Abstract
Childhood adversity (CA) and adulthood traumatic experiences (ATEs) are common and unequally distributed in the general population. Early stressors may beget later stressors and alter life-course trajectories of stressor exposure. Gender differences exist regarding the risk of specific stressors. However, few studies have examined the associations between specific types of CA and ATEs. Using a large-scale sample of older adults, we aimed to (a) determine if specific or cumulative CA increased the risk for specific or cumulative ATEs and (b) examine whether these associations were moderated by gender. In a sample from the U.S. Health and Retirement Study (N =15,717; Mage = 67.57 years, SD = 10.54), cross-sectional Poisson and logistic regression models were fitted to assess the specific and cumulative associations between CA and ATEs. Overall, cumulative CA was associated with a larger risk ratio of ATEs, adjusted for covariates: aRRRs =1.28, 1.63, and 1.97 for 1, 2, and 3–4 adverse events in childhood, respectively. Cumulative CA was particularly strongly associated with adulthood physical attacks, aOR = 5.66, and having a substance-abusing spouse or child, aOR = 4.00. Childhood physical abuse was the strongest independent risk factor for cumulative ATEs, aRRR = 1.49, and most strongly associated with adulthood physical attacks, aOR = 3.41. Gender moderated the association between cumulative CA and cumulative ATEs, with slightly stronger associations between cumulative CA and ATEs for women than men. Given that CA and ATEs perpetuate health disparities worldwide, reducing their incidence and effects should be major priorities for public health.
Childhood adversity (CA) and adulthood trauma exposure (ATE) are highly prevalent in the general population (Benjet et al., 2016; Copeland et al., 2007; Green et al., 2010; Hussey et al., 2006; Kilpatrick et al., 2013). These stressful experiences, particularly those that occur during childhood, such as physical abuse and parental substance abuse, have been linked to negative long-term outcomes ranging from mental health problems and suicide attempts to major medical illnesses and even premature mortality (Anda et al., 2006; Brown et al., 2009; Clemens et al., 2018; Dube et al., 2001, 2003; Felitti et al., 1998; Johnson et al., 2020; Logan-Greene et al., 2014; O'Donovan et al., 2015; Puterman et al., 2020; Riedl et al., 2019). Despite the strong effects of CA on mental and physical health outcomes, our understanding of the various pathways that link adverse events during childhood to ill health remains incomplete. One possibility is that early adversity alters the trajectories of stress exposure in later life, increasing the risk for trauma exposure in adulthood. Therefore, to further our understanding of stress exposures and their associations across the life-course, we investigated the association between CA and ATEs in a large, community-based sample of older adults from the Health and Retirement Study (HRS).
Population-based studies have shown high prevalence rates of CA and ATEs worldwide (Kessler et al., 2010, 2017). Approximately 50%–70% of children in the United States are exposed to some kind of adverse event during childhood, with multiple adversities common among those affected (Copeland et al., 2007; Felitti et al., 1998; Green et al., 2010; Hussey et al., 2006). In these studies, the CA construct includes a broad array of experiences, including items directly related to emotional and physical abuse, neglect, family instability, and parental substance abuse, which are typically summed to create a cumulative index of different exposure types (Dube et al., 2001; Felitti et al., 1998). Worldwide studies of life-course trauma exposure have demonstrated that over two-thirds of individuals experience at least one traumatic event in their life course, and approximately one-third of the population experiences four or more such events (Benjet et al., 2016; Kessler et al., 2017). The lifetime prevalence of traumatic experiences in the United States is high—60%–90%—with multiple exposures being very common (Benjet et al., 2016; Breslau et al., 1998; Kilpatrick et al., 2013; Norris, 1992). In light of these exposure rates, it is important to understand how stressful childhood events are related to ATEs.
Two related theoretical models attempt to explain the potent impact of CA on health: early embedding in critical periods and life-course stress models. First, childhood is a critical period for the development and integrity of major biological systems and psychological processes. Childhood is a particularly vulnerable phase of high plasticity, as there are major shifts in the development of brain structure and functioning, the hormonal system and stress responses, and many other important systems (Heim et al., 2010; Kolb & Gibb, 2014; McCrory et al., 2017; McCrory & Viding, 2015). Furthermore, childhood is a critical period for the development of cognitive and emotional processes, and emotional and social information processing enables personal and social functioning in adulthood. However, interruptions in such development could lead to maladaptation and latent vulnerability in adulthood (McCrory et al., 2017; McCrory & Viding, 2015; McLaughlin et al., 2019, 2020). In line with such models, recent studies have shown that adverse experiences that occur during specific age ranges in childhood are associated with altered neurodevelopment, accelerated maturation, and epigenetic changes (Callaghan & Tottenham, 2016; Dunn et al., 2018; Hambrick et al., 2019; McCrory et al., 2017; Szyf & Bick, 2013).
Second, CA may alter later trajectories of stress exposure, increasing the overall lifespan burden of stressor exposure. Life-course stress theories, such as cumulative inequality theory, state that “social systems generate inequality, which is manifested over the lifespan via demographic and developmental processes, and that personal trajectories are shaped by the accumulation of risk, available resources, perceived trajectories, and human agency” (Ferraro & Shippee, 2009, p. 334). Similarly, stress proliferation theories argue that people who experience adversity are at an increased risk of experiencing additional later adversities, including traumatic stress exposures (Pearlin et al., 2005). In line with these life-course perspectives, studies have shown that CA is associated with increased adult life stress exposures and perceived distress (Manyema et al., 2018; Nurius et al., 2015). The evidence for a life-course stress accumulation perspective is further supported by dose–dependent effects that link cumulative CA to later adverse outcomes (Anda et al., 2006; Berens et al., 2017; Dube et al., 2001, 2003; Felitti et al., 1998; Logan-Greene et al., 2014). Understanding the distributions of exposures from a life-course perspective might open up possibilities for strategic interventions to counteract maladaptation and latent vulnerability following early adverse experiences.
Although the overall cumulative number of trauma exposures tends to be higher in men than in women, additional gender differences in exposure can be found when focusing on specific categories of events, such as sexual abuse (Benjet et al., 2016; Hatch & Dohrenwend, 2007; Tolin & Foa, 2008). Several reviews and large-scale studies on gender differences in overall trauma exposure have shown that women are less likely to experience traumatic events compared to men (Breslau, 2002; Breslau et al., 1998; Hatch & Dohrenwend, 2007; Tolin & Foa, 2008). However, when examining specific types of exposure, women have been found to have a higher risk than men of experiencing adverse sexual incidents and equal risk of experiencing nonsexual abuse (Olff, 2017; Tolin & Foa, 2008). Furthermore, women have been shown to be less likely to be exposed to accidents and disasters, nonsexual assaults, witnessing death or injury, and military trauma than men (Tolin & Foa, 2008). During childhood specifically, no significant gender differences in overall cumulative exposure have been found; however, girls were found to experience more sexual abuse than boys (Tolin & Foa, 2008). Despite the higher rates of overall trauma exposure in men, women have a higher risk of developing posttraumatic stress disorder (PTSD), which may partly be due to differences in the types of traumatic events men and women experience (Breslau, 2002; Breslau et al., 1998; Olff, 2017; Tolin & Foa, 2008). Overall, the literature has demonstrated differences in trauma exposure with regard to gender as well as the importance of focusing not only on cumulative exposure scores but also on specific exposure types.
