never, Sometimes and Often. Higher scores imply a greater presence of the mood in question in all the dimensions. The internal consistency of the scales was acceptable in previous studies (α > 0.77) (Rieffe et al., 2008) and, in the current study, average scores of 0.70.
Finally, the Somatic Complaints List (SCL) was used to evaluate somatic complaints (Rieffe et al., 2007; Rieffe et al., 2006). This questionnaire was developed to identify the frequency with which subjects experience and feel pain. It consists of 11 items with a three-point Likert scale (1 = never, 2 = sometimes, 3 = often). This instrument has proven to be highly reliable in both previous studies (α > 0.84) (Rieffe et al., 2006, Rieffe et al., 2007) and the current one.
Finally, an ad hoc register was developed to collect data on the age and gender of the participants, their employment status during the state of alert, whether they have a chronic physical illness and/or psychological problems prior to state of alert, and finally, the loss of a close relative due to COVID-19.
Procedure
The individuals who participated in this research were the parents of teenagers in the Valencian Community recruited through social networks such as Facebook, Twitter, Instagram or WhatsApp and also through school principals with whom contact had been made prior to the pandemic. Their participation was voluntary and anonymous, after giving informed consent, fulfilling the requirements of the Helsinki declaration. They were also informed that the data disclosed would be used exclusively for academic-scientific purposes. The questionnaire was administered through the limesurvey online platform at all times during the evaluation (both cross-sectional and longitudinal), starting two weeks after the beginning of the state of alert in Spain (28 March 2020) and continuing for 8 consecutive weeks. The last evaluation took place on 9 May, when alert state de-escalation process (Phase 1) began in Spain.
Three points in time were taken into account for evaluation in this study: time 1 (just 2–3 weeks after the state of alert was declared), time 2 (6 weeks after the state of alert was declared) and time 3 (final evaluation moment, 9 weeks after the state of alert was declared in Spain). The study was voluntary, and it was necessary to have participated in all the times registered to be able to access a draw for a gift voucher at the FNAC.
Statistical analysis
The data were analyzed using version 24.0 of the SPSS statistical software package. Frequency analysis and descriptive statistics were performed to explore the data. t-tests were used to compare the existence of significant differences between mood, anxiety, depression, stress and somatic complaints depending on the presence of a previous chronic physical illness, a chronic psychological problem or the death of a loved one due to COVID. ANOVA tests were used to compare mood, anxiety, depression, stress, and somatic complaints depending on employment status. Pearson's correlations were used to analyze the relationship between the variables studied. Hierarchical stepwise regression was performed to predict anxiety, stress, and depression among caregivers over time 1 (two-three weeks of state of alert). Repeated ANOVA measurements were performed to compare quality of sleep and emotional experiences after two to three weeks, after six weeks and after nine weeks since the state of alert was declared.
Results
Descriptive statistics of mood, somatic complaints, resilience and anxiety, depression, and stress at the initial time of assessment
Regarding descriptive data, mean subject scores of 1.44 were obtained on the somatic complaints scale (SD = 0.34; range 0–4), indicating low-moderate scores in the somatization variable.
As for levels of depression (M = 6.84 SD = 7.34; Range 0–42), anxiety (M = 5.18; SD = 6.38; Range 0–42) and stress (M = 12.49; SD = 7.86; Range 0–42), the subjects generally presented average scores indicating low levels in these variables. Stress scores, although within moderate levels, were the highest compared to anxiety and depression.
The mean scores for the evaluation of moods using the MOOD were as follows: anger (M = 1.96; SD = 0.30; range 1–3), sadness (M = 1.64; SD = 0.41; range 1–3), fear (M = 1.84; SD = 0.47; range 1–3) and happiness (M = 2.41; SD = 0.46; range 1–3). The data show moderate scores in all the dimensions, those for happiness being the highest.
Finally, a mean score of 28.20 (SD = 6.96, range 0–40) was obtained for levels of resilience, indicating moderate scores for adaptation and resilience in the face of adversity.
Relationships between variables
Resilience (Table 1 ) was related in a positive way with the happiness mood and in a negative way with the rest of variables (sadness, fear, somatic complaints, anxiety, depression and stress), showing moderate negative relations. Anxiety, depression, and stress were positively related to somatic complaints and to moods such as sadness and fear, but negatively to happiness. Finally, somatic complaints were positively related to sad and fearful moods but negatively to happiness. The only variable that virtually showed no significant correlations was anger.
Table 1.
