Abstract
The United States (US) is on track to achieve the 90-90-90 targets set forth by UNAIDS and the National HIV/AIDS strategy, yet significant racial disparities in HIV care outcomes remain, particularly for young Black men who have sex with men (YBMSM). Research has demonstrated that various types of violence are key aspects of syndemics that contribute to disparities in HIV risk. However, little research has looked collectively at cumulative violent experiences and how those might affect HIV treatment and care outcomes. Drawing on extant literature and theoretical underpinnings of syndemics, we provide a conceptual model that highlights how continuous traumatic violence experienced by YBMSM may affect HIV outcomes and contribute to racial disparities in HIV outcomes. The findings of this focused review suggest a need for research on how continuous exposure to various types of violence influence HIV prevention and treatment outcomes for young Black MSM.
Keywords: HIV continuum of care, syndemics, violence, Black MSM, racial disparities
Introduction
The United States (US) is on track to achieve the 90-90-90 targets set forth by UNAIDS and the National HIV/AIDS strategy (90% of persons living with HIV know their status; 90% of persons with diagnosed infection prescribed antiretroviral therapy (ART); and 90% of those on ART virally suppressed).1,2 Yet, this progress has been woefully unequal when considered by race, sexuality, and age.3 Black MSM continue to face the greatest burden of HIV. Data from 2018 suggest that 1 in 2 Black MSM are projected to acquire HIV in their lifetimes, compared to 1 in 11 white MSM.4 HIV diagnosis rates are between 22 and 33 times higher among Black individuals as compared to white.5 These disparities are more pronounced among young (aged 15-29 years old) Black MSM (YBMSM); nationally, these young men are three and five times more likely than their Latinx and white counterparts, respectively, to be living with HIV.6 Despite having fewer sex partners and less condomless sex than their white counterparts,7,8 YBMSM account for nearly half of all HIV diagnoses among MSM aged 18-29, compared to 19% among white young MSM.9
Additionally, Black MSM fare worse on all dimensions of the HIV continuum of care outcomes (i.e., awareness of HIV status, initiation in care, retention in care, medication adherence, and viral load suppression) relative to their white MSM counterparts.10,11 Research suggests that more Black MSM, compared to white or Latinx MSM, are infected but unaware of their HIV status.12,13 Awareness of HIV infection is particularly low among MSM under the age of 30.14 Once diagnosed, estimates indicate that only approximately 53% of Black MSM living with HIV are retained in care,15 and Black people living with HIV are less likely to adhere to ART long enough to be virally suppressed compared to individuals of other races or ethnicities.16–18 ART prescriptions among persons in HIV care increased overall from 89% in 2009 to 94% in 2013, yet fewer Blacks than Latinx or whites received ART prescriptions.16,19 Among Black MSM in care, approximately 52% are virally suppressed (as compared to 59% and 67% of white MSM, respectively).15 Mirroring trends in HIV diagnosis, young Black MSM face worse outcomes along the HIV care continuum than any other age cohort.7 YBMSM are least likely to be retained in HIV care7 and are at particularly high risk of poor ART adherence and, thus, having a detectable viral load;17,20 only about 45% of YBMSM are virally suppressed, compared to 60% of young white MSM.15
Syndemic Theory
These disparities in HIV prevention and treatment are likely attributable to syndemic factors, or the co-occurrence and interaction of social conditions and inequities,21 including violence, early-life adversities, substance use, depression, and homophobia.22 Syndemic theory demonstrates how health, social, and psychological conditions can co-occur and be mutually-reinforcing, 23 to collectively increase disease burden for certain populations,21,24 including HIV.23 Singer (1996) proposed the SAVA syndemic to understand the mutually reinforcing nature of substance abuse, violence, and AIDS/HIV evident among low-income racial and ethnic minority men.21,24 Researchers have continued to study how syndemic factors influence HIV risk among MSM. For example, in the EXPLORE study with a cohort of over 4,000 MSM, researchers demonstrated that accumulation of five syndemic factors (i.e., depression, alcohol, stimulant, and polydrug use, and childhood sexual abuse) predicts HIV seroconversion among MSM.25 While most commonly applied to HIV risk26–28 or incidence,25,29 syndemics research has also examined the effects of syndemics on outcomes for people living with HIV. The overall effects of syndemics on HIV care outcomes has been found to increase with each additional syndemic factor, such that every increase in syndemic factors (polysubstance use, depression, violence, sexual risk) was associated with higher viral load.30
Yet, since its introduction, syndemic theory has only minimally been applied to explain the HIV burden experienced by Black MSM.31–33 In research with a large sample of Black MSM, greater syndemic burden (i.e., an additive index consisting of measures of depression, childhood sexual abuse, alcohol and drug use, and intimate partner violence) was associated with increased HIV risk behaviors and increased likelihood of HIV infection.29 Additionally, data from the Multicenter AIDS Cohort Study demonstrate the interrelated nature of psychosocial health conditions among Black MSM including parental abuse, gay and non-gay related victimization, and internalized homophobia and their association with sexual risk behaviors.26 Relatively little attention has been paid to the influence of syndemics on HIV prevention. Recently, Chandler and colleagues (2020) sought to fill this gap and found that, surprisingly, Black MSM who reported syndemic factors (e.g. substance use, depression) were more likely to report an HIV test in the previous 6 months, and more likely to report using PrEP, than Black MSM who reported no syndemic factors.34,35 These findings suggest that individual-level factors (e.g. substance use) may be less relevant for understanding HIV disparities than social and structural syndemic conditions.34
Violence syndemics
Violence has been identified as a critical, and still understudied, aspect of syndemics.36 Violence is the intentional use of physical force or power, threatened or actual, that results in or has a high likelihood of resulting in injury, death, or psychological harm or maldevelopment.37 Although included as part of Singer’s early syndemic research,24 there continues to be a lack of understanding about how various types of violence influence HIV outcomes. Most research, for example, focuses on a specific type of violence exposure (e.g. childhood sexual abuse or intimate partner violence)26,38,39 and its relationship to HIV outcomes, rather than looking collectively and interactively at several types of experiences of violence. Much of the research on violence as part of syndemics focuses on interpersonal violence, with less attention to the social and structural manifestations of violence, including police and neighborhood violence.40 Additionally, there is little research on the ways in which various types of violence are co-occurring and reinforcing of one another, creating a syndemic of violence. Understanding the role of violence in syndemics among YBMSM is particularly needed, given that Black youth are significantly more likely to witness and be victims of violence than white or Latinx youth.41
Continuous traumatic violence
There is increasing recognition that individuals who are chronically exposed to violence, including social and structural forms of violence, may be particularly vulnerable to poor health outcomes.42 Similar to continuous traumatic stress, which includes chronic exposure to stressful life experiences,43,44 continuous traumatic violence (also known as chronic violence exposure) refers to situations in which individuals repeatedly face violence or threats of violence in their everyday lives for prolonged periods of time. This violence can present as continuous danger or ongoing threats that can manifest as structural, economic, psychological, interpersonal and social violence.44–46 An important characteristic of continuous traumatic violence is the existence of a current, ongoing threat rather than an isolated traumatic event or prior traumas in which the threat has ceased.47 A small but growing body of literature has started to examine continuous traumatic violence and its effects on HIV risk and treatment outcomes.48,49 Chronic exposure to violence has been found to be associated with condomless sex,50,51 PTSD, and substance misuse42 among Black adolescent males. Although understudied, longitudinal research has demonstrated that the effects of violence and trauma on HIV prevention and treatment operate through a person’s overall level of exposure experienced over time, rather than a change observed within a confined timeframe,52 highlighting the importance of examining continuous traumatic violence across the lifespan. Continuous traumatic violence may play a key role in understanding racial disparities evident along the HIV care continuum.
Chronic exposure to violence may be more detrimental to health and resiliency than episodic exposures,53 resulting in hypervigilance,54 chronic psychological dysregulation, and the undermining of health seeking or promoting behaviors.53 Individual victimization of any of these types of violence is essential for understanding HIV disparities experienced by YBMSM, as they disproportionately experience such violence types.55,56 But, of equal importance, is the continuous exposure over time experienced by some YBMSM to household violence, violence among peer networks, and neighborhood violence. In order to adequately understand the comprehensive and longitudinal impact of violence on the syndemics of HIV, we must consider continuous traumatic violence and the interconnected nature of multiple types of violence. Continuous traumatic violence for YBMSM is particularly salient in urban areas, which have long histories of place-based police and neighborhood violence coupled with health disparities due to racial segregation and disinvestment. Individuals living in resource-constrained communities of color in the US are disproportionately impacted by violence,57 and Black youth are significantly more likely to witness and be victims of violence than other youth.41 In Chicago, for example, neighborhoods that have high violence rates often bear the disproportionate burden of high STI/HIV rates.58 Greater exposure to community violence is associated with more sexual partners, inconsistent condom use59,60 and increased sexual risk behaviors.51,61 Additionally, race-based policing practices have been identified as a community-level HIV vulnerability,62 as perceived racism is a driver of sexual risk behaviors.63,64 Black MSM report high rates of being stopped and questioned by police, which may increase vulnerability to HIV and poor HIV care outcomes via psychological distress, racial discrimination, and condom-carrying behaviors.62 Racial discrimination, for example, is a well-documented driver of sexual risk behavior.63,64
An intersectional framework of syndemics
Researchers have suggested that syndemics experienced by Black men may be best approached in combination with an intersectional framework that accounts for the intersecting systems and oppressions that reinforce syndemics.65,66 Developed by Black feminist scholars,67–69 intersectionality examines how multiple social identities intersect and reflect intersecting social and structural inequities.67,68 For example, young Black MSM’s experiences with violence and HIV may reflect interlocking systems of oppression and privilege due to racism, heterosexism, sexism, and ageism. Intersectionality can complement syndemic theory by drawing attention to the systems and structures that influence syndemic conditions. Syndemic conditions such as community and police violence, criminal justice involvement, substance use, and psychological distress are created and upheld by broader structures of power and systems of oppression.70 Yet, syndemic research frequently examines individual-level conditions (e.g. interpersonal violence) without adequately considering the relevant social structures that reinforce those individual-level factors.33,71 Accounting for the unique and varied experiences of young Black MSM, particularly those rooted in structural intersectional oppression, may provide a more comprehensive understanding of syndemics.