Despite the high prevalence rates of CA and ATEs, their associations with increased risks for diseases of aging, and the rapid aging of the global population, only a small number of studies have investigated the prevalence of CA and ATEs in older populations. Little is known about how CA alters the risk for ATEs across the life-course, which is particularly important because CA and ATEs are some of the strongest known risk factors for a broad range of adverse health outcomes in later life (Clemens et al., 2018; Johnson et al., 2020; Logan-Greene et al., 2014; Riedl et al., 2019). Many previous studies have lacked a life-course perspective and have had insufficient sample sizes to investigate specific combinations and patterns of trauma exposure. In addition, beyond well-known gender differences in exposure to adverse events in childhood and ATEs, little is known about gender and its impact on the associations between specific types of CA and ATEs. We add to this growing literature by investigating associations between specific types of CA and specific ATEs. In particular, our study aims were to (a) determine whether CA would be shown to increase the risk for ATEs in a large-scale sample of older adults, with a focus on whether specific types of CA or cumulative CA were associated with specific or cumulative ATEs, and (b) examine if these associations were moderated by gender.
Method
Participants
In the HRS, a longitudinal study of a population-based U.S. sample, more than 40,000 individuals over 50 years of age and their spouses were interviewed (Fisher & Ryan, 2018) from 1992 through the present. The original HRS study population included community-dwelling adults in the contiguous United States born during the years 1931 to 1941, with a 2:1 oversampling of African American and Hispanic populations. This sample has been refreshed with new birth cohorts over the years with participants born during 1890–1931 and 1941–1959, leading to the current HRS population (Fisher & Ryan, 2018; Sonnega et al., 2014). The actual panel of HRS participants at each wave of data collection is much smaller than the total amount of participants, as some participants have already died, and others entered the panel at a later date. Therefore, the sample size of each wave is approximately 20,000 (HRS, 2017c). The HRS is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan.
Procedure
Starting in 2006, the HRS implemented a psychosocial questionnaire that included assessments of CA and ATEs (Clarke et al., 2008; Smith et al., 2017). After the interview section of the HRS, which is conducted at each wave of data collection, participants answered a questionnaire on different psychosocial domains, called the “leave behind” (LB) questionnaire (Clarke et al., 2008; Smith et al., 2017). Response rates for these questionnaires were high: Between 73% and 88% of eligible participants responded to the LB questionnaire over the course of assessments (Smith et al., 2017). At the start of each interview, respondents received a written informed consent document, were read a confidentiality statement, and gave oral consent to take part in the interview. Ethical approval for the HRS was granted from the University of Michigan Institutional Review Board and the study has been conducted according to the principles of the Declaration of Helsinki.
For the current study, data from respondents of the assessments administered in 2008, 2010, and 2012 were analyzed (HRS, 2014b, 2017a, 2017b). Missing CA and ATE values in the 2010 wave were replaced with data from the 2006 wave (HRS, 2014a). All participants from the original sample who had completed all ATE-related measures and were at least 50 years old at the time of their assessment were included in the analyses. A total of 15,717 participants met these inclusion criteria: In the final analytic sample, 40.1% of all participants were from the 2008 assessment, 46.1% were from the 2010 wave, and 13.4% were from 2012.
Measures
Childhood Adversity
Childhood adversity was evaluated using four items from a list of lifetime potentially traumatic events (Krause et al., 2004). Participants indicated whether they had ever experienced any of four adverse events before the age of 18 years. These incidences included: repeating a year of school, having had trouble with the police (added in 2008), parental alcohol or drug use that caused family problems, and physical abuse by a parent (Clarke et al., 2008; Smith et al., 2017). We examined the reliability of this measure by assessing the 4-year test–retest reliability of these items in more than 10,000 participants. We found high agreement in scoring on these items, which ranged from 92.4% and 96.0%. The cumulative index was created by summing different childhood exposures. We combined three to four types of CA into one category to have a group that was sufficiently large (i.e., 1.9% of the total sample).
Adulthood Trauma Exposure
Adulthood traumatic experiences were assessed using seven items from a list of lifetime potentially traumatic events (Krause et al., 2004). Respondents reported whether they had experienced each of seven events at any point during their life. If participants experienced an incident, they were asked to indicate the year the most recent exposure occurred. We excluded events that were reported to have occurred before 18 years of age from the ATE scores. The potentially traumatic events included: having lost a child; having experienced a major fire, flood, earthquake, or natural disaster; having fired a weapon in combat or been fired upon in combat; having had a spouse, partner, or child addicted to drugs or alcohol; having been the victim of a serious physical attack or assault; having had a life-threatening illness or accident; and having had a spouse or child who experienced a life-threatening illness or accident (Clarke et al., 2008; Smith et al., 2017). A cumulative ATE index was created by summing the different adulthood exposure types.
Covariates
All covariates were derived from the RAND HRS Detailed Imputations File 2014 (Version 2; RAND, 2018). These files were developed at RAND with funding from the National Institute on Aging and the Social Security Administration. We extracted the following variables from the RAND HRS data: age (i.e., year of trauma exposure assessment minus year of birth) and gender (i.e., participants self-identified as men or women). As in previous studies of HRS participants with regard to CA and ATEs (Puterman et al., 2016), race/ethnicity (Caucasian [non-Hispanic], African American [non-Hispanic], Hispanic, other [non-Hispanic]) and childhood socioeconomic status (SES) were included as covariates. Childhood SES was measured using information on parental educational attainment, defined as fulfilling at least 8 years of school. Parental educational attainment for both parents was queried; the higher score was used for parental education if data from both parents, and the single available value was used if only one parent responded to the item.
Data Analysis
Demographic characteristics, study descriptive information, and prevalence rates of CA and ATEs, by gender, are provided in Tables 1 and 2. Several different sets of cross-sectional analyses were conducted: Poisson regressions for the cumulative ATE index and logistic regressions for specific ATEs as outcomes. Adjusted relative risk ratios (aRRRs) are reported for Poisson regressions, and adjusted odds ratios (aORs) are reported for logistic regressions, with respective 95% confidence intervals (CIs). Adulthood trauma exposure scores (i.e., count of trauma types) markedly decreased from reporting zero ATEs to seven ATEs, and the mean and standard deviation of cumulative ATEs was very similar (M = 1.199, SD = 1.202), suggesting the data were not overdispersed and met the assumption for Poisson models. First, we examined whether cumulative CA was associated with cumulative and specific ATEs, controlling for age, gender, race/ethnicity, and parental educational attainment (see Table 3). Each column in Table 3 indicates a distinct multivariate regression model. Second, we examined whether specific types of CA were associated with cumulative and specific ATEs, controlling for age, gender, race/ethnicity, and parental educational attainment (see Table 4); in these models, the effects of specific types of CA were independent (i.e., mutually adjusted) of each other. Third, all models were recalculated including an interaction term for CA and gender. If the findings indicated significant interactions, the models were rerun stratified by gender, and these findings were subsequently reported. Tables and plots for all other findings resulting from gender-stratified analyses are available in the Supplementary Materials. All statistical analyses were conducted in R through RStudio (Version 3.5.2; 2018). The plots were created using the R-packages “sjPlot” (Lüdecke, 2018) and “ggplot2” (Wickham, 2016). The proportions of missing items regarding descriptive information and CAs are reported in Table 1. As the proportion of missingness was small (i.e., 7%) and the missingness was largely unrelated to study demographics, we decided to do complete case analyses. The p values for all models are indicated at the levels of < .05, < .01, and < .001. However, as large sample sizes may cause very small effects to be highly significant, we have focused our interpretation of the data on the largest effect sizes of our findings (i.e., aRRRs and aORs). We did not adjust p values for multiple testing; therefore, all analyses were descriptive and exploratory in nature.
Table 1.
