Abstract
Background:
To explore the accuracy and security of 3-dimensional (3D) printing technology combined with guide plates in the preoperative planning of thoracic tuberculosis and the auxiliary placement of pedicle screws during the operation.
Methods:
Retrospective analysis was performed on the data of 60 cases of thoracic tuberculosis patients treated with 1-stage posterior debridement, bone graft fusion, and pedicle screw internal fixation in the Department of Orthopedics, Zhejiang Chinese Medicine and Western Medicine Integrated Hospital from March 2017 to February 2019. There were 31 males and 29 females; age: 41 to 52 years old, with an average of (46.6 ± 2.0) years old. According to whether 3D printing personalized external guide plates are used or not, they are divided into 2 groups: 30 cases in 3D printing group (observation group), and 30 cases in pedicle screw placement group (control group). A 1:1 solid model of thoracic spinal tuberculosis and personalized pedicle guide plates was created using the 3D printing technology combined with guide plates in the observation group. Stability and accuracy tests were carried out in vitro and in vivo. 30 patients in the control group used conventional nail placement with bare hands. The amount of blood loss, the number of fluoroscopy, the operation time, and the occurrence of adverse reactions related to nail placement were recorded. After the operation, the patients were scanned by computed tomography to observe the screw position and grade the screw position to evaluate the accuracy of the navigation template. All patients were followed up for more than 1 year. Visual Analogue Scale scores, erythrocyte sedimentation rate, and C-reactive protein were evaluated before surgery, 6 months after surgery, and 12 months after surgery.
Results:
Sixty patients were followed up for 6 to 12 months after surgery. One hundred seventy-five and 177 screws were placed in the 3D printing group and the free-hand placement group, respectively. The rate of screw penetration was only 1.14% in the 3D-printed group (all 3 screws were grade 1) and 6.78% in the free-hand nail placement group (12 screws, 9 screws were grade 1 and 3 screws were grade 2). The difference was statistically significant (P = .047). The operation time of the 3D printing group ([137.67 ± 9.39] minutes), the cumulative number of intraoperative fluoroscopy ([4.67 ± 1.03] times), and the amount of intraoperative blood loss ([599.33 ± 83.37] mL) were significantly less than those in the manual nail placement group ([170.00 ± 20.48] minutes, [9.38 ± 1.76] times, [674.6 ± 83.61] mL). The differences were statistically significant (P < .05). There was no significant difference in VAS score and Oswestry disability index score between the 2 groups of patients before operation, 3 and 6 months after operation (P > .05).
Conclusion:
The 3D printing technology combined with guide plate is used in thoracic spinal tuberculosis surgery to effectively reduce the amount of bleeding, shorten the operation time, and increase the safety and accuracy of nail placement.
Keywords: 3D printing guide plate, accuracy, freehand technique, spinal tuberculosis, thoracic pedicle screws
1. Introduction
In recent years, the global incidence of tuberculosis has significantly increased, and the number of patients with spinal tuberculosis has also gradually increased. Spinal tuberculosis accounts for 1% to 2% of all tuberculosis infections and 75% of bone and joint tuberculosis. The disability rate of these tuberculosis infections will be higher if not treated timely.[1] The pedicle screw internal fixation system is currently recognized as a relatively reliable fixation method. However, misplacement of pedicle screws occurs from time to time, which affects the patient's postoperative treatment effect, especially because of the special anatomy of the thoracic spine, it is difficult to identify the tubercular convex deformity and normal anatomical landmarks, making screw implantation more difficult. At present, 3-dimensional (3D) printing technology has good clinical and scientific applications in bone tumor resection, pelvic fracture, joint replacement, spine surgery, and so on.[2,3] However, there are few reports about the application of 3D printing technology in preoperative planning and intraoperative guide plate nail placement for patients with thoracic tuberculosis. This study used preoperative 3D printing of the physical model of the thoracic spine tuberculosis lesion area to design an individualized pedicle guide template, and applied it in the in vitro model and actual surgery to explore the accuracy, safety, and stability of its auxiliary placement of pedicle screws.
