Abstract
While the COVID-19 pandemic in the United States disproportionately impacts marginalized communities, no empiric US-based research has focused specifically on transgender and gender nonbinary (TGNB) people. We examined the pandemic’s impact on an established longitudinal cohort of TGNB individuals (N=208) by administering an online survey between March-June 2020. We used multivariable linear regression to examine reduced LGBTQ/TGNB community support and disruptions in gender-affirming health care as predictors of psychological distress during the pandemic. We found that the pandemic exacerbated ongoing mental health disparities for TGNB individuals. Furthermore, reduced LGBTQ/TGNB support was associated with increased psychological distress during the pandemic. Interruption and/or delay in gender-affirming health care was not associated with increased psychological distress during the pandemic. Special attention is needed to address the unique ways in which TGNB individuals were affected by the COVID-19 pandemic. This includes increasing access to LGBTQ/TGNB community support and addressing long-standing health disparities.
Keywords: COVID-19, transgender, mental health, gender-affirming medical care, depression, anxiety
Due to existing structural inequalities, the COVID-19 pandemic is anticipated to more severely affect already-marginalized population groups, including lesbian, gay, bisexual, transgender, and queer (LGBTQ) populations (Bowleg, 2020; Kline, 2020; Salerno et al., 2020). In addition to population-level responses to the pandemic (e.g., economic shutdown resulting in job loss, mandatory quarantines), transgender and gender nonbinary (TGNB) people may experience stressors related to their gender identity and may be at risk during the pandemic due to ongoing health disparities, healthcare access barriers, and unique healthcare needs (i.e., gender-affirming health care for those TGNB individuals who need it) (Wang et al., 2020). Few COVID-19 studies have focused on TGNB people (Torres et al., 2020), and none were conducted in the US.
Ongoing mental health disparities for TGNB people
Research documents that multiple ongoing health disparities affected TGNB people even before the COVID-19 pandemic (National Academy of Medicine, 2011; Reisner et al., 2016). Most TGNB health disparities research focuses on mental health and finds high rates of depression, anxiety, suicidal thoughts and behaviors, and non-suicidal self-injury (Marshall et al., 2016; Reisner et al., 2015; Valentine & Shipherd, 2018). The prevailing model used to explain this is minority stress theory, which posits that chronic stress from living with a socially stigmatized identity is additive to general stressors for TGNB individuals and contributes to health disparities (Hendricks & Testa, 2012). This “minority stress” is the product of societal prejudice, discrimination, and internalized stigma. For example, many TGNB people experience employment discrimination based on their gender identity and/or gender expression (James et al., 2016). Empirical research examining a wide variety of outcomes, including depression and anxiety, supports the deleterious effects of minority stressors on mental health among TGNB people (Bockting et al., 2013; Breslow et al., 2015; Jackman et al., 2018; Rood et al., 2016; Tebbe & Moradi, 2016).
Role of social support in buffering minority stress
Minority stress theory also posits that resilience factors such as social support and community connectedness may buffer the negative effects of social stigma on the mental health of TGNB people (Hendricks & Testa, 2012; Meyer, 2003). Research demonstrates that both general social support and TGNB-specific support are protective against symptoms of anxiety and depression (Budge et al., 2013; Budge et al., 2014; Pflum et al., 2015). TGNB-specific support may also buffer the negative effects of discrimination on psychological distress among U.S. TGNB adults (Bockting et al., 2013; Valente et al., 2020).
Gender-affirming medical care improves psychological wellbeing for some TGNB people
TGNB individuals have unique health needs, including gender-affirming hormonal and surgical interventions that many TGNB people need to align their bodies with their gender identity (World Professional Association for Transgender Health, 2011). These interventions may also help other people perceive a TGNB person’s gender as they experience it, thus facilitating gender-affirming social interactions (Costa & Colizzi, 2016). While not all TGNB people need gender-affirming medical interventions, for those who do, this can reduce psychological distress and increase psychological well-being (Fisher et al., 2016; Murad et al., 2010; White Hughto & Reisner, 2016). Delaying gender-affirming hormonal interventions may negatively affect psychological well-being among TGNB people who need such interventions (Colizzi et al., 2014).
Access to gender-affirming medical care during COVID-19
Even before the pandemic, availability of gender-affirming healthcare providers was limited in many parts of the U.S. (Cohen et al., 2020). Additionally, insurance coverage for gender-affirming surgery varies by state and health insurance carrier (Padula & Baker, 2017). This landscape became more complex with the Trump administration’s reversal of transgender healthcare protections in the Affordable Healthcare Act (Padula & Baker, 2017; Simmons-Duffin, 2020) and the subsequent, ongoing legal challenges to this reversal (Schmidt, 2020).
Beginning in March 2020, healthcare systems in the U.S. ceased providing non-essential (i.e., non-emergent) healthcare services to combat the spread of COVID-19 (COVIDSurg Collaborative, 2020). This move may have further restricted access to gender-affirming medical care; such interruptions in gender-affirming care may increase psychological distress among TGNB people (Flaherty et al., 2020; van der Miesen et al., 2020).
Present study
Public health researchers have called for studies to understand the impact of the COVID-19 pandemic on marginalized groups, including TGNB individuals (Gorczynski & Fasoli, 2020; Sevelius et al., 2020). The present study describes the effects of the pandemic on an established multi-site longitudinal cohort of U.S. TGNB individuals. We leverage this longitudinal data in conjunction with newly collected data during the pandemic to investigate changes in mental health. To examine factors specific to TGNB people, we hypothesized that loss of support from the LGBTQ/TGNB community and interruptions in gender-affirming health care during the pandemic would be associated with increased psychological distress.
Material and Methods
Sample Recruitment
This study is part of Project AFFIRM, a multi-site longitudinal cohort study of TGNB individuals in New York City, San Francisco, and Atlanta. The original cohort was established through purposive, venue-based recruitment. Quota sampling stratified by city, sex-assigned-at-birth, and age was used to ensure cohort diversity. In 2019, as part of a sub-study of Latinx TGNB individuals, an additional 24 participants from New York City joined the cohort. Inclusion criteria for both groups of cohort members were aged 16 years or older, transgender-identified, and fluency in English or Spanish. Because the online COVID-19 survey was only available in English (due to budget constraints), monolingual Spanish-speaking individuals were not invited to participate.
