Abstract
Despite the highly publicized beneficial effects of physical activity, 51.1% of middle-aged US adults do not achieve the recommended minimum of aerobic physical activity needed to maintain health. A sedentary lifestyle can be attributed in part to a lack of self-control and there is some evidence that self-control strategies can be improved with targeted interventions. The overall aim of this study is to test self-control as a behavior change mechanism for physical activity and to investigate whether a smartphone-based self-control intervention can increase physical activity among sedentary middle-aged adults. This protocol describes the design of a randomized controlled trial with two experimental conditions: The self-control treatment group and the control group. Both groups track their daily physical activity using a Fitbit step counter for eight weeks. Additionally, the self-control intervention group receives a 7-week smartphone-based self-control intervention to learn strategies how to potentiate desirable impulses or weaken undesirable ones. It is expected that the self-control treatment group will show greater increases in physical activity and that changes last longer compared to the control group. All participants will be assessed at pretest (baseline), at the end of each week (weeks 1–7), at posttest (week 8), and at follow-up (week 12). If this self-control intervention proves effective, this digital approach would represent a low-threshold and cost-effective approach to increasing physical activity. Such an intervention could be delivered to a large number of people to improve their health outcomes in the long run.
Trial Registration: ClinicalTrials.gov: NCT04522141
Keywords: Self-control, Physical activity, Behavior change, Smartphone-based intervention
Introduction
There is compelling evidence that an active lifestyle has broad benefits for cognitive, physical, and psychological health1–3 and a lack of physical activity is one of the leading causes of preventable death worldwide4. However, despite the highly publicized benefits of physical activity, 51.1% of middle-aged US adults between 35 and 65 years of age do not achieve the recommended minimum of aerobic physical activity needed to maintain health5–7. Middle-aged adults, an often under-studied population, are at a pivotal point in their lifespan as they may be setting up behaviors and forming habits that will endure into their older age, when physical health problems increase and physical activity tends to decrease8–10. As such, effective intervention programs that target increases in physical activity in middle-aged adults are urgently needed11. Factors that contribute to an inactive lifestyle include not only an individual’s health status or the social and environmental context, but also psychological factors such as an self-control12.
Self-control is the ability to suppress or control impulsive actions, emotions, and desires in favor of desired alternatives and enables people to reach long-term goals (such as sticking to regular exercise) despite the presence of short-term desires and distractions13–15. If people frequently fail to reach their goals, this is often due to low levels in the personality facet of self-control. High self-control is related to various positive outcomes such as better work performance, better interpersonal functioning, greater well-being, as well as better health behaviors and health outcomes including higher levels of physical activity16–22. In contrast, low self-control is linked to problematic health behaviors such as poor eating and a sedentary lifestyle23,24. Research suggests that the key to successfully keeping up an active lifestyle in the long run may lie in the ability to be self-controlled as people with higher self-control are better able to form strong habits that last25. Also, individuals with higher levels in the broader trait of conscientiousness are better able to increase their daily steps in the context of a physical activity intervention26.
The modification of personality facets such as self-control through interventions to promote well-being and healthy aging is a research priority of the National Institute of Aging27. Previous research also indicates that the goal to increase self-control is one of the most prevalent personality change goals28. Just recently, initial attempts have been made to directly change personality facets with the help of explicit interventions29. These first studies have shown that such interventions can help people to become more self-controlled and that changes peaked after just a few weeks of intervention. However, it remains unclear from previous research whether a targeted increase in self-control with the help of an intervention can have an effect on daily health behaviors such as physical activity, especially among those who have an inactive lifestyle. This research constitutes the first to test whether a self-control intervention has an effect on physical activity.
Objectives
This study is a pilot study at Stage 1 as defined in the NIH Stage Model of Behavioral Interventions30. Stage 1 research includes the development and modification of a behavioral intervention as well as the piloting and testing of its efficacy in a research setting with a focus on short-term maintenance effects. The overall goal of this pilot study is to test the efficacy of a smartphone-based self-control intervention to increase physical activity among sedentary adults who are at risk for poor health. The specific aims of the study are threefold: The first aim is to test the efficacy of a self-control intervention to increase physical activity by comparing two experimental conditions (i.e., self-control treatment group vs. control group). It is expected that those who receive the self-control intervention, will show greater increases in physical activity compared to people in the control group, who do not receive the self-control intervention. Moreover, it is expected that effects in the self-control treatment group will last longer compared to any changes in the control group. The second aim is to compare changes in self-control between the self-control group and the control group. It is expected that people in the self-control group will show greater changes in self-control compared to people in the control group. The third aim is to examine self-control as a behavior change mechanism for physical activity. It is expected that those who show greater increases in self-control will also show greater increases in physical activity. Self-control is expected to mediate the relationship between condition and physical activity (Figure 1).
Figure 1.
