Abstract
Background:
Preeclampsia is one of the leading causes of maternal mortality in the United States. It disproportionately affects non-Hispanic Black (NHB) women, but little is known about how preeclampsia and other cardiovascular disease (CVD) risk factors vary among different subpopulations of NHB women in the US. We investigated the prevalence of preeclampsia by nativity (US- vs. foreign-born) and duration of US residence among NHB women.
Methods:
We analyzed cross-sectional data from the Boston Birth Cohort (1998–2016), with a focus on NHB women. We performed multivariable logistic regression to investigate associations between preeclampsia, nativity and duration of US residence after controlling for potential confounders.
Results:
Of 2,697 NHB women, 40.5% were foreign-born. Relative to them, US-born NHB women were younger, in higher percentage current smokers, had higher prevalence of obesity (BMI≥ 30Kg/m2) and maternal stress, but lower educational level. The age-adjusted prevalence of preeclampsia was 12.4% and 9.1% among US-born and foreign-born women respectively. When further categorized by duration of US residence, the prevalence of all studied CVD risk factors except for diabetes, was lower among foreign-born NHB women with <10 vs. ≥10 years of US residence. Additionally, the odds of preeclampsia in foreign-born NHB women with duration of US residence <10 years was 37% lower than in US-born NHB women. In contrast, the odds of preeclampsia in foreign-born NHB women with duration of US residence ≥10 years was not significantly different from that of US-born NHB women after adjusting for potential confounders.
Conclusions:
The prevalence of preeclampsia and other CVD risk factors is lower in foreign-born than US-born NHB women. The “healthy immigrant effect”, which typically results in health advantages for foreign-born women, appears to wane with longer duration of US residence (≥ 10 years). Further research is needed to better understand these associations.
Keywords: Preeclampsia, Health Disparities, Cardiovascular Diseases, Nativity, non-Hispanic Blacks
Subject Terms: Race and Ethnicity, Risk Factors, Women, Preeclampsia
INTRODUCTION
Background:
Preeclampsia is among the leading causes of maternal mortality in the United States (US) and continues to be a major cause of maternal and fetal morbidity.1 Its incidence is increasing, and currently, it affects approximately 5% of all pregnancies in the US,2 with wide variations based on race, ethnicity and pre-existing cardio-metabolic risk factors.3 Preeclampsia can lead to serious maternal complications such as eclampsia, stroke, and multiple organ failure.4,5 Importantly it has been identified as among the most preventable causes of maternal morbidity and mortality.6 The 2019 ACC/AHA Cardiovascular disease (CVD) Prevention Guidelines recognizes preeclampsia as a sex specific risk enhancing factor for subsequent cardiovascular and cerebrovascular disease in women.7 Women with a history of preeclampsia have an increased risk of chronic hypertension, ischemic heart disease, heart failure, premature vascular aging, and stroke compared to women with normotensive pregnancies.8–10 Given the rising US incidence, and effects on pregnancy morbidity and mortality and long term cardiovascular health, preeclampsia represents a significant public health concern.11
Studies have documented a higher risk of preeclampsia, other forms of pregnancy related hypertension, and CVD among non-Hispanic Black (NHB) women in the US compared to their non-Hispanic White (NHW) counterparts.12–17 Not only are NHB women disproportionately affected by preeclampsia, they are also more likely to die from its complications than NHW women.18–20 There is considerable heterogeneity in the NHB population in the US based on nativity, immigration status, and other socio-economic measures.21 Yet most studies that investigated these disparities in preeclampsia and related outcomes have examined NHB women as a homogenous group, with little attention to nativity. Two factors by which NHB women differ are nativity or place of birth (foreign- vs US-born) and the duration of US residence among foreign-born NHB women. Duration of US residence has been used as a proxy for acculturation in previous studies.22,23 Variations may exist in the risks of preeclampsia, CVD risk factors and adverse pregnancy outcomes between NHB women based on these two factors.
Although immigrants are often considered a vulnerable population and at higher risk of adverse health outcomes, several studies have reported a paradox: immigrant (foreign-born) women tend to have better reproductive health outcomes compared to their US-born counterparts, despite poorer socioeconomic profiles.24–26 This has previously been demonstrated in the rate of preterm births and small-for-gestational-age (SGA) among NHB women by maternal nativity.27 This epidemiologic paradox has been attributed to the selective immigration of healthy and educated immigrants into their host country (healthy immigrant effect) and the protective cultural norms of immigrants.28,29 There is also evidence that this foreign-born advantage may wane with acculturation to the host country.25,30 Among NHB women residing in the US, little is known about nativity related disparities in the prevalence of preeclampsia. Further, the impact of duration of US residence—a proxy of acculturation- has not been well investigated in association with preeclampsia among NHB women. With 13.5% of the US population being foreign-born (2016)31 and the growing immigrant population in the US, it is important that these differences in risks are explored to understand how immigration status and duration of residence in the US affect the risk of preeclampsia among NHB women.
Objective:
In this study, we explored the prevalence of preeclampsia among NHB women, focusing specifically on preeclampsia prevalence among the subgroups defined by nativity and duration of US residence, while controlling for other known risk factors.
METHODS
Data Source and Study Design:
Data from the Boston Birth Cohort (BBC) were utilized for this study and it is available on request from the Johns Hopkins Center on the Early Life Origins of Diseases.32 This study is a secondary data analysis exploring the associations between maternal nativity, duration of US residence, and prevalence of preeclampsia and associated CVD risk factors among NHB women in the US. We used the 1998–2016 data from the BBC with 8,509 mother-baby dyads recruited at Boston Medical Center (BMC), which serves a predominantly low-income, minority, inner-city patient population. The BBC was started in 1998 with an initial case-control design to study the determinants of low birthweight and preterm births. A case of preterm birth or low birthweight was matched to 2 age- and ethnicity-matched controls (term birth with normal birthweight). The cohort has particular focus on the interaction of environmental factors and genetic variants in adverse reproductive outcomes such as preterm births, pregnancy complications, and pediatric health problems.33 Mothers who delivered live singleton births at the BMC (from 1998–2016) were recruited within 24–72 hours after delivery and included in the cohort after they had given a written informed consent. Multiple gestations, pregnancies resulting from in vitro fertilization, neonates with chromosomal abnormalities, and major birth defects were excluded.33,34 After informed consent was obtained, standardized questionnaire interview was conducted to obtain sociodemographic data (including place of birth and length in the US), and maternal and infant electronic medical records (EMR) were reviewed to obtain clinical data on birth outcomes and pregnancy complications including preeclampsia.34 The BBC was approved by the Institutional Review Board (IRB) of Boston University Medical Center and the IRB of Johns Hopkins Bloomberg School of Public Health. This current study did not require review by an IRB since it used de-identified data from the BBC.
This study focused on data from 2,760 women of the BBC who self-reported as NHB. Of these, 2,697 had data on the main outcome of interest (preeclampsia) and their place of birth, with 1,606 (59.5%) being US-born and 1,091 (40.5%) foreign-born. Among foreign-born NHB women, only 766 had data on duration of residence in the US; thus, a total of 325 foreign-born NHB women missing this information were excluded from the analysis of the prevalence of preeclampsia by duration of US residence. (Figure 1).