Continuous traumatic violence and HIV outcomes among YBMSM: A proposed model
Guided by extant literature and theoretical underpinnings of syndemics, the continuous traumatic violence and HIV outcomes model (Figure 1) highlights the relationship among various forms of violence and the relationship between continuous traumatic violence and HIV risk and care outcomes. While accumulating evidence demonstrates the relationship between HIV and violence, there remains a paucity of research on this topic with YBMSM and a lack of understanding about how violence contributes to HIV outcomes and the ways in which we can protect against these outcomes. We provide an overview of the empirical literature that examines the syndemic relationships between various types of violence and the ways in which violent experiences collectively contribute to HIV risk and care outcomes.
Figure 1.
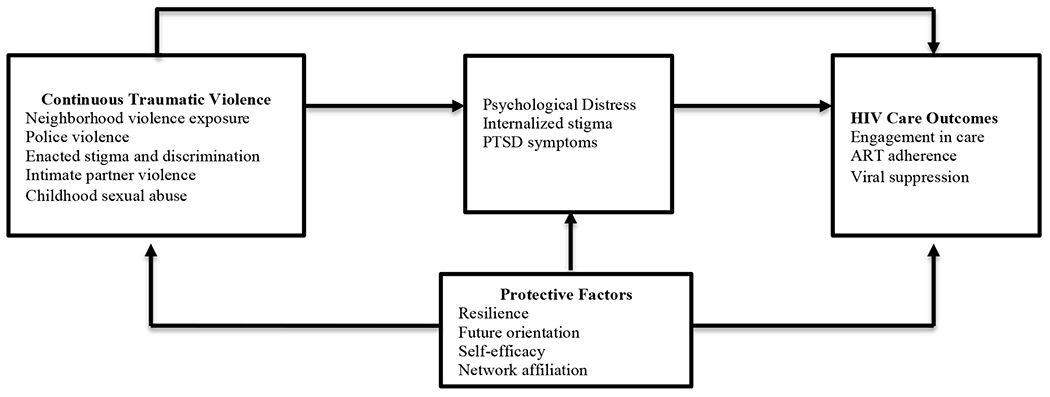
Continuous traumatic violence and HIV outcomes among YBMSM model
The proposed model suggests that experiences of violence, consisting of neighborhood violence, police violence, enacted stigma and discrimination, intimate partner violence, and childhood sexual abuse, can be chronic, cumulative, and mutually reinforcing, creating a violence syndemic. Similarly, those cumulative experiences of violence can both directly and indirectly (via psychological distress, internalized stigma, and PTSD symptoms) influence HIV care outcomes. There are also likely several protective factors including resilience, future orientation, self-efficacy, and network affiliation that may buffer the effects of violence. This model builds on existing empirical literature, summarized below.
Continuous traumatic violence experienced by YBMSM: A review of the evidence
Literature search
This is a focused review of published scientific literature on various experiences of violence among young Black MSM in the US and the ways in which violence operates as a syndemic. In early 2020, we conducted a literature review using PubMed, JSTOR, and Psychinfo to identify articles on violence in association with HIV prevention, risk, and treatment. Keywords included “violence and HIV,” “chronic violence exposure and HIV,” “violence syndemic” and “violence and Black MSM.” We also searched for specific types of violence known to affect MSM and/or Black men: childhood sexual abuse, race- and sexuality-based stigma and discrimination, neighborhood violence, police violence, and intimate partner violence. Although our focus was specific to young Black MSM, given the paucity of research on chronic violence exposure and violence syndemics among this population, we reviewed literature on violence among MSM of all ages and races and ethnicities. All searches focused on articles published in English. We reviewed abstracts to eliminate any unrelated studies (e.g. studies not in the US or those with women). Relevant research included both witnessing and experiencing violence and the effects of violence along all steps on the HIV continuum of care, including HIV prevention and risk. However, given the lack of research on violence along each step of the care continuum for Black MSM, particularly with regard to syndemic conditions, we have organized our review by type of violence, summarizing existing literature.
Neighborhood violence
The intersections of neighborhood violence, urban poverty, and HIV incidence are well documented among MSM.25,26,72,73 In particular, an extensive literature review has documented that neighborhood violence exposures, including victimization and witnessing violence, are correlated with increased HIV risk behaviors among Black youth including early sexual debut, having sex while under the influence of drugs or alcohol, and having sex without a condom.48,74 In research in Chicago, nearly 60% of adult participants reported lifetime exposure to neighborhood violence, and neighborhood violence was associated with HIV sexual risk behaviors among Black youth.50–74–78 Similarly, longitudinal research with YBMSM has shown that having a close friend or neighbor who was robbed or attacked is associated with more fragmented social network ties, which is in turn associated with higher reports of using drugs while having sex.79 Less research has examined how community violence exposure influences engagement in care, ART adherence, or viral suppression among YBMSM. However, some research has shown that neighborhood violence is positively associated with greater psychological distress, hard drug use, use of marijuana to facilitate sex, and condomless anal intercourse and negatively associated with ART adherence among YBMSM living with HIV.80,81
Police violence
There is clear evidence that communities that experience high rates of neighborhood violence also experience elevated levels of police violence.82,83 Continued police violence among Black men and the recent rise in support for the Black Lives Matter movement in response to the death of George Floyd,84 have thrust issues of racism and police violence into the forefront. Little research has examined the effects of police violence on HIV outcomes for YBMSM. Predominantly Black communities experience a higher burden of policing, arrests, and violent interactions with police, which may disproportionately affect Black MSM.85,86 Residential segregation is one of the most robust indicators associated with racial disparities in police shootings of unarmed victims.87 States with higher levels of structural racism (measured by segregation, economic, employment, education, and incarceration indices), have significantly higher Black-white disparities in rates of police shootings of unarmed victims.87,88 In a recent analysis of police violence, lifetime prevalence of police violence among Black individuals was nearly 18% for physical violence, 31% for psychological violence, and 29% for neglect, rates significantly higher than experienced by white and Latinx individuals.89 Another study of excessive police violence estimated that Black men were 21 times more likely to be killed by police than white men.90 Experience with police violence has also been found to be associated with greater odds of psychotic experiences and suicidal ideation and attempts among urban residents.89 In another recent study,54 among those who had ever been stopped by police, stops that met the criterion for being a traumatic event (participants who thought their lives were in danger or that they would be seriously injured) were associated with high levels of psychological distress. Notably, police violence had nearly twice the effect on psychological distress than exposure to other forms of neighborhood violence.54
Yet, there is a dearth of research on the effects of police violence on YBMSM, or Black MSM living with HIV. Reported experiences of police violence are highest among communities of color and individuals who identified as gay or transgender.89 In one of the only studies examining incarceration history and involvement with police among Black MSM, researchers found that police and law enforcement discrimination was associated with greater psychological distress and lower willingness to use HIV pre-exposure prophylaxis (PrEP) and incarceration and recent arrest were associated with greater sexual risk.91 Repeated arrests and episodes of incarceration can exacerbate the structural disadvantage that Black MSM experience by reducing access to housing, employment, medical care, and social services, which can create barriers along the entire HIV care continuum.62,92,93 Furthermore, incarceration can be a particularly violent experience for Black MSM, who face higher likelihood of sexual victimization from staff and other inmates while in prison.94 Importantly, data on police violence also provide some evidence of a violence syndemic, highlighting the association between police and other types of violence. For example, among a large urban sample, individuals who reported intimate partner violence or adverse childhood experiences (including child abuse) were significantly more likely to be exposed to all subtypes of police violence.89
Stigma and discrimination
We conceptualize stigma associated with race, sexuality, or HIV status as a form of structural violence,95 which may manifest as discrimination, marginalization, and physical violence. This conceptualization reflects the ways in which stigma is embedded in political, social and economic systems in the US to fuel inequity, injustice, and harm.96 Given the prevalence and intersection of racism, homophobia, and HIV-stigma, Black MSM may frequently contend with stigma and discrimination.97 For example, studies have identified high frequencies of reported discrimination based on race (40%), HIV status (38%) and sexual identity (33%) among Black men living with HIV, and further found that greater perceived discrimination was associated with lower ART adherence, increased AIDS symptoms, and lower likelihood of having an undetectable viral load.98,99 Among Black MSM living with HIV, researchers have found that individuals who reside in neighborhoods with higher rates of poverty experience more frequent hate crimes related to their sexual identity. Additionally, neighborhood-related stressors are related to more frequent discrimination based on race, sexuality, and HIV status.100
HIV-related discrimination has also been associated with lower ART adherence among people living with HIV.99,101 Similarly, exposure to crime and experiences of sexual and physical trauma are associated with greater perceived HIV stigma and concerns about initiating ART.102 There is also evidence that stigma and discrimination from health care providers can influence HIV care outcomes. Among Black MSM, perceived stigma or mistreatment due to sexual identity or race from health care providers is associated with longer elapsed time since last appointment with an HIV provider.103 These experiences of stigma can increase stress, limit social support, and increase sexual and drug-related risk behaviors among young MSM.104–106
Intimate partner violence (IPV)
Rates of lifetime IPV among MSM range from 15.4% to 51%,107 yet the relationship between IPV and HIV outcomes are still not well understood. Among Black MSM, receptive condomless anal intercourse at last sexual encounter, greater number of sexual partners in the last 30 days, and IPV were significantly associated with HIV prevalence and incidence.108 A meta-analysis demonstrated that being a survivor of IPV was associated with increased risk of alcohol or drug use, depressive symptoms, condomless anal sex, and being HIV positive.109 The relationship between IPV and sexual behaviors may be more complex for YBMSM, who are more likely to have older sexual partners and less experience negotiating safer sex than older MSM.110 Among young MSM, previous studies have found IPV to be associated with an increase in sexual risk behaviors.111,112 However, research by Chandler and colleagues found that among Black MSM, syndemic conditions may actually increase HIV prevention efforts. In their research, men with one or more syndemic factors (including IPV, substance use, and depression), were more likely to have had an HIV screening within the past 6 months.34 Similarly, syndemic conditions (IPV, substance use, and depression) were associated with increased likelihood to use HIV preexposure prophylaxis (PrEP).35
Among MSM living with HIV, IPV may lead to disruptions in care. IPV has been associated with a higher rate of clinically relevant interruptions in care, including an increased rate of HIV-related hospitalizations after diagnosis.113 Similarly, among a diverse sample of MSM in Miami, researchers found that greater syndemic burden (including IPV), was associated with ART non-adherence and lower odds of viral suppression.114
Childhood sexual abuse (CSA)
Childhood sexual abuse (CSA) is forced or unwanted sex before the age of 18 with someone five or more years older.115 Experiences of CSA can have significant emotional and behavioral effects for MSM. Research has shown that the prevalence of CSA among MSM is higher than among men in the general population.116 A number of studies have shown a strong and positive relationship between CSA and higher rates of HIV risk behaviors117 and infections among MSM,118 and poorer HIV continuum of care outcomes.117 Among Black MSM living with HIV, experiences of CSA are associated with greater number of sexual partners.119 CSA is also closely linked with other syndemic factors. For example, individuals reporting CSA are significantly more likely to have symptoms of depression and to report using nonprescription drugs.120–122 Substance use and psychological distress have been common pathways linking CSA to sexual behaviors.120 Related to other experiences of violence, CSA is associated with adult IPV,123 further compounding the effects of CSA and IPV. Studies have identified elevated rates of CSA and IPV among Black MSM, where CSA was associated with multiple HIV sexual risk behaviors.39,119 Black MSM who have experienced CSA also report high levels of PTSD and substance use.122
Continuous traumatic violence and the HIV care continuum
Given the stark disparities YBMSM face along the HIV care continuum, it is imperative to identify factors that reinforce violence syndemics to contribute to HIV disparities. A deeper understanding of how these multiple dimensions of violence may interact and influence HIV risk, engagement in care, and ART adherence among YBMSM is needed.