Study Characteristics, by Gender
| Total | ||
|---|---|---|
| na | %b | |
| Gender | ||
| Women | 9,164 | 58.3 |
| Men | 6,553 | 41.7 |
| Race/ethnicity | ||
| Caucasian | 11,159 | 71.1 |
| African American | 2,478 | 15.8 |
| Hispanic | 1,628 | 10.4 |
| Other | 433 | 2.8 |
| Missing | 19 | - |
| Parental educational attainment (years) | ||
| < 8 | 1,950 | 13.3 |
| ≥ 8 | 12,742 | 86.7 |
| Missing | 1,025 | - |
Note.
Number of observations.
Percentages are based on observed cases without missing data.
Table 2.
Childhood Adversity (CA) and Adulthood Traumatic Experiences (ATEs), by Gender
| Gender | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Women | Men | Statistical test | Cramer’s V | ϕ | p | ||||
| Cumulative CA | na | %b | na | %b | na | %b | ||||
| 0 | 10,350 | 66.5 | 6,422 | 70.7 | 3,928 | 60.5 | ||||
| 1 | 3,849 | 24.7 | 2,054 | 22.6 | 1,795 | 27.7 | ||||
| 2 | 1,080 | 6.9 | 506 | 5.6 | 574 | 8.8 | χ2(3, N = 15,576) = 226.75 | .12 | < .001 | |
| 3–4 | 297 | 1.9 | 102 | 1.1 | 195 | 3.0 | ||||
| Missing | 141 | 0.9 | ||||||||
| Cumulative ATEs | ||||||||||
| 0 | 5,926 | 37.7 | 3,489 | 38.1 | 2,437 | 37.2 | ||||
| 1 | 4,806 | 30.6 | 2,815 | 30.7 | 1991 | 30.4 | ||||
| 2 | 2,954 | 18.8 | 1,726 | 18.8 | 1,228 | 18.7 | ||||
| 3 | 1,383 | 8.8 | 779 | 8.5 | 604 | 9.2 | χ2(4, N = 15,717) = 6.49 | .02 | .166 | |
| ≥ 4 | 648 | 4.1 | 355 | 3.9 | 293 | 4.5 | ||||
| Specific types of CA | ||||||||||
| Repeat school year | 2,460 | 15.7 | 1,055 | 11.6 | 1,405 | 21.5 | χ2(1, N = 15,664) = 285.41 | −.14 | < .001 | |
| Missing | 53 | 0.3 | ||||||||
| Trouble with police | 874 | 5.6 | 142 | 1.6 | 732 | 11.2 | χ2(1, N = 15,642) = 671.26 | −.21 | < .001 | |
| Missing | 75 | 0.5 | ||||||||
| Parental substance abuse | 2,551 | 16.3 | 1,508 | 16.5 | 1,043 | 15.0 | χ2(1, N = 15,650) = 0.77 | .01 | .382 | |
| Missing | 67 | 0.4 | ||||||||
| Parental physical abuse | 1,101 | 7.0 | 702 | 7.7 | 399 | 6.1 | χ2(1, N = 15,649) = 14.1 | .03 | < .001 | |
| Missing | 68 | 0.4 | - | - | ||||||
| Specific ATEs | ||||||||||
| Child died | 2,461 | 15.7 | 1,577 | 17.2 | 884 | 13.5 | χ2(1, N = 15,717) = 39.73 | .05 | < .001 | |
| Major disaster | 2,544 | 16.2 | 1,412 | 15.4 | 1,132 | 17.3 | χ2(1, N = 15,717) = 9.67 | .02 | .002 | |
| Military combat | 838 | 5.3 | 28 | 0.3 | 810 | 12.4 | χ2(1, N = 15,717) = 1,097.70 | .26 | < .001 | |
| Family member with substance addiction | 2,828 | 17.0 | 1,963 | 21.4 | 865 | 13.2 | χ2(1, N = 15,717) = 174.43 | .11 | < .001 | |
| Physical attack | 948 | 6.0 | 586 | 6.4 | 362 | 5.5 | χ2(1, N = 15,717) = 4.96 | .02 | .026 | |
| Illness/accident | 3,874 | 24.7 | 1,958 | 21.4 | 1,916 | 29.2 | χ2(1, N = 15,717) = 127.07 | .09 | < .001 | |
| Family member illness/accident | 4,163 | 26.5 | 2,609 | 28.5 | 1,554 | 23.7 | χ2(1, N = 15,717) = 44.14 | .05 | < .001 | |
Note.
Number of observations.
Percentages for “missing” information is based on all cases; percentages for exposure items are based on observed cases only.
Table 3.
Associations Between Cumulative CA and Adulthood Traumatic Experiences (ATEs)
| 1 type of CA | 2 types of CA | 3–4 Types of CA | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Type of ATE | aRRR | aOR | 95% CI | aRRR | aOR | 95% CI | aRRR | aOR | 95% CI |
| Cumulative ATEs | 1.28*** | [1.23, 1.32] | 1.63*** | [1.54, 1.72] | 1.97*** | [1.80, 2.15] | |||
| Death of child | 1.21*** | [1.09, 1.35] | 1.63*** | [1.36, 1.94] | 1.89*** | [1.36, 2.59] | |||
| Disaster | 1.30*** | [1.17, 1.44] | 1.55*** | [1.31, 1.82] | 1.53** | [1.13, 2.03] | |||
| Military combat | 1.05 | [0.87, 1.26] | 1.55** | [1.18, 2.02] | 2.13*** | [1.39, 3.17] | |||
| Family member substance addiction | 1.74*** | [1.58, 1.92] | 2.71*** | [2.33, 3.15] | 4.00*** | [3.08, 5.17] | |||
| Illness/accident | 2.07*** | [1.76, 2.43] | 3.94*** | [3.19, 4.84] | 5.66*** | [4.09, 7.72] | |||
| Family member illness/accident | 1.27*** | [1.17, 1.39] | 1.53*** | [1.32, 1.77] | 1.86*** | [1.43, 2.41] | |||
Note. N=14,552. Analyses controlled for age, gender, race/ethnicity, and parental educational attainment. aRRR = adjusted relative risk ratio (from Poisson regressions); aOR = adjusted odds ratio (from logistic regressions).
p < .01.
p < .001.
Table 4.
Associations Between Specific Types of Childhood Adversity (CA) and Adulthood Traumatic Experiences (ATEs)
| CA type | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Repeat of school year | Trouble with police | Parental substance abuse | Parental physical abuse | |||||||||
| Type of ATE | aRRR | aOR | 95% CI | aRRR | aOR | 95% CI | aRRR | aOR | 95% CI | aRRR | aOR | 95% CI |
| Cumulative ATEs | 1.08*** | [1.04, 1.13] | 1.25*** | [1.18, 1.34] | 1.28*** | [1.23, 1.33] | 1.49*** | [1.42, 1.57] | ||||
| Death of child | 1.32*** | [1.16, 1.49] | 1.18 | [0.94, 1.46] | 1.15* | [1.01, 1.31] | 1.36*** | [1.13, 1.62] | ||||
| Disaster | 1.11 | [0.99, 1.26] | 1.21* | [1.00, 1.45] | 1.18** | [1.05, 1.33] | 1.47*** | [1.25, 1.72] | ||||
| Military combat | 1.18 | [0.98, 1.42] | 1.28 | [0.98, 1.64] | 1.17 | [0.94, 1.45] | 1.36 | [0.99, 1.84] | ||||
| Family member substance addiction | 1.10 | [0.98, 1.25] | 1.72*** | 1.97*** | [1.77, 2.19] | 1.80*** | [1.55, 2.08] | |||||
| Physical attack | 1.25* | [1.04, 1.49] | 1.92*** | [1.51, 2.43] | 1.54*** | [1.30, 1.82] | 3.41*** | [2.82, 4.12] | ||||
| Illness/accident | 1.12* | [1.00, 1.24] | 1.27** | [1.08, 1.49] | 1.37*** | [1.24, 1.52] | 1.70*** | [1.48, 1.96] | ||||
| Family member illness/accident | 0.94 | [0.84, 1.05] | 1.27** | [1.07, 1.50] | 1.28*** | [1.15, 1.41] | 1.65*** | [1.43, 1.90] | ||||
Note. N = 14,552 observations. Analyses controlled for age, gender, race/ethnicity, and parental educational attainment. aRRR = adjusted relative risk ratio (from Poisson regressions); aOR = adjusted odds ratio (from logistic regressions).
p < .05.
p < .01.
p < .001.