Figure 1:
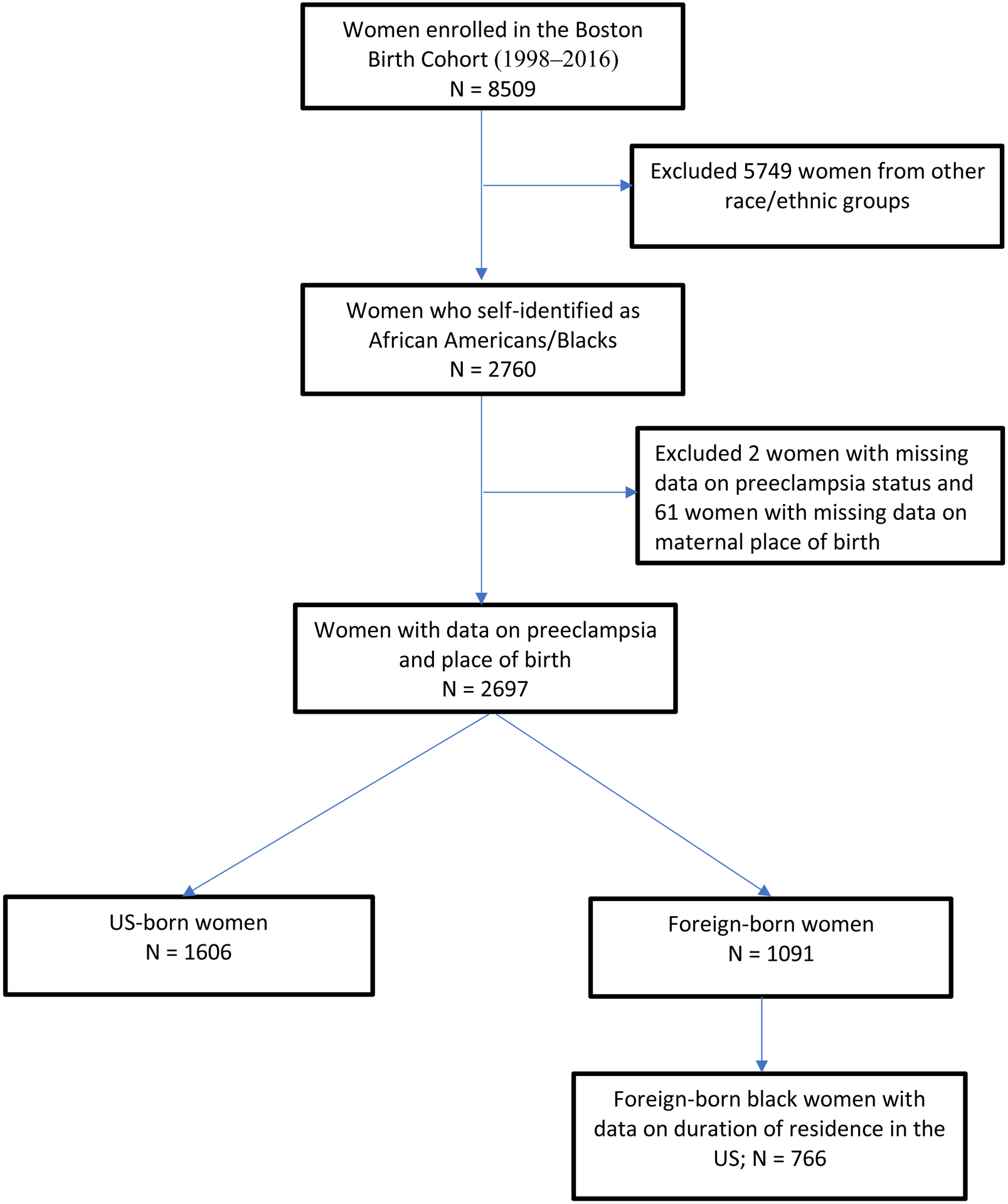
Flowchart of analytic population
Variables:
The BBC includes information on maternal race/ethnicity, place of birth, sociodemographic characteristics, and traditional risk factors of preeclampsia and other adverse pregnancy and birth outcomes. Self-reported maternal sociodemographic characteristics included maternal age at delivery (<20, 20–34 or ≥35 years); parity (0, 1 or 2+); and maternal education (secondary school or less, GED/High School graduate or college education/degree). Also available were data on other risk factors for preeclampsia including self-reported maternal perceived stress (mild, moderate, or severe), smoking in pregnancy (yes/no), history of hypertension (yes/no), diabetes (none, gestational and chronic) and body mass index (BMI <25, 25.0–29.9 and ≥30 kg/m2). Chronic hypertension, chronic and gestational diabetes mellitus status were based on physician diagnosis as documented in the EMR. BMI was calculated from self-reported weight and height.
Persons who were born in any of the 50 US states, the District of Columbia and other US territories were considered US-born, and those born outside these regions were considered foreign-born. Duration of U.S residence was defined as the number of years between immigration into the U.S and the index pregnancy and was categorized as <10 years or ≥ 10 years. The cutoff of 10 years was used as persons residing in the US for ≥10 years are regarded as having higher acculturation and those residing <10 years as having lower acculturation.35
The primary outcome of interest in this study was preeclampsia. Clinical diagnosis of preeclampsia in the index pregnancy was obtained from the mothers’ medical records using ICD-9 or 10 code, diagnosis name, or keyword. Preeclampsia was defined according to the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy, as systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg on at least two occasions, and proteinuria ≥1+ on at least two occasions after 20 weeks’ gestation. For women with chronic hypertension, worsening hypertension (SBP≥160 mmHg or DBP ≥110 mmHg) was required for the diagnosis of preeclampsia to be met.36 For analysis purposes, we grouped all women with preeclampsia, eclampsia, and HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome into one “preeclampsia” group.
Statistical Methods:
We used Pearson’s chi squared and Fischer exact tests to explore the differences in maternal sociodemographic and medical risk factors by maternal place of birth and duration of US residence. A missing category was included for variables with >1% missing values, and this included BMI and maternal education. Logistic regression analysis with nested models was used to obtain unadjusted and adjusted prevalence odds ratios (aPOR) of preeclampsia by maternal nativity as well as by duration of US residence. Model 1 was unadjusted; Model 2 was age-adjusted; Model 3 was adjusted for maternal age, hypertension, parity, BMI, diabetes, education, smoking and general stress. Predictive margins were used to obtain the adjusted proportion and marginal effects for the models. To examine whether the duration of US residence was associated with the risk of preeclampsia for foreign-born women, we stratified the women into those with duration of residence <10 years and those with ≥10 years of US residence. Results were considered statistically significant at p ≤0.05. Stata version 14.2 was used for all statistical analyses in this study.
RESULTS
The study sample comprised of 1,606 (59.5%) US-born and 1,091 (40.5%) foreign-born NHB women. For the foreign-born population, 42.4% was from the Caribbean, 36.3% from Sub-Saharan Africa, and 21.3% from other regions. The overall prevalence of preeclampsia was 11.1% in this study sample.