Correlations with dimensions of MOOD, CD-RISC and DASS-21 in time 1.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Resilience | 1 | ||||||||
| Sadness | −0.43⁎⁎ | 1 | |||||||
| Fear | −0.32⁎ | 0.38⁎⁎ | 1 | ||||||
| Anger | 0.08 | 0.25 | −0.01 | 1 | |||||
| Happiness | 0.49⁎⁎⁎ | −0.44⁎⁎ | −0.35⁎ | 0.41⁎⁎ | 1 | ||||
| Somatic complaints | −0.45⁎⁎ | 0.46⁎⁎⁎ | 0.29⁎ | −0.22 | −0.46⁎⁎⁎ | 1 | |||
| Depression | −0.44⁎⁎ | 0.60⁎⁎⁎ | 0.36⁎ | −0.03 | −0.45⁎⁎ | 0.43⁎⁎ | 1 | ||
| Anxiety | −0.54⁎⁎⁎ | 0.61⁎⁎⁎ | 0.66⁎⁎⁎ | 0.05 | −0.47⁎⁎⁎ | 0.48⁎⁎⁎ | 0.61⁎⁎⁎ | 1 | |
| Stress | −0.50⁎⁎⁎ | 0.63⁎⁎⁎ | 0.36⁎ | −0.01 | −0.53⁎⁎⁎ | 0.49⁎⁎ | 0.65⁎⁎⁎ | 0.67⁎⁎⁎ | 1 |
Note. 1 = resilience; 2 = sadness; 3 = fear; 4 = Anger; 5 = happiness; 6 = somatic complaints; 7 = depression; 8 = anxiety; 9 = stress.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Predictors of anxiety, depression, and stress in early caregivers
The predictive power of the studied variables was subsequently analyzed using a hierarchical regression model (HRM). The criterion variables were anxiety, depression, and stress. The predictor variables were resilience, somatic complaints, and mood dimensions (anger, sadness, fear, and happiness). Three differential steps were established in the model (Table 2 ): first, variables related to resilience were included; then somatic complaints were added, and finally, mood dimensions were introduced.
Table 2.
Hierarchical regression model predicting anxiety, depression, and stress.
| Predictor | Anxiety |
Depression |
Stress |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ΔR2 | ΔF | β | t | ΔR2 | ΔF | β | t | ΔR2 | ΔF | β | t | |
| Step 1 | 0.29 | 30.41⁎⁎⁎ | 0.39 | 46.28⁎⁎⁎ | 0.27 | 27.10⁎⁎⁎⁎ | ||||||
| Resilience | −0.22 | −1.97⁎ | −0.28 | −2.58⁎⁎ | −0.07 | −0.64 | ||||||
| Step 2 | 0.06 | 6.25⁎⁎ | 0.08 | 10.19⁎⁎ | 0.13 | 15.19⁎⁎⁎ | ||||||
| Somatic complaints | 0.21 | 1.74 | 0.15 | 1.24 | 0.22 | 1.88 | ||||||
| Step 3 | 0.16 | 5.61⁎⁎⁎ | 0.08 | 3.17⁎⁎ | 0.14 | 5.20⁎⁎⁎ | ||||||
| Anger | 0.06 | 0.57 | 0.02 | 0.18 | 0.15 | 1.49 | ||||||
| Fear | 0.42 | 4.16⁎⁎⁎ | 0.09 | 0.86 | 0.09 | 0.90 | ||||||
| Sadness | 0.05 | 0.33 | 0.29 | 2.18⁎ | 0.22 | 1.62 | ||||||
| Happiness | 0.05 | 0.39 | −0.10 | −0.84 | −0.26 | −2.13⁎ | ||||||
| Durbin-Watson | 1.79 | 1.78 | 2.12 | |||||||||
| R2ajd | 0.47⁎⁎⁎ | 0.50⁎⁎⁎ | 0.49⁎⁎⁎ | |||||||||
Note. ΔR2 = change in R2; ΔF = change in F; ß = regression coefficient; t = value of t-test statistic.
p ≤ 0.05.
p ≤ 0.01.
p ≤ 0.001.
In the anxiety prediction model, in the first step, the resilience variable significantly explained 29% of the variance in the first step (ΔR2 = 0.29, p ≤ .001). In the second step, the somatic complaints variable explained 6% of the variance (ΔR2 = 0.06, p = .02). In the last step, mood dimensions explained 16% of the variance of anxiety (ΔR2 = 0.16, p ≤ .001.) In this final step, resilience was the variable that presented a significant negative beta coefficient (β = −0.22; p = .05) and fear showed a significant positive beta coefficient (β = 0.43; p ≤ .001).