Data Sources and Data Collection
We have completed three waves of data collection for Project AFFIRM (Baseline, Wave 2, and Wave 3) via in-person semi-structured interviews. The present study utilizes data from Baseline and Wave 3 assessments, which took place in 2016 and 2019 respectively, and a subsequent online survey administered via Qualtrics between March and June 2020. All study procedures were approved by the New York State Psychiatric Institute/Columbia University Institutional Review Board. Prior to each interview, we obtained informed consent from participants over age 18 and assent from participants ages 16–17; the IRB waived parental consent for those under age 18 because of the risks associated with disclosure of gender identity to parents. For the online survey, participants reviewed and acknowledged informed consent information and could contact the investigators with questions.
Measures
Age, race, and ethnicity were assessed at Baseline (original cohort) or Wave 3 (2019 recruits) using 2010 U.S. Census measures (U.S. Census Bureau, 2010). Individuals who selected Hispanic ethnicity were coded as “Latinx/Hispanic,” producing a 4-way race/ethnicity variable: White, non-Hispanic; Latinx/Hispanic; Black/African American; Other (included Asian, Native Hawaiian or other Pacific Islander). Using the date on which baseline information was provided, we standardized each participant’s age to the date they completed the COVID-19 survey. For bivariate analyses, we used the original AFFIRM age stratification categories (16–20, 21–24, 25–39, 40–59, 60+). For this cohort of transgender individuals, gender identity was assessed at Wave 3 with the following question: “Which of the following best describes your current gender identity (Please choose one)?” Response options were woman, man, transgender woman/male-to-female (MTF), transgender man/female-to-male (FTM), nonbinary, genderqueer, and another. Individuals who responded nonbinary, genderqueer, or “another” were classified as having a nonbinary gender identity. All others were classified as having a binary gender identity. Participants were also asked about their sex-assigned-at-birth (male or female). Participants who selected a feminine or nonbinary gender identity and reported male sex-assigned-at-birth were categorized as transfeminine spectrum. Participants who selected a masculine or nonbinary gender identity and reported female sex-assigned-at-birth were categorized as transmasculine spectrum. On the COVID-19 survey, participants also reported their household size (U.S. Census Bureau, 2010).
To understand the prevalence of potential COVID-19 symptoms, respondents were asked if they had experienced any of the following since March 1, 2020 (i.e., just after the first confirmed US COVID-19 case): cough, fever, or shortness of breath (Centers for Disease Control and Prevention, 2020). Individuals who reported one or more of these were classified as having a symptom that could be associated with COVID-19. These individuals were asked whether they received a diagnostic test for COVID-19 and, if so, whether the test was positive. We asked only about diagnostic testing because the first COVID-19 antibody test was not Food and Drug Administration (FDA) authorized until April 1, 2020 (U.S. Food and Drug Administration, 2020).
We used the Pandemic Stress Index (PSI) (Harkness et al., 2020) to assess the impact of the COVID-19 pandemic on respondents’ daily lives. In the PSI, participants are first asked, “What are you doing/did you do during COVID-19 (coronavirus)?” and mark-all-that-apply among a 19-item list of potential impacts (e.g., “practicing social distancing,” “isolating or quarantining yourself,” and “not working”). Each response triggered additional probes (e.g., whether an unemployed individual lost their job during the pandemic). Next, participants used a 5-point Likert scale (ranging from “not at all” to “extremely”) to rate the degree to which the pandemic has impacted their daily life. For this study, we focused on four elements of the PSI: practicing social distancing, isolating/quarantining, not working, and the Likert scale question because the other PSI questions focus on mental health, which we measured in more detail using the Brief Symptom Inventory-18 (see below).
Survey respondents were asked to separately indicate if they had experienced reduced access to LGBTQ-specific or TGNB-specific community support such as community centers, support groups, bars/clubs, athletic groups, or senior centers since March 1, 2020. Because LGBTQ-specific and TGNB-specific support overlap, we combined these into a single category for analysis.
In Wave 3 and the online COVID-19 survey, we used the Brief Symptoms Inventory (BSI-18) (Derogatis, 2001) to assess psychological distress. The BSI-18 has 18 items on which respondents use a 5-point Likert scale, ranging from “not at all” (1) to “extremely” (5), to rate the degree to which they experience various psychiatric symptoms. The sum of the 18-items produces the Global Severity Index (raw-score GSI; internal consistency = 0.92). The BSI-18 has three validated sub-scales: anxiety (internal consistency = 0.88), depression (internal consistency= 0.87), and somatization (internal consistency =0.82). Based on previous research (Derogatis, 2001), “clinically significant psychological distress” is defined as T-score≥63 (i.e., >90th percentile) on the GSI or on ≥2 subscales. Sub-scale t-scores ≥63 are considered clinically significant.
In the COVID-19 survey, participants were also asked if they had taken gender-affirming hormones in the past three months. Those who answered affirmatively were asked, “In the past 3 months, have you experienced any difficulty obtaining your hormone medication (e.g., ran out of medication, unable to get refills, unable to reach your healthcare provider)?” We asked those who had not taken gender-affirming hormones in the past three months, “Had you wanted to start gender-affirming hormones but experienced a delay in doing so (e.g., appointment cancellations, restrictions on travel)?” We asked about the past three months because this period encompassed the time just prior to and during the onset of the pandemic. For analysis, we combined interrupted and delayed hormone therapy into a single variable because both represent barriers to gender-affirming hormone therapy. We also asked participants if they had had an upcoming gender-affirming surgery cancelled or postponed.
Data Analysis
First, we used frequencies/percentages for categorical variables and means/standard deviations for continuous variables to describe sample demographics, social distancing measures, and changes in participants’ lives during the pandemic with regard to reduced LGBTQ/TGNB-specific support, psychological distress, and access to gender-affirming hormonal and surgical care. For psychological distress, we used paired sample t-tests to compare the mean pre-pandemic raw-score GSI (Wave 3) to the COVID-19 survey raw-score GSI. We used McNemar’s tests to compare the pre-pandemic versus pandemic rates of “clinically significant psychological distress” as measured by the GSI and the three BSI-18 sub-scales.
Because our primary hypothesis concerned reduction in LGBTQ/TGNB-specific support and disruptions in gender-affirming health care as predictors of psychological distress during the pandemic, we next used independent sample t-tests to examine bivariate differences in mean pandemic raw-score GSI based on whether a participant had experienced reduced LGBTQ/TGNB-specific support, interrupted/delayed gender-affirming hormone therapy, or cancelled/postponed gender-affirming surgery. We also examined bivariate differences in mean pandemic raw-score GSI by age, gender identity (transfeminine versus transmasculine spectrum), race/ethnicity, nonbinary versus binary identity, employment status, household size, and study site.
