A randomized clinical trial found that brief sexual risk reduction counseling increased condom use for men and women and reduced clinic revisits for women receiving sexually transmitted infection services in Cape Town, South Africa.
Abstract
Background
Evidence-based interventions are needed to stem sexually transmitted infections (STIs). Clinic-delivered counseling remains an important avenue for effective STI prevention.
Methods
A 3-arm randomized clinical trial compared (a) STI health education control condition, (b) risk reduction counseling, and (c) enhanced partner notification counseling. Men and women (n = 1050) were recruited from an STI clinic in Cape Town, South Africa. After baseline assessments, participants were randomly allocated to receive 1 of the 3 single-session counseling interventions and were followed up for 9 months of behavioral assessments and 12 months of electronic medical records abstraction for STI clinic services.
Results
Sexual risk reduction counseling reported greater condom use than did the other 2 conditions during the 3 and 6 months follow-ups. In addition, women receiving risk reduction counseling were significantly less likely to have returned for STI clinic services but did not differ in the number of STI clinic visits over the year.
Conclusions
Brief single-session STI prevention counseling demonstrates significant targeted outcomes. The findings suggest that counseling approaches to both increase condom use and enhance partner notification may offer more robust and sustained outcomes and should be tested in future research.
Brief counseling interventions that aim to increase condom use have demonstrated efficacy in reducing sexually transmitted infections (STIs).1 These interventions are conceptually grounded in cognitive-behavioral theoretical models of health behavior change, such as the Information-Motivation-Behavioral Skills (IMB) model.2,3 Intended to inform HIV risk reduction interventions, the IMB model has proven useful in building behavioral skills with the aim of increasing condom use.4–7 The IMB model posits that condom use is a function of information on the behavior, motivation to change the behavior, and having the requisite behavioral skills to perform the behavior.8
In addition to condom use, public health approaches to preventing STI also rest on notifying sex partners of those who are diagnosed and treated for an STI. Partner notification in resource constrained settings relies on patients who have been diagnosed with an STI to self-notify their partners and encourage them to get tested and treated. When effective, partner notification interrupts the chain of STI transmission by reducing community-level disease burden. We recently reported the effects of an intervention from the current trial designed to enhance partner notification in South Africa.9 We found that the single 45-minute counseling session grounded in the IMB model significantly increased notifications to sex partners during a 2-week period; specifically, 64% of patients receiving enhanced partner notification counseling notified partners relative to 53% of patients in a health education counseling control condition. However, we did not find a significant effect of enhanced partner notification counseling on the number of STI clinic visits during a 12-month period.
The aims of this article are to fully report the behavioral and STI outcomes from our 3-arm randomized trial in which we tested brief risk reduction sexual behavior change counseling as well as brief enhanced partner notification counseling along with a brief STI education session that served as a control condition. Participants were followed up for 9 months after counseling to monitor risk behavior change. We extend our previous analysis to examine STI clinic visits using 2 approaches, the number of STI clinic visits for 12 months as a continuous variable and the occurrence of any return STI clinic visit for 12 months as a dichotomous variable. In settings where syndromic management of STIs is the standard of care, STI clinic visits are a proxy for risk exposures and offer an objective indicator of STI occurrence in the absence of biological STI screening. We hypothesized that risk reduction counseling would result in greater condom use than the enhanced partner notification and health education conditions, and that both the risk reduction and enhanced partner notification conditions would result in fewer participants returning for STI clinic visits compared with the STI education control condition. We also hypothesized that all 3 counseling models would increase STI prevention knowledge and reduce HIV stigma beliefs, whereas only risk reduction and enhanced partner notification interventions would increase self-efficacy for practicing STI preventive behaviors.
METHODS
Participant Recruitment and Enrollment
Sexually transmitted infection clinic patients were referred by nurse clinicians to participate in a prevention counseling study. All patients referred who were 18 years and older and were being presumptively treated for an STI at the clinic were invited to participate. Recruitment occurred in the clinic waiting area on the day of their STI visits. Patients who enrolled in the study were scheduled for a baseline assessment and counseling session in which they received informed consent, a computerized baseline assessment, and a single counseling session. Sampling occurred throughout all hours of clinic operation between June 2014 and August 2017. After providing informed consent, participants completed an interview, described hereinafter, that included participant characteristics and partner-by-partner sex behaviors.
Study Design and Procedures
Figure 1 shows the flow of participants through the trial. Immediately after baseline assessments, participants were randomly allocated with a 1:1:1 ratio to receive (a) health education counseling, (b) behavioral skills building sexual risk reduction counseling, or (c) enhanced partner notification counseling. Participants were scheduled for follow-up assessments 2 weeks and 3, 6, and 9 months after counseling. The 2-week partner notification outcomes are reported elsewhere.9 Participants had the option to complete interviews in English or isiXhosa. In addition, participants provided consent for the researchers to access their electronic clinical records over the subsequent 12 months to code clinic visits and extract new STI visits. Participants received approximately US$10 for each completed assessment.
Figure 1.