In the depression prediction model, in the first step, the resilience variable significantly explained 38% of the variance (ΔR2 = 0.38, p ≤ .001). In the second step, somatic complaints explained 8% of the variance (ΔR2 = 0.08, p = .01). In the last step, mood dimensions explained 8% of the variance of depression (ΔR2 = 0.08 p = .02.) In this final step, resilience was the variable that presented a significant negative beta coefficient (β = −0.28; p = .02) and sadness showed a significant positive beta coefficient (β = 0.29; p = .03).
In the last model (stress), in the first step, resilience significantly explained 27% of the variance (ΔR2 = 0.27, p ≤ .001). In the second step, somatic complaints explained 13% of the variance (ΔR2 = 0.13, p ≤ .001). In the last step, mood dimensions explained 14% of the variance of depression (ΔR2 = 0.08 p = .02.). In this final step, happiness was the variable that presented a significant negative beta coefficient (β = −0.26; p = .03).
Comparison of means of the variables according to the presence of chronic physical illness and/or previous psychological problems and at the different evaluation times
Statistically significant differences were found at time 1 for sadness (t 77 = −2.96; p = .01; d = 0.81) and depression (t 76 = −2.52; p = .02; d = 0.92). The subjects who presented a sadder mood and higher levels of depression were those who had a psychological problem prior to the state of alert. These differences were not observed at time 2 or 3. There were no differences depending on the presence of a chronic physical illness in any of the variables and times analyzed.
Comparison of averages of variables according to working conditions at different times
Statistically significant differences in depression were found at time 1 (F 77 = 3.76; p = .01; η2 = 0.17) between caregivers of adolescents who continued to work at their jobs during state of alert and caregivers who were unemployed, the latter showing higher levels of depression. At time 2 (6 weeks after the state of alert was declared), differences were found between the same groups for the somatic complaints variable (F 39 = 3.51; p = .02; η2 = 0.29), the sadness mood variable (F 39 = 2.62; p = .05; η2 = 0.23) and the fear mood variable (F 39 = 4.05; p = .01; η2 = 0.32). According to these results, unemployed people presented more somatic complaints, felt sadder and more afraid. Finally, similar results to those mentioned above for time 1 and 2 were found for the depression variable at time 3 (F 31 = 3.56; p = .02; η2 = 0.34).
Longitudinal analysis of mood, somatic complaints and anxiety, depression, stress and resilience, compared at different times
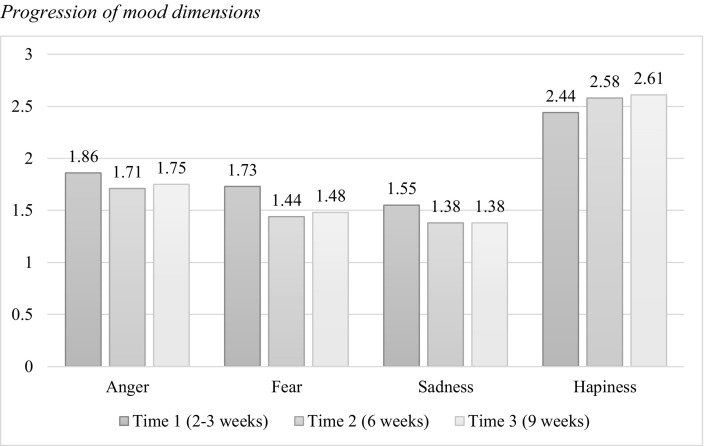
Table 3 shows that the scores for anger and fear among the caregivers of adolescents were higher at time 1 than at time 2. In the case of fear, the same trend also persisted at time 3. Nevertheless, in the first weeks of state of alert (time 1), the scores (Fig. 2 ) indicate a tendency for the subjects to feel more angry, more afraid, and sadder. However, as time passed, these scores declined slightly and the feeling of being happier with the passing of time increased.
Table 3.