Sociodemographic and Cardiovascular Risk Factors by Maternal Place of Birth
There were significant differences between several CVD risk factors and baseline characteristics between the two groups [Table 1]. Compared to US-born women, more foreign-born women were older (>34 years) at time of delivery (21.0% vs 10.3%; p<0.001) and less foreign-born women were younger (<20 years) at the time of delivery (7.4% vs 18.6%; p<0.001). Although foreign-born women were more likely to be overweight, US-born women had a higher prevalence of obesity (≥30 kg/m2) (27.6% vs 19.6%; p<0.001) and chronic diabetes (4.1% vs 3.8%; p<0.001) compared to the foreign-born women. However, the foreign-born women were more likely to have gestational diabetes mellitus (GDM) as compared to US-born women (7.3% vs 4.9%; p<0.001). In terms of high-risk behaviors for CVD, US-born women had a significantly higher prevalence of smoking in pregnancy (20.5% vs 4.9%; p<0.001) compared to the foreign-born women. Maternal stress and education levels were also significantly different between the two groups. US-born women reported more moderate or severe stress during pregnancy than foreign-born women (74.3% vs 60.3%; p<0.001); they were also more likely to have lower levels of education (66.3% vs. 53.6% without college degree; p<0.001). Interestingly, the prevalence of pre-existing hypertension did not differ significantly between US- and foreign-born women (7.8% vs 7.2%, p=0.601)
Table 1:
Comparison of Maternal Characteristics by Maternal Place of Birth among Non-Hispanic Black Women in the Boston Birth Cohort (1998–2016)
| Maternal characteristics | Total n = 2697 (%) | US-born n = 1606 (%) | Foreign-born n = 1091 (%) | p-value |
|---|---|---|---|---|
| Maternal Age at Delivery (years) | <0.001 | |||
| <20 | 380(14.1) | 299(18.6) | 81(7.4) | |
| 20–34 | 1923(71.3) | 1142(71.1) | 781(71.6) | |
| >34 | 394(14.6) | 165(10.3) | 229(21.0) | |
| Parity | 0.065 | |||
| 0 | 1114(41.3) | 681(42.4) | 433(39.7) | |
| 1 | 762(28.3) | 427(26.6) | 335(30.7) | |
| 2+ | 821(30.4) | 498(31.0) | 323(29.6) | |
| Chronic Hypertension | 0.601 | |||
| No | 2493(92.4) | 1481(92.2) | 1012(92.8) | |
| Yes | 204(7.6) | 125(7.8) | 79(7.2) | |
| BMI (kg/m2) | <0.001 | |||
| <25 | 1176(43.6) | 694(43.2) | 482(44.2) | |
| 25.0–29.9 | 744(27.6) | 418(26.0) | 326(29.9) | |
| ≥30 | 657(24.4) | 443(27.6) | 214(19.6) | |
| Missing | 120(4.4) | 51(3.2) | 69(6.3) | |
| Diabetes Mellitus | 0.025 | |||
| No | 2431(90.1) | 1461(91.0) | 970(88.9) | |
| Gestational | 158(5.9) | 78(4.9) | 80(7.3) | |
| Chronic Diabetes | 108(4.0) | 67(4.1) | 41(3.8) | |
| Smoking in index pregnancy | <0.001 | |||
| No | 2314(85.8) | 1276(79.5) | 1038(95.1) | |
| Yes | 383(14.2) | 330(20.5) | 53(4.9) | |
| Maternal stress (general) | <0.001 | |||
| mild | 846(31.4) | 413(25.7) | 433(39.7) | |
| moderate | 1500(55.6) | 962(59.9) | 538(49.3) | |
| severe | 351(13.0) | 231(14.4) | 120(11.0) | |
| Maternal Education | <0.001 | |||
| Secondary School or Less | 640(23.7) | 433(27.0) | 207(19.0) | |
| GED/High School Graduate | 1008(37.4) | 631(39.3) | 377(34.6) | |
| College Education/Degree | 993(36.8) | 509(31.7) | 484(44.4) | |
| Missing | 56(2.1) | 33(2.0) | 23(2.0) |
BMI – Body Mass Index
GED – General Education Development
Prevalence of Preeclampsia by Maternal Place of Birth
The age-adjusted prevalence of preeclampsia was 12.4% and 9.1% in US-born and foreign-born women, respectively [Figure 2]. Foreign-born NHB women had 27% lower odds of preeclampsia compared to US-born NHB women after adjusting for maternal age, hypertension, parity, smoking, BMI, diabetes, education, and general stress (OR=0.73 CI 0.55–0.97) [Table 2].
Figure 2:
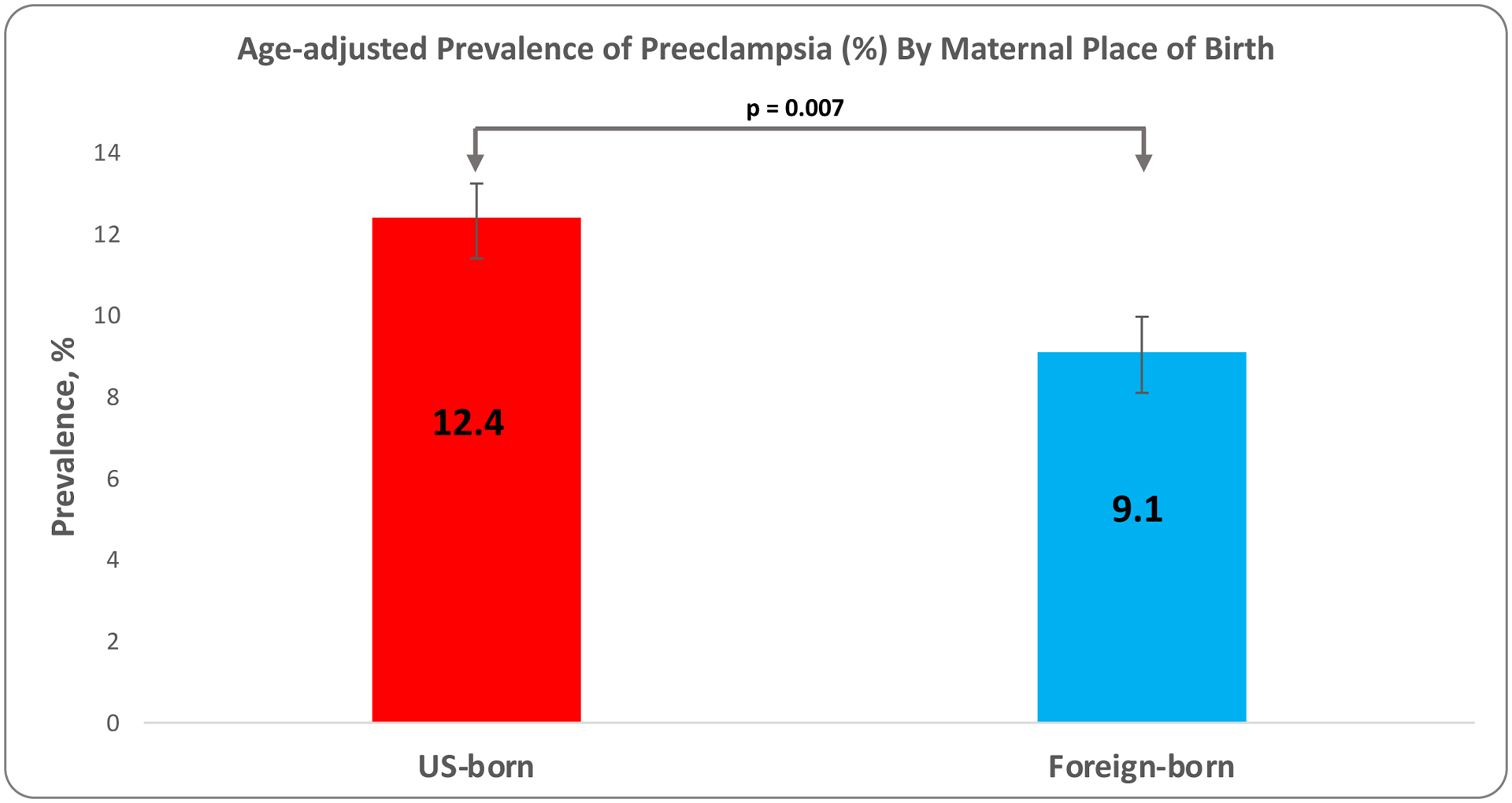
Age-adjusted prevalence of preeclampsia by maternal place of birth
Table 2:
Crude and Adjusted Odds Ratios with 95 % Confidence Intervals for Association between Preeclampsia and Maternal Place of Birth among Non-Hispanic Black Women in the Boston Birth Cohort (1998–2016)
| Maternal place of birth | N | % preeclampsia | OR and 95% CI for Preeclampsia | |||||
|---|---|---|---|---|---|---|---|---|
| Model 1 n = 2697 | p-value | Model 2 n = 2697 | p-value | Model 3 n = 2697 | p-value | |||
| US-born | 1606 | 12.20 | REF | REF | REF | |||
| Foreign-born | 1091 | 9.35 | 0.74 [0.58 – 0.96] | 0.021 | 0.70 [0.54 – 0.91] | 0.007 | 0.73[0.55–0.97] | 0.031 |
| Model 1: Unadjusted Model 2: Age-adjusted Model 3: Model 2 + hypertension, parity, BMI, diabetes, education, smoking and general stress | ||||||||