Psychological distress
Psychological distress, including depression, anxiety, and PTSD are hypothesized to be major mediating pathways linking various dimensions of continuous traumatic violence to poorer engagement and retention in HIV care for YBMSM. Rates of depression, anxiety, internalized stigma, and other psychological barriers are high among youth living with HIV.124 YBMSM who have experienced greater neighborhood violence had nearly five times the odds of psychological distress compared to those experiencing less neighborhood violence.125 Prior research has also found that YBMSM who experienced IPV were more likely to have greater psychological distress including suicidal ideation, where CSA was positively associated with the number of suicide attempts.126
Internalized stigma
Internalized stigma refers to the internalization or acceptance of prejudice, stereotypes, and negative views as a product of social bias.127 Internalized stigma can contribute to feelings of shame and lower self-worth, exacerbating the effects of violence on HIV disparities.128–130 For example, several studies have shown that internalized HIV stigma was associated with greater depressive symptoms, longer gaps in HIV medical care, and lower likelihood of anti-retroviral (ART) medication initiation and adherence.131–133 Internalized HIV stigma has also been linked to psychosocial outcomes and lower antiretroviral medication adherence;134 persons living with HIV with internalized HIV stigma may face concerns about being seen taking HIV medications, subsequently reducing adherence.135 Among YBMSM, internalized HIV stigma has been linked to greater psychological distress,104 which can negatively influence decisions to seek medical care.136
Racial and sexuality-related stigmas may have cumulative effects. Recent research has demonstrated that, among Black MSM, higher levels of internalized racial and sexuality-related stigma were associated with greater HIV/STI internalized stigma following diagnosis of HIV or an STI.137 The extant research on internalized stigma has tended to focus exclusively on a single type of stigma (e.g., HIV stigma),133,138,139 leading to an incomplete understanding of the ways in which stigma contributes to disparities in HIV outcomes. This is particularly problematic in understanding the HIV epidemic among Black MSM, as they are often exposed to high levels of multiple stigmas at the same time, including HIV status, socioeconomic status, sexual identity, and race.32,140–142 Additional research is needed to understand intersectional internalized stigmas and their collective effects on HIV outcomes especially for YBMSM.
Posttraumatic stress disorder (PTSD)
Post-traumatic stress disorder (PTSD) is a lasting mental health condition associated with exposure to a traumatic life event. PTSD symptoms, including re-experiencing (e.g. nightmares), avoidance, and arousal (e.g. overly alert or easily startled),143 may emerge in response to continued exposure to various forms of violence and stigma.64 Although understudied among Black MSM, PTSD symptoms and traumatic stress have been found to contribute to poorer physical and cognitive functioning among people living with HIV.144 Additionally, HIV-related discrimination is significantly associated with PTSD symptoms, as it may be a reminder of prior trauma (particularly hate crimes) and serve as a form of revictimization, aggravating PTSD symptoms.99 Research has demonstrated that racial discrimination is associated with PTSD among Black men, increasing risk for contracting HIV.145 Yet, relatively little work has teased out how PTSD symptoms may influence HIV outcomes for people living with HIV who have extensive histories of violence.
Protective factors
In addition to understanding the pathways by which violence may influence HIV outcomes, it is equally important to identify potential protective factors that could serve as points of intervention.
Resilience
Despite exposure to syndemic conditions, many YBMSM exhibit resilience,146 or the ability to overcome the negative effects of adversity to successfully cope with trauma.147 Meyer (2015) described two types of resilience: individual-based resilience (i.e., personal agency) and community-based resilience (i.e., connectedness to community and social resources).148 The majority of research on resilience focuses on individual-level resilience and has a tendency to place responsibility on overcoming adversity on stigmatized individuals, without adequate consideration of one’s environment or resources.149 In contrast, community-level resilience resources (e.g., access to community organizations) are seen as mitigating factors that are external to the individual and have the potential to help individuals overcome adversity.150 Community-level resilience reflects a community’s capacity to empower marginalized individuals via affirming social norms and values, inclusive policies, and safe and inclusive community spaces and health centers.151
In an exploratory study with Black MSM living with HIV, researchers found evidence that HIV-related stigma was associated with a range of interruptions in health care, and that resilience was associated with positive HIV care outcomes.152 Another study explored resilience processes in young MSM living with HIV and found that relationships with healthcare organizations and groups were a key strategy in managing their HIV, especially community-based support groups for youth who were recently diagnosed and those that were peer-led.153
Finally, although we conceptualize stigma and discrimination as a form of violence, there is also evidence that resilience processes in response to intersectional stigma may buffer the effects of stigma and discrimination for Black MSM living with HIV.154,155 Supportive social networks of YBMSM have been found to improve coping with intersectional discrimination and stigma and foster empowerment through role-modeling, self-advocacy, and encouragement.155 Additionally, research has found that coping strategies Black MSM living with HIV use to cope with racism may be adapted to cope with homophobia or HIV-related stigma.156 Interventions that support coping and response to intersectional stigma and discrimination may be important in improving HIV care outcomes for YBMSM living with HIV.157
Future orientation and self-efficacy
Future orientation is related to positive development in adolescence and may be a critical aspect of resilience as adolescents make choices and pathways to develop their personal and professional identities.158 Similarly, self-efficacy has recently been situated within resilience theory when examining risk behaviors among adolescents, as positive self-efficacy may buffer the negative forces or stressors of daily life.159 Several studies have documented that high future orientation (i.e., the ability to see a future self and forecast goals) and self-efficacy consistently mitigated the negative effects of neighborhood violence, interpersonal violence and family distress on HIV-related risk behaviors; further, high future orientation was correlated with more health seeking behaviors among YBMSM residing in highly economically disadvantaged and racially segregated Chicago neighborhoods.160–164
Network affiliation and linkages
Historically, urban gay communities and nonprofits developed out of overwhelmingly white gay networks.136 Thus, LGBTQ spaces that promote resilience in response to homonegativity may at the same time be a source of racism for MSM of color.72 In response, LGBTQ spaces designed by and for Black MSM have emerged to create safe spaces that reflect the needs of the Black LGBTQ community. Network affiliations (i.e., number and strength of connections to Black and gay communities) are also associated with differing HIV related risk and health promoting behaviors.165 Additionally, gay community involvement among Black MSM may have protective effects.135 The house and ball communities, for example, have served as important resources, particularly for YBMSM, providing supportive resources and an extended family network.75
Community ties to the Black community may be particularly salient for YBMSM. Research in Chicago, which has a high racial segregation index,166,167 has demonstrated that YBMSM were more likely to live in Black neighborhoods, had mostly same race friends and sexual partners168 and experienced racism in the gay community and wider society.169 Other research has shown that closeness with the mainstream gay community is associated with increased odds of living with HIV, higher rates of transactional sex, and increased sex under the influence of substances.165 In contrast, strong connections to the Black community is associated with lower odds of living with HIV.165 Accordingly, there is a need to understand how various social network ties and characteristics may influence the relationship between violence syndemics and HIV among YBMSM.170
Methodological challenges and future research directions
In order to guide and support future research that would empirically test this proposed conceptual model for YBMSM, we highlight several important methodological challenges and areas for future research. Prior studies have only assessed limited types of violence, which might lead to an overestimation of the effects of a particular type of violence exposure given that many of these forms of violence tend to co-occur. Police and neighborhood violence tend to co-occur,54 as do CSA and IPV.123,171 Such overestimations might impede a more precise estimation of salient correlates, which can hamper effective assessment and intervention efforts. Additionally, as highlighted throughout this review, there is a significant lack of research on the experiences of violence among YBMSM. Inferences are made based on research with white MSM or older Black MSM, but the intersecting stigma and oppression facing many young Black MSM create unique experiences with violence that require additional attention. The presence of race-based violence, and the ways in which race underpins the broader social and political systems in the US, creates experiences that cannot be gleaned from syndemic research with white MSM.172 While some existing research on trauma and resilience can more broadly provide some insights into how violence may influence HIV prevention and treatment among YBMSM, we lack a clear understanding of which types of violence contribute to various behaviors, negatively impacting our ability to design and administer appropriate interventions.