2. Materials and methods
2.1. Inclusion and exclusion criteria
2.1.1. Inclusion criteria
-
(1)
Thoracic spinal tuberculosis was diagnosed based on the following factors: (1) clinical manifestations: history of chest and back pain with or without spinal cord compression symptoms; (2) imaging findings (X-rays, computed tomography [CT], and magnetic resonance imaging): obvious destruction of the thoracic spine, but the scope of vertebral destruction was limited to 2 adjacent vertebrae; without attachment destruction (Fig. 1); and (3) the pathological examination of preoperative puncture specimens accorded with pathological changes of spinal tuberculosis: tuberculous granulomatosis; the genetic test of the puncture specimen was positive for X-pert
-
(2)
Age between 40 and 65 years
-
(3)
Regular antituberculosis preoperative treatment for >3 weeks without obvious tuberculosis manifestations with body temperature of <37.5°C
-
(4)
Patients and family members who provided signed informed consents
-
(5)
Ethics Committee of Zhejiang Chinese Medicine and Western Medicine Integrated Hospital/Hangzhou Red Cross Hospital approved the study.
Figure 1.
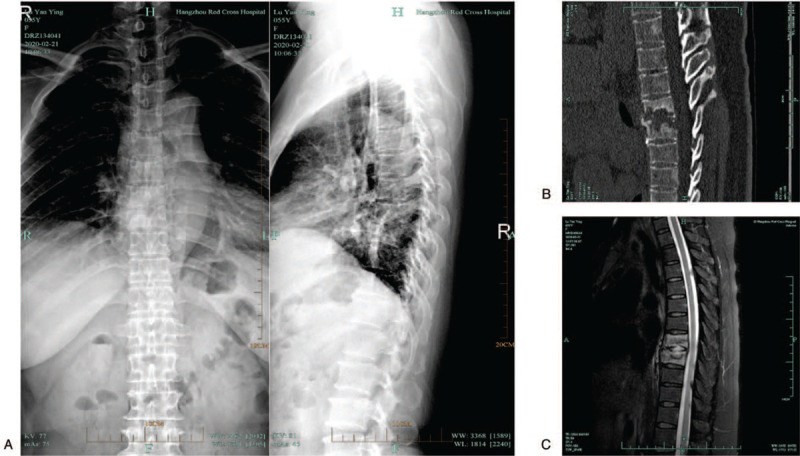
Preoperative imaging data of patients with thoracic spine tuberculosis. (A) X-ray lateral view of the thoracolumbar spine, showing high density of T7 and T8 vertebral bodies, bone destruction, and narrowed intervertebral space. (B) It is a sagittal CT scan of the thoracic spine, showing the destruction of T7 and T8 vertebral bodies and the formation of cavities. (C) Sagittal radiographs of thoracic spine MRI fat-reducing images, showing high signal shadows of T7 and T8 vertebral bodies, and destruction of intervertebral discs. CT = computed tomography, MRI = magnetic resonance imaging.
2.1.2. Exclusion criteria
-
(1)
history of other rheumatic disorders, spinal tumors, or severe abnormalities in the liver and kidney function;
-
(2)
history of active tuberculosis;
-
(3)
lack of autonomy or inability to participate in the 12-month follow-up;
-
(4)
resistance to tuberculosis medications; and
-
(5)
mental illness and inability to perform effective doctor–patient communication.
2.2. Subjects
According to the above-mentioned case selection criteria, 60 cases of thoracic tuberculosis patients with clear surgical indications from March 2017 to February 2019 were selected. According to whether 3D printing personalized external guide plates are used or not, they are divided into 2 groups: 3D printing group (observation group) 30 cases, 16 males and 14 females; age 42 to 51 years old. Involved segments: 1 case at T1–2 segment, 1 case at T2–3 segment, 1 case at T3–4 segment, 3 cases at T4–5 segment, 3 cases at T5–6 segment, 5 cases at T6–7 segment, 6 cases in T7–8 segment, 2 cases in T8–9 segment, 2 cases in T9–10 segment, 3 cases in T10–11 segment, and 3 cases in T11–12 segment. There were 30 cases in the freehand nail placement group (control group), including 15 males and 15 females, aged 41 to 52 years old. Segment distribution of all patients: 1 case at T1–2, T2–3, and T3–4, 2 cases at T4–5 and T5–6, 6 cases at T6–7, 7 cases at T7–8, 2 cases at T8–9, 1 case at T9–10, 4 cases at T10–11, and 3 cases at T11-12.