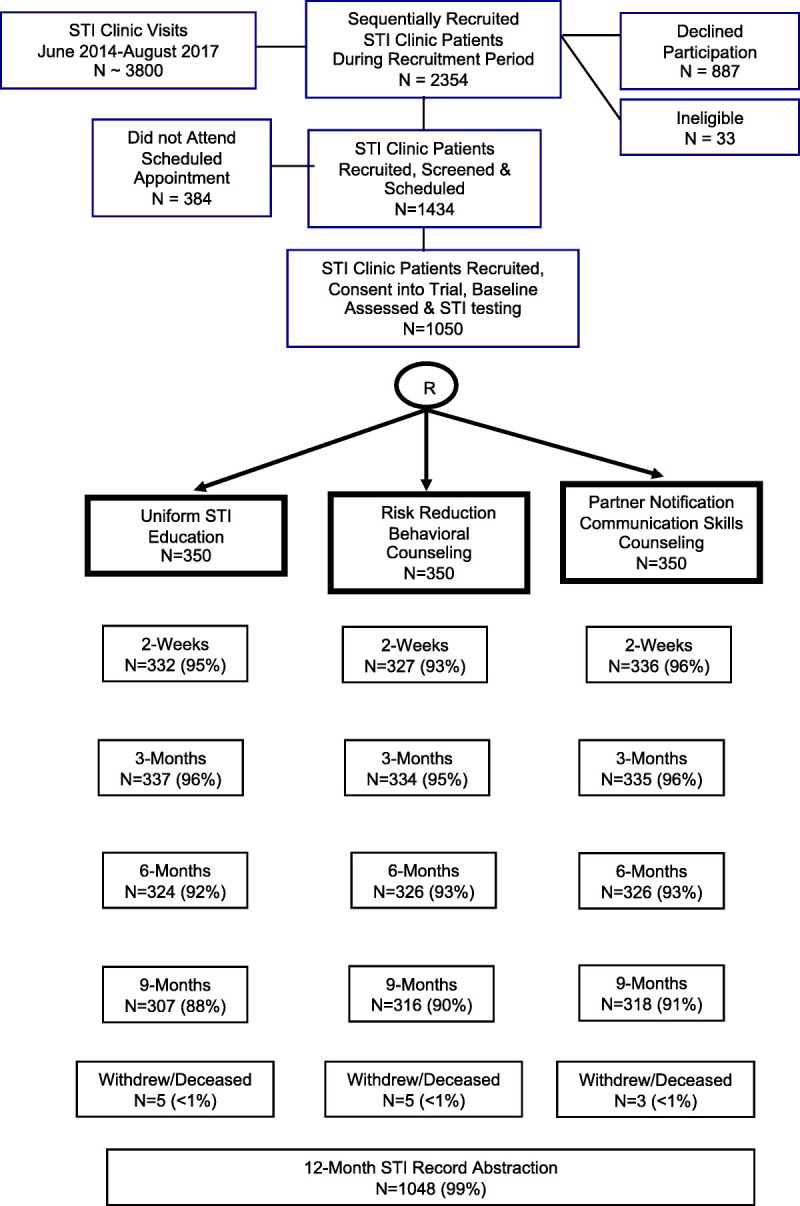
Flow of participants through the 3-arm randomized trial.
Ethical Review and Trial Registry
All study procedures were approved by the University of Connecticut and the South African Medical Research Council institutional review boards. The trial was registered with the Pan African Clinical Trial Registry (www.pactr.org) PACTR201606001682364.
Randomization and Blinding
Participants were allocated by the study recruitment and scheduling staff to treatment conditions using a randomization list generated at http://www.randomization.com. We generated a 3 equal-size block/group randomization scheme for allocating individuals to 1 of the 3 treatment conditions. Partners of already enrolled participants were yoked to the same condition. Otherwise, randomization was not breached throughout the trial. Recruitment, screening, and assessment staff remained blinded to condition throughout the study, and counselors never conducted assessments of participants that they counseled.
Adverse Events
There was one adverse event during the course of the trial. A male participant reported having a sexual partner under the age of consent. The institutional review board determined that the case required breaching confidentiality to comply with mandatory reporting statutes.
Intervention Conditions
Participants were randomized to 1 of the 3 intervention conditions. Two women lay counselors who were bilingual in English and isiXhosa languages delivered the counseling to men and women across all 3 conditions in keeping with standard clinic services. To reduce risk of cross-contamination, all 3 conditions were manualized and used tabletop flipcharts to guide the sessions. Counselors met weekly with the project management team to review sessions and monitor fidelity. With participant consent, counseling sessions were audio-recorded and reviewed by project management for quality assurance.
STI Health Education Counseling
Health education counseling served as a comparison condition in this trial. The counseling consisted of a single 20-minute session in which the counselor provided information on STI/HIV prevention, symptoms, transmission, testing, and treatment. The counselor answered participants' questions and corrected misconceptions. This condition was designed to provide a uniform standardized version of the current lay counselor activities offered in South African STI services.
Risk Reduction Counseling
The risk reduction counseling condition was adapted from a single 45-minute session STI prevention intervention that has demonstrated efficacy for STI prevention in previous trials.5 This risk reduction counseling is grounded in the IMB model of behavior change.3 As described elsewhere,10 the information component of the counseling reviewed facts about STI transmission and risk behaviors, discussed the local prevalence of STI, clarified misconceptions, dispelled STI myths, and described HIV antibody testing. The motivation component integrated motivational counseling techniques that included motivation for change and strengthening commitment to change. The final component of the risk reduction counseling focused on behavioral self-management, sexual communication, and condom use skills building. Counselors explained how to recognize environmental and cognitive-affective cues that serve as “triggers” for high-risk situations, including mood states, substance use, places, and sexual partner characteristics. Correct male and female condom use was instructed and modeled allowing participants to practice condom application on wooden models with corrective feedback from the counselor. Behavioral rehearsal was conducted in role-plays to enhance risk reduction skills. The session ended with participants creating personalized goals and a risk reduction plan that they took with them.