ANOVA repeated measures of mood, anxiety, depression, stress, and somatic complaints.
| T1 M (SD) |
T2 M (SD) |
T3 M (SD) |
Wilks Lambda | ηp2 | Pairwise comparisons |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Time | (I-J) | Error | LLCI 95% | ULCI 95% | |||||||
| Anxiety | 3.33 (3.75) | 3.33 (3.55) | 3.33(6.79) | 1 | 0.001 | T1 | T2 | 0.01 | 0.95 | −2.69 | 2.69 |
| T1 | T3 | 0.01 | 2.13 | −6.02 | 6.01 | ||||||
| T2 | T3 | 0.01 | 1.95 | −5.51 | 5.51 | ||||||
| Depression | 6.17 (6.24) | 4.17 (4.93) | 5.67 (8.34) | 0.88 | 0.12 | T1 | T2 | 2 | 1.86 | −3.24 | 7.24 |
| T1 | T3 | 0.50 | 2.39 | −6.23 | 7.24 | ||||||
| T2 | T3 | −1.50 | 1.93 | −6.93 | 3.93 | ||||||
| Stress | 10.67 (4.77) | 8.67 (3.94) | 8.83 (6.90) | 0.52 | 0.48 | T1 | T2 | 2 | 1.23 | −1.47 | 5.47 |
| T1 | T3 | 1.83 | 1.19 | −1.53 | 5.20 | ||||||
| T2 | T3 | −0.17 | 2.11 | −6.12 | 5.78 | ||||||
| Anger | 1.86 (0.27) | 1.71 (0,27) | 1.75(0.34) | 0.77 | 0.23 | T1 | T2 | 0.15⁎⁎⁎ | 0.06 | 0.01 | 0.29 |
| T1 | T3 | 0.11 | 0.06 | −0.05 | 0.27 | ||||||
| T2 | T3 | −0.04 | 0.06 | −0.18 | 0.10 | ||||||
| Fear | 1.73 (0.45) | 1.44 (0.29) | 1.48(0.31) | 0.62 | 0.38 | T1 | T2 | 0.29⁎ | 0.09 | 0.07 | 0.51 |
| T1 | T3 | 0.25⁎ | 0.07 | 0.08 | 0.42 | ||||||
| T2 | T3 | −0.04 | 0.06 | −0.19 | 0.11 | ||||||
| Sadness | 1.55 (0.28) | 1.38 (0.32) | 1.38 (0.30) | 0.76 | 0.24 | T1 | T2 | 0.17 | 0.07 | −0.01 | 0.35 |
| T1 | T3 | 0.17 | 0.07 | −0.02 | 0.36 | ||||||
| T2 | T3 | 0.01 | 0.7 | −0.19 | 0.19 | ||||||
| Happiness | 0.84 | T1 | T2 | −0.14 | 0.07 | −0.33 | 0.05 | ||||
| 2.44 (0.41) | 2.58 (0.39) | 2.61 (0.44) | 0.12 | T1 | T3 | −0.17 | 0.08 | −0.39 | 0.05 | ||
| T2 | T3 | 0.14 | 0.07 | −0.05 | 0.33 | ||||||
| Somatic complaints | 0.95 | T1 | T2 | 0.02 | 0.04 | −0.10 | 0.13 | ||||
| 1.32 (0.26) | 1.30 (0.20) | 1.33 (0.24) | 0.01 | T1 | T3 | −0.12 | 0.06 | −0.17 | 0.14 | ||
| T2 | T3 | −0.03 | 0.04 | −0.12 | 0.06 | ||||||
| Resilience | 0.99 | T1 | T2 | – | – | – | – | ||||
| 29.13 (0.82) | – | 28.94 (0.77) | 0.01 | T1 | T3 | 0.19 | 0.56 | −0.95 | 1.32 | ||
| T2 | T3 | – | – | – | – | ||||||
Note: ηp2 = partial Eta Square; T1 = Two-three weeks of confinement; T2 = Six weeks of confinement; T3 = Nine weeks of confinement; LLCI = Lower limit confidence interval; ULCI = Upper limit confidence interval.
p < .05.
p < .01.
Fig. 2.
Progression of mood dimensions.
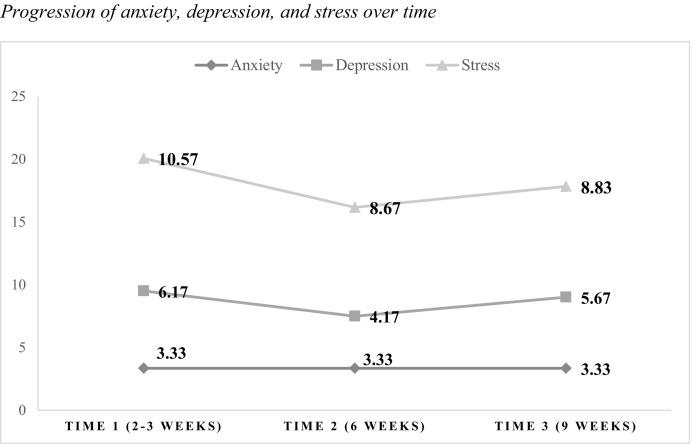
No major differences were found between the different assessment times as regards levels of anxiety, depression, and stress, although as Fig. 3 indicates, the averages at time 1 were slightly higher in for depression and stress. In the case of stress, there was a tendency to decline between time 2 and 3. In the case of depression, the levels remained slightly lower until time 2 and tended to increase until time 3. Finally, anxiety levels remained similar over time. In general, stress presented the highest levels compared to the rest of the dimensions analyzed.