2.3. Preparation of 3D-printed models and guide plates
2.3.1. Production of 3D models
A dual-source spiral CT was used to scan the spinal tuberculosis lesion area in the observation group to obtain tomographic images of lesion segments that were saved in DICOM format and input to the computer. The MIMCS software was used to generate 3D images. A fully fitted and interactive screen display design method was used to locate and sort defects around the Computer Aided Design 3D model through image segmentation and registration to extract the area of interest. The surface is drawn without data loss to obtain a triangular mesh image. The 3D model is generated after filling. After “slicing” the STL file, the information is processed using the program to control the 3D printing equipment in turn, and the diseased vertebra is copied layer by layer. Reconstruction results are outputted in STL format, and the 3D model data of the vertebral body is inputted to a 3D printer through a digital interface.
2.3.2. Preparation of surgical guides
Virtual nail channels and support columns were designed by segmenting the peelable bone surface, using the “MedCAD” function in the medical imaging software Mimics, creating a new “Cylinder” and adjusting its properties, and rotating or expanding the nail channel at any angle. The diameter of the rod was measured to determine if it penetrated the bone around the nail channel, and it was repeatedly adjusted to a predetermined ideal position. The measurement distance in Measurements can be used to determine the distance from the nail entry point to the ideal depth and nail axis and obtain screw data with appropriate length and diameter. Then, the positioning plane of the navigation module was cut through simulation/cut orthogonal to the screen (that is, the bone surface that can be peeled off during actual surgery), including the medial edge of the transverse process, the lamina, and the lateral edge of the spinous process. A solid body block is established on the surface as a navigation module. The base plate, the ventral side of the solid body, and the anatomical shape of the local bone surface are placed in an inverted structure, which are completely complementary, and can be well fixed. A navigation module with a nail track is designed, constituting a combination of a nail track bar, a support column, and a solid body constitute with a nail track, and a Boolean subtraction operation was performed to obtain the prototype of the navigation module, irrelevant parts were cut, module corners were trimmed, and the shaped navigation module with nail track was obtained.
2.3.3. 3D printing navigation module entity
The navigation module model in STL format was exported to the software MakerWare supporting the 3D printer for batch printing. After adjusting the printing properties, a polylactic acid was used to print out the navigation module entity and clear the nail path.
2.3.4. Designing a surgical plan and simulating surgery
Combined with computer virtual analysis, virtual nail placement in the 3D-printed model was performed to measure the diameter and length of the pedicle screw, the direction of the nail insertion, and the distance between the nail insertion point and posterior midline. Especially in the virtual placement of diseased vertebrae, the extent of lesion removal and the size of the bone graft bed should be determined. CT lesion scans of areas with lesions are used to obtain cross-section images of the lesion segment. Triangulated grid images are obtained by surface drawing without data loss, and the specific 3D size of the bone defect was analyzed and calculated. The bone defect area of the lesion and important tissues such as the spinal cord and blood vessels during nail placement should be avoided to achieve a satisfactory nail placement trajectory. Then, a 3D print was used to create a solid spine model and guide plate, and the guide plate was used to preset nails on the 1:1 solid spine model to intuitively identify the trajectory and length of the nail (Fig. 2).
Figure 2.
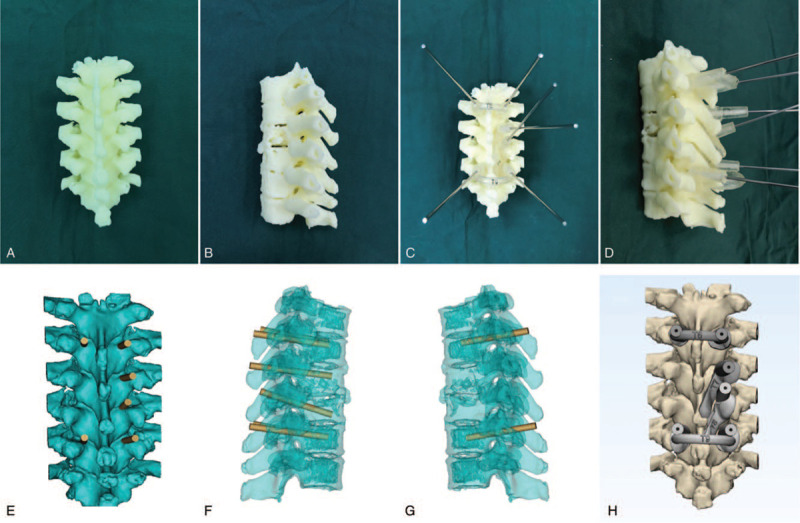
Schematic diagram of the 3D printed model and surgical guide plate of patients with thoracic spine tuberculosis. (A, B) They are the front view and side view solid images of 3D printed diseased vertebral models accurately digitized according to medical imaging software. (C, D) Front and side views of the 3D navigation module implanted with nail channels. (E, F, G) It is the virtual front view, left side view, and right side view of the computer software simulating the 3D printing guide computer. (H) The computer accurately simulates the front view of the vertebral pedicle implanted after the diseased vertebral body. 3D = 3-dimensional.