Enhanced Partner Notification
This condition was also informed by the IMB model and was delivered in a single 45-minute counseling session. The lay counselors provided information on preventing the spread of STIs and used interactive, motivation-enhancing and skills-building exercises to promote the notification, and referral of their recent sex partners. The counselors presented a menu of options for partner notification and referral, which included face-to-face communication, telephone calls, text messages, e-mail, delivery of a referral card, and inviting partners to attend the clinic together with index patients, as well as provider-assisted referral options undertaken by the lay counselor while maintaining the index patient's anonymity. The counselors assisted the participant to choose the best option for each partner. The counselor probed for challenges that may be encountered in notifying partners and conducted role play rehearsals and problem-solving challenges. The session ended with specific goals for the participant to achieve with respect to partner notification.
Measures
Participant Characteristics
Participants reported their demographic characteristics including age, sex, education, marital status, whether they had children, HIV testing and treatment history, and history of STI symptoms and diagnoses. To assess alcohol use, participants reported how often and how much they typically drink (frequency and quantity) using the Alcohol Use Disorders Identification Test for Consumption scale.11,12 Participants also reported their use of cannabis, amphetamines, and other drugs. The HIV testing history component asked about whether participants had been tested for HIV and the results of their most recent HIV test.
Primary STI Outcome
The primary outcome for this trial was return STI visits over the course of 12 months after counseling. Sexually transmitted infection diagnoses and treatment based on syndromic approach were extracted from a citywide electronic medical records system. Sexually transmitted infection visits therefore represent all city of Cape Town health clinic STI visits during the 12-month period. We report 2 approaches to examining STI visits. First, as reported previously,9 we examined the number of annual STI clinic visits as a continuous variable. Second, we report for the first time the occurrence of any returning STI visit during the 12 months, a dichotomous outcome.
Primary Sexual Behavior Outcomes
Participants identified by first name or nickname up to 5 sex partners during the prior 3 months. Identifiers were recorded on a form by the interviewer along with responses to detailed questions regarding partner characteristics, relationship history, and sexual behaviors. For each partner, participants reported the number of times they had vaginal and anal intercourse during the previous 3 months. Condom use was assessed using a continuous 100-point rating scale representing the percent of times condoms were used with each partner, separately for vaginal and anal intercourse, ranging from no condom use (0% condom use) to every occasion (100% condom use). This measure was adapted from a validated 100-point rating scale that has become standard for estimating the proportion of medications taken to assess HIV treatment adherence.13
Secondary Outcomes
STI Prevention Knowledge
Four heterogeneous items assessed STI risk and prevention-related knowledge. Items were adapted from a measure reported by Carey and Schroder14 and reflected information on STI transmission, responded to as “Yes, this true,” “No, this is not true,” or “I do not know.” Example items included “A person can stop taking STI medication when symptoms go away” and “You can tell if a sex partner has an STI just by looking at them?” Correct responses were summed across items.
HIV Stigma
We administered a 6-item adaptation of the HIV Stigma Scale developed for use in southern Africa.15 The stigma items reflect negative beliefs about people living with HIV, shamefulness of the behavior of people living with HIV, and the endorsement of social sanctions against people living with HIV, such as “People who have HIV/AIDS are cursed” and “People who have HIV/AIDS should be ashamed.” Stigma items were responded to on 4-point rating scales from “1 = strongly disagree” to “4 = strongly agree.” Responses were averaged across items, with higher scores indicating greater stigma (α = 0.65).
Prevention Skills Self-Efficacy
Defined as the personal sense of confidence that one can perform specific behaviors under specified conditions, self-efficacy is commonly used as a proxy for behavioral skills.16,17 The current self-efficacy scale consisted of 8 items including “How confident are you that you can tell a casual sex partner that you had an STI” and “How confident are that you can talk to your main sex partner about the need to use condoms?” Items were responded to on an 11-point response set, with 0 indicating “not at all confident” and 10 indicating “very confident.” Responses were averaged across items to create a single self-efficacy score, with higher scores indicating stronger self-efficacy (α = 0.79).
Statistical Power
The sample size was determined using an effect size of 20% reduction in STI based on previous trials.1,5 Using an α level of 0.05, a sample size of 1050 distributed across 3 conditions and partitioned by gender was determined sufficient to allow for the detection of a 0.20 difference in annual STI events across 3 conditions × gender with a power of 0.80.
Data Analyses
We first conducted analyses to examine the integrity of the randomization procedures and study design.18 All primary and secondary outcome analyses used an intent-to-treat approach. Outcome analyses tested models that included main effects for intervention condition and participant gender, and the intervention condition × gender interactions. Baseline scores were included as covariates in all analyses and all models used robust estimators. Planned contrasts with least significant difference adjustment were used to test for simple effects.
The primary outcome analyses tested study hypotheses regarding intervention effects on return STI visits and sexual behaviors. For STI outcomes, analyses were performed on the chart-abstracted STI visits using generalized linear models. Poisson distribution was used for the number of return STI visits, a count variable, and binomial distribution for having any return STI visit, a dichotomous variable. For repeated behavioral assessments, we used generalized estimating equations (GEEs) for the 3-, 6-, and 9-month follow-up, controlling for baseline values. Along with intervention condition and gender, as well as their interaction, we included the repeated measures variable and its interaction with each factor in all models. Poisson distribution was used for count data (i.e., number of sex acts) and linear distributions for scaled data (e.g., percent condom use and theoretical constructs). Wald χ2 statistics are reported with statistical significance defined as P < 0.05.