We then used multivariable linear regression analyses to separately examine reduced LGBTQ/TGNB-specific support and disruption in gender-affirming hormonal/surgical care as predictors of psychological distress (raw-score GSI) during the pandemic. We first controlled for age and sex-assigned-at-birth because these are known to be associated with mental health, particularly as measured by the GSI (Derogatis, 2001), and because they were factors by which recruitment of the AFFIRM cohort was stratified. We also included demographic factors that showed statistically significant differences in GSI in bivariate analyses. Finally, to control for pre-pandemic mental health, we added Wave 3 raw-score GSI to these models.
Results
Impact of COVID-19 on TGNB individuals
Out of 280 individuals who completed Wave 3, 214 completed the online survey (76.4% retention). After excluding participants (n=6) with incomplete online survey data for psychological distress (GSI) and/or reduced LGBTQ/TGNB-specific support, the analytic sample contained 208 individuals. Table 1 describes demographic characteristics of COVID-19 survey participants and ways that participants’ lives were impacted during the pandemic. There were no statistically significant differences between survey completers and non-completers by age, race/ethnicity, or nonbinary versus binary gender identity. A significantly higher percentage (X2=11.808, df=1, p=.001) of eligible transmasculine individuals completed the COVID-19 survey (n=166; 75.3%), compared to eligible transfeminine individuals (n=85; 56.7%). There was a lower COVID-19 survey response rate (X2=6.468, df=2, p=.030) from Atlanta (n=52; 55.9%), compared to New York (n=118; 72.0%) and San Francisco (n=93; 68.8%). There were no statistically significant differences in mean pre-pandemic GSI between transmasculine (16.73 +/− 12.14) and transfeminine individuals (17.04 +/− 13.49) or among study sites (t=−.166, df=197, p=.868).
Table 1.
Demographic characteristics and COVID-19 pandemic impacts on a multi-site longitudinal cohort of transgender and gender nonbinary individuals (N=208).
| Characteristic | Mean ± SD or n(%) |
|---|---|
| Age | 37.8 years ± 13.1 |
| Atlanta | 55 (26.5%) |
| Transfeminine spectrum | 89 (42.8%) |
| Nonbinary gender identity | 57 (27.4%) |
| Other | 36 (17.3%) |
| Household size | 2.3 people ± 1.5 (range 1–9) |
| Living alone | 63 (30.3%) |
| Impact/Experience during the Pandemic (since March 1, 2020) | Mean ± SD or n(%) |
| Not at all | 0 (0%) |
| Tested positive for COVID-19 | 1 (0.004%) |
| Isolation/quarantine | 93 (44.7%) |
| Unemployment rate | 62 (29.8%) |
| Job loss during the pandemic | 35 (16.8%) |
| Personal financial loss | 117 (56.3%) |
| Inadequate access to basic supplies (e.g., food and medicine) | 62 (29.8%) |
Participants reported reduced access to LGBTQ/TGNB-specific support and gender-affirming health care during the pandemic. Access to LGBTQ-specific and TGNB-specific support services was reduced for 113 individuals (54.3%) and 91 individuals (43.8%), respectively. Out of 208 TGNB individuals, 23 participants (11.1%) reported having a previously scheduled gender-affirming surgery cancelled or postponed; 68 participants (32.7%) experienced an interruption in receiving (n=55) or a delay in starting (n=13) gender-affirming hormones.
Regarding psychological distress, the average raw-score GSI was significantly higher during the pandemic, compared to pre-pandemic (Wave 3) ratings (19.02 pandemic versus 16.86 pre-pandemic, t=2.659, df=198, p=.008). A significantly higher percentage of respondents met criteria for “clinically significant psychological distress” during the pandemic, compared to pre-pandemic ratings (n=87; 41.8% versus n=66; 31.7% pre-pandemic, p=.011; Figure 1a). Compared to pre-pandemic assessments, a higher percentage of survey respondents met criteria for clinically significant depressive (n=86; 41.3% versus n=59; 28.4% pre-pandemic, X2=12.75, p<.001) and anxiety symptoms (n=86; 41.3% versus n=65; 31.3% pre-pandemic, X2=5.97, p=.015). There was no significant difference, compared to pre-pandemic assessments, in the percentage of survey respondents with severe somatization (n=59; 28.4% pandemic versus n=52; 25.0% pre-pandemic, X2=.65, p=.419).
Figure 1.