2.4. Surgical methods
Sixty patients underwent the procedure by the same group of surgeons. Patients were placed in a prone position according to their spine arc, while the abdomen was suspended to reduce bleeding intraoperatively. A curved incision was made around the diseased vertebral body, the skin was pulled and the deep fascia was cut, and the erector spinae was stripped along the spinous process to expose the lamina and articular processes. In the observation group, after exposing the vertebral body, the navigation module entity was tightly locked with the bone surface around the lamina in the operative field. The finger was pressed to fix the module, and the Kirschner wire was slowly pierced through the navigation module channel into the bone behind the pedicle. After electric drilling to obtain the expected length, the navigation template and Kirschner wire were removed consecutively, the guide wire was inserted, and the hole with a tap was reamed and the screws with the measured length and diameter were inserted in the direction of the nail channel (Fig. 3). The lesions were resected according to the pre-assessed size, and bone grafts were completed, the connecting rod was installed. The control group was referred to the residual joint space of the transverse and upper and lower articular processes. The thoracic vertebrae were inserted using the Roy–Camille method. Three or 4 vertebrae were fixed to the diseased vertebra and the upper and lower vertebrae. C-arm X-ray machine fluoroscopy confirms that the position of the pedicle screw is good, and the nail tail was installed using a connection system to tighten its nuts after stretching the diseased vertebra. After completing the fixation, the C-arm X-ray machine was used for fluoroscopy again to confirm that the screw position was reset well, and the cross-link was installed. Postoperatively, the incision was flushed with conventional lesion removal with the bone graft fusion, drainage tubes were placed, and then the incision was closed. A 12-lead nerve electrophysiological monitoring was used during the intraoperative routine application. The pedicle screw rod system produced by the Shanghai Sanyou Medical Co., Ltd was used for internal fixation.
Figure 3.
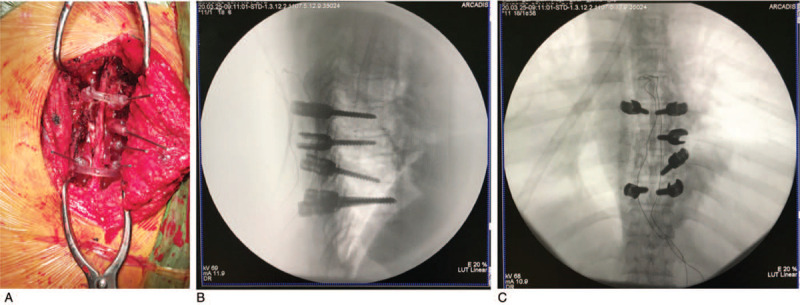
Thoracic vertebral tuberculosis patients with guide plate assisted nail placement and intraoperative nail placement perspective view. (A) It is a visual observation that the entity of the navigation module used in the operation is tightly locked with the bone surface around the lamina in the operation field. (B, C) It is the lateral and orthotopic thoracic spine of the pedicle screw accurately implanted through the navigation module channel.
2.5. Postoperative treatment
After the operation, continue the original anti-tuberculosis program, add enough fluid and nutrition, and perform regular postoperative tests to observe the electrolyte balance. Patients with hypoproteinemia should be injected with albumin immediately, and the drainage tube should be removed when the negative pressure drainage flow <30 mL/d in the postoperative incision. After 6 weeks in bed, wear a brace to protect the movement out of bed.
2.6. Postoperative follow-up and functional evaluation
Effectiveness and safety evaluation: record the patient's operation time, intraoperative blood loss, and the number of intraoperative fluoroscopy. Postoperative spinal X-rays and thin-slice CT + 3D reconstruction were reviewed in both groups. According to the CT evaluation of the screw and pedicle, the accuracy of the nail placement was evaluated according to methods proposed by Kawaguchi et al[2] and Lu et al,[3] with the following evaluation standard: grade 0 screw, the pedicle screw is completely at the pedicle within; Grade 1 screw, the pedicle screw breaks through pedicle cortex at <2 mm; Grade 2 screw, the pedicle screw breaks through pedicle cortex at ≥2 mm and <4 mm; and Grade 3 screw, the screw breaks through the pedicle cortex at ≥4 mm. Grades 0 and 1 are acceptable screws, whereas grades 2 and 3 are unacceptable screws.