OR – Odds Ratio
CI – Confidence Interval
Sociodemographic and Cardiovascular Risk Factors by Duration of US Residence
The distribution of CVD risk factors differed with the number of years of US residence for foreign-born NHB women [Table 3]. The prevalence of obesity was highest among US-born NHB women, followed by foreign-born women with ≥10 years of residence, and much lower in foreign-born with <10 years of residence (27.6% vs 23.3% vs 17.1%, respectively; p<0.001). In terms of high-risk behaviors, the US-born NHB women had the highest prevalence of smoking in pregnancy, followed by foreign-born women with ≥10 and <10 years of US residence (20.5% vs 3.1% vs 1.7%, respectively; p<0.001). The prevalence of chronic diabetes was highest in foreign-born women with <10 years of residence than in those with ≥10 years of residence and US-born women (4.3% vs 3.5% vs 4.1%, respectively; marginally significant at p=0.074). A similar pattern was observed with gestational diabetes, but with US-born women having the least prevalence (8.1% vs 6.2% vs 4.9%, respectively; marginally significant at p=0.074). Maternal stress and education level were also unfavorable for US-born women. Reports of moderate or severe stress were highest in US-born NHB women, followed by foreign-born NHB women with ≥10 and <10 years of US residence and (74.3% vs 70.9% vs 49.5%, respectively; p<0.001). They were also most likely to have lower level of education (66.3% vs 51.6% vs 53.2% without college degree; p<0.001) compared to their foreign-born counterparts with ≥10 and <10 years of US residence, respectively.
Table 3:
Comparison of Maternal Characteristics by Duration of Residence among Non-Hispanic Black Women in the Boston Birth Cohort (1998–2016)
| Maternal characteristics | Total n = 2372 (%) | US-born n = 1606 (%) | Foreign-born with <10 years n = 539 | Foreign-born with ≥10 years n = 227 | p-value |
|---|---|---|---|---|---|
| Maternal Age at Delivery (years) | <0.001 | ||||
| <20 | 338(14.3) | 299(18.6) | 18(3.3) | 21(9.2) | |
| 20–34 | 1698(71.6) | 1142(71.1) | 408(75.7) | 148(65.2) | |
| >34 | 336(14.2) | 165(10.3) | 113(21.0) | 58(25.6) | |
| Parity | 0.007 | ||||
| 0 | 993(41.9) | 681(42.4) | 233(43.2) | 79(34.8) | |
| 1 | 667(28.1) | 427(26.6) | 171(31.7) | 69(30.4) | |
| 2+ | 712(30.0) | 498(31.0) | 135(25.1) | 79(34.8) | |
| Chronic Hypertension | 0.460 | ||||
| No | 2187(92.2) | 1481(92.2) | 501(92.9) | 205(90.3) | |
| Yes | 185(7.8 | 125(7.8) | 38(7.1) | 22(9.7) | |
| BMI (kg/m2) | <0.001 | ||||
| <25 | 1031(43.5) | 694(43.2) | 234(43.4) | 103(45.4) | |
| 25.0–29.9 | 652(27.5) | 418(26.0) | 170(31.5) | 64(28.2) | |
| ≥30 | 588(24.8) | 443(27.6) | 92(17.1) | 53(23.3) | |
| Missing | 101(4.2) | 51(3.2) | 43(8.0) | 7(3.1) | |
| Diabetes Mellitus | 0.074 | ||||
| No | 2138(90.1) | 1461(91.0) | 472(87.6) | 205(90.3) | |
| Gestational | 136(5.8) | 78(4.9) | 44(8.1) | 14(6.2) | |
| Chronic Diabetes | 98(4.1) | 67(4.1) | 23(4.3) | 8(3.5) | |
| Smoking in index pregnancy | <0.001 | ||||
| No | 2026(85.4) | 1276(79.5) | 530(98.3) | 220(96.9) | |
| Yes | 346(14.6) | 330(20.5) | 9(1.7) | 7(3.1) | |
| Maternal stress (general) | |||||
| mild | 751(31.7) | 413(25.7) | 272(50.5) | 66(29.1) | |
| moderate | 1316(55.5) | 962(59.9) | 220(40.8) | 134(59.0) | <0.001 |
| severe | 305(12.8) | 231(14.4) | 47(8.7) | 27(11.9) | |
| Maternal Education | |||||
| Secondary School or Less | 567(23.9) | 433(27.0) | 100(18.5) | 34(15.0) | <0.001 |
| GED/High School Graduate | 901(38.0) | 631(39.3) | 187(34.7) | 83(36.6) | |
| College Education/Degree | 869(36.6) | 509(31.7) | 250(46.4) | 110(48.4) | |
| Missing | 35(1.5) | 33(2.0) | 2(0.4) | 0(0.00) |
BMI – Body Mass Index
GED – General Education Development
Prevalence of Preeclampsia by Duration of U.S Residence
Preeclampsia prevalence was highest in the US-born NHB women when compared to foreign-born irrespective of the number of years of US residence. The age-adjusted prevalence of preeclampsia among NHB US-born, foreign-born with ≥10 years of residence and foreign-born with <10 years of residence was 12.4%, 8.8% and 8.2% respectively [Figure 3]. In the fully adjusted model, the odds of preeclampsia in foreign-born NHB women with duration of US residence <10 years was 37% lower than in US-born NHB women (OR = 0.63; CI 0.43–0.92). In contrast, the odds of preeclampsia in foreign-born NHB women with duration of US residence ≥10 years was not significantly different from that of US-born Black women after adjusting for potential confounders [Table 4].