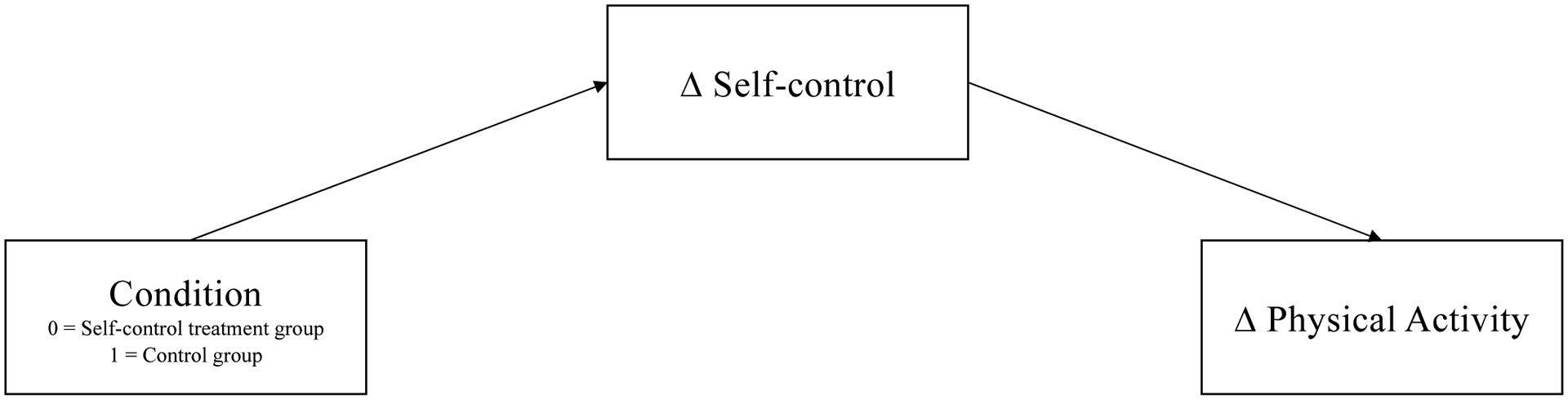
Change in Self-control as a Mechanism between Condition and Change in Physical Activity
Methods
This study has been approved by the University’s Institutional Review Board at Brandeis University (#20100R) and the protocol has been registered at ClinicalTrials.gov (#NCT04522141). Informed consent will be obtained from each participant. Ethical issues will be continuously considered. There is a data and safety monitoring plan and a safety officer is assigned to the study. Any adverse events will be recorded and reported.
Participants
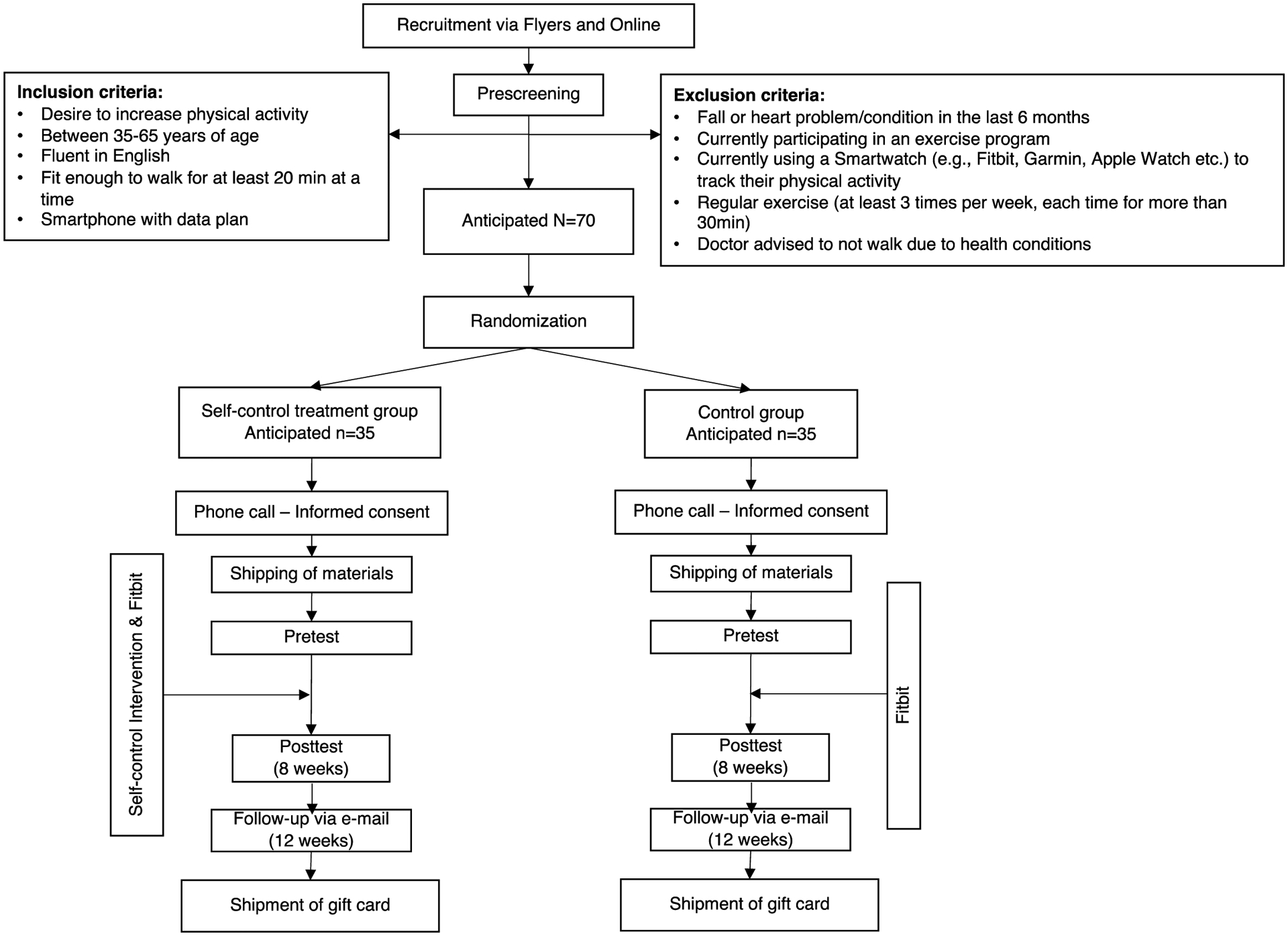
A total of 70 sedentary middle-aged adults, who are at risk for poor health, will be enrolled. Participants will be recruited from across the US with a focus on the Northeastern states by posting flyers on public boards in libraries, churches, shopping centers/malls, or grocery stores. Moreover, we will post advertisements online on Social Media, on Craigslist, and on findparticipants.com. Advertisements will be sent out in diverse communities to increase the likelihood that participants represent the socioeconomic, gender, racial, and ethnic distribution of the Northeast area of the US. As reimbursement, participants will receive a Fitbit Charge 4 step counter, which they can keep after the end of the study. In addition, as an added incentive, all participants will receive $25 for completing all aspects of the study.
Participants will be included if they indicate they want to become more physically active, are between 35 and 65 years, are fluent in English, fit enough to walk for at least 20 minutes at a time, and own a smartphone (Android or iPhone) with a data plan. Participants will be excluded if they have experienced a fall or heart problem/condition in the last 6 months, are currently participating in an exercise program to increase physical activity or currently using a Smartwatch (e.g., Fitbit, Garmin, Apple Watch etc.) to track their physical activity, already exercise (all types of exercise as defined by the person) at least 3 times per week and for more than 30 minutes at a time, and/or if a doctor has advised them to not walk due to health conditions.
Study Design and Procedure