Fig. 3.
Progression of anxiety, depression, and stress over time.
Finally, no differences were observed in either the somatic complaints or the resilience capacity of adolescent caregivers. Nevertheless, in descriptive terms, there was a tendency for somatic complaints to be maintained over time and another trend for resilience capacity to be slightly reduced.
Consequences of COVID-19 on the variables studied
Finally, we analyzed the influence of the death of a loved one on the mean scores obtained in the variables obtained at time 2 (after one and a half months of state of alert) and in time 3. Statistically significant differences were found for stress (t 30 = −1.99; p = .05; d = 0.84), sadness (t 32 = −2.28; p = .03; d = 0.92), fear (t 32 = −2.00; p = .05; d = 0.83) and anger (t 32 = −2.51; p = .02; d = 1.04). At the time points moments analyzed, people who had experienced the loss of a close one due to COVID-19 presented a sadder state of mind, with more anger, greater sensation of fear and higher levels of stress.
Discussion
To date, very few longitudinal and cross-sectional studies have been conducted in Spain on parents of adolescents aimed at addressing risk factors and mental health protection during the COVID-19 pandemic. This is a major gap in research, as adolescents, as part of the pediatric population, have differential difficulties and needs, which can place a greater emotional burden on family members. Our study simultaneously considers sociodemographic and clinical factors, psychopathology, the presence of positive and negative emotions, and resilience. The existing research analyzes these variables separately, using either cross-sectional or longitudinal designs, but not mixed designs (Orgilés et al., 2020; Prime, Wade, & Browne, 2020; Wang et al., 2020a, Wang et al., 2020b). By means of the mixed design, we can arrive at a greater understanding of the well-being, functioning and family adjustment of parents of adolescents.
The objective of our research is to determine the adjustment and the psycho-emotional impact (emotionality, anxious, depressive symptoms, stress and somatization) in the COVID-19 pandemic among the parents of adolescents, carrying out a cross-sectional and longitudinal study. We also aim to understand the role of resilience in this context.
Our results show that at the beginning of the pandemic, parents had low levels of psychopathology, accompanied by low negative emotionality, a moderate presence of positive emotions (happiness) and resilience. According to the literature, most people will adapt successfully to stressful life events. When analyzing these factors, our findings point to the importance of considering both positive and negative aspects in adjusting to stressful events. The presence of distress does not prevent positive emotions, since negative and positive affect are different constructs (Stanton & Revenson, 2007). In this respect, Fredrickson (2001) highlights how experiencing positive emotions can increase a person's resources and act as a buffer against the negative physiological consequences of stress. Emotional adjustment must therefore be understood in a context that is a dynamic and continuous process, in which an individual's psychological state can change as the psychosocial demands change, taking into account that the experience is subjective (Stanton & Revenson, 2007).
As regards the prediction of mental health indicators, it should be noted that the lowest levels of resilience were relevant for predicting both anxiety and depression. Our results confirm that resilience plays an important role in mental health, and specifically in coping with the pandemic. Our data are particularly relevant since other authors of recent studies have reported data like ours in their results. In their studies, lower levels of resilience to the COVID-19 pandemic were associated with higher levels of psychopathology and even greater suicide risk (Killgore et al., 2020). Our study highlights the importance of promoting intervention programs aimed at improving resilience in the family environment, specifically in the parents of adolescents, since the improvement of mental health in one member of the system can improve the mental health of the rest of the system (Liu et al., 2020).