In the statistical data analysis, the 0-level nail placement was defined as accurate nail placement, and the nail placement accuracy was calculated to determine whether nerve, blood vessel, and spinal cord injuries occurred.
Functional evaluation: The VAS score was used to evaluate the degree of pain relief before operation, 6 months after operation and 12 months after operation. The Oswestry disability index (ODI) evaluates spinal function, which consists of 9 questions including pain level, lifting, self-care ability in daily activities, lifting, walking, sitting, standing, sleeping, travel, and social activities. There are 6 options for the question, with a score of 0–5 points, 0 points means no dysfunction, 5 points means the most severe dysfunction, add the 9 option selection points and calculate the percentage of the highest score (45 points). Calculation method: actual score/45 × 100% = ODI, the closer the ODI is to 100%, the more severe the dysfunction.
2.7. Statistical methods
Statistical analysis was performed using SPSS 19.0 (IBM Corporation) software, and for the measurement data, Kolmogorov–Smirnov was used to test whether it conforms to the normal distribution. For measurement data conforming to a normal distribution are expressed as (x ± s), and the count data was tested by χ2. The operation time, intraoperative blood loss, and number of perspectives were measured. The t-test was used to compare differences between the 2 groups. For count data, χ2 test was used. P < .05 was considered statistically significant.
3. Results
3.1. Basic information comparison
Patients in the 3D printing group and the manual nail placement group completed the operation successfully. There were no complications such as neurovascular injury during the operation. Postoperative pathological examination confirmed tuberculosis, and Xpert examination was positive and no drug-resistant cases. All patients were followed up for 6 to 12 months. There were no complications such as mixed infection, deep vein thrombosis of lower extremities, recurrence of tuberculosis, loosening of pedicle screws, and unsubscription. The preoperative gender, age, and follow-up time of the 2 groups of patients were not statistically different (P > .05), and they were comparable. See Table 1.
Table 1.
Comparison of basic conditions of the 2 groups of patients.
| Groups | Gender (male/female, n) | Age (x ± s, yr) | Follow-up time (mo) |
| Observation group | 16/14 | 46.40 ± 2.67 | 12 |
| Control group | 15/15 | 46.17 ± 2.34 | 12 |
| χ2/t value | 0.067 | 0.360 | |
| P-value | .796 | .720 |
3.2. Comparison of the operation time, intraoperative blood loss, and the number of intraoperative fluoroscopy between the 2 groups
The operation time of the 3D printing group was (137.67 ± 9.39) minutes, which was significantly shorter than the (170.00 ± 20.48) minutes of the manual nail placement group, and the difference was statistically significant (t = –7.706, P < .001); intraoperative blood loss was (599.33 ± 83.37) mL, which is significantly less than (674.6 ± 83.61) mL of patients in the manual nail placement group, the difference is statistically significant (t = –3.292, P < .001); the number of intraoperative fluoroscopy is (4.67 ± 1.03) times, Significantly less than (9.38 ± 1.96) times in the free-hand nail placement group, the difference was statistically significant (t = –12.258, P < .001). See Table 2.
Table 2.
Comparison of intraoperative blood loss, operation time, number of fluoroscopy, and number of nails in the 2 groups.