RESULTS
Clinic nurses made 2354 STI patient referrals to the study, of which 33 were ineligible and 887 declined participation. In addition, 384 of those who were eligible and scheduled for enrollment did not attend the enrollment appointment. A final sample of 1050 participants were enrolled in the trial (Fig. 1). Overall, there was 90% retention in the trial cohort during 9-month observation, with 98% of 12 months of clinical records available for review. There were no significant differences between conditions for retention rates at any time point. Participants had 34 partners enrolled in the study, and they were evenly distributed across conditions. Gender was not stratified by design but was evenly distributed across conditions. There were no significant differences across conditions for any demographic characteristics, and demographic characteristics were not associated with attrition (Table 1).
TABLE 1.
Baseline Characteristics of Trial Participants Allocated to the 3 Intervention Conditions
| Health Education | Risk Reduction | Enhanced Partner Notification | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Women | 173 | 50 | 174 | 51 | 175 | 50 |
| Men | 177 | 50 | 176 | 49 | 175 | 50 |
| MSM | 3 | 1 | 6 | 2 | 5 | 2 |
| Identified race as Black/African | 341 | 97 | 344 | 98 | 340 | 97 |
| Men circumcised | 147 | 84 | 151 | 85 | 157 | 90 |
| Currently married | 32 | 9 | 24 | 7 | 23 | 7 |
| Living with a partner | 60 | 19 | 66 | 20 | 64 | 20 |
| High school completion | 150 | 42 | 172 | 49 | 151 | 43 |
| HIV positive | 73 | 23 | 66 | 20 | 66 | 20 |
| Hazardous alcohol use* | 213 | 61 | 240 | 69 | 232 | 66 |
| Any drug use | 77 | 22 | 82 | 23 | 79 | 23 |
| Mean | SD | Mean | SD | Mean | SD | |
| Age, y | 29.4 | 7.8 | 28.6 | 7.2 | 29.5 | 6.9 |
| No. sex partners, past 3 mo | ||||||
| Main partners | 0.9 | 0.3 | 0.9 | 0.4 | 1.0 | 0.4 |
| Casual partners | 0.8 | 1.2 | 0.8 | 1.2 | 0.8 | 1.4 |
| Once-off partners | 0.4 | 1.0 | 0.5 | 1.4 | 0.5 | 1.9 |
| Total partners | 2.1 | 1.6 | 2.3 | 1.9 | 2.3 | 3.1 |
There were no significance between conditions on baseline characteristics.
*Hazardous alcohol use defined by Alcohol Use Disorders Identification Test for Consumption scores greater the 3 for men and greater than 2 for women.
Primary STI Outcome
Analyses of the number of STI visits (i.e., the continuous count of STI visits) did not differ across counseling conditions (Wald χ2 = 1.06, P = 0.58), and there was no counseling condition × gender interaction (Wald χ2 = 3.91, P = 0.14; Table 2). However, the main effect of gender was significant (Wald χ2 = 6.39, P = 0.01); men had more return visits than did women. Analyses for having returned to the clinic at least once for an STI visit during the 12 months after counseling (i.e., dichotomous STI visit) found that the difference between counseling conditions was not significant (Wald χ2 = 1.44, P = 0.48). There was again a significant main effect of gender (Wald χ2 = 6.81, P = 0.01); men were more likely to have returned for an STI visit than women. In addition, the counseling condition × participant gender interaction was significant (Wald χ2 = 6.02, P = 0.04); women receiving the risk reduction counseling were significantly less likely to have returned for an STI visit than men and women in the other conditions (Fig. 2).
TABLE 2.
Sexual Behaviors and Condom Use Outcomes for the 3 Intervention Conditions
| Health Education | Risk Reduction | Enhanced Partner Notification | Condition | Condition × Gender | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | Wald χ2 | P | Wald χ2 | P | |
| Any return STI visits, 12 mo | ||||||||||
| All participants | 91 | 26 | 81 | 23 | 81 | 23 | 1.44 | 0.48 | 6.02 | 0.04 |
| Men | 51 | 29 | 54 | 30 | 40 | 23 | ||||