On the other hand, in predicting stress in parents of adolescents, low positive emotionality was the most relevant variable. Our data indicate the importance of promoting positive emotions in the family system, since family environments characterized by affection and positive emotions foster the adaptation of the members of the system (Prime, Wade, & Browne, 2020). However, this adjustment may be influenced by the presence of additional difficulties (Espada et al., 2020). Parents who already had a previous mental health problem or those who lost their job or a loved one during the pandemic have shown more worrying and worse levels of mental health indicators (Brooks et al., 2020; Campbell, 2020; Zhai and Du, 2020a, Zhai and Du, 2020b). It is important at this point to note that the deaths of their loved ones were recent. This greater presence of emotional symptoms and negative emotionality could therefore be considered part of the process of adjustment to the loss (Lenferink et al., 2020). This is especially important in the case of deaths caused by COVID-19, because on most occasions, family members have not had the opportunity to say goodbye to their loved one. Therefore, in the future, it would be interesting to carry out follow-up evaluations of these parents' mental health, a year or more after the loss of their loved one.
As far as the longitudinal study of variables is concerned, the mental health of the parents seems to have improved over time. Resilience remained stable, always presenting moderate or high values. These findings are contrary to what the literature suggests, and as such we recommend further longitudinal studies to clarify the behavior of these variables. The studies reviewed point out how in the face of the COVID pandemic, mental health can be maintained or may even deteriorate (Espada et al., 2020; Inchausti et al., 2020). These data, which are a priori contradictory, are better explained if the sociodemographic and clinical variables studied are considered. Our research would suggest other variables, such as the loss of a job or a loved one, the presence of a previous mental health problem and greater negative emotionality, which are mainly associated with worse mental health outcomes (Brooks et al., 2020; Campbell, 2020; Zhai and Du, 2020a, Zhai and Du, 2020b). Therefore, we point out the need to consider socio-demographic and clinical variables as a whole.
However, the parents in our sample with previous physical health problems presented no worse mental health outcomes than those without physical health problems, although these data may be due to the fact that the pathologies they presented were not directly life-threatening, and did not put them at greater risk in terms of the pandemic. They were instead chronic conditions which they had lived with for a long time.
Practical implications
Together with the data from future research that could be carried out to support the results of our study, it will be possible to design better intervention protocols that incorporate the improvement of resilience and positive family environment as tools for protection against adversity, particularly given that the situation we are experiencing remains uncertain. It will therefore be possible to foster their adaptation to stressful life events and to prevent possible physical and mental health problems caused by this terrible global pandemic. These family interventions should have the promotion of a positive family climate among their main characteristics, as well as the strengthening of positive emotions and resilience, thereby improving the emotional adaptation of the family system.
Limitations
Nevertheless, despite the potential of our study, it has a small sample of parents of teenagers — 44% of the sample was lost to follow-up, which may partially influence the results of the study. However, it is expected in longitudinal studies or online nature of the study to have a certain drop-off, even more considering the exceptional situation we are going through. In addition, the number of weeks between first collection and time 1 and 2 may also have affected the drop-off. As a result, the characteristics of our sample and the type of sampling carried out being that generalizing the results to the general population is difficult. Further studies are needed to replicate this research, perhaps through the collection a probability sample that more adequately represents the characteristics and particular features of the parents of Spanish adolescents during the COVID-19 pandemic. Another limitation is that the reason for the sample loss was not studied; thus, it would be advisable for future studies to consider this phenomenon. Future research should evaluate the family climate as well as parental styles to gain a deeper understanding of the needs of the family system. Similarly, it would be interesting to have the evaluation of adolescents, therefore, future studies could evaluate family dyads to gain a better understanding of emotional adjustment during confinement.
Conclusions
In conclusion, our study highlights the importance of resilience in the adjustment of parents of adolescents, as well as positive emotions in the family system, which are key aspects of adjustment to stressful life situations.
Acknowledgments
Acknowledgements
Funding: This research was supported by grants from the Spanish Ministry of Science, Innovation and Universities (PSI2017-84005-R), the State Agency of Research and the European Regional Development Fund (FEDER) from the European Union. LLT is a beneficiary of the Ayuda de Atracció a Talent de la Universidad de Valencia (0113/2018).
Declaration of Competing Interest
None.