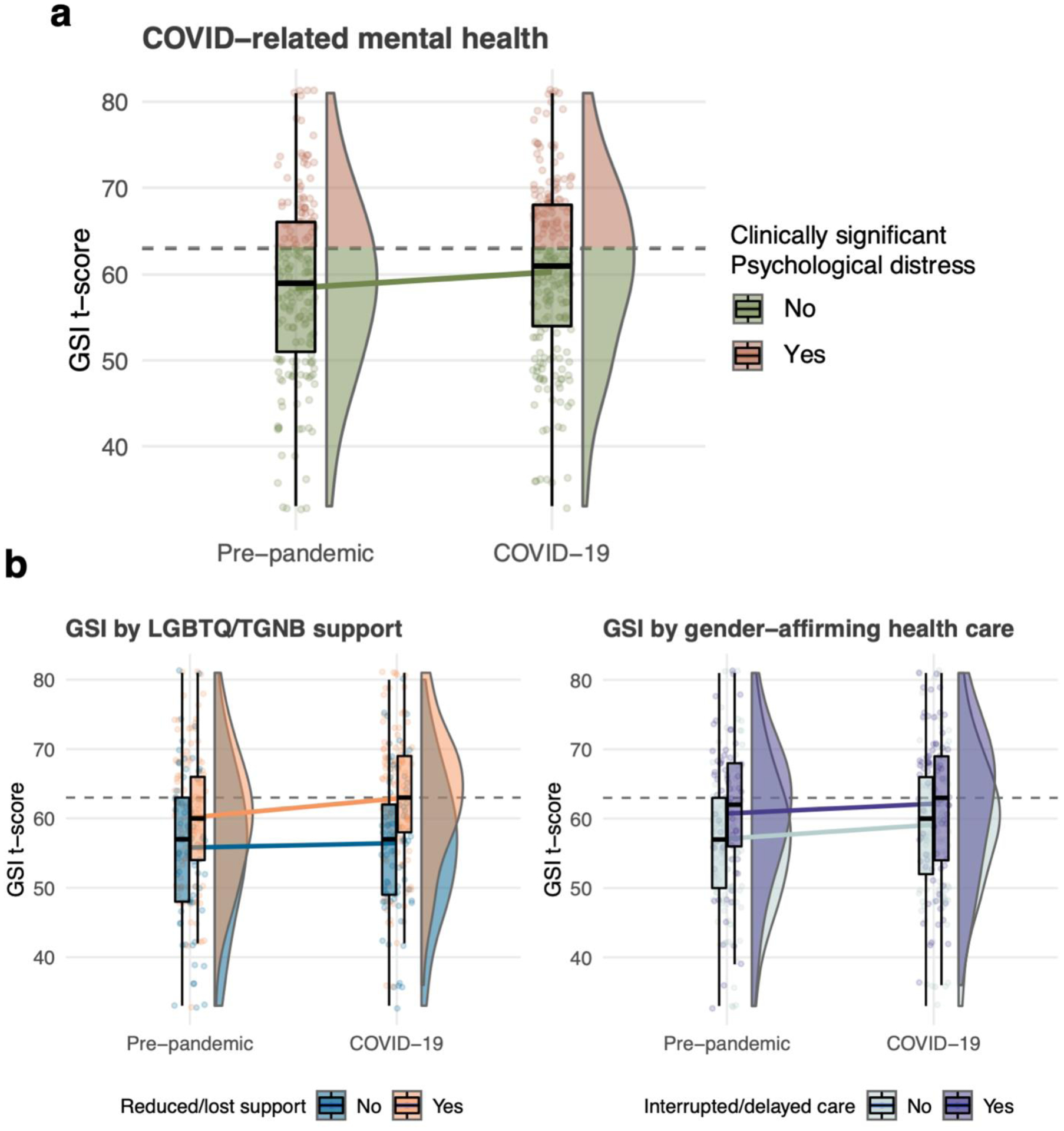
COVID-19 pandemic-related changes in psychological distress, as measured by the BSI-18 Global Severity Index (GSI) score. (a) Overall trend in GSI between pre-pandemic and COVID-19 assessments, across the full cohort of TGNB individuals (N=208). Points represent individual observations, boxplots and half-violin plots show the shift in the full distribution. Color shows the proportion of participants with GSI scores classified as “clinically significant.” (b) Differential trends in pandemic-related GSI based on reduction of LGBTQ/TGNB-specific support (left) and disrupted gender-affirming healthcare (right). Colored points, boxplots, and half-violin plots show subgroup-specific changes in GSI.
Bivariate difference in psychological distress during the pandemic
Table 2 describes bivariate relationships between raw-score GSI and demographic characteristics. The mean GSI during the pandemic did not differ significantly (p>.05) between transfeminine and transmasculine spectrum individuals or by age, race/ethnicity, study site, employment status, or household size (living alone versus with others). The mean GSI for nonbinary individuals was greater than the mean GSI for binary individuals (22.54 +/−13.54 versus 18.00 +/− 12.85, t=2.226, df=206, p=.027).
Table 2.
Demographic comparisons of psychological distress, as measured by the Global Severity Index (raw score), in a multi-site longitudinal cohort of transgender and gender nonbinary individuals (N=208).
| Global Severity Index Mean +/− SD | t or F statistic (df) | p-value | |
|---|---|---|---|
| 60+ | 13.40 +/− 11.27 | ||
| Atlanta | 19.11 +/− 12.29 | ||
| Transfeminine spectrum | 17.25 +/− 13.20 | ||
| Nonbinary | 22.54 +/− 13.84 | ||
| Other | 20.56 +/− 15.78 | ||
| Living with others | 19.57 +/− 13.09 | ||
| Unemployed | 19.69 +/− 13.66 |
Respondents with reduced LGBTQ/TGNB-specific support had a higher mean GSI (22.51 +/− 13.52 versus 14.33 +/− 11.23, t=−4.567, df=206, p<.001), compared to those without such reductions. People who experienced interrupted or delayed gender-affirming hormone therapy reported significantly higher mean GSI (22.29 +/− 14.56 versus 17.76 +/− 12.35, t=−2.337, df=206, p=.02). There was no significant difference in mean GSI based on whether someone experienced a canceled or postponed gender-affirming surgery. Taken together, individuals who had experienced difficulty accessing gender-affirming care (hormones and/or surgery) reported higher mean GSI compared to individuals who maintained access or were not pursuing these treatments (21.65 +/− 14.31 versus 17.71 +/− 12.34, t=−2.111, df=206, p=.036). Over half (n=13; 56.5%) of individuals who experienced a cancelled or postponed surgery also experienced interrupted gender-affirming hormone therapy. For this reason, we combined these groups in multivariable analyses.
Multivariable Findings
Table 3 presents multivariable linear regression results for reduced LGBTQ/TGNB community support and disrupted gender-affirming health care as predictors of psychological distress (raw-score GSI) during the pandemic. We first controlled for age and transfeminine versus transmasculine spectrum identity as described in the Materials and Methods section as well as binary versus nonbinary gender identity because these two groups had shown significant differences in mean raw-score GSI in bivariate analyses. Controlling for these variables, reduced LGBTQ/TGNB support during the pandemic was associated with greater GSI (i.e., greater psychological distress) (B=7.42, t=4.19, p<.001). Next, we controlled for pre-pandemic GSI. Reduced LGBTQ/TGNB support remained significantly associated with greater GSI (B=4.94, t=3.29, p=.001; Figure 1b). We also tested the interaction of reduced LGBTQ/TGNB social support and pre-pandemic GSI, which was not significant (p>.05).
Table 3.