| Women | 40 | 23 | 27 | 16 | 41 | 23 | ||||
| No. return STI visits, 12 mo | Mean | SE | Mean | SE | Mean | SE | ||||
| All participants | 0.32 | 0.03 | 0.27 | 0.03 | 0.29 | 0.03 | 1.06 | 0.58 | 3.91 | 0.14 |
| Men | 0.38 | 0.05 | 0.38 | 0.04 | 0.29 | 0.04 | ||||
| Women | 0.27 | 0.04 | 0.20 | 0.04 | 0.29 | 0.04 | ||||
| Vaginal sex occasions | Mean | SD | Mean | SD | Mean | SD | ||||
| Baseline All participants |
28.6 | 41.7 | 33.7 | 69.9 | 29.7 | 48.7 | 1.79 | 0.40 | 0.79 | 0.67 |
| Men | 35.7 | 5.4 | 36.4 | 80.2 | 34.3 | 61.5 | ||||
| Women | 21.1 | 26.3 | 30.8 | 57.1 | 25.0 | 29.7 | ||||
| 3 mo | ||||||||||
| All participants | 22.0 | 25.6 | 31.3 | 70.5 | 22.4 | 30.5 | ||||
| Men | 24.8 | 26.7 | 39.0 | 89.6 | 25.4 | 36.1 | ||||
| Women | 19.2 | 24.3 | 23.0 | 40.0 | 19.3 | 23.2 | ||||
| 6 mo | ||||||||||
| All participants | 27.9 | 42.4 | 31.0 | 68.4 | 28.3 | 38.1 | ||||
| Men | 35.5 | 53.9 | 39.0 | 91.3 | 30.1 | 38.3 | ||||
| Women | 20.4 | 24.5 | 22.8 | 28.8 | 26.5 | 38.0 | ||||
| 9 mo | ||||||||||
| All participants | 33.5 | 44.7 | 40.0 | 76.3 | 32.3 | 69.4 | ||||
| Men | 40.0 | 48.2 | 47.5 | 98.5 | 37.7 | 91.2 | ||||
| Women | 27.1 | 40.0 | 32.3 | 42.1 | 27.0 | 37.6 | ||||
| Vaginal sex, % condom use | ||||||||||
| Baseline | ||||||||||
| All participants | 40.8 | 33.8 | 41.1 | 34.7 | 40.1 | 34.3 | 10.16 | 0.01 | 1.63 | 0.44 |
| Men | 40.2 | 31.8 | 42.2 | 35.1 | 42.1 | 32.7 | ||||
| Women | 41.4 | 35.9 | 39.8 | 34.3 | 38.0 | 35.9 | ||||
| 3 mo | ||||||||||
| All participants | 53.9 | 40.1 | 60.0 | 40.4 | 50.9 | 39.6 | ||||
| Men | 54.1 | 40.1 | 61.0 | 40.1 | 52.6 | 38.8 | ||||
| Women | 53.4 | 41.5 | 58.9 | 40.9 | 49.1 | 40.4 | ||||
| 6 mo | ||||||||||
| All participants | 49.5 | 40.8 | 59.5 | 39.5 | 52.2 | 41.2 | ||||
| Men | 45.7 | 41.0 | 61.7 | 39.4 | 53.7 | 39.6 | ||||
| Women | 53.3 | 40.5 | 57.4 | 39.7 | 50.7 | 42.9 | ||||
| 9 mo | ||||||||||
| All participants | 50.2 | 40.2 | 56.3 | 40.9 | 51.6 | 41.8 | ||||
| Men | 45.6 | 38.4 | 56.2 | 39.3 | 50.7 | 41.1 | ||||
| Women | 54.9 | 41.5 | 56.5 | 42.7 | 52.5 | 42.7 | ||||
| Anal sex occasions | ||||||||||
| Baseline | ||||||||||
| All participants | 0.8 | 6.4 | 1.0 | 6.9 | 0.4 | 1.8 | 0.62 | 0.73 | 4.21 | 0.12 |
| Men | 0.6 | 3.1 | 1.5 | 8.5 | 0.5 | 2.3 | ||||
| Women | 1.1 | 8.7 | 0.6 | 4.6 | 0.2 | 0.8 | ||||
| 3 mo | ||||||||||
| All participants | 0.4 | 2.7 | 1.2 | 8.2 | 0.7 | 6.3 | ||||
| Men | 0.5 | 3.3 | 1.8 | 10.4 | 1.0 | 8.3 | ||||
| Women | 0.4 | 1.8 | 0.6 | 4.7 | 0.5 | 3.1 | ||||
| 6 mo | ||||||||||
| All participants | 0.4 | 2.9 | 0.5 | 3.2 | 0.7 | 4.0 | ||||
| Men | 0.4 | 3.6 | 0.8 | 4.5 | 1.1 | 5.3 | ||||
| Women | 0.3 | 2.0 | 0.2 | 1.0 | 0.3 | 1.8 | ||||
| 9 mo | ||||||||||
| All participants | 0.5 | 2.6 | 0.3 | 2.2 | 0.6 | 6.3 | ||||
| Men | 0.5 | 3.3 | 0.6 | 3.1 | 0.1 | 0.9 | ||||
| Women | 0.5 | 1.8 | 0.1 | 0.7 | 1.1 | 8.7 | ||||
| Anal sex, % condom use | ||||||||||
| Baseline | ||||||||||
| All participants | 20.6 | 34.5 | 27.3 | 39.1 | 30.2 | 40.9 | 1.21 | 0.54 | 4.59 | 0.10 |
| Men | 24.5 | 38.5 | 32.1 | 42.9 | 32.5 | 38.9 | ||||
| Women | 14.4 | 26.8 | 20.1 | 32.4 | 27.4 | 43.9 | ||||
| 3 mo | ||||||||||
| All participants | 42.3 | 44.6 | 46.0 | 44.7 | 36.8 | 44.1 | ||||
| Men | 51.3 | 45.7 | 52.5 | 43.2 | 39.0 | 42.9 | ||||
| Women | 30.2 | 40.3 | 34.8 | 45.4 | 33.9 | 46.0 | ||||
| 6 mo | ||||||||||
| All participants | 40.5 | 42.2 | 49.6 | 44.4 | 48.5 | 45.5 | ||||
| Men | 43.5 | 42.7 | 54.3 | 43.7 | 53.2 | 44.7 | ||||
| Women | 36.9 | 41.8 | 43.1 | 44.9 | 41.7 | 46.3 | ||||
| 9 mo | ||||||||||
| All participants | 44.0 | 44.2 | 56.2 | 43.8 | 51.9 | 46.7 | ||||
| Men | 41.7 | 42.4 | 57.4 | 42.6 | 54.9 | 45.9 | ||||
| Women | 46.9 | 46.6 | 54.5 | 45.7 | 48.8 | 47.6 | ||||
Figure 2.