Results
Descriptive Statistics
In total, 15,717 participants were included in the present analyses. The mean participant age was 67.57 years (SD = 10.55, range: 50–101 years). Table 1 presents the distributions of gender, race/ethnicity, and parental educational attainment. Regarding AC, 29.3% of participants were exposed to one of the four potentially traumatic childhood events listed; for ATEs, 61.1% were exposed to one of the seven events. Men were more likely to experience cumulative CA than women; however, there were no gender differences in cumulative ATEs on the descriptive level (see Table 2). When focusing on specific types of CA, women were less likely to repeat a year of school or have had trouble with the police than men, and they were slightly more likely to have been physically abused. With regard to gender differences for specific ATEs, women were more likely than men to have lost a child and less likely to have experienced a major disaster. Compared to men, women were much less likely to report experiencing combat-related trauma; much more likely to report a substance-addicted spouse, partner, or child; slightly more likely to have been physically attacked; less likely to report an illness or accident; and more likely to report a family member’s illness or accident (see Table 2).
Associations Between Childhood Adversity and Adulthood Trauma Exposure
Cumulative CA and ATEs
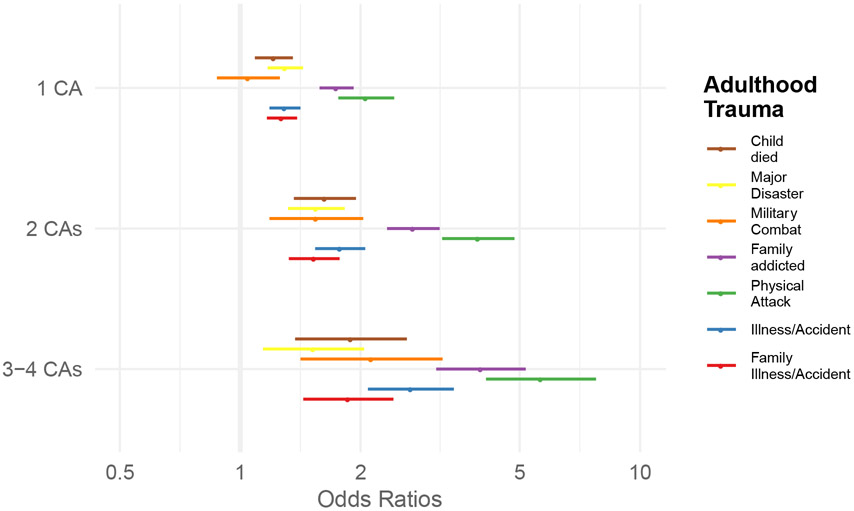
Overall, cumulative CA was associated with cumulative ATEs (see Table 3). Compared to experiencing no CA, experiencing one type of CA was related to a higher relative risk of cumulative ATEs, aRRR = 1.28, 95% CI [1.23, 1.32]. The addition of more types of CAs further heightened the risk for reporting more cumulative ATEs: aRRR = 1.63, 95% CI [1.54, 1.72] for two types of CA and aRRR = 1.97, 95% CI [1.80, 2.15] for three or four types of CA. Similar patterns were observed when examining specific ATEs, with participants who experienced more adverse events during childhood having higher odds of reporting subsequent specific ATEs (see Table 3). The largest effects were seen in the associations between cumulative CA (i.e., three or four types of CA) and a substance-addicted family member, aOR = 4.00, 95% CI [3.08, 5.17], and experiencing a physical attack, aOR = 5.66, 95% CI [4.09, 7.72].
Specific Types of CA and ATEs
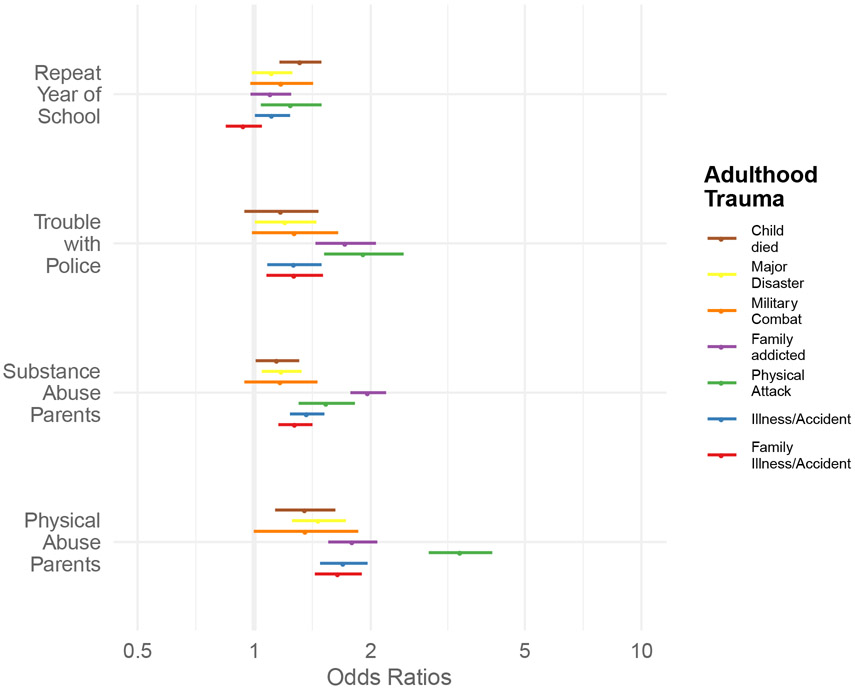
Assessing different types of CAs showed each event to be associated with cumulative ATEs independently (i.e., mutually adjusted; see Table 4). Physical abuse had the strongest association with cumulative ATEs, aRRR = 1.49, 95% CI [1.42, 1.57], followed by parental drug or alcohol problems, aRRR = 1.28, 95% CI [1.23, 1.33]; trouble with the police, a RRR = 1.25, 95% CI [1.18, 1.34]; and repeating a year of school, aRRR = 1.08, 95% CI [1.04, 1.13], after adjusting for age, gender, race/ethnicity, and parental educational attainment. Specific types of CA had distinct associations with specific ATEs; the association patterns can be seen in Table 4 and Figure 2. The largest effects were found in the association between physical abuse in childhood and adulthood physical attacks, aOR = 3.41, 95% CI [2.82, 4.12], and the association between parental substance abuse during childhood and a substance-addicted spouse, partner, or child later in life, aOR = 1.80, 95% CI [1.55, 2.08].
Figure 2. Associations Between Specific Types of Childhood Adversity and Specific Types of Adulthood Trauma Exposure.
Note. All analyses controlled for age, sex, race/ethnicity, and parental education. Error bars indicate 95% confidence intervals of the corresponding odds ratios.