| Groups | Intraoperative blood loss (mL) | Operation time (min) | Number of perspectives (times) | Number of nails (n) | Nail placement accuracy (%) |
| Observation group | 599.33 ± 83.37 | 137.67 ± 9.39 | 4.67 ± 1.03 | 175 | 98.86 |
| Control group | 674.6 ± 83.61 | 170.00 ± 20.48 | 9.38 ± 1.76 | 177 | 93.22 |
| χ2/t value | −3.292 | −7.706 | −12.258 | 6.134 | |
| P-value | .002 | .000 | .000 | .047 |
3.3. Comparison of the safety and functional assessment results of the 2 groups
A total of 175 screws were placed in 30 patients in the 3D printing group, of which 172 were in level 0, 3 were in level 1, 0 were in level 2, and 0 were in level 3. There are 177 nails in the freehand nailing group, including 165 at level 0, 9 at level 1, 3 at level 2, and 0 at level 3. The screw penetration rate of the 3D printing group is only 1.14% (all of the 3 are level 1). The screw penetration rate in the nail placement group was 6.78% (a total of 12 screws, 9 of which were grade 1 and 3 were grade 2), the difference was statistically significant (P = .047). See Table 3. There was a statistically significant difference in the VAS scores between the 2 groups of patients at 3 and 6 months after surgery and the preoperative VAS score (P < .05), but there was no statistically significant difference between the 2 groups (P > .05). The difference in ODI scores between the 2 groups at 3 and 6 months after surgery was statistically significant (P < .05), but there was no significant difference between the 2 groups (P > .05). See Table 4.
Table 3.
Comparison of VAS scores between 2 groups of patients.
| VAS score | |||
| Groups | Preoperative | 6 mo after operation | 12 mo after operation |
| Observation group | 7.00 ± 1.23 | 2.27 ± 1.04 | 1.53 ± 0.73 |
| Control group | 7.27 ± 1.26 | 2.80 ± 0.92 | 2.03 ± 0.81 |
| χ2/t value | −0.830 | −2.090 | −2.513 |
| P-value | .410 | .041 | .015 |
Table 4.
Comparison of VAS and ODI scores between the 2 groups before and after surgery.
| VAS scores | ODI scores | |||||
| Groups | Preoperative | 3 mo after surgery | 6 mo after surgery | Preoperative | 3 mo after surgery | 6 mo after surgery |
| Observation group | 7.00 ± 1.23 | 2.27 ± 1.04 | 1.60 ± 0.72 | 82.06 ± 7.43 | 21.36 ± 6.50 | 10.67 ± 4.68 |
| Control group | 7.27 ± 1.26 | 2.67 ± 0.76 | 1.87 ± 0.63 | 83.70 ± 7.54 | 23.50 ± 6.52 | 13.07 ± 5.39 |
| t-value | −0.830 | −1.694 | −1.523 | −0.845 | −1.270 | −1.841 |
| P-value | .410 | .096 | .133 | .401 | .209 | .071 |
ODI = Oswestry disability index.
4. Discussion
Patients with thoracic spinal tuberculosis usually need to undergo surgical treatment based on the results of systemic antituberculosis treatment. Due to the particularity and complexity of the local anatomical structure of the thoracic spine, combined with anatomical variations caused by tuberculous bone destruction, vertebral arch screws were sometimes misplaced intraoperatively. According to published reports, the use of X-ray fluoroscopy and traditional anatomical landmarks when placing pedicle screws in the thoracic spine intraoperatively has resulted in an unacceptable rate of 10% to 41%.[4,5] Therefore, for each thoracic vertebral body, the nailing point and angle should be individually designed, especially for the nail placement of tuberculosis vertebrae.[6] The traditional posterior approach of thoracic spine exposure cannot observe all the pedicles under direct vision. The nail placement technique relies on the identification of intraoperative anatomical landmarks. The angle and direction of the nail placement depends entirely on the experience and feel of the surgeon, even with experienced surgeons. Even experienced surgeons may also have poor screw placement. In addition, the position of the guide needle under C-type X-ray machine fluoroscopy is often difficult to achieve satisfactory at 1 time, and repeated fluoroscopy adjustment is required, which not only increases the operation time consumed by adjusting the C-arm X-ray machine, but also increases the X-ray radiation to the doctor and patient. At the same time, repeatedly adjusting the position of the guide needle often hinders subsequent needle insertion, resulting in failure of nail placement. 3D printing combined with navigation template technology is designed by collecting 3D anatomical information of the back of the patient's spine, and its guide plate can fully adhere to the patient's spinal bone structure.[7] Especially in the case of pedicle structure variation and vertebral tuberculosis, technical advantages of the navigation template can be better reflected, because the nail insertion point and angle are designed through the guide channel preoperatively, and the navigation template can match the individual anatomy of the patient and complete the auxiliary nail placement.[8] Preoperatively, CT scans of thoracic spinal tuberculosis and adjacent segment vertebrae were performed and used to design an ideal nail entry channel in the computer. By printing a solid thoracic spine model of 1:1 size, the guide plate was placed on the external model and physical nails were presented. Meanwhile, the effects of nail placement on diseased vertebrae and adjacent normal segments were observed to increase the accuracy of nail placement for intraoperative applications and improve the safety of surgery.[9,10] From the clinical work perspective, the key point of thoracic pedicle screw placement lies in the choice of screw diameter and screw insertion point and angle. Preoperative application design software can measure the maximum diameter and length of the screw and design the optimal nail entry point and angle.[8,11,13]
The use of navigation templates to assist nail placement perspective can significantly improve the accuracy of nail placement and to adjust the angle of the nail during repeated radioscopy, which reduces the radiation exposure of doctors and patients intraoperatively.[12,14] In this study, a total of 175 screws were inserted with the assistance of 3D printed guide plates. The operation time, intraoperative blood loss, and intraoperative fluoroscopy times were significantly lower than those in the manual nail placement group. The postoperative CT showed that the screw position was basically the same as the preoperative design. The screw penetration rate was lower than that of the free-hand placement group, the difference was statistically significant (P = .047). The results show that the 3D printing physical model combined with the fixation of thoracic vertebra tuberculosis for the treatment of thoracic tuberculosis could reduce the surgical injury of patients, shorten the operation time, reduce the amount of X-ray radiation of doctors and patients, and improve the accuracy and safety of thoracic vertebra tuberculosis fixation.