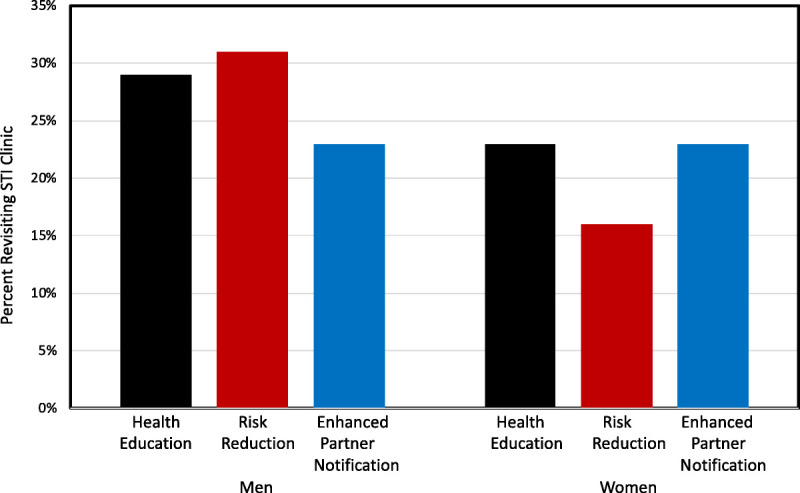
Percentages of male and female participants who returned for an STI clinic visit within 12 months after receiving the 3 counseling conditions.
Primary Sexual Behavior Outcomes
Results of the GEE models for vaginal intercourse occasions controlling for baseline indicated that there were no differences between counseling conditions and the counseling × gender interaction was not significant (Table 2). There was a significant effect of assessment time (Wald χ2 = 29.23, P = 0.01); rates of vaginal intercourse increased over time. For condom use during vaginal intercourse, results showed a significant main effect of counseling condition (Wald χ2 = 10.16, P = 0.01); participants receiving risk reduction counseling reported greater condom use across genders and assessment periods (Fig. 3). There were no other significant main effects or interactions for condom use during vaginal intercourse. With respect to anal intercourse, rates of behavior were generally low and the only significant effect was the counseling condition × gender × assessment time interaction (Wald χ2 = 10.54, P = 0.03); women receiving enhanced partner notification counseling indicated higher rates of anal intercourse at the 9-month follow-up than men and women in the other conditions. Finally, for condom use during anal intercourse, the main effect for gender was significant (Wald χ2 = 7.42, P = 0.01); men reported greater condom use during anal intercourse than did women. There were no other significant main effects or interactions.
Figure 3.
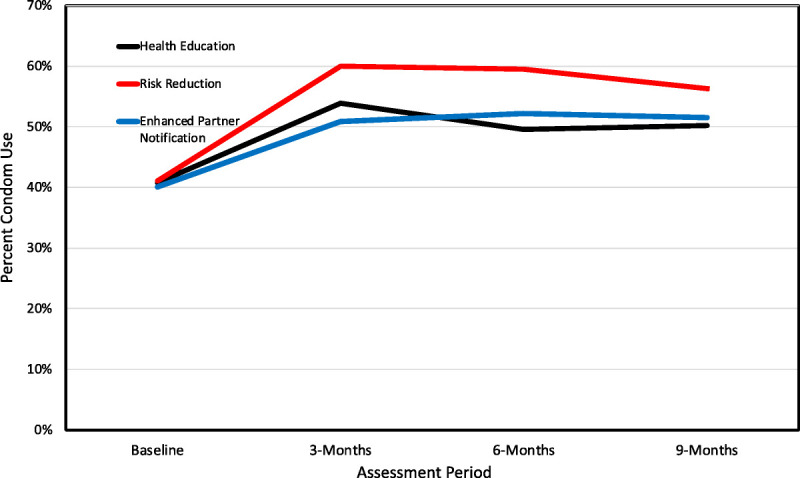
Mean use of condoms during vaginal intercourse during assessment periods for participants receiving the 3 counseling conditions.
Secondary Outcomes
Results of the GEE models for the STI knowledge controlling for baseline showed that there was a significant effect of assessment time (Wald χ2 = 12.03, P = 0.01); knowledge scores increased over assessments, with the highest scores at the 9-month follow-up. Results also showed that HIV stigma scores decreased significantly over time (Wald χ2 = 32.87, P = 0.01), and there was a significant gender × assessment time interaction (Wald χ2 = 10.24, P = 0.01); stigma scores for women decreased significantly more so than did stigma scores for men. There were no other main effects or interactions for HIV stigma. Finally, analyses showed that there were no significant effects for prevention skills self-efficacy (Table 3).
TABLE 3.