Figure 3:
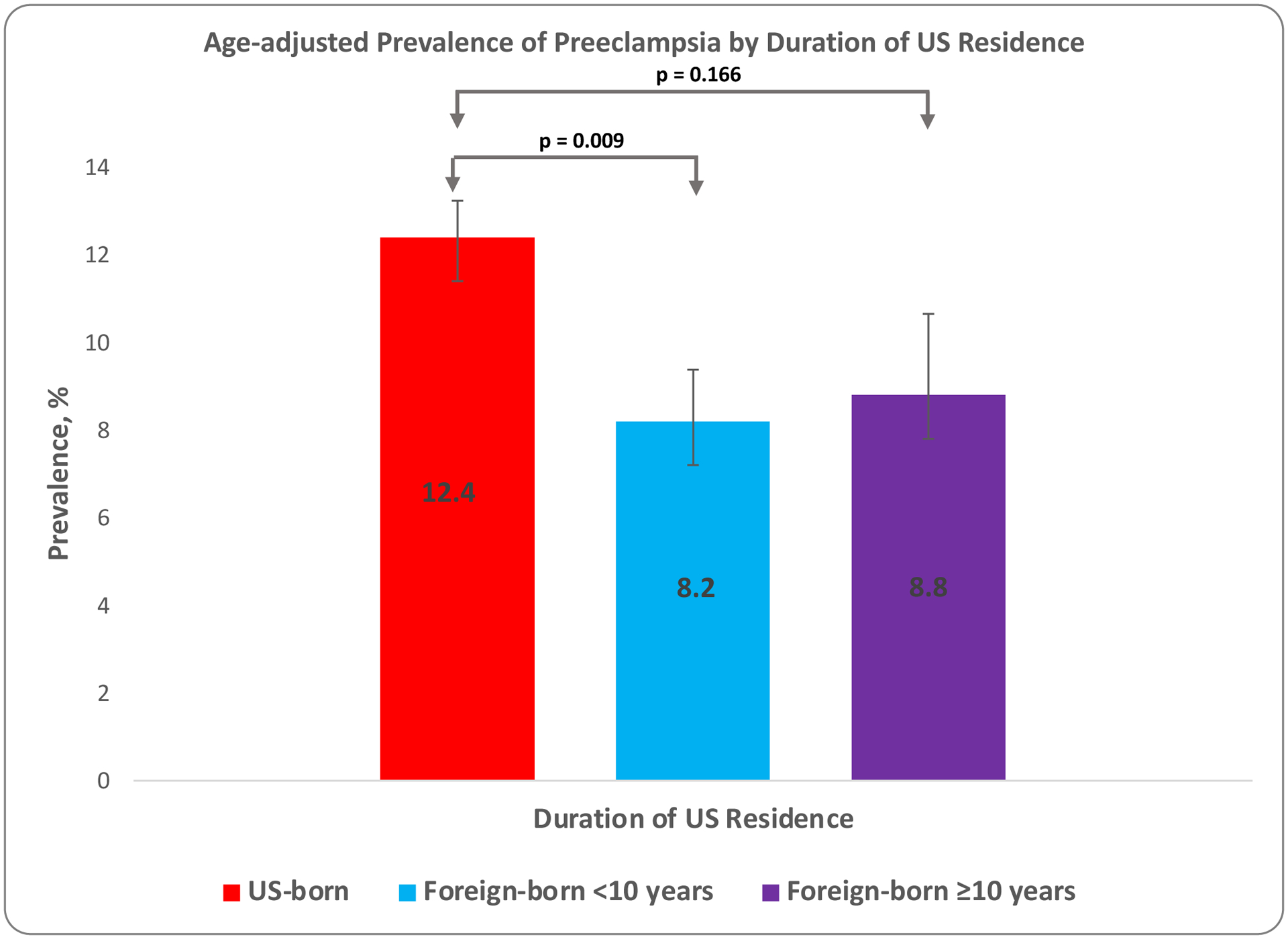
Age-adjusted prevalence of preeclampsia by duration of US residence
Table 4:
Crude and adjusted Odds Ratios with 95 % Confidence Intervals for Association between Preeclampsia and Duration of Residence among Non-Hispanic Black Women in the Boston Birth Cohort (1998–2016)
| Duration of Stay in the US | N | % with preeclampsia | OR and 95% CI for Preeclampsia | |||||
|---|---|---|---|---|---|---|---|---|
| Model 1 N = 2372 | p-value | Model 2 N =2372 | p-value | Model 3 N =2372 | p-value | |||
| US-Born | 1606 | 12.20 | REF | REF | REF | |||
| Foreign-born <10 years | 539 | 8.53 | 0.67[0.48–0.94] | 0.020 | 0.63[0.45–0.89] | 0.009 | 0.63[0.43–0.92] | 0.018 |
| Foreign-born ≥10 years | 227 | 9.25 | 0.73[0.46–1.18] | 0.199 | 0.68[0.42–1.10] | 0.116 | 0.64[0.38–1.07] | 0.091 |
| Model 1: Unadjusted Model 2: Age-adjusted Model 3: Model 2 + hypertension, parity, BMI, diabetes, education, smoking and general stress | ||||||||
OR – Odds Ratio
CI – Confidence Interval
DISCUSSION:
This study illustrates heterogeneity in the prevalence of preeclampsia in a large, inner-city NHB US population. The overall prevalence of preeclampsia in this study sample was 11.1%, compared to about 3.3% in Massachusetts, and about 5% in the US.2,37
The age-adjusted prevalence of preeclampsia among US-born and foreign-born NHB women was 12.4% and 9.1% respectively. While foreign-born NHB women who had been in the US for <10 years had 37% lower odds of preeclampsia compared to US-born NHB women, foreign-born NHB women with ≥10 years of stay did not have significantly different odds of preeclampsia compared to their US-born counterparts. Also, the prevalence of CVD risk factors such as obesity and smoking, was higher among US-born compared to foreign-born NHB women. Among foreign-born women, the prevalence of chronic hypertension, obesity, smoking and reports of moderate or severe stress, was higher among those with ≥10 years of US residences compared to those with <10 years of US residence. Likewise, the prevalence of preeclampsia changed with duration of residence in the US, suggesting that CVD risk factors and socioeconomic factors such as educational status and maternal stress are important indicators of overall health status.