Multivariable linear regression results from a longitudinal cohort of TGNB individuals (N=208) to investigate reduced LGBTQ/TGNB community support and disrupted gender-affirming health care as predictors of psychological distress (raw-score GSI score) during the COVID-19 pandemic.
| Variable | Model A Adjusted R2 = .126 B (p-value) |
Model B Adjusted R2 = .413 B (p-value) |
|---|---|---|
| Reduced LGBTQ/TGNB community support | 7.42 (p<.001) | 4.94 (p=.001) |
| Age | −0.19 (p=.007) | −0.08 (p=.184) |
| Transfeminine spectrum identity | −0.69 (p=.712) | −2.55 (p=.108) |
| Nonbinary identity | −2.29 (p=.260) | 0.34 (p=.842) |
| Pre-pandemic (Wave 3) GSI score | -------- | 0.59 (p<.001) |
| Variable | Model A Adjusted R2 = .073 B (p-value) |
Model B Adjusted R2 = .387 B (p-value) |
| Disrupted gender-affirming health care | 4.19 (p=.028) | 2.22 (p=.159) |
| Age | −0.18 (p=.015) | −0.07 (p=.228) |
| Transfeminine spectrum identity | −2.35 (p=.238) | −3.50 (p=.035) |
| Nonbinary identity | −1.18 (p=.160) | −0.05 (p=.980) |
| Pre-pandemic (Wave 3) GSI score | -------- | 0.61 (p<.001) |
LGBTQ: lesbian, gay, bisexual, transgender, and queer; TGNB: transgender and gender nonbinary; GSI: Global Severity Index
Controlling for the same demographic variables as in the previous model, interruption/delay in gender-affirming health care during the pandemic were associated with greater GSI (B=4.19, t=2.22, p=.028). However, after controlling for pre-pandemic GSI, this association was no longer significant (B=2.24, t=1.42, p=.159; Figure 1b).
Discussion
This is one of the first studies to examine the impact of the COVID-19 pandemic on TGNB individuals and is unique in using a longitudinal cohort to investigate changes in psychological distress compared to the pre-pandemic period. In certain respects, TGNB individuals were impacted by the pandemic and public health measures to control its spread in much the same way as the general population (i.e., social distancing, isolation/quarantine). In other ways, TGNB people were impacted uniquely during the pandemic, particularly in relation to LGBTQ/TGNB-specific support and access to gender-affirming health care.
COVID-19 infection rates
Approximately one-third of respondents reported at least one potential symptom of COVID-19. However, very few of these individuals were tested for the virus. This is not surprising given the limited availability of diagnostic testing during the time-period in which the survey was administered. In the beginning of the pandemic, testing was reserved for symptomatic individuals who required hospitalization. Now that testing is more widely available throughout the U.S., data collection should include information about gender identity to more precisely characterize the infection rate among TGNB individuals.
Demographics differences in psychological distress during the pandemic
We did not find any age, gender identity (transmasculine versus transfeminine), race/ethnicity, or study site differences in psychological distress during the pandemic. Our null findings about differences in mental health by race/ethnicity are consistent with other studies that found high rates of severe psychological distress among TGNB individuals overall (compared to the general population) but not differentially more severe based on race/ethnicity within TGNB samples (Moradi et al., 2016; Pflum et al., 2015; Yang et al., 2015). Lack of difference by study site was surprising because the pandemic affected New York City earlier and more severely than other regions. Additional research is needed to understand this finding, including how the economic shutdowns and COVID-19 prevention specifically affected the operation of LGBTQ/TGNB-oriented organizations and support structures in different regions of the U.S.
In bivariate analyses, we found that nonbinary respondents reported significantly greater psychological distress compared to participants with a binary identity; a finding that did not persist in multivariable analyses. Prior research into this topic has been similarly mixed, with some studies finding that nonbinary and binary transgender individuals may experience mental health problems at different rates (Jones et al., 2019; Newcomb et al., 2020; Rimes et al., 2017; Thorne et al., 2019). One potential reason for this variability is that the mental health disparities observed between nonbinary and binary transgender individuals may be confounded by other demographics differences between these two groups. For example, nonbinary individuals are typically younger on average than binary individuals (Harrison et al., 2011; James et al., 2016). This was also true in our study and may explain why the association of nonbinary identity with greater psychological distress was no longer significant after controlling for age and other demographic covariates. Our multivariable findings could also reflect the fact that social distancing measures were applied broadly at a population level, and therefore disruptions in LGBTQ/TGNB community support and gender-affirming health care may have impacted nonbinary and binary transgender individuals similarly.
Impacts of the COVID-19 pandemic on TGNB individuals occurred in the context of ongoing disparities
Our findings highlight how common pandemic-related effects on daily life may have impacted TGNB individuals more severely than the general population due to ongoing inequalities and health disparities. One example is unemployment and job loss. By July 2020, the U.S. unemployment rate had increased to 10.2%, from 6.5% in July 2019 (U.S. Bureau of Labor Statistics, 2020b). The unemployment rate during the pandemic was higher for TGNB individuals in this study (29.8%). This is due to a 13.0% pre-pandemic unemployment rate in this sample, which is much higher than the February 2020 overall U.S. unemployment rate (3.5%) (U.S. Bureau of Labor Statistics, 2020a). This is consistent with the TGNB unemployment rate reported in other studies (Herman & O’Neill, 2020).
Similar to employment, changes in psychological distress among TGNB individuals during the pandemic occurred in the context of ongoing mental health disparities. A recent CDC report described the mental-health toll of the COVID-19 pandemic (Czeisler et al., 2020), with 40.9% of individuals reporting an adverse mental health condition; 30.9% with depressive or anxiety symptoms. While the CDC report did not collect information about gender identity, previous research shows that depressive and anxiety disorders occur at disproportionately high rates among TGNB individuals (Bockting et al., 2013; National Academy of Medicine, 2011; Nuttbrock et al., 2014; Streed et al., 2018). In the present study, the pre-pandemic rate of clinically significant psychological distress was already high (31.7%). Therefore, it is noteworthy that in the present study the pandemic was associated with a significant increase in psychological distress among TGNB individuals, because this increase occurred in the context of an elevated baseline level of distress. These high pre-pandemic levels place TGNB individuals at risk for crossing the threshold into clinically significant symptomatology with even modest increases in symptoms, as is evidenced in this study by significant increases in the rate of clinically significant psychological distress.
TGNB-specific impacts of the COVID-19 pandemic
The COVID-19 pandemic also impacted TGNB individuals in two ways that are unique compared to the general population: (1) reduced access to LGBTQ/TGNB-specific support and (2) impeded access to gender-affirming medical/surgical care.
Over half of survey respondents reported reduced access to LGBTQ/TGNB-specific support. Other research has demonstrated the importance of these types of support in providing gender-affirmation and augmenting general support structures (Bockting et al., 2016; Pflum et al., 2015). Our findings show that losing access to LGBTQ/TGNB-specific supports was associated with greater psychological distress, even after controlling for pre-pandemic mental health symptoms. The loss of this type of support may represent a reduction in identity affirmation, which has been associated with resilience and decreased risk for mental health symptoms among TGNB individuals (Bockting et al., 2013; Budge et al., 2013; Budge et al., 2014; Pflum et al., 2015). Future research is needed to investigate how LGBTQ/TGNB-specific support services were impacted by the pandemic and to evaluate alternative (e.g., web-based) services for this population.