These challenges also highlight the need to apply an intersectional lens to syndemics research.65 Syndemics research too frequently focuses on individual exposures to violence without adequate recognition of the importance of oppression and power and the ways experiences of violence can vary based on the intersection at which an individual exists (e.g. race, sexuality, ability, socioeconomic status). Future research must continue to contextualize experiences of violence or syndemics experienced by YBMSM and contribute to interventions that are systemic or multi-level in nature, rather than focused at marginalized individuals. Additionally, an intersectional lens will help researchers consider the diversity within Black MSM populations, including sexual orientation, sexual identity, skin tone, socioeconomic status, and ability/disability. In our review, few studies explored or acknowledged this diversity. Thus, much of our existing literature refers to YBMSM as a single, monolithic group.
To advance the proposed conceptual model, qualitative formative research is needed to clarify, refine, and expand existing and proposed metrics and measures of violence syndemics. Qualitative data can be used to trace the trajectories of violence exposures and their intersectional impact on participants’ HIV history and continuum of care engagement. Qualitative data would also provide important insights into how individual and social types of resilience might help moderate the impact of violence syndemics on HIV continuum of care outcomes. For example, while community connections are typically understood to be protective, the reality may be more complicated for individuals who face racism and homonegativity from within communities to which they belong.
Finally, longitudinal research is also warranted to understand various dimensions of violence, their interactions and how they accumulate, and their impacts on each step of the HIV care continuum. Most of the research studies we highlight in this paper are cross sectional studies, limiting their ability to uncover intersecting and developmental effects on YBMSM. Longitudinal studies are needed to assess the short- and long-term effects of exposures to violence, the variation in cumulative violence effects, and violence syndemics effects on prevention, engagement and retention in care, ART adherence, viral load suppression. Longitudinal research must also apply methods that help identify syndemics and how they might evolve over time. For example, latent transition analysis (LTA), has demonstrated success in identifying various profiles of syndemics, changes in syndemic factors over time, and the ways in which protective factors (i.e. social support) may attenuate the effects of syndemic conditions for different individuals.172 Additionally, latent class analysis (LCA) has been used to identify patterns of HIV prevention and treatment and can help capture typically unmeasured patterns of concentration and interaction of syndemic factors.173,174
In addition, large enough representative sample sizes are needed so that various permutations of violence and their individual and additive effects can be ascertained. Respondent driven sampling (RDS) approaches can be very useful to address the challenge of sampling hard to reach populations.175 Similarly, studies have also recruited longitudinal community cohorts through a variety of community-based online and in-person strategies,39,175,176 including venue-based sampling, which can be particularly useful in reaching typically underrepresented samples.177
Limitations
This was not a systematic review and thus, our review may not have included all relevant literature. However, we are addressing significant gaps in the literature by proposing a conceptual model based on the available empirical literature that explores how violence syndemics might impact the HIV care continuum and factors that may influence those relationships. A more robust systematic review or meta-analysis is warranted. An empirical test of the conceptual model would help to identify more precise relationships between violence syndemics and specific HIV care continuum outcomes. There are certain areas of the literature that have received considerably less empirical attention and thus, the ways in which violence interacts with other syndemic conditions and effects each step of the care continuum remains unclear. Further, this review focused specifically on YBMSM in the US and thus, literature on the effects of violence on HIV care with populations outside of the US were not included. Violence is systematic in nature, influenced by social and political environments. Thus, the experiences of men in other countries may not apply to the experiences of YBMSM in urban communities in the US. Where possible, we identified the specific point in the HIV continuum affected by factors, however, an empirical test of the conceptual model would help to identify measurable relationships between violence syndemics and specific HIV care continuum outcomes. Even with these limitations, we are advancing scholarly understanding by proposing a conceptual model based on the available empirical literature that examines how violence syndemics might impact the HIV care continuum and the factors that may influence that relationship.
Conclusion
The proposed conceptual model advances our understanding of HIV disparities, especially the role of multiple dimensions of violence, to evaluate violence syndemics and their independent and interactive correlation with engagement and retention in care, HIV medication adherence, and viral suppression. There is a need to identify the most salient aspects of violence associated with engagement and retention in care and ART adherence among YBMSM, which can inform actionable public health strategies to reduce HIV disparities.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Contributor Information
Katherine G. Quinn, Medical College of Wisconsin, Center for AIDS Intervention Research
Antoinette Spector, Medical College of Wisconsin, Institute for Health Equity.
Lois Takahashi, University of Southern California.
Dexter R. Voisin, University of Toronto
References
- 1.Levi J, Raymond A, Pozniak A, Vernazza P, Kohler P, Hill A. Can the UNAIDS 90-90-90 target be achieved? A systematic analysis of national HIV treatment cascades. BMJ Glob Heal. 2016;1(2):e000010. doi: 10.1136/bmjgh-2015-000010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.White House Office of National AIDS Policy. National HIV/AIDS Strategy for the United States: Updated to 2020. Washington, DC: The White House; 2015. https://www.aids.gov/federal-resources/national-hiv-aids-strategy/nhas-update.pdf [Google Scholar]
- 3.Irene Hall H, Brooks JT, Mermin J. Can the United States achieve 90-90-90? Curr Opin HIV AIDS. 2019;14(6):464–470. doi: 10.1097/COH.0000000000000578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hess K, Hu X, Lansky A, Mermin J, Hall HI. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017;27(4):238–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crepaz N, Hess KL, Purcell DW, Hall HI. Estimating national rates of HIV infection among MSM, persons who inject drugs, and heterosexuals in the United States. AIDS. 2019;33(4):701–708. doi: 10.1097/QAD.0000000000002111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Millett G, Flores F, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: A meta-analysis of HIV risk behaviors. AIDS. 2007;21:2083–2091. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and and Prevention. HIV and Youth. Atlanta, GA; 2018. https://www.cdc.gov/hiv/pdf/group/age/youth/cdc-hiv-youth.pdf. [Google Scholar]
- 8.Friedman SR, Cooper HLF, Osborne AH. Structural and social contexts of HIV Risk among African Americans. Am J Public Health. 2009;99(6):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitsch A, Singh S, Li J, Balaji A, Linley L, Selik R. Age-Associated Trends in Diagnosis and Prevalence of Infection with HIV Among Men Who Have Sex with Men — United States, 2008–2016. MMWR Morb Mortal Wkly Rep. 2018. doi: 10.15585/mmwr.mm6737a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoots BE, Finlayson TJ, Wejnert C, Paz-Bailey G. Updated Data on Linkage to Human Immunodeficiency Virus Care and Antiretroviral Treatment among Men Who Have Sex with Men - 20 Cities, United States. J Infect Dis. 2017;216(7):808–812. doi: 10.1093/infdis/jix007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hightow-Weidman L, LeGrand S, Choi SK, Egger J, Hurt CB, Muessig KE. Exploring the HIV continuum of care among young black MSM. PLoS One. 2017;12(6):e0179688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Millett, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–348. [DOI] [PubMed] [Google Scholar]
- 13.Maulsby C, Millett G, Lindsey K, et al. HIV among black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav. 2014;18(l):10–25. [DOI] [PubMed] [Google Scholar]
- 14.(CDC) C for DC and P. Prevalence and awareness of HIV infection among men who have sex with men --- 21 cities, United States, 2008. MMWR Morbidity Mortal Wkly Rep. 2010;59(37): 1201–1207. doi:mm5937a2 [pii] [PubMed] [Google Scholar]