The observed lower prevalence of preeclampsia among foreign-born women compared to their native-born counterparts is consistent with the results of some studies that have explored the association between maternal nativity and risk of hypertension in pregnancy.24–26 Singh et al. found that immigrant women in most racial/ethnic groups had lower rates of maternal hypertension than their US-born counterparts. For instance, NHB immigrants had a 31% lower risk than US-born NHB.24 This observation has also been documented in the risk of preterm births.27,38 Elsayed et al. found that among black women in Newark, New Jersey, immigrant women had 60% lower risk of preterm births compared to their US-born counterparts after adjusting for social and behavioral variables.38 This has also been documented in the prevalence of CVD risk factors such as obesity;39–41 A study that used the 2000–2013 National Health Interview Survey (NHIS) data found the age-standardized prevalence of obesity to be generally lower among foreign-born women (32.8%) compared to their US-born (48.7%) NHB counterparts.39
These studies, like ours, document an epidemiological paradox -- the rates of adverse health or pregnancy outcomes, with the exception of GDM, tend to be lower among immigrant women compared to their native-born counterparts of the same race or ethnicity. This foreign-born “advantage” may partly be explained by the “healthy immigrant effect”, which posits that immigrants must inherently be healthy to be able to migrate from the sending countries into their host country.28 Again, through selective immigration, immigrants tend to be more educated and are able to make healthier life choices.42,43 In our sample, foreign-born NHB women had higher levels of education, a characteristic that is expected to contribute to better pregnancy outcomes.28,44
Another reason for this foreign-born “advantage” may be protective cultural norms of immigrant women. Although not all immigrant cultures are protective, cultural norms and values such as less smoking, minimal drinking, healthier dietary preferences, as well as adequate social support may be protective for foreign-born women.29 In our study, US-born black women were about 5 times more likely than foreign-born women to have smoked during pregnancy. Studies examining smoking and other health behaviors among NHB women have also made similar observations.39,45,46
The foreign-born advantage tends to diminish with increasing duration of US residence.25,30,47 As demonstrated in our study, the prevalence of preeclampsia and other CVD risk factors was higher in foreign-born women with longer US residence (≥10 years) compared to those with shorter residence (<10 years). In the study by Elsayed et al. that explored the impact of immigration and duration of US residence on the length of gestation among black women, while recent immigrants had longer gestation compared to US-born blacks, the length of gestation for immigrants who had been in the US for at least 10 years was not different from that of the US-born women.38 Additionally a recent study in a multi-ethnic immigrant population from NHIS showed that among immigrants from diverse ethnic backgrounds, longer length of residence in the US was associated with increased odds of obesity, hyperlipidemia, and cigarette smoking even after adjusting for relevant confounding factors.48
This waning of the health advantage in NHB immigrants with time may be attributed to acculturation and associated unhealthy assimilation: as foreign-born women stay longer, they adopt some aspects of the US culture such as the unhealthy diet, risky health behaviors, and sedentary lifestyle, among others, which may increase the prevalence of CVD risk factors and preeclampsia in this group.
A key message for health care professionals is that race is self-assigned and may therefore not be enough to explain the diversity within a racial group. Although the prevalence of preeclampsia has been reported to be 5%2, racial and ethnic minority groups such as NHB women are widely reported to be disproportionately affected by preeclampsia.5,49 Black immigrants account for about 8.7% of the nation’s Black population.50 According to the US Census bureau, by 2060, 17% of the US NHB population will be immigrants.51 As this population continues to grow, we need to continue to examine the several systemic influences in maternal and pregnancy outcomes. We need to examine the impact of health inequities, implicit biases, structural racism, and disparities in access to care, maternal social support and the impact of acculturation on minority immigrants. There needs to be a framework for examining the role of these systemic and individual risk factors that influence preeclampsia. Specifically examining the role of health behaviors, environmental factors, race, and acculturation on the burden of the disease may help in the quest for effective strategies to reduce the disproportionate burden of preeclampsia on this minority population.
Study limitations:
The results of our study should be considered in light of some limitations. The BBC is a high-risk cohort since it oversamples women with preterm births. This may explain the high prevalence of preeclampsia reported in this study. In this study, women with preeclampsia, eclampsia and HELLP syndrome were put together in a single group due to limited sample size. Future studies with larger sample size should examine preeclampsia, eclampsia, and HELLP as separate groups to explore their shared and unique risk factors and pathogenesis. Also, one major risk factor for preeclampsia is previous pregnancy with preeclampsia.52 Information on this, and other measures of social determinants of health such as employment, access to healthcare and neighborhood, were lacking in this cohort and hence not adjusted for in our analyses. We were therefore unable to explore the social determinants of health completely as our study did not capture all the different constructs such as unemployment, health care services, housing etc. Additionally, maternal race/ethnicity and place of birth were self-reported. Also, foreign-born women were from different countries, but we were underpowered to estimate the effects of specific countries of origin on the risk of preeclampsia among foreign-born women. Again, 325 of the foreign-born women did not have data on their duration of residence in the US and so were excluded in the analyses of the association between duration of US residence and prevalence of preeclampsia among foreign-born women. Finally, since the BBC is a high-risk cohort and predominantly low-income population, NHB women in this cohort may not be representative of the NHB population in the US and so generalizability of our findings may be limited.
One notable strength of this study is that the BBC is a rich source of data for studying adverse pregnancy outcomes such as preeclampsia, preterm births and low birth weight and broad array of socio-demographic and clinical risk factors.
Conclusion:
The findings of this study suggest that the prevalence of traditional CVD risk factors, and sex-specific risk factors namely preeclampsia are lower among foreign-born NHB women compared to US-born NHB women. Duration of residence in the US is also associated with the risk of preeclampsia among foreign-born women, with women with shorter duration of residence having a significantly lower odds of preeclampsia compared to US-born NHB women, whereas those with longer duration of residence do not have significantly different odds of preeclampsia compared to US-born NHB women. Our findings support the foreign-born advantage and the waning of this advantage with longer duration of residence. Our findings provide insight into the heterogeneity of NHB women in terms of preeclampsia risk and associated risk factors; if further confirmed, may help inform more precise risk assessment and intervention. Our findings also illustrate that preeclampsia risk can be influenced by both biological and social determinants and underscore the need of transdisciplinary research to address racial/ethnic disparity in preeclampsia and related conditions.
Supplementary Material
What is known
Preeclampsia is a significant cause of maternal morbidity and mortality worldwide and in the United States, and it disproportionately affects non-Hispanic Black women.
Not much is known about the association of maternal place of birth and duration of residence with the prevalence of preeclampsia and other cardiovascular (CV) risk factors among non-Hispanic Black (NHB) women residing in the US.
What the study adds:
The prevalence of preeclampsia and other CV risk factors was higher among US- compared to foreign-born NHB women: US-born NHB women were younger, in higher percentage current smokers, had higher baseline prevalence of obesity (BMI≥ 30Kg/m2) and maternal stress, and the age-adjusted prevalence of preeclampsia among US- and foreign-born NHB women was 12.4% and 9.1% respectively.
Longer duration of US residence was associated with a higher prevalence of preeclampsia and other CV risk factors among foreign-born NHB women: Foreign-born women with ≥10 years of US residence had higher prevalence of chronic hypertension, obesity, smoking and maternal stress than those with <10 years of US residence, and the age-adjusted prevalence of preeclampsia among foreign-born with ≥10 years vs <10 years of US residence was 8.8% and 8.2% respectively.