Nearly one-third of survey respondents reported an interruption/delay in gender-affirming hormone therapy; 11% reported having a gender-affirming surgery cancelled or postponed during the pandemic. These numbers were expected because hospitals throughout the U.S. cancelled non-emergent surgeries during the pandemic, including gender-affirming surgeries (COVIDSurg Collaborative, 2020). However, some advocates challenged the classification of gender-affirming surgeries as “elective” (Bellamy Walker, 2020; Clarendon, 2020; Savage & Banerji, 2020), citing the role of gender-affirming health care in reducing psychological distress associated with gender incongruence (i.e., gender dysphoria) and improving psychosocial functioning (Fisher et al., 2016; Murad et al., 2010; White Hughto & Reisner, 2016). Therefore, it was surprising to find that interruptions in gender-affirming care were not associated with greater psychological distress during the pandemic, after controlling for pre-pandemic mental health. While it is possible that we were underpowered to detect a significant association, it is also possible that pre-pandemic mental health is a more potent predictor of worsening mental health during the pandemic. Another potential explanation for this finding is that the majority of respondents who reported interruptions in care reported difficulty with access to hormones, and we were not able to ascertain the duration or type of interruption (e.g., receiving a refill two weeks late versus missing testosterone entirely for two months). The impact of interrupted gender-affirming health care might also be affected by the way healthcare providers discussed these delays with their patients (e.g., validation of distress and a plan to reschedule versus an automated voice message).
Limitations
This study has several limitations. First, while our retention rate was high at 76%, differential attrition could have impacted findings (particularly when comparing transmasculine and transfeminine individuals). It is possible that those most affected by the pandemic were less likely to respond to this survey. Second, survey measures were developed in the context of what was known about COVID-19 in March 2020. Since then, the CDC’s COVID-19 symptom list has expanded, COVID-19 diagnostic testing is more widely available, antibody testing is FDA-authorized, and local, state, and federal regulations designed to prevent the spread of COVID-19 continue to evolve. We also did not examine respondents’ political orientation, which may be correlated with views on the pandemic and public health measures taken to prevent its spread (Agley, 2020; Callow et al., 2020). This study uses self-report measures, which introduce the possibility of social desirability and recall bias. Our analysis also focused on formal LGBTQ/TGNB community supports and does not include more informal support from family and friends. Finally, this study relies on a non-probability sample from three U.S. cities, limiting generalizability to other groups of TGNB individuals.
Conclusion
This study examined the impact of the COVID-19 pandemic on a longitudinal cohort of TGNB individuals. We found that the pandemic exacerbated ongoing disparities for TGNB individuals (e.g., employment, mental health). TGNB individuals were also impacted in unique ways. Reductions in LGBTQ/TGNB community support predicted greater psychological distress during the pandemic. This finding is clinically relevant given the ongoing mental health disparities for TGNB individuals. Epidemiologic data collection during the ongoing pandemic must include information about gender identity in order to more precisely understand the impact on TGNB individuals. Furthermore, policy-makers tasked with developing programs to assist individuals during and after the pandemic should pay special attention to meeting the unique needs of TGNB individuals while also addressing the long-standing disparities that impact the health and wellbeing of TGNB individuals.
Acknowledgments:
The authors would like to thank the diverse community advisory board that advised on all aspects of the AFFIRM study. This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grants number R01 HD079603, Walter Bockting, PI). Dr. Kidd’s participation in this research was made possible through a training grant from the National Institute on Drug Abuse (T32-DA007294-24, Frances Levin, PI) and a career-development award from the National Institute on Alcohol Abuse and Alcoholism (K23-AA028296-01, Jeremy Kidd, PI). Dr. Jackman’s participation in this research was made possible through a training grant from the National Institute of Nursing Research (T32NR007969, Suzanne Bakken, PI).
Footnotes
Declaration of Interests: The authors have no conflicts of interest to disclose.
References
- Agley J (2020). Assessing changes in US public trust in science amid the COVID-19 pandemic. Public Health, 183, 122–125. 10.1016/j.puhe.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellamy Walker T (2020). Elective surgeries were postponed during the coronavirus outbreak But my gender-affirming surgery isn’t optional — it’s lifesaving. Insider, Inc. https://www.businessinsider.com/my-gender-affirming-surgery-isnt-elective-its-life-saving-2020-3 [Google Scholar]
- Bockting W, Coleman E, Deutsch MB, Guillamon A, Meyer I, Meyer W 3rd, Reisner S, Sevelius J, & Ettner R (2016). Adult development and quality of life of transgender and gender nonconforming people. Curr Opin Endocrinol Diabetes Obes, 23(2), 188–197. 10.1097/MED.0000000000000232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, & Coleman E (2013). Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health, 103(5), 943–951. 10.2105/AJPH.2013.301241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L (2020). We’re not all in this together: On COVID-19, intersectionality, and structural inequality. Am J Public Health, 110(7), 917 10.2105/AJPH.2020.305766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslow AS, Brewster ME, Velez BL, S. W, Geiger E, & Soderstrom B (2015). Resilience and collective action: Exploring buffers against minority stress for transgender individuals. Psychol Sex Orientat Gend Divers, 2, 253. [Google Scholar]
- Budge SL, Adelson JL, & Howard KA (2013). Anxiety and depression in transgender individuals: the roles of transition status, loss, social support, and coping. J Consult Clin Psychol, 81(3), 545–557. 10.1037/a0031774 [DOI] [PubMed] [Google Scholar]
- Budge SL, Rossman HK, & Howard KAS (2014). Coping and psychological distress among genderqueer individuals: The moderating effect of social support. J LGBT Issues Couns, 8(1), 95–117. 10.1080/15538605.2014.853641 [DOI] [Google Scholar]