- 15.Singh S, Mitsch A, Wu B. HIV Care Outcomes Among Men Who Have Sex With Men With Diagnosed HIV Infection — United States, 2015. MMWR Morb Mortal Wkly Rep. 2017. doi: 10.15585/mmwr.mm6637a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crepaz N, Dong X, Wang X, Hernandez AL, Irene Hall H. Racial and ethnic disparities in sustained viral suppression and transmission risk potential among persons receiving HIV care - United States, 2014. Morb Mortal Wkly Rep. 2018. doi: 10.15585/mmwr.mm6704a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simoni JM, Huh D, Wilson IB, et al. Racial/Ethnic disparities in ART adherence in the United States: findings from the MACH14 study. J Acquir Immune Defic Syndr. 2012;60(5):466–472. doi: 10.1097/QAI.0b013e31825db0bd [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dailey AF, Johnson AS, Wu B. HIV care outcomes among blacks with diagnosed HIV — United States, 2014. Morb Mortal Wkly Rep. 2017. doi: 10.15585/mmwr.mm6604a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bradley H, Mattson CL, Beer L, Huang P, Shouse RL. Increased antiretroviral therapy prescription and HIV viral suppression among persons receiving clinical care for HIV infection. AIDS. 2016. doi: 10.1097/QAD.0000000000001164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacDonell K, Naar-King S, Huszti H, Belzer M. Barriers to medication adherence in behaviorally and perinatally infected youth living with HIV. AIDS Behav. 2013;17(1):86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singer M AIDS and the health crisis of the U.S. urban poor; the perspective of critical medical anthropology. Soc Sci Med. 1994;39(7):931–948. [DOI] [PubMed] [Google Scholar]
- 22.Herrick AL, Lim SH, Plankey MW, et al. Adversity and syndemic production among men participating in the multicenter AIDS cohort study: A life-course approach. Am J Public Health. 2013. doi: 10.2105/AJPH.2012.300810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tsai AC, Burns BFOO. Syndemics of psychosocial problems and HIV risk: A systematic review of empirical tests of the disease interaction concept. Soc Sci Med. 2015;139:26–35. doi: 10.1016/j.socscimed.2015.06.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singer M A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq Creat Sociol. 1996. [Google Scholar]
- 25.Mimiaga MJ, O’Cleirigh C, Biello KB, et al. The effect of psychosocial syndemic production on 4-year HIV incidence and risk behavior in a large cohort of sexually active men who have sex with men. J Acquir Immune Defic Syndr. 2015. doi: 10.1097/QAI.0000000000000475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dyer TP, Shoptaw S, Guadamuz TE, et al. Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. J Urban Heal. 2012;89(4):697–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mizuno Y, Borkowf C, Millett GA, Bingham T, Ayala G, Stueve A. Homophobia and racism experienced by Latino men who have sex with men in the United States: correlates of exposure and associations with HIV risk behaviors. AIDS Behav. 2012;16(3):724–735. [DOI] [PubMed] [Google Scholar]
- 28.Mustanski B, Phillips G, Ryan DT, Swann G, Kuhns L, Garofalo R. Prospective effects of a syndemic on HIV and STI incidence and risk behaviors in a cohort of young men who have sex with men. AIDS Behav. 2017;21(3):845–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O’Leary A, Jemmott IB, Stevens R, Rutledge SE, Icard LD. Optimism and education buffer the effects of syndemic conditions on HIV status among African American men who have sex with men. AIDS Behav. 2014;18(11):2080–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lriedman MR, Stall R, Silvestre AJ, et al. Effects of syndemics on HIV viral load and medication adherence in the multicentre AIDS cohort study. AIDS. 2015;29(9): 1087–1096. doi: 10.1097/QAD.0000000000000657 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuhns LM, Hotton AL, Garofalo R, et al. An Index of Multiple Psychosocial, Syndemic Conditions Is Associated with Antiretroviral Medication Adherence Among HIV-Positive Youth. AIDS Patient Care STDS. 2016;30(4):185–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Quinn KG, Reed SJ, Dickson-Gomez J, Kelly JA. An Exploration of Syndemic Factors That Influence Engagement in HIV Care Among Black Men. Onal Health Res. 2018;28(7). doi: 10.1177/1049732318759529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilson PA, Nanin J, Amesty S, Wallace S, Cherenack EM, Fullilove R. Using syndemic theory to understand vulnerability to HIV infection among Black and Latino men in New York City. J Urban Heal. 2014;91(5):983–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chandler CJ, Bukowski LA, Matthews DD, et al. Examining the Impact of a Psychosocial Syndemic on Past Six-Month HIV Screening Behavior of Black Men who have Sex with Men in the United States: Results from the POWER Study. AIDS Behav. 2020;24:428–436. doi: 10.1007/s10461-019-02458-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chandler CJ, Bukowski LA, Matthews DD, et al. Understanding the impact of a syndemic on the use of pre-exposure prophylaxis in a community-based sample of behaviorally PrEP-eligible BMSM in the United States. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2020;32(5). doi: 10.1080/09540121.2019.1659921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reuel Friedman M, Sang JM, Bukowski LA, et al. HIV Care Continuum Disparities among Black Bisexual Men and the Mediating Effect of Psychosocial Comorbidities. J Acquir Immune Defic Syndr. 2018. doi: 10.1097/QAI.0000000000001631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002;360(9339). doi: 10.1016/S0140-6736(02)11133-0 [DOI] [PubMed] [Google Scholar]
- 38.Wu E, El-Bassel N, McVinney LD, et al. The Association Between Substance Use and Intimate Partner Violence Within Black Male Same-Sex Relationships. J Interpers Violence. 2015;30(5). doi: 10.1177/0886260514536277 [DOI] [PubMed] [Google Scholar]
- 39.Wu E Childhood sexual abuse among Black men who have sex with men: A cornerstone of a syndemic? PLoS One. 2018;13(11). doi: 10.1371/journal.pone.0206746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Godley BA, Adimora AA. Syndemic theory, structural violence and HIV among African-Americans. Curr Opin HIV AIDS. 2020;15(4). doi: 10.1097/COH.0000000000000634 [DOI] [PubMed] [Google Scholar]
- 41.Crouch JL, Hanson RF, Saunders BE, Kilpatrick DG, Resnick HS. Income, race/ethnicity, and exposure to violence in youth: Results from the national survey of adolescents. J Community Psychol. 2000;28(6):625–641. [Google Scholar]
- 42.Richardson J, Robillard A. The Least of These: Chronic Exposure to Violence and HIV Risk Behaviors Among African American Male Violent Youth Offenders Detained in an Adult Jail. J Black Psychol. 2013;39(1). doi: 10.1177/0095798412447645 [DOI] [Google Scholar]
- 43.Straker G, Team SC. The continuous traumatic stress syndrome: the single therapeutic interview. Psychol Soc. 1987;8. [Google Scholar]
- 44.Straker G Continuous traumatic stress: Personal reflections 25 years on. Peace Confl. 2013. doi: 10.1037/a0032532 [DOI] [Google Scholar]
- 45.Kira IA, Ashby JS, Lewandowski L, Alawneh AWN, Mohanesh J, Odenat L. Advances in continuous traumatic stress theory: Traumatic dynamics and consequences of intergroup conflict: The Palestinian adolescents case. Psychology. 2013;4(04):396. [Google Scholar]
- 46.Eagle G Prof, Kaminer D. Continuous traumatic stress: Expanding the lexicon of traumatic stress. Peace Confl. 2013. doi: 10.1037/a0032485 [DOI] [Google Scholar]
- 47.Greene T, Itzhaky L, Bronstein I, Solomon Z. Psychopathology, risk, and resilience under exposure to continuous traumatic stress: A systematic review of studies among adults living in Southern Israel. Traumatology (Tallahass Fla). 2018;24(2). doi: 10.1037/trm0000136 [DOI] [Google Scholar]
- 48.Voisin DR, Jenkins EJ, Takahashi L. Toward a conceptual model linking community violence exposure to HIV-related risk behaviors among adolescents: directions for research. J Adolesc Heal. 2011;49(3):230–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Voisin DR, Neilands TB. Low school engagement and sexual behaviors among African American youth: examining the influences of gender, peer norms, and gang involvement. Child Youth Serv Rev. 2010;32:51–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Voisin DR. Victims of community violence and HIV sexual risk behaviors among African American adolescent males. J HIV AIDS Prev Editc Adolesc Child. 2003;5(3–4):87–110. doi: 10.1300/j129v05n03_05 [DOI] [Google Scholar]
- 51.Voisin DR. The relationship between violence exposure and HIV sexual risk behaviors: Does gender matter? Am J Orthopsychiatiy. 2005;75(4):497. [DOI] [PubMed] [Google Scholar]
- 52.Harkness A, Bainter SA, O’Cleirigh C, Mendez NA, Mayer KH, Safren SA. Longitudinal Effects of Syndemics on ART Non-adherence Among Sexual Minority Men. AIDS Behav. 2018. doi: 10.1007/s10461-018-2180-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mcewen BS, Gianaros PJ. Central role of the brain in stress and adaptation: links to soceioeconomic status, health, and disease. Arm NY Acad Sci. 2010;1186(The Biology of Disadvantage): 190–222. doi: 10.1111/j.1749-6632.2009.05331.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Smith A, Voisin D, Yang J, Tung E. Keeping your guard up: Hypervigilance among urban residents affected by community and police violence. Health Aff. 2019;38(10): 1662–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brunson RK, Miller J. Gender, race, and urban policing the experience of African American youths. Gend Soc. 2006;20(4): 531–552. [Google Scholar]