References
- European Centre for Disease Prevention and Control Covid-19. 2020. https://qap.ecdc.europa.eu/public/extensions/COVID-19/COVID-19.html
- Alavi M., Latif A.A., Ninggal M.T., Mustaffa M.S., Amini M. Family functioning and attachment among young adults in Western and non-Western societies. The Journal of Psychology. 2020;154(5):346–366. doi: 10.1080/00223980.2020.1754153. [DOI] [PubMed] [Google Scholar]
- Andrews J.L., Foulkes L., Blakemore S.-J. Peer influence in adolescence: Public-health implications for COVID-19. Trends in Cognitive Sciences. 2020;8(4):585–587. doi: 10.1016/j.tics.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bados A., Solanas A., Andrés R. Psycometric properties of the Spanish version of depression, anxiety and stress scales (DASS) Psicothema. 2005;17(4):679–683. http://dialnet.unirioja.es/servlet/articulo?codigo=1314066 [Google Scholar]
- Bobes J., Bascaran M., García-Portilla M., Bousoño M., Saiz P., Wallance D. Banco de instrumentos básicos de psiquiatría clínica. Psiquiatría Editorial. 2001 [Google Scholar]
- Brailovskaia J., Margraf J. Predicting adaptive and maladaptive responses to the Coronavirus (COVID-19) outbreak: A prospective longitudinal study. International Journal of Clinical and Health Psychology. 2020;20(3):183–191. doi: 10.1016/j.ijchp.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron E.E., Joyce K.M., Delaquis C.P., Reynolds K., Protudjer J.L.P., Roos L.E. Maternal psychological distress & mental health service use during the COVID-19 pandemic. Journal of Affective Disorders. 2020;276:765–774. doi: 10.1016/j.jad.2020.07.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell A.M. An increasing risk of family violence during the Covid-19 pandemic: Strengthening community collaborations to save lives. Forensic Science International: Reports. 2020;2:100089. doi: 10.1016/j.fsir.2020.100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell-Sills L., Stein M. Psychometric analysis and refinement of the Connor–Davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of Traumatic Stress. 2007;20:1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- Clara I., Cox B., Enns M. Confirmatory factor analysis of the depression–anxiety–stress scales in depressed and anxious patients. Journal of Psychopathology and Behavioral Assessment. 2001;23:61–67. doi: 10.1023/A:1011095624717. [DOI] [Google Scholar]
- Collins C., Landivar L.C., Ruppanner L., Scarborough W.J. COVID-19 and the gender gap in work hours. Gender, Work and Organization. 2020:1–12. doi: 10.1111/gwao.12506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor K.M., Davidson J.R.T. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC) Depression and Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Coronavirus Resource Center COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) 2021. https://coronavirus.jhu.edu/map.html
- Crawford J.R., Henry J.D. The depression anxiety stress scales: Normative data and latent structure in a large non-clinical sample. British Journal of Clinical Psychology. 2003;42:111–131. doi: 10.1348/014466503321903544. [DOI] [PubMed] [Google Scholar]
- Daza P., Novy D., Stanley M., Averill P. The depression anxiety stress Scale-21: Spanish translation and validation with a Hispanic sample. Journal of Psychopathology and Behavioral Assessment. 2002;24:195–205. doi: 10.1023/A:1016014818163. [DOI] [Google Scholar]
- El-Masri M., Ramsay A., Ahmed H.M., Ahmad T. Positive sentiments as coping mechanisms and path to resilience: The case of Qatar blockade. Information, Communication & Society. 2020:1–19. doi: 10.1080/1369118X.2020.1748086. [DOI] [Google Scholar]
- Espada J.P., Orgilés M., Piqueras J.A., Morales A. Las Buenas Prácticas en la Atención Psicológica Infanto-juvenil ante el COVID-19. Clínica y Salud. 2020;31(2):109–113. doi: 10.5093/clysa2020a14. [DOI] [Google Scholar]
- Fonseca-Pedrero E., Paino M., Lemos-Giráldez S., Muñiz J. Propiedades psicométricas de la escala de depresión, ansiedad y estrés versión 21 (DASS-21) eun universitarios españoles. Ansiedad y Estrés. 2010;16(2–3):215–226. [Google Scholar]
- Fredrickson B.L. The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. The American Psychologist. 2001;56(3):218–226. doi: 10.1037/0003-066x.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt K. The COVID-19 pandemic: Technology use to support the wellbeing of children. Journal of Pediatric Nursing. 2020;53:88–90. doi: 10.1016/j.pedn.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Górriz A., Prado-Gascó V.J., Villanueva L., Ordónez A., González R. The MOOD questionnaire : Adaptation and validation of the Spanish version. Psicothema. 2013;25(2):252–257. doi: 10.7334/psicothema2012.201. [DOI] [PubMed] [Google Scholar]