- Callow MA, Callow DD, & Smith C (2020). Older adults’ intention to socially isolate once COVID-19 stay-at-home orders are replaced with “safer-at-home” public health advisories: A survey of respondents in Maryland. J Appl Gerontol, 39(11), 1175–1183. 10.1177/0733464820944704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). ICD-10-CM official coding guidelines - Supplemental coding encounters related to COVID-19 coronavirus outbreak: Feburary 20, 2020-March 31, 2020. https://www.cdc.gov/nchs/data/icd/interim-coding-advice-coronavirus-March-2020-final.pdf
- Clarendon D (2020). Gender affirming surgery is being delayed or canceled because of the coronavirus pandemic. Conde Nast. https://www.teenvogue.com/story/gender-affirming-surgery-coronavirus-pandemic [Google Scholar]
- Cohen W, Maisner RS, Mansukhani PA, & Keith J (2020). Barriers to finding a gender affirming surgeon. Aesthetic Plast Surg. e-pub ahead of print. 10.1007/s00266-020-01883-z [DOI] [PubMed] [Google Scholar]
- Colizzi M, Costa R, & Todarello O (2014). Transsexual patients’ psychiatric comorbidity and positive effect of cross-sex hormonal treatment on mental health: Results from a longitudinal study. Psychoneuroendocrinology, 39, 65–73. 10.1016/j.psyneuen.2013.09.029 [DOI] [PubMed] [Google Scholar]
- Costa R, & Colizzi M (2016). The effect of cross-sex hormonal treatment on gender dysphoria individuals’ mental health: A systematic review. Neuropsychiatr Dis Treat, 12, 1953–1966. 10.2147/NDT.S95310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVIDSurg Collaborative. (2020). Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br J Surg, 107, 1440–1449. 10.1002/bjs.11746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler ME, Lane RI, Petrosky E, Wiley JF, Christensen A, Njai R, Weaver MD, Robbins R, Facer-Childs ER, Barger LK, Czeisler CA, Howard ME, & Rajaratnam SMW (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep, 69(32), 1049–1057. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR (2001). Brief Symptom Index (BSI 18). National Computer Systems, Pearson Inc. [Google Scholar]
- Fisher AD, Castellini G, Ristori J, Casale H, Cassioli E, Sensi C, Fanni E, Amato AM, Bettini E, Mosconi M, Dettore D, Ricca V, & Maggi M (2016). Cross-sex hormone treatment and psychobiological changes in transsexual persons: Two-year follow-up data. J Clin Endocrinol Metab, 101(11), 4260–4269. 10.1210/jc.2016-1276 [DOI] [PubMed] [Google Scholar]
- Flaherty AJ, Sharma A, Crosby DL, & Nuara MJ (2020). Should gender-affirming surgery be prioritized during the covid-19 pandemic? Otolaryngol Head Neck Surg. e-pub ahead of print. 10.1177/0194599820939072 [DOI] [PubMed] [Google Scholar]
- Gorczynski P, & Fasoli F (2020). LGBTQ+ focused mental health research strategy in response to COVID-19. Lancet Psychiatry, 7(8), e56 10.1016/S2215-0366(20)30300-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness A, Behar-Zusman V, & Safren SA (2020). Understanding the impact of COVID-19 on Latino sexual minority men in a US HIV hot spot. AIDS Behav, 24(7), 2017–2023. 10.1007/s10461-020-02862-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison J, Grant J, & Herman JL (2011). A gender not listed here: Genderqueers, gender rebels, and otherwise in the national transgender discrimination survey. LGBTQ Policy Journal, 2, 13–24. [Google Scholar]
- Hendricks ML, & Testa RJ (2012). A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the minority stress model. Prof Psychol Res Pre, 43(5), 460–467. 10.1037/a00229597 [DOI] [Google Scholar]
- Herman JL, & O’Neill K (2020). Vulnerabilities to COVID-19 among transgender adults in the US. The Williams Institute, UCLA-School of Law; https://escholarship.org/content/qt55t297mc/qt55t297mc.pdf [Google Scholar]
- Jackman KB, Dolezal C, Levin B, Honig JC, & Bockting WO (2018). Stigma, gender dysphoria, and nonsuicidal self-injury in a community sample of transgender individuals. Psychiatry Res, 269, 602–609. 10.1016/j.psychres.2018.08.092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James SE, Herman JL, Rankin S, Kiesling M, Mottet L, & Anafi M (2016). The Report of the 2015 U.S. Transgender Survey. National Center for Transgender Equality; https://transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf [Google Scholar]
- Jones BA, Bouman WP, Haycraft E, & Arcelus J (2019). Mental health and quality of life in non-binary transgender adults: A case control study. Int J Transgend, 20(2–3), 251–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline NS (2020). Rethinking COVID-19 vulnerability: A call for LGTBQ+ im/migrant health equity in the United States during and after a pandemic. Health Equity, 4(1), 239–242. 10.1089/heq.2020.0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall E, Claes L, Bouman WP, Witcomb GL, & Arcelus J (2016). Non-suicidal self-injury and suicidality in trans people: A systematic review of the literature. Int Rev Psychiatry, 28(1), 58–69. 10.3109/09540261.2015.1073143 [DOI] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol Bull, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moradi B, Tebbe EA, Brewster ME, Budge SL, Lenze A, Ege E, Schuch E, Arango S, Angelone N, Mender E, Hiner DL, Huscher K, Painter J, & Flores MJ (2016). A content analysis of literature on trans people and issues: 2002–2012. Couns Psychol, 44(7), 960–995. [Google Scholar]
- Murad MH, Elamin MB, Garcia MZ, Mullan RJ, Murad A, Erwin PJ, & Montori VM (2010). Hormonal therapy and sex reassignment: A systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol (Oxf), 72(2), 214–231. 10.1111/j.1365-2265.2009.03625.x [DOI] [PubMed] [Google Scholar]
- National Academy of Medicine. (2011). The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, D.C.: The National Academies of Press. [PubMed] [Google Scholar]
- Newcomb ME, Hill R, Buehler K, Ryan DT, Whitton SW, & Mustanski B (2020). High burden of mental health problems, substance use, violence, and related psychosocial factors in transgender, nonbinary, and gender diverse youth and young adults. Arch Sex Behav, 49, 645–659. 10.1007/s10508-019-01533-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuttbrock L, Bockting W, Rosenblum A, Hwahng S, Mason M, Macri M, & Becker J (2014). Gender abuse, depressive symptoms, and substance use among transgender women: A 3-year prospective study. Am J Public Health, 104(11), 2199–2206. 10.2105/AJPH.2014.302106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padula WV, & Baker K (2017). Coverage for gender-affirming care: Making health insurance work for transgender Americans. LGBT Health, 4(4), 244–247. 10.1089/lgbt.2016.0099 [DOI] [PubMed] [Google Scholar]