- 56.Seth P, Jackson JM, DiClemente RJ, Fasula AM. Community trauma as a predictor of sexual risk, marijuana use, and psychosocial outcomes among detained African-American female adolescents. Vulnerable Child Youth Stud. 2017;12(4):353–359. doi: 10.1080/17450128.2017.1325547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Centers for Disease Control and Prevention. 2010 Wed-based Injury Statistics Query and reporting System (wisqars). National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, http://www.cdc.gov/injury/wisqars/fatal/html Published 2010. [Google Scholar]
- 58.Bechteler S 100 Years and Counting: The Enduring Legacy of Racial Residential Segregation in Chicago in the Post-Civil Rights Era. Chicago, IL, IL; 2016. https://www.thechicagourbanleague.org/cms/lib07/IL07000264/Centricity/Domain/l/CULtivatePart1_ResidentialSegregationandHousing-Transportation_FinalDraft_3-1-16_10P.pdf. [Google Scholar]
- 59.Walsh JL, Senn TE, Carey MP. Exposure to different types of violence and subsequent sexual risk behavior among female sexually transmitted disease clinic patients: A latent class analysis. Psychol Violence. 2012;2:339. doi: 10.1037/a0027716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wilson HW, Woods BA, Emerson E, Donenberg GR. Patterns of violence exposure and sexual risk in low-income, urban African American girls. Psychol Violence. 2012;2(2): 194. doi: 10.1037/a0027265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Brady SS. Lifetime Community Violence Exposure and Health Risk Behavior among Young Adults in College. J Adolesc Heal. 2006;39:610. doi: 10.1016/j.jadohealth.2006.03.007 [DOI] [PubMed] [Google Scholar]
- 62.Parker CM, Parker RG, Philbin MM, Hirsch JS. The Impact of Urban US Policing Practices on Black Men Who Have Sex with Men’s HIV Vulnerability: Ethnographic Findings and a Conceptual Model for Future Research. J Urban Heal. 2018;95(2): 171–178. doi: 10.1007/s11524-017-0220-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fields EL, Bogart LM, Galvan FH, Wagner GJ, Klein DJ, Schuster MA. Association of discrimination-related trauma with sexual risk among HIV-positive African American men who have sex with men. Am J Public Health. 2013;103(5):875–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bowleg L, Burkholder GJ, Massie JS, et al. Racial discrimination, social support, and sexual hiv risk among black heterosexual men. AIDS Behav. 2013;17(1):407–418. doi: 10.1007/s10461-012-0179-0 [DOI] [PubMed] [Google Scholar]
- 65.Quinn K Applying an intersectional framework to understand syndemic conditions among young Black gay, bisexual, and other men who have sex with men. Soc Sci Med. 2019. doi: 10.1016/j.socscimed.2019.112779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ferlatte O, Salway T, Trussler T, Oliffe JL, Gilbert M. Combining intersectionality and syndemic theory to advance understandings of health inequities among Canadian gay, bisexual and other men who have sex with men. Crit Public Health. 2018. doi: 10.1080/09581596.2017.1380298 [DOI] [Google Scholar]
- 67.Crenshaw KW. Demarginalizing the intersection of race and sex: a black feminist critique of antidiscrimination doctrine, feminist theory, and antiracist politics. Univ Chic Leg Forum. 1989;139:139–167. [Google Scholar]
- 68.Collins PH. Moving beyond gender: intersecionality and scientific knowledge In: Feree MM, Lorber J, Hess BB, eds. Revisioning Gender. Walnut Creek, CA: AltaMira Press; 2000:261–284. [Google Scholar]
- 69.Bowleg L When black + lesbian + woman Φ black lesbian woman: the methodological challenges of qualitative and quantitative intersectionality research . Sex Roles. 2008;59:312–325. [Google Scholar]
- 70.Wyatt GE, Gomez CA, Hamilton AB, Valencia-Garcia D, Gant LM, Graham CE. The Intersection of Gender and Ethnicity in HIV Risk, Interventions, and Prevention New Frontiers for Psychology. Am Psychol. 2013;68(4):247–260. doi: 10.1037/a0032744 [DOI] [PubMed] [Google Scholar]
- 71.de Silva DT, Bouris A, Voisin D, Schneider J. Social networks moderate the syndemic effect of psychosocial and structural factors on HIV risk among young Black transgender women and men who have sex with men. AIDS Behav. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: further evidence of a syndemic. Am J Public Health. 2012; 102( 1): 156–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stall R, Mills TC, Williamston J. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93:939–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Voisin DR, Patel S, Hong JS, Takahashi L, Gaylord-Harden N. Behavioral health correlates of exposure to community violence among African-American adolescents in Chicago. Child Youth Serv Rev. 2016;69:97–105. doi: 10.1016/j.childyouth.2016.08.006 [DOI] [Google Scholar]
- 75.Voisin D, Takahashi L, Berringer K, Burr S, Kuhnen J. “Sex is violence”: African-American parents’ perceptions of the link between exposure to community violence and youth sexual behaviours. Child Fam Soc Work. 2016. doi: 10.1111/cfs.12162 [DOI] [Google Scholar]
- 76.Voisin DR, Salazar LF, Crosby R, DiClemente RJ, Yarber WL, Staples-Horne M. Witnessing community violence and health-risk behaviors among detained adolescents. Am J Orthopsychiatry. 2007;77(4):506. doi: 10.1037/0002-9432.77.4.506 [DOI] [PubMed] [Google Scholar]
- 77.Voisin DR, Tan K, Tack AC, Wade D, DiClemente R. Examining Parental Monitoring as a Pathway From Community Violence Exposure to Drug Use, Risky Sex, and Recidivism Among Detained Youth. J Soc Serv Res. 2012. doi: 10.1080/01488376.2012.716020 [DOI] [Google Scholar]
- 78.Voisin DR, Hotton AL, Neilands TB. Testing pathways linking exposure to community violence and sexual behaviors among African American youth. J Youth Adolesc. 2014;43(9): 1513–1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Skaathun B, Voisin DR, Cornwell B, Lauderdale DS, Schneider JA. A Longitudinal Examination of Factors Associated with Network Bridging Among YMSM: Implications for HIV Prevention. AIDS and Behavior. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Quinn K, Voisin DR, Bouris A, Schneider J. Psychological distress, drug use, sexual risks and medication adherence among young HIV-positive Black men who have sex with men: exposure to community violence matters. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2016;28(7). doi: 10.1080/09540121.2016.1153596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Voisin DR, Hotton AL, Schneider JA, et al. The relationship between life stressors and drug and sexual behaviors among a population-based sample of young Black men who have sex with men in Chicago. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2017. doi: 10.1080/09540121.2016.1224303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Krivo LJ, Peterson RD, Kuhl DC. Segregation, racial structure, and neighborhood violent crime. Am J Sociol. 2009;114(6):1765–1802. doi: 10.1086/597285 [DOI] [PubMed] [Google Scholar]
- 83.Hipp JR. Spreading the wealth: The effect of the distribution of income and race/ethnicity across households and neighborhoods on city crime trajectories. Criminology. 2011;49(3):631–665. doi: 10.1111/j.1745-9125.2011.00238.x [DOI] [Google Scholar]
- 84.Cohn N, Quealy K. How Public Opinion Has Moved on Black Lives Matter. New York Times; https://www.nytimes.com/interactive/2020/06/10/upshot/black-lives-matter-attitudes.html. [Google Scholar]
- 85.Brewer RA, Magnus M, Kuo I, Wang L, Liu T-Y, Mayer KH. The high prevalence of incarceration history among Black men who have sex with men in the United States: associations and implications. Am J Public Health. 2014;104(3):448–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lim JR, Sullivan PS, Salazar L, Spaulding AC, DiNenno EA. History of arrest and associated factors among men who have sex with men. J Urban Heal. 2011. ;88(4):677–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mesic A, Franklin L, Cansever A, et al. The Relationship Between Structural Racism and Black-White Disparities in Fatal Police Shootings at the State Level. J Natl Med Assoc. 2018;110(2): 106–116. doi: 10.1016/j.jnma.2017.12.002 [DOI] [PubMed] [Google Scholar]
- 88.Siegel M, Sherman R, Li C, Knopov A. The Relationship between Racial Residential Segregation and Black-White Disparities in Fatal Police Shootings at the City Level, 2013–2017. J Natl Med Assoc. 2019;111(6):580–587. doi: 10.1016/j.jnma.2019.06.003 [DOI] [PubMed] [Google Scholar]
- 89.DeVylder JE, Jun HJ, Fedina L, et al. Association of Exposure to Police Violence With Prevalence of Mental Health Symptoms Among Urban Residents in the United States. JAMA Netw open. 2018;l(7):e184945. doi: 10.1001/jamanetworkopen.2018.4945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ryan Gabrielson; Ryann Grochowski Jones; Eric Sagara. Deadly Force, in Black and White. ProPublica. 2014. https://www.propublica.org/article/deadly-force-in-black-and-white.