STI Knowledge, HIV Stigma, and Prevention Self-Efficacy Outcomes for the 3 Intervention Conditions
| Health Education | Risk Reduction | Enhanced Partner Notification | Condition | Condition × Gender | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Wald χ2 | P | Wald χ2 | P | |
| STI knowledge | ||||||||||
| Baseline | ||||||||||
| All participants | 2.8 | 1.0 | 2.8 | 0.9 | 2.6 | 0.9 | 4.59 | 0.10 | 4.37 | 0.11 |
| Men | 2.8 | 1.0 | 2.9 | 0.9 | 2.6 | 0.9 | ||||
| Women | 2.7 | 1.0 | 2.8 | 1.0 | 2.7 | 0.9 | ||||
| 3 mo | ||||||||||
| All participants | 3.0 | 0.9 | 3.1 | 0.9 | 3.1 | 0.9 | ||||
| Men | 3.1 | 0.9 | 3.0 | 0.9 | 3.0 | 0.8 | ||||
| Women | 2.9 | 0.8 | 3.2 | 0.8 | 3.1 | 0.9 | ||||
| 6 mo | ||||||||||
| All participants | 3.1 | 0.9 | 3.1 | 0.8 | 3.2 | 0.8 | ||||
| Men | 3.2 | 0.8 | 3.1 | 0.9 | 3.1 | 0.7 | ||||
| Women | 3.1 | 0.9 | 3.2 | 0.8 | 3.3 | 0.8 | ||||
| 9 mo | ||||||||||
| All participants | 3.1 | 0.8 | 3.2 | 0.8 | 3.2 | 0.8 | ||||
| Men | 3.1 | 0.9 | 3.2 | 0.8 | 3.1 | 0.9 | ||||
| Women | 3.1 | 0.8 | 3.1 | 0.8 | 3.2 | 0.8 | ||||
| HIV stigma | ||||||||||
| Baseline | ||||||||||
| All participants | 2.3 | 0.5 | 2.3 | 0.4 | 2.3 | 0.4 | 4.48 | 0.10 | 0.77 | 0.68 |
| Men | 2.3 | 0.4 | 2.3 | 0.5 | 2.3 | 0.04 | ||||
| Women | 2.3 | 0.04 | 2.3 | 0.4 | 2.3 | 0.4 | ||||
| 3 mo | ||||||||||
| All participants | 1.2 | 0.4 | 1.1 | 0.3 | 1.2 | 0.4 | ||||
| Men | 1.2 | 0.4 | 1.1 | 0.4 | 1.2 | 0.4 | ||||
| Women | 1.2 | 0.4 | 1.1 | 0.3 | 1.2 | 0.3 | ||||
| 6 mo | ||||||||||
| All participants | 1.2 | 0.3 | 1.1 | 0.3 | 1.1 | 0.3 | ||||
| Men | 1.1 | 0.3 | 1.1 | 0.4 | 1.1 | 0.3 | ||||
| Women | 1.2 | 0.4 | 1.1 | 0.3 | 1.1 | 0.2 | ||||
| 9 mo | ||||||||||
| All participants | 1.1 | 0.3 | 1.1 | 0.3 | 1.1 | 0.3 | ||||
| Men | 1.2 | 0.3 | 1.1 | 0.4 | 1.1 | 0.4 | ||||
| Women | 1.1 | 0.3 | 1.1 | 0.2 | 1.1 | 0.2 | ||||
| Prevention self-efficacy | ||||||||||
| Baseline | ||||||||||
| All participants | 8.1 | 1.6 | 8.0 | 1.7 | 7.9 | 1.7 | 5.17 | 0.07 | 0.12 | 0.94 |
| Men | 8.2 | 1.5 | 8.0 | 1.6 | 7.9 | 1.8 | ||||
| Women | 7.9 | 1.7 | 8.1 | 1.9 | 8.0 | 1.7 | ||||
| 3 mo | ||||||||||
| All participants | 8.1 | 1.7 | 8.3 | 1.6 | 8.4 | 1.5 | ||||
| Men | 8.1 | 1.7 | 8.2 | 1.6 | 8.4 | 1.5 | ||||
| Women | 8.1 | 1.8 | 8.3 | 1.7 | 8.5 | 1.5 | ||||
| 6 mo | ||||||||||
| All participants | 8.2 | 1.6 | 8.3 | 1.6 | 8.4 | 1.6 | ||||
| Men | 8.1 | 1.7 | 8.3 | 1.5 | 8.4 | 1.6 | ||||
| Women | 8.3 | 1.5 | 8.3 | 1.6 | 8.3 | 1.7 | ||||
| 9 mo | ||||||||||
| All participants | 8.1 | 1.8 | 8.4 | 1.6 | 8.4 | 1.7 | ||||
| Men | 8.2 | 1.7 | 8.6 | 1.4 | 8.5 | 1.6 | ||||
| Women | 8.2 | 1.7 | 8.5 | 1.5 | 8.4 | 1.7 | ||||
DISCUSSION
Extending previously reported results that demonstrated the single-session enhanced partner notification intervention included in this trial increased informing recent sex partners of their STI,9 our first hypothesis in the current report was confirmed; the single-session risk reduction counseling intervention resulted in greater use of condoms than did the other 2 conditions. The increase in condom use occurred within a context of increased occurrences of vaginal intercourse and relatively low rates of anal intercourse. The change in condom use represents a nearly 50% increase over baseline at the 3- and 6-month follow-ups. Our second hypothesis, however, was not fully confirmed in that we did not see significant impacts on STI for the risk reduction and enhanced partner notification counseling conditions. Women receiving the risk reduction counseling were significantly less likely to return to an STI clinic during the follow-up. The difference between the continuous and dichotomous STI outcomes is due to multiple STI visits among a small number of participants, therefore driving-up the annual rates of visits at the event level. Finally, our third hypothesis that all 3 counseling conditions would increase STI prevention knowledge and reduce HIV stigma beliefs was also confirmed, suggesting that increasing STI knowledge may have a direct benefit of reducing HIV stigma beliefs. However, we did not find that the risk reduction and enhanced partner notification interventions significantly increased self-efficacy for practicing STI preventive behaviors.
Overall, we conclude that enhanced partner notification counseling may have an impact on the prevalence of STI beyond the individual by reducing community disease burden, but we did not observe impacts on index patients. In contrast, risk reduction counseling may reduce individual-level risks for reexposure to an STI, particularly among women. Our trial design was intended to test divergent outcomes of partner notification and condom use to achieve the same end, namely, reductions in subsequent STI. Our findings, however, suggest that neither approach alone may be sufficient to achieve durable reductions in STI. A combined approach that aims to both reduce the prevalence of STI at the community-level through enhanced partner notification and reduce individual-level risks for STI through condom use and other sexual behavior changes may prove more effective and should be investigated in future research.