Gender-Moderated Association Between CA and ATEs
To investigate gender-moderations, we added an interaction term of Gender x Cumulative CA into the previously described models; if this interaction term was significant (i.e., p < .05), we report herein on these specific findings from subsequent gender-stratification. Overall, we found higher adjusted relative risk ratios in women for the association between cumulative CA and cumulative ATEs: one type of CA, aRRR = 1.30, 95% CI [1.24, 1.36]; two types of CA, aRRR = 1.69 95% CI [1.56, 1.82]; three or four types of CA, aRRR = 2.10 95% CI [1.81, 2.42], compared to men: one types of CA, aRRR = 1.24 95% CI [1.17, 1.31]; two types of CA, aRRR = 1.57 95% CI [1.45, 1.70]; three or four types of CA, aRRR = 1.92 95% CI [1.71, 2.15]. Physical abuse was strongly associated with adulthood physical attacks overall, but the association was stronger in women compared to men, aOR = 3.91, 95% CI [3.10; 4.91] for women and aOR = 2.60, 95% CI [1.64; 3.08] for men. All models with Gender x CA interactions as well as the models from the gender-stratified analyses are reported in the Supplementary Materials (Supplementary Tables S5-S8, Supplementary Figures S1-S4). Most models that were used to investigate the association between CA and ATEs, however, were not moderated by gender (see Supplementary Materials).
Discussion
In this cross-sectional large-scale study of over 15,000 older adults, we found that more cumulative childhood adversity was associated with more cumulative adulthood trauma exposure across the life course. Exposure to three or more of the four categories of CA almost doubled an individual’s risk for experiencing an additional ATE compared to no CA exposure. We also observed that the association between cumulative CA and ATEs varied depending on the specific ATE assessed. The largest associations between CA and specific ATEs were observed for having a substance-addicted spouse or child and experiencing adulthood physical attack. Moreover, physical abuse in childhood was the strongest independent contributor to cumulative ATEs (mutually adjusted for other CA items) as well as for the specific ATE of a physical attack. Finally, these associations of cumulative CA and cumulative ATEs were moderated by gender, with CA more strongly associated with ATEs in women compared to men. With regard to specific stressors, cumulative childhood adversity was more strongly associated with physical attacks in women compared to men. However, most of the specific associations between CA and ATEs were not moderated by gender. These results emphasize the important role that CA may play in determining the pattern of life-course trauma exposure and highlight that associations between CA and ATEs are generally similar in men and women, with some important exceptions.
Our findings add to the current literature of large-scale and population-based studies that have found associations between early adversity and adulthood stressors and perceived distress, suggesting that CA might lead to circumstances that heighten the risk for later stressor exposure (Manyema et al., 2018; Nurius et al., 2015). Moreover, adult stressor exposure might then moderate or mediate the direct association between CA and psychological distress in young adulthood (Manyema et al., 2018) and in this way may lead to long-term adverse outcomes. Given that stressors in adulthood increase the risk for mental health problems, such as depression and suicide (Fowler et al., 2013; Jeon et al., 2014; Panagioti et al., 2009), as well as physical ill-health (e.g., poor health behaviors, inflammation, and telomere length; Lee & Park, 2018; Lin et al., 2016; Puterman et al., 2016), these findings are particularly important to disentangle.
We found parental physical abuse and parental substance abuse to be strongly associated with ATEs, particularly with regard to being physically attacked in adulthood and having a substance-abusing child or partner in later life. Previous findings have shown that adversities often co-occur and cluster in families and that these clusters of maladaptive family functioning are strongly related to the onset of mental disorders (Green et al., 2010; Kessler et al., 2010). A cohort study of over 80,000 Danish children born in 1966 showed that parental alcohol abuse was associated with multiple adverse outcomes, such as increased mortality, self-destructive behaviors, hospitalization due to violence, higher rates of teenage pregnancy, and unemployment (Christoffersen & Soothill, 2003). In fact, just under 50% of the participants in our analysis who reported physical abuse also reported parental substance abuse. The high rates of co-occurrence make it unsurprising that these types of CA were the two most strongly associated contributors to adulthood trauma exposure.
Our findings regarding gender differences in exposure to our subset of types of CA and ATEs support previous population-based studies that have reported that women have a lower cumulative incidence of potentially traumatic exposures than men (Breslau, 2002; Breslau et al., 1998; Hatch & Dohrenwend, 2007; Tolin & Foa, 2008). However, it is important to note that these overall differences are small compared to the differences in exposure between women and men for specific categories of traumatic experiences (Hatch & Dohrenwend, 2007; Tolin & Foa, 2008). Women in our study were much less likely than men to repeat a year of school or to have had trouble with the police, and they were slightly more likely to be physically abused. Beyond differences between genders with regard to CA and ATE exposure, we found that gender significantly moderated the association between cumulative CA and ATEs. Overall, our findings show that CA is related to ATEs for both men and women. However, the risk for women was slightly higher overall compared to men, particularly the risk of adulthood physical attacks for women who were physically abused in childhood.
From a theoretical point of view, our data are in line with both the early embedding and life-course stress theories. First, our data support life-course stress theories that state that inequality cumulates across a life course (Ferraro & Shippee, 2009; Ferraro et al., 2009; Pearlin et al., 2005; Schafer et al., 2011). In particular, our data indicate that individuals who experience CA are more likely to experience later trauma exposure. These associations in our sample extended even into old age. Unsurprisingly, the largest effects were found for the two types of CA that originated in the family, were interpersonal in nature, and often co-occurred (i.e., physical abuse and parental substance abuse). The effects observed for these exposures are consistent with the concept of revictimization, which states and supports the idea that early abuse and neglect are closely related to later revictimization (Widom et al., 2008). In particular, types of CA that are relatively more traumatic in nature, such as physical abuse, might influence social information processing (e.g., enhanced threat detection and hostile attribution biases), emotion processing (e.g., heightened reactivity with poor regulation), and accelerated aging (e.g., early pubertal timing and later cellular aging), which might, in turn, predict psychopathology (McLaughlin et al., 2020) and increase the risk for later exposure. In this sense, the adaption to unsafe and hostile environments, such as growing up with parental substance abuse, might cause social, emotional, and neurocognitive alterations that confer vulnerability (McCrory et al., 2017; McCrory & Viding, 2015). It is also possible that the effects of deprivation, neglect, and interpersonal adversities might occur by impairing attachment security (Fox et al., 2017; McLaughlin, 2016). Other sociological explanations might include lower SES, neighborhood stress, discrimination, and education, which might moderate and mediate the association between early and later exposure. Thus, there are diverse mechanisms by which CA may increase the risk of ATEs. Our findings add to the growing research that is uncovering important domains that can be leveraged in preventive strategies and interventions to target these specific mechanisms of interest (McLaughlin et al., 2019).
Our findings should be interpreted in light of several important limitations. First, differences in the prevalence rates of stressors, particularly those that occur in childhood, are common in the literature due to the use of different measures (Miller et al., 2011; Moffitt & Klaus-Grawe Think, 2013). The current study used a narrow measure of CA and ATEs, with only four items to assess CA and seven to assess ATEs. This measure lacked many important other exposure types, such as sexual abuse and neglect/deprivation. Future research might benefit from advanced methods of measuring childhood adversity that include more specific characteristics of these experiences, such as the timing, duration, and severity of the exposure (Crosswell & Lockwood, 2020; Slavich & Shields, 2018; Teicher & Parigger, 2015). Second, the present analyses were only cross-sectional, and the measures of trauma exposure were retrospective, with multiple decades between exposure and recall, which can lead to recall biases (Hardt & Rutter, 2004). A recent meta-analysis reported only a small overlap between prospective and retrospective assessments of adversity, which raises questions regarding the validity of retrospective assessments (Baldwin et al., 2019); however, the authors found a higher agreement for clear-cut forms of adversity. The potentially traumatic events analyzed in the present study had a high agreement over time as they mostly referred to distinct events; this was demonstrated by the high test–retest agreement we found for the four types of CA included in our measure. Third, sampling weights were not implemented; therefore, the findings are not true population-based estimates. Finally, studies that investigate older populations might find biased estimates due to methodological artifacts as selection effects (e.g., selective mortality and survivor effects) inherent to older populations, which might lead to underestimated trauma incidence among the oldest participants (Arrighi & Hertz-Picciotto, 1994; Bürgin et al., 2020; Heiss, 2011; Picciotto & Hertz-Picciotto, 2015; Zajacova & Burgard, 2013). Furthermore, varying prevalence rates for different traumatic exposures across certain age ranges in old age might be observed due to age, period, or cohort effects (Bürgin et al., 2020; Creamer & Parslow, 2008; Krause et al., 2004).