The current study uses a two-armed randomized controlled trial design with assessments at pretest (baseline), weekly assessments at the end of every week (weeks 1 to 7), posttest (week 8), and follow-up (week 12). Participants will be randomly assigned into two experimental conditions to ensure that the two conditions are fully randomized with respect to participants’ baseline characteristics (allocation concealment). Thirty-five participants are randomized into each condition. Also, participants are blinded in terms of their experimental condition. The flow diagram of the study is shown in Figure 2.
Figure 2.
Flow diagram of the study
Recruitment flyers and advertisements specify: “Do you want to be more active, but find yourself making excuses to avoid exercise?” Flyers and advertisements also include a web link for interested participants. This web link will provide detailed information about the study and interested participants will be asked to fill out a screening questionnaire to check for all inclusion and exclusion criteria. If they are eligible for the study, they will be asked to provide their phone number and home postal address so we can send them the study materials. After that, participants will be randomly assigned into one of the two experimental conditions: The self-control treatment group or the control group. A research assistant will call all eligible participants to receive their informed consent by phone, to help them installing the MindHike smartphone application on their own smartphone, and to answer any questions. Once informed consent is given, we will ship participants a Fitbit Charge 4 step counter, instruction materials, a face mask, and a stylus pen to their home postal address.
Both the self-control treatment group and the control group will use the MindHike smartphone application and will use a Fitbit. The control group will receive a more basic version of the MindHike app which only sends them daily reminders to sync their step data, charge their Fitbit and asks them for their daily mood. The self-control treatment group will receive the version of the MindHike app which delivers the self-control intervention. MindHike is a smartphone application which can prompt participants with messages using a chatbot system. The app is pre-packaged, which means that the app will deliver the same dialogues automatically to all participant in each condition. There is no bi-directional communication, but participants click on predesignated responses to advance the dialogue.