The guide plate is based on CT data to plan the screw path, which requires accurate path planning and accurate measurement of channel diameter, length, and angle. Since the guide plate is designed and printed before the operation, it is necessary to completely remove the periosteum, fascia, and completely expose the spinous process during the operation to complete the guide plate application. Therefore, it is difficult to completely avoid muscle traction or incomplete exposure causes deviation. In fact, according to our experience, these errors can often be ignored. Preoperative CT scanning and guide plate production increase the economic burden of patients, but the accuracy of the guide plate navigation saves doctors and patients operative time, reduces the number of fluoroscopy, and reduces the risk of surgery. We believe that the patient's benefit is relatively greater. The use of 3D printing to prepare solid models and guides also has certain limitations.[19] First, the individualized and precise 3D-printed models and guides have high requirements for image data, and hospitals need to be obtain high-resolution imaging equipment. Second, the design and production of 3D-printed models and guides take some time and are not used for emergency surgery. In addition, the design and production process of models and guides need to have corresponding software and equipment. The production process is complex and difficult to promote. Moreover, error links were inevitable in the 3D printing design and production process, such as possible errors in the 3D model reconstruction. Errors caused by the low accuracy of the printer can affect the accuracy of the model and guide plate nails.[20] Although the navigation template can improve the accuracy of nail placement, it should be used intraoperatively after the guide pin is inserted and after the nail placement is completed with a C-arm X-ray machine to further confirm the position of the guide pin and screw.[15] At the same time, this study has limitations such as the small number of cases, lack of large sample cases, and short follow-up time, which requires further prospective randomized controlled studies. In the future, further statistical analysis of spinal tuberculosis surgery time and bleeding volume at the same site and segment should be performed. Further analysis and comparison of the correlation between the simulation and actual nail placement are essential to confirm the advantages of this study and its clinical significance.[16–18]
In summary, 3D printing technology combined with guide plate is a safe, effective, and accurate auxiliary placement of pedicle screw devices. It can overcome the disadvantages of expensive navigation equipment, many times of free-hand fluoroscopy, time-consuming and repeated adjustments, and provides a new idea for the treatment of thoracic tuberculosis.
Author contributions
Conceptualization: Yifan Wang, Qi Zheng.
Data curation: Yifan Wang.
Formal analysis: Yifan Wang.
Investigation: Yanghui Jin.
Supervision: Shiyuan Shi.
Validation: Yanghui Jin, Yingjie Dai.
Visualization: Yingjie Dai.
Writing – original draft: Yifan Wang, Qi Zheng.
Writing – review & editing: Shiyuan Shi.
Glossary
Abbreviations: 3D = 3-dimensional, ODI = Oswestry disability index.