Our data indicate that CA and ATEs may be inextricably linked. Studies that consider the life-course effects of CA may need to consider ATEs as a potential contributor to any findings, and studies that consider the effects of ATEs need to consider that individuals who report more ATEs are likely to have experienced a larger burden of CA. In addition, a shared and clearer nosology and taxonomy of stressors in general, and of associations between CA and ATEs in particular, would lay the conceptual groundwork for future investigations (Epel et al., 2018; McLaughlin, 2016). Further, recent studies have analyzed life-course stressors using person-oriented approaches (e.g., latent class/profile/trajectory models; (Hajat, et al., 2020); these approaches or a combination of person- and item-oriented models might help disentangle exposure trajectories. Of further interest for future research are factors that moderate and mediate associations between CA and ATEs, such as adult SES, substance abuse, and attachment style. Another interesting topic that needs further investigation is the clustering of stressors and traumatic experiences within households and in couple dyads; such analyses are possible using HRS data (Crosswell et al., 2018) but were beyond the scope of the present study. Further, given the older age of the HRS population and the history of the military draft in the United States, future research might investigate differences in the relation between CA and military combat exposure in pre- versus postdraft cohorts. As CA was related to ATEs, our data provide additional evidence that early prevention and intervention should be a major priority for public health. In particular, cumulative CA, physical abuse, substance abuse by parents were strongly related to later ATEs. As stressful childhood experiences often cluster within families (Green et al., 2010; Kessler et al., 2010), programs aimed at improving family functioning and preventing parental substance abuse and physical abuse may be particularly beneficial.
The current study adds to existing evidence of the associations between CA and ATEs, extends these findings into older age, and suggests differences in the associations between specific types of exposure. Both men and women who have experienced multiple types of CA were shown to have increased odds for later ATEs; however, the effects were stronger for women. As CA is unequally distributed in the population and highly intertwined with later adversities, targeting the impact of CA at its roots is warranted. Safe childhoods confer lifelong benefits.
Supplementary Material
Figure 1. Associations Between Cumulative Childhood Adversity and Specific Types of Adulthood Traumatic Experiences.
Note. All analyses controlled for age, sex, race/ethnicity, and parental education. Error bars indicate 95% confidence intervals of the corresponding odds ratios.
Acknowledgments
The Health and Retirement Study is sponsored by the National Institute on Aging (U01AG009740) and is conducted by the University of Michigan. RAND HRS Detailed Imputations Files were developed at RAND with funding from the National Institute on Aging and the Social Security Administration. David Bürgin was supported by a Mobility Fellowship from the Dr. Betond Bonde Funds from the Freie Akademische Gesellschaft (FAG) Basel (Basel, Switzerland). Aoife O’Donovan was supported by a U.S. National Institute of Mental Health K01 Career Development Award (5K01MH109871).
Footnotes
Open Practices Statement
For this study, we analyzed archival data from the larger HRS that are not under our direct control; requests to access the data should be directed to the relevant archive. All datasets analyzed in this study are openly available and referenced within the manuscript. Data is accessible online after registration at https://hrspubs.sites.uofmhosting.net. Requests for the complete analysis scripts and code can be sent via email to the lead author at david.buergin@upk.ch.
References
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Dube SR, & Giles WH (2006). The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clin Neuroscience, 256(3), 174–186. 10.1007/s00406-005-0624-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrighi HM, & Hertz-Picciotto I (1994). The evolving concept of the healthy worker survivor effect. Epidemiology, 5(2), 189–196. https://10.1097/00001648-199403000-00009 [DOI] [PubMed] [Google Scholar]
- Baldwin JR, Reuben A, Newbury JB, & Danese A (2019). Agreement between prospective and retrospective measures of childhood maltreatment: A systematic review and meta-analysis. JAMA Psychiatry, 76(6), 584–593. 10.1001/jamapsychiatry.2019.0097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, Shahly V, Stein DJ, Petukhova M, Hill E, Alonso J, Atwoli L, Bunting B, Bruffaerts R, Caldas-de-Almeida JM, de Girolamo G, Florescu S, Gureje O, Huang Y, … Koenen KC (2016). The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychological Medicine, 46(2), 327–343. 10.1017/S0033291715001981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berens AE, Jensen SKG, & Nelson CA (2017). Biological embedding of childhood adversity: from physiological mechanisms to clinical implications. BMC medicine, 15(1), 135 10.1186/s12916-017-0895-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N (2002). Gender differences in trauma and posttraumatic stress disorder. Journal of Gender Specific Medicine, 5(1), 34–40. [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, & Andreski P (1998). Trauma and posttraumatic stress disorder in the community: The 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry, 55(7), 626–632. 10.1001/archpsyc.55.7.626 [DOI] [PubMed] [Google Scholar]
- Brown DW, Anda RF, Tiemeier H, Felitti VJ, Edwards VJ, Croft JB, & Giles WH (2009). Adverse childhood experiences and the risk of premature mortality. American Journal of Preventative Medicine, 37(5), 389–396. 10.1016/j.amepre.2009.06.021 [DOI] [PubMed] [Google Scholar]
- Bürgin D, Boonmann C, Schmid M, Tripp P, & O’Donovan A (2020). Fact or artifact? Childhood adversity and adulthood trauma in the U.S. population-based Health and Retirement Study. European Journal of Psychotraumatology, 11(1), 1721146 10.1080/20008198.2020.1721146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan BL, & Tottenham N (2016). The stress acceleration hypothesis: Effects of early-life adversity on emotion circuits and behavior. Current Opinion in Behavioral Sciences, 7, 76–81. 10.1016/j.cobeha.2015.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christoffersen MN, & Soothill K (2003). The long-term consequences of parental alcohol abuse: A cohort study of children in Denmark. Journal of Substance Abuse Treatment, 25(2), 107–116. 10.1016/s0740-5472(03)00116-8 [DOI] [PubMed] [Google Scholar]
- Clarke P, Fisher G, House J, Smith J, & Weir D (2008). Guide to content of the HRS psychosocial leave-behind participant lifestyle questionnaires: 2004 & 2006. University of Michigan; http://www-personal.umich.edu/~mkimball/keio/6.%20surveys/HRS2006LBQscale%20copy.pdf [Google Scholar]
- Clemens V, Huber-Lang M, Plener PL, Brahler E, Brown RC, & Fegert JM (2018). Association of child maltreatment subtypes and long-term physical health in a German representative sample. European Journal of Psychotraumatology, 9(1), 1510278 10.1080/20008198.2018.1510278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Keeler G, Angold A, & Costello EJ (2007). Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry, 64(5), 577–584. 10.1001/archpsyc.64.5.577 [DOI] [PubMed] [Google Scholar]
- Creamer M, & Parslow R (2008). Trauma exposure and posttraumatic stress disorder in the elderly: A community prevalence study. American Journal of Geriatric Psychiatry, 16(10), 853–856. 10.1097/01.JGP.0000310785.36837.85 [DOI] [PubMed] [Google Scholar]