- Pflum SR, Testa RJ, Balsam KF, Goldblum PB, & Bongar B (2015). Social support, trans community connectedness, and mental health symptoms among transgender and gender nonconforming adults. Psychol Sex Orientat Gend Divers, 2(3), 281–286. 10.1037/sgd0000122 [DOI] [Google Scholar]
- Reisner SL, Poteat T, Keatley J, Cabral M, Mothopeng T, Dunham E, Holland CE, Max R, & Baral SD (2016). Global health burden and needs of transgender populations: A review. Lancet, 388(10042), 412–436. 10.1016/S0140-6736(16)00684-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Vetters R, Leclerc M, Zaslow S, Wolfrum S, Shumer D, & Mimiaga MJ (2015). Mental health of transgender youth in care at an adolescent urban community health center: A matched retrospective cohort study. J Adolesc Health, 56(3), 274–279. 10.1016/j.jadohealth.2014.10.264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimes KA, Goodship N, G. U, Baker D, & West E (2017). Non-binary and binary transgender youth: Comparison of mental health, suicidality, substance use and victimization experiences. Int J Transgend, 20(2–3), 230–340. 10.1080/15532739.2017.1370627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rood BA, Reisner SL, Surace FI, Puckett JA, Maroney MR, & Pantalone DW (2016). Expecting rejection: Understanding the minority stress experiences of transgender and gender-nonconforming individuals. Transgend Health, 1(1), 151–164. 10.1089/trgh.2016.0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salerno JP, Williams ND, & Gattamorta KA (2020). LGBTQ populations: Psychologically vulnerable communities in the COVID-19 pandemic. Psychol Trauma, 12(S1), S239–S242. 10.1037/tra0000837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage R, & Banerji A (2020). Anxieties mount for trans people as coronavirus delays surgeries. Thomson Reuters Foundation. https://www.reuters.com/article/uk-health-coronavirus-lgbt-trfn/anxieties-mount-for-trans-people-as-coronavirus-delays-surgeries-idUSKCN21R3NJ
- Schmidt S (2020). Federal judge blocks Trump administration from ending transgender health-care protections. https://www.washingtonpost.com/dc-md-va/2020/08/17/federal-judge-blocks-trump-administration-ending-transgender-healthcare-protections/
- Sevelius JM, Gutierrez-Mock L, Zamudio-Haas S, McCree B, Ngo A, Jackson A, Clynes C, Venegas L, Salinas A, Herrera C, Stein E, Operario D, & Gamarel K (2020). Research with marginalized communities: Challenges to continuity during the COVID-19 pandemic. AIDS Behav, 24(7), 2009–2012. 10.1007/s10461-020-02920-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons-Duffin S (2020). Transgender Health Protections Reversed By Trump Administration. National Public Radio. https://www.npr.org/sections/health-shots/2020/06/12/868073068/transgender-health-protections-reversed-by-trump-administration
- Streed CG Jr., McCarthy EP, & Haas JS (2018). Self-reported physical and mental health of gender nonconforming transgender adults in the United States. LGBT Health, 5(7), 443–448. 10.1089/lgbt.2017.0275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tebbe EA, & Moradi B (2016). Suicide risk in trans populations: An application of minority stress theory. J Couns Psychol, 63(5), 520–533. 10.1037/cou0000152 [DOI] [PubMed] [Google Scholar]
- Thorne N, Witcomb GL, Nieder T, Nixon E, Yip A, & Arcelus J (2019). A comparison of mental health symptomatology and levels of social support in young treatment seeking transgender individuals who identify as binary and non-binary. Int J Transgend, 20(2–3), 241–250. 10.1080/15532739.2018.1452660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres TS, Hoagland B, Bezerra DRB, Garner A, Jalil EM, Coelho LE, Benedetti M, Pimenta C, Grinsztejn B, & Veloso VG (2020). Impact of COVID-19 pandemic on sexual minority populations in Brazil: An analysis of social/racial disparities in maintaining social distancing and a description of sexual behavior. AIDS Behav. e-pub ahead of print. 10.1007/s10461-020-02984-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics. (2020a). 19.2 percent of the unemployed had been jobless for 27 weeks or more in February 2020. https://www.bls.gov/opub/ted/2020/19-point-2-percent-of-the-unemployed-had-been-jobless-for-27-weeks-or-more-in-february-2020.htm#:~:text=In%20February%202020%2C%20the%20unemployment,19.2%20percent%20in%20February%202020.
- U.S. Bureau of Labor Statistics. (2020b). State employment and unemployment summary - July 2020. https://www.bls.gov/news.release/laus.nr0.htm
- U.S. Census Bureau. (2010). U.S. Census 2010. https://www.census.gov/2010census/pdf/2010_Questionnaire_Info.pdf
- U.S. Food and Drug Administration. (2020). qSARS-CoV-2 IgG/IgM Rapid Test. https://www.fda.gov/media/136622/download
- Valente PK, Schrimshaw EW, Dolezal C, LeBlanc AJ, Singh AA, & Bockting WO (2020). Stigmatization, resilience, and mental health among a diverse community sample of transgender and gender nonbinary individuals in the U.S. Arch Sex Behav, 49, 2649–2660. 10.1007/s10508-020-01761-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentine SE, & Shipherd JC (2018). A systematic review of social stress and mental health among transgender and gender non-conforming people in the United States. Clin Psychol Rev. 10.1016/j.cpr.2018.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Miesen AI, Raaijmakers D, & van de Grift TC (2020). “You have to wait a little longer”: Transgender (mental) health at risk as a consequence of deferring gender-affirming treatments during COVID-19. Arch Sex Behav, 49(5), 1395–1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Pan B, Liu Y, Wilson A, Ou J, & Chen R (2020). Health care and mental health challenges for transgender individuals during the COVID-19 pandemic. Lancet Diabetes Endocrinol, 8(7), 564–565. 10.1016/S2213-8587(20)30182-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White Hughto JM, & Reisner SL (2016). A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals. Transgend Health, 1(1), 21–31. 10.1089/trgh.2015.0008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Professional Association for Transgender Health. (2011). Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People (7th ed.). [Google Scholar]
- Yang MF, Manning D, van den Berg JJ, & Operario D (2015). Stigmatization and mental Health in a diverse sample of transgender women. LGBT Health, 2(4), 306–312. 10.1089/lgbt.2014.0106 [DOI] [PMC free article] [PubMed] [Google Scholar]