References
- [1].Jain AK, Jain S. Instrumented stabilization in spinaltuberculosis. Int Orthop 2012;36:285–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Kawaguchi Y, Nakano M, Yasuda T, et al. Develop- ment of a new technique for pedicle screw and Magerl screw in- sertion using a 3-dimensional image guide. Spine 2012;37:1983–8. [DOI] [PubMed] [Google Scholar]
- [3].Lu S, Xuy Q, Chen. GP, et al. Efficacy and accuracy of a novel rapid prototyping drill template for cervical pedicle screw placement. Comput Aided Surg 2011;16:240–8. [DOI] [PubMed] [Google Scholar]
- [4].Vaccaro AR, Rizzolo SJ, Allardyce TJ, et al. Placement of pedicle screws in the thoracic spine. Part I: morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am 1995;77:1193–9. [DOI] [PubMed] [Google Scholar]
- [5].Guzey FK, Emel E, Hakan SM, et al. Accuracy of pedicle screw placement for upper and middle thoracic pathologies without coronal plane spinal deformity using conventional methods. J Spinal Disord Tech 2006;19:436–41. [DOI] [PubMed] [Google Scholar]
- [6].Li Z, Xu D, Li F, et al. Design and application of a novel patient-specific 3D printed drill navigational guiding template in percutaneous thoracolumbar pedicle screw fixation: a cadaveric study. J Clin Neurosci 2020;73:294–8. [DOI] [PubMed] [Google Scholar]
- [7].Wang F, Li CH, Liu ZB, et al. The effectiveness and safety of 3-dimensional printed composite guide plate for atlantoaxial pedicle screw: a retrospective study. Medicine (Baltimore) 2019;98:e13769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Feng ZH, Li XB, Phan K, et al. Design of a 3D navigation template to guide the screw trajectory in spine: a step-by-step approach using Mimics and 3-Matic software. J Spine Surg 2018;4:645–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kim JW, Lee Y, Seoet J, et al. Clinical experience with three-dimensional printing techniques in orthopedic trauma. J Orthop Sci 2018;23:383–8. [DOI] [PubMed] [Google Scholar]
- [10].Yu Z, Zhang G, Chen X, et al. Application of a novel 3D drill template for cervical pedicle screw tunnel design: a cadaveric study. Eur Spine J 2017;26:2348–56. [DOI] [PubMed] [Google Scholar]
- [11].Sugawara T, Higashiyama N, Kaneyama S, et al. Accurate and simple screw insertion procedure with patient-specific screw guide templates for posterior C1-C2 fixation. Spine (Phila Pa 1976) 2017;42:E340–6. [DOI] [PubMed] [Google Scholar]
- [12].Gao F, Wang Q, Liu C, et al. Individualized 3D printed model-assisted posterior screw fixation for the treatment of craniovertebral junction abnormality: a retrospective study. J Neurosurg Spine 2017;27:29–34. [DOI] [PubMed] [Google Scholar]
- [13].Diment LE, Thompson MS, Bergmann JHM. Clinical efficacy and effectiveness of 3D printing: a systematic review. BMJ Open 2017;7:e016891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Jiang LH, Tan MS, Dong L, et al. Accuracy assessment of a 3D printed navigational guiding template for atlantoaxial pedicle screw placement. J Spine Surg 2016;14:205–10. [Google Scholar]
- [15].Dea N, Fisher CG, Batke J, et al. Economic evaluation comparing intraoperative cone beam CT-based navigation and conventional fluoroscopy for the placement of spinal pedicle screws: a patient-level data cost-effectiveness analysis. Spine J 2016;16:23–31. [DOI] [PubMed] [Google Scholar]
- [16].Wanibuchi M, Noshiro S, Sugino T, et al. Training for skull base surgery by using a colored temporal bone model created by three dimensional printing technology. World Neurosurg 2016;91:66–72. [DOI] [PubMed] [Google Scholar]
- [17].Wu AM, Shao ZX, Wang JS, et al. The accuracy of a method for printing three-dimensional spinal models. PLoS One 2015;10:e0124291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Eltes PE, Kiss L, Bartos M, et al. Geometrical accuracy evaluation of an affordable 3D printing technology for spine physical models. J Clin Neurosci 2020;72:438–46. [DOI] [PubMed] [Google Scholar]
- [19].Liu J, He X, Gao Z, et al. Design and preliminary biomechanical analysis of a novel motion preservation device for lumbar spinal disease after vertebral corpectomy. Arch Orthop Trauma Surg 2019;139:751–60. [DOI] [PubMed] [Google Scholar]
- [20].Tong Y, Kaplan DJ, Spivak JM, et al. Three-dimensional printing in spine surgery: a review of current applications. Spine J 2020;20:833–46. [DOI] [PubMed] [Google Scholar]