- 91.English D, Carter JA, Bowleg L, Malebranche DJ, Talan AJ, Rendina HJ. Intersectional social control: The roles of incarceration and police discrimination in psychological and HIV-related outcomes for Black sexual minority men. Soc Sci Med. 2020. doi: 10.1016/j.socscimed.2020.113121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hotton AL, Chen YT, Schumm P, et al. Socio-Structural and Neighborhood Predictors of Incident Criminal Justice Involvement in a Population-Based Cohort of Young Black MSM and Transgender Women. J Urban Heal. 2020. doi: 10.1007/s11524-020-00428-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Iroh PA, Mayo H, Nijhawan AE. The HIV care cascade before, during, and after incarceration: A systematic review and data synthesis. Am J Public Health. 2015;105(7):e5–e16. doi: 10.2105/AJPH.2015.302635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Beck AJ, Berzofsky M, Caspar R, Krebs C. Sexual Victimization in Prisons and Jails Reported by Inmates, 2011–12. US Dep Justice. 2013;(May). [Google Scholar]
- 95.Farmer P An anthropology of structural violence. Curr Anthropol. 2004;45(3):305–325. [Google Scholar]
- 96.Farmer PE, Nizeye B, Stulac S, Keshavjee S. Structural violence and clinical medicine. PLoS Med. 2006;3(10):e449. doi: 10.1371/journal.pmed.0030449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Diaz RM, Ayala G, Bein E. Sexual risk as an outcome of social oppression: data from a probability sample of Latino gay men in three US cities. Cult Divers Ethn Minor Psychol. 2004;10:255–267. [DOI] [PubMed] [Google Scholar]
- 98.Bogart LM, Wagner GJ, Galvan FH, Klein DJ. Longitudinal relationships between antiretroviral treatment adherence and discrimination due to HIV-serostatus, race, and sexual orientation among African-American men with HIV. Ann Behav Med. 2010;40(2): 184–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bogart LM, Wagner GJ, Galvan FH, Landrine H, Klein DJ, Sticklor LA. Perceived discrimination and mental health symptoms among black men with HIV. Cult Divers Ethn Minor Psychol. 2011;17(3):295–302. doi: 10.1037/a0024056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dale SK, Bogart LM, Galvan FH, Wagner GJ, Pantalone DW, Klein DJ. Discrimination and hate crimes in the context of neighborhood poverty and stressors among HIV-positive African-American men who have sex with men. J Community Health. 2016;41(3):574–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Thrasher AD, Earp JAL, Golin CE, Zimmer CR. Discrimination, distrust, and racial/ethnic disparities in antiretroviral therapy adherence among a national sample of HIV-infected patients. J Acquir Immune Defic Syndr. 2008. doi: 10.1097/QAI.0b013e3181845589 [DOI] [PubMed] [Google Scholar]
- 102.Soto T, Komaie G, Neilands TB, Johnson MO. Exposure to crime and trauma among HIV-infected men who have sex with men: Associations with HIV stigma and treatment engagement. J Assoc Nurses AIDS Care. 2013. doi: 10.1016/j.jana.2012.11.008 [DOI] [PubMed] [Google Scholar]
- 103.Eaton LA, Driffin DD, Kegler C, et al. The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. Am J Public Health. 2015;105(2):e75–e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Quinn K, Voisin DRDRDR, Bouris A, et al. Multiple Dimensions of Stigma and Health Related Factors Among Young Black Men Who Have Sex with Men. AIDS Behav. 2017;21(1):207–216. doi: 10.1007/s10461-016-1439-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Radcliffe J, Doty N, Hawkins LA, Gaskins CS, Beidas R, Rudy BJ. Stigma and sexual health risk in HIV-positive African American young men who have sex with men. AIDS Patient Care STDS. 2010;24:493–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rosario M, Scrimshaw EW, Hunter J. A model of sexual risk behaviors among young gay and bisexual men: Longitudinal associations of mental health, substance abuse, sexual abuse, and the coming-out process. AIDS Educ Prev. 2006;18(5):444–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Goldberg NG, Meyer IH. Sexual Orientation Disparities in History of Intimate Partner Violence: Results From the California Health Interview Survey. J Interpers Violence. 2013. doi: 10.1177/0886260512459384 [DOI] [PubMed] [Google Scholar]
- 108.Beymer MR, Harawa NT, Weiss RE, et al. Are Partner Race and Intimate Partner Violence Associated with Incident and Newly Diagnosed HIV Infection in African-American Men Who Have Sex with Men? J Urban Heal. 2017;94(5):666–675. doi: 10.1007/s11524-017-0169-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Buller AM, Devries KM, Howard LM, Bacchus LJ. Associations between Intimate Partner Violence and Health among Men Who Have Sex with Men: A Systematic Review and Meta-Analysis. PLoS Med. 2014. doi: 10.1371/journal.pmed.1001609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Anema A, Marshall BDL, Stevenson B, et al. Intergenerational sex as a risk factor for HIV among young men who have sex with men: A scoping review. Curr HIV AIDS Rep. 2013; 10(4):398–407. doi: 10.1007/s11904-013-0187-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Stults CB, Javdani S, Greenbaum CA, Kapadia F, Halkitis PN. Intimate partner violence and sex among young men who have sex with men. J Adolesc Heal. 2016;58(2):215–222. doi: 10.1016/j.jadohealth.2015.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kubicek K, McNeeley M, Collins S. Young Men Who Have Sex With Men’s Experiences With Intimate Partner Violence. J Adolesc Res. 2016;31 (1): 143–175. doi: 10.1177/0743558415584011 [DOI] [Google Scholar]
- 113.Greenwood RM, Schaefer-McDaniel NJ, Winkel G, Tsemberis SJ. Decreasing psychiatric symptoms by increasing choice in services for adults with histories of homelessness. Am J Community Psychol. 2005;36(3–4):223–238. [DOI] [PubMed] [Google Scholar]
- 114.Glynn TR, Safren SA, Carrico AW, et al. High Levels of Syndemics and Their Association with Adherence, Viral Non-suppression, and Biobehavioral Transmission Risk in Miami, a U.S. City with an HIV/AIDS Epidemic. AIDS Behav. 2019;23(11). doi: 10.1007/s10461-019-02619-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Arreola S, Neilands T, Pollack L, Paul J, Catania J. Childhood sexual experiences and adult health sequelae among gay and bisexual men: Defining childhood sexual abuse. J Sex Res. 2008;45(3). doi: 10.1080/00224490802204431 [DOI] [PubMed] [Google Scholar]
- 116.Paul JP, Catania J, Pollack L, Stall R. Understanding childhood sexual abuse as a predictor of sexual risk-taking among men who have sex with men: The Urban Men’s Health Study. Child Abus Negl. 2001. doi: 10.1016/S0145-2134(01)00226-5 [DOI] [PubMed] [Google Scholar]
- 117.Boroughs MS, Valentine SE, Ironson GH, et al. Complexity of Childhood Sexual Abuse: Predictors of Current Post-Traumatic Stress Disorder, Mood Disorders, Substance Use, and Sexual Risk Behavior Among Adult Men Who Have Sex with Men. Arch Sex Behav. 2015. doi: 10.1007/s10508-015-0546-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mimiaga MJ, Noonan E, Donnell D, et al. Childhood sexual abuse is highly associated with HIV risk-taking behavior and infection among MSM in the EXPLORE study. J Acquir Immune Defic Syndr. 2009. doi: 10.1097/QAI.0b013e3181a24b38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Williams JK, Wilton L, Magnus M, et al. Relation of childhood sexual abuse, intimate partner violence, and depression to risk factors for HIV among black men who have sex with men in 6 US cities. Am J Public Health. 2015;105(12):2473–2481. doi: 10.2105/AJPH.2015.302878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Holmes WC, Foa EB, Sammel MD. Men’s pathways to risky sexual behavior: Role of co-occurring childhood sexual abuse, posttraumatic stress disorder, and depression histories. In: Journal of Urban Health. ; 2005. doi: 10.1093/jurban/jti028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lloyd S, Operario D. HIV risk among men who have sex with men who have experienced childhood sexual abuse: Systematic review and meta-analysis. AIDS Educ Prev. 2012. doi: 10.1521/aeap.2012.24.3.228 [DOI] [PubMed] [Google Scholar]
- 122.Downing MJ, Benoit E, Brown D, et al. Early Sexual Experiences, Mental Health, and Risk Behavior among Black Non-Hispanic and Hispanic / Latino Men Who Have Sex with Men (MSM). J Child Sex Abus. 2020;29(1). doi: 10.1080/10538712.2019.1685618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Welles SL, Corbin TJ, Rich JA, Reed E, Raj A. Intimate partner violence among men having sex with men, women, or both: Early-life sexual and physical abuse as antecedents. J Community Health. 2011;36(3):477–485. doi: 10.1007/s10900-010-9331-9 [DOI] [PubMed] [Google Scholar]
- 124.Zanoni BC, Mayer KH. The adolescent and young adult HIV cascade of care in the United States: exaggerated health disparities. AIDS Patient Care STDS. 2014;28(3):128–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Quinn K, Voisin DRDRDR, Bouris A, Schneider J. Psychological distress, drug use, sexual risks and medication adherence among young HIV-positive Black men who have sex with men: exposure to community violence matters. AIDS Care. 2016;28(7):866–872. doi: 10.1080/09540121.2016.1153596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wilton L, Chiasson MA, Nandi V, et al. Characteristics and Correlates of Lifetime Suicidal Thoughts and Attempts Among Young Black Men Who Have Sex With Men (MSM) and Transgender Women. J Black Psychol. 2018;44(3):273–290. doi: 10.1177/0095798418771819 [DOI] [Google Scholar]
- 127.Herek GM, Gillis JR, Cogan JC. Internalized stigma among sexual minority adults: Insights from a social psychological perspective. J Couns Psychol. 2009;56(1):32. [Google Scholar]
- 128.Lee RS, Kochman A, Sikkema KJ. Internalized stigma among people living with HIV-AIDS. AIDS Behav. 2002;6(4):309–319. [Google Scholar]
- 129.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Rice WS, Crockett KB, Mugavero MJ, Raper JL, Atkins GC, Turan B. Association between internalized HIV-related stigma and HIV care visit adherence. J Acquir Immune Defic Syndr. 2017;76(5):482–487. doi: 10.1097/QAI.0000000000001543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Logie CH, Lacombe-Duncan A, Wang Y, et al. Pathways from HIV-related stigma to antiretroviral therapy measures in the HIV care cascade for women living with HIV in Canada. J Acquir Immune Defic Syndr. 2018. doi: 10.1097/QAI.0000000000001589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Turan B, Smith W, Cohen MH, et al. Mechanisms for the negative effects of internalized HIV-related stigma on antiretroviral therapy adherence in women: The mediating roles of social isolation and depression. J Acquir Immune Defic Syndr. 2016;72(2): 198–205. doi: 10.1097/QAI.0000000000000948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Turan B, Budhwani H, Fazeli PL, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav. 2017;21(1):283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Seghatol-Eslami VC, Dark HE, Raper JL, Mugavero MJ, Turan JM, Turan B. Brief Report: Interpersonal and Intrapersonal Factors as Parallel Independent Mediators in the Association between Internalized HIV Stigma and ART Adherence. J Acquir Immune Defic Syndr. 2017. doi: 10.1097/QAI.0000000000001177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chesney MA. Critical delays in HIV testing and care: the potential role of stigma. Am Behav Sci. 1999;42(7): 1162–1174. [Google Scholar]