On the first study day, all participants will fill in a pretest questionnaire. The MindHike application will send a web link that forwards participants to this online questionnaire. All participants will be asked to wear their Fitbit every day during the entire study from when they wake up to when they go to bed. During the first study week, participants are only asked to wear the Fitbit to document the number of steps taken to establish an objective measurement of steps before the intervention. All participants will be contacted by the MindHike app twice each day for eight weeks. The first message is a push notification which reminds all participants to wear their Fitbit so they can get used to it. The timing of this Fitbit is set to 7 a.m. by default but participants can change the time if they get up earlier or later in the morning. The second daily push notification asks participants to open the MindHike app and to read through a short daily pre-packaged chat in the app. Again, the time for this second push notification can be customized by each participant. During the first week, this pre-packaged chat will only remind participants of both groups to sync their step data with the Fitbit app and to charge their Fitbit. After this baseline week, the study will last for 7 more weeks and participants will still receive a push notification reminder to wear their Fitbit at customized times in the morning. Across the study, participants will also fill in weekly assessments of self-control at the end of each week. After the seven weeks, participants will fill in a posttest assessment. The MindHike application will send them the web link to the online posttest. After the posttest, participants do not use the MindHike application anymore but we will contact them via e-mail for a last online follow-up assessment four weeks later.
Control Group
After the first study week (baseline week), all participants will receive a push notification which reminds them to open the app at least once per day. If they open the app, participants will receive a pre-packaged chat. These daily pre-packaged chats will differ between the two treatment groups. Although both groups will use the MindHike application at the same frequency, the daily pre-packaged chat for the control group will only include a reminder to sync their step data, charge their Fitbit and ask them for their daily mood.
Self-Control Treatment Group
The daily pre-packaged chat for the self-control treatment group will include a short coaching session to deliver the components of the self-control intervention. Figure 3 depicts screenshots of interface examples of the MindHike app. The original intervention was developed in German and targets self-control in general without focusing on a specific life domain31. For this study, the intervention was adapted to specifically target self-control in the domain of physical activity.
Figure 3.

Interface examples of the MindHike app
Note. The dashboard of the app (left); settings options (middle); and a chat-based interaction (right).
As part of the intervention, participants of the self-control treatment group set themselves a specific physical activity goal such as “Each evening after dinner, I will go for a 20-minute walk”. The self-control intervention will teach participants different strategies on how to achieve their personal goal. In general, participants learn how to change their behaviors in ways that potentiate their desirable impulses or weaken their undesirable ones. The intervention is based on the process model of self-control32. This theoretical model will be used to describe the timeline of the development of impulses to participants. The goal of the self-control intervention is to target each stage of this theoretical model (i.e., (1) how to proactively select situations, (2) how to proactively change certain situations, (3) how to shift attention in a given situation, (4) how to change appraisal of a given situation, and (5) how to change behaviors in a given situation). Interventional components include specific behavioral tasks (e.g., If-then plans33), self-reflection tasks, and short film clips for psychoeducational purposes. Every week of the 7-week intervention, participants focus on one of the five stages of the self-control process model, while the first week is an introductory week on self-control and the last week serves to practice all learned strategies in everyday life. Each stage of the five stages of the self-control process model will be introduced with a short video clip. For more details, see the detailed content of the intervention31.
Measures
This study includes a screening assessment for inclusion and exclusion criteria, a pretest, weekly assessments at the end of weeks 1–7, a posttest at week 8, and a follow-up assessment at week 12. The same measures will be used for both groups. To administer questionnaires, participants will automatically receive web links via the MindHike application, which will forward them to Qualtrics online questionnaires. We will use the Fitabase platform to manage the continuously tracked step data of participants’ Fitbits. A summary of all measures can be found in Table 1.
Table 1.
Summary of measures
| Type of outcome | Measure | Timeline | |
|---|---|---|---|
| Steps per day | Primary outcome | Fitbit Charge 4 | Daily across 8 weeks |
| Physical activity | Primary outcome | IPAQ short version (Craig et al., 2003) | Pretest, Posttest, Follow-up |
| Self-control | Primary outcome | BSCS (Tangney, Baumeister, & Boone, 2004) | Pretest, End of each week (weeks 1–7), Posttest, Follow-up |
| Big Five personality traits | Secondary outcome | BFI-2 (Soto & John, 2017) | Pretest, Posttest, Follow-up |
| Exercise self-efficacy | Secondary outcome | (Neupert, Lachman, & Whitbourne, 2009) | Pretest, Posttest, Follow-up |
| Satisfaction with life | Secondary outcome | SWLS (Diener et al., 1985) | Pretest, Posttest, Follow-up |
| Sense of control | Secondary outcome | (Lachman & Weaver, 1998) | Pretest, Posttest, Follow-up |
| Cognitive performance | Secondary outcome | Stop & Go Switch Task / Backward Digit Span Task / Immediate Word List Recall (Lachman et al., 2014) | Pretest, Posttest, Follow-up |
| Demographics | Covariate | Pretest | |
| Self-reported functional status | Covariate | SF-36 (Ware & Sherbourne, 1992) | Pretest |
| Self-reported health status | Covariate | GHQ-12 (Goldberg & Hillier, 1979) | Pretest |
| Smoking status | Covariate | Posttest | |
| Fitbit on dominant vs. non-dominant wrist | Covariate | Posttest |
Primary outcome measures.