Our trial had important limitations that should be considered when interpreting the results. The study was conducted in a single STI clinic, suggesting that caution in generalizing the results is warranted. The clinical context of this study relied on syndromic management of STI, a broad stroke approach that lacks specificity. Our STI data were the product of this system and are therefore limited by this unspecified approach. In addition, our measures relied heavily on self-report instruments of sexual behavior and may therefore be subject to underreporting of sexual practices and overreporting of condom use. It should also be noted that our measure of self-efficacy seems to have had ceiling effects that further limited our ability to detect change in this variable. Furthermore, we only included electronic health records from the City of Cape Town Health Department and not those of the Provincial Health Department. We may therefore have missed STI events occurring outside the city health system. In addition, the STI rates among women are likely suppressed given that women are less likely to present with STI symptoms than men. Finally, it should be noted that this trial did not include a condition that combined partner notification with risk reduction behavioral skills counseling, as would have been included in a full-factorial design. With these limitations in mind, we believe that our trial findings have implications for future research.
The next generation of STI prevention counseling interventions may achieve greater success by both reducing community disease burden through enhanced partner notification and reducing individual risks by increasing condom use. From the perspective of the current study, the enhanced partner notification components could be integrated into risk reduction counseling with minimal added time. Risk reduction counseling already encompasses sexual communication skills building around sexual risk negotiation and discussing condom use. The same communication skills building activities can be broadened and applied to strategies for partner notification as they were in the enhanced partner notification condition. Interventions that aim to both increase partner notification and increase condom use may synergize to reduce risks and should be tested in future research.
Footnotes
This work was supported by the National Institutes of Health/National Institute of Child Health and Development (R01HD074560).
Conflict of Interest and Sources of Funding: None declared.
Contributor Information
Ellen Banas, Email: ellen.banas@perceptionprograms.org.
Moira Kalichman, Email: moira.kalichman@perceptionprograms.org.
Sarah Dewing, Email: sarahdewing@gmail.com.
Karen Jennings, Email: Karen.Jennings@capetown.gov.za.
Johann Daniels, Email: johann.daniels10@gmail.com.
Marcel Berteler, Email: marcel.berteler@capetown.gov.za.
Catherine Mathews, Email: catherine.mathews@mrc.ac.za.
REFERENCES
- 1.Eaton LA Huedo-Medina TB Kalichman SC, et al. Meta-analysis of single-session behavioral interventions to prevent sexually transmitted infections: Implications for bundling prevention packages. Am J Public Health 2012; 102:e34–e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull 1992; 111:455–474. [DOI] [PubMed] [Google Scholar]
- 3.Fisher JD, Fisher WA. Theoretical approaches to individual-level change. In: Peterson J, DiClemente R, eds. HIV Prevention Handbook. New York: Kluwer Academic/Plenum Press, 2000:3–55. [Google Scholar]
- 4.Simbayi LC Kalichman SC Skinner D, et al. Theory-based HIV risk reduction counseling for sexually transmitted infection clinic patients in Cape Town, South Africa. Sex Transm Dis 2004; 31:727–733. [DOI] [PubMed] [Google Scholar]
- 5.Kalichman SC Cain D Eaton L, et al. Randomized clinical trial of brief risk reduction counseling for sexually transmitted infection clinic patients in Cape Town, South Africa. Am J Public Health 2011; 101:e9–e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pitpitan EV Kalichman SC Garcia RL, et al. Mediators of behavior change resulting from a sexual risk reduction intervention for STI patients, Cape Town, South Africa. J Behav Med 2015; 38:194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kalichman SC Cain D Weinhardt L, et al. Experimental components analysis of brief theory-based HIV/AIDS risk-reduction counseling for sexually transmitted infection patients. Health Psychol 2005; 24:198–208. [DOI] [PubMed] [Google Scholar]
- 8.Weinhardt LS, Mosack KE, Swain GR. Development of a computer-based risk-reduction counseling intervention: Acceptability and preferences among low-income patients at an urban sexually transmitted infection clinic. AIDS Behav 2007; 11:549–556. [DOI] [PubMed] [Google Scholar]
- 9.Mathews C Lombard C Kalichman M, et al. Effects of enhanced STI partner notification counselling and provider-assisted partner services on partner referral and the incidence of STI diagnosis in Cape Town, South Africa: Randomised controlled trial. Sex Transm Infect 2020; sextrans-2020-054499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalichman SC Simbayi LC Vermaak R, et al. HIV/AIDS risk reduction counseling for alcohol using sexually transmitted infections clinic patients in Cape Town, South Africa. J Acquir Immune Defic Syndr 2007; 44:594–600. [DOI] [PubMed] [Google Scholar]
- 11.Maisto SA Conigliaro J McNeil M, et al. An empirical investigation of the factor structure of the AUDIT. Psychol Assess 2000; 12:346–353. [DOI] [PubMed] [Google Scholar]
- 12.Allen JP Litten RZ Fertig JB, et al. A review of the research on the Alcohol Use Disorders Identification Test (AUDIT). Alcohol Clin Exp Res 1997; 21:613–619. [PubMed] [Google Scholar]
- 13.Finitsis DJ Pellowski JA Huedo-Medina TB, et al. Visual analogue scale (VAS) measurement of antiretroviral adherence in people living with HIV (PLWH): A meta-analysis. J Behav Med 2016; 39:1043–1055. [DOI] [PubMed] [Google Scholar]
- 14.Carey MP, Schroder KE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Educ Prev 2002; 14:172–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalichman SC Simbayi LC Jooste S, et al. Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behav 2005; 9:135–143. [DOI] [PubMed] [Google Scholar]
- 16.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev 1977; 84:191–215. [DOI] [PubMed] [Google Scholar]
- 17.Bandura A. Self-efficacy: the Exercise of Control. New York: W.H. Freeman, 1997. ix, 604 p. [Google Scholar]
- 18.Jurs S, Glass G. The effect of experimental mortality on the internal and external validity of the randomized comparative experiment. J Exp Educ 1971; 40:62–66. [Google Scholar]