- 137.Earnshaw VA, Reed NM, Watson RJ, Maksut JL, Allen AM, Eaton LA. Intersectional internalized stigma among Black gay and bisexual men: A longitudinal analysis spanning HIV/sexually transmitted infection diagnosis. Journal of Health Psychology. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Rendina HJ, Gamarel KE, Pachankis JE, Ventuneac A, Grov C, Parsons JT. Extending the Minority Stress Model to Incorporate HIV-Positive Gay and Bisexual Men’s Experiences: a Longitudinal Examination of Mental Health and Sexual Risk Behavior. Ann Behav Med. 2017;51(2):147–158. doi: 10.1007/s12160-016-9822-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Turan B, Rice WS, Crockett KB, et al. Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: The mediating role of depression. AIDS. 2019;33(3):571–576. doi: 10.1097/QAD.0000000000002071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Peterson JL, Jones KT. HIV prevention for black men who have sex with men in the United States. Am J Public Health. 2009;99(6):976–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Malebranche DJ, Fields EL, Bryant LO, Harper SR. Masculine socialization and sexual risk behaviors among Black men who have sex with men: A qualitative exploration. Men Masc. 2009;12(1):90–112. [Google Scholar]
- 142.Quinn K, Dickson-Gomez J. Homonegativity, Religiosity, and the Intersecting Identities of Young Black Men Who Have Sex with Men. AIDS Behav. 2016;22(1):51–64. doi: 10.1007/s10461-015-1200-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The posttraumatic diagnostic scale. Psychol Assess. 1997. doi: 10.1037/1040-3590.9.4.445 [DOI] [Google Scholar]
- 144.Leserman J, Whetten K, Lowe K, Stangl D, Swartz MS, Thielman NM. How trauma, recent stressful events, and PTSD affect functional health status and health utilization in HIV-infected patients in the South. Psychosom Med. 2005. doi: 10.1097/01.psy.0000160459.78182.d9 [DOI] [PubMed] [Google Scholar]
- 145.Bowleg L, Fitz CC, Burkholder GJ, et al. Racial discrimination and posttraumatic stress symptoms as pathways to sexual HIV risk behaviors among urban Black heterosexual men. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2014;26(8):1050–1057. doi: 10.1080/09540121.2014.906548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Herrick AL, Lim SH, Wei C, et al. Resilience as an untapped resource in behavioral intervention design for gay men. AIDS Behav. 2011;15(1):25–29. [DOI] [PubMed] [Google Scholar]
- 147.Herrick AL, Stall R, Goldhammer H, Egan JE, Mayer KH. Resilience as a research framework and as a cornerstone of prevention research for gay and bisexual men: theory and evidence. AIDS Behav. 2014; 18(1):1–9. [DOI] [PubMed] [Google Scholar]
- 148.Meyer IH. Resilience in the Study of Minority Stress and Health of Sexual and Gender Minorities. Psychol Sex Orientat Gend Divers. 2015;2(3):209–213. doi: 10.1037/sgd0000132 [DOI] [Google Scholar]
- 149.Lepore S, Revenson T. Resilience and posttraumatic growth: Recovery, resistence, and reconfiguration In: Calhoun L, Tedeschi R, eds. Handbook of Posttraumatic Growth: Research & Practice. Mahwah, NJ, NJ: Lawrence Erlbaum Associates Publishers; 2006:24–46. [Google Scholar]
- 150.Fergus S, Zimmerman MA. ADOLESCENT RESILIENCE: A Framework for Understanding Healthy Development in the Face of Risk. Annu Rev Public Health. 2005;26(1):399–419. doi: 10.1146/annurev.publhealth.26.021304.144357 [DOI] [PubMed] [Google Scholar]
- 151.McConnell EA, Janulis P, Phillips G, Truong R, Birkett M. Multiple minority stress and LGBT community resilience among sexual minority men. Psychol Sex Orientat Gend Divers. 2018;5(1):1–12. doi: 10.1037/sgd0000265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Brewer R, Hood KB, Moore M, et al. An Exploratory Study of Resilience, HIV-Related Stigma, and HIV Care Outcomes Among Men who have Sex with Men (MSM) Living with HIV in Louisiana. AIDS Behav. 2020. doi: 10.1007/s10461-020-02778-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Harper GW, Bruce D, Hosek SG, Isabel Fernandez M, Rood BA. Resilience processes demonstrated by young gay and bisexual men living with HIV: Implications for intervention. AIDS Patient Care STDS. 2014;28(12):666–676. doi: 10.1089/apc.2013.0330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Hussen SA, Harper GW, Rodgers CRR, Van Den Berg JJ, Dowshen N, Hightow-Weidman LB. Cognitive and behavioral resilience among young gay and bisexual men living with HIV. In: LGBT Health. Vol 4 ; 2017. doi: 10.1089/lgbt.2016.0135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Barry MC, Threats M, Blackburn NA, et al. “Stay strong! keep ya head up! move on! it gets better!!!!”: resilience processes in the healthMpowerment online intervention of young black gay, bisexual and other men who have sex with men. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2018;30(sup5). doi: 10.1080/09540121.2018.1510106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Bogart LM, Dale SK, Christian J, et al. Coping with discrimination among HIV-positive Black men who have sex with men. Cult Health Sex. 2017;19(7):723–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Bogart LM, Dale SK, Daffin GK, et al. Pilot intervention for discrimination-related coping among HIV-positive black sexual minority men. Cult Divers Ethn Minor Psychol. 2018. doi: 10.1037/cdp0000205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Di Maggio I, Ginevra MC, Nota L, Soresi S. Development and validation of an instrument to assess future orientation and resilience in adolescence. J Adolesc. 2016. doi: 10.1016/j.adolescence.2016.06.005 [DOI] [PubMed] [Google Scholar]
- 159.Veselska Z, Geckova AM, Orosova O, Gajdosova B, van Dijk JP, Reijneveld SA. Self-esteem and resilience: The connection with risky behavior among adolescents. Addict Behav. 2009. doi: 10.1016/j.addbeh.2008.11.005 [DOI] [PubMed] [Google Scholar]
- 160.So S, Voisin DR, Burnside A, Gaylord-Harden NK. Future orientation and health related factors among African American adolescents. Child Youth Serv Rev. 2016. doi: 10.1016/j.childyouth.2015.11.026 [DOI] [Google Scholar]
- 161.Kim D, Bassett S, Takahashi L, Voisin D. What does self-esteem have to do with behavioral health among low-income African American youth? J Youth Stud. [Google Scholar]
- 162.Morotta P, Voisin D. Pathways to delinquency and substance use among African American youth: Does future orientation mediate the effects of peer norms and parental monitoring? J Health Psychol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Voisin D, Kim D, Basett S, Morotto P. Pathways linking family stress to youth delinquency and substance use: Exploring the mediating roles of self-efficacy and future orientation. J Health Psychol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Kim D, Bassett S, So S, Voisin D. Pathways linking family stress to youth mental health problems: Exploring the mediating roles of self-efficacy and future orientation. J Orthopsychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Hotton AL, Keene L, Corbin DE, Schneider J, Voisin DR. The relationship between Black and gay community involvement and HIV-related risk behaviors among Black men who have sex with men. J Gay Lesbian Soc Serv. 2018. doi: 10.1080/10538720.2017.1408518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Semuels A Chicago’s Awful Divide. Atl. https://www.theatlantic.com/business/archive/2018/03/chicago-segregation-poverty/556649/.
- 167.Taeuber K Racial Residential Segregation, 28 Cities, 1970–1980. 1983. [Google Scholar]
- 168.Mays VM, Cochran SD, Zamudio A. HIV prevention research: are we meeting the needs of African American men who have sex with men? J Black Psychol. 2004;30(1):78–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Battle J, Cohen CJ, Warren D, Fergerson G, Audam S. Say It Loud, I’m Black and I In Proud: Black Pride Survey 2000. Washington DC; 2000. [Google Scholar]
- 170.de Silva DT, Bouris A, Voisin D, et al. Social networks moderate the syndemic effect of psychosocial and structural factors on HIV risk among young Black transgender women and men who have sex with men. AIDS Behav. 2019. doi: 10.1007/s10461-019-02575-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.K.F. B, K. L, B. B. Sexual revictimization and mental health: A comparison of lesbians, gay men, and heterosexual women. J Interpers Violence. 2011;26(9):1798–1814. doi: 10.1177/0886260510372946 [DOI] [PubMed] [Google Scholar]
- 172.Turpin R, Dyer T, Dangerfield D, Liu H, Mayer KH. Syndemic latent transition analysis in the HPTN 061 cohort: Prospective interactions between trauma, mental health, social support, and substance use. Drug Alcohol Depend. 2020. doi: 10.1016/j.drugalcdep.2020.108106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Mustanski B, Andrews R, Herrick A, Stall R, Schnarrs PW. A Syndemic of Psychosocial Health Disparities and Associations With Rifor Attempting Suicide Among Young Sexual Minority Men. Am J Public Health. 2014. doi: 10.2105/AJPH.2013.301744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Bourey C, Stephenson R, Bautista-Arredondo S. Syndemic vulnerability and condomless sex among incarcerated men in Mexico city: A latent class analysis. AIDS Behav. 2018;22(12). doi: 10.1007/s10461-018-2216-0 [DOI] [PubMed] [Google Scholar]
- 175.Heimer R Critical issues and further questions about respondent-driven sampling: Comment on Ramirez-Valles, et al. (2005). AIDS Behav. 2005;9(4):403–408. doi: 10.1007/s10461-005-9030-1 [DOI] [PubMed] [Google Scholar]
- 176.Duncan DT, Chaix B, Regan SD, et al. Collecting Mobility Data with GPS Methods to Understand the HIV Environmental Riskscape Among Young Black Men Who Have Sex with Men: A Multi-city Feasibility Study in the Deep South. AIDS Behav. 2018;22(9). doi: 10.1007/s10461-018-2163-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Gwadz M,M Cleland Exploring Factors Associated with Recent HIV Testing among Heterosexuals at High Risk for HIV Infection Recruited with Venue-based Sampling. J AIDS Clin Res. 2016;07(02). doi: 10.4172/2155-6113.1000544 [DOI] [PMC free article] [PubMed] [Google Scholar]