Primary outcome measures include the assessment of physical activity and self-control over time. Objective physical activity (i.e., daily step counts) will be assessed continuously using Fitbit Charge 4 step counters for eight weeks (1-week baseline and 7-week intervention). Self-reported physical activity will be assessed at pretest, at posttest, and a follow-up assessment using the short version of the International Physical Activity Questionnaire (IPAQ34). Self-control will be assessed at pretest, at the end of weeks 1–7, at posttest, and follow-up assessment using the Brief Self-control Scale (BSCS19), which is a reliable and well-validated measure.
Secondary outcome measures.
In addition, secondary outcome measures will be assessed to explore whether they show differential change over time between the two conditions. Additional outcome measures include the Big Five personality traits (BFI-235), exercise self-efficacy36, satisfaction with life (SWLS37), and sense of control38. Moreover, there are a number of studies that show that even basic walking can have positive effects on cognitive functioning39,40. Thus, we also include sensitive measures of cognitive performance to see if they show changes over time (Stop & Go Switch Task, Backward Digit Span Task, and Immediate Word List Recall Test41). These secondary outcome measures will be assessed at pretest, posttest, and follow-up assessment.
Screening measures.
A screening questionnaire will be administered to determine eligibility based on the inclusion and exclusion criteria mentioned above.
Other covariates.
Covariates, which may affect the effects of the intervention, will be assessed. These covariates include age, gender, education, income, work status, race and ethnicity, marital status, weight, height, smoking, self-reported functional status (SF-3642), self-reported health status (GHQ-1243), and if they wear the Fitbit on the dominant or non-dominant wrist. Covariates will be assessed at pretest or posttest.
Statistical Analyses
Sample size and power considerations.
We conducted a power analysis for repeated measures and between-group effects based on the between-group effect size found in a previous physical activity intervention study44. The power analysis with an α error level of 0.05, a statistical power (1-β) of 0.80, a correlation of 0.50 between the pretest, posttest, and follow-up assessment, and a Cohen’s f = .30 suggests a sample size of at least N = 62. As we learned from previous similar smartphone-based physical activity studies, about 10% of participants who sign up for the study discontinue their participation. As such, we will recruit a total of 70 middle-aged adults.
Data analyses
Missing data analyses will be performed and the type of missing data (i.e., random or non-random) will guide the handling of missing data (e.g., data imputation, estimation techniques). We will use linear conditional multilevel models and the lme4 package in R to test our research questions. Multilevel analyses can handle missing data in the outcome variables45.
First, to test the if the two groups increase their physical activity, we will test if the two groups increase their daily steps across the 56 days and if self-reported physical activity changed from pretest to posttest and follow-up for each group individually. To test if there is differential change in daily steps and self-reported physical activity between the two groups, we will use the entire sample and include a time by group interaction term as a Level 2 predictor in the multilevel models.
Second, to examine if the two groups increase their levels of self-control over time, we will test if there is an increase in overall self-control from pretest to posttest and follow-up for each group individually. Moreover, we will test if participants increase their weekly levels of self-control from week 1 to week 7. To test if there is differential change in overall and weekly self-control, we will also use the entire sample and include a time by group interaction term as a Level 2 predictor in the multilevel models.
Third, to examine self-control as a mechanism of behavior change, we will examine whether individuals who report greater changes in self-control show greater changes in their physical activity (daily steps and self-reported physical activity). More specifically, we will run multilevel models with repeated self-control as a Level 1 predictor of physical activity with condition as a Level 2 moderator. Moreover, we will use PROCESS46 in SPSS and Level 2 – Level 1 – Level 1 (2-1-1) multilevel mediation analyses in R to test whether self-control mediates the relationship between condition and physical activity.
Finally, we will use multilevel models in R45 to explore whether there is differential change over time in secondary outcomes such as the Big Five personality traits, exercise self-efficacy, satisfaction with life, sense of control, and cognitive performance.
Discussion
A report from the National Center for Health Statistics and the CDC reported that only about 20% of US adults meet the recommended threshold for aerobic and strength-training activity10 and this percentage even decreases with age. This study represents the first to test the efficacy of a self-control intervention to increase physical activity in a sample of sedentary middle-aged adults. It is expected that those who receive the self-control intervention will show greater increases in physical activity and that the effects will last longer compared to the control group.