This study supports the “foreign-born advantage” among NHB women and the waning of this advantage with longer duration of residence in the US
Sources of Funding:
The Boston Birth Cohort (the parent study) is supported in part by the National Institutes of Health (NIH) grants (2R01HD041702, R01HD086013, R01HD098232, and R01ES031272). This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the US Government
ABBREVIATIONS AND ACRONYMS
- ACC
American College of Cardiology
- AHA
American Heart Association
- BBC
Boston Birth Cohort
- BMI
body mass index
- CAD
coronary artery disease
- CI
confidence interval
- CVD
cardiovascular disease
- GDM
gestational diabetes mellitus
- NHB
non-Hispanic Blacks
- OR
odds ratio
- SDOH
social determinants of health
Footnotes
Disclosures: None
REFERENCES:
- 1.Shih T, Peneva D, Xu X, Sutton A, Triche E, Ehrenkranz R, Paidas M, Stevens W. The Rising Burden of Preeclampsia in the United States Impacts Both Maternal and Child Health. Am J Perinatol. 2015;33:329–338. doi: 10.1055/s-0035-1564881 [DOI] [PubMed] [Google Scholar]
- 2.Fingar RK, Mabry-Hernandez I, Ngo-Metzger Q, Wolff T, Steiner AC, Elixhauser A. Delivery Hospitalizations Involving Preeclampsia and Eclampsia, 2005–2014: Statistical Brief #222. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); 2017. Accessed November 1, 2020 https://www.ncbi.nlm.nih.gov/books/NBK442039/#sb222.s1 [Google Scholar]
- 3.Catov JM, Ness RB, Kip KE, Olsen J. Risk of early or severe preeclampsia related to pre-existing conditions. Int J Epidemiol. 2007;36:412–419. doi: 10.1093/ije/dyl271 [DOI] [PubMed] [Google Scholar]
- 4.Ying W, Catov JM, Ouyang P. Hypertensive Disorders of Pregnancy and Future Maternal Cardiovascular Risk. J Am Heart Assoc. 2018;7:e009382. doi: 10.1161/jaha.118.009382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.ACOG Practice Bulletin No. 202: Gestational Hypertension and Preeclampsia. Obstet Gynecol. 2019;133:e1–e25. doi: 10.1097/AOG.0000000000003018 [DOI] [PubMed] [Google Scholar]
- 6.Bernstein PS, Martin JN, Barton JR, Shields LE, Druzin ML, Scavone BM, Frost J, Morton CH, Ruhl C, Slager J, et al. National Partnership for Maternal Safety. Obstet Gynecol. 2017;130:347–357. doi: 10.1097/AOG.0000000000002115 [DOI] [PubMed] [Google Scholar]
- 7.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e596–e646. doi: 10.1161/CIR.0000000000000678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu P, Haththotuwa R, Kwok CS, Babu A, Kotronias RA, Rushton C, Zaman A, Fryer AA, Kadam U, Chew-Graham CA, et al. Preeclampsia and future cardiovascular health. Circ Cardiovasc Qual Outcomes. 2017;10:e003497. doi: 10.1161/CIRCOUTCOMES.116.003497 [DOI] [PubMed] [Google Scholar]
- 9.Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: Systematic review and meta-analysis. Br Med J. 2007;335:974–977. doi: 10.1136/bmj.39335.385301.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Honigberg MC, Zekavat SM, Aragam K, Klarin D, Bhatt DL, Scott NS, Peloso GM, Natarajan P. Long-Term Cardiovascular Risk in Women With Hypertension During Pregnancy. J Am Coll Cardiol. 2019;74:2743–2754. doi: 10.1016/j.jacc.2019.09.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wallis AB, Saftlas AF, Hsia J, Atrash HK. Secular trends in the rates of preeclampsia, eclampsia, and gestational hypertension, United States, 1987–2004. Am J Hypertens. 2008;21:521–526. doi: 10.1038/ajh.2008.20 [DOI] [PubMed] [Google Scholar]
- 12.Knuist M, Bonsel GJ, Zondervan HA, Treffers PE. Risk factors for preeclampsia in nulliparous women in distinct ethnic groups: A prospective cohort study. Obstet Gynecol. 1998;92:174–178. doi: 10.1016/S0029-7844(98)00143-4 [DOI] [PubMed] [Google Scholar]
- 13.Miranda ML, Swamy GK, Edwards S, Maxson P, Gelfand A, James S. Disparities in maternal hypertension and pregnancy outcomes: Evidence from North Carolina, 1994–2003. Public Health Rep. 2010;125:579–587. doi: 10.1177/003335491012500413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shen JJ, Tymkow C, MacMullen N. Disparities in maternal outcomes among four ethnic populations. Ethn Dis. 2005;15:492–497. [PubMed] [Google Scholar]
- 15.Tanaka M, Jaamaa G, Kaiser M, Hills E, Soim A, Zhu M, Shcherbatykh IY, Samelson R, Bell E, Zdeb M, et al. Racial disparity in hypertensive disorders of pregnancy in New York state: A 10-year longitudinal population-based study. Am J Public Health. 2007;97:163–170. doi: 10.2105/AJPH.2005.068577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gillespie CD, Hurvitz KA. Prevalence of Hypertension and Controlled Hypertension - United States, 2007–2010 - PubMed.; 2013. Accessed September 12, 2020 https://pubmed.ncbi.nlm.nih.gov/24264505/ [PubMed]
- 17.Ghosh G, Grewal J, Männistö T, Mendola P, Chen Z, Xie Y, Laughon SK. Racial/ethnic differences in pregnancy-related hypertensive disease in nulliparous women. Ethn Dis. 2014;24:283–289. Accessed July 28, 2020 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4171100/ [PMC free article] [PubMed] [Google Scholar]
- 18.Shahul S, Tung A, Minhaj M, Nizamuddin J, Wenger J, Mahmood E, Mueller A, Shaefi S, Scavone B, Kociol RD, et al. Racial disparities in comorbidities, complications, and maternal and fetal outcomes in women with preeclampsia/eclampsia. Hypertens Pregnancy. 2015;34:506–515. doi: 10.3109/10641955.2015.1090581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Melillo G Racial Disparities Persist in Maternal Morbidity, Mortality and Infant Health. Published 2020. Accessed July 28, 2020 https://www.ajmc.com/conferences/ada-2020/racial-disparities-persist-in-maternal-morbidity-mortality-and-infant-health
- 20.Centers for Disease Control and Prevention. State-Specific Maternal Mortality Among Black and White Women -- United States, 1987–1996. Accessed July 28, 2020 https://www.cdc.gov/mmwr/preview/mmwrhtml/mm4823a3.htm
- 21.Lee H, Kershaw KN, Hicken MT, Abdou CM, Williams ES, Rivera-O’Reilly N, Jackson JS. Cardiovascular disease among black Americans: Comparisons between the U.S. Virgin Islands and the 50 U.S. States. Public Health Rep. 2013;128:170–178. doi: 10.1177/003335491312800307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: A systematic review of public health studies with Hispanic populations in the United States. Soc Sci Med. 2009;69:983–991. doi: 10.1016/j.socscimed.2009.05.011 [DOI] [PubMed] [Google Scholar]
- 23.Commodore-Mensah Y, Ukonu N, Obisesan O, Aboagye JK, Agyemang C, Reilly CM, Dunbar SB, Okosun IS. Length of residence in the united states is associated with a higher prevalence of cardiometabolic risk factors in immigrants: A contemporary analysis of the national health interview survey. J Am Heart Assoc. 2016;5:e004059. doi: 10.1161/JAHA.116.004059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singh GK, Siahpush M, Liu L, Allender M. Research Article Racial/Ethnic, Nativity, and Sociodemographic Disparities in Maternal Hypertension in the United States. Int J Hypertens. 2014;2018:7897189–7897189. doi: 10.1155/2018/7897189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Naimy Z, Grytten J, Monkerud L, Eskild A. The prevalence of pre-eclampsia in migrant relative to native Norwegian women: a population-based study. BJOG An Int J Obstet Gynaecol. 2015;122:859–865. doi: 10.1111/1471-0528.12978 [DOI] [PubMed] [Google Scholar]