- Crosswell AD, & Lockwood KG (2020). Best practices for stress measurement: How to measure psychological stress in health research. Health Psychology Open, 7(2), 2055102920933072. 10.1177/2055102920933072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosswell AD, Suresh M, Puterman E, Gruenewald T, Lee J, & Epel ES (2018). Advancing research on psychological stress and aging with the Health and Retirement Study: Looking back to launch the field forward. The Journals of Gerontology, 75(5), 970–980. 10.1093/geronb/gby106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, & Giles WH (2001). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the Adverse Childhood Experiences Study. JAMA, 286(24), 3089–3096. 10.1001/jama.286.24.3089 [DOI] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Giles WH, & Anda RF (2003). The impact of adverse childhood experiences on health problems: Evidence from four birth cohorts dating back to 1900. Preventative Medicine, 37(3), 268–277. 10.1016/s0091-7435(03)00123-3 [DOI] [PubMed] [Google Scholar]
- Dunn EC, Soare TW, Simpkin AJ, Suderman MJ, Zhu Y, Klengel T, Smith AD, Ressler K, & Relton CL (2018). Sensitive periods for the effect of childhood adversity on DNA methylation: Results from a prospective, longitudinal study. Biological Psychiatry, 85(10), 838–849. 10.1016/j.biopsych.2018.12.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epel ES, Crosswell AD, Mayer SE, Prather AA, Slavich GM, Puterman E, & Mendes WB (2018). More than a feeling: A unified view of stress measurement for population science. Frontiers in Neuroendocrinology, 49, 146–169. 10.1016/j.yfrne.2018.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventative Medicine, 14(4), 245–258. 10.1016/s0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Ferraro KF, & Shippee TP (2009). Aging and cumulative inequality: How does inequality get under the skin? Gerontologist, 49(3), 333–343. 10.1093/geront/gnp034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro KF, Shippee TP, & Schafer MH (2009). Cumulative inequality theory for research on aging and the life course In Bengston VL, Gans D, Pulney NM & Silversteinm M (Eds.), Handbook of theories of aging (pp. 413–433). Springer. [Google Scholar]
- Fisher GG, & Ryan LH (2018). Overview of the Health and Retirement Study and Introduction to the Special Issue. Work, Aging and Retirement, 4(1), 1–9. 10.1093/workar/wax032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler JC, Allen JG, Oldham JM, & Frueh BC (2013). Exposure to interpersonal trauma, attachment insecurity, and depression severity. Journal of Affective Disorders, 149(1–3), 313–318. 10.1016/j.jad.2013.01.045 [DOI] [PubMed] [Google Scholar]
- Fox NA, Nelson CA, & Zeanah CH (2017). The effects of psychosocial deprivation on attachment: Lessons from the Bucharest early intervention project. Psychodynamic Psychiatry, 45(4), 441–450. 10.1521/pdps.2017.45.4.441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2010). Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 67(2), 113–123. 10.1001/archgenpsychiatry.2009.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat A, Nurius P, & Song C (2020). Differing trajectories of adversity over the life course: Implications for adult health and well-being. Child Abuse and Neglect, 102, 104392 10.1016/j.chiabu.2020.104392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hambrick EP, Brawner TW, & Perry BD (2019). Timing of early-life stress and the development of brain-related capacities. Frontiers in Behavioral Neuroscience, 13, 183 10.3389/fnbeh.2019.00183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardt J, & Rutter M (2004). Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. Journal of Child Psychology and Psychiatry, 45(2), 260–273. 10.1111/j.1469-7610.2004.00218.x [DOI] [PubMed] [Google Scholar]
- Hatch SL, & Dohrenwend BP (2007). Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES, and age: A review of the research. American Journal of Community Psychology, 40(3–4), 313–332. 10.1007/s10464-007-9134-z [DOI] [PubMed] [Google Scholar]
- Health and Retirement Study. (2014a). 2006 HRS Core (Final) (v.3.0) public use dataset. University of Michigan. [Google Scholar]
- Health and Retirement Study. (2014b). 2008 HRS Core (Final) (v.3.0) public use dataset. University of Michigan. [Google Scholar]
- Health and Retirement Study. (2017a). 2010 HRS Core (Final) (v.5.1) public use dataset. [Google Scholar]
- Health and Retirement Study. (2017b). 2012 HRS Core (Final) (v.2.0) public use dataset. University of Michigan. [Google Scholar]
- Health and Retirement Study. (2017c). Sample sizes and response rates. Survey Research Center, Institute for Social Research, University of Michigan; https://hrs.isr.umich.edu/sites/default/files/biblio/ResponseRates_2017.pdf [Google Scholar]
- Heim C, Shugart M, Craighead WE, & Nemeroff CB (2010). Neurobiological and psychiatric consequences of child abuse and neglect. Developmental Psychobiology, 52(7), 671–690. 10.1002/dev.20494 [DOI] [PubMed] [Google Scholar]
- Heiss F (2011). Dynamics of self-rated health and selective mortality. Empirical Economics, 40(1), 119–140. 10.1007/s00181-010-0422-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussey JM, Chang JJ, & Kotch JB (2006). Child maltreatment in the United States: Prevalence, risk factors, and adolescent health consequences. Pediatrics, 118(3), 933–942. 10.1542/peds.2005-2452 [DOI] [PubMed] [Google Scholar]
- Jeon HJ, Park J-I, Fava M, Mischoulon D, Sohn JH, Seong S, Park JE, Yoo I, & Cho MJ (2014). Feelings of worthlessness, traumatic experience, and their comorbidity in relation to lifetime suicide attempt in community adults with major depressive disorder. Journal of Affective Disorders, 166, 206–212. 10.1016/j.jad.2014.05.010 [DOI] [PubMed] [Google Scholar]
- Johnson J, Chaudieu I, Ritchie K, Scali J, Ancelin M-L, & Ryan J (2020). The extent to which childhood adversity and recent stress influence all-cause mortality risk in older adults. Psychoneuroendocrinology, 111, 104492 10.1016/j.psyneuen.2019.104492 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, Degenhardt L, de Girolamo G, Dinolova RV, Ferry F, Florescu S, Gureje O, Haro JM, Huang Y, Karam EG, Kawakami N, Lee S, Lepine J-P, Levinson, … Koenen KC (2017). Trauma and PTSD in the WHO World Mental Health Surveys. European Journal of Psychotraumatology, 8(sup5), 1353383 10.1080/20008198.2017.1353383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Aguilar-Gaxiola S, Alhamzawi AO, Alonso J, Angermeyer M, Benjet C, Bromet E, Chatterji S, de Girolamo G, Demyttenaere K, Fayyad J, Florescu S, Gal G, Gureje O, Haro JM, … Williams DR (2010). Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. British Journal of Psychiatry, 197(5), 378–385. 10.1192/bjp.bp.110.080499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26(5), 537–547. 10.1002/jts.21848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolb B, & Gibb R (2014). Searching for the principles of brain plasticity and behavior. Cortex, 58, 251–260. 10.1016/j.cortex.2013.11.012 [DOI] [PubMed] [Google Scholar]
- Krause N, Shaw BA, & Cairney J (2004). A descriptive epidemiology of lifetime trauma and the physical health status of older adults. Psychology of Aging, 19(4), 637–648. 10.1037/0882-7974.19.4.637 [DOI] [PubMed] [Google Scholar]
- Lee SY, & Park CL (2018). Trauma exposure, posttraumatic stress, and preventive health behaviours: A systematic review. Health Psychology Review, 12(1), 75–109. 10.1080/17437199.2017.1373030 [DOI] [PubMed] [Google Scholar]