This study includes several novel aspects. First, this randomized controlled trial aims to test self-control as a behavior change mechanism that may underlie the behavioral pattern of physical activity, which is in line with the goal of the NIH Science of Behavior Change (SOBC) Common Fund Program47. Research has demonstrated the importance of self-control for the prediction of health outcomes18. Indeed, self-control is seen as a key component for policy-makers who seek to enhance the physical health of the population48,49. Although previous research suggests that, for example, the building of implementation intentions can be an effective strategy to increase physical activity33,44, these effects were short lived and dissipated after one month. Intervening on self-control as a behavior change mechanism could produce more long-lasting effects since results of a previous personality intervention study suggest that changes in personality facets could be maintained until 6 weeks after the end of the intervention29. Second, the entire self-control intervention study will be delivered via the MindHike smartphone application without any in-person meetings with participants. In recent years, the use of smartphone applications for health interventions has become increasingly popular and a review article on app-based interventions found that smartphone applications can be effective to improve diet and physical activity50. Smartphone applications are promising and useful tools for delivering behavior change interventions51,52 while enabling future tests of the effectiveness of the intervention at a larger scale. Smartphone applications are cost-effective and low-threshold and allow delivery of the intervention with a relatively high dosage without personal contact. That is, people can be prompted with interventional components in their everyday life independent of time and place as most people have their smartphone with them nearly all the time52. As such, the self-control intervention is inexpensive and time-efficient in its delivery. Finally, the study will focus on middle-aged adults to evaluate the effect of the self-control intervention. Middle-aged adults are an often-understudied population and at a pivotal point in their lifespan where physical activity tends to decrease but they can establish behavioral patterns and form habits that endure into their older age and can promote healthy aging.
Despite these strengths and novel aspects of the study, there are some limitations that need to be noted. First, maintaining compliance among participants may be challenging without any in-person meetings with participants. The entire study will span across three months and will require commitment from participants to use the MindHike application and the Fitbit device every day for two months and complete three lengthy online questionnaires. Multiple strategies which have been suggested to reduce attrition in randomized trials53 will be used. First, we will call eligible participants to review and complete their informed consent by phone. Second, we will send out printed step-by-step manuals to explain participants how to use the MindHike app and the Fitbit in detail. Third, we will send out reminder e-mails if participants do not complete the three lengthy online questionnaires or if they do not synchronize their Fitbit with our data collection platform within three days. Fourth, the MindHike app sends two daily push notifications to remind participants to open the MindHike app at least once each day and to wear the Fitbit. Finally, participants receive a Fitbit Charge 4 as well as $25 if they complete all aspects of the study. However, participants may still forget to use the app or wear the Fitbit in their hectic daily lives. If participants are not committed to the 3-month study and drop out, the final sample may be selective, limiting generalization of the study findings. Second, this randomized controlled trial only includes adults aged 35–65 years to focus on middle-aged adults, but future research will be needed to explore the benefits of the self-control intervention with adults younger than 35 or older than 65. Third, this study only focuses on short-term maintenance effects and includes a follow-up assessment four weeks after the end of the intervention. If this study proves effective, a clinical trial with a larger sample and longer follow-up assessments will be needed to test the effectiveness of the intervention. Finally, previous research suggests considerable variability in accuracy across different physical activity monitors, placement sites (e.g., wrist or hip), speeds of activity, and conditions (e.g., free-living condition or treadmill)54. In this study, we will use the wrist-worn Fitbit Charge 4, one of Fitbit’s newest fitness trackers, to track participants’ physical activity. To the best of our knowledge, the accuracy of the Fitbit Charge 4 has not been evaluated empirically so far. However, previous versions of the wrist-worn Fitbit Charge 4 have been used in several studies to assess step counts, with reasonable success55.
In summary, this study has the potential to make a valuable contribution to advance our understanding of the underlying processes and mechanisms that lead to increased and sustained physical activity in middle-aged adults. Results from this study will provide information about the efficacy of a smartphone-based self-control intervention to support physical activity in middle-aged adults. To the extent that this self-control intervention proves effective, it would represent a low-threshold and cost-effective approach to increasing physical activity. This digital coaching approach could be delivered to a large number of people at the same time to improve their health outcomes in the long run.
Funding
Support for this study is provided by grant P30 AG048785 from the National Institute on Aging, National Institutes of Health (NIA/NIH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kohl HW, Craig CL, Lambert EV, et al. The pandemic of physical inactivity: Global action for public health. Lancet. 2012;380(9838):294–305. doi: 10.1016/S0140-6736(12)60898-8 [DOI] [PubMed] [Google Scholar]
- 2.Powell KE, Paluch AE, Blair SN. Physical activity for health: What kind? how much? how intense? on top of what? Annu Rev Public Health. 2011;32:349–365. doi: 10.1146/annurev-publhealth-031210-101151 [DOI] [PubMed] [Google Scholar]
- 3.Sanders LMJ, Hortobágyi T, la B van Gemert S, Van Der Zee EA, Van Heuvelen MJG. Dose-response relationship between exercise and cognitive function in older adults with and without cognitive impairment: A systematic review and meta-analysis. PLoS One. 2019;14(1):1–24. doi: 10.1371/journal.pone.0210036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–1757. doi: 10.1016/S0140-6736(06)68770-9 [DOI] [PubMed] [Google Scholar]
- 5.Ashe MC, Miller WC, Eng JJ, Noreau L. Older adults, chronic disease and leisure-time physical activity. Gerontology. 2009;55(1):64–72. doi: 10.1159/000141518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults: A systematic review of longitudinal studies, 19962011. Am J Prev Med. 2011;41(2):207–215. doi: 10.1016/j.amepre.2011.05.004 [DOI] [PubMed] [Google Scholar]
- 7.Center for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion, Division of Nutrition, Physical Activity, and Obesity. https://www.cdc.gov/nccdphp/dnpao/data-trends-maps/index.html. Accessed November 11, 2020.