- 26.Sole KB, Staff AC, Laine K. The association of maternal country of birth and education with hypertensive disorders of pregnancy: A population-based study of 960 516 deliveries in Norway. Acta Obstet Gynecol Scand. 2018;97:1237–1247. doi: 10.1111/aogs.13393 [DOI] [PubMed] [Google Scholar]
- 27.Elo IT, Vang Z, Culhane JF. Variation in Birth Outcomes by Mother’s Country of Birth Among Non-Hispanic Black Women in the United States. Matern Child Health J. 2014;18:2371–2381. doi: 10.1007/s10995-014-1477-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ichou M, Wallace M. The Healthy Immigrant Effect: The role of educational selectivity in the good health of migrants. Demogr Res. 2019;40:61–94. doi: 10.4054/DEMRES.2019.40.4 [DOI] [Google Scholar]
- 29.National Research Council (US) and Institute of Medicine (US) Committee on the Health and Adjustment of Immigrant Children and Families; Hernandez DJ E. Immigration and Infant Health: Birth Outcomes of Immigrant and Native-Born Women - Children of Immigrants - NCBI Bookshelf. National Academies Press (US); 1999. Accessed April 18, 2020 https://www.ncbi.nlm.nih.gov/books/NBK224443/ [PubMed] [Google Scholar]
- 30.Ray JG, Vermeulen MJ, Schull MJ, Singh G, Shah R, Redelmeier DA. Results of the recent immigrant pregnancy and perinatal long-term evaluation study (RIPPLES). CMAJ. 2007;176:1419–1426. doi: 10.1503/cmaj.061680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jacobs P Where the Nation’s Foreign-Born Live Has Changed Over Time. Published 2019. Accessed July 29, 2020 https://www.census.gov/library/stories/2019/05/where-nations-foreign-born-live-has-changed-over-time.html
- 32.Center on the Early Life Origins of Disease - Population, Family, and Reproductive Health - Departments - Johns Hopkins Bloomberg School of Public Health. Accessed November 3, 2020 https://www.jhsph.edu/departments/population-family-and-reproductive-health/center-on-early-life-origins-of-disease/index.html
- 33.Boston Birth Cohort Study - Full Text View - ClinicalTrials.gov. Accessed October 29, 2020 https://clinicaltrials.gov/ct2/show/NCT03228875
- 34.Wang X, Zuckerman B, Pearson C, Kaufman G, Chen C, Wang G, Niu T, Wise PH, Bauchner H, Xu X. Maternal cigarette smoking, metabolic gene polymorphism, and infant birth weight. J Am Med Assoc. 2002;287:195–202. doi: 10.1001/jama.287.2.195 [DOI] [PubMed] [Google Scholar]
- 35.Berry JW. Acculturation and adaptation: health consequences of culture contact among circumpolar peoples. Arctic Med Res. 1990;49:142–150. Accessed October 28, 2020 https://pubmed-ncbi-nlm-nih-gov.proxy1.library.jhu.edu/2206174/ [PubMed] [Google Scholar]
- 36.Roccella EJ. Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol. 2000;183:s1–s22. doi: 10.1067/mob.2000.107928 [DOI] [PubMed] [Google Scholar]
- 37.Roberts CL, Ford JB, Algert CS, Antonsen S, Chalmers J, Cnattingius S, Gokhale M, Kotelchuck M, Melve KK, Langridge A, et al. Population-based trends in pregnancy hypertension and pre-eclampsia: An international comparative study. BMJ Open. 2014;1:e000101. doi: 10.1136/bmjopen-2011-000101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elsayed A, Amutah-Onukagha NN, Navin L, Gittens-Williams L, Janevic T. Impact of Immigration and Duration of Residence in US on Length of Gestation Among Black Women in Newark, New Jersey. J Immigr Minor Heal. 2019;21:1095–1101. doi: 10.1007/s10903-018-0813-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mehta NK, Elo IT, Ford ND, Siegel KR. Obesity among U.S.- and Foreign-Born Blacks by Region of Birth. Am J Prev Med. 2015;49:269–273. doi: 10.1016/j.amepre.2015.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bennett GG, Wolin KY, Askew S, Fletcher R, Emmons KM. Immigration and Obesity Among Lower Income Blacks*. Obesity. 2007;15:1391–1394. doi: 10.1038/oby.2007.166 [DOI] [PubMed] [Google Scholar]
- 41.Elo IT, Culhane JF. Variations in health and health behaviors by nativity among pregnant black women in Philadelphia. Am J Public Health. 2010;100:2185–2192. doi: 10.2105/AJPH.2009.174755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. J Health Econ. 2010;29:1–28. doi: 10.1016/j.jhealeco.2009.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: How education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82:816–820. doi: 10.2105/AJPH.82.6.816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guruge S, Collins Enid, Bender A. Working with Immigrant Women: Guidelines for Mental Health Professionals.; 2010. Accessed September 11, 2020 https://covid19.acs-aec.acerspyro.ca/wp-content/uploads/2019/05/CITC-2010-Summer-Ete-L-1.pdf#page=116
- 45.Cabral H, Fried LE, Levenson S, Amaro H, Zuckerman B. Foreign-born and US-born Black women: Differences in health behaviors and birth outcomes. Am J Public Health. 1990;80:70–72. doi: 10.2105/AJPH.80.1.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Turkson-Ocran RAN, Nmezi NA, Botchway MO, Szanton SL, Golden SH, Cooper LA, Commodore-Mensah Y. Comparison of Cardiovascular Disease Risk Factors Among African Immigrants and African Americans: An Analysis of the 2010 to 2016 National Health Interview Surveys. J Am Heart Assoc. 2020;9:e013220. doi: 10.1161/JAHA.119.013220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ray JG, Wanigaratne S, Park AL, Bartsch E, Dzakpasu S, Urquia ML. Preterm preeclampsia in relation to country of birth. J Perinatol. 2016;36:718–722. doi: 10.1038/jp.2016.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Premkumar A, Debbink MP, Silver RM, Haas DM, Simhan HN, Wing DA, Parry S, Mercer BM, Iams J, Reddy UM, et al. Association of Acculturation With Adverse Pregnancy Outcomes. Obstet Gynecol. 2020;135:301–309. doi: 10.1097/AOG.0000000000003659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Johnson JD, Louis JM. Does Race or Ethnicity Play a Role in the Origin, Pathophysiology, and Outcomes of Preeclampsia? An Expert Review of the Literature. Am J Obstet Gynecol. 2020;S0002–9378:30769–9. doi: 10.1016/j.ajog.2020.07.038 [DOI] [PubMed] [Google Scholar]
- 50.Anderson M A Rising Share of the U.S. Black Population Is Foreign Born | Pew Research Center. Published April 9, 2015. Accessed September 18, 2020 https://www.pewsocialtrends.org/2015/04/09/a-rising-share-of-the-u-s-black-population-is-foreign-born/#fn-20232-1 [Google Scholar]
- 51.Brown A U.S. immigrant population projected to rise, even as share falls among Hispanics, Asians | Pew Research Center. Published March 9, 2015. Accessed September 18, 2020 https://www.pewresearch.org/fact-tank/2015/03/09/u-s-immigrant-population-projected-to-rise-even-as-share-falls-among-hispanics-asians/
- 52.Bartsch E, Medcalf KE, Park AL, Ray JG, Al-Rubaie ZTA, Askie LM, Berger H, Blake J, Graves L, Kingdom JC, et al. Clinical risk factors for pre-eclampsia determined in early pregnancy: Systematic review and meta-analysis of large cohort studies. BMJ. 2016;353:i1753. doi: 10.1136/bmj.i1753 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