- Inchausti F., García-Poveda N., Prado-Abril J., Sánchez-Reales S. Clínica y Salud. 2020;31(2):105–107. doi: 10.5093/clysa2020a11. [DOI] [Google Scholar]
- Killgore W.D.S., Taylor E.C., Cloonan S.A., Dailey N.S. Psychological resilience during the COVID-19 lockdown. Psychiatry Research. 2020;291:113216. doi: 10.1016/j.psychres.2020.113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenferink L.I.M., Nickerson A., de Keijser J., Smid G.E., Boelen P.A. Trajectories of grief, depression, and posttraumatic stress in disaster-bereaved people. Depression and Anxiety. 2020;37(1):35–44. doi: 10.1002/da.22850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Ge T., Jiang Q. Changing family relationships and mental health of Chinese adolescents: The role of living arrangements. Public Health. 2020;186:110–115. doi: 10.1016/j.puhe.2020.06.026. [DOI] [PubMed] [Google Scholar]
- Liu C.H., Zhang E., Wong G.T.F., Hyun S., Hahm H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research. 2020;290:113172. doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck depression and anxiety inventories. Behaviour Research and Therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Ministerio de Sanidad, C. y B. S. (2020). Situación del COVID en España. https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/situacionActual.htm
- Notario-Pacheco B., Solera-Martínez M., Serrano-Parra M.D., Bartolomé-Gutiérrez R., García-Campayo J., Martínez-Vizcaíno V. Reliability and validity of the Spanish version of the 10-item Connor-Davidson Resilience Scale (10-item CD-RISC) in young adults. Health and Quality of Life Outcomes. 2011;9(1):63. doi: 10.1186/1477-7525-9-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgilés M., Morales A., Delvecchio E., Francisco R., Pedro M., Espada J.P. Coping behaviors and psychological disturbances in youth affected by the COVID-19 health crisis. 2020. [DOI] [PMC free article] [PubMed]
- Orkaizagirre-Gómara A., Sánchez De Miguel M., Ortiz de Elguea J., Ortiz de Elguea A. Testing general self-efficacy, perceived competence, resilience, and stress among nursing students: An integrator evaluation. Nursing & Health Sciences. 2020;22(3):529–538. doi: 10.1111/nhs.12689. [DOI] [PubMed] [Google Scholar]
- Orte, C., Ballester, L., & Nevot, L. (2020). Apoyo Familiar ante el COVID-19 en España. https://www.researchgate.net/publication/341151936_APOYO_FAMILIAR_ANTE_EL_COVID-19_EN_ESPANA
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rieffe C., Oosterveld P., Miers A.C., Meerum Terwogt M., Ly V. Emotion awareness and internalising symptoms in children and adolescents: The Emotion Awareness Questionnaire revised. Personality and Individual Differences. 2008;45(8):756–761. doi: 10.1016/j.paid.2008.08.001. [DOI] [Google Scholar]
- Rieffe C., Oosterveld P., Terwogt M.M. An alexithymia questionnaire for children: Factorial and concurrent validation results. Personality and Individual Differences. 2006;40(1):123–133. doi: 10.1016/j.paid.2005.05.013. [DOI] [Google Scholar]
- Rieffe C., Terwogt M.M., Petrides K.V., Cowan R., Miers A.C., Tolland A. Psychometric properties of the Emotion Awareness Questionnaire for children. Personality and Individual Differences. 2007;43(1):95–105. doi: 10.1016/j.paid.2006.11.015. [DOI] [Google Scholar]
- Silva N., Bullinger M., Sommer R., Rohenkohl A., Witt S., Quitmann J. Children’s psychosocial functioning and parents’ quality of life in paediatric short stature: The mediating role of caregiving stress. Clinical Psychology & Psychotherapy. 2018;25(1):e107–e118. doi: 10.1002/cpp.2146. [DOI] [PubMed] [Google Scholar]
- Stanton A., Revenson T. In: Foundations of Health Psychology. Howard S., Roxane C.S., editors. Oxford University Press; 2007. Adjustment to chronic disease: Progress and promise in research; pp. 214–244. [Google Scholar]
- United Nations New York: Intergovernmental Organization. (2020). Children vulnerable to abuse and violence during coronavirus lockdowns, UN experts warn; [about 2 screens]. https://news.un.org/en/story/2020/04/1061282
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) Internaional Journal of Enviromental Research and Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S.…Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. 2020;7(4) doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai Y., Du X. Loss and grief amidst COVID-19: A path to adaptation and resilience. Brain, Behavior, and Immunity. 2020;87:80–81. doi: 10.1016/j.bbi.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai Y., Du X. Addressing collegiate mental health amid COVID-19 pandemic. Psychiatry Research. 2020;288:113003. doi: 10.1016/j.psychres.2020.113003. [DOI] [PMC free article] [PubMed] [Google Scholar]