- Lin JE, Neylan TC, Epel E, & O'Donovan A (2016). Associations of childhood adversity and adulthood trauma with C-reactive protein: A cross-sectional population-based study. Brain, Behavior, and Immunity, 53, 105–112. 10.1016/j.bbi.2015.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan-Greene P, Green S, Nurius PS, & Longhi D (2014). Distinct contributions of adverse childhood experiences and resilience resources: A cohort analysis of adult physical and mental health. Social Work in Health Care, 53(8), 776–797. 10.1080/00981389.2014.944251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lüdecke D (2018). sjPlot: Data visualization for statistics in social science: R package (Version 2.6.2.9000). 10.5281/zenodo.1308157 [DOI] [Google Scholar]
- Manyema M, Norris SA, & Richter LM (2018). Stress begets stress: The association of adverse childhood experiences with psychological distress in the presence of adult life stress. BMC Public Health, 18(1), 835 10.1186/s12889-018-5767-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrory EJ, Gerin MI, & Viding E (2017). Annual research review: Childhood maltreatment, latent vulnerability, and the shift to preventative psychiatry—the contribution of functional brain imaging. Journal of Child Psychology and Psychiatry, 58(4), 338–357. 10.1111/jcpp.12713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrory EJ, & Viding E (2015). The theory of latent vulnerability: Reconceptualizing the link between childhood maltreatment and psychiatric disorder. Development and Psychopathology, 27(2), 493–505. 10.1017/S0954579415000115 [DOI] [PubMed] [Google Scholar]
- McLaughlin KA (2016). Future directions in childhood adversity and youth psychopathology. Journal of Clinical Child and Adolescent Psychology, 45(3), 361–382. 10.1080/15374416.2015.1110823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Colich NL, Rodman AM, & Weissman DG (2020). Mechanisms linking childhood trauma exposure and psychopathology: A transdiagnostic model of risk and resilience. BMC Medicine, 18(1), 96 10.1186/s12916-020-01561-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, DeCross SN, Jovanovic T, & Tottenham N (2019). Mechanisms linking childhood adversity with psychopathology: Learning as an intervention target. Behaviour Research and Therapy, 118, 101–109. 10.1016/j.brat.2019.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, & Parker KJ (2011). Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin, 137(6), 959–997. 10.1037/a0024768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, & Klaus-Grawe Think T (2013). Childhood exposure to violence and lifelong health: Clinical intervention science and stress-biology research join forces. Developmental Psychopathology, 25(402), 1619–1634. 10.1017/S0954579413000801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH (1992). Epidemiology of trauma: Frequency and impact of different potentially traumatic events on different demographic groups. Journal of Consulting and Clinical Psychology, 60(3), 409–418. 10.1037/0022-006X.60.3.409 [DOI] [PubMed] [Google Scholar]
- Nurius PS, Green S, Logan-Greene P, & Borja S (2015). Life-course pathways of adverse childhood experiences toward adult psychological well-being: A stress process analysis. Child Abuse and Neglect, 45, 143–153. 10.1016/j.chiabu.2015.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donovan A, Cohen BE, Seal KH, Bertenthal D, Margaretten M, Nishimi K, & Neylan TC (2015). Elevated risk for autoimmune disorders in Iraq and Afghanistan veterans with posttraumatic stress disorder. Biological Psychiatry, 77(4), 365–374. 10.1016/j.biopsych.2014.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff M (2017). Sex and gender differences in post-traumatic stress disorder: An update. European Journal of Psychotraumatology, 8(sup4), 1351204 10.1080/20008198.2017.1351204 [DOI] [Google Scholar]
- Panagioti M, Gooding P, & Tarrier N (2009). Post-traumatic stress disorder and suicidal behavior: A narrative review. Clinical Psychology Review, 29(6), 471–482. 10.1016/j.cpr.2009.05.001 [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schieman S, Fazio EM, & Meersman SC (2005). Stress, health, and the life course: Some conceptual perspectives. Journal of Health and Social Behavior, 46(2), 205–219. 10.1177/002214650504600206 [DOI] [PubMed] [Google Scholar]
- Picciotto S, & Hertz-Picciotto I (2015). Commentary: Healthy worker survivor bias: A still-evolving concept. Epidemiology, 26(2), 213–215. 10.1097/EDE.0000000000000233 [DOI] [PubMed] [Google Scholar]
- Puterman E, Gemmill A, Karasek D, Weir D, Adler NE, Prather AA, & Epel ES (2016). Lifespan adversity and later adulthood telomere length in the nationally representative U.S. Health and Retirement Study. Proceedings of the National Academy of Sciences of the United States of America, 113(42), E6335–E6342. 10.1073/pnas.1525602113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puterman E, Weiss J, Hives BA, Gemmill A, Karasek D, Mendes WB, & Rehkopf DH (2020). Predicting mortality from 57 economic, behavioral, social, and psychological factors. Proceedings of the National Academy of Sciences of the United States of America, 117(28), 16273–16282. 10.1073/pnas.1918455117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- RAND. (2018). HRS detailed imputations file 2014 (V2). https://www.rand.org/well-being/social-and-behavioral-policy/centers/aging/dataprod/income-wealth-imputation.html
- Riedl D, Beck T, Exenberger S, Daniels J, Dejaco D, Unterberger I, & Lampe A (2019). Violence from childhood to adulthood: The influence of child victimization and domestic violence on physical health in later life. Journal of Psychosomatic Research, 116, 68–74. 10.1016/j.jpsychores.2018.11.019 [DOI] [PubMed] [Google Scholar]
- RStudio Team. (2016). RStudio: Integrated development for R. http://www.rstudio.com/
- Schafer MH, Ferraro KF, & Mustillo SA (2011). Children of misfortune: Early adversity and cumulative inequality in perceived life trajectories. American Journal of Sociology, 116(4), 1053–1091. 10.1086/655760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, & Shields GS (2018). Assessing lifetime stress exposure using the Stress and Adversity Inventory for Adults (Adult STRAIN): An overview and initial validation. Psychosomatic Medicine, 80(1), 17–27. 10.1097/PSY.0000000000000534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J, Ryan LH, Sonnega A, & Weir DR (2017). Psychosocial and lifestyle questionnaire 2006–2016. Survey Research Center, Institute for Social Research; https://hrs.isr.umich.edu/sites/default/files/biblio/HRS%202006-2016%20SAQ%20Documentation_07.06.17_0.pdf. [Google Scholar]
- Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, & Weir DR (2014). Cohort profile: The Health and Retirement Study (HRS). International Journal of Epidemiology, 43(2), 576–585. 10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szyf M, & Bick J (2013). DNA methylation: A mechanism for embedding early life experiences in the genome. Child Development, 84(1), 49–57. 10.1111/j.1467-8624.2012.01793.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, & Parigger A (2015). The Maltreatment and Abuse Chronology of Exposure (MACE) scale for the retrospective assessment of abuse and neglect during development. PLoS One, 10(2), e0117423 10.1371/journal.pone.0117423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolin DF, & Foa EB (2008). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Trauma: Theory, Research, Practice, and Policy, S(1), 37–85. 10.1037/1942-9681.S.1.37 [DOI] [PubMed] [Google Scholar]
- Wickham H (2016). ggplot2: elegant graphics for data analysis. Springer. [Google Scholar]
- Widom CS, Czaja SJ, & Dutton MA (2008). Childhood victimization and lifetime revictimization. Child Abuse and Neglect, 32(8), 785–796. 10.1016/j.chiabu.2007.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajacova A, & Burgard SA (2013). Healthier, wealthier, and wiser: A demonstration of compositional changes in aging cohorts due to selective mortality. Population Research and Policy Review, 32(3), 311–324. 10.1007/s11113-013-9273-x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.