- 8.Lachman ME, Teshale S, Agrigoroaei S. Midlife as a pivotal period in the life course: Balancing growth and decline at the crossroads of youth and old age. Int J Behav Dev. 2015;39(1):20–31. doi: 10.1177/0165025414533223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lachman ME. Mind the gap in the middle: A call to study midlife. Res Hum Dev. 2015;12(3–4):327–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clarke TC, Norris T, Schiller JS. Early Release of Selected Estimates Based on Data from the 2016 National Health Interview Survey. Washington, DC; 2017. [Google Scholar]
- 11.Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Heal. 2018;6(10):e1077–e1086. doi: 10.1016/S2214-109X(18)30357-7 [DOI] [PubMed] [Google Scholar]
- 12.Bauman AE, Reis RS, Sallis JF, et al. Correlates of physical activity: Why are some people physically active and others not? Lancet. 2012;380(9838):258–271. doi: 10.1016/S0140-6736(12)60735-1 [DOI] [PubMed] [Google Scholar]
- 13.Chapman BP, Hampson S, Clarkin J. Personality-informed interventions for healthy aging: Conclusions from a National Institute on Aging workshop. Dev Psychol. 2014;50(5):1426–1441. doi: 10.1038/jid.2014.371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Duckworth AL. The significance of self-control. Proc Natl Acad Sci U S A. 2011;108(7):2639–2640. doi: 10.1073/pnas.1019725108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krueger RF, Caspi A, Moffitt TE, White J, Stouthamer-Loeber M. Delay of gratification, psychopathology, and personality: Is low self-control specific to externalizing problems? J Pers. 1996;64(1):107–129. doi: 10.1111/j.1467-6494.1996.tb00816.x [DOI] [PubMed] [Google Scholar]
- 16.Bogg T, Roberts BW. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychol Bull. 2004;130(6):887–919. doi: 10.1037/0033-2909.130.6.887 [DOI] [PubMed] [Google Scholar]
- 17.Hill PL, Roberts BW. The role of adherence in the relationship between conscientiousness and perceived health. Heal Psychol. 2011;30(6):797–804. doi: 10.1038/jid.2014.371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moffitt TE, Arseneault L, Belsky D, et al. A gradient of childhood self-control predicts health, wealth, and public safety. Proc Natl Acad Sci U S A. 2011;108(7):2693–2698. doi: 10.1073/pnas.1010076108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tangney JP, Baumeister RF, Boone AL. High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. J Pers. 2004;72(2):271–324. doi: 10.1111/j.0022-3506.2004.00263.x [DOI] [PubMed] [Google Scholar]
- 20.Turiano NA, Chapman BP, Gruenewald TL, Mroczek DK. Personality and the leading behavioral contributors of mortality. Heal Psychol. 2015;34(1):51–60. doi: 10.1037/hea0000038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Ridder DTD, Lensvelt-Mulders G, Finkenauer C, Stok FM, Baumeister RF. Taking stock of self-control: A meta-analysis of how trait self-control relates to a wide range of behaviors. Personal Soc Psychol Rev. 2012;16(1):76–99. doi: 10.1177/1088868311418749 [DOI] [PubMed] [Google Scholar]
- 22.Allemand M, Job V, Mroczek DK. Self-control development in adolescence predicts love and work in adulthood. J Pers Soc Psychol. 2019;117(3):621–634. doi: 10.1037/pspp0000229.Self-Control [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Allen MS, Laborde S. The role of personality in sport and physical activity. Curr Dir Psychol Sci. 2014;23(6):460–465. doi: 10.1177/0963721414550705 [DOI] [Google Scholar]
- 24.Wilson KE, Dishman RK. Personality and physical activity: A systematic review and meta-analysis. Pers Individ Dif. 2015;72:230–242. doi: 10.1016/j.paid.2014.08.023 [DOI] [Google Scholar]
- 25.Gillebaart M, Adriaanse MA. Selfcontrol predicts exercise behavior by force of habit, a conceptual replication of Adriaanse et al. (2014). Front Psychol. 2017;8:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stieger M, Robinson SA, Bisson AN, Lachman ME. The relationship of personality and behavior change in a physical activity intervention: The role of conscientiousness and healthy neuroticism. Pers Individ Dif. 2020;166(March):110224. doi: 10.1016/j.paid.2020.110224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.NIA Workshop. Modifying Facets of Personality to Promote Well-Being and Healthier Aging; 2016. https://www.nia.nih.gov/sites/default/files/d7/personality_meeting_summary_final.pdf. [Google Scholar]
- 28.Stieger M, Eck M, Rüegger D, Kowatsch T, Flückiger C, Allemand M. Who wants to become more conscientious, more extraverted, or less neurotic with the help of a digital intervention? J Res Pers. 2020;87. [Google Scholar]
- 29.Stieger M, Wepfer S, Rüegger D, Kowatsch T, Roberts BW, Allemand M. Becoming more conscientious or more open to experience? Effects of a two-week smartphone-based intervention for personality change. Eur J Pers. 2020;(34):345–366. [Google Scholar]
- 30.Onken L, Carroll K, Shoham V, Cuthbert B, Riddle M. Reenvisioning clinical science: Unifying the discipline to improve the public health. Clin Psychol Sci. 2014;2:22–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Allemand M, Keller L, Gmür B, Gehriger V, Oberholzer T, Stieger M. MindHike, a digital coaching application to promote self-control: Rationale, content, and study protocol. Front Psychiatry. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duckworth AL, Gendler TS, Gross JJ. Situational strategies for self-control. Perspect Psychol Sci. 2016;11(1):35–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gollwitzer PM. Implementation intentions: Strong effects of simple plans. Am Psychol. 1999;54(7):493. [Google Scholar]
- 34.Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sport Exerc. 2003;35(8):1381–1395. [DOI] [PubMed] [Google Scholar]
- 35.Soto CJ, John OP. The next Big Five Inventory (BFI-2): Developing and assessing a hierarchical model with 15 facets to enhance bandwidth, fidelity, and predictive power. J Pers Soc Psychol. 2017;113(1):117–143. doi: 10.2214/ajr.170.6.9609152 [DOI] [PubMed] [Google Scholar]
- 36.Neupert SD, Lachman ME, Whitbourne SB. Exercise self-efficacy and control beliefs: Effects on exercise behavior after an exercise intervention for older adults. J Aging Phys Act. 2009;17(1):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Diener ED, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49(1):71–75. [DOI] [PubMed] [Google Scholar]
- 38.Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. J Pers Soc Psychol. 1998;74(3):763. [DOI] [PubMed] [Google Scholar]
- 39.Kramer AF, Erickson KI. Capitalizing on cortical plasticity: Influence of physical activity on cognition and brain function. Trends Cogn Sci. 2007;11(8):342–348. [DOI] [PubMed] [Google Scholar]
- 40.Erickson KI, Hillman CH, Kramer AF. Physical activity, brain, and cognition. Curr Opin Behav Sci. 2015;(4):27–32. [Google Scholar]
- 41.Lachman ME, Agrigoroaei S, Tun PA, Weaver SL. Monitoring cognitive functioning: Psychometric properties of the Brief Test of Adult Cognition by Telephone. Assessment. 2014;21(4):404–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992:473–483. [PubMed] [Google Scholar]
- 43.Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med. 1979;9(1):139–145. [DOI] [PubMed] [Google Scholar]
- 44.Robinson SA, Bisson AN, Hughes ML, Ebert J, Lachman ME. Time for change: Using implementation intentions to promote physical activity in a randomised pilot trial. Psychol Heal. 2019;34(2):232–254. doi: 10.1080/08870446.2018.1539487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.R Core Team. A Language and Environment for Statistical Computing, Vienna, Austria: Available at: https://www.R-project.org/ 2020. [Google Scholar]
- 46.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford publications; 2017. [Google Scholar]
- 47.Nielsen L, Riddle M, King JW, et al. The NIH Science of Behavior Change Program: Transforming the science through a focus on mechanisms of change. Behav Res Ther. 2018;(101):3–11. doi: 10.1016/j.brat.2017.07.002.The [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Heckman JJ, Kautz T. Hard evidence on soft skills. Labour Econ. 2012;19(4):451–464. doi: 10.1016/j.labeco.2012.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kautz T, Heckman JJ, Diris R, Ter Weel B, Borghans L. Fostering and Measuring Skills: Improving Cognitive and Non-Cognitive Skills to Promote Lifetime Success. Vol w20749; 2014. doi: 10.1134/S0031918X1801009X [DOI] [Google Scholar]
- 50.Schoeppe S, Alley S, Van Lippevelde W, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: A systematic review. Int J Behav Nutr Phys Act. 2016;13(1):127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Klasnja P, Pratt W. Managing health with mobile technology. Interactions. 2014;21(1):66–69. doi: 10.1145/2540992 [DOI] [Google Scholar]
- 52.Marsch L, Lord S, Dallery J. Behavioral Healthcare and Technology: Using Science-Based Innovations to Transform Practice. Oxford University Press; 2014. [Google Scholar]
- 53.Brueton V, Tierney J, Stenning S, et al. Strategies to reduce attrition in randomised trials. Trials. 2011;12(S1):A128. [Google Scholar]
- 54.An HS, Jones GC, Kang SK, Welk GJ, Lee JM. How valid are wearable physical activity trackers for measuring steps?. Eur J Sport Sci. 2017;17(3):360–368. [DOI] [PubMed] [Google Scholar]
- 55.Evenson KR, Goto MM, Furberg RD. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int J Behav Nutr Phys Act. 2015;12(1):159. [DOI] [PMC free article] [PubMed] [Google Scholar